Abstract
The objective of this study was to evaluate the longitudinal course of psychiatric disorders in children of parents with and without panic disorder and major depression as they transition through the period of risk from early to late childhood. Over a 5-year follow-up, we compared the course of psychiatric disorders in offspring of parents with panic disorder, major depression, or neither disorder. Subjects consisted of 233 offspring (from 151 families) with baseline and follow-up assessments. Subjects were comprehensively assessed with structured diagnostic interviews. Anxiety disorders at baseline were used to predict anxiety disorders and major depression at follow-up using stepwise logistic regression. Separation anxiety disorder significantly increased the risk for the subsequent development of specific phobia, agoraphobia, panic disorder, and major depression, even after parental panic and depression were covaried. Agoraphobia significantly increased the risk for subsequent generalized anxiety disorder. These findings suggest that separation anxiety disorder is a major antecedent disorder for the development of panic disorder and a wide range of other psychopathological outcomes, and that it increases the risk for subsequent psychopathology even among children already at high familial risk for anxiety or mood disorder.
Keywords: panic disorder, separation anxiety disorder, depression, children, comorbidity, family, high risk
In early work, our group reported that parental panic disorder with agoraphobia increased the risk for both anxiety disorders and major depression in offspring (Biederman, et al., 1991). Similar results were reported by Weissman and colleagues (Weissman, et al., 1984), who found an increased risk for anxiety disorders in children whose parents had major depression and agoraphobia or panic disorder. These results were supported in a more recent, large, controlled study of children at high and low risk for panic disorder (Biederman, et al., 2001). This study showed that parental panic disorder increased the risk for panic disorder, agoraphobia, and separation anxiety disorder.
The prospective follow-up of these children at risk into late childhood and early adolescence also showed that these children were at risk for a wide range of anxiety disorders and that frequently other anxiety disorders emerged before the onset of panic disorder. These results are consistent with previous work in referred and non-referred adults with panic disorder (Biederman, et al., 2005) documenting that panic disorder is commonly preceded by other anxiety disorders.
One of the antecedent childhood disorders frequently associated with panic disorder in the extant literature is separation anxiety disorder. Early findings by some investigators suggested a specific link between childhood separation anxiety disorder and panic disorder in adulthood (Gittelman and Klein, 1984, Weissman, et al., 1984). Recent findings from referred and non-referred adults showed that separation anxiety disorder and overanxious disorder were independent predictors of subsequent panic disorder but separation anxiety disorder was the best predictor of early onset panic disorder (Biederman, et al., 2005). Other investigators suggested that other anxiety disorders may also be linked to the risk for subsequent panic disorder (Aronson and Logue, 1987, Aschenbrand, et al., 2003, Moreau and Follett, 1993, Otto, et al., 1994, Pollack, et al., 1996). However, because much of this work was based on retrospective reports from adults, and because discrepant findings were found with regard to the outcome of child separation anxiety disorder (Aschenbrand, et al., 2003, Klein, 1995), more work is needed to examine the prospective prediction of panic disorder in children. Identifying developmental trajectories toward panic disorder would set the stage for targeted primary preventive or early intervention programs.
Previous longitudinal studies have focused mainly on predicted outcomes of the broad category anxiety disorders, finding, for example, that anxiety in childhood was a risk factor for anxiety, depression, or substance abuse in adolescence (Costello, et al., 2003) or that anxiety comorbid with depression was more stable over time than anxiety disorder alone (Merikangas, et al., 2003). This current study seeks to examine the development of individual DSM-IV anxiety disorders, similar to the longitudinal approach used by Pine et al. (Pine, et al., 1998) in adolescents and young adults.
The main aim of this study was to examine whether developmental trajectories towards the development of pediatric panic disorder are found in children. To this end, we analyzed data from our large, longitudinal follow-up study of well-characterized children at high and low risk for panic disorder and major depression. As a first step in the study of developmental trajectories, our analysis focuses on sequential associations between specific disorders, using data from two waves of data collection. Specifically, we examined whether specific anxiety disorders in early childhood predicted other anxiety disorders or major depression in later childhood and adolescence. Based on the prior literature (Biederman, et al., 2005, Gittelman and Klein, 1984, Weissman, et al., 1984), we hypothesized that separation anxiety disorder would be a potent predictor of subsequent panic disorder in children at risk.
Methods
Subjects
Subjects were derived from a previously described (Biederman, et al., 2006) follow-up study of children at high and low risk for panic disorder and major depression ascertained through parent probands treated for panic disorder, major depression, and control parents. Parents were recruited from clinical referrals and advertising in the local media. Comparison parents were recruited through advertisements to hospital personnel and in community newspapers. Control proband selection was guided by contemporary epidemiologic methodology, which dictates that the sampling of controls should be drawn from the exposure distribution of the source population that gave rise to the cases (Miettinen, 1985). Comparison parents were free of major anxiety disorders or mood disorders. Parents with panic disorder and/or major depression were selected on the basis of having been treated for these disorders. Both parents from each family were assessed at baseline with the SCID for DSM-III-R (Spitzer, et al., 1990). There were no constraints on treatment in offspring. For the purpose of this analysis we used 233 offspring from 151 families who had diagnostic data at baseline and follow-up assessments. Of the 151 families, 43 had parents with panic disorder and major depression (N=99 offspring), 11 had parents with panic disorder and no major depression (N=18 offspring), 30 had parents with major depression and no panic disorder (N=40 offspring), and 67 had parents without panic disorder and without major depression (N=76 offspring). The majority of parent probands were female (92%, 139/151). Ages at baseline assessment of the offspring ranged from 5 to 13 years (mean age=6.4 years; median=6 years) and 123 (53%) were male. Ages at follow-up assessment ranged from 7 to 18 years (mean age=10.9 years; median=11 years). Of 233 subjects, 221 (95%) were Caucasian, 202 (87%) came from intact families, and 94% came from higher socioeconomic levels (1, 2, or 3 on the Hollingshead 5-point scale (Hollingshead, 1975)). The Institutional Review Board at Massachusetts General Hospital approved this study protocol. All parents signed written consent and children assented to study procedures.
Assessment Procedures
Data were collected at two time points. The first (Wave 1) was the baseline assessment, conducted when the sample was originally recruited, between 1993-1998. The second (Wave 2) was conducted approximately five years later, between 1999-2004. Because some families were easier to reach at follow-up than others, there was variability in the follow-up period of offspring who were assessed at both time points (mean: 4.5 years, SD: 1.5 years).
Psychiatric assessments of the children at baseline relied on the DSM-III-R criteria and were previously described (Biederman, et al., 2001). Assessments at follow-up were based on the DSM-IV Schedule of Affective Disorders and Schizophrenia for school-aged children –Epidemiological Version (K-SADS-E) (Orvaschel, 1994) for subjects <18 years and the Structured Clinical Interview for DSM-IV (SCID) (First, et al., 1997) (supplemented with modules from the K-SADS-E to assess childhood diagnoses) for subjects age18 years. We conducted indirect interviews with the mothers for all subjects and direct interviews with subjects ≥12 years. Discrepant reports between the youth and the mother report were handled by considering a disorder positive if DSM diagnostic criteria were unequivocally met in either the child (12 years and older) or the mother's interview. At both time points we assessed lifetime presence of disorders.
The raters had undergraduate degrees in psychology and were trained to high levels of inter-rater reliability. Different interviewers were used for each member of the family. Different interviewers were also used for the parent and the child in cases when both were interviewed about a child. Interviewers at follow-up were blind to all information collected at baseline. A committee of board-certified child and adult psychiatrists and licensed psychologists who were blind to the subject's ascertainment status, referral source, and all other data (from baseline and follow-up) resolved diagnostic uncertainties. Diagnoses presented for review were considered positive only if a consensus was achieved that criteria were met to a degree that would be considered clinically meaningful. In addition, diagnoses followed DSM-III-R (baseline) and DSM-IV (follow-up) criteria, so that if a symptom was endorsed that was clearly due to another disorder, it was not coded twice. For example, the diagnosis of agoraphobia required that the child avoid certain situations (e.g., elevators, going outside alone), require a companion in the situation, or endure it with intense anxiety because of a fear of developing anxiety symptoms. If the avoidance was clearly related to separation anxiety disorder, social phobia, or another anxiety condition, agoraphobia was not diagnosed. Anxiety or avoidance that was developmentally normative (e.g. separation anxiety in infancy/toddlerhood) was also not coded. The principal investigators (JB and JFR) supervised the interviewers throughout the study.
Statistical Analyses
Analyses were conducted using STATA, version 9.0 (Stata Corporation, 2005). Lifetime anxiety disorders at baseline (separation anxiety disorder, specific phobia, overanxious disorder, agoraphobia, social phobia, and panic disorder) were used to predict new lifetime disorders at follow-up (separation anxiety disorder, specific phobia, generalized anxiety disorder, agoraphobia, social phobia, panic disorder, and major depression) using stepwise logistic regression with a removal criterion of P≥0.20. That is, each model included a single follow-up disorder as the outcome and six baseline anxiety disorders as predictors to determine the independent predictive value of anxiety disorders at baseline. Major depressive disorder was included as an outcome due to its extensively documented relationship with anxiety disorders (Costello, et al., 2003, Harrington, et al., 1990, Merikangas, et al., 2003, Pine, et al., 1998, Warner, et al., 1995, Weissman, et al., 1984). In addition to baseline disorders, parental diagnoses (major depression [MD] and panic disorder [PD]) were included in the models to assure that any significant findings were independent of the ascertainment of the family. Age at follow-up assessment was also included in all statistical models. A subject was not included in a model if the subject had a full diagnosis of the outcome disorder at baseline or at follow-up reported an age of onset of the outcome disorder that preceded the subject's baseline interview. That is, only subjects who did not have the outcome disorder at baseline were included in the model for that outcome disorder. To account for the assumption that each observation was not independent of all other observations (i.e., multiple children per family), we used robust estimates of variance so that p-values would not be underestimated (Liang and Zeger, 1986). All tests were two-tailed with alpha set at 0.05.
Results
Two hundred thirty-three (77%) of the 303 offspring assessed at baseline (excluding subjects older than 13 years at baseline) were reassessed at follow-up. There were no significant differences between offspring returning at follow-up and offspring lost to follow-up on baseline age (P=0.08), gender (P=0.38), ethnicity (P=0.45), family intactness (P=0.67), socioeconomic status (P=0.89), and lifetime global assessment of functioning (P=0.45). The rate of successful follow-up did not significantly vary by parental diagnosis of PD and MD (P=0.10).
The sample we assessed already had high lifetime rates of disorders at baseline. Specifically, at baseline, 30% (71/233) of the offspring had at least one lifetime anxiety disorder (39% [39/99] of offspring with parental PD+MD, 33% [6/18] of offspring with parental PD only, 32% [13/40] of offspring with parental MD only, and 17% [13/76] of offspring of control parents). At baseline, 15% (36/233) of the offspring had two or more lifetime anxiety disorders (23% [23/99] of offspring with parental PD+MD, 22% [4/18] of offspring with parental PD only, 15% [6/40] of offspring with parental MD only, and 4% [3/76] of offspring of control parents). Lifetime rates of anxiety disorders at baseline ranged from 18% for separation anxiety disorder, n=41) and 14% for specific phobia (n=33), to 9% for overanxious disorder (n=21) and agoraphobia (n=21), and finally 6% for social phobia (n=15) and 3% for panic disorder (n=6).
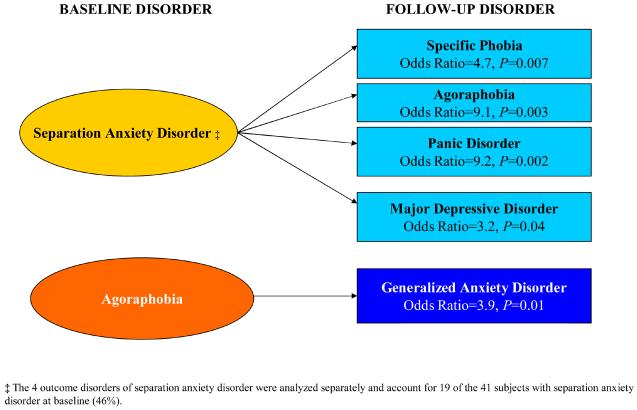
Analysis of trajectories for the development of psychopathology in children revealed that separation anxiety disorder significantly increased the risk for subsequent development of specific phobia, agoraphobia, panic disorder, and major depression (Figure 1). Agoraphobia increased the risk for later generalized anxiety disorder.
Figure 1.
Risk for psychopathology at follow-up given presence of anxiety disorder at baseline.
Specifically, the rate of specific phobia at follow-up was higher in subjects with separation anxiety disorder at baseline than without separation anxiety disorder at baseline (26% [6/23] versus 7% [11/157], OR=4.7, 95% CI [1.5,14.4], P=0.007, OR=Odds Ratio, CI=Confidence Interval; N=53 excluded due to specific phobia at baseline or the onset of specific phobia reported at follow-up preceded age at baseline interview). The rate of agoraphobia at follow-up was higher in subjects with baseline separation anxiety disorder than without baseline separation anxiety disorder (27% [6/22] versus 4% [8/182], OR=9.1, CI [2.1,38.9], P=0.003; N=29 excluded due to agoraphobia at baseline or the onset of agoraphobia reported at follow-up preceded age at baseline interview). The rate of panic disorder at follow-up was higher in subjects with baseline separation anxiety disorder than without separation anxiety disorder (14% [5/35] versus 4% [7/190], OR=9.2, CI [2.3,36.9], P=0.002; N=8 excluded due to panic disorder at baseline or the onset of panic disorder reported at follow-up preceded age at baseline interview). The rate of major depression at follow-up was higher in subjects with baseline separation anxiety disorder than without (17% [6/35] versus 4% [8/182], OR=3.2, CI [1.0,10.2], P=0.04; N=16 excluded due to major depression at baseline or the onset of major depression reported at follow-up preceded age at baseline interview). Of the 41 subjects with separation anxiety disorder at baseline, 4 subjects had two new diagnoses of specific phobia, agoraphobia, panic disorder, or major depression at follow-up, 15 subjects had only one of these new diagnoses at follow-up, and 22 subjects did not develop any new diagnoses at follow-up.
The rate of generalized anxiety disorder at follow-up was higher in subjects with baseline agoraphobia than without agoraphobia (39% [7/18] versus 11% [22/197], OR=3.9, CI [1.3,11.3], P=0.01; N=18 excluded due to generalized anxiety disorder at baseline or the onset of generalized anxiety disorder reported at follow-up preceded age at baseline interview). No baseline anxiety disorder significantly predicted separation anxiety disorder or social phobia at follow-up.
Discussion
Analysis of the development of psychopathology in a large longitudinal sample of offspring of parents with and without panic disorder and major depression revealed that separation anxiety disorder significantly increased the risk for the subsequent development of agoraphobia, generalized anxiety disorder, panic disorder, and major depression, while agoraphobia significantly increased the risk for subsequent generalized anxiety disorder. These findings indicate that separation anxiety disorder may help identify a group of children at very high risk for a wide range of adverse psychopathological outcomes within a population already at risk by virtue of parental psychopathology.
Even after controlling for the presence of other anxiety disorders, separation anxiety disorder was the best predictor of panic disorder. These findings are consistent with an early literature by Gittelman and Klein (Gittelman and Klein, 1984, Klein, 1995) and by Weissman and colleagues (Weissman, et al., 1984), that suggested a link between childhood separation anxiety disorder and risk for panic disorder in adulthood, and with more recent findings in referred and non-referred adults showing that separation anxiety disorder was the best predictor of early onset panic disorder (Biederman, et al., 2005). This latter result confirms previously reported findings in the literature (Goodwin, et al., 2001) and indicates that the association between separation anxiety disorder and early onset panic disorder is not due to referral bias, since this was an non-referred sample.
Our finding that separation anxiety disorder conferred risk for disorders other than panic as well is consistent with other studies (Aronson and Logue, 1987, Moreau and Follett, 1993, Otto, et al., 1994, Pollack, et al., 1996). For example, in a 7-year prospective follow-up study of referred children and adolescents diagnosed with separation anxiety disorder, generalized anxiety disorder, or social phobia (Aschenbrand, et al., 2003), children with separation anxiety disorder did not show elevated rates of panic disorder compared to children with generalized anxiety disorder or social phobia, but did show higher rates of specific phobia, obsessive compulsive disorder, and posttraumatic stress disorder. Our results are also consistent with the literature from retrospective studies of adults. For example, Lipsitz et al (Lipsitz, et al., 1994) found a significantly higher prevalence of childhood separation anxiety disorder in adults with two or more anxiety disorders suggesting that separation anxiety disorder may be a risk factor for multiple anxiety syndromes in adulthood. In addition, Biederman et al. (Biederman, et al., 2005) found in samples of referred and non-referred adults that both separation anxiety disorder and overanxious disorder were independent predictors of subsequent panic disorder. This discrepancy with the current findings with regard to GAD may reflect a difference between pediatric and adult onset panic disorder. In fact, Biederman et al. (Biederman, et al., 2005) showed that separation anxiety disorder was the best predictor of panic disorder in the adults who had an onset of panic disorder before age 18.
Our findings support the idea that childhood separation anxiety disorder may reflect an underlying anxiety diathesis that increases susceptibility to a range of subsequent adult anxiety disorders. Alternatively, separation anxiety in childhood may influence learned responses to anxiety and tendencies toward avoidance (Otto, et al., 2001).
On the other hand, longitudinal findings by Pine et al. (Pine, et al., 1998) did not find adolescent separation anxiety disorder (average age at baseline=13.7 years) to be a significant predictor of anxiety disorders or major depression at follow-up. Our younger sample (average age at baseline=6.4 years) enabled us to assess the longitudinal effects of childhood separation anxiety disorder.
The finding that pediatric agoraphobia was a predictor of subsequent generalized anxiety disorder is novel. Since this was not a hypothesized outcome, our results could be attributed to chance. As such, this finding should be considered preliminary until replicated and confirmed in future research.
The finding that social phobia did not predict subsequent panic disorder is discrepant with retrospective data reported by Otto et al (Otto, et al., 2001, Otto, et al., 1994). These investigators reported that social phobia was the most prevalent reported childhood anxiety disorder in a sample of 100 adult patients with panic disorder. Although the reasons for these discrepant finding are unknown, they could reflect differences between referred and non-referred individuals or the fact that panic disorder emerged in our sample in childhood whereas in the Otto et al. study (Otto, et al., 2001, Otto, et al., 1994) it did so in adulthood suggesting that different risk factors may be responsible for early versus late onset panic disorder. Other prospective studies have found that social phobia is a significant risk factor for subsequent depression (Bittner, et al., 2004, Stein, et al., 2001). Although our results did not support these previous findings, the young age of our sample meant that we could not fully assess the children's chance of developing these disorders. Following these offspring into later adolescence and adulthood may reveal the link between social phobia and major depression or between social phobia and adult-onset panic disorder.
Specific phobia, although common at baseline, did not significantly predict development of any anxiety disorders or major depression. This is consistent with the literature suggesting that specific phobias are common disorders of childhood that do not herald the likelihood of other, more severe forms of anxiety or mood disorders (Fyer, et al., 1995, Pine, et al., 1998, Shaffer, et al., 1996).
Although major depression is frequently comorbid with panic disorder, in this sample panic disorder did not predict subsequent major depression, consistent with results from the National Comorbitity Survey (Kessler, et al., 1998). However, since our sample is still within the period of risk for panic disorder, a longer follow-up is needed to confirm these findings.
Our results inform the targeting of prevention studies to individuals at risk for future anxiety disorders, namely offspring of parents with panic disorder or depression who present with separation anxiety disorder or agoraphobia. Studies of prevention protocols could focus on teaching children strategies for managing anxiety without resorting to avoidance behaviors, and on teaching parents ways to model and facilitate adaptive coping (Hirshfeld-Becker and Biederman, 2002). Studies are needed to ascertain whether treating separation anxiety disorder or childhood agoraphobia in early childhood with cognitive-behavioral therapy could prevent the onset of subsequent disorders.
Our findings should be viewed in the context of the study's methodological limitations. Any interpretation of these findings must be tempered by the fact that these children are still early in the risk period for anxiety and depressive disorders. Future waves of assessment of this sample will deepen our understanding of trajectories of disorder, and may lead to different inferences about patterns of risk. In addition, our findings derive from a group of high-risk children, many of whom were the offspring of parents with panic disorder. It is not known whether these same trajectories would be seen in children without family history of panic disorder. The time between the onset of the predictor and outcome variables was not analyzed. However, because the analysis used baseline disorders to predict follow-up disorders, we can estimate that the average time between the onset of predictor disorders and outcome disorders would be the average time between assessments (i.e., 4.5 years). While subjects with separation anxiety disorder were at increased risk for agoraphobia, we did not examine whether these subjects continue to meet criteria for separation anxiety disorder. Considering the overlapping symptoms of these disorders, future work will benefit from further assessment of this issue. Because of the wide age range of the sample, informants of older versus younger participants may have differed in their recall of early symptoms. However, since age at follow-up was covaried, this difference would not be expected to affect our results.
Although raters were blind to the ascertainment status of the offspring, parents were not. The assessment of psychopathology in the children younger than 12 years was based on interviews with the mothers only, which may have led to underestimates of the true rates of psychopathology in offspring. Psychiatric disorders in parents may have affected the reported rates of childhood symptoms. Psychiatric patients may exaggerate symptoms in their children, or alternatively, mothers without psychopathology may under-report problem behaviors (Mick, et al., 2000). We did not directly interview children under age twelve about their lifetime diagnoses, because younger children are limited in their expressive and receptive language abilities, lack the ability to map events in time, and have limited powers of abstraction. Several studies (Edelbrock, et al., 1985, Schwab-Stone, et al., 1994) have documented poor reliability of reports of psychopathology by children under twelve. In addition, Breton et al. (Breton, et al., 1995) found that children aged 9 to 11 understood only about 40 percent of the questions from the Diagnostic Interview Schedule for Children (Version 2.5). In contrast, Faraone et al. (Faraone, et al., 1995) and others (Fallon and Schwab-Stone, 1994) have shown high reliability for maternal reports of psychopathology, even over a one-year period. In addition, through relying on parent-reports for diagnoses in children 11 and under and combining data from parent- and child-reports in children 12 and older, we introduced method variance in our study. However, we opted for this approach, because using only the parent reports for children over 11 might result in our missing important information about symptoms that adolescents, but not their parents, can report. Moreover, because the age of subjects (and therefore the assessment method used) was covaried in all analyses, this additional method variance cannot confound our findings. Future waves of data collection, in which all children in our sample will be old enough to be directly interviewed about their lifetime symptoms, will enable us to deepen our current findings. Although our study collected data at two time points, lifetime diagnoses were based on retrospective report and may have been subject to recall bias (Angold and Costello, 1996). Because the proband parents were clinically referred, the generalizability of our findings is limited to offspring of referred subjects. Also, because the large majority of subjects were Caucasians from intact families and higher levels of social class, further work is needed to determine if our results generalize beyond these constraints.
Despite these considerations, this large prospective follow-up study of children at risk growing up provides compelling evidence for the critical role of separation anxiety disorder as a key antecedent risk factor for subsequent panic disorder. Results also indicate that separation anxiety disorder may help identify a group of children at very high risk for a range of adverse psychopathological outcomes. Further work is needed to determine if the results found in this unique sample reflect developmental patterns in the general population.
Acknowledgment
This project is supported by the National Institute of Mental Health grant MH-47077-05
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Angold A, Costello E. Toward establishing an empirical basis for the diagnosis of oppositional defiant disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1205–1212. doi: 10.1097/00004583-199609000-00018. [DOI] [PubMed] [Google Scholar]
- Aronson TA, Logue CM. On the longitudinal course of panic disorder: Development history and predictors of phobic complications. Comprehensive Psychiatry. 1987;28:344–355. doi: 10.1016/0010-440x(87)90071-x. [DOI] [PubMed] [Google Scholar]
- Aschenbrand SG, Kendall PC, Webb A, Safford SM, Flannery-Schroeder E. Is childhood separation anxiety disorder a predictor of adult panic disorder and agoraphobia? A seven-year longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1478–85. doi: 10.1097/00004583-200312000-00015. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Hirshfeld-Becker DR, Friedman D, Robin JA, Rosenbaum JF. Patterns of Psychopathology and Dysfunction in High-Risk Children of Parents With Panic Disorder and Major Depression. American Journal of Psychiatry. 2001;158:49–57. doi: 10.1176/appi.ajp.158.1.49. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty C, Faraone S, Hirshfeld-Becker DR, Henin A, Rauf A, Scott M, Pollack M, Rosenbaum J. Childhood antecedents to panic disorder in referred and non referred adults. Journal of Child and Adolescent Psychopharmacology. 2005;15:549–561. doi: 10.1089/cap.2005.15.549. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty C, Hirshfeld-Becker DR, Henin A, Faraone SV, Dang D, Jakubowski A, Rosenbaum J. A controlled longitudinal five year follow-up study of children at high and low risk for panic disorder and major depression. Psychological Medicine. 2006;36:1141–1152. doi: 10.1017/S0033291706007781. [DOI] [PubMed] [Google Scholar]
- Biederman J, Rosenbaum JF, Bolduc EA, Faraone SV, Hirshfeld DR. A high risk study of young children of parents with panic disorder and agoraphobia with and without comorbid major depression. Psychiatry Research. 1991;37:333–348. doi: 10.1016/0165-1781(91)90068-z. [DOI] [PubMed] [Google Scholar]
- Bittner A, Goodwin RD, Wittchen HU, Beesdo K, Hofler M, Lieb R. What characteristics of primary anxiety disorders predict subsequent major depressive disorder? Journal of Clinical Psychiatry. 2004;65:618–26. doi: 10.4088/jcp.v65n0505. quiz 730. [DOI] [PubMed] [Google Scholar]
- Breton J, Bergeron L, Valla J, Lepine S, Houde L, Gaudet N. Do children aged 9 through 11 years understand the DISC version 2.25 questions? Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:946–956. doi: 10.1097/00004583-199507000-00019. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–44. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Edelbrock C, Costello AJ, Dulcan MK, Kalas R, Conover NC. Age differences in the reliability of the psychiatric interview of the child. Child Development. 1985;56:265–275. [PubMed] [Google Scholar]
- Fallon T, Schwab-Stone M. Determinants of reliability in psychiatric surveys of children aged 6-11 years: A test-retest study. Journal of Child Psychology and Psychiatry. 1994;35:1391–1408. doi: 10.1111/j.1469-7610.1994.tb01282.x. [DOI] [PubMed] [Google Scholar]
- Faraone S, Biederman J, Milberger S. How reliable are maternal reports of their children's psychopathology?: One year recall of psychiatric diagnoses of ADHD children. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:1001–1008. doi: 10.1097/00004583-199508000-00009. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders-Clinician Version (SCID-CV) American Psychiatric Press; Washington, DC: 1997. [Google Scholar]
- Fyer AJ, Mannuzza S, Chapman TF, Martin LY, Klein DF. Specificity in familial aggregation of phobic disorders. Archives of General Psychiatry. 1995;52:564–573. doi: 10.1001/archpsyc.1995.03950190046007. [DOI] [PubMed] [Google Scholar]
- Gittelman R, Klein DF. Relationship between separation anxiety and panic and agoraphobic disorders. Psychopathology. 1984;17:56–65. doi: 10.1159/000284078. [DOI] [PubMed] [Google Scholar]
- Goodwin R, Lipsitz J, Chapman T, Mannuzza S, Fyer A. Obsessive compulsive disorder and separation anxiety comorbidity in early onset panic disorder. Psychological Medicine. 2001;31:1307–1310. doi: 10.1017/s0033291701004366. [DOI] [PubMed] [Google Scholar]
- Harrington R, Fudge H, Rutter M, Pickles A, Hill J. Adult outcomes of childhood and adolescent depression I: Psychiatric status. Archives of General Psychiatry. 1990;47:465–473. doi: 10.1001/archpsyc.1990.01810170065010. [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker DR, Biederman J. Rationale and principles for early intervention with young children at risk for anxiety disorders. Clinical Child and Family Psychology Review. 2002;5:161–72. doi: 10.1023/a:1019687531040. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four Factor Index of Social Status. Yale Press; New Haven: 1975. [Google Scholar]
- Kessler RC, Stang PE, Wittchen HV, Ustun TB, Roy-Burne PP, Walters EE. Lifetime panic-depression comorbidity in the National Comorbidity Survey. Archives of General Psychiatry. 1998;55:801–808. doi: 10.1001/archpsyc.55.9.801. [DOI] [PubMed] [Google Scholar]
- Klein RG. Is panic disorder associated with childhood separation anxiety disorder? Clinical Neuropharmacology. 1995;18:S7–S14. [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Lipsitz JD, Martin LY, Mannuzza S, Chapman TF, Liebowitz MR, Klein DF, Fyer AJ. Childhood separation anxiety disorder in patients with adult anxiety disorders. American Journal of Psychiatry. 1994;151:927–929. doi: 10.1176/ajp.151.6.927. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Zhang H, Avenevoli S, Acharyya S, Neuenschwander M, Angst J. Longitudinal trajectories of depression and anxiety in a prospective community study: the Zurich Cohort Study. Archives of General Psychiatry. 2003;60:993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- Mick E, Santangelo S, Wypij D, Biederman J. Impact of maternal depression on ratings of comorbid depression in adolescents with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:314–319. doi: 10.1097/00004583-200003000-00013. [DOI] [PubMed] [Google Scholar]
- Miettinen OS. Theoretical Epidemiology. John Wiley; New York: 1985. [Google Scholar]
- Moreau D, Follett C. Panic disorder in children and adolescents. Child and Adolescent Psychiatric Clinics of North America. 1993;2:581–602. [Google Scholar]
- Orvaschel H. Schedule for Affective Disorder and Schizophrenia for School-Age Children Epidemiologic Version. Nova Southeastern University, Center for Psychological Studies; Ft. Lauderdale: 1994. [Google Scholar]
- Otto M, Pollack MH, Maki KM, Gould RA, Worthington JJ, Smoller JW, Rosenbaum J. Childhood history of anxiety disorders among adults with social phobia: Rates, correlates, and comparisons with patients with panic disorder. Depression and Anxiety. 2001;14:209–213. doi: 10.1002/da.1068. [DOI] [PubMed] [Google Scholar]
- Otto MW, Pollock MH, Rosenbaum JF, Sachs GS, Asher RH. Childhood history of anxiety in adults with panic disorder: Association with anxiety sensitivity and comorbidity. Harvard Review of Psychiatry. 1994;1:288–293. doi: 10.3109/10673229409017091. [DOI] [PubMed] [Google Scholar]
- Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry. 1998;55:56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Pollack MH, Otto MW, Sabatino S, Majcher D, Worthington JJ, McArdle ET, Rosenbaum JF. Relationship of childhood anxiety to adult panic disorder: Correlates and influence on course. American Journal of Psychiatry. 1996;153:376–381. doi: 10.1176/ajp.153.3.376. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone M, Fallon T, Briggs M, Crowther B. Reliability of diagnostic reporting for children aged 6-11 years: a test-retest study of the Diagnostic Interview Schedule for Children- Revised. American Journal of Psychiatry. 1994;151:1048–54. doi: 10.1176/ajp.151.7.1048. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Dulcan M, Davies M, Piacentini J, Schwab-Stone M, Lahey B, Bourdon K, Jensen P, Bird H, Canino G, Regier D. The NIMH diagnostic interview schedule for children version 2.3 (DISC-2.3): Description, acceptability, prevalence rates, and performance in the MECA study. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R: Non-Patient Edition (SCID-NP, Version 1.0) American Psychiatric Press; Washington, DC: 1990. [Google Scholar]
- Stata Corporation . Stata User's Guide: Release 9. Stata Corp LP; College Station, TX: 2005. [Google Scholar]
- Stein MB, Fuetsch M, Muller N, Hofler M, Lieb R, Wittchen HU. Social anxiety disorder and the risk of depression: a prospective community study of adolescents and young adults. Archives of General Psychiatry. 2001;58:251–6. doi: 10.1001/archpsyc.58.3.251. [DOI] [PubMed] [Google Scholar]
- Warner V, Mufson L, Weissman M. Offspring at high and low risk for depression and anxiety: Mechanisms of psychiatric disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:786–797. doi: 10.1097/00004583-199506000-00020. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Leckman JF, Merikangas KR, Gammon GD, Prusoff BA. Depression and anxiety disorders in parents and children: Results from the Yale Family Study. Archives of General Psychiatry. 1984;41:845–852. doi: 10.1001/archpsyc.1984.01790200027004. [DOI] [PubMed] [Google Scholar]