Abstract
The ongoing outbreak of highly pathogenic avian influenza virus (HPAIV) in birds, the incidence of transmission to humans with a resulting high mortality rate, and the possibility of a human pandemic warrant the development of effective human vaccines against HPAIV. We developed an experimental live-attenuated vaccine for direct inoculation of the respiratory tract based on recombinant avian Newcastle disease virus (NDV) expressing the hemagglutinin (HA) glycoprotein of H5N1 HPAIV (NDV-HA). Expression of the HPAIV HA gene slightly reduced NDV virulence, as evidenced by the increased mean embryo death time and reduced replication in chickens. NDV-HA was administered to African green monkeys in two doses of 2 × 107 infectious units each with a 28-day interval to evaluate the systemic and local antibody responses specific to H5N1 HPAIV. The virus was shed only at low titers from the monkeys, indicative of safety. Two doses of NDV-HA induced a high titer of H5N1 HPAIV-neutralizing serum antibodies in all of the immunized monkeys. Moreover, a substantial mucosal immunoglobulin A response was induced in the respiratory tract after one and two doses. The titers of neutralizing antibodies achieved in this study suggest that the vaccine would be likely to prevent mortality and reduce morbidity caused by the H5N1 HPAIV. In addition, induction of a local immune response in the respiratory tract is an important advantage that is likely to reduce or prevent transmission of the virus during an outbreak or a pandemic. This vaccine is a candidate for clinical evaluation in humans.
Highly pathogenic avian influenza virus (HPAIV) is widespread in birds and occasionally is transmitted to humans, with a resulting high incidence of mortality. In addition, HPAIV can adapt to humans and create a pandemic. In particular, the H5N1 virus has caused 278 reported human infections and 168 deaths (60% mortality [http://www.who.int/csr/disease/avian_influenza/country/cases_table_2007_03_12/en/index.html, as of 2 April 2007]). The development of vaccines against HPAIV has been impeded by its apparent poor immunogenicity (21, 25). In addition, the large-scale production of virus that would be required for a conventional killed vaccine would pose biosafety concerns (19), and a conventional live vaccine would entail risks of genetic exchange with circulating influenza virus strains. We recently evaluated the avian paramyxovirus Newcastle disease virus (NDV) as a vaccine vector administered to the respiratory tract in nonhuman primates and showed that it was highly attenuated and yet induced a substantial immune response against expressed foreign antigens (2). NDV also has the advantage of having a negligible incidence of recombination, which essentially eliminates the concern of genetic exchange with circulating viruses. Here, we have assessed the immunogenicity of recombinant NDV expressing the hemagglutinin (HA) protein of an H5N1 HPAIV virus (NDV-HA) in African green monkeys after respiratory tract mucosal immunization. The vaccine was well tolerated and induced substantial local and systemic immune responses, demonstrating that NDV has potential as a live virus candidate vaccine against HPAIV.
MATERIALS AND METHODS
Generation of recombinant NDV expressing HPAIV HA.
The HA open reading frame (ORF) from HPAIV strain A/Vietnam/1203/2004 (H5N1) virus was optimized for human expression (with the proteolytic cleavage site preserved) (DNA 2.0, Menlo Park, CA) and amplified by PCR. The primers were designed to incorporate an XbaI cleavage site at each end, an NDV gene junction, and an additional sequence in order to maintain the genome length in a multiple of six, which is a requirement for efficient NDV replication (14). The primers also placed the initiation codon in a context favorable for translation and included NDV-specific transcription gene start and gene end sequences. The PCR product was cloned directly into a unique XbaI site in a complete cloned cDNA of the NDV antigenome (mesogenic strain Beaudette C) (2, 23). The NDV recombinant was recovered in HEp-2 cells and passaged in DF-1 chicken embryo fibroblasts (15). The integrity of the inserts was confirmed by reverse transcription-PCR analysis of viral RNA, followed by sequence analysis.
Analysis of HA mRNA and protein.
DF-1 cells were infected with NDV or NDV-HA at a multiplicity of infection of 3 PFU per cell. After 24 h the total RNA was isolated by using an RNeasy total RNA isolation kit (QIAGEN, Valencia, CA). Then, 1.5 μg of total RNA was separated on a 1.2% denaturing agarose gel, transferred to a Hybond N+ membrane (GE Healthcare Bio-Sciences Corp., Piscataway, NJ), and analyzed by Northern blot hybridization (9) with a double-stranded DNA probe prepared from a PCR product of the HA gene cDNA by using the Megaprime DNA labeling system (GE Healthcare Bio-Sciences Corp.) and [α-32P]dCTP. For protein analysis, the cells and the overlying medium were harvested at 24 h postinfection. The cells were lysed in 1× NuPAGE LDS sample loading buffer (Invitrogen, Carlsbad, CA) containing 5% (vol/vol) β-mercaptoethanol and heated at 95°C for 10 min. The medium was clarified by low-speed centrifugation, and virus particles were purified one or two times by ultracentrifugation in a 40 to 60% (wt/wt) sucrose step gradient (26,000 rpm for 90 min in an SW28 rotor [Beckman Coulter, Fullerton, CA]). Virus was collected from the 40 to 60% sucrose interface, concentrated by centrifugation at 90,000 × g, and resuspended in NMH buffer (50 mM HEPES, 150 mM NaCl, 100 mM MgSO4 [pH 7.5]) prior to freezing or reapplication to a sucrose gradient. Virions were reduced and denatured as described above or were further analyzed in native form as follows. Cross-linking studies were done by the addition of formaldehyde to purified virions to a final concentration of 3.7%, followed by incubation at 37°C for 1 h, after which the virions were reduced and denatured. Cell lysates, purified virions, and formaldehyde-treated samples were separated on NuPAGE 10% Bis-Tris gels (Invitrogen) under denaturing and reducing conditions and then transferred to Hybond-P membranes (GE Healthcare Bio-Sciences Corp.). In addition, native NDV and NDV-HA virions were heated for 95°C for 1 h (to reduce and denature the sample without the introduction of reducing or denaturing reagents that might diffuse during electrophoresis and affect other lanes) or left untreated, mixed with NativePAGE sample buffer (Invitrogen) to a final concentration of 1% digitonin, and subjected to electrophoresis on 4 to 16% NativePAGE gels (Invitrogen) under nonreducing and nondenaturing conditions. Native gels were then transferred to Hybond P membranes as described above. Membranes from either reducing/denaturing gels or native gels were blocked in phosphate-buffered saline containing 2% (wt/vol) bovine serum albumin and 0.2% (vol/vol) Tween 20 and incubated with chicken anti-NDV serum (Charles River Laboratories, Wilmington, MA), rabbit polyclonal antibody raised against a synthetic peptide representing the H5N1 HA1 protein (Prosci, Inc., Poway, CA), or a mouse monoclonal antibody raised against recombinant HPAIV HA derived from strain A/Vietnam/1203/2004 (BEI Resources, Manassas, VA). The membranes were incubated with horseradish peroxidase-conjugated goat anti-rabbit immunoglobulin G (IgG; Kirkegaard & Perry Laboratories, Gaithersburg, MD), goat anti-mouse IgG (Kirkegaard & Perry Laboratories), or rabbit anti-chicken IgG (Jackson Immunoresearch Laboratories, Inc., West Grove, PA), developed with ECL detection reagents (GE Healthcare Bio-Sciences Corp.), and exposed to X-ray film. Densitometry was performed on undersaturated film exposures by using Kodak Molecular Imaging Software version 4.0 (Eastman Kodak Company, Rochester, NY). The virion preparations were also analyzed by silver staining of sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) gels using the SilverQuest kit (Invitrogen) according to the manufacturer's recommendations.
Immunoelectron microscopy.
Purified virus particles were bound to 200-mesh Formvar/carbon-coated nickel grids (Electron Microscopy Sciences, Hatfield, PA). For immunolabeling studies, grids were blocked in phosphate-buffered saline containing 2% globulin-free bovine serum albumin (Sigma-Aldrich, St. Louis, MO) and incubated with chicken anti-NDV polyclonal antiserum (Charles River Laboratories) or rabbit anti-HA polyclonal antiserum (Prosci, Inc.). Grids were washed in blocking solution and incubated in goat anti-rabbit IgG antiserum conjugated to 10-nm gold beads (Ted Pella, Inc., Redding, CA) or goat anti-chicken IgG antiserum conjugated to 6-nm gold beads (Electron Microscopy Sciences). The grids received a final wash, followed by negative staining with 1% ammonium molybdate. Grids that were not subjected to immunolabeling were stained with ammonium molybdate immediately after binding to the grid. Grids were examined under a model H7500 transmission electron microscope (Hitachi High Technologies, Schaumburg, IL) at 80 kV. All images were obtained by using an XR100 digital camera system (Advanced Microscopy Techniques, Danvers, MA).
Virological and serological assays.
NDV titers were determined by plaque assay using monolayers of DF-1 cells, which were fixed with ethanol and stained with crystal violet for enumeration of plaques. HPAIV titers (50% tissue culture infectious dose units/ml) were determined on monolayers of Madin-Darby canine kidney cells. NDV-specific serum antibodies were detected by using an HAIV assay with turkey erythrocytes as previously described (2). Serum antibodies specific for HA protein were detected by IgG isotype-specific enzyme-linked immunosorbent assays (ELISAs) essentially as previously described (20). Briefly, 96-well Immulon 1B plates (Dynex Technologies, Inc., Chantilly, VA) were coated with 40 ng of baculovirus-expressed, purified HPAI H5 HA protein (Protein Sciences Corp.)/well. Fourfold serial dilutions of monkey sera were then applied to each well, starting at a dilution of 1:40. The secondary antibody utilized was rabbit anti-monkey-IgG (Kirkegaard & Perry Laboratories), followed by detection with alkaline phosphatase-conjugated goat anti-rabbit antibody (Kirkegaard & Perry Laboratories). The plates were visualized by the addition of pNPP substrate (Sigma-Aldrich), and the resultant optical density at 405 nm was recorded. The reported titer is the log2 of the reciprocal serum dilution at which the optical density was double the background and above 0.2. To detect IgA in nose/throat wash (NW) and tracheal lavage (TL) samples, the samples were concentrated (see below) and analyzed as described above for IgG with several differences. We tested twofold serial dilutions of concentrated mucosal samples, starting at a dilution of 1:2. The secondary antibody used for detection was goat anti-monkey IgA conjugated to horseradish peroxidase (Kirkegaard & Perry Laboratories). Bound antibodies were visualized by the addition of SureBlue 3,3′,5,5′-tetramethylbenzidine (TMB) 1-component peroxidase substrate (Kirkegaard & Perry Laboratories), incubation for 30 min, and the addition of SureBlue TMB stop solution (Kirkegaard & Perry Laboratories). The optical density was measured at 450 nm. The titers were normalized to the total IgA content in each sample, as determined by quantitative IgA ELISA. Briefly, plates were coated with goat anti-monkey IgA (Kirkegaard & Perry Laboratories). Dilutions (1:100 or 1:300) of NW samples or TL samples were then added to each well in triplicate, followed by detection and visualization as described above. To calculate the IgA mass, the resultant optical densities from NW and TL samples were compared to a purified human IgA (Kirkegaard & Perry Laboratories) standard curve. The specificity of the assay for IgA was confirmed by a lack of reactivity of the primary antibody with purified human IgG (Kirkegaard & Perry Laboratories).
To assess the ability of NDV-specific and HPAIV-specific antibodies to neutralize NDV-HA, 250 PFU of NDV-HA or empty NDV vector were combined with serial dilutions of heat-inactivated naive African green monkey serum, NDV-immune African green monkey serum, or HPAIV strain A/Vietnam/1203/2004-immune sheep serum (kindly provided by George Kemble, Medimmune Vaccines). The virus-serum mixtures were incubated at 37°C for 1 h, and the residual NDV infectivity was assayed by titration in DF-1 cells.
Pathogenicity of NDV-HA in chickens.
Mean embryo death time and pathogenicity studies were performed essentially as previously described (11, 23). Briefly, serial dilutions of virus were administered in the allantoic cavity of 9-day-old embryonated chicken eggs (five per virus). The eggs were incubated at 37°C and analyzed three times per day to assess viability. To evaluate pathogenicity in birds, 4-week-old chickens were inoculated with 5 × 104 PFU per nostril and 2 × 104 PFU per eye of NDV or NDV-HA (six animals per virus). The animals were sacrificed on day 4, and samples were taken from the lungs, liver, kidney, intestines, spleens, and brains. Tissue homogenates were prepared, and the virus content was assayed by plaque titration in DF-1 cells. These studies were performed under Animal Biosafety Level 3 conditions.
Immunization of African green monkeys.
African green monkeys (Cercopithecus aethiops), confirmed to be seronegative for NDV by HAI assay, were immunized by the intranasal and intratracheal routes with 107 PFU of NDV-HA per site as described previously (3). On day 42, the animals were inoculated with L-15 medium (Invitrogen) (one-dose group) or NDV-HA (two-dose group) as described above. To assess shedding of the vaccine, NT and TL samples were taken on days 2 and 4 after the first dose essentially as previously described (3), except that greater volumes of medium were used to improve the efficiency of detection of shed virus: 6 ml (3 ml per nostril) for NW and 30 ml for TL per animal. The vaccine virus in NW and TL samples was analyzed by titration in DF-1 cells. To analyze mucosal antibody responses, NW and TL samples were taken on days 0, 42, 56, and 70. After collection, NW and TL samples were concentrated to a final volume of ∼0.5 ml using Vivaspin 30,000 molecular-weight cutoff columns (Sartorius Corp., Edgewood, NY). Animals were observed for any signs of clinical symptoms throughout the course of the study. All primate experiments were performed at Bioqual, Inc. (Rockville, MD), a site approved by the Association for Assessment and Accreditation of Laboratory Care International with a protocol approved by the Animal Care and Use Committee of the National Institute of Allergy and Infectious Disease.
RESULTS
Design, construction, and in vitro characterization of the vaccine virus.
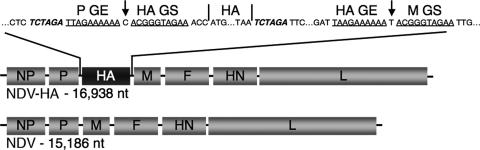
The influenza virus HA glycoprotein is the major viral neutralization and protective antigen. The sequence of the ORF encoding the HA of the HPAIV strain A/Vietnam/1203/2004 (H5N1), a virus isolated from a fatal human infection (8), was codon optimized for expression in mammalian cells. The optimized ORF was placed under the control of NDV transcription signals and inserted into the genome of the mesogenic NDV Beaudette C strain as an additional gene between the P and M genes (Fig. 1). NDV-HA recombinant virus was recovered as described previously (15) and grew to titers of 107.5 to 108.0 PFU/ml in DF-1 chicken embryo cells, similar to those obtained for the parental NDV (not shown), indicating that the HA insert resulted in little or no attenuation in vitro.
FIG. 1.
Genome of recombinant NDV bearing the HPAIV H5 HA coding sequence as an additional gene located between the P and M genes (NDV-HA). A cDNA of the codon-optimized HPAIV HA ORF was cloned into the P-M junction of the NDV antigenomic cDNA using XbaI sites (italicized) such that it was placed under the control of a set of NDV gene start (GS) and gene end (GE) transcription signals (underlined) directing its expression as a separate mRNA. NDV genes are shown as gray boxes, and the HPAIV HA insert is indicated as a black box. The nucleotide sequence spanning the inserted transcription cassette is shown at the top of the figure as positive-sense DNA. The single intergenic nucleotide located on either side of the inserted transcriptional unit is indicated by an arrow.
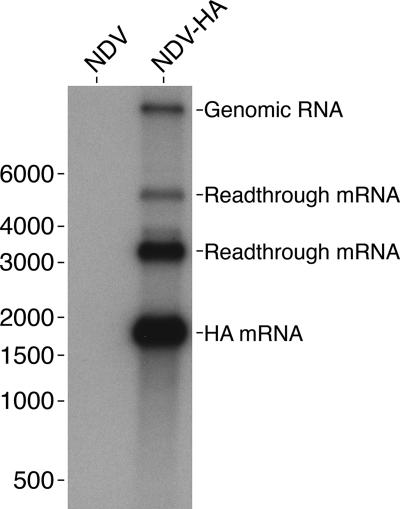
Since premature termination of transcription of the HA gene was observed when it was inserted into the genome of a lentogenic strain of NDV (28), we examined the transcription of the gene in the infected DF-1 cells by Northern blotting (Fig. 2). The most abundantly expressed product had the expected size of the HA mRNA with no smaller bands observed, suggesting a lack of premature transcription termination for our vaccine construct. The larger observed products likely correspond to the full-length genome and various transcriptional readthrough products. Western blot analysis showed that the NDV parent and its NDV-HA derivative expressed similar levels of NDV-specific proteins in DF-1 cells (Fig. 3A, lanes 2 and 3, respectively) and produced similar quantities of released virions (lanes 4 and 5, respectively). Western blot analysis with antibodies specific to the HA1 subunit, which is the larger of the two disulfide linked subunits that constitute the mature HA protein (22), identified a band of the appropriate mobility in cell lysates of NDV-HA, but not in NDV-infected cells (Fig. 3A, lanes 8 and 7, respectively).
FIG. 2.
Northern blotting analysis of the HA transcripts. A portion (1.5 μg) of total intracellular RNA from cells infected with NDV or NDV-HA (as indicated) was separated on a 1.2% agarose gel, transferred to a membrane, and analyzed by hybridization with a radiolabeled HA-specific DNA probe. The positions and nucleotide lengths of single-stranded RNA markers (RiboRuler; Fermentas, Hanover, MD) are shown to the left. The most abundant product had the expected mobility of the full-length HA mRNA, with less abundant bands representing genomic RNA and unidentified readthrough transcripts, as indicated on the right.
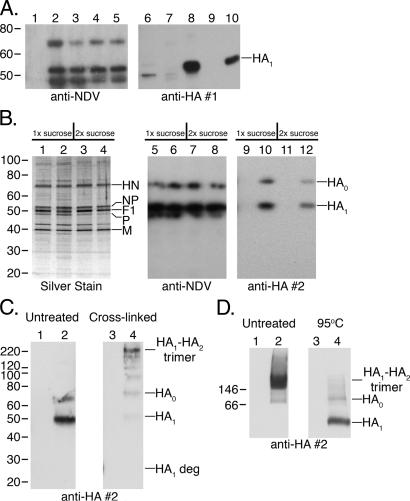
FIG. 3.
Analysis of the expression of the HA protein, its incorporation into the vector particle, and trimerization. (A) Western blot analysis of NDV- and NDV-HA-infected cells and purified virions. Virions were purified from the clarified medium supernatants from infected cells by centrifugation over a sucrose gradient. Whole-cell lysates and purified virions were subjected to SDS-PAGE under denaturing and reducing conditions, followed by Western blot analysis of duplicate gels using antiserum raised against NDV virions (lanes 1 to 5) or a synthetic peptide representing the HPAIV HA1 subunit (lanes 6 to 10). Lanes 1 and 6, uninfected cell lysate; lanes 2 and 7, NDV-infected cell lysate; lanes 3 and 8, NDV-HA-infected cell lysate; lanes 4 and 9, purified NDV virions; lanes 5 and 10, purified NDV-HA virions. Cell lysate samples represent approximately equal numbers of cells, and virion samples represent approximately equal proportions of the purified virus preparations. (B) Analysis of NDV-HA following one (1x sucrose) and two (2x sucrose) rounds of purification by sucrose gradient centrifugation. Samples were subjected to SDS-PAGE under reducing and denaturing conditions. The gel in the panel on the left was analyzed by silver staining; the other two panels are replicate gels that were analyzed by Western blotting with polyclonal antibodies raised against NDV virions (middle panel) or a monoclonal antibody specific to the HA protein (right panel). Lanes 1, 3, 5, 7, 9, and 11, purified NDV virions; lanes 2, 4, 6, 8, 10, and 12, purified NDV-HA virions. The major NDV proteins HN, NP, F1, P, and M were identified according to published studies (2, 7, 18, 29). (C) Cross-linking analysis of the HA protein present in sucrose gradient-purified NDV-HA virions. Aliquots of NDV virions (lanes 1 and 3) or NDV-HA virions (lanes 2 and 4) were mock-treated (lanes 1 and 2) or subjected to cross-linking with formaldehyde (lanes 3 and 4). The samples were subjected to denaturing/reducing SDS, followed by Western blotting with an HA-specific monoclonal antibody. All of the lanes are from a single gel. (D) Nondenaturing PAGE analysis of the HA protein present in sucrose gradient-purified NDV-HA virions. Aliquots of NDV virions (lanes 1 and 3) or NDV-HA virions (lanes 2 and 4) were left undenatured (lanes 1 and 2) or were heated at 95°C for 1 h (lanes 3 and 4), which was done to reduce and denature the samples without introducing diffusible reducing or denaturing agents that might affect adjacent lanes during PAGE. The samples were subjected to nondenaturing PAGE and analyzed by Western blotting with the HA-specific monoclonal antibody. All of the lanes were from a single gel. Molecular masses (in kilodaltons), shown to the left of the blots, were determined by loading a MagicMark XP marker (Invitrogen) on the reducing gels and a NativeMark marker (Invitrogen) on the nonreducing gel.
The HA protein is incorporated into the viral particles but does not increase pathogenicity of the viruses.
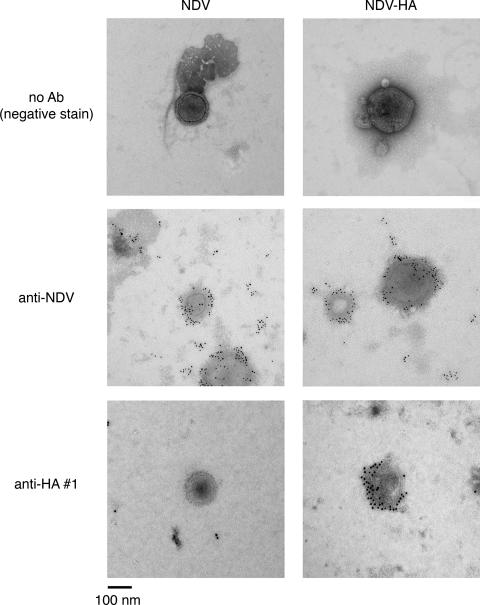
We next subjected NDV and NDV-HA released from infected cells to one or two rounds of sucrose gradient centrifugation followed by SDS-PAGE and silver staining to investigate the purity and content of the preparations (Fig. 3B). The predominant bands in the purified virion preparations corresponded to major NDV proteins (Fig. 3B, left panel). Western blot analysis with anti-NDV antibodies (Fig. 3A, left panel, lanes 4 and 5, and 3B, middle panel) revealed NDV HN and F1 proteins in all viral preparations, and analysis with two different anti-HPAI HA antibodies (Fig. 3A, right panel, lanes 9 and 10, and 3B, right panel) demonstrated the presence of HA1 and the HA0 precursor protein in purified NDV-HA but not in purified NDV. This confirmed the expression of the HA protein and indicated that it is incorporated into the vector virions. However, since both the HA1 and the HA0 proteins comigrated with the more abundant NDV F1 and HN proteins, respectively, they could not be identified by silver staining (Fig. 3B, left panel). In the particular set of blots shown in Fig. 3A, the amount of NDV-specific proteins in the samples of cell lysates versus purified virions was essentially equivalent (lanes 2 and 3 versus lanes 4 and 5, respectively), whereas in the same sample set there was 4.3-fold more HA1 protein in the cell lysate compared to the virion preparation, as determined by densitometric analysis of the blots (Fig. 3A, lanes 8 and 10, respectively). This suggested that the cell-associated HA protein was incorporated into the vector particle with 23% of the efficiency of the vector-specific proteins. Immunoelectron microscopy further confirmed the presence of HPAIV HA protein in the NDV vector virion (Fig. 4). However, NDV and NDV-HA were found to be equally sensitive to complete neutralization by NDV-specific antibodies, and neither virus was sensitive to HPAIV-specific neutralizing antibodies (results not shown). This suggests that the incorporated HA protein did not significantly mediate infection in that setting, at least not in the presence of NDV antibodies.
FIG. 4.
Immunoelectron microscopy of purified NDV and NDV-HA virus particles. Purified virus preparations were adsorbed to grids, and antigens were detected with the same NDV- and HPAIV HA1-specific antibodies used in the Western blot analysis in Fig. 3, as indicated at the left, followed by gold-bead-labeled secondary antibodies. The grids were subjected to negative staining and analyzed by transmission electron microscopy. The virus particle size and morphology correspond to that previously described for NDV: generally rounded particles 100 to 500 nm in diameter (1).
To determine whether the HA protein incorporated into the NDV-HA virions was present in trimers, as would be expected if it was correctly folded and processed, we treated purified NDV and NDV-HA virions with formaldehyde as a cross-linking agent and subjected the preparations to SDS-PAGE under reducing and denaturing conditions followed by Western blot analysis with an HA1-specific monoclonal antibody (Fig. 3C). This showed that formaldehyde-treated virion-associated HA contained a major species that migrated with the expected mobility of an HA1-HA2 trimer, while in the untreated samples, only the monomeric form of the protein was detected. As a second approach, nondenaturing PAGE analysis of purified NDV-HA virions showed that virion-associated HA migrated as a single major high-molecular-weight species with an electrophoretic mobility that was appropriate to be a HA1-HA2 trimer (Fig. 3D). Treatment of the sample at 95°C prior to PAGE resulted in dissociation of the high-molecular-weight complex into discrete bands corresponding to the mobility of the HA0 and HA1 species (Fig. 3D). These results indicate that, as in influenza virions, the HA protein present in the NDV-HA virions was a trimer.
In some cases, insertion of foreign genes into genomes of nonsegmented negative strand viruses results in their reduced ability to replicate at otherwise permissive temperatures (6). To test this possibility, we titrated 107.5 PFU of the NDV or NDV-HA viruses in multiple monolayers of DF-1 cells, incubated the monolayers for 3 days at various temperatures, and determined the virus titers by staining the monolayers with crystal violet. The following titers were observed for NDV and NDV-HA, respectively: at 37°C, 107.6 and 107.6 PFU, and at 39°C, 107.4 and 107.4 PFU. At 41°C, only small pinpoint plaques were observed, and the titers were 107.0 and 106.6 PFU, respectively. No plaques were observed at 43°C. This suggests that insertion of the HA gene did not confer a significant increase in temperature sensitivity on the NDV vector.
When NDV and NDV-HA were inoculated in serial dilutions into embryonated eggs, the mean embryo death time was 56 h for NDV and 61 h for NDV-HA (not shown). We also inoculated chickens by the intranasal and ocular routes with 105 PFU of NDV or NDV-HA per chicken, sacrificed the animals on day 4, and analyzed the levels of infectious virus in the lungs, spleen, liver, kidney, gut, and brain. Although NDV was detected in all six animals inoculated, NDV-HA was detected in only one of six inoculated animals (data not shown). Thus, expression of the HPAIV HA protein by NDV and its incorporation into the vector particle did not confer any additional virulence or significantly change its tissue tropism in this natural avian host; on the contrary, the presence of the HA insert was somewhat attenuating.
Safety and shedding of the vaccine in a nonhuman primate model.
To evaluate the safety and immunogenicity of NDV-HA in a primate model, eight African green monkeys were immunized by the intranasal and intratracheal routes with 107 PFU of NDV-HA per site. On day 42 after the initial immunization, four of the animals received a second dose of the vaccine via the same route, while the other four animals received medium alone. Serum samples, combined NW specimens, and TL specimens were taken at various time points to assess shedding of the NDV vector and the development of systemic and local humoral immune responses. After the first inoculation, seven of the eight animals had evidence of NDV shedding detected in NW and/or TL specimens taken on days 2 and 4 (Table 1). Most samples contained only a small quantity of infectious virus, with titers between 101 and 102 PFU/ml. However, three animals had titers between 102 and 103 PFU/ml in at least one site on at least 1 day, and one animal had a titer of 103.9 PFU/ml in the NW on day 2. In a separate experiment (results not shown), two African green monkeys received 107 PFU of the empty NDV vector, and comparable virus titers were detected in the TL samples (PFU/ml): 102.5 and 101.8 on day 2 and <100.7 and 102.8 on day 4. These results indicate that the HA insert did not detectably affect replication in a nonhuman primate model. We did not analyze vaccine virus shedding after the second dose because our experience with intranasal paramyxovirus-vectored vaccines (4) indicates that the first dose of a vaccine typically prevents detectible shedding of the second dose. However, since the second dose usually boosts the immune response, it is likely that there is limited replication not detectable by sampling of respiratory tract secretions. The comparable levels of replication of NDV-HA and the empty NDV vector in monkeys are in contrast to the data in chickens in which the insert was attenuating (see above). This difference may be explained by the greater level of NDV infection in the natural chicken host, thus allowing for detection of subtle differences in viral replication. Successful vaccines or promising vaccine candidates against human influenza, parainfluenza, and respiratory syncytial viruses typically are shed at titers of 103 to 105 PFU/ml in clinical trials (5, 12, 13), and it is clear that their immunogenicity depends on replication. In comparison, NDV-HA appears to be highly attenuated, perhaps slightly more attenuated than these other live vaccines.
TABLE 1.
Shedding of the NDV-HA vaccine virus in the upper and lower respiratory tracts of African green monkeys after a single inoculationa
| Animal no. | NW (log10 PFU/ml)
|
TL (log10 PFU/ml)
|
||
|---|---|---|---|---|
| Day 2 | Day 4 | Day 2 | Day 4 | |
| 1 | 1.5 | 1.0 | 2.3 | 2.5 |
| 2 | 3.9 | <1.0 | 2.0 | 2.0 |
| 3 | 1.0 | <1.0 | 2.6 | 2.7 |
| 4 | 1.3 | <1.0 | 1.8 | 1.9 |
| 5 | <1.0 | 1.0 | 1.0 | 1.0 |
| 6 | 1.3 | 1.0 | 2.7 | 3.0 |
| 7 | <1.0 | <1.0 | 1.8 | 1.8 |
| 8 | <1.0 | <1.0 | <1.0 | <1.0 |
African green monkeys were infected on day 0 by intranasal and intratracheal routes with 107 PFU of NDV-HA per site. NW and TL samples were obtained on days 2 and 4 after the first dose as described in Materials and Methods. This was part of the experiment shown in Table 2.
Induction of mucosal immune response in the respiratory tract.
To assess local immune responses to the H5 HA protein, we used an ELISA based on baculovirus-expressed H5 HA to measure HA-specific IgA in the upper (NW) and lower (TL) respiratory tract (Table 2). A single vaccine dose did not induce an increase in HA-specific IgA in NW specimens on day 42 after immunization, whereas two doses induced a 17-fold increase by day 70 (28 days after the second dose). In TL specimens, a single dose induced a 47-fold increase in HA specific IgA on day 42 after immunization, whereas two doses induced a further 14-fold increase compared to the one dose group by day 56 (14 days after the second dose). The difference between the one-dose and two-dose groups diminished to fourfold between days 56 and 70 due to a twofold increase in antibody titers in the former group and a twofold decrease in the latter.
TABLE 2.
Mucosal antibody responses in immunized African green monkeys after immunization with NDV-HAa
| Dose group | Animal no.b | HA-specific IgA ELISA titerc
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| NW
|
TL
|
||||||||
| Day 0 | Day 42 | Day 56 | Day 70 | Day 0 | Day 42 | Day 56 | Day 70 | ||
| One dose | 1 | 5.0 | 4.7 | 3.8 | 4.5 | 2.3 | 5.0 | 4.7 | 5.5 |
| 2 | 5.6 | 3.8 | 4.8 | 3.7 | 0.5 | 3.2 | 3.3 | 5.2 | |
| 3 | 4.2 | 3.9 | 4.0 | 3.4 | 1.5 | 5.5 | 5.9 | 6.4 | |
| 4 | 5.2 | 5.9 | 9.5 | 4.7 | 2.1 | 7.4 | 8.4 | 8.0 | |
| Mean | 5.0 | 4.6 | 5.5 | 4.0 | 1.6 | 5.3 | 5.6 | 6.3† | |
| Two doses | 5 | 5.4 | 4.3 | 5.5 | 6.9 | 0.8 | 6.8 | 7.3 | 5.7 |
| 6 | 3.9 | 4.3 | 7.3 | 8.9 | 1.0 | 9.4 | 10.2 | 11.2 | |
| 7 | 3.8 | 4.3 | 7.5 | 11.1 | 1.7 | 10.9 | 10.1 | 9.4 | |
| 8 | 3.2 | 3.4 | 7.2 | 5.2 | 1.1 | 7.6 | 10.1 | 7.2 | |
| Mean | 4.1 | 4.1 | 6.9 | 8.1*d | 1.2 | 8.7 | 9.4 | 8.4‡ | |
Animals were immunized by intranasal and intratracheal routes with 107 PFU per site on day 0 (one-dose group) or on days 0 and 42 (two-dose group).
Mean, mean log2 titer for the four animals in each group.
Mucosal wash specimens were concentrated, and HA-specific IgA titers were determined by ELISA using purified H5 HA as an antigen. These titers were then normalized according to the concentration of total IgA in each sample, which was determined by quantitative ELISA. Titers below the detection limit of 1 were assigned a value of 0.5 prior to normalization. Comparison of the day 0 and the day 70 value using the unpaired Student t test assuming equal variance:
P < 0.05
P < 0.001
P < 0.01.
Comparison of the day 70 value for the two-dose group and the one-dose group using the unpaired Student t test assuming equal variance: P < 0.05.
The vaccine induces high titers of HPAIV neutralizing antibodies.
We next evaluated systemic antibody responses to the vaccine in serum (Table 3). After a single dose of vaccine, all of the animals had a vigorous serum antibody response to the NDV vector as measured by an NDV-specific hemagglutinin inhibition (HAI) assay (Table 2). There also was a substantial increase in NDV-specific HAI titer after the second dose (Table 2). This suggests that the immune response to the first dose did not completely restrict replication of the second dose of the virus, although because of the limitations of using nonhuman primates we did not directly confirm that UV-inactivated virus did not induce a response in primed animals.
TABLE 3.
Serum antibody responses in immunized African green monkeys after immunization with NDV-HAa
| Dose group | Animal no.b | NDV HAI titer
|
HA-specific serum IgG ELISA titer
|
H5N1 HPAIV serum neutralizing antibody titerc
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day 0 | Day 42 | Day 56 | Day 70 | Day 0 | Day 42 | Day 56 | Day 70 | Day 0 | Day 42 | Day 56 | Day 70 | ||
| One dose | 1 | 1.0 | 3.0 | 3.0 | 4.0 | ≤3.3 | 9.3 | 9.3 | 9.3 | ≤2.3 | ≤2.3 | ≤2.3 | ≤2.3 |
| 2 | ≤1.0 | 5.0 | 5.0 | 5.0 | ≤3.3 | 9.3 | 9.3 | 9.3 | ≤2.3 | ≤2.3 | ≤2.3 | ≤2.3 | |
| 3 | ≤1.0 | 4.0 | 5.0 | 5.0 | ≤3.3 | 7.3 | 9.3 | 9.3 | ≤2.3 | ≤2.3 | ≤2.3 | ≤2.3 | |
| 4 | ≤1.0 | 4.0 | 4.0 | 4.0 | ≤3.3 | 9.3 | 9.3 | 9.3 | ≤2.3 | ≤2.3 | ≤2.3 | ≤2.3 | |
| Mean | 1.0 | 4.0 | 4.3 | 4.5d | 3.3 | 8.8 | 9.3 | 9.3 | 2.3 | 2.3 | 2.3 | 2.3 | |
| Two doses | 5 | ≤1.0 | 4.0 | 5.0 | 6.0 | ≤3.3 | 7.3 | 13.3 | 11.3 | ≤2.3 | ≤2.3 | 8.7 | 6.8 |
| 6 | ≤1.0 | 4.0 | 6.0 | 5.0 | ≤3.3 | 7.3 | 11.3 | 11.3 | ≤2.3 | ≤2.3 | 5.6 | 4.6 | |
| 7 | ≤1.0 | 3.0 | 7.0 | 7.0 | ≤3.3 | 9.3 | 13.3 | 13.3 | ≤2.3 | ≤2.3 | 8.3 | 7.7 | |
| 8 | ≤1.0 | 4.0 | 7.0 | 7.0 | ≤3.3 | 9.3 | 17.3 | 15.3 | ≤2.3 | ≤2.3 | 8.8 | 6.8 | |
| Mean | 1.0 | 3.8 | 6.3 | 6.3d,e | 3.3 | 8.3 | 13.8 | 12.8d,e | 2.3 | 2.3 | 7.9 | 6.5d,f | |
Animals were immunized by intranasal and intratracheal routes with 107 PFU per site on day 0 (one-dose group) or on days 0 and 42 (two-dose group).
Mean, mean log2 titer for the four animals in each group. Titers below the detection limit of 2, 5.3, and 3.3 were assigned values of 1.0, 3.3, and 2.3 for the NDV HAI titer, serum IgG titer, and serum neutralizing antibody titer, respectively.
Neutralizing titers are defined as the inverse serum dilution resulting in complete neutralization in 50% of the wells.
Comparison of the day 0 and the day 70 value using the unpaired Student t test assuming equal variance: P < 0.001.
Comparison of the day 70 value for the two-dose group and the one-dose group using the unpaired Student t test assuming equal variance: P < 0.05.
Comparison of the day 70 value for the two-dose group and the one-dose group using the unpaired Student t test assuming equal variance: P < 0.001.
We then used ELISA to measure HA-specific serum IgG titers. A single vaccine dose induced a 39-fold rise in mean serum IgG titer by day 42 that was maintained through day 70, the last day of sampling. A second dose of NDV-HA resulted in a 23-fold-greater level of mean IgG compared to the one dose group on day 56, or a total 1,448-fold increase over the background level (day 0). The IgG titer in two of the four animals that received two doses of the vaccine was slightly decreased between days 56 and 70, an effect that was not observed in any animals that received a single vaccine dose. Nevertheless, the mean titer in the two-dose group on day 70 was 11-fold greater than in the one-dose group and 724-fold above the mean background level (day 0).
Serum samples were next analyzed for their ability to neutralize infectious HPAIV A/Vietnam/1203/2004 virus. Interestingly, despite the substantial induction of HA-specific serum IgG titers observed after either one or two doses of the vaccine, only sera collected after the second dose of the vaccine had detectable HPAIV-neutralizing titers. By day 56 (14 days after the second dose), all four animals achieved neutralizing antibody titers at or above 1:40. A titer of 1:40 determined by HAI has classically been viewed as predictive of protection in human adults (10); however, it is unclear how well HAI titers and protection of human adults against HPAIV correlates with a neutralization titer in nonhuman primates. The neutralizing titers decreased by day 70 (28 days after the second dose) but still remained well above 1:40 in three of four animals. The remaining animal in the two-dose group (animal 6) had a neutralization titer of 1:25 on day 70, which nonetheless likely would be sufficient to prevent death or severe disease upon HPAIV infection, particularly considering that it was associated with a robust mucosal IgA response in every animal.
DISCUSSION
In this study, we have developed a vaccine candidate, NDV-HA, for immunization against H5N1 HPAIV and have tested it in a nonhuman primate model. NDV-HA was highly attenuated in African green monkeys, suggesting that it would also be satisfactorily attenuated in humans. Every animal that received one vaccine dose had substantial serum IgG and mucosal IgA responses detectable by ELISA. Induction of both systemic and local immunity is significant in that, while IgG responses are clearly important for protection, local IgA is thought to be the most potent mediator of protection in the respiratory tract and is particularly important for heterotypic immunity (16). In addition, all four animals receiving two doses of the vaccine achieved serum neutralizing antibody titers equal to or exceeding those considered to be protective against influenza A virus infection.
Other researchers are developing NDV as a possible vaccine vector for protection of birds against HPAIV infection (24, 28), which would provide a bivalent vaccine against two pathogens. We are interested in NDV as a human vaccine vector based on its high level of host range restriction in primates (2). A recent study demonstrated protective efficacy of an NDV-vectored HPAIV vaccine in mice (7). However, the mouse model is an uncertain predictor of NDV-based vaccine efficacy in humans for two reasons. First, it is unrealistic to expect that the level of host range restriction in rodents will be the same as in primates. Second, rodent models frequently provide overly optimistic evaluations of vaccine efficacy. For example, whole-virus inactivated vaccines against avian influenza viruses were highly immunogenic in mice and ferrets (17, 18) but very poorly immunogenic in humans (21, 26, 27). Whether it will be possible to make a single NDV-HA virus that would be acceptably attenuated and immunogenic in both poultry and humans is unclear.
As a human vaccine vector against HPAIV, NDV has several particular advantages. The intranasal route of administration is particularly well suited for the control of a respiratory virus and provides for needle-free immunization and is thus suitable for mass immunization. NDV is highly attenuated for replication in primates and is inefficiently shed. Its replication in nonhuman primates appears to be restricted to the respiratory tract, precluding concerns associated with spread to distal sites. NDV has a negligible incidence of recombination and thus could be used in prospective immunization against HPAIV with negligible risk of genetic exchange with circulating viruses. NDV can be grown efficiently in both embryonated chicken eggs and in Vero cells qualified for vaccine production. These findings identify NDV-HA as a potentially effective vaccine against HPAIV that should be further evaluated in clinical trials.
Acknowledgments
We thank Bradley Finneyfrock for performing the manipulations with the nonhuman primates. We also thank Ernest Williams and Fatemeh Davoodi for performing the NDV HAI assays.
This research was supported in part by the Intramural Research Program of the National Institute of Allergy and Infectious Disease, National Institutes of Health.
We have no commercial interests in vaccines against avian influenza virus.
Footnotes
Published ahead of print on 22 August 2007.
REFERENCES
- 1.Alexander, D. J. 1991. Newcastle disease and other paramyxovirus infections, p. 496-519. In B. W. Calnek, H. J. Barnes, C. W. Beard, W. M. Reid, and H. W. Yoder, Jr (ed.), Diseases of poultry, 9th ed. Iowa State University Press, Ames, IA.
- 2.Bukreyev, A., Z. Huang, L. Yang, S. Elankumaran, M. St. Claire, B. R. Murphy, S. K. Samal, and P. L. Collins. 2005. Recombinant Newcastle disease virus expressing a foreign viral antigen is attenuated and highly immunogenic in primates. J. Virol. 79:13275-13284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bukreyev, A., E. W. Lamirande, U. J. Buchholz, L. N. Vogel, W. R. Elkins, M. St Claire, B. R. Murphy, K. Subbarao, and P. L. Collins. 2004. Mucosal immunization of African green monkeys (Cercopithecus aethiops) with an attenuated parainfluenza virus expressing the SARS coronavirus spike protein for the prevention of SARS. Lancet 363:2122-2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bukreyev, A., P. E. Rollin, M. K. Tate, L. Yang, S. R. Zaki, W. J. Shieh, B. R. Murphy, P. L. Collins, and A. Sanchez. 2007. Successful topical respiratory tract immunization of primates against Ebola virus. J. Virol. 81:6379-6388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clements, M. L., M. H. Snyder, A. J. Buckler-White, E. L. Tierney, W. T. London, and B. R. Murphy. 1986. Evaluation of avian-human reassortant influenza A/Washington/897/80 x A/Pintail/119/79 virus in monkeys and adult volunteers. J. Clin. Microbiol. 24:47-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Durbin, A. P., M. H. Skiadopoulos, J. M. McAuliffe, J. M. Riggs, S. R. Surman, P. L. Collins, and B. R. Murphy. 2000. Human parainfluenza virus type 3 (PIV3) expressing the hemagglutinin protein of measles virus provides a potential method for immunization against measles virus and PIV3 in early infancy. J. Virol. 74:6821-6831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ge, J., G. Deng, Z. Wen, G. Tian, Y. Wang, J. Shi, X. Wang, Y. Li, S. Hu, Y. Jiang, C. Yang, K. Yu, Z. Bu, and H. Chen. 2007. Newcastle disease virus-based live attenuated vaccine completely protects chickens and mice from lethal challenge of homologous and heterologous H5N1 avian influenza viruses. J. Virol. 81:150-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Govorkova, E. A., J. E. Rehg, S. Krauss, H. L. Yen, Y. Guan, M. Peiris, T. D. Nguyen, T. H. Hanh, P. Puthavathana, H. T. Long, C. Buranathai, W. Lim, R. G. Webster, and E. Hoffmann. 2005. Lethality to ferrets of H5N1 influenza viruses isolated from humans and poultry in 2004. J. Virol. 79:2191-2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grosfeld, H., M. G. Hill, and P. L. Collins. 1995. RNA replication by respiratory syncytial virus (RSV) is directed by the N, P, and L proteins; transcription also occurs under these conditions but requires RSV superinfection for efficient synthesis of full-length mRNA. J. Virol. 69:5677-5686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hobson, D., R. L. Curry, A. S. Beare, and A. Ward-Gardner. 1972. The role of serum haemagglutination-inhibiting antibody in protection against challenge infection with influenza A2 and B viruses. J. Hyg. 70:767-777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang, Z., S. Elankumaran, A. S. Yunus, and S. K. Samal. 2004. A recombinant Newcastle disease virus (NDV) expressing VP2 protein of infectious bursal disease virus (IBDV) protects against NDV and IBDV. J. Virol. 78:10054-10063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karron, R. A., R. B. Belshe, P. F. Wright, B. Thumar, B. Burns, F. Newman, J. C. Cannon, J. Thompson, T. Tsai, M. Paschalis, S. L. Wu, Y. Mitcho, J. Hackell, B. R. Murphy, and J. M. Tatem. 2003. A live human parainfluenza type 3 virus vaccine is attenuated and immunogenic in young infants. Pediatr. Infect. Dis. J. 22:394-405. [DOI] [PubMed] [Google Scholar]
- 13.Karron, R. A., P. F. Wright, R. B. Belshe, B. Thumar, R. Casey, F. Newman, F. P. Polack, V. B. Randolph, A. Deatly, J. Hackell, W. Gruber, B. R. Murphy, and P. L. Collins. 2005. Identification of a recombinant live attenuated respiratory syncytial virus vaccine candidate that is highly attenuated in infants. J. Infect. Dis. 191:1093-1104. [DOI] [PubMed] [Google Scholar]
- 14.Kolakofsky, D., T. Pelet, D. Garcin, S. Hausmann, J. Curran, and L. Roux. 1998. Paramyxovirus RNA synthesis and the requirement for hexamer genome length: the rule of six revisited. J. Virol. 72:891-899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krishnamurthy, S., Z. Huang, and S. K. Samal. 2000. Recovery of a virulent strain of Newcastle disease virus from cloned cDNA: expression of a foreign gene results in growth retardation and attenuation. Virology 278:168-182. [DOI] [PubMed] [Google Scholar]
- 16.Liew, F. Y., S. M. Russell, G. Appleyard, C. M. Brand, and J. Beale. 1984. Cross-protection in mice infected with influenza A virus by the respiratory route is correlated with local IgA antibody rather than serum antibody or cytotoxic T-cell reactivity. Eur. J. Immunol. 14:350-356. [DOI] [PubMed] [Google Scholar]
- 17.Lipatov, A. S., E. Hoffmann, R. Salomon, H. L. Yen, and R. G. Webster. 2006. Cross-protectiveness and immunogenicity of influenza A/Duck/Singapore/3/97(H5) vaccines against infection with A/Vietnam/1203/04(H5N1) virus in ferrets. J. Infect. Dis. 194:1040-1043. [DOI] [PubMed] [Google Scholar]
- 18.Lu, X., T. M. Tumpey, T. Morken, S. R. Zaki, N. J. Cox, and J. M. Katz. 1999. A mouse model for the evaluation of pathogenesis and immunity to influenza A (H5N1) viruses isolated from humans. J. Virol. 73:5903-5911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luke, C. J., and K. Subbarao. 2006. Vaccines for pandemic influenza. Emerg. Infect. Dis. 12:66-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McAuliffe, J., L. Vogel, A. Roberts, G. Fahle, S. Fischer, W. J. Shieh, E. Butler, S. Zaki, M. St Claire, B. Murphy, and K. Subbarao. 2004. Replication of SARS coronavirus administered into the respiratory tract of African green, rhesus and cynomolgus monkeys. Virology 330:8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nicholson, K. G., A. E. Colegate, A. Podda, I. Stephenson, J. Wood, E. Ypma, and M. C. Zambon. 2001. Safety and antigenicity of non-adjuvanted and MF59-adjuvanted influenza A/Duck/Singapore/97 (H5N3) vaccine: a randomised trial of two potential vaccines against H5N1 influenza. Lancet 357:1937-1943. [DOI] [PubMed] [Google Scholar]
- 22.Palese, P., and M. L. Shaw. 2007. Orthomyxoviridae: the viruses and their replication, p. 1647-1689. In D. M. Knipe and P. M. Howley (ed.), Fields virology, 5th ed., vol. 2. Lippincott/The Williams & Wilkins Co., Philadelphia, PA. [Google Scholar]
- 23.Panda, A., Z. Huang, S. Elankumaran, D. D. Rockemann, and S. K. Samal. 2004. Role of fusion protein cleavage site in the virulence of Newcastle disease virus. Microb. Pathog. 36:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park, M. S., J. Steel, A. Garcia-Sastre, D. Swayne, and P. Palese. 2006. Engineered viral vaccine constructs with dual specificity: avian influenza and Newcastle disease. Proc. Natl. Acad. Sci. USA 103:8203-8208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rimmelzwaan, G. F., E. C. Claas, G. van Amerongen, J. C. de Jong, and A. D. Osterhaus. 1999. ISCOM vaccine induced protection against a lethal challenge with a human H5N1 influenza virus. Vaccine 17:1355-1358. [DOI] [PubMed] [Google Scholar]
- 26.Stephenson, I., R. Bugarini, K. G. Nicholson, A. Podda, J. M. Wood, M. C. Zambon, and J. M. Katz. 2005. Cross-reactivity to highly pathogenic avian influenza H5N1 viruses after vaccination with nonadjuvanted and MF59-adjuvanted influenza A/Duck/Singapore/97 (H5N3) vaccine: a potential priming strategy. J. Infect. Dis. 191:1210-1215. [DOI] [PubMed] [Google Scholar]
- 27.Stephenson, I., K. G. Nicholson, R. Gluck, R. Mischler, R. W. Newman, A. M. Palache, N. Q. Verlander, F. Warburton, J. M. Wood, and M. C. Zambon. 2003. Safety and antigenicity of whole virus and subunit influenza A/Hong Kong/1073/99 (H9N2) vaccine in healthy adults: phase I randomised trial. Lancet 362:1959-1966. [DOI] [PubMed] [Google Scholar]
- 28.Veits, J., D. Wiesner, W. Fuchs, B. Hoffmann, H. Granzow, E. Starick, E. Mundt, H. Schirrmeier, T. Mebatsion, T. C. Mettenleiter, and A. Romer-Oberdorfer. 2006. Newcastle disease virus expressing H5 hemagglutinin gene protects chickens against Newcastle disease and avian influenza. Proc. Natl. Acad. Sci. USA 103:8197-8202. [DOI] [PMC free article] [PubMed] [Google Scholar]