Abstract
Effective antiviral drugs are essential for early control of an influenza pandemic. It is therefore crucial to evaluate the possible threat posed by neuraminidase (NA) inhibitor-resistant influenza viruses with pandemic potential. Four NA mutations (E119G, H274Y, R292K, and N294S) that have been reported to confer resistance to NA inhibitors were each introduced into recombinant A/Vietnam/1203/04 (VN1203) H5N1 influenza virus. For comparison, the same mutations were introduced into recombinant A/Puerto Rico/8/34 (PR8) H1N1 influenza virus. The E119G and R292K mutations significantly compromised viral growth in vitro, but the H274Y and N294S mutations were stably maintained in VN1203 and PR8 viruses. In both backgrounds, the H274Y and N294S mutations conferred resistance to oseltamivir carboxylate (50% inhibitory concentration [IC50] increases, >250-fold and >20-fold, respectively), and the N294S mutation reduced susceptibility to zanamivir (IC50 increase, >3.0-fold). Although the H274Y and N294S mutations did not compromise the replication efficiency of VN1203 or PR8 viruses in vitro, these mutations slightly reduced the lethality of PR8 virus in mice. However, the VN1203 virus carrying either the H274Y or N294S mutation exhibited lethality similar to that of the wild-type VN1203 virus. The different enzyme kinetic parameters (Vmax and Km) of avian-like VN1203 NA and human-like PR8 NA suggest that resistance-associated NA mutations can cause different levels of functional loss in NA glycoproteins of the same subtype. Our results suggest that NA inhibitor-resistant H5N1 variants may retain the high pathogenicity of the wild-type virus in mammalian species. Patients receiving NA inhibitors for H5N1 influenza virus infection should be closely monitored for the emergence of resistant variants.
The highly pathogenic H5N1 influenza viruses have severely affected the poultry industry and posed a serious threat to human health, resulting in >50% fatality among more than 300 confirmed human cases (49). Although these viruses have yet to acquire efficient transmissibility between humans, their wide geographical dissemination, broad host range, and high pathogenicity raise concern about the severity of a possible pandemic. In the early stage of an influenza pandemic, unless antigenically matched vaccines are available, antivirals offer the best hope of preventing the spread of infection. The two classes of antivirals available for influenza prophylaxis and treatment are the adamantanes (amantadine and rimantadine), which target the M2 ion channel of influenza A virus, and neuraminidase (NA) inhibitors (NAIs) (oseltamivir and zanamivir), which target the NA glycoproteins of influenza A and B viruses.
One of the disadvantages of antiviral therapy is the emergence of drug-resistant variants. Fully pathogenic and transmissible adamantane-resistant H1N1 and H3N2 influenza virus variants emerge rapidly posttreatment (15, 17). Further, a high percentage of the recently isolated human H3N2 (4) and avian highly pathogenic H5N1 (23, 42) influenza viruses contain M2 amino acid changes that could confer resistance to adamantanes. Zanamivir-resistant influenza A virus variants have been isolated only from immunocompromised patients (11, 24). Depending on the detection method, oseltamivir-resistant variants have been identified in approximately 5% to 18% of children and fewer than 1% of adults during treatment and in approximately 0.5% of 2,287 worldwide community isolates (16, 27, 33, 43, 48). It is not clear at what frequency oseltamivir-resistant variants emerge during treatment in patients infected with H5N1 viruses. To date, only a few reports are available; they describe the emergence of variants with H274Y or N294S NA amino acid substitutions in five oseltamivir-treated patients with H5N1 virus infection (8, 29, 35, 40).
The clinical relevance of NAI-resistant H5N1 variants is unknown, and it is not clear whether their phenotype will resemble that of resistant H1N1 variants. NAI-resistant variants have been reported to have compromised viral fitness (5, 12, 18, 25, 44). In the N1 subtype, an oseltamivir-resistant A/Texas/36/91 (H1N1) clinical isolate with an H274Y NA mutation was less infectious than the wild-type virus in vitro and in vivo (25). However, a recombinant A/WSN/33 (H1N1) virus with the H274Y NA mutation showed compromised replication efficiency only at early time points in vitro (1, 2) and was as lethal to mice as the wild-type virus (1). In the three case reports describing the emergence of NAI-resistant H5N1 variants in five patients, the clinical outcomes differed. In one case, a subpopulation of variants containing H274Y or N294S NA mutations was identified in a patient with H5N1 virus in Vietnam receiving a prophylactic dose (75 mg once daily) of oseltamivir; the therapeutic dose (75 mg twice daily) was then given, and the patient survived (29). The second report described the identification of H274Y NA mutants as the dominant virus population in two other H5N1-infected patients in Vietnam during or shortly after oseltamivir treatment; both patients succumbed (8). The most recent report described the detection of the N294S NA mutation from specimens collected from two patients with H5N1 virus in Egypt before and after oseltamivir treatment; the source of the NA mutation is under investigation, and both patients succumbed to infection (40).
Because of the importance of optimal pandemic preparedness, it is essential to determine whether oseltamivir-resistant H5N1 variants retain their infectivity and pathogenicity in mammalian hosts. The potential clinical significance of such variants as evaluated using small animal models may provide insights for clinical management of human H5N1 infection. We used mutagenesis and plasmid-based reverse genetics (20, 41) to generate recombinant A/Vietnam/1203/04 (H5N1) influenza viruses (VN1203) containing either the wild-type NA or a single amino acid change at NA residue 119 (E→G), 274 (H→Y), 292 (R→K), or 294 (N→S). For comparison, we generated recombinant A/Puerto Rico/8/34 (H1N1) influenza viruses (PR8) carrying the same NA mutations. The fitnesses and pathogenicities of the recombinant viruses were characterized in vitro and in vivo.
MATERIALS AND METHODS
Compounds.
The NAI oseltamivir carboxylate (oseltamivir) [(3R,4R,5S)-4-acetamido-5-amino-3-(1-ethylpropoxy)-1-cyclohexene-1-carboxylic acid] was provided by F. Hoffmann-La Roche, Inc. (Basel, Switzerland); zanamivir (4-guanidino-Neu5Ac2en) was provided by the R.W. Johnson Pharmaceutical Research Institute (Raritan, NJ). The compounds were dissolved in distilled water, and aliquots were stored at −20°C until they were used.
Cells.
Madin-Darby canine kidney (MDCK) cells and human embryonic kidney cells transformed with large T antigen (293T cells) were obtained from the American Type Culture Collection (Manassas, VA). MDCK cells transfected with cDNA encoding human 2,6-sialyltransferase (MDCK-SIAT1 cells) were kindly provided by Mikhail N. Matrosovich and maintained as described previously (32, 50).
Generation of recombinant influenza viruses.
The construction of plasmids containing the full-length cDNA of PR8 (H1N1) or VN1203 (H5N1) influenza viruses was described previously (19, 41). Mutations encoding substitutions at conserved NA residues (E119G, H274Y, R292K, and N294S) were separately introduced into the NA plasmids by using a QuikChange site-directed mutagenesis kit (Stratagene, La Jolla, CA). The constructed plasmids were sequenced to ensure their identity to the field strain. Recombinant viruses were rescued by transfecting 293T cells (20). One passage in MDCK cells (at a multiplicity of infection [MOI] of 0.01 to 0.001 PFU/cell with incubation at 37°C for 72 h) was used to prepare stocks of all recombinant viruses except the recombinant VN1203 wild-type virus, which was prepared in 10-day-old embryonated chicken eggs (0.1 ml transfection supernatant was injected into the allantoic cavities of the eggs and incubated at 35°C for 48 h). The hemagglutinin (HA) and NA gene sequences of all stock recombinant viruses were verified. All experiments with recombinant VN1203 (H5N1) viruses were conducted in a USDA-approved biosafety level 3+ containment facility.
Infectivity.
The 50% tissue culture infectious dose (TCID50 ) was determined in MDCK and MDCK-SIAT1 cells with 10-fold serially diluted viruses incubated at 37°C for 72 h. The 50% egg infectious dose (EID50 ) was determined in 10-day-old embryonated chicken eggs with 10-fold serially diluted viruses incubated at 35°C for 48 h. The TCID50 and EID50 values were calculated by the Reed-Muench method (38).
Replication kinetics.
To determine multistep growth curves, MDCK and MDCK-SIAT1 cells were infected with viruses at an MOI of 0.0001 PFU/cell. After incubation, the cells were washed and overlaid with infection medium [minimal essential medium with 0.3% bovine serum albumin and 1 μg/ml l- (tosylamido-2-phenyl)ethylchloromethylketone (TPCK)-treated trypsin]. TPCK-trypsin was not added for infection with recombinant H5N1 viruses, which have a multiple-basic-amino-acid motif at the HA cleavage site. Supernatants were collected 12, 24, 36, 48, and 60 h postinfection and stored at −70°C for titration.
Plaque assays.
Confluent MDCK cells were incubated at 37°C for 1 h with 10-fold serial dilutions of virus in 1 ml infection medium. The cells were then washed and overlaid with freshly prepared minimal essential medium containing 0.3% bovine serum albumin and 0.9% Bacto agar, with or without 1 μg/ml TPCK-trypsin, and incubated at 37°C for 72 h. The plaques were stained with 0.1% crystal violet solution containing 10% formaldehyde, and the PFU per ml were determined.
NA activity.
A modified fluorometric assay was used to determine the NA activities of the recombinant viruses (13, 36). We measured the NA enzyme kinetics at pH 6.5 with 33 mM 2-(N-morpholino)ethanesulfonic acid hydrate (MES) (Sigma-Aldrich, Inc., St. Louis, MO), 4 mM CaCl2, and fluorogenic substrate 2′-(4-methylumbelliferyl)-α-d-N-acetylneuraminic acid (MUNANA) (Sigma-Aldrich, Inc., St. Louis, MO), with a final substrate concentration of 0 to 3333.3 μM. All recombinant viruses were standardized to an equivalent dose of 107.5 PFU/ml. The reaction was conducted at 37°C in a total volume of 50 μl, and the fluorescence of the released 4-methylumbelliferone was measured every 92 s for 45 min in a Fluoroskan II instrument (Labsystems, Helsinki, Finland) using excitation and emission wavelengths of 355 and 460 nm, respectively. The enzyme kinetic data were fit to the Michaelis-Menten equation by using nonlinear regression (GraphPad Prism 4; GraphPad, San Diego, CA) to determine the Michaelis constant (Km) and maximum velocity (Vmax ) of substrate conversion.
NA inhibition assays.
NA inhibition was assayed with viruses standardized to equivalent NA enzyme activity. Viruses were first incubated with oseltamivir or zanamivir at concentrations of 0.00005 to 10 μM at 37°C for 30 min, and the mixtures were then incubated with MUNANA substrate at a final concentration of 167 μM (13) at 37°C for 30 min. The reaction was stopped by adding 150 μl stop solution (0.014 M NaCl and 0.1 M glycine in 25% ethanol, pH 10.7). The drug concentration that inhibited 50% of the NA enzymatic activity (IC50 ) was determined from the dose-response curve.
Reverse transcription-PCR and sequencing.
The NA genes of viruses that formed morphologically different plaques were analyzed as follows. The plaques were visualized by staining with 0.01% neutral red and were individually picked and incubated overnight at 4°C in 250 μl of phosphate-buffered saline (PBS). The RNeasy kit (QIAGEN, Chatsworth, CA) was used to extract viral RNA, and the one-step reverse transcription-PCR kit (QIAGEN) and universal primers (21) were used for amplification. Amplified viral sequences obtained after passage in MDCK cells were analyzed by direct sequencing or with TOPO TA cloning kit for sequencing (Invitrogen). The sequences were determined by the Hartwell Center for Bioinformatics and Biotechnology at St. Jude Children's Research Hospital by using BigDye Terminator (version 3) chemistry and synthetic oligonucleotides. Samples were analyzed on Applied Biosystems 3700 DNA analyzers.
Pathogenicity and lethality in BALB/c mice.
To determine the 50% mouse lethal dose (MLD50 ), we anesthetized groups of five female 6-week-old BALB/c mice (Jackson Laboratories, Bar Harbor, ME) with isoflurane and intranasally inoculated them with 50 μl of 10-fold serial dilutions of recombinant VN1203 (H5N1) or PR8 (H1N1) viruses in PBS. The MLD50 values were calculated after a 21-day observation period by the Reed-Muench method (38). The determined values for 1 MLD50 of the recombinant viruses were expressed as PFU. To monitor survival, we inoculated groups of 15 and 10 mice, respectively, with recombinant VN1203 (10 PFU/mouse) or PR8 (100 PFU/mouse) viruses. To evaluate the replication kinetics and pathogenicities of the recombinant viruses in vivo, we euthanized three mice on days 1, 3, and 6 after inoculation; removed the lungs, brain, and blood; and homogenized the organs and suspended them in 1 ml of PBS. Virus titers in each organ and blood sample were determined by inoculating embryonated chicken eggs with serial dilutions of the suspensions. Titers were calculated by the method of Reed and Muench (38) and expressed as mean log10 EID50 /ml ± standard deviation (SD). Animal use was conducted under applicable laws and guidelines, with prior approval of the St. Jude Children's Research Hospital Animal Care and Use Committee.
RESULTS
Generation and in vitro characterization of the recombinant viruses.
We introduced the E119G, H274Y, R292K, and N294S NA mutations into the background of recombinant VN1203 (H5N1) influenza virus (yielding the constructs VN1203-E119G, VN1203-H274Y, VN1203-R292K, and VN1203-N294S) and into the background of recombinant PR8 (H1N1) influenza virus (yielding the constructs PR8-E119G, PR8-H274Y, PR8-R292K, and PR8-N294S). The recombinant VN1203-H274Y and VN1203-N294S H5N1 virus constructs grew to comparable titers in eggs, MDCK cells, and MDCK-SIAT1 cells (Table 1). They formed homogeneous large plaques (diameter, 1.7 to 2.8 mm) in MDCK cells, although the VN1203-H274Y plaques were smaller than the VN1203 plaques (P < 0.05). Sequence analysis of the stock virus and individual plaques obtained in MDCK cells revealed that the introduced H274Y and N294S NA mutations were stably maintained in the VN1203 virus, and no additional HA mutations were observed (data not shown). In contrast, the growth of VN1203-E119G and VN1203-R292K viruses in eggs or MDCK cells was approximately 1 to 3 logs lower than that of the wild-type VN1203 virus (Table 1). In addition, the VN1203-E119G and VN1203-R292K viruses formed a mixture of small and large plaques in MDCK cells. Direct sequencing of the stock VN1203-E119G virus or sequence analysis of individually picked large and small plaques revealed that the E119G NA mutation was stably maintained in both small and large plaques, but individually picked large plaques contained a subpopulation with a V→F amino acid change at residue 200 or an R→K change at residue 212 of HA (numbering is based on the H5 HA glycoprotein throughout). The stock VN1203-R292K virus contained a mixture of viruses with R or K at NA residue 292 as well as an Y157H substitution in the HA. The yields of VN1203-E119G and V1203-R292K viruses in cell culture were less than that of the recombinant VN1203 virus (Table 1).
TABLE 1.
Growth of the recombinant H5N1 and H1N1 influenza viruses
| Recombinant virus | Viral yielda in:
|
Plaque sized | ||
|---|---|---|---|---|
| Eggsb | MDCK cellsc | MDCK-SIAT1 cellsc | ||
| H5N1 viruses | ||||
| VN1203 | 9.4 ± 0.4 | 8.7 ± 0.2 | 8.9 ± 0.3 | 2.8 ± 0.3 |
| VN1203-H274Y | 9.1 ± 0.1 | 9.0 ± 0.2 | 8.8 ± 0.7 | 1.7 ± 0.4* |
| VN1203-N294S | 9.2 ± 0.0 | 8.7 ± 0.1 | 8.7 ± 0.4 | 2.1 ± 0.3 |
| VN1203-E119G | 8.4 ± 0.2 | 6.6 ± 0.4* | 5.4 ± 0.1* | Heterogeneouse |
| VN1203-R292K | 8.0 ± 0.6 | 7.8 ± 0.2* | 7.4 ± 0.1* | Heterogeneous |
| H1N1 viruses | ||||
| PR8 | 10.0 ± 0.4 | 8.4 ± 0.1 | 8.4 ± 0.1 | 0.9 ± 0.1 |
| PR8-H274Y | 8.6 ± 0.2* | 7.8 ± 0.2 | 7.7 ± 0.3 | 0.5 ± 0.1* |
| PR8-N294S | 9.5 ± 0.4 | 8.4 ± 0.1 | 7.8 ± 0.3 | 0.8 ± 0.1 |
| PR8-E119G | 7.1 ± 0.5* | 5.8 ± 1.1* | 4.6 ± 1.5* | Heterogeneous |
| PR8-R292K | 7.0 ± 0.4* | 5.3 ± 1.5* | 4.0 ± 1.9* | Heterogeneous |
*, P < 0.05 compared to value for wild-type virus.
Values are the log10 EID50 ± SD/ml from three independent determinations.
Values are the log10 TCID50 ± SD/ml from three independent determinations.
Plaque assays were performed in MDCK cells. Values are mean plaque diameter (mm) ± SD as measured by using the Finescale comparator (Los Angeles, CA).
Heterogeneous plaques ranged in size from pinpoints to the size of the recombinant wild-type virus plaques.
Of the recombinant PR8 (H1N1) viruses, only virus carrying the N294S NA mutation showed growth comparable to that of the PR8 virus in eggs, MDCK cells, and MDCK-SIAT1 cells (Table 1). The PR8-H274Y virus formed smaller plaques (P < 0.05) and replicated to a lower titer in eggs than did PR8 virus (Table 1). The PR8-E119G and PR8-R292K viruses showed the most compromised growth and formed a mixture of small and large plaques in MDCK cells, as had the VN1203-E119G and VN1203-R292K viruses (Table 1). The genetic stability of the PR8-H274Y and PR8-N294S viruses was further analyzed with the TOPO TA cloning kit for sequencing (Invitrogen). Ten plasmids of the NA genes were sequenced for each virus, and all clones contained the introduced NA mutation.
Overall, our results suggested that the H274Y and N294S NA mutations are stably maintained in the recombinant VN1203 (H5N1) or PR8 (H1N1) virus background. Recombinant VN1203 or PR8 viruses with these two mutations generally showed growth comparable to that of the homologous wild-type virus, with the exception of 25-fold-reduced yields of the PR8-H274Y virus in eggs. Clearly, the E119G and R292K mutations cannot be stably maintained in either virus background. Therefore, recombinant viruses with these mutations were not further characterized.
Susceptibility to NAIs in vitro.
An enzymatic NA inhibition assay was used to characterize the susceptibilities of recombinant VN1203 (H5N1) and PR8 (H1N1) viruses to oseltamivir and zanamivir (Table 2). The susceptibilities of VN1203-H274Y and PR8-H274Y viruses to oseltamivir were markedly reduced (mean IC50 increases, 1,672-fold and 292-fold, respectively). NA inhibition assays showed that both viruses are susceptible to zanamivir. The susceptibilities of VN1203-N294S and PR8-N294S viruses to oseltamivir were moderately reduced (mean IC50 increases, 21-fold and 83-fold, respectively). A slightly reduced susceptibility of VN1203-N294S and PR8-N294S viruses to zanamivir was detected by NA inhibition assay (mean IC50 increase, threefold). Overall, our results confirmed that H274Y and N294S mutations in the N1 subtype confer resistance to oseltamivir (1, 29); in addition, a slightly reduced susceptibility to zanamivir was detected with the N294S mutation.
TABLE 2.
Susceptibility of the recombinant H5N1 and H1N1 influenza viruses to NAIs
| Recombinant virus | NA inhibition assay results for:
|
|||
|---|---|---|---|---|
| Oseltamivir
|
Zanamivir
|
|||
| Mean IC50 ± SD (nM)a | Fold changeb | Mean IC50 ± SD (nM) | Fold change | |
| H5N1 viruses | ||||
| VN1203 | 0.3 ± 0.1 | 1 | 1.4 ± 0.4 | 1 |
| VN1203-H274Y | 501.7 ± 135.4 | 1,672 | 2.4 ± 0.7 | 2 |
| VN1203-N294S | 6.4 ± 2.0 | 21 | 4.3 ± 0.7 | 3 |
| H1N1 viruses | ||||
| PR8 | 4.2 ± 0.9 | 1 | 0.7 ± 0.1 | 1 |
| PR8-H274Y | 1,226.6 ± 371.0 | 292 | 0.8 ± 0.1 | 1 |
| PR8-N294S | 350.1 ± 10.4 | 83 | 2.3 ± 0.1 | 3 |
The concentration of NAIs that reduced NA activity by 50% relative to a reaction mixture containing virus but no inhibitor. Values are from three independent experiments.
Multiple of the value obtained for the recombinant wild-type virus.
Replication kinetics in vitro.
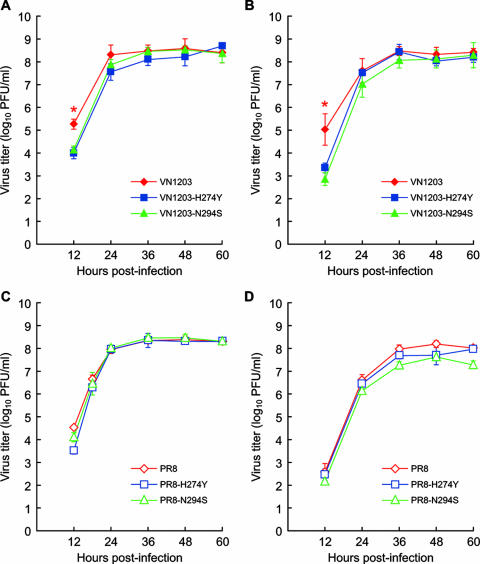
To further evaluate the effect of the H274Y and N294S NA mutations on viral growth, we assayed the yields of the recombinant VN1203 (H5N1) and PR8 (H1N1) viruses after multiple replication cycles in MDCK cells (which exhibit more α-2,3-linked terminal sialic acid [SA] than α-2,6-linked terminal SA on the cell surface) and MDCK-SIAT1 cells (which exhibit more α-2,6-linked terminal SA than α-2,3-linked terminal SA on the cell surface) (32). At 12 hours after infection, the yields of the VN1203 (H5N1) recombinant viruses carrying the drug-resistant NA mutations H274Y and N294S were only approximately 1 log lower than that of the VN1203 (H5N1) virus in both MDCK and MDCK-SIAT1 cells (Fig. 1A and B). However, at 24 h after infection, these viruses reached titers comparable to those of the VN1203 (H5N1) virus in both cell lines (Fig. 1A and B). The recombinant PR8 (H1N1) viruses did not show significantly altered replication kinetics in either MDCK or MDCK-SIAT1 cells (Fig. 1C and D). Therefore, neither the H274Y nor the N294S drug-resistant NA mutation significantly impaired the replication efficiency of the VN1203 (H5N1) or PR8 (H1N1) viruses in vitro, regardless of avian-like (α-2,3-linked) or human-like (α-2,6-linked) SA distribution on the cell surface.
FIG. 1.
Replication kinetics of the recombinant viruses in vitro. (A and B) Multistep growth curves for the recombinant VN1203, VN1203-H274Y, and VN1203-N294S viruses in MDCK (A) and MDCK-SIAT1 (B) cells. (C and D) Multistep growth curves for the recombinant PR8, PR8-H274Y, and PR8-N294S viruses in MDCK (C) and MDCK-SIAT1 (D) cells. Confluent cells were infected with recombinant viruses at an MOI of 0.0001 PFU/cell. The virus yield was titrated in MDCK cells at 12, 24, 36, 48, and 60 h postinfection. Each data point represents viral yield (log10 PFU ± SD/ml) from three independent experiments. *, P < 0.05 compared to value for wild-type virus.
We further verified the stability of H274Y and N294S mutations after multiple cycles of replication in MDCK or MDCK-SIAT1 cells. We analyzed the HA and NA sequences of PR8-H274Y and PR8-N294S recombinant viruses at 60 h postinfection at an MOI of 0.0001 PFU/cell. Direct sequencing revealed the stability of the H274Y and N294S mutations in the recombinant PR8 virus background, as no changes was detected in the HA and NA genes.
Pathogenicity and lethality in vivo.
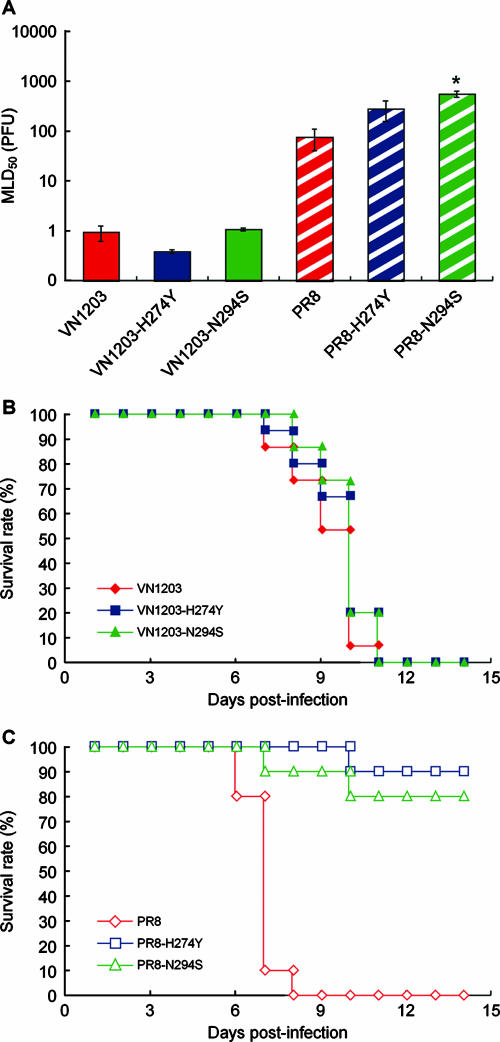
Using a BALB/c mouse model, we compared the lethalities of the NAI-resistant recombinant viruses with those of the VN1203 (H5N1) and PR8 (H1N1) viruses. The VN1203, VN1203-H274Y, and VN1203-N294S viruses were all highly lethal at the inoculation dose of 10 PFU/mouse (1 MLD50 values for the VN1203, VN1203-H274Y, and VN1203-N294S viruses were approximately 1 PFU) (Fig. 2A). No significant differences were observed in the survival rate or mean survival days (range, 9.2 ± 0.3 to 9.8 ± 0.2 days) between the three H5N1 viruses at inoculation dose of 10 PFU/mouse (Fig. 2B). Virus titers in blood, brain, and lungs on days 1, 3, and 6 postinoculation did not reveal significant differences in the replication kinetics of the three H5N1 viruses in vivo (Fig. 3A). Therefore, the recombinant VN1203 (H5N1) viruses with the H274Y or N294S NA mutation are NAI resistant and show no loss of lethality or pathogenicity in BALB/c mice.
FIG. 2.
Lethality of the recombinant viruses in a BALB/c mouse model. (A) MLD50 s of the recombinant viruses (expressed in PFU ± SD). (B and C) Survival of BALB/c mice inoculated with 10 PFU of recombinant VN1203, VN1203-H274Y, or VN1203-N294S virus (B) or 100 PFU of recombinant PR8, PR8-H274Y, or PR8-N294S virus (C). *, P < 0.05 compared to value for wild-type virus.
FIG. 3.
Virus titers in BALB/c mouse tissue at 1, 3, and 6 days after inoculation (d.p.i.). (A) Titers (log10 EID50 /ml) in blood, brain, and lungs after inoculation with 10 PFU of recombinant VN1203, VN1203-H274Y, or VN1203-N294S virus. (B) Titers (log10 EID50 /ml) in lungs after inoculation with 100 PFU of recombinant PR8, PR8-H274Y, or PR8-N294S virus. Each data point represents the value in an inoculated mouse, and the lines represent the mean values from three mice.
The lethalities of the PR8-H274Y and PR8-N294S viruses was 3.7-fold (P = 0.24) and 7-fold (P < 0.05) less than that of the recombinant PR8 (H1N1) virus, respectively. The mean MLD50 s ± SD of the PR8, PR8-H274Y, and PR8-N294S viruses were 74 ± 34, 277 ± 122, and 546 ± 80 PFU, respectively (Fig. 2A). After inoculation with 100 PFU of virus, the survival rates were 0% for PR8, 90% for PR8-H274Y, and 80% for PR8-N294S virus (Fig. 2C). However, we found no significant differences between the PR8, PR8-H274Y, and PR8-N294S virus titers in mouse lungs on day 1, 3, or 6 postinoculation (Fig. 3B). No virus was detected in the blood or the brains of mice on days 1, 3, and 6 after inoculation with the PR8 (H1N1) viruses (data not shown). When the inoculation dose was increased to 1,000 PFU, no significant difference in survival rate was observed between mice inoculated with the PR8, PR8-H274Y, and PR8-N294S viruses (survival rate, 0% [data not shown]).
Overall, we observed that the VN1203-H274Y and VN1203-N294S viruses exhibit lethality or pathogenicity comparable to that of the recombinant VN1203 (H5N1) virus in mice. In the recombinant PR8 (H1N1) virus background, the H274Y and N294S mutations slightly reduced the lethality of recombinant PR8 (H1N1) viruses (3.7-fold and 7-fold reductions, respectively).
NA enzyme kinetics.
To evaluate the impact of the H274Y and N294S mutations on NA enzyme activity, we determined the NA enzyme Kms and Vmax s of recombinant viruses standardized to an equivalent virus dose of 107.5 PFU/ml (Table 3). The Km provides an approximation of the substrate concentration required for significant catalysis to occur, while the Vmax provides an approximation for the NA enzyme activity at the given standardized virus dose. The Km values determined with MUNANA substrate concentrations of 0 to 3333.3 μM were in general higher than the Km values reported for expressed H1N1 (37, 47) or H5N1 (37) virus NA protein determined at a substrate concentration of 5 to 100 μM. The Km values of the PR8-H274Y and PR8-N294S NA were significantly higher (P < 0.05) than that of PR8 NA, suggesting that activation of catalysis by the mutant NA requires a higher substrate concentration (Table 3). The N294S mutation increased the Km of VN1203 NA, but the difference was not statistically significant (Table 3). Interestingly, the H274Y mutation lowered the Km of VN1203 NA, but again the difference was not statistically significant (Table 3). Overall, the H274Y and N294S NA mutations had less effect on the Km value of VN1203 NA than on that of PR8 NA.
TABLE 3.
NA enzyme kinetics of the recombinant H5N1 and H1N1 influenza viruses
| Recombinant virus | Mean Km ± SE (μM)a (95% CI) |
Vmax ratio
|
|
|---|---|---|---|
| Parental NAb | VN1203 NAc | ||
| H5N1 viruses | |||
| VN1203 | 213.7 ± 73.5 (47.48-379.9) | 1.00 | 1.00 |
| VN1203-H274Y | 94.4 ± 32.1 (21.74-167.1) | 0.28 | 0.28 |
| VN1203-N294S | 266.0 ± 58.9 (132.7-399.3) | 0.33 | 0.33 |
| H1N1 viruses | |||
| PR8 | 84.6 ± 16.1 (48.26-121.0) | 1.00 | 0.07 |
| PR8-H274Y | 275.5 ± 28.5 (211.1-339.9) | 0.88 | 0.06 |
| PR8-N294S | 359.2 ± 40.1 (268.6-449.8) | 0.88 | 0.06 |
The substrate concentration that resulted in a half-maximal catalytic rate. The enzyme kinetic data were fit to the Michaelis-Menten equation using GraphPad Prism 4. Values are from triplicates of one representative experiment.
Ratio of the NA Vmax of the respective recombinant viruses to the Vmax of the parental VN1203 or PR8 NA.
Ratio of the NA Vmax of the respective recombinant viruses to the Vmax of VN1203 NA. The recombinant VN1203, VN1203-H274Y, VN1203-N294S, and PR8 viruses were tested in parallel, and the ratios of PR8-H274Y and PR8-N294S to VN1203 were calculated on the basis of parallel tests of PR8, PR8-H274Y, and PR8-N294S viruses.
We determined the NA enzymatic Vmax of each recombinant virus at a standardized amount of virus, and the ratios of the Vmax s of the recombinant virus and parental NA glycoproteins are shown in Table 3. The Vmax ratio is used as an indicator for relative NA activity between virus constructs. The Vmax ratio of VN1203-H274Y versus VN1203 was 0.28, and that of VN1203-N294S versus VN1203 was 0.33 (P < 0.05), suggesting that both mutations significantly decrease VN1203 NA enzyme activity (Table 3; Fig. 4A). The H274Y and N294S mutations also reduced the activity of the PR8 NA (Vmax ratios, 0.88) (Table 3, Fig. 4B). We then determined the NA enzymatic Vmax ratios of all viruses in relation to VN1203 virus and observed that the ratio of the Vmax of the PR8 (H1N1) viruses to that of VN1203 (H5N1) was only 0.06 to 0.07 (Table 3 and Fig. 4A).
FIG. 4.
NA enzyme kinetics of the recombinant viruses, showing the substrate conversion velocity (V0 ) of NA as a function of substrate concentration. (A) Recombinant VN1203, VN1203-H274Y, VN1203-N294S, and PR8 viruses; (B) recombinant PR8 viruses. The fluorogenic MUNANA substrate was used at final concentrations of 0 to 3333 μM. All recombinant viruses were standardized to an equivalent virus dose of 107.5 PFU/ml. The reaction was conducted at 37°C, and fluorescence was measured every 92 s for 45 min using excitation and emission wavelengths of 355 and 460 nm, respectively.
Overall, the Km values suggest that the VN1203 NA function was less affected by the H274Y and N294S mutations than that of the PR8 NA glycoprotein. We observed that the NA activity of the avian-like VN1203 virus was significantly greater than that of the human-like PR8 virus. Although the NA activity of VN1203 virus was reduced by the H274Y or N294S mutation, it remained sufficiently high to sustain the fitness of the NAI-resistant mutants in vitro and in the BALB/c mouse model.
DISCUSSION
To evaluate whether oseltamivir-resistant H5N1 variants retain their infectivity and pathogenicity in mammalian hosts, we studied the effects of four NAI resistance associated NA mutations in recombinant VN1203 (H5N1) and PR8 (H1N1) viruses. We observed that two introduced NA mutations (H274Y and N294S) were stably maintained in N1 NA subtype, while the other two NA mutations (E119G and R292K) were not genetically stable. We further observed that the H274Y or N294S NA mutation slightly reduced the lethality of PR8 (H1N1) recombinant viruses in BALB/c mice, while uncompromised lethality and pathogenicity were observed with the VN1203 (H5N1) recombinant viruses carrying the H274Y or N294S NA mutation. The potential ability of oseltamivir-resistant H5N1 variants to retain their high pathogenicity in mammalian species should be taken into consideration in the clinical management of infected patients, as the emergence of resistant H5N1 variant should be closely monitored. The different enzyme kinetic parameters (Vmax and Km) of avian-like VN1203 NA and human-like PR8 NA suggest that resistance-associated NA mutations can cause different levels of functional loss in NA glycoproteins of the same subtype.
The E119G and R292K NAI resistance mutations impaired the growth of VN1203 (H5N1) and PR8 (H1N1) viruses in vitro; plaques of heterogeneous size were formed, and sequence analysis revealed that a subpopulation of the viruses had acquired HA mutations or had lost the introduced NA mutation and reverted to the wild-type NA sequence. The difficulty of rescuing recombinant A/WSN/33 (H1N1) virus with the E119G or R292K mutation has been reported previously (1, 2). In contrast, in the N2 and N9 subtypes, E119G and R292K are the NA mutations commonly reported to be associated with NAI resistance (10, 14, 34). It is likely that structural differences between group 1 (N1, N4, N5, and N8 subtypes) and group 2 (N2, N3, N6, N7, and N9) NA glycoproteins (39) determine the instability of the E119G and R292K NA mutations in the group 1 NA glycoproteins.
H274Y is the NA mutation most frequently associated with NAI resistance in the N1 subtype (10), whereas the N294S mutation was first discovered in H3N2 human influenza virus isolated from oseltamivir-treated patients (27). Subpopulations of variants carrying the H274Y or N294S mutation have been identified in H5N1-infected patients after oseltamivir treatment (8, 29, 35, 40). H274 and N294 are framework residues that are conserved among all influenza virus NA subtypes (6, 7). Previous reports have shown that amino acid changes at conserved NA residues would decrease NA enzyme activity and may affect viral fitness (12, 26, 34). We observed that H274Y and N294S mutations decreased the enzymatic activity of both VN1203 and PR8 NA glycoproteins; however, the reduced NA activity caused only a slight reduction in lethality of the PR8-H274Y and PR8-N294S viruses in BALB/c mice and had no effect on the fitness of the VN1203-H274Y and VN1203-N294S viruses. This observation may be explained by (i) the significantly higher enzyme activity of the VN1203 NA glycoprotein than of PR8 NA glycoprotein and (ii) the significant increase in Km values caused by these two mutations in the PR8 NA glycoprotein but not in the VN1203 NA glycoprotein. Sequence alignment identified 78 amino acid differences between the VN1203 and PR8 NAs. Structurally, the VN1203 and PR8 NA glycoproteins have a 20-amino-acid deletion and a 15-amino-acid deletion in their stalk regions, respectively, and the avian-like VN1203 NA has a potential secondary SA binding site (45). Further analysis is required to clarify the molecular determinants that distinguish VN1203 and PR8 NA function. However, our results clearly show that avian-like and human-like NA glycoproteins of the same subtype may undergo different levels of NA functional loss as the result of resistance-associated NA mutations.
In virus preparations of similar concentration, Kobasa and coauthors observed higher levels of NA activity in avian than in human influenza viruses (28). A comparison of N2 NA enzyme activities in duck and human influenza viruses isolated between 1957 and 1968 also showed significantly higher NA activity in avian isolates (28). However, it is not completely clear whether decreased NA activity is required for adaptation of avian influenza virus to mammalian hosts. On the other hand, a deletion in the NA stalk region that reduces NA activity (30) has been considered a molecular marker associated with adaptation of avian influenza viruses to domestic poultry (3). With the H274Y and N294S mutations that reduced the high NA enzymatic activity of H5N1 viruses without compromising the fitness of the virus, it is not clear if these mutations may provide an alternative route for adaptation of avian influenza virus to domestic poultry. The VN1203 (H5N1) virus we studied was isolated from a fatal human case of H5N1 infection and has demonstrated high pathogenicity and lethality in both avian (chickens and ducks) (22) and mammalian (mice and ferrets) species (9, 31, 41). We have observed that VN1203 NA possesses significantly higher enzymatic activity than A/Hong Kong/156/97 (H5N1) virus NA (unpublished results). It is not clear whether H5N1 viruses have acquired increased NA activity since 1997 or whether H5N1 influenza viruses of both clades 1 and 2 have high NA enzymatic activity.
We observed that H274Y and N294S NA mutations in the recombinant PR8 (H1N1) virus background resulted in 3.7- and 7-fold reductions in virus lethality in mice, respectively. Similar observations have been reported by Abed et al., using recombinant A/WSN/33 (H1N1) virus: the recombinant virus carrying the H274Y NA mutation showed lethality comparable to that of the wild-type virus, and the recombinant virus carrying the N294S NA mutation had decreased virus titer in the lungs as well as an approximately 1-log-reduced MLD50 value (1). However, in the recombinant VN1203 (H5N1) virus background, we observed that neither the H274Y nor the N294S NA mutation compromised the lethality or pathogenicity of the virus. The fitness of oseltamivir-resistant H5N1 variants has been evaluated in ferrets previously, and it was observed that an oseltamivir-resistant H5N1 variant carrying an H274Y NA mutation replicated less efficiently than the wild-type virus in the ferret upper respiratory tract, as reflected by nasal wash titers (29). The studied oseltamivir-resistant H5N1 variant was derived from a patient who received a prophylactic dose of oseltamivir. The patient recovered from H5N1 infection after receiving the treatment dose of oseltamivir. The virus used in the study, A/Honoi/30408/2005 (H5N1), is likely not highly pathogenic in ferrets, as nasal washes can be obtained from ferrets inoculated with 2 × 105 PFU at day 7 or 9 postinoculation. In the present study, we used a human H5N1 isolate (A/Vietnam/1203/04) that has been shown by several groups to be highly lethal and pathogenic in mice and ferrets (9, 31). At the inoculation dose of 2 × 105 PFU, ferrets inoculated with A/Vietnam/1203/04 virus would have succumbed to infection by day 9 postinoculation (9). It is likely that the differences in virus pathogenicity may have contributed to the different observations described by Le et al. (29) and in the present study. Further studies are required to characterize NAI-resistant variants that emerged from H5N1 viruses with different pathogenicities.
NAIs are being stockpiled in many countries to prepare for a potential H5N1 pandemic; however, the emergence of resistant variants must be factored into any optimal preparedness strategy. The high replication efficiencies of some of the H5N1 influenza viruses (41) and the high enzyme activities of the avian-like NA glycoproteins suggest that NAI-resistant H5N1 influenza viruses may be more difficult to control than the resistant seasonal human influenza virus variants. Identification of the H274Y NA mutation in two avian H5N1 influenza virus isolates (A/swan/Astrakhan/1/2005 and A/chicken/Hong Kong/3123.1/2002; GenBank accession numbers DQ320136 and DQ250158, respectively) as well as in isolates from the two H5N1 patients in Egypt prior to oseltamivir treatment (40) further suggests that this mutation can be maintained stably in nature. Current NAIs were designed on the basis of the group 2 NA structure (46), which differs from the group 1 NA structure (39). As a result, viral fitness may not be severely compromised in resistant variants with group 1 NA, as it is in some resistant variants with group 2 NA (50). Future efforts should focus on refining the design of current NAIs, developing new classes of anti-influenza agents, and exploring possible combination therapy regimens. Meanwhile, the emergence of resistant variants among H5N1-infected patients receiving NAI treatment should be closely monitored.
Acknowledgments
We thank Suzanne Jackowski and Jeremy Mallari for great advice; Patrick Seiler, John Franks, Jennifer McClaren, and Cedric Proctor for technical assistance; Klo Spelshouse for illustrations; and Sharon Naron for editorial assistance.
This work was supported by the National Institute of Allergy and Infectious Diseases, National Institutes of Health, grants A195357 and A157570 and contract no. HHSN266200700005C, and by the American Lebanese Syrian Associated Charities (ALSAC).
Footnotes
Published ahead of print on 12 September 2007.
REFERENCES
- 1.Abed, Y., M. Baz, and G. Boivin. 2006. Impact of neuraminidase mutations conferring influenza resistance to neuraminidase inhibitors in the N1 and N2 genetic backgrounds. Antiviral Ther. 11:971-976. [PubMed] [Google Scholar]
- 2.Abed, Y., N. Goyette, and G. Boivin. 2004. A reverse genetics study of resistance to neuraminidase inhibitors in an influenza A/H1N1 virus. Antiviral Ther. 9:577-581. [PubMed] [Google Scholar]
- 3.Banks, J., E. S. Speidel, E. Moore, L. Plowright, A. Piccirillo, I. Capua, P. Cordioli, A. Fioretti, and D. J. Alexander. 2001. Changes in the haemagglutinin and the neuraminidase genes prior to the emergence of highly pathogenic H7N1 avian influenza viruses in Italy. Arch. Virol. 146:963-973. [DOI] [PubMed] [Google Scholar]
- 4.Bright, R. A., M. J. Medina, X. Xu, G. Perez-Oronoz, T. R. Wallis, X. M. Davis, L. Povinelli, N. J. Cox, and A. I. Klimov. 2005. Incidence of adamantane resistance among influenza A (H3N2) viruses isolated worldwide from 1994 to 2005: a cause for concern. Lancet 366:1175-1181. [DOI] [PubMed] [Google Scholar]
- 5.Carr, J., J. Ives, L. Kelly, R. Lambkin, J. Oxford, D. Mendel, L. Tai, and N. Roberts. 2002. Influenza virus carrying neuraminidase with reduced sensitivity to oseltamivir carboxylate has altered properties in vitro and is compromised for infectivity and replicative ability in vivo. Antiviral Res. 54:79-88. [DOI] [PubMed] [Google Scholar]
- 6.Colman, P. M., P. A. Hoyne, and M. C. Lawrence. 1993. Sequence and structure alignment of paramyxovirus hemagglutinin-neuraminidase with influenza virus neuraminidase. J. Virol. 67:2972-2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colman, P. M., J. N. Varghese, and W. G. Laver. 1983. Structure of the catalytic and antigenic sites in influenza virus neuraminidase. Nature 303:41-44. [DOI] [PubMed] [Google Scholar]
- 8.de Jong, M. D., T. T. Tran, H. K. Truong, M. H. Vo, G. J. Smith, V. C. Nguyen, V. C. Bach, T. Q. Phan, Q. H. Do, Y. Guan, J. S. Peiris, T. H. Tran, and J. Farrar. 2005. Oseltamivir resistance during treatment of influenza A (H5N1) infection. N. Engl. J. Med. 353:2667-2672. [DOI] [PubMed] [Google Scholar]
- 9.Govorkova, E. A., J. E. Rehg, S. Krauss, H. L. Yen, Y. Guan, M. Peiris, T. D. Nguyen, T. H. Hanh, P. Puthavathana, H. T. Long, C. Buranathai, W. Lim, R. G. Webster, and E. Hoffmann. 2005. Lethality to ferrets of H5N1 influenza viruses isolated from humans and poultry in 2004. J. Virol. 79:2191-2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gubareva, L. V. 2004. Molecular mechanisms of influenza virus resistance to neuraminidase inhibitors. Virus Res. 103:199-203. [DOI] [PubMed] [Google Scholar]
- 11.Gubareva, L. V., M. N. Matrosovich, M. K. Brenner, R. C. Bethell, and R. G. Webster. 1998. Evidence for zanamivir resistance in an immunocompromised child infected with influenza B virus. J. Infect. Dis. 178:1257-1262. [DOI] [PubMed] [Google Scholar]
- 12.Gubareva, L. V., M. J. Robinson, R. C. Bethell, and R. G. Webster. 1997. Catalytic and framework mutations in the neuraminidase active site of influenza viruses that are resistant to 4-guanidino-Neu5Ac2en. J. Virol. 71:3385-3390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gubareva, L. V., R. G. Webster, and F. G. Hayden. 2002. Detection of influenza virus resistance to neuraminidase inhibitors by an enzyme inhibition assay. Antiviral Res. 53:47-61. [DOI] [PubMed] [Google Scholar]
- 14.Gubareva, L. V., R. G. Webster, and F. G. Hayden. 2001. Comparison of the activities of zanamivir, oseltamivir, and RWJ-270201 against clinical isolates of influenza virus and neuraminidase inhibitor-resistant variants. Antimicrob. Agents Chemother. 45:3403-3408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hayden, F. G. 1997. Antivirals for pandemic influenza. J. Infect. Dis. 176(Suppl. 1):S56-S61. [DOI] [PubMed] [Google Scholar]
- 16.Hayden, F. G. 2006. Antiviral resistance in influenza viruses—implications for management and pandemic response. N. Engl. J. Med. 354:785-788. [DOI] [PubMed] [Google Scholar]
- 17.Hayden, F. G., R. B. Belshe, R. D. Clover, A. J. Hay, M. G. Oakes, and W. Soo. 1989. Emergence and apparent transmission of rimantadine-resistant influenza A virus in families. N. Engl. J. Med. 321:1696-1702. [DOI] [PubMed] [Google Scholar]
- 18.Herlocher, M. L., J. Carr, J. Ives, S. Elias, R. Truscon, N. Roberts, and A. S. Monto. 2002. Influenza virus carrying an R292K mutation in the neuraminidase gene is not transmitted in ferrets. Antiviral Res. 54:99-111. [DOI] [PubMed] [Google Scholar]
- 19.Hoffmann, E., S. Krauss, D. Perez, R. Webby, and R. G. Webster. 2002. Eight-plasmid system for rapid generation of influenza virus vaccines. Vaccine 20:3165-3170. [DOI] [PubMed] [Google Scholar]
- 20.Hoffmann, E., G. Neumann, Y. Kawaoka, G. Hobom, and R. G. Webster. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. USA 97:6108-6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoffmann, E., J. Stech, Y. Guan, R. G. Webster, and D. R. Perez. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146:2275-2289. [DOI] [PubMed] [Google Scholar]
- 22.Hulse-Post, D. J., K. M. Sturm-Ramirez, J. Humberd, P. Seiler, E. A. Govorkova, S. Krauss, C. Scholtissek, P. Puthavathana, C. Buranathai, T. D. Nguyen, H. T. Long, T. S. Naipospos, H. Chen, T. M. Ellis, Y. Guan, J. S. Peiris, and R. G. Webster. 2005. Role of domestic ducks in the propagation and biological evolution of highly pathogenic H5N1 influenza viruses in Asia. Proc. Natl. Acad. Sci. USA 102:10682-10687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ilyushina, N. A., E. A. Govorkova, and R. G. Webster. 2005. Detection of amantadine-resistant variants among avian influenza viruses isolated in North America and Asia. Virology 341:102-106. [DOI] [PubMed] [Google Scholar]
- 24.Ison, M. G., L. V. Gubareva, R. L. Atmar, J. Treanor, and F. G. Hayden. 2006. Recovery of drug-resistant influenza virus from immunocompromised patients: a case series. J. Infect. Dis. 193:760-764. [DOI] [PubMed] [Google Scholar]
- 25.Ives, J. A., J. A. Carr, D. B. Mendel, C. Y. Tai, R. Lambkin, L. Kelly, J. S. Oxford, F. G. Hayden, and N. A. Roberts. 2002. The H274Y mutation in the influenza A/H1N1 neuraminidase active site following oseltamivir phosphate treatment leaves virus severely compromised both in vitro and in vivo. Antiviral Res. 55:307-317. [DOI] [PubMed] [Google Scholar]
- 26.Jackson, D., W. Barclay, and T. Zurcher. 2005. Characterization of recombinant influenza B viruses with key neuraminidase inhibitor resistance mutations. J. Antimicrob. Chemother. 55:162-169. [DOI] [PubMed] [Google Scholar]
- 27.Kiso, M., K. Mitamura, Y. Sakai-Tagawa, K. Shiraishi, C. Kawakami, K. Kimura, F. G. Hayden, N. Sugaya, and Y. Kawaoka. 2004. Resistant influenza A viruses in children treated with oseltamivir: descriptive study. Lancet 364:759-765. [DOI] [PubMed] [Google Scholar]
- 28.Kobasa, D., K. Wells, and Y. Kawaoka. 2001. Amino acids responsible for the absolute sialidase activity of the influenza A virus neuraminidase: relationship to growth in the duck intestine. J. Virol. 75:11773-11780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Le, Q. M., M. Kiso, K. Someya, Y. T. Sakai, T. H. Nguyen, K. H. Nguyen, N. D. Pham, H. H. Ngyen, S. Yamada, Y. Muramoto, T. Horimoto, A. Takada, H. Goto, T. Suzuki, Y. Suzuki, and Y. Kawaoka. 2005. Avian flu: isolation of drug-resistant H5N1 virus. Nature 437:1108. [DOI] [PubMed] [Google Scholar]
- 30.Luo, G., J. Chung, and P. Palese. 1993. Alterations of the stalk of the influenza virus neuraminidase: deletions and insertions. Virus Res. 29:141-153. [DOI] [PubMed] [Google Scholar]
- 31.Maines, T. R., X. H. Lu, S. M. Erb, L. Edwards, J. Guarner, P. W. Greer, D. C. Nguyen, K. J. Szretter, L. M. Chen, P. Thawatsupha, M. Chittaganpitch, S. Waicharoen, D. T. Nguyen, T. Nguyen, H. H. Nguyen, J. H. Kim, L. T. Hoang, C. Kang, L. S. Phuong, W. Lim, S. Zaki, R. O. Donis, N. J. Cox, J. M. Katz, and T. M. Tumpey. 2005. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J. Virol. 79:11788-11800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matrosovich, M., T. Matrosovich, J. Carr, N. A. Roberts, and H. D. Klenk. 2003. Overexpression of the alpha-2,6-sialyltransferase in MDCK cells increases influenza virus sensitivity to neuraminidase inhibitors. J. Virol. 77:8418-8425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McKimm-Breschkin, J., T. Trivedi, A. Hampson, A. Hay, A. Klimov, M. Tashiro, F. Hayden, and M. Zambon. 2003. Neuraminidase sequence analysis and susceptibilities of influenza virus clinical isolates to zanamivir and oseltamivir. Antimicrob. Agents Chemother. 47:2264-2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McKimm-Breschkin, J. L. 2000. Resistance of influenza viruses to neuraminidase inhibitors. Antiviral Res. 47:1-17. [DOI] [PubMed] [Google Scholar]
- 35.Normile, D., and M. Enserink. 2007. Avian influenza. With change in the seasons, bird flu returns. Science 315:448. [DOI] [PubMed] [Google Scholar]
- 36.Potier, M., L. Mameli, M. Belisle, L. Dallaire, and S. B. Melancon. 1979. Fluorometric assay of neuraminidase with a sodium (4-methylumbelliferyl-alpha-d-N-acetylneuraminate) substrate. Anal. Biochem. 94:287-296. [DOI] [PubMed] [Google Scholar]
- 37.Rameix-Welti, M. A., F. Agou, P. Buchy, S. Mardy, J. T. Aubin, M. Veron, W. S. van der, and N. Naffakh. 2006. Natural variation can significantly alter the sensitivity of influenza A (H5N1) viruses to oseltamivir. Antimicrob. Agents Chemother. 50:3809-3815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reed, L. J., and H. Muench. 1938. A simple method for estimating fifty percent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 39.Russell, R. J., L. F. Haire, D. J. Stevens, P. J. Collins, Y. P. Lin, G. M. Blackburn, A. J. Hay, S. J. Gamblin, and J. J. Skehel. 2006. The structure of H5N1 avian influenza neuraminidase suggests new opportunities for drug design. Nature 443:45-49. [DOI] [PubMed] [Google Scholar]
- 40.Saad, M. D., B. R. Boynton, K. C. Earhart, M. M. Mansour, H. L. Niman, N. M. Elsayed, A. L. Nayel, A. S. Abdelghani, H. M. Essmat, E. M. Labib, E. A. Ayoub, and M. R. Monteville. 2007. Detection of oseltamivir resistance mutation N294S in humans with influenza A H5N1. Options for the Control of Influenza VI. Toronto, Canada.
- 41.Salomon, R., J. Franks, E. A. Govorkova, N. A. Ilyushina, H. L. Yen, D. J. Hulse-Post, J. Humberd, M. Trichet, J. E. Rehg, R. J. Webby, R. G. Webster, and E. Hoffmann. 2006. The polymerase complex genes contribute to the high virulence of the human H5N1 influenza virus isolate A/Vietnam/1203/04. J. Exp. Med. 203:689-697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smith, G. J., T. S. Naipospos, T. D. Nguyen, J. de, D. Vijaykrishna, T. B. Usman, S. S. Hassan, T. V. Nguyen, T. V. Dao, N. A. Bui, Y. H. Leung, C. L. Cheung, J. M. Rayner, J. X. Zhang, L. J. Zhang, L. L. Poon, K. S. Li, V. C. Nguyen, T. T. Hien, J. Farrar, R. G. Webster, H. Chen, J. S. Peiris, and Y. Guan. 2006. Evolution and adaptation of H5N1 influenza virus in avian and human hosts in Indonesia and Vietnam. Virology 350:258-268. [DOI] [PubMed] [Google Scholar]
- 43.Stilianakis, N. I., A. S. Perelson, and F. G. Hayden. 2002. Drug resistance and influenza pandemics. Lancet 359:1862-1863. [DOI] [PubMed] [Google Scholar]
- 44.Tai, C. Y., P. A. Escarpe, R. W. Sidwell, M. A. Williams, W. Lew, H. Wu, C. U. Kim, and D. B. Mendel. 1998. Characterization of human influenza virus variants selected in vitro in the presence of the neuraminidase inhibitor GS 4071. Antimicrob. Agents Chemother. 42:3234-3241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Varghese, J. N., P. M. Colman, D. A. van, T. J. Blick, A. Sahasrabudhe, and J. L. Kimm-Breschkin. 1997. Structural evidence for a second sialic acid binding site in avian influenza virus neuraminidases. Proc. Natl. Acad. Sci. USA 94:11808-11812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.von Itzstein, M., W. Y. Wu, G. B. Kok, M. S. Pegg, J. C. Dyason, B. Jin, P. T. Van, M. L. Smythe, H. F. White, S. W. Oliver, et al. 1993. Rational design of potent sialidase-based inhibitors of influenza virus replication. Nature 363:418-423. [DOI] [PubMed] [Google Scholar]
- 47.Wang, M. Z., C. Y. Tai, and D. B. Mendel. 2002. Mechanism by which mutations at His274 alter sensitivity of influenza A virus n1 neuraminidase to oseltamivir carboxylate and zanamivir. Antimicrob. Agents Chemother. 46:3809-3816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ward, P., I. Small, J. Smith, P. Suter, and R. Dutkowski. 2005. Oseltamivir (Tamiflu(R)) and its potential for use in the event of an influenza pandemic. J. Antimicrob. Chemother. 55(Suppl. 1):i5-i21. [DOI] [PubMed] [Google Scholar]
- 49.World Health Organization. 2007. Epidemic and pandemic alert and response (EPR). World Health Organization, Geneva, Switzerland.
- 50.Yen, H. L., L. M. Herlocher, E. Hoffmann, M. N. Matrosovich, A. S. Monto, R. G. Webster, and E. A. Govorkova. 2005. Neuraminidase inhibitor-resistant influenza viruses may differ substantially in fitness and transmissibility. Antimicrob. Agents Chemother. 49:4075-4084. [DOI] [PMC free article] [PubMed] [Google Scholar]