Abstract
Bacillus collagen-like protein of anthracis (BclA) is an immunodominant glycoprotein located on the exosporium of Bacillus anthracis. We hypothesized that antibodies to this spore surface antigen are largely responsible for the augmented immunity to anthrax that has been reported for animals vaccinated with inactivated spores and protective antigen (PA) compared to vaccination with PA alone. To test this theory, we first evaluated the capacity of recombinant, histidine-tagged, nonglycosylated BclA (rBclA) given with adjuvant to protect A/J mice against 10 times the 50% lethal dose of Sterne strain spores introduced subcutaneously. Although the animals elicited anti-rBclA antibodies and showed a slight but statistically significant prolongation in the mean time to death (MTD), none of the mice survived. Similarly, rabbit anti-rBclA immunoglobulin G (IgG) administered intraperitoneally to mice before spore inoculation increased the MTD statistically significantly but afforded protection to only 1 of 10 animals. However, all mice that received suboptimal amounts of recombinant PA and that then received rBclA 2 weeks later survived spore challenge. Additionally, anti-rBclA IgG, compared to anti-PA IgG, promoted a sevenfold-greater uptake of opsonized spores by mouse macrophages and markedly decreased intramacrophage spore germination. Since BclA has some sequence similarity to human collagen, we also tested the extent of binding of anti-rBclA antibodies to human collagen types I, III, and V and found no discernible cross-reactivity. Taken together, these results support the concept of rBclA as being a safe and effective boost for a PA-primed individual against anthrax and further suggest that such rBclA-enhanced protection occurs by the induction of spore-opsonizing and germination-inhibiting antibodies.
Spores of Bacillus anthracis, the causative agent of anthrax, are the infectious form of the organism and can persist in soil in a dormant stage for decades (25). Although herbivores are the primary reservoir of anthrax, humans can contract anthrax, albeit rarely, if inoculated with spores cutaneously, orally, or inhalationally (8). Although anthrax is typically seen only in individuals involved in certain occupations, the potential for infection of larger numbers of people by the aerosol route is of public health concern because of the misuse of B. anthracis spores that occurred in the United States in 2001 (9).
One way to protect vulnerable individuals and populations against anthrax is through a strategy of prophylactic immunization. Currently, the anthrax vaccine adsorbed (AVA) preparation is the only licensed anthrax vaccine for use in the United States. AVA is comprised of a formalin-treated, aluminum salt-adsorbed, cell-free culture filtrate from an attenuated strain of B. anthracis (3). Although AVA is considered to be safe and effective, the utility of the vaccine is limited by its availability, reactogenicity, requirement for the administration of multiple doses (3), and the generally adverse publicity that the vaccine has received (32). AVA is considered to induce protection against anthrax primarily through the elicitation of an immune response to the protective antigen (PA) in the preparation (31, 32). Indeed, the strongest correlate of immunity to anthrax, although not considered a perfect association, is the level of antibodies to PA (26). Since PA serves as the cell-binding component for both edema factor and lethal factor (10) and because the lethality of anthrax is attributed primarily to toxemia (as well as septicemia) (25), elicitation of neutralizing antibodies to PA is considered to be key to the induction of immunity to anthrax. For these reasons, the next-generation anthrax vaccine will be based on PA (31, 32). However, the extent of protection provided by purified PA or recombinant PA (rPA) against lethal anthrax infection in several different animal models has proven to be variable (2, 12, 17, 19, 20, 34, 35). Indeed, findings from two groups (23, 34) strongly indicate that PA-based vaccines are less protective than live-spore vaccines against virulent strains of B. anthracis. Moreover, Brossier and colleagues demonstrated that formaldehyde-inactivated spores increased the protective efficacy of PA-based vaccines despite similar anthrax lethal toxin-neutralizing activities of sera from animals given PA alone versus those given PA plus formaldehyde-inactivated spores (4). Additionally, attenuated, nontoxinogenic, and nonencapsulated recombinant B. anthracis spore vaccines conferred better protection against lethal anthrax spore challenge than vegetative-cell vaccines (5, 18), observations that support a role for spore-associated antigen(s) in protective immunity. Since whole spore-based vaccines are not acceptable for human use in the United States, one alternative approach might be to incorporate individual spore antigens as additives or adjuncts to a PA-based vaccine.
To identify the best such spore antigen(s), we elected to first focus on immunogens that are located on the outermost surface of the spore. B. anthracis spores are covered with a loosely fitting balloon-like structure called the exosporium from which hair-like structures project (30). For our study here, we chose to first examine the major component of those exosporium appendages, the glycoprotein BclA. BclA stands for bacillus collagen-like protein of anthracis and was so named because of similarities in repeat region numbers and amino acid motifs with collagens. BclA is a particularly attractive target because the antibody response generated against spores is directed primarily against this molecule, specifically to its protein and not carbohydrate constituents (29). Moreover, Hahn et al. recently showed that immunization with a combination of PA- and BclA-encoding plasmids conferred significantly better protection than immunization with PA- or BclA-only-encoding plasmids in outbred mice challenged with the fully virulent Ames strain of B. anthracis (15).
In this investigation, we discovered that A/J mice immunized with nonglycosylated BclA (recombinant BclA [rBclA]) alone or given rabbit anti-rBclA immunoglobulin G (IgG) passively exhibited a statistically significant increase in mean time to death (MTD) after challenge with an otherwise lethal dose of B. anthracis Sterne spores. Furthermore, we observed that rBclA administered as a boost after primary immunization with suboptimal amounts of rPA conferred full protection against lethal anthrax spore challenge of A/J mice. Possibly as an explanation for this enhanced protection, we also found that rabbit anti-rBclA IgG enhanced opsonophagocytosis of spores by murine macrophages and inhibited intramacrophage spore germination. Lastly, and most critical for any possible future use of BclA as an anthrax vaccine adjunct or component, anti-rBclA antibodies did not react with human collagens.
MATERIALS AND METHODS
B. anthracis strain, preparation of spores, and spore surface protein extract (SSPE).
B. anthracis Sterne strain 34F2 was obtained from the Naval Medical Research Center. B. anthracis was induced to sporulate on Leighton-Doi medium (22). The broth was inoculated with a culture of B. anthracis cells grown overnight and incubated for 72 h at 30°C with slow agitation. The spores were harvested by centrifugation and resuspended in and then washed three times with sterile cold water. Spores were then purified through a Hypaque-76 gradient (Nycomed, Inc., Princeton, NJ), washed three times in cold sterile water, and stored at 4°C. Prior to use of spores for challenge of animals, an aliquot of the purified washed spores was heated at 65°C for 30 min, diluted, and plated onto trypticase soy agar to obtain viable counts. Since heat treatment kills the vegetative form but not the spore form of B. anthracis, the CFU of viable bacilli recovered after heat treatment reflect the number of spores within the sample.
SSPEs were derived by incubation of 109 spores in 1 ml of buffer that contained 0.1 M l-dithiothreitol, 0.5% sodium dodecyl sulfate, and 0.1 M NaCl (pH 10.0) at 37°C for 2 1/2 h essentially as outlined previously by Aronson and Fitz-James (1). The spores were then harvested by centrifugation at 16,000 × g for 10 min, and the supernatant that contained the SSPE was removed and stored at 4°C.
Preparation of rBclA.
Our procedures for the construction of a recombinant Escherichia coli strain that expresses rBclA with an N-terminal six-histidine tag and for purification of that protein by nickel affinity chromatography are also described in detail elsewhere (3a). In brief, we amplified the sequence of bclA from the Sterne strain by PCR based on primers designed from the sequence of the Ames strain (National Center for Biotechnology Information [NCBI] website at http://www.ncbi.nlm.nih.gov/entrez/viewer.fcgi?db=nucleotide&val=3026019), purified the PCR product, inserted the DNA fragment into the expression vector pET15b (Novagen, San Diego, CA), and then sequenced the gene in the resulting recombinant plasmid to verify that no changes had occurred during the PCR process. A bclA-containing plasmid was then transformed into E. coli BL21(DE3) pLysS according to the pET system manual (Novagen, San Diego, CA). The BclA protein with a six-His tag was expressed from that transformant and subjected to His-Trap nickel affinity column chromatography with the ÁKTA fast-phase liquid chromatography system (GE Healthcare, Piscataway, NJ).
Rabbit anti-rBclA and anti-PA IgG.
Preparation of rabbit anti-rBclA IgG has also been detailed (3a). Briefly, rabbits were vaccinated multiple times at monthly intervals with 50 ng of purified rBclA in Freund's complete adjuvant for the first inoculation and Freund's incomplete adjuvant for all subsequent immunizations. IgG fractions of the immune sera were obtained by passage over protein G columns. These anti-rBclA antibodies recognized rBclA, SSPEs of spores, and whole spores.
Human anti-PA IgG was prepared by two separate chromatography steps. First, IgG was isolated from the serum of an individual who had received the United Kingdom-licensed anthrax vaccine by passage of the serum through a protein A column (Pierce, Rockford, IL) according to the manufacturer's instructions (21). Second, the anti-PA component of that IgG fraction was isolated by binding to and elution from a PA affinity column. That affinity column was prepared by coupling 1 mg of B. anthracis rPA (kindly provided by Les Baillie, University of Maryland Biotechnology Institute) to 1 ml of EAH Sepharose 4B (GE Healthcare, Waukesha, WI [formerly Amersham Biosciences]) through a carbodiimide-mediated coupling reaction. The purified IgG obtained by elution from the protein A column was cycled three times through the washed PA-EAH Sepharose 4B affinity column to separate non-PA-specific IgG from PA-specific IgG. The affinity column was then washed with phosphate-buffered saline (PBS) (pH 7.4), and PA-specific IgG was eluted from the column with 0.15 M glycine-HCl (pH 2.5). The acidic fractions were immediately neutralized with 0.15 M Tris.
Animals, immunization, and challenge.
Six- to eight-week-old female A/J mice were obtained from Jackson Laboratories (Bar Harbor, ME) and quarantined for 1 week before use. Preimmune serum samples were collected from mice by tail nicks. The next day, the mice were immunized intraperitoneally with either PBS (pH 7.4), purified rPA (BEI Sciences, Manassas, VA), or rBclA in PBS mixed 1:1 with TiterMax Gold, a water-in-oil adjuvant (TiterMax USA Inc., Norcross, GA), in a total volume of 100 μl. The mice were bled on day 14 and boosted as described above on day 15. The mice were bled again on day 28 and challenged subcutaneously on day 29 with 10 times the 50% lethal dose (LD50) of Sterne spores (about 104 spores). The animals were then monitored twice daily for survival through day 15 after challenge.
ELISAs to measure anti-rPA and anti-rBclA antibodies.
Enzyme-linked immunosorbent assays (ELISAs) were done to assess anti-rPA and anti-rBclA mouse serum IgG responses. Purified rBclA or rPA (100 ng of each in 100 μl PBS) were used to coat the wells of a “U”-bottom 96-well microtiter plate (Thermo Electron Corp., Milford, MA), and the microtiter plates were incubated at 4°C overnight. The microtiter plates were then washed three times in PBS that contained 0.05% Tween 20 (PBST), and the sites on the wells to which antigen had not bound were blocked by incubation overnight at 4°C with 200 μl per well of PBST that contained 5% dry milk. Microtiter plate wells were washed again three times with PBST, and 100 μl of a single 1:100 dilution of each mouse pre- and postimmunization serum sample was then added to the appropriate well of the plate. Each mouse serum sample was tested in triplicate. The microtiter plates were then incubated for 2 h at 37°C, after which the wells of the plates were washed three times with PBST. Next, 100-μl aliquots of the secondary antibody, goat anti-mouse IgG conjugated to horseradish peroxidase (Bio-Rad, Hercules, CA) at a dilution of 1:10,000 in PBS, were added to wells that contained mouse serum or positive monoclonal antibodies (see below); the plates were then incubated at room temperature for 1 h. The secondary antibody was detected with 3,3′,5,5′-tetramethylbenzidine peroxidase (Bio-Rad, Hercules, CA), and the microtiter plates were incubated at room temperature for 15 min to permit color development. One hundred microliters of 1 M H2SO4 was then added to quench the reaction, and the intensity of the yellow in each well was measured by measuring the optical density at 450 nm (OD450) in an ELISA microtiter reader (Microtek; Molecular Devices, Sunnyvale, CA). The average intensity of the ELISA reading from the 1:100 dilution of each postimmune serum sample prepared in triplicate was determined after subtracting the average OD450 readings of triplicate 1:100 dilutions of preimmune serum from the same animal. (Note that none of the preimmune serum samples reacted more than threefold above the background.) The positive controls for the anti-rPA and anti-rBclA ELISAs were a monoclonal anti-PA antibody (14B7, originally prepared by S. Little and provided by the National Naval Medical Center) (24) and rabbit anti-rBclA antibody (IgG) diluted 1:5,000 and 1:10,000 in PBS, respectively.
Passive immunization.
For the preexposure prophylaxis experiment, 5- to 6-week-old female A/J mice (10 mice per group) were given a single intraperitoneally administered dose of either 0.1 ml of PBS, 0.5 mg in 0.1 ml of anti-rBclA IgG, or normal rabbit IgG 30 to 40 min prior to subcutaneous (back of neck) challenge with 1 × 104 (∼10 LD50s) of B. anthracis Sterne spores. All mice were observed for survival twice daily for 15 days postchallenge.
Effect of anti-rBclA antibody on uptake and killing of spores.
Thioglycolate-elicited peritoneal macrophages from Crl:CD-1 (ICR) BR mice (Charles River, Wilmington, ME) were collected, cultured, allowed to rest overnight, and infected with spores at a multiplicity of infection of 1 as detailed elsewhere previously (21); the number of macrophage-associated B. anthracis spores was determined as described previously (21). Reagents used for these studies included RPMI 1640 (Gibco-BRL, Frederick, MD), fetal bovine serum (Atlanta Biologicals, Lawrenceville, GA), gentamicin, and PBS (both purchased from Biosource International, Rockville, MD). Thioglycolate Medium, Brewer Modified, was obtained from Becton Dickinson (Cockeysville, MD). For these experiments, spores were mixed in 100-μl aliquots (106 spores) with an equal volume of 40 μg/ml of anti-rBclA IgG or anti-rPA IgG in RPMI or 100 μl RPMI alone and incubated at 4°C for 30 min on a rotator. Opsonized spores were then added to the macrophages. The infected macrophages were then incubated at 37°C in 5% CO2 for 30 min to allow phagocytosis of the treated spores to occur in RPMI medium without fetal bovine serum or antibiotics. As an additional control, spores were mixed, as described above, with 20 μl of complement (baby rabbit complement; Cedarlane, Westbury, NY) and then added to the macrophages. The infected macrophages were washed and incubated for another 30 min in the presence of gentamicin to kill any extracellular vegetative B. anthracis. The macrophages were then washed further and lysed with cold distilled water, and viable CFU were determined. Aliquots from each sample were also incubated at 65°C for 30 min prior to plate counting to ascertain the number of ungerminated intracellular spores. Additional experiments, in which intracellular germination of spores was monitored in macrophages incubated in the presence of gentamicin for an additional 4 or 24 h, were also done.
Study of cross-reactivity of rBclA with human collagens.
An ELISA was designed to assess any cross-reactivity between BclA and human collagen types I, III, and V. For this purpose, purified rBclA, SSPEs, whole spores, or human collagen type I, type III, or type V (100 ng in 100 μl PBS) was used to coat the wells of a U-bottom 96-well microtiter plate (Thermo Electron Corp., Milford, MA). These microtiter plates were incubated at 4°C overnight. The next day, the plates were washed three times in PBST, and the wells were the blocked overnight at 4°C with 200 μl per well of PBST that contained 5% dry milk. Primary antibodies for this ELISA included an anti-BclA monoclonal antibody (EG4; Critical Reagent Program, U.S. Department of Defense), rabbit anti-rBclA IgG (as described above), an anti-spore rabbit polyclonal antibody (designated 733 and kindly provided by Susan Welkos, USAMRIID) that recognizes primarily BclA, and rabbit anti-human collagen type I, III, and V sera (Chemicon, Temecula, CA). Dilutions of these antibodies (1:10,000 for anti-human collagen types I and V, anti-rBclA IgG, and 733 and 1:5,000 for anti-human collagen type III and EG4) were added to the appropriate wells, and the microtiter plates were incubated for 2 h at 37°C. Antibody dilutions were selected based on the manufacturer's recommendations (the anti-collagen antibodies) or because they were several dilutions below the titer against the homologous immunogen (for example, an anti-rBclA IgG ELISA titer against rBclA of ≥1:200,000). The wells of the plates were then washed three times with PBST. Next, 100 μl of the appropriate secondary antibody, goat anti-mouse or goat anti-rabbit IgG conjugated to horseradish peroxidase, was added at a dilution of 1:10,000 in PBS, and the plates were incubated at room temperature for 1 h. Substrate addition and color development were performed as detailed above in the description of the anti-rBclA and anti-rPA ELISA.
RESULTS
Recombinant BclA is immunogenic but not protective, when given alone, against spore challenge.
We initiated our search for a recombinant spore protein that might serve as an additive to or a booster for a PA-based vaccine by focusing on rBclA. Our reasons for this selection were twofold. First, BclA is the most immunogenic protein on the spore surface (28). Second, BclA is in the outermost substance on the exosporium and, therefore, most readily targeted by the host immune system.
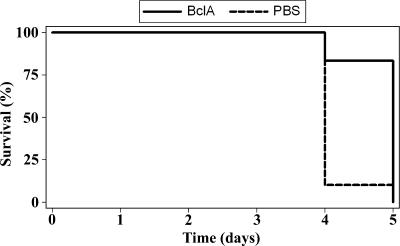
When rBclA was injected intraperitoneally into A/J mice with Titermax Gold, all animals developed a strong antibody response as measured by ELISA (average OD450 reading for six mice by ELISA of 1.6 [range, 1.0 to 2.1]). However, when the same group of animals was challenged with 10 LD50s of Sterne strain spores, none of the animals survived, although the MTD was slightly but statistically significantly prolonged compared to those of unimmunized controls (Fig. 1). Thus, rBclA alone, although immunogenic, cannot function as a vaccine to protect against anthrax in this animal model.
FIG. 1.
Time to death of A/J mice after immunization with rBclA (alone) followed 4 weeks later by subcutaneous challenge with 10 LD50s of B. anthracis Sterne strain 34F2 spores (∼104 spores). The MTD for the vaccinated group was 4.8 days; the MTD for the group given PBS (mixed 1:1 with Titermax) was 4.1 days. This difference in the MTD was statistically significant (P = 0.0045) by the Kaplan-Meier test. The average anti-rBclA ELISA OD450 response for a 1:100 serum dilution of the rBclA-immunized mouse group was 1.6 (data not shown).
Preexposure passive therapy with high-titer rabbit anti- rBclA IgG prolongs MTD of spore-challenged mice.
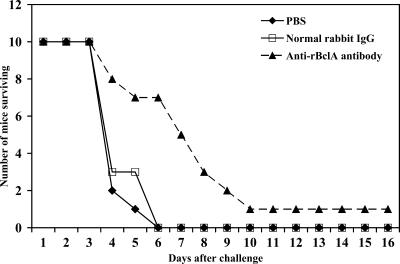
We then asked whether anti-rBclA could protect or increase the MTD when given immediately prior to spore challenge. Three groups of 10 mice each were intraperitoneally injected with PBS, 0.5 mg of normal IgG derived from rabbit serum, or anti-rBclA IgG. After a 30- to 40-min interval, these mice were challenged subcutaneously with 10 times the lethal dose of B. anthracis Sterne strain spores (1 × 104 spores). All of the control mice (one group given PBS and one group given normal rabbit serum IgG) died by day 6 (MTD of 4.3 days for both control groups), but the mice injected with anti-rBclA IgG survived statistically significantly longer (MTD of 6.8 days [P = 0.0002 as determined by the Kaplan-Meier test]) than did either of the control groups. In fact, 1 of 10 mice administered rabbit anti-rBclA IgG was alive at the time (15 days) that the study was terminated (Fig. 2). Thus, our findings from both active immunization with rBclA and passive administration of anti- rBclA IgG indicate that anti-rBclA antibodies extend the survival of mice challenged with anthrax spores.
FIG. 2.
Impact of administration of rabbit anti-rBclA IgG given 1 h before subcutaneous challenge of A/J mice with 10 LD50s of B. anthracis Sterne strain 34F2 spores (∼104 spores) on animal survival. The MTD of mice given PBS or passively administrated normal rabbit IgG before spore challenge was 4.3 days for each group, compared to 6.8 days for mice that received rabbit anti-rBclA IgG. This difference in MTD was statistically significant as assessed by the Kaplan-Meier test (P = 0.0002).
Priming with suboptimal levels of PA followed by rBclA fully protects mice from spore challenge.
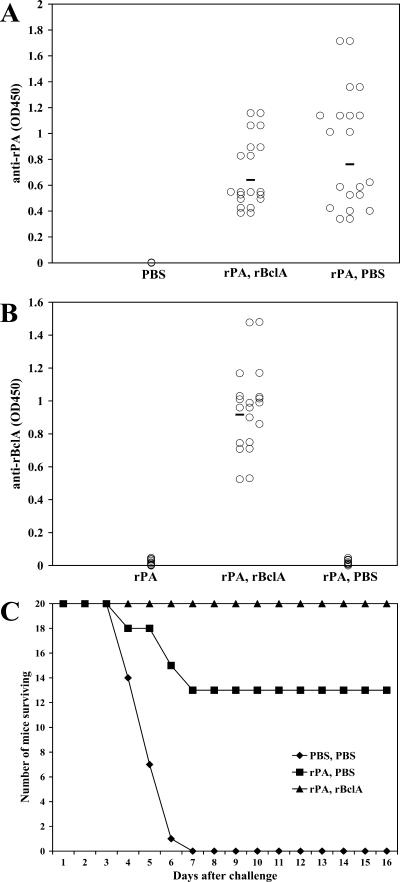
Next, we sought to assess whether mice immunized with a suboptimal concentration of rPA could be protected from anthrax spore challenge by the incorporation of rBclA into the immunization schedule. For that purpose, we first immunized groups of mice with different concentrations of rPA and challenged them with spores. We determined that a single 50-ng dose of rPA protected approximately 50% of the mice (data not shown) upon spore challenge. We then immunized mice with 50 ng of rPA (the suboptimal dose) and 10 μg rBclA. When given with rBclA, rPA-immunized mice did not elicit the same ELISA OD450 intensity of anti-rPA antibodies as they did when rPA was given alone (the average anti-rPA OD450 reading when rPA was given alone was 1.5; the average OD450 reading when rPA was given with rBclA was 1.1). Also, and perhaps because of the less intense rPA antibody response, the mice that were immunized with both antigens simultaneously were not protected from anthrax spore challenge (0/10 survivors). Next, we immunized mice with rPA and administered a booster with rBclA at 2 weeks. When this immunization schedule was followed, the mice developed an adequate antibody response to rPA (Fig. 3A) as well as antibodies to rBclA (Fig. 3B), and, most importantly, the animals were fully protected (Fig. 3C). This rBclA-mediated boost in protection compared to protection of mice given suboptimal amounts of rPA alone was statistically significant (P = 0.001). Therefore, we conclude that immunization with suboptimal amounts of the vegetative antigen PA followed by a boost with the exosporium antigen rBclA is a protective anthrax vaccine regimen in this mouse model.
FIG. 3.
Protection of A/J mice primed with suboptimal amounts of PA (mixed 1:1 with Titermax) and boosted with rBclA (mixed 1:1 with Titermax) from subcutaneous challenge with 10 LD50s of B. anthracis Sterne strain 34F2 spores (∼104 spores). A/J mice were injected with 50 ng of rPA or PBS as a control (each mixed 1:1 with Titermax), which was followed 2 weeks later with PBS or 10 μg of rBclA (each mixed 1:1 with Titermax). Spores were administered 2 weeks after the rBclA or PBS boost. (A and B) Individual mouse antibody ELISA OD450 responses against rPA (A) or rBclA (B). (C) Survival curve after subcutaneous challenge with 10 LD50s of B. anthracis Sterne strain 34F2 spores (∼104 spores) (P = 0.001). Each circle represents the average of triplicate OD450 values of a 1:100 dilution of postimmune serum from which average preimmune values were subtracted for that mouse. Horizontal bars represent the average OD450 reading of that immunization group.
Inhibitory effect of anti-rBclA antibody on germination in macrophages.
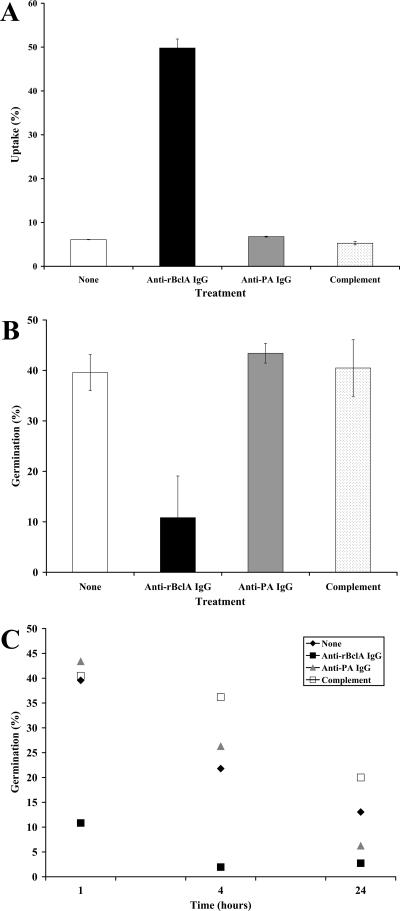
B. anthracis spores are believed to germinate within macrophages (14, 16). Since anti-rBclA antibodies are directed against the outermost component of the exosporium, such antibodies might contribute to protection against anthrax by functioning as opsonins that increase the uptake and perhaps even killing of spores in macrophages. To test this theory, we studied the effect of anti-rBclA IgG on the opsonization and germination of spores in mouse peritoneal macrophages. The macrophages were cultured with B. anthracis Sterne spores (multiplicity of infection of 1) in the presence of 40 μg of anti-rBclA IgG or anti-PA IgG as a control. Anti-rBclA IgG increased spore uptake by macrophages sevenfold over that of anti-PA IgG under our experimental conditions (Fig. 4A). Moreover, the degree of spore germination within 1 h (i.e., an initial period of 30 min to permit uptake of spores by the macrophages and an additional 30 min for incubation of the infected macrophages in medium with gentamicin to kill any extracellular B. anthracis) was assessed by heat treatment of the samples obtained. In the macrophages exposed to spores treated with anti-PA IgG, intracellular germinated spores represented approximately 40% of the total interacting spores and were not different than untreated- or complement-treated spores (Fig. 4B). However, in the macrophages exposed to spores mixed with anti-rBclA IgG, only 10% of the phagocytized spores germinated (Fig. 4B). Furthermore, as shown in Fig. 4C, intracellular germination of spores opsonized with anti-rBclA IgG remained minimal in macrophages cultured for 4 and for 24 h (germination of intracellular spores/vegetative outgrowth, as assessed by heat-sensitive bacterial counts over total counts, were 2% and 3%, respectively, at those time points) compared to that of spores treated with anti-PA IgG (26% and 6% for 4 and 24 h of macrophage incubation, respectively). These results indicate that anti-rBclA IgG has both an opsonizing effect and a sustained germination-inhibiting effect on spores within macrophages maintained in vitro.
FIG. 4.
Enhanced opsonophagocytosis and killing of B. anthracis Sterne strain 34F2 spores by mouse peritoneal macrophages when spores were incubated with rBclA IgG. (A) Uptake of spores treated with either anti-PA IgG, anti-rBclA IgG, complement, or nothing by macrophages after 1 h of incubation. (B) Intracellular germination of spores treated as described above after 1 h of incubation with macrophages. (C) Intramacrophage germination of treated spores over time (1-h time point shown in B is included here for estimation of rates). Data in A to C were obtained from three independent experiments, each done in duplicate. Data in A and B are shown as means ± standard deviations of values.
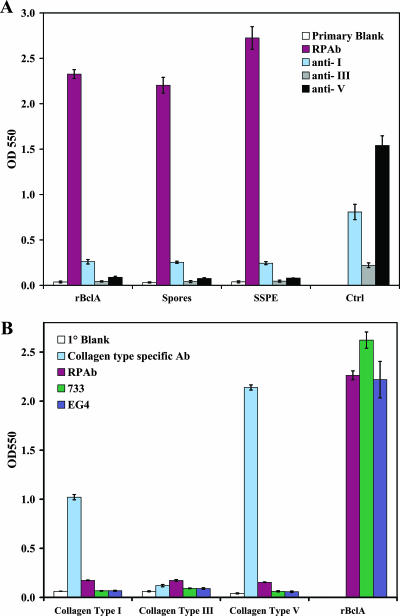
Lack of cross-reactivity between BclA and human collagens.
Although BclA does not have overall amino acid similarity to human collagen, this exosporium glycoprotein does contain repeated sequences of amino acids that resemble motifs found in human collagen. Indeed, the name bacillus collagen-like protein of anthracis was derived based on these similarities. To address the possibility that BclA and human collagens are cross-reactive, a finding that would rule out any use of the exosporium antigen in a next-generation anthrax vaccine, we did a series of ELISA tests. We found that antibodies made by the inoculation of spores or rBclA did not cross-react with human collagen (Fig. 5A), nor did anti-human collagen (types I, III, and V) antibodies bind to spores, SSPE, or rBclA (Fig. 5B). We surmise that the administration of rBclA to humans should not lead to an autoimmune response to collagens.
FIG. 5.
Absence of cross-reactivity between anti-rBclA antibodies and human collagen. (A) Anti-human-collagen (types I, III, and V) antibodies did not bind to spores, SSPE, or rBclA. (B) Antibodies made by inoculation of spores or rBclA did not cross-react with human collagen types I, III, and V. Abbreviations: RPAb, anti-rBclA rabbit polyclonal antibody; αI, anti-collagen I antibody; αIII, anti-collagen III antibody; αV, anti-collagen V antibody; 733, rabbit antispore antibody; EG4, monoclonal anti-BclA antibody. Samples were tested in triplicate. Bars shown are means ± standard deviations of values.
DISCUSSION
The major finding in this study was that a specific spore surface antigen, rBclA, augmented the protection afforded by rPA against anthrax in a mouse model. The supplementary protection provided by boosting rPA-primed mice with rBclA correlated with the capacity of active immunization with rBclA or passive administration of anti-rBclA rabbit IgG to prolong the MTD of spore-challenged mice. Furthermore, an explanation of the impact of rBclA IgG on immunity was provided by the observation that such antibodies enhance the opsonophagocytosis of spores by mouse macrophages while concomitantly decreasing intracellular spore germination. The importance of the latter observation cannot be overstated because spore germination within macrophages is considered to be a key step in the pathogenesis of anthrax. In support of the possible use of this spore surface-based antigen as a boost for a PA-based antianthrax vaccine for humans, we detected little or no cross-reactivity between rBclA and human collagen types I, III, and V.
Our observation that anti-rBclA IgG led to a prolongation in the MTD of anthrax spore-challenged mice is consistent with data from a recent report by Enkhtuya et al. (11). Those investigators demonstrated protection of mice from anthrax by passive immunization of the animals with anti-spore IgG isolated from immune sera of rabbits inoculated multiple times with formalin-fixed spores of a nonencapsulated, nontoxinogenic B. anthracis mutant strain. By Western blotting, those antispore antibodies recognized a number of spore surface antigens (11), and one of the immunoreactive proteins was consistent in mass with glycosylated BclA (∼250 kDa). We speculate that part if not most of the dose-dependent protection against anthrax spore challenge afforded the mice passively immunized with anti-spore IgG in the investigation by Enkhtuya and colleagues (11) likely resulted from the anti-BclA component of that IgG.
The mechanism by which our anti-rBclA IgG prolonged the survival of B. anthracis spore-challenged mice was not defined in this study. Nevertheless, based on our in vitro data that showed enhanced uptake and reduced spore germination within murine macrophages after opsonization with this IgG, we propose the following model. Anti-rBclA antibodies bind to the hair-like structures on the outside of spores and act as opsonins to enhance spore uptake by phagocytic cells. Within the macrophages, the tightly bound antibodies to BclA hinder the access of germinants to germinant receptors and decrease the extent of spore germination. In turn, such an anti-rBclA IgG-mediated reduction in intramacrophage spore germination leads to a delay in vegetative cell formation and, consequently, a later onset of lethal and edema toxin production and a subsequent extension of the time until death. In fact, we speculate that if enough antibodies were given before challenge, one might see survival of a substantial fraction of challenged animals, as did Enkhtuya and coworkers when they administered 0.5 mg anti-spore IgG per mouse (11). The observations of Enkhtuya et al., that anti-spore IgG is opsonic and promotes a reduction in germination of spores in macrophages, are strikingly similar to our results in comparable assays with anti-rBclA IgG. Again, the anti-spore IgG used by Enkhtuya et al. and coworkers appeared to recognize BclA and therefore had an anti-BclA component. Lastly, Welkos et al. previously showed that antispore serum reduces the extent of germination in vitro (34). Therefore, our results, taken with the previously described observations of Enkhtuya et al. and Welkos and colleagues, support the idea that antispore antibodies, particularly those directed against the outermost component of the exosporium, can reduce the total load of spores capable of germinating to become toxin-expressing vegetative cells and/or delay the onset of germination.
Our findings with anti-PA IgG as an opsonin of Sterne strain spores reveal, at most, a small antigerminating effect at 24 h (but not 1 or 4 h) of incubation of anti-PA IgG-treated spores in thioglycolate-elicited peritoneal murine macrophages compared to untreated spores ingested by the same type of macrophages (Fig. 4C). The absence of a significant impact of anti-PA IgG on intramacrophage spore germination is in contrast to a report by Cote and colleagues (6), who showed that anti-PA antibodies enhanced the uptake and germination of Ames spores by RAW 264.7 murine macrophages. The reasons for the discrepancy between their results and ours is not clear but may reflect variations in methods or reagents used by the two groups, e.g., spore strain, method of spore preparation, or type of macrophage used in the assay. Our data are, however, consistent with previous reports from one of us (21, 27, 33), who used the same type of macrophages and anti-spore-germination assay system that was employed in this investigation. Regardless of the reasons for the discordance of our results with those of the previous report by Cote and coworkers (6) on the antigerminating capacity of anti-PA antibodies, the findings here indicate that anti-rBclA IgG is a much more effective spore opsonin and antigermination inducer in macrophages than is anti-PA IgG.
Immunization with rBclA led to a slight but significant prolongation in MTD after spore challenge of A/J mice, but that immunogen alone was not protective. The failure to fully protect animals with such a spore surface-based antigen is not surprising given the requirement in most animal model systems to stimulate antitoxin immunity through inoculation with PA, the cell-binding component for edema factor and lethal factor (4). Our ability to protect mice by first immunizing them with suboptimal doses of PA supports the observation by Brossier et al., who reported previously that 100% of mice immunized with PA and formaldehyde-inactivated spores were spared from an otherwise lethal challenge with anthrax spores (4). Additionally, and more directly related to our findings, Hahn and colleagues reported that immunization with a combination of PA- and BclA-encoding DNA led to significantly better survival of outbred NMRI mice challenged with fully virulent Ames strain spores than did immunization with only PA- or only BclA-encoding plasmids (15). Nevertheless, the best protection afforded mice in that study was seen with live Sterne strain spores (avirulent for the NMRI mice that they used in their study) and rPA. That observation not withstanding, Sterne spores, whether live or irradiated, are not likely to be a component of any future anthrax vaccine for use in humans in the United States.
Although the methodology used by Hahn and colleagues (15) differed from ours in several ways, i.e., type of immunogen employed (DNA-based versus protein-based vaccine), sensitivity of animal model (NMRI mice versus A/J mice), and rigor of challenge (Ames versus Sterne), their findings and ours led to the same conclusion: rBclA augments PA-based protection against anthrax spore challenge in a sensitive animal system. One major difference between our data and theirs is that we observed an rBclA-mediated additive protective effect only when we gave that immunogen after inoculation of suboptimal concentrations of rPA. (Note that we used suboptimal doses of rPA so as to see augmentation of protection; a single higher dose of rPA in A/J mice is protective.) In fact, when we immunized mice with 50 ng of rPA and 10 μg of rBclA together, the average anti-rPA antibody reactivity, as measured by OD450 in an ELISA, was lower than the anti-rPA antibody response from mice given rPA alone. We interpreted that result to mean that the coadministration of such different concentrations of rPA and rBclA dampened the PA response. Although we did try a number of different regimens (lower doses of rBclA [0.1 to 5 μg]) (data not shown) given simultaneously with 50 ng of rPA, none of the schemes worked as well as our protocol of priming with suboptimal PA and boosting with rBclA. With this immunization strategy, we not only observed higher antibody responses to rPA but also saw full protection of mice. One potential means of reducing the level of BclA needed (and then perhaps vaccinating concomitantly with PA) is to substitute rBclA with the native glycosylated form of the immunogen expressed from B. anthracis. We have initiated studies to express and purify such an immunogen, and we also intend to assess the degree of protection afforded by vaccination of more resistant mice than the A/J strain with rBclA or glycosylated rBclA and PA followed by challenge with the fully virulent Ames strain.
For several autoimmune diseases, and specifically rheumatoid arthritis and systemic lupus erythematosus, common themes are the abnormal appearance of collagen within diseased sites and the presence of anticollagen antibodies in the patient's serum (13). Moreover, autoimmune diseases can be induced in experimental animals after exposure to collagen (7). Since BclA shares some sequence patterns with human collagens, we asked whether any anti-human-collagen antibodies might be elicited by inoculation of animals with rBclA. We found no evidence that antispore or anti-rBclA antibodies cross-reacted with human collagen type I, III, or V. We also observed no reactivity between anti-human-collagen antibodies obtained commercially and whole spores, SSPEs, or rBclA. In sum, rBclA appears to be a safe spore-associated antigen that could serve as a PA-based vaccine boost or, if conditions for PA and rBclA coadministration can be developed, perhaps even an additional component of a PA vaccine.
Acknowledgments
This work was supported by NIAID-NIH grant AI53397, NIAID-NIH Middle Atlantic Regional Centers for Excellence grant U54 AI57168, and USUHS grant G173HS.
We thank Cara Olsen, the USUHS Biostatistician, for expert statistical analysis.
The opinions and assertions in this paper are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Navy or the Department of Defense. This research was conducted in compliance with the Animal Welfare Act. All animal use protocols were reviewed and approved by the Institutional Animal Care and Use Committee of the Uniformed Services University.
Editor: R. P. Morrison
Footnotes
Published ahead of print on 4 September 2007.
REFERENCES
- 1.Aronson, A. I., and P. Fitz-James. 1976. Structure and morphogenesis of the bacterial spore coat. Bacteriol. Rev. 40:360-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bozue, J. A., N. Parthasarathy, L. R. Phillips, C. K. Cote, P. F. Fellows, I. Mendelson, A. Shafferman, and A. M. Friedlander. 2005. Construction of a rhamnose mutation in Bacillus anthracis affects adherence to macrophages but not virulence in guinea pigs. Microb. Pathog. 38:1-12. [DOI] [PubMed] [Google Scholar]
- 3.Brachman, P. S., H. Gold, S. A. Plotkin, F. R. Fekety, M. Werrin, and N. R. Ingraham. 1962. Field evaluation of a human anthrax vaccine. Am. J. Public Health 52:632-645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3a.Brahmbhatt, T. N, B. K. Janes, E. S. Stibitz, S. C. Darnell, P. Sanz, S. B. Rasmussen, and A. D. O'Brien. 2007. Bacillus anthracis exosporium protein BclA affects spore germination, interaction with extracellular matrix proteins, and hydrophobicity. Infect. Immun. 75:5233-5239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brossier, F., M. Levy, and M. Mock. 2002. Anthrax spores make an essential contribution to vaccine efficacy. Infect. Immun. 70:661-664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen, S., I. Mendelson, Z. Altboum, D. Kobiler, E. Elhanany, T. Bino, M. Leitner, I. Inbar, H. Rosenberg, Y. Gozes, R. Barak, M. Fisher, C. Kronman, B. Velan, and A. Shafferman. 2000. Attenuated nontoxinogenic and nonencapsulated recombinant Bacillus anthracis spore vaccines protect against anthrax. Infect. Immun. 68:4549-4558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cote, C. K., C. A. Rossi, A. S. Kang, P. R. Morrow, J. S. Lee, and S. L. Welkos. 2005. The detection of protective antigen (PA) associated with spores of Bacillus anthracis and the effects of anti-PA antibodies on spore germination and macrophage interactions. Microb. Pathog. 38:209-225. [DOI] [PubMed] [Google Scholar]
- 7.Cremer, M. A., E. F. Rosloniec, and A. H. Kang. 1998. The cartilage collagens: a review of their structure, organization, and role in the pathogenesis of experimental arthritis in animals and in human rheumatic disease. J. Mol. Med. 76:275-288. [DOI] [PubMed] [Google Scholar]
- 8.Dixon, T. C., M. Meselson, J. Guillemin, and P. C. Hanna. 1999. Anthrax. N. Engl. J. Med. 341:815-826. [DOI] [PubMed] [Google Scholar]
- 9.Doolan, D. L., D. A. Freilich, G. T. Brice, T. H. Burgess, M. P. Berzins, R. L. Bull, N. L. Graber, J. L. Dabbs, L. L. Shatney, D. L. Blazes, L. M. Bebris, M. F. Malone, J. F. Eisold, A. J. Mateczun, and G. J. Martin. 2007. The US Capitol bioterrorism anthrax exposures: clinical epidemiological and immunological characteristics. J. Infect. Dis. 195:174-184. [DOI] [PubMed] [Google Scholar]
- 10.Elliott, J. L., J. Mogridge, and R. J. Collier. 2000. A quantitative study of the interactions of Bacillus anthracis edema factor and lethal factor with activated protective antigen. Biochemistry 39:6706-6713. [DOI] [PubMed] [Google Scholar]
- 11.Enkhtuya, J., K. Kawamoto, Y. Kobayashi, I. Uchida, N. Rana, and S. Makino. 2006. Significant passive protective effect against anthrax by antibody to Bacillus anthracis inactivated spores that lack two virulence plasmids. Microbiology 152:3103-3110. [DOI] [PubMed] [Google Scholar]
- 12.Fellows, P. F., M. K. Linscott, B. E. Ivins, M. L. Pitt, C. A. Rossi, P. H. Gibbs, and A. M. Friedlander. 2001. Efficacy of a human anthrax vaccine in guinea pigs, rabbits, and rhesus macaques against challenge by Bacillus anthracis isolates of diverse geographical origin. Vaccine 19:3241-3247. [DOI] [PubMed] [Google Scholar]
- 13.Gioud, M., A. Meghlaoui, O. Costa, and J. C. Monier. 1982. Antibodies to native type I and II collagens detected by an enzyme linked immunosorbent assay (ELISA) in rheumatoid arthritis and systemic lupus erythematosus. Coll. Relat. Res. 2:557-564. [DOI] [PubMed] [Google Scholar]
- 14.Guidi-Rontani, C., M. Weber-Levy, E. Labruyere, and M. Mock. 1999. Germination of Bacillus anthracis spores within alveolar macrophages. Mol. Microbiol. 31:9-17. [DOI] [PubMed] [Google Scholar]
- 15.Hahn, U. K., R. Boehm, and W. Beyer. 2006. DNA vaccination against anthrax in mice—combination of anti-spore and anti-toxin components. Vaccine 24:4569-4571. [DOI] [PubMed] [Google Scholar]
- 16.Hanna, P. C., D. Acosta, and R. J. Collier. 1993. On the role of macrophages in anthrax. Proc. Natl. Acad. Sci. USA 90:10198-10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ivins, B., P. Fellows, L. Pitt, J. Estep, J. Farchaus, A. Friedlander, and P. Gibbs. 1995. Experimental anthrax vaccines: efficacy of adjuvants combined with protective antigen against an aerosol Bacillus anthracis spore challenge in guinea pigs. Vaccine 13:1779-1784. [DOI] [PubMed] [Google Scholar]
- 18.Ivins, B. E., J. W. Ezzell, Jr., J. Jemski, K. W. Hedlund, J. D. Ristroph, and S. H. Leppla. 1986. Immunization studies with attenuated strains of Bacillus anthracis. Infect. Immun. 52:454-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ivins, B. E., M. L. Pitt, P. F. Fellows, J. W. Farchaus, G. E. Benner, D. M. Waag, S. F. Little, G. W. Anderson, Jr., P. H. Gibbs, and A. M. Friedlander. 1998. Comparative efficacy of experimental anthrax vaccine candidates against inhalation anthrax in rhesus macaques. Vaccine 16:1141-1148. [DOI] [PubMed] [Google Scholar]
- 20.Ivins, B. E., S. L. Welkos, S. F. Little, M. H. Crumrine, and G. O. Nelson. 1992. Immunization against anthrax with Bacillus anthracis protective antigen combined with adjuvants. Infect. Immun. 60:662-668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kang, T. J., M. J. Fenton, M. A. Weiner, S. Hibbs, S. Basu, L. Baillie, and A. S. Cross. 2005. Murine macrophages kill the vegetative form of Bacillus anthracis. Infect. Immun. 73:7495-7501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leighton, T. J., and R. H. Doi. 1971. The stability of messenger ribonucleic acid during sporulation in Bacillus subtilis. J. Biol. Chem. 246:3189-3195. [PubMed] [Google Scholar]
- 23.Little, S. F., and G. B. Knudson. 1986. Comparative efficacy of Bacillus anthracis live spore vaccine and protective antigen vaccine against anthrax in the guinea pig. Infect. Immun. 52:509-512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Little, S. F., S. H. Leppla, and E. Cora. 1988. Production and characterization of monoclonal antibodies to the protective antigen component of Bacillus anthracis toxin. Infect. Immun. 56:1807-1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mock, M., and A. Fouet. 2001. Anthrax. Annu. Rev. Microbiol. 55:647-671. [DOI] [PubMed] [Google Scholar]
- 26.Pittman, P. R., S. L. Norris, J. G. Barrera Oro, D. Bedwell, T. L. Cannon, and K. T. McKee, Jr. 2006. Patterns of antibody response in humans to the anthrax vaccine adsorbed (AVA) primary (six-dose) series. Vaccine 24:3654-3660. [DOI] [PubMed] [Google Scholar]
- 27.Raines, K. W., T. J. Kang, S. Hibbs, G. L. Cao, J. Weaver, P. Tsai, L. Baillie, A. S. Cross, and G. M. Rosen. 2006. Importance of nitric oxide synthase in the control of infection by Bacillus anthracis. Infect. Immun. 74:2268-2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Steichen, C., P. Chen, J. F. Kearney, and C. L. Turnbough, Jr. 2003. Identification of the immunodominant protein and other proteins of the Bacillus anthracis exosporium. J. Bacteriol. 185:1903-1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steichen, C. T., J. F. Kearney, and C. L. Turnbough, Jr. 2005. Characterization of the exosporium basal layer protein BxpB of Bacillus anthracis. J. Bacteriol. 187:5868-5876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sylvestre, P., E. Couture-Tosi, and M. Mock. 2002. A collagen-like surface glycoprotein is a structural component of the Bacillus anthracis exosporium. Mol. Microbiol. 45:169-178. [DOI] [PubMed] [Google Scholar]
- 31.Turnbull, P. C. 2000. Current status of immunization against anthrax: old vaccines may be here to stay for a while. Curr. Opin. Infect. Dis. 13:113-120. [DOI] [PubMed] [Google Scholar]
- 32.Turnbull, P. C. 1991. Anthrax vaccines: past, present and future. Vaccine 9:533-539. [DOI] [PubMed] [Google Scholar]
- 33.Weaver, J., T. J. Kang, K. W. Raines, G. L. Cao, S. Hibbs, P. Tsai, L. Baillie, G. M. Rosen, and A. S. Cross. 2007. Protective role of Bacillus anthracis exosporium in macrophage-mediated killing by nitric oxide. Infect. Immun. 75:3894-3901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Welkos, S. L., and A. M. Friedlander. 1988. Comparative safety and efficacy against Bacillus anthracis of protective antigen and live vaccines in mice. Microb. Pathog. 5:127-139. [DOI] [PubMed] [Google Scholar]
- 35.Zaucha, G. M., L. M. Pitt, J. Estep, B. E. Ivins, and A. M. Friedlander. 1998. The pathology of experimental anthrax in rabbits exposed by inhalation and subcutaneous inoculation. Arch. Pathol. Lab. Med. 122:982-992. [PubMed] [Google Scholar]