Abstract
Isolates of Clostridium perfringens type D produce the potent epsilon-toxin (a CDC/U.S. Department of Agriculture overlap class B select agent) and are responsible for several economically significant enterotoxemias of domestic livestock. It is well established that the epsilon-toxin structural gene, etx, occurs on large plasmids. We show here that at least two of these plasmids are conjugative. The etx gene on these plasmids was insertionally inactivated using a chloramphenicol resistance cassette to phenotypically tag the plasmid. High-frequency conjugative transfer of the tagged plasmids into the C. perfringens type A strain JIR325 was demonstrated, and the resultant transconjugants were shown to act as donors in subsequent mating experiments. We also demonstrated the transfer of “unmarked” native ɛ-toxin plasmids into strain JIR325 by exploiting the high transfer frequency. The transconjugants isolated in these experiments expressed functional ɛ-toxin since their supernatants had cytopathic effects on MDCK cells and were toxic in mice. Using the widely accepted multiplex PCR approach for toxin genotyping, these type A-derived transconjugants were genotypically type D. These findings have significant implications for the C. perfringens typing system since it is based on the toxin profile of each strain. Our study demonstrated the fluid nature of the toxinotypes and their dependence upon the presence or absence of toxin plasmids, some of which have for the first time been shown to be conjugative.
The gram-positive anaerobe Clostridium perfringens is the causative agent of severe gastrointestinal disease (including enterotoxemia and enteritis) in animals and gas gangrene and food poisoning in humans (13, 23, 34). C. perfringens isolates produce many different toxins but are divided into toxin types A to E based solely on the production of four major toxins: α-toxin (encoded by the plc gene), β-toxin (cpb), ɛ-toxin (etx), and ι-toxin (iap) (14, 25).
C. perfringens strains of all five toxin types produce the chromosomally encoded α-toxin, and type C, D, and E isolates also produce plasmid-encoded β-toxin, ɛ-toxin, and ι-toxin, respectively. Type B isolates produce α-toxin, β-toxin, and ɛ-toxin. The demonstration that the genes encoding three of these typing toxins are found on large virulence plasmids led to the hypothesis that C. perfringens types B to E may represent type A strains that have received toxin-encoding plasmids by horizontal gene transfer (7, 21).
In C. perfringens conjugative plasmids are associated primarily with resistance to antibiotics, particularly tetracycline (1, 2). The paradigm C. perfringens tetracycline resistance plasmid, pCW3, has been sequenced, and its conjugation region, the tcp locus, has been shown to be essential for conjugative plasmid transfer (4). All known conjugative C. perfringens plasmids have the tcp region (4). Until recently, there was little or no evidence that the toxin plasmids from C. perfringens may be conjugative, with the exception of the enterotoxin (CPE) plasmid (5). Subsequent studies have shown that the tcp locus is present in several CPE plasmids, as well as β-, ɛ-, and ι-toxin plasmids from C. perfringens type C, D, and E strains, respectively (4, 16, 30). Recently, it was shown that type D isolates may harbor several large plasmids (48 to 110 kb), which could carry up to three different toxin genes (30). These plasmids have not yet been shown to be conjugative, but some were shown to carry the tcp region (4, 30).
ɛ-Toxin is a pore-forming cytotoxin and is one of the most potent clostridial toxins (33). It is classified as an overlap class B select agent by the CDC and U.S. Department of Agriculture due to its potential for misuse as a bioterrorism agent. ɛ-Toxin-producing type D isolates are the etiological agents of highly lethal enterotoxemias, particularly in sheep and goats (13, 35). The exact role of ɛ-toxin in C. perfringens type D disease is still unknown; however, this potent neurotoxin is thought to mediate the rapid decline of diseased animals by entering the bloodstream and exerting both systemic and neurological effects (13, 35, 37). In addition, in goats, ɛ-toxin can produce severe damage to the intestinal tract without having to be absorbed into the systemic circulation (37).
The potent nature of ɛ-toxin and type D-mediated disease highlights the importance of understanding the mechanisms by which plasmids carrying the etx gene and other lethal toxin genes are disseminated. To this end, we tagged two type D ɛ-toxin plasmids by insertionally inactivating the etx gene with a chloramphenicol resistance cassette and used these marked plasmids to determine if the plasmids were conjugative. Here we report the first demonstration of the conjugative transfer of both marked and unmarked wild-type ɛ-toxin plasmids from type D to type A strains of C. perfringens and characterization of the resultant transconjugants.
MATERIALS AND METHODS
Bacterial strains and culture conditions.
All strains and plasmids used in this study are shown in Table 1. Strains were grown overnight in FTG medium (Oxoid) and then on TSC agar, C. perfringens agar base (TSC and SFP; Oxoid) containing 0.04% d-cycloserine (Sigma). When required, antimicrobial agents were added to solid media at the following concentrations: chloramphenicol, 30 μg ml−1; thiamphenicol, 30 μg ml−1; rifampin, 20 μg ml−1; nalidixic acid, 20 μg ml−1; streptomycin, 1 mg ml−1; tetracycline, 10 μg ml−1; and saturated potassium chlorate, 1% (vol/vol). Agar cultures were grown in an atmosphere containing 10% CO2 and 10% H2 in N2 at 37°C overnight.
TABLE 1.
Bacterial strains and plasmids
| Strain or plasmid | Descriptiona | Source or reference(s) |
|---|---|---|
| C. perfringens strains | ||
| CN1020 | Type D wild-type strain, carries 48-kb ɛ-toxin plasmid pJIR3118 | Burroughs-Wellcome Collection via R. G. Wilkinson |
| CN3718 | Type D wild-type strain, carries 48-kb ɛ-toxin plasmid pJIR3119 | Burroughs-Wellcome Collection via R. G. Wilkinson |
| JIR325 | Strain 13 Rifr Nalr | 12 |
| JIR4195 | JIR325(pCW3) Rifr Nalr Tcr | P. Johanesen, D. Lyras, and J. Rood, unpublished |
| JIR4394 | Strain 13 Strr Chlr | 4 |
| JIR4825 | JIR4394(pCW3) Strr Chlr Tcr | J. Parsons, T. Bannam, and J. Rood, unpublished |
| JIR4981 | CN1020(pJIR3120) Δetx::catP Cmr/Tmr | Transformant |
| JIR4982 | CN3718(pJIR3121) Δetx::catP Cmr/Tmr | Transformant |
| JIR4983 | JIR325(pJIR3120) Rifr Nalr Cmr/Tmr | Transconjugant, JIR4981 × JIR325 |
| JIR4985 | JIR325(pJIR3121) Rifr Nalr Cmr/Tmr | Transconjugant, JIR4982 × JIR325 |
| JIR12012 | JIR325(pJIR3118) Rifr Nalr | Transconjugant, CN1020 × JIR325 |
| JIR12013 | JIR325(pJIR3118) Rifr Nalr | Transconjugant, CN1020 × JIR325 |
| Plasmids | ||
| pCW3 | 47 kb, conjugative, Tcr | 4, 27 |
| pMTL9301 | E. coli-C. difficile shuttle vector, 7.1 kb, C. difficile repA Emr | 22 |
| pJIR2783 | Clostridial suicide plasmid, 6.1 kb, pT7Blue-3 backbone ΔblaΩermB, ΔkanΩoriT, EcoRIΩcatP, Emr Cmr | Recombinant |
| pJIR2906 | 8.4-kb plasmid with Asp718/PstI-digested 2.3-kb 5′ etx PCR product cloned into KpnI/PstI-digested pJIR2783, Emr Cmr | Recombinant |
| pJIR2907 | 9.9-kb plasmid, pJIR2906 with 1.5-kb 3′ etx PCR product cloned into XbaI (T4 filled), Emr Cmr | Recombinant |
| pJIR3076 | 6.9-kb plasmid, pJIR2907 digested with XmnI and religated to remove oriT and ermB, Cmr | Recombinant |
| pJIR3077 | 14-kb Δetx::catP recombination vector, 7.1-kb FspI-digested pMTL9301 vector ligated into KpnI/NotI-digested pJIR3076.ColE1, C. difficile repA oriT ermB Δetx::catP Emr Cmr/Thr | Recombinant |
| pJIR3118 | Wild-type 48-kb ɛ-toxin plasmid from CN1020 | |
| pJIR3119 | Wild-type 48-kb ɛ-toxin plasmid from CN3718 | |
| pJIR3120 | pJIR3118 Δetx::catP, Cmr/Tmr | Transformation with pJIR3077 recombination vector |
| pJIR3121 | pJIR3119 Δetx::catP, Cmr/Tmr | Transformation with pJIR3077 recombination vector |
Rifr, Nalr, Tcr, Strr, Chlr, Emr, and Cmr/Tmr, resistance to rifampin, resistance to nalidixic acid, resistance to tetracycline, resistance to streptomycin, resistance to potassium chlorate, resistance to erythromycin, and resistance to chloramphenicol and thiamphenicol, respectively.
Conjugation experiments.
Mixed plate mating was carried out as previously described (24, 26), except that selection was on TSC agar supplemented with the appropriate antibiotics. The recipients were the strain 13 derivatives JIR325 (rifampin and nalidixic acid resistant) and JIR4394 (streptomycin and potassium chlorate resistant). The donor strains were the type D Δetx::catP mutants JIR4981 and JIR4982. Transconjugants were selected on TSC agar containing thiamphenicol, rifampin, and nalidixic acid when JIR325 was the recipient and on TSC agar containing thiamphenicol, streptomycin, and potassium chlorate when JIR4394 was the recipient. The conjugative transfer efficiency was defined as the number of transconjugants per donor cell. Strains carrying pCW3 were used as positive controls in all mating experiments.
In the unmarked plasmid conjugations, the type D strain CN1020 was used as the donor and JIR325 was used as the recipient. After mating as described above, derivatives of JIR325 were selected on agar medium containing rifampin and nalidixic acid. Transconjugants were identified by colony hybridization carried out according to the manufacturer's instructions (Roche), using a digoxigenin (DIG)-labeled etx probe.
Preparation of culture supernatants.
Culture supernatants from 4-h (late-log-phase) TPG broth cultures (10) were centrifuged at 6,700 × g for 10 min, and this was followed by filter sterilization using a 0.45-μm-pore-size filter (Millipore). To activate ɛ-toxin activity, 0.05% trypsin (1:250; Sigma) was added, and the culture supernatants were incubated at 37°C for 30 min prior to use in Madin-Darby canine kidney (MDCK) cell assays for cytotoxicity. When required, supernatants were concentrated 10-fold using Amicon ultracentrifugation columns (10,000-Da cutoff). For each strain supernatants from cultures grown on at least three separate occasions were assayed.
Molecular methods.
C. perfringens genomic DNA for use as a template in PCRs was prepared as described previously (4). Plasmid DNA from Escherichia coli was isolated by alkaline lysis (QIAGEN). PCR amplification using Pfo polymerase and 0.5 μM of each primer was performed using 30 cycles of denaturation (95°C), annealing (55°C), and extension (72°C). Extension times were varied from 1 to 4 min depending on the expected PCR product length. QIAquick PCR purification kits were used to purify PCR products before cloning, sequencing, or DIG labeling. C. perfringens typing was performed using a multiplex PCR assay as previously described (8). PCR products were separated on a 1% agarose gel by electrophoresis. Restriction endonuclease digestion, agarose gel electrophoresis, and DNA ligation were performed using standard laboratory methods (28). All oligonucleotide sequences are shown in Table S1 in the supplemental material.
Construction of C. perfringens mutants by allelic exchange.
Based on the sequence of the ɛ-toxin plasmid pJGS1721 (G. Myers, I. Paulsen, J. G. Songer, B. McClane, R. Titball, J. Rood, and S. Melville, unpublished data) primers JRP2240 and JRP2241 were designed to amplify an upstream 2.3-kb fragment which incorporated the first 248 nucleotides of the etx gene and 2 kb of upstream sequence. A 1.5-kb downstream fragment that included the last 265 nucleotides of etx and 1.2 kb of downstream sequence was amplified with primers JRP2112 and JRP2242. These fragments were cloned into pJIR2783 on either side of the catP gene, resulting in the 9.9-kb plasmid pJIR2907. Digestion of pJIR2907 with XmnI and religation resulted in deletion of the oriT site and ermB gene, yielding the 6.9-kb plasmid pJIR3076. The 7.1-kb FspI fragment of pMTL9301 (22) was cloned into NotI/KpnI-digested pJIR3076 to construct the 14-kb recombination vector pJIR3077, which then was introduced into the wild-type type D strains CN1020 and CN3718 by electroporation (31). Thiamphenicol-resistant transformants were isolated and passaged in nonselective FTG broth and then plated onto TSC agar containing thiamphenicol. Thiamphenicol-resistant colonies were patched onto medium containing erythromycin (to ensure that free pJIR3077 did not persist), and erythromycin-sensitive colonies were chosen for further analysis.
Southern hybridization.
Genomic and plasmid DNA was digested with HindIII, and fragments were separated by electrophoresis on 0.8% agarose gels. DNA was visualized by ethidium bromide staining prior to transfer to nitrocellulose membranes. DIG labeling, hybridization, chemiluminescent detection, stripping, and reprobing were carried out as described in the DIG user's manual (Roche). DIG-labeled probes were generated by PCR using the following primers: for etx, JRP2074 and JRP2495; for catP, JRP2142 and JRP2143; for ermB, JRP1924 and JRP1925; for repA, JRP2457 and JRP2465; and for tcpH, JRP1758 and JRP1661.
PFGE.
C. perfringens genomic DNA was embedded in agarose plugs, and the uncut genomic DNA was subjected to pulsed-field gel electrophoresis (PFGE) prior to transfer to nylon membranes and Southern hybridization using a DIG-labeled etx probe, as described previously (30).
Cell culture and cytotoxicity assays.
MDCK cells were grown in Dulbecco's modified Eagle's medium supplemented with 2 mM glutamate, 10% fetal calf serum, and 100 U/ml of streptomycin and penicillin (Invitrogen). For cytotoxicity assays, six-well tissue culture trays were seeded with 2 × 105 cells/well and incubated overnight in 5% CO2 to obtain semiconfluence. Cell monolayers were washed three times with phosphate-buffered saline and immersed in 1 ml of Dulbecco's modified Eagle's medium prior to addition of 50 μl of trypsin-treated or non-trypsin-treated culture supernatant. Cytopathic effects were observed using an inverted confocal microscope (Olympus 1X71) with a 37°C heated stage over a 24-h period. For neutralization of ɛ-toxin activity, monoclonal antibody (MAb) 5B7 (kindly provided by Paul Hauer, Center for Veterinary Biologics, Ames, IA) (9) was added to trypsin-treated culture supernatants and incubated at room temperature for 1 h as described previously (29) before addition of the treated supernatant to MDCK cell monolayers. As a negative control, culture supernatants were treated with a polyclonal antibody reactive against the ErmB RNA methylase.
Quantification of α-toxin, perfringolysin O, and ɛ-toxin levels in culture supernatants.
α-Toxin was assayed (32) using nutrient agar supplemented with 4% egg yolk by reference to a C. perfringens phospholipase C standard (Sigma). The total protein content was determined using a bicinchoninic acid kit (Pierce), and the specific activity was expressed in phospholipase C units/mg of total protein. Perfringolysin O activity on horse red cells was determined by a doubling dilution assay; the perfringolysin O titer was defined as the reciprocal of the last dilution showing complete hemolysis (36). ɛ-Toxin levels were determined by comparing the chemiluminescent signal intensities for known ɛ-toxin standards with the test samples in Western blots, using ɛ-toxin MAb 5B7, as described previously (29).
Mouse intravenous injection model.
The toxicity of the strains was analyzed using a mouse intravenous assay to calculate the 50% lethal dose (LD50) of culture supernatant, as previously described (29). Briefly, sterile culture supernatants were incubated with 0.05% trypsin (1:250; Difco) for 30 min at 37°C and then serially diluted twofold (between 1:100 and 1:1,600) in 1% peptone water. Then 0.5 ml of each relevant dilution was injected intravenously into pairs of mice. As a negative control, mice were inoculated with trypsinized 1% peptone water. The double reciprocal of the highest dilution inducing lethality (within 48 h) in at least one of the paired mice was defined as the LD50. Two independent batches of filtered culture supernatants were assayed, and the results were expressed as the average of the LD50 values for each batch. Experimental procedures involving animals were approved by the Animal Care and Use Committee of the California Animal Health and Food Safety Laboratory, University of California, Davis (permit 04-11593).
RESULTS
Tagging the ɛ-toxin plasmids with catP.
The objective of these studies was to determine if the ɛ-toxin plasmids are conjugative. From our previous study of type D strains of C. perfringens (29) we chose two ɛ-toxin-producing isolates, CN1020 and CN3718, which were transformable using standard laboratory methods and had been determined to have the type D genotype by multiplex PCR. CN1020 harbors a single, approximately 48-kb plasmid, now designated pJIR3118, which carries IS1151, the etx gene, and the tcp locus (30). CN3718 also has a single 48-kb etx plasmid (data not shown), designated pJIR3119.
The ɛ-toxin plasmids in these strains were marked with the catP gene, which confers chloramphenicol and thiamphenicol resistance, so that resistance could be used as a selective marker for plasmid transfer. We utilized a novel insertional inactivation approach based on the successful mutagenesis of several genes in Clostridium difficile in a previous study (18). In that study, an E. coli-C. perfringens recombination vector that was relatively unstable in C. difficile was used to introduce the insertionally inactivated gene and allow time for recombination events to occur. Growth in the absence of the plasmid-determined resistance marker followed by screening for resistance to the gene used for insertional inactivation enabled selection for chromosomal mutants. It was reasoned that it might be possible to use the reverse approach in C. perfringens, and subsequent stability assays showed that the E. coli-C. difficile shuttle vector pMTL9301 (18), which confers erythromycin resistance, was unstable in C. perfringens in the absence of selective pressure (data not shown).
A pMTL9301-based recombination vector, pJIR3077, that contained an etx gene that had been insertionally inactivated with catP was constructed and used to transform the type D strains CN1020 and CN3718. After initial growth in the presence of thiamphenicol and subsequent growth in absence of antibiotics to provide time for the loss of pJIR3077, thiamphenicol-resistant, erythromycin-sensitive colonies were selected as potential Δetx::catP mutants.
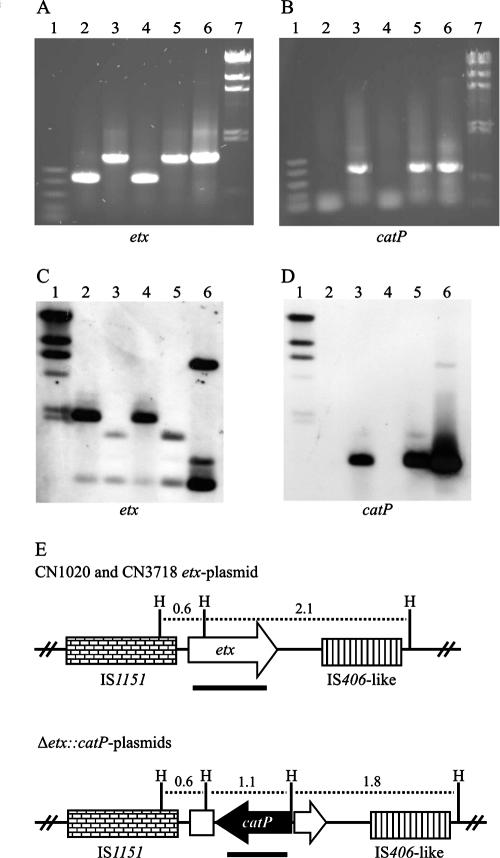
Genomic DNA from these putative mutants was analyzed initially by PCR. An 805-bp etx fragment was amplified from CN1020 and CN3718 (Fig. 1A, lanes 2 and 4), and a 1.5-kb fragment was amplified from the mutants and the suicide vector (Fig. 1A, lanes 3, 5, and 6). As expected, catP-specific PCR products were amplified from the mutants but not from the wild-type strains (Fig. 1B). The absence of ermB- and repA-specific PCR products in the mutants (data not shown) indicated that the vector did not persist in these strains. These results are as predicted for insertional inactivation of the etx genes by allelic exchange.
FIG. 1.
Confirmation of Δetx::catP mutants. (A and B) PCR analysis using etx- and catP-specific primers, respectively. Lanes 2 to 6 contained strains CN1020, JIR4891, CN3718, and JIR4892 and recombination plasmid pJIR3077, respectively. Lanes 1 and 7 contained size markers (Promega PCR marker and HindIII-digested λcI857, respectively). (C and D) Southern blots of HindIII-digested genomic DNA obtained using etx- and catP-specific probes, respectively. The contents of lanes 2 to 6 were the same as those described above. Lane 1 contained HindIII-digested λcI857 molecular size markers. (E) Representation of the etx region (based on previous studies [30]) in the wild-type ɛ-toxin plasmids pJIR3118 and pJIR3119, compared to the same region after insertional inactivation of the etx gene by allelic exchange with the recombination vector pJIR3077. The positions of HindIII sites (H) are indicated, as are the sizes of the predicted HindIII fragments (in kb). The etx and catP probes used for Southern blotting are indicated by the solid lines under the genes.
Southern hybridization of HindIII-digested DNA from the wild-type and mutant strains confirmed the insertional inactivation of the etx gene. Hybridization with an etx-specific probe showed that the 2.1-kb etx band in the wild-type strains had been replaced by a 1.8-kb band in the mutants (Fig. 1C), as predicted (Fig. 1E). In addition, only the mutants had the 1.1-kb band that hybridized to the catP probe. Probes specific for ermB and repA hybridized only to the recombination vector pJIR3077 (data not shown). These data provided convincing evidence that etx mutants had been successfully constructed by double-crossover events. The mutants were designated JIR4981 and JIR4982, and their mutated plasmids were designated pJIR3118Δetx::catP or pJIR3120 and pJIR3119Δetx::catP or pJIR3121, respectively. Southern blotting with the plasmid-specific tcpH gene, which is part of the tcp conjugation locus (4), confirmed that an etx-derived plasmid was still present in these strains (data not shown).
Marked ɛ-toxin plasmids are conjugative.
To determine if the plasmids from these type D strains were conjugative, we used the tagged Δetx::catP mutants as donors in separate mixed plate matings, using the type A strain JIR325 as the recipient. Transconjugants were selected on medium containing thiamphenicol, selecting for the marked plasmids, and on medium containing rifampin and nalidixic acid, selecting for the recipient. No colonies were observed in control matings that involved only the donor or recipient strains. Conjugative transfer of thiamphenicol resistance (i.e., the marked plasmids) was observed at very high frequencies comparable to those observed for the paradigm tetracycline resistance plasmid, pCW3 (Table 2). PCR analysis confirmed that the plasmids had indeed been transferred into strain JIR325. In particular, a Δetx::catP-specific fragment was amplified from the transconjugants but not from the recipient strain, and the cpb2 gene, which was specific for the type A recipient, was amplified from the transconjugants but not from the donor (Fig. 2A). In addition, two of the resultant transconjugants, JIR4983 and JIR4985, one from each donor, could be used as donors in subsequent matings and yielded transfer frequencies similar to those of the original type D-to-type A matings (Table 2).
TABLE 2.
Transfer of marked etx plasmids
| Donor | Recipient | Plasmid | Plasmid properties | Transfer frequencya |
|---|---|---|---|---|
| JIR4981 | JIR325 | pJIR3120 | pJIR3118 Δetx::catP (Tmr) | (2.9 ± 4.0) × 10−1 |
| JIR4982 | JIR325 | pJIR3121 | pJIR3119 Δetx::catP (Tmr) | (3.8 ± 6.6) × 10−2 |
| JIR4825 | JIR325 | pCW3 | Tcr | (2.0 ± 2.0) × 10−1 |
| JIR4983 | JIR4394 | pJIR3120 | pJIR3118 Δetx::catP (Tmr) | (4.8 ± 3.9) × 10−1 |
| JIR4985 | JIR4394 | pJIR3121 | pJIR3119 Δetx::catP (Tmr) | (1.0 ± 6.3) × 10−1 |
| JIR4195 | JIR4394 | pCW3 | Tcr | (5.7 ± 2.3) × 10−2 |
The transfer frequencies are expressed as the number of transconjugants per donor cell and are the averages of at least three separate biological replicates.
FIG. 2.
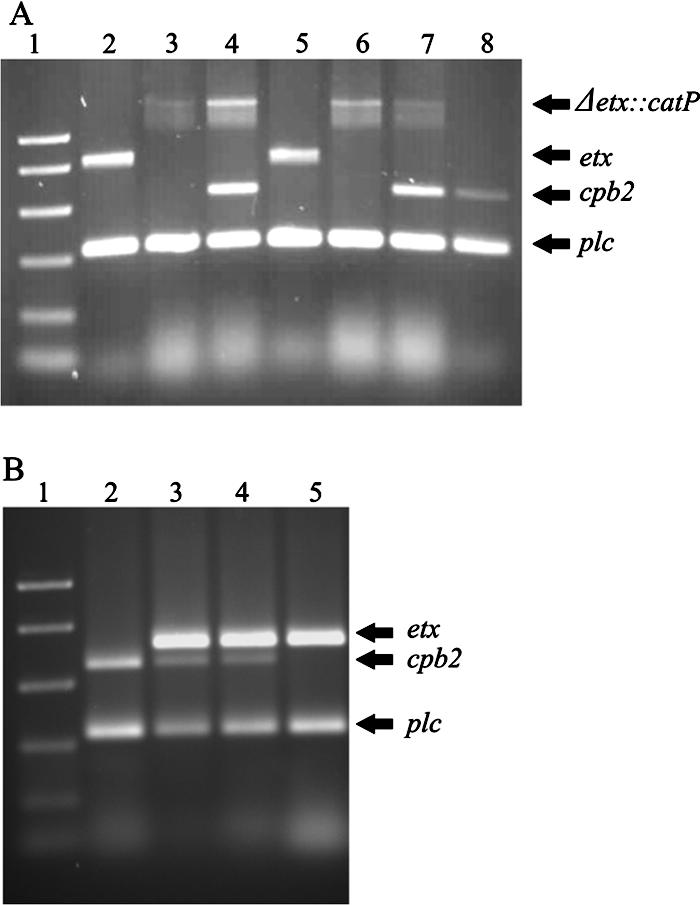
Multiplex PCR analysis of the wild type and transconjugants. (A) Lanes 2 to 8 contained type D strain CN1020, CN1020 etx mutant JIR4981, JIR4981 × JIR325 transconjugant JIR4983, type D strain CN3718, CN3178 etx mutant JIR4982, JIR4982 × JIR325 transconjugant JIR4985, and JIR325, respectively. Lane 1 contained Promega PCR molecular size markers. (B) Lanes 2 to 5 contained strains JIR325, JIR12012, JIR12013, and CN1020, respectively. Lane 1 contained Promega PCR molecular size markers.
Conjugative transfer of an unmarked type D ɛ-toxin plasmid.
The high transfer frequencies suggested that we might be able to detect transfer of the native ɛ-toxin plasmid from a type D strain to a type A strain without marking the plasmid. To this end, plate matings were performed using CN1020 as the donor and JIR325 as the recipient. In these unmarked plasmid conjugation experiments, transconjugants carrying the etx gene were detected, by colony hybridization using an etx-specific probe, at a frequency of 0.8%, and the results were confirmed by PCR analysis (data not shown). Two of these independently derived JIR325(pJIR3118) transconjugants, JIR12012 and JIR12013, were chosen for further study.
Multiplex PCR analysis revealed that the conjugative transfer of the ɛ-toxin plasmid to a type A strain converted this strain to a genotypically type D isolate.
A multiplex PCR assay (8) that detects six C. perfringens lethal toxin genes, etx (ɛ-toxin), plc (α-toxin), cpb (β-toxin), cpb2 (β2-toxin), cpe (CPE), and iap (enzymatic component of ι-toxin), was used to analyze the unmarked transconjugants. By definition, type A strains carry the plc gene and may have other accessory toxin genes, such as cpb2 or cpe, but do not have the etx, cpb, and iap genes. By contrast, type D strains have both the plc and etx genes. In this assay the type D donors CN1020 and CN3718 were both etx+ plc+ and cpb2 negative, and the type A recipient JIR325 was plc+ cpb2+ and etx negative (Fig. 2A and 2B). The multiplex PCR profiles of the unmarked etx+ transconjugants, JIR12012 and JIR12013, identified these strains as C. perfringens type D strains since they had PCR products of the expected sizes when both the plc and etx primers were used, despite the fact that the recipient in these matings was the type A strain JIR325 (Fig. 2B). Both strains were clearly derived from JIR325 since they carried the cpb2 gene. Finally, the use of tcpH primers provided evidence that a conjugative plasmid carrying the tcp region had been transferred (data not shown).
PFGE confirms the movement of large ɛ-toxin plasmids.
To confirm that ɛ-toxin plasmids had been transferred in these experiments, PFGE followed by Southern blotting was carried out using uncut genomic DNA (30). Using an etx-specific probe, a single hybridizing band at approximately 48 kb was detected for the parent type D strain CN1020 and for the JIR325-derived transconjugants containing the native ɛ-toxin plasmid pJIR3118 (data not shown). Similar results were obtained with the marked transconjugants derived from the type D strain CN3718, but no hybridization was observed with JIR325. These results are consistent with the conjugative transfer of the etx plasmids and their maintenance in the transconjugants.
ɛ-Toxin plasmids have a tcp conjugation region that is very similar to that of pCW3.
To determine if the tcp conjugation region was also present in the ɛ-toxin plasmids, we analyzed genomic DNA from the marked plasmids pJIR3120 and pJIR3121. PCR analysis was performed with 27 primer combinations that together encompassed the entire tcp locus, from the intP gene to the dcm gene (4). The tcp conjugation region was present in both plasmids, and most primer pairs generated products that were the same size as those for pCW3. However, there was some variation in the tcpF and tcpH regions, as previously shown with another ɛ-toxin plasmid, pJGS1721 (4).
Type A transconjugants express ɛ-toxin, α-toxin, and perfringolysin O.
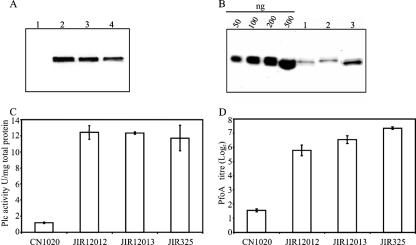
To determine if the etx gene was expressed in the type A background and if the ɛ-toxin plasmid had any effect on the production of other toxins, Western blotting was done with culture supernatants using ɛ-toxin MAb 5B7. The results showed that the type A-derived transconjugants that originated from transfer of the native ɛ-toxin plasmid pJIR3118 produced levels of ɛ-toxin (Fig. 3) that were 2.5-fold lower than the expression levels in the type D donor. However, the transconjugants produced α-toxin and perfringolysin O at levels comparable to those produced by the type A recipient strain (Fig. 3C and D). These results showed that the lower level of production of α-toxin and perfringolysin O in the type D strain was not the result of the presence of a repressor gene in the ɛ-toxin plasmid.
FIG. 3.
Toxin production by pJIR3118-derived transconjugants. (A) Western blotting of culture supernatants with anti-ɛ-toxin MAb 5B7. Lanes 1 to 4 contained JIR325, CN1020, JIR12012, and JIR12013, respectively. (B) Quantification of ɛ-toxin in culture supernatants of transconjugants JIR12012 and JIR12013 (lanes 1 and 2, respectively) and CN1020 (lane 3). The other lanes contained different concentrations of the purified ɛ-toxin standard (50 to 500 ng). (C and D) Phospholipase C (Plc) and perfringolysin O (PfoA) activities of the strains indicated. The data are the averages for three independent biological samples.
ɛ-Toxin produced in the type A-derived transconjugants is active on MDCK monolayers and is lethal in the mouse intravenous injection model.
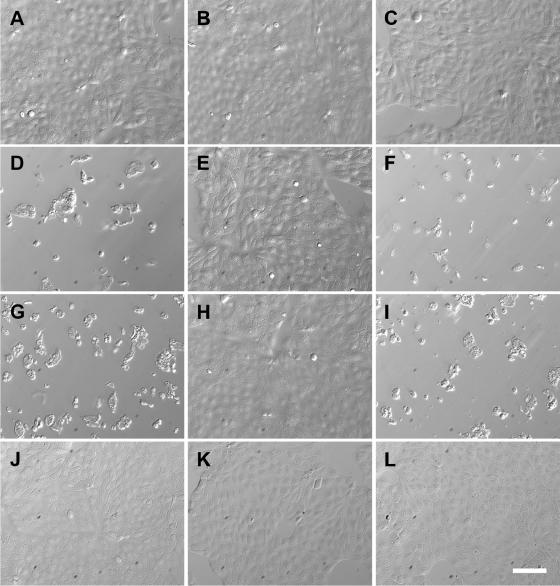
ɛ-Toxin is expressed as a relatively inactive protoxin that is activated after cleavage of both N-terminal and C-terminal domains by either trypsin or extracellular proteases produced by C. perfringens (15). Since purified, trypsin-treated ɛ-toxin is known to be cytotoxic to MDCK cells (19, 20), we treated culture supernatants from several strains with trypsin to activate any ɛ-toxin that was present and examined the cytopathic effects on MDCK cell monolayers. In initial experiments cell rounding and blebbing were observed as soon as 30 min after inoculation with culture supernatants that contained activated ɛ-toxin, and severe loss of adherence and obvious cytotoxicity was apparent after 24 h. After 24 h, trypsin-treated supernatants from CN1020 or CN3718, diluted at least 10-fold, still caused clear cytopathic effects (Fig. 4). Culture supernatants of JIR325 derivatives carrying the native ɛ-toxin plasmid also were highly toxic to the MDCK cells (Fig. 4 and data not shown). By comparison, MDCK cells incubated for 24 h with trypsin-treated undiluted culture supernatants from JIR325 or with either JIR4983 or JIR4985 (JIR325 derivatives carrying the mutated Δetx::catP plasmids) showed no significant changes.
FIG. 4.
ɛ-Toxin-mediated cytopathic effects of culture supernatants. Monolayers of MDCK cells were incubated for 24 h in the presence of trypsin-treated culture supernatants from different strains before examination with an Olympus 1X71 inverted microscope. ImageJ 1.37v software (http://rsb.info.nih.gov/ij/index.html) was used to view the images. (A) JIR325. (B) CN1020 Δetx::catP. (C) Medium alone. (D) CN1020. (E) CN1020 pretreated with MAb 5B7. (F) CN1020 pretreated with ErmB-specific antibody. (G) JIR12012 [JIR325(pJIR3118)]. (H) JIR12012 pretreated with MAb 5B7. (I) JIR12012 pretreated with ErmB-specific antibody. (J) JIR4983 [JIR325(pJIR3118Δetx::catP)]. (K) JIR4983 pretreated with MAb 5B7. (L) JIR4983 pretreated with ErmB-specific antibody. The culture supernatant from CN1020 was diluted 50-fold prior to use. Bar, 100 μm.
Pretreatment with an MAb that was specific for ɛ-toxin completely abrogated the destructive effects of trypsin-activated supernatants on the MDCK cells. However, a control polyclonal antibody specific for the unrelated ErmB RNA methylase protein had no effect (Fig. 4). In addition, non-trypsin-treated supernatants of JIR325 and the transconjugants caused no cytopathic effects. These data demonstrated that active ɛ-toxin in the culture supernatants, not other toxins such as α-toxin or perfringolysin O, was responsible for the cytopathic effects on the MDCK cells.
Finally, trypsin-treated supernatants were tested for the ability to cause disease in the mouse intravenous injection model (29). The results showed that the type A-derived JIR325(pJIR3118) transconjugants had toxicity (141 to 400 minimal lethal doses) comparable to that of their type D parent strain, CN1020 (141 to 200 minimal lethal doses). Supernatants from JIR325 were not lethal under these conditions. These data confirmed that conjugative transfer of a native ɛ-toxin plasmid from a type D strain to a type A strain can convert the latter to an ɛ-toxin-producing, phenotypically type D strain whose products are lethal for mice.
DISCUSSION
Previous studies have revealed conjugative transfer of numerous pCW3-related tetracycline resistance plasmids (1, 2, 11) and a cpe plasmid (6) between type A strains of C. perfringens. The potential for conjugative transfer of the ɛ-toxin plasmids was suggested previously since these plasmids have the tcp conjugation genes (4, 16, 30), which are present in all known conjugative plasmids from C. perfringens. In this study we showed that two ɛ-toxin plasmids can transfer by conjugation. Conjugation was initially demonstrated by using a novel genetic method to construct genetically marked derivatives of these plasmids and then using the marker to select for transconjugants. The efficiency of transfer was so high that in subsequent matings it was possible to isolate transconjugants without any selection for the donor, which has not been achieved before in C. perfringens. In addition, this is the first report of intraspecies conjugative transfer between type D and type A strains of C. perfringens. Since the resultant transconjugants from these matings could act as donors in subsequent mating experiments, these 48-kb ɛ-toxin plasmids must encode all of the functions required for conjugation. C. perfringens has many different toxin-encoding plasmids, and many of these plasmids carry the tcp conjugation locus (4, 16, 30). Based on the current results and the highly conserved nature of the tcp regions, it is highly likely that many, if not all, of these toxin plasmids will prove to be conjugative.
The movement of an unmarked wild-type ɛ-toxin plasmid into a type A recipient enabled us to analyze etx gene expression in a type A background. In this background, functional ɛ-toxin was produced and the transconjugants were both genotypically and phenotypically type D, as determined by multiplex PCR analysis and toxin assays. These results provide experimental evidence, at least for type D strains, that the different toxin types of C. perfringens result from the horizontal transfer of toxin-carrying plasmids (7, 21); that is, as other workers have suggested, type B, C, D, and E isolates of C. perfringens may represent type A strains that have acquired a conjugative toxin-encoding plasmid (7, 21). However, due to the extensive genetic diversity found even in type A strains, a view of strain typing based only on toxin carriage may be simplistic and inadequate. Recently, analysis of the toxin plasmids of 23 type D isolates revealed considerable variation in both the size and the number of large plasmids. Isolates carrying the etx, cpe, and cpb2 genes on a single plasmid or on three distinct plasmids were identified (30). Clearly, a typing system that can discriminate between the chromosomal background and the plasmid content of an isolate would be more useful for strain typing and would provide a more accurate picture of which genetic elements C. perfringens requires for host specificity and virulence.
It was recently demonstrated that ɛ-toxin is responsible for the lethality of type D culture supernatants in the intravenous mouse lethality assay (29). In this study we demonstrated that activated culture supernatants from type A-derived etx+ transconjugants caused ɛ-toxin-mediated MDCK cell cytotoxicity and were lethal in the intravenous mouse model, even though they had less ɛ-toxin than the parent type D strain. If ɛ-toxin is the only type D-specific requirement for type D-mediated enterotoxemia, then our type A-derived transconjugants should be virulent in a large animal model of disease. However, if there is more to the relationship between disease and strain type than just the production of ɛ-toxin, then the transconjugants may not colonize the sheep gastrointestinal tract and cause disease.
C. perfringens type A and type D isolates can coexist as commensals in the gastrointestinal tracts of ruminants, which provides ample opportunity for the conjugative transfer of toxin plasmids. Although it is generally accepted that ɛ-toxin production is required for type D-mediated disease to occur, the precise process by which disease develops is not fully understood. The overgrowth of commensal ɛ-toxin-producing strains in the gastrointestinal tract due to changes in feeding, environmental stress, or the entry of exogenous type D strains has been suggested to be the potential trigger for disease (3, 17, 35). Our results suggest an alternative scenario for the sudden onset of enterotoxemic disease, as first suggested for human non-food-borne disease mediated by plasmid-determined CPE production (6). Under certain conditions, adherent resident C. perfringens type A cells may be converted into ɛ-toxin-producing type D strains by conjugative transfer of an ɛ-toxin plasmid from either resident or exogenous type D cells. This process would exponentially increase the number of ɛ-toxin-producing bacteria in the gastrointestinal tract. In particular, if transfer can occur in vivo, then it would no longer be necessary for an exogenous type D strain to have the ability to colonize the gastrointestinal tract; the strain would simply need to be able to survive long enough to transfer its toxin plasmid to the resident adherent flora.
Supplementary Material
Acknowledgments
We thank Trudi Bannam, Wee Lin Teng, and Jennifer Parsons for helpful discussions. Paul Hauer is thanked for kindly supplying MAbs against ɛ-toxin.
This research was supported by grant AI056177-03 and training grant T32 AI060525-01A1 from the National Institute of Allergy and Infectious Diseases and by funds from the Australian Research Council Centre of Excellence in Structural and Functional Microbial Genomics.
Footnotes
Published ahead of print on 24 August 2007.
Supplemental material for this article may be found at http://jb.asm.org/.
REFERENCES
- 1.Abraham, L. J., and J. I. Rood. 1985. Molecular analysis of transferable tetracycline resistance plasmids from Clostridium perfringens. J. Bacteriol. 161:636-640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abraham, L. J., A. J. Wales, and J. I. Rood. 1985. Worldwide distribution of the conjugative Clostridium perfringens tetracycline resistance plasmid, pCW3. Plasmid 14:37-46. [DOI] [PubMed] [Google Scholar]
- 3.Adamson, R. H., J. C. Ly, M. Fernandez-Miyakawa, S. Ochi, J. Sakurai, F. Uzal, and F. E. Curry. 2005. Clostridium perfringens epsilon-toxin increases permeability of single perfused microvessels of rat mesentery. Infect. Immun. 73:4879-4887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bannam, T. L., W. L. Teng, D. Bulach, D. Lyras, and J. I. Rood. 2006. Functional identification of conjugation and replication regions of the tetracycline resistance plasmid pCW3 from Clostridium perfringens. J. Bacteriol. 188:4942-4951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brynestad, S., and P. E. Granum. 1999. Evidence that Tn5565, which includes the enterotoxin gene in Clostridium perfringens, can have a circular form which may be a transposition intermediate. FEMS Microbiol. Lett. 170:281-286. [DOI] [PubMed] [Google Scholar]
- 6.Brynestad, S., M. R. Sarker, B. A. McClane, P. E. Granum, and J. I. Rood. 2001. Enterotoxin plasmid from Clostridium perfringens is conjugative. Infect. Immun. 69:3483-3487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Canard, B., B. Saint-Joanis, and S. T. Cole. 1992. Genomic diversity and organization of virulence genes in the pathogenic anaerobe Clostridium perfringens. Mol. Microbiol. 6:1421-1429. [DOI] [PubMed] [Google Scholar]
- 8.Garmory, H. S., N. Chanter, N. P. French, D. Bueschel, J. G. Songer, and R. W. Titball. 2000. Occurrence of Clostridium perfringens beta2-toxin amongst animals, determined using genotyping and subtyping PCR assays. Epidemiol. Infect. 124:61-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hauer, P. J., and N. E. Clough. 1999. Development of monoclonal antibodies suitable for use in antigen quantification potency tests for clostridial veterinary vaccines. Dev. Biol. Stand. 101:85-94. [PubMed] [Google Scholar]
- 10.Johnston, J. L., J. Sloan, J. A. Fyfe, J. K. Davies, and J. I. Rood. 1997. The recA gene from Clostridium perfringens is induced by methyl methanesulphonate and contains an upstream Cheo box. Microbiology 143:885-890. [DOI] [PubMed] [Google Scholar]
- 11.Lyras, D., and J. I. Rood. 1996. Genetic organization and distribution of tetracycline resistance determinants in Clostridium perfringens. Antimicrob. Agents Chemother. 40:2500-2504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lyristis, M., A. E. Bryant, J. Sloan, M. M. Awad, I. T. Nisbet, D. L. Stevens, and J. I. Rood. 1994. Identification and molecular analysis of a locus that regulates extracellular toxin production in Clostridium perfringens. Mol. Microbiol. 12:761-777. [DOI] [PubMed] [Google Scholar]
- 13.McClane, B. A., F. A. Uzal, M. F. Miyakawa, D. Lyerly, and T. Wilkins. 2007. The enterotoxic clostridia, p. 698-752. In M. Dworkin, S. Falkow, E. Rosenburg, K. H. Schleifer, and S. E. (ed.), The prokaryotes: a handbook on the biology of bacteria, vol. 4. Springer-Verlag, New York, NY. [Google Scholar]
- 14.McDonel, J. L. 1980. Clostridium perfringens toxins (type A, B, C, D, E). Pharmacol. Ther. 10:617-635. [DOI] [PubMed] [Google Scholar]
- 15.Minami, J., S. Katayama, O. Matsushita, C. Matsushita, and A. Okabe. 1997. Lambda-toxin of Clostridium perfringens activates the precursor of epsilon-toxin by releasing its N- and C-terminal peptides. Microbiol. Immunol. 41:527-535. [DOI] [PubMed] [Google Scholar]
- 16.Miyamoto, K., D. J. Fisher, J. Li, S. Sayeed, S. Akimoto, and B. A. McClane. 2006. Complete sequencing and diversity analysis of the enterotoxin-encoding plasmids in Clostridium perfringens type A non-food-borne human gastrointestinal disease isolates. J. Bacteriol. 188:1585-1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Niilo, L. 1980. Clostridium perfringens in animal disease: a review of current knowledge. Can. Vet. J. 21:141-148. [PMC free article] [PubMed] [Google Scholar]
- 18.O'Connor, J. R., D. Lyras, K. A. Farrow, V. Adams, D. R. Powell, J. Hinds, J. K. Cheung, and J. I. Rood. 2006. Construction and analysis of chromosomal Clostridium difficile mutants. Mol. Microbiol. 61:1335-1351. [DOI] [PubMed] [Google Scholar]
- 19.Payne, D. W., E. D. Williamson, H. Havard, N. Modi, and J. Brown. 1994. Evaluation of a new cytotoxicity assay for Clostridium perfringens type D epsilon toxin. FEMS Microbiol. Lett. 116:161-167. [DOI] [PubMed] [Google Scholar]
- 20.Petit, L., M. Gibert, D. Gillet, C. Laurent-Winter, P. Boquet, and M. R. Popoff. 1997. Clostridium perfringens epsilon-toxin acts on MDCK cells by forming a large membrane complex. J. Bacteriol. 179:6480-6487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Petit, L., M. Gibert, and M. R. Popoff. 1999. Clostridium perfringens: toxinotype and genotype. Trends Microbiol. 7:104-110. [DOI] [PubMed] [Google Scholar]
- 22.Purdy, D., T. A. T. O'Keeffe, M. Elmore, M. Herbert, A. McLeod, M. Bokori-Brown, A. Ostrowski, and N. P. Minton. 2002. Conjugative transfer of clostridial shuttle vectors from Escherichia coli to Clostridium difficile through circumvention of the restriction barrier. Mol. Microbiol. 46:439-452. [DOI] [PubMed] [Google Scholar]
- 23.Rood, J. I. 2007. Clostridium perfringens and histotoxic disease, p. 753-770. In M. Dworkin, S. Falkow, E. Rosenberg, K.-H. Schleifer, and E. Stackebrandt (ed.), The prokaryotes: a handbook on the biology of bacteria, vol. 4. Springer-Verlag, New York, NY. [Google Scholar]
- 24.Rood, J. I. 1983. Transferable tetracycline resistance in Clostridium perfringens strains of porcine origin. Can. J. Microbiol. 29:1241-1246. [DOI] [PubMed] [Google Scholar]
- 25.Rood, J. I., and S. T. Cole. 1991. Molecular genetics and pathogenesis of Clostridium perfringens. Microbiol. Rev. 55:621-648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rood, J. I., E. A. Maher, E. B. Somers, E. Campos, and C. L. Duncan. 1978. Isolation and characterization of multiply antibiotic-resistant Clostridium perfringens strains from porcine feces. Antimicrob. Agents Chemother. 13:871-880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rood, J. I., V. N. Scott, and C. L. Duncan. 1978. Identification of a transferable resistance plasmid (pCW3) from Clostridium perfringens. Plasmid 1:563-570. [DOI] [PubMed] [Google Scholar]
- 28.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual, 2nd ed. Cold Spring Harbor Laboratory, Cold Spring Harbor, NY.
- 29.Sayeed, S., M. E. Fernandez-Miyakawa, D. J. Fisher, V. Adams, R. Poon, J. I. Rood, F. A. Uzal, and B. A. McClane. 2005. Epsilon-toxin is required for most Clostridium perfringens type D vegetative culture supernatants to cause lethality in the mouse intravenous injection model. Infect. Immun. 73:7413-7421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sayeed, S., J. Li, and B. A. McClane. 2007. Virulence plasmid diversity In Clostridium perfringens type D isolates. Infect. Immun. 75:2391-2398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scott, P. T., and J. I. Rood. 1989. Electroporation-mediated transformation of lysostaphin-treated Clostridium perfringens. Gene 82:327-333. [DOI] [PubMed] [Google Scholar]
- 32.Sloan, J., T. A. Warner, P. T. Scott, T. L. Bannam, D. I. Berryman, and J. I. Rood. 1992. Construction of a sequenced Clostridium perfringens-Escherichia coli shuttle plasmid. Plasmid 27:207-219. [DOI] [PubMed] [Google Scholar]
- 33.Smedley, J. G., III, D. J. Fisher, S. Sayeed, G. Chakrabarti, and B. A. McClane. 2004. The enteric toxins of Clostridium perfringens. Rev. Physiol. Biochem. Pharmacol. 152:183-204. [DOI] [PubMed] [Google Scholar]
- 34.Songer, J. G. 1997. Clostridial diseases of animals, p. 153-182. In J. I. Rood, B. A. McClane, J. G. Songer, and R. W. Titball (ed.), The clostridia: molecular biology and pathogenesis. Academic Press, London, United Kingdom.
- 35.Songer, J. G. 1996. Clostridial enteric diseases of domestic animals. Clin. Microbiol. Rev. 9:216-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stevens, D. L., J. Mitten, and C. Henry. 1987. Effects of α and θ toxins from Clostridium perfringens on human polymorphonuclear leukocytes. J. Infect. Dis. 156:324-333. [DOI] [PubMed] [Google Scholar]
- 37.Uzal, F. A. 2004. Diagnosis of Clostridium perfringens intestinal infections in sheep and goats. Anaerobe 10:135-143. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.