Abstract
Background
The prevalence of patients with mental health problems in general practice is high, and at least one-third of these problems last for 6 months or longer. Patients with these problems take up more time during a consultation and attend more frequently.
Aim
This study investigated the effectiveness of problem-solving treatment for primary care patients with mental health problems. The hypothesis was that patients receiving problem-solving treatment from a nurse would have fewer symptoms after 3 months, or a lower attendance rate, compared with patients receiving the usual care from the GP.
Design of the study
Randomised clinical trial.
Setting
Twelve general practices in Amsterdam and 12 nurses from a mental healthcare institution.
Method
A sample of patients aged ≥18 years were screened for mental health problems with the general health questionnaire (GHQ–12) in the waiting room of the general practices, and were randomised. Patients receiving the problem-solving treatment were required to complete four to six treatment sessions, while patients in the control group were treated as usual by the GP.
Results
No significant difference was found between the groups in terms of improved psychopathology or a decrease in attendance rate. Post-hoc analyses showed a sub-group of patients with more severe pathology who may benefit from problem-solving treatment.
Conclusion
The main results show that problem-solving treatment provided by a nurse adds little to the usual care from the GP for frequent attenders with mental health problems. Post-hoc analyses show that there may be a sub-group of more severely depressed patients who could benefit from problem-solving treatment.
Keywords: anxiety, depression, family practice, nurses, problem-solving, treatment
INTRODUCTION
The prevalence of attenders with mental health problems in general practice is high.1 Most of the patients with these problems experience symptoms of anxiety and depression, which affect up to a third of all patients in general practice.2 Health problems related to anxiety and/or depression also have a major impact on the quality of life of patients, and at least one-third of these problems are experienced for 6 months or longer.3
For the GP, consultations with patients who have health problems related to anxiety and depression frequently pose a challenge for which there are two main reasons. Firstly, the limited time that is available: patients take up more time during a consultation and attend more frequently than other patients, often with vague reasons for their visit.4 Secondly, the implementation of treatment is often difficult: the guidelines for anxiety and depressive disorders recommend psychotropic drugs, counselling, or referral to specialist services for anxiety and depressive disorders.5,6 Nevertheless, many patients can not be treated according to these guidelines because they have different preferences. Although psycho-pharmacy may be effective, it sometimes does have unwanted side effects, there can be a risk of dependency, and patient adherence is often poor.7 Most patients prefer structured counselling,8 but they seldom receive it.9 Due to the demand-driven, time-restricted nature of general practice they usually receive unstructured generic counselling. There is also evidence that for those patients who receive a more structured form of psychological intervention from their GP, its effectiveness is not assessed.1
In order to optimise the care provided for patients with symptoms of anxiety and/or depression, evidence-based treatment covering a wide range of mental health problems is desirable, feasible, and necessary.10
The aim of this study was to evaluate a brief psychological treatment that can be provided in primary care: problem-solving treatment. This has been evaluated in earlier studies, and there is evidence that it can be provided by nurses, and can be an effective way of helping patients with mental health problems in primary care by enabling them to solve everyday problems, in particular patients who suffer from major depression.11,12
This study investigated the effect of problem-solving treatment on feelings of depression and anxiety, and on attendance rates, when provided by mental health nurses for patients with mental health problems in primary care. Patients are defined here as patients with three or more consultations in the previous 6 months. The hypothesis was that patients receiving problem-solving treatment from a nurse would have fewer symptoms after 3 months or a lower attendance rate, compared with patients receiving usual care from the GP.
METHOD
Patient recruitment and selection
Full details of the design of the study have been previously published.13 Between November 2003 and May 2005, consecutive patients were screened for the presence of mental health problems at one of the 12 general practices in and around Amsterdam, the Netherlands. Patients who were eligible for participation were those who screened positive (that is, a negative score on more than three out of 12 questions) on the General Health Questionnaire (GHQ–12),14–16 had visited their GP three times or more in the previous 6 months, were over 18 years of age, were able to speak Dutch, and were willing to undergo brief psychological treatment. Psychiatric and medical comorbidities were not reasons for exclusion, unless they were potentially life threatening (that is, suicidal ideation and terminal medical illness) or were expected to severely limit the patient's participation or adherence to treatment (that is, psychosis, dementia, severe personality disorders, severe somatisation, and current substance abuse). Patients who had received treatment from a mental health professional during the previous year were also excluded.
How this fits in
Patients who consult their GP because they have health problems related to anxiety and depression frequently pose a challenge in daily practice. This is due to the limited time available during the consultation and the sometimes difficult implementation of treatment. Problem-solving treatment seems to be an adequate method for patients with such problems and can be provided by mental health nurses in general practice. The results of this study suggest that problem-solving treatment provided by a nurse adds little to the usual care from the GP for patients with mental health problems.
Recruitment of community nurses
Nurses from one of the mental healthcare organisations in Amsterdam were willing to cooperate. This resulted in the participation of 12 enthusiastic nurses with varying nursing backgrounds, but all with experience working in mental health care.
The training programme
The training programme consisted of two parts. In the first part, the nurses were trained by two members of a group of researchers that developed problem-solving treatment for primary care.17 Training consisted of workshops that focused on the features of mental health problems in primary care, the theory and rationale of problem-solving treatment, and role-play exercises supervised by the trainers. The role playing was videotaped and evaluated. In the second part, the nurses treated four pilot patients, closely supervised by a cognitive behavioural therapist. Audiotapes were made during treatment of the pilot patients and feedback was given during supervision sessions. They also filled in forms during the sessions according to the problem-solving treatment protocols, and these were handed in to the researcher at the end of the treatment. After completing these two parts of the training the nurses could start treating patients in the trial in the same manner as they had treated the patients in the pilot.
Problem-solving treatment
D'Zurilla and Goldfried defined problem-solving therapy for the first time in 1971.18 In 1995, Gath and Mynors-Wallis conducted an experiment based on a fundamental form of this therapy in primary care and called it problem-solving treatment.19 The treatment is brief (less than 4 hours), and focuses on practical skill building. It consists of a maximum of six sessions, each of which contains seven steps of problem solving (Box 1), which are applied in a systematic manner to achieve problem resolution for everyday problems, such as not being able to do all the housework in one day, or not being able to do activities they like. The rationale is that the treatment increases the patient's understanding of the relationship between everyday problems and psychological symptoms. The goal of problem-solving treatment is to stimulate an active attitude towards these everyday problems, and by reaching goals in the everyday problems, achieve a reduction in mental health problems.
Box 1. Problem-solving treatment.
-
▸
Problem-solving treatment contains seven stages:
Explanation and rationale
Problem definition
Establishing achievable goals
Generating solutions
Selecting preferred solution
Implementing solution
Evaluation of progress
-
▸
Characteristics
4–6 sessions
First session maximum 60 minutes, following sessions maximum 30 minutes
Strategy for coping with present and future problems
Role of therapist decreasing: patient taking over control.
Randomised clinical trial
After the intake assessments, the patients were randomly assigned to one of the two treatment conditions: problem-solving treatment provided by a mental health nurse, or usual care from the GP. Randomisation was performed at patient level; half of the patients were randomised either to the problem-solving treatment group or to a usual care group. Random-permuted blocks of four were made to ensure the equal distribution of patients. An external researcher performed this concealed allocation, and independent interviewers evaluated the patients. All patients gave written informed consent before randomisation.
Assessments
The participants received written questionnaires at baseline, and 3 months after the intervention. The primary outcome was a reduction of symptom severity measured by the Hospital Anxiety and Depression Scale (HADS).20 The secondary outcome was reduction of symptoms measured with the Patient Health Questionnaire (PHQ).21 This provides diagnoses at a syndrome level in this research; improvement in problem solving skills according to the Social Problem Solving Inventory-Revised (SPSI–R);22 psychological and physical wellbeing by the Short-Form 36.23 A detailed description of the assessment questionnaires has been published previously.13
Power calculation
The calculation of the study size was based on a clinically-relevant difference between interventions with an effect size of 0.4 on the primary outcome HADS measurement.24 A total score of 8 points (SD 4; difference of 2) in the intervention group was estimated. To detect this difference with a two-sided significance level (α) of 0.05 and a power (1−β) of 0.80, a sample size of 130 patients was needed, divided into two groups of 65.25 Taking into account a dropout rate of 20%, a sample size of 160 was estimated.
Statistical analysis
Baseline similarity was studied. Differences within the groups were compared with paired t-tests to assess changes over time. General linear models (univariate) and logistic regression (binary) with baseline measurement as a covariate were used to investigate the effect of the intervention (that is, the difference in outcome between the problem-solving treatment group and the usual care after 3 months, corrected for outcome measurements at baseline). The level of significance was set at P<0.05. Finally, two post-hoc analyses were performed. All analysis were performed in SPSS (version 10).
RESULTS
Pre-treatment characteristics
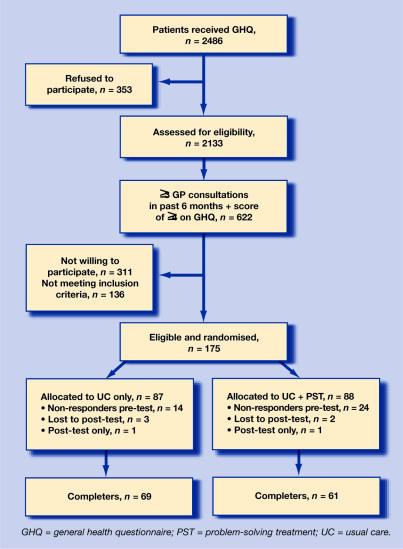
Between October 2003 and March 2005, 130 patients completed the assessments. The patients who dropped out at baseline and were lost to follow up (n = 45) showed no differences with regard to age or sex compared with those who completed the study. Dropout was 21% (18/87) in the control group and 31% (27/88) for problem-solving treatment, with no significant difference between the groups (χ2 = 2.287, degrees of freedom = 1, P = 166). Reasons for dropout were: unwilling to participate after providing written informed consent; no longer any problems; and too much strain. A flowchart of the participants can be found in Figure 1. As expected, baseline assessment was similar for both groups (Table 1).
Figure 1.
Flowchart of participants.
Table 1.
Baseline characteristics.
| Usual care n (%) | Problem-solving treatment n (%) | Total n (%) | |
|---|---|---|---|
| Mean age, years (SD) | 52.5 (15.1) | 53.3 (14.4) | 52.8 (14.7) |
| Female sex | 46 (75.4) | 46 (66.7) | 92 (70.8) |
| Married/cohabiting | 28 (45.9) | 33 (47.8) | 61 (46.9) |
| Education level | |||
| Low | 16 (26.2) | 13 (18.8) | 29 (22.3) |
| Medium | 18 (29.5) | 21 (30.4) | 39 (30) |
| High | 23 (37.7) | 29 (42) | 52 (40) |
| Minimum of 1 diagnosis MINI | 37 (60.7) | 39 (56.5) | 76 (58.5) |
| GHQ, mean (SD) | 7.84 (2.7) | 7.36 (2.4) | 7.58 (2.6) |
GHQ = general health questionnaire. MINI = Mini International Neuropsychiatric Interview.
Main treatment effects
Symptom severity
The HADS depression symptom level improved significantly for patients in the problem-solving treatment group (mean difference 1.92; 95% CI = 0.95 to 2.88) but also for patients in the control group (mean difference 1.26; 95% CI = 0.42 to 2.10). The HADS anxiety symptom level also improved significantly post treatment in both groups (problem-solving treatment mean difference 1.45, [95% CI = 0.51 to 2.39] versus usual care mean difference 1.43; [95% CI = 0.63 to 2.24]). After correction for baseline scores, post-test values did not reach statistical significance (Table 2).
Table 2.
ANCOVA and logistic regression for differential treatment effects with the pre test as covariate.
| Usual care group | Problem-solving treatment group | F | P-value | |
|---|---|---|---|---|
| HADS, mean (SD) | 8.97 (4.1) | 8.17 (3.9) | ||
| Anxiety pre | 7.54 (4.1) | 6.72 (3.7) | 0.35a | 0.558 |
| Anxiety post | 7.67 (4.0) | 7.12 (3.8) | ||
| Depression pre | 6.41 (4.0) | 5.20 (3.8) | 2.41a | 0.123 |
| Depression post | 16.54 (7.0) | 15.25 (7.0) | ||
| Total pre | 13.91 (7.4) | 11.92 (6.9) | 1.37a | 0.243 |
| Total post | ||||
| SPSI-R, mean (SD) | ||||
| SPSI-R pre | 90.94 (13.1) | 85.49 (12.4) | ||
| SPSI-R post | 92.06 (12.3) | 90.06 (10.9) | 1.83a | 0.179 |
| SF-36, mean (SD) | ||||
| Physical components score pre | 41.17 (11.4) | 46.49 (1.7) | ||
| Physical components score post | 43.43 (12.0) | 49.33 (11.3) | 2.25a | 0.136 |
| Mental components score pre | 37.75 (11.1) | 38.11 (10.3) | ||
| Mental components score post | 40.20 (12.4) | 41.78 (10.9) | 0.74a | 0.391 |
| Frequency of consulting GP, mean (SD) | ||||
| Pre | 3.28 (2.7) | 2.83 (3.0) | ||
| Post | 1.47 (2.1) | 1.39 (1.5) | 0.007b | 0.932 |
F (1,128).
F (1,117). ANCOVA = analysis of covariance (F). HADS = Hospital Anxiety and Depression Scale. Post = post treatment. Pre = pre treatment. SPSI–R = Social Problem Solving Inventory-Revised.
Problem solving skills
The standardised total score of the SPSI–R improved significantly at post treatment for patients in the problem-solving treatment group as well as for patients in the control group (problem-solving treatment mean difference −5.46, [95% CI = −8.10 to −2.81] versus usual care mean difference −2.00; [95% CI = −3.95 to −0.052]). Analysis of covariance with pre-treatment as covariate showed no significant difference at post treatment (Table 2).
Psychological and physical wellbeing
The SF−36 has two composite scales for mental and physical wellbeing. After treatment, patients in the problem-solving treatment group experienced an improvement in their mental wellbeing (mean difference −3.77; [95 % CI = −6.33 to −1.98]), as well as in their physical wellbeing (mean difference −2.84; [95% CI = −4.91 to −0.78]). Patients in the control group showed no significant improvement. However, after correction for baseline values, this effect disappeared (Table 2).
Mental health problems
The PHQ allows sub-threshold and full diagnoses (at syndrome level). The three most frequently occurring diagnoses (major depressive disorder, panic disorder, and somatic disorder) were analysed. For all three diagnoses no significant differences between the groups were found with χ2 tests on post treatment.
Frequency of attendance
The frequency of attendance in both groups declined significantly with 1.5 visits in 12 weeks. Paired t-tests showed a statistically significant decline in both groups, but after correction for baseline no differences were found (Table 2).
Post-hoc analyses
To evaluate the effects on the most relevant mental health problems, depression and anxiety, the HADS score was dichotomised (≥8 yes/no). This is the clinically-relevant HADS cut-off point for case finding in the general practice population.19,25,26 Taking this cut-off into account for the depression sub-scale, a significant improvement was found in patients in the problem-solving treatment group who were suffering from depression (26 on pre treatment and 15 on post treatment versus 33 on pre treatment and 30 on post treatment for usual care). In the problem-solving treatment group the symptoms of depression declined significantly, in contrast with the scores in the control group (odds ratio [OR] = 0.651, 95% CI = 0.447 to 0.948). For the HADS anxiety sub-scale no significant difference was found between the groups.
The second post-hoc analysis was based on the hypothesis that patients with one or more mental health problems would benefit most from problem-solving treatment. Therefore the diagnosis measured with the PHQ was separated (≥1 yes/no). Every patient who scored ≥1 diagnosis was included in the analysis. Pre treatment there were 35 patients in the problem-solving treatment group with ≥1 diagnosis, and post treatment there were only 17. The effect of the interventions was investigated with logistic regression. In this respect, logistic regression with the baseline number of PHQ diagnoses as covariate, confirmed this hypothesis because it revealed a main effect in the problem-solving treatment group concerning the number of the diagnoses (OR = 0.675; 95% CI = 0.448 to 0.964). The patients in control group decreased from 44 to 35. There was no significant decline in the number of diagnoses in the control group.
DISCUSSION
Summary of main findings
This study demonstrates that problem-solving treatment provided by a nurse adds little to usual care from the GP for patients with mental health problems. However, the post-hoc-analyses showed an outcome which suggests that there may be a sub-group of patients with more severe psychopathology who may benefit more from problem-solving treatment. The results of this trial also suggest that problem-solving treatment, provided by a trained nurse, for patients who are severely depressed (HADS ≥8) or for patients with more than one diagnosis (at syndrome level) may be an effective intervention. For all other primary care patients with mental health problems this study provides no convincing evidence that GPs should recommend problem-solving treatment provided by nurses.
Comparison with existing literature
Recently, another trial in primary care trial focused on problem-solving treatment provided by community health nurses. The patients who received problem-solving treatment were compared with patients who received usual care from their GP. Both groups were treated for common mental health problems. This trial demonstrated a lack of effect.16 The current findings point in the same direction. In earlier studies a clear effect of problem-solving treatment provided by nurses was found in patients with major depression.12,27,28 The diagnostic heterogeneity of general practice may limit the potential effect of problem-solving treatment.29,30
Strengths and limitations of the study
Because of the sample size, this trial makes a relevant qualitative contribution to the existing knowledge about problem-solving treatment and the heterogeneous population of general practice. This heterogeneous study population is typical for general practice, but a homogenous sample of patients may not have been identified as an entry criterion of the number of consultations in the last 6 months was perhaps too low. In the Netherlands in 2005 a mean consult frequency of three visits a year was considered an average.31 But, taking the ages into account (no limit to age) it is not possible to state that this was a very sick group. A higher threshold is recommended. A period of 6 months was chosen because of the high rates of spontaneous recovery in this period32 and it was thought that this would also be valid for the target group. It may have included too many patients with mild or self-limiting problems which could potentially be harmful. This could have influenced the effectiveness of the study and perhaps explains the 25% dropout rate. Half of the patients who were approached (n = 311) did not participate in this project and there is no information about their motivation.
Implications for future research and clinical practice
To decide which general practice patients profit most from problem-solving treatment provided by nurses, the GP should assess the patients' ability to ‘psychologise’ (in contrast with ‘somatise’) and the high severity of the depression and/or multiple psychopathology. The substantial number of dropouts in this study supports the usual stepped-care approach of general practice: many patients ‘no longer had problems anymore’. In agreement with Kendrick et al,16 limiting specialised problem-solving treatment to patients who do not recover with usual care from their GP is proposed. Further research is needed to determine if the results of this study can be replicated in a recruited sub-group with a higher number of patients, and to investigate how to identify this group in a feasible way in general practice. In addition, research is needed to identify specific sub-groups who benefit most from problem-solving treatment, or to develop additional primary care interventions for these patients.
Acknowledgments
We would like to thank all the patients who participated in the screening as well as the study, all GPs and their assistance and all the participating mental health nurses.
Funding body
This project was funded by the Health Research and Development Council (ZONMW, number 4200.0001) in the Netherlands
Ethical approval
The Medical Ethics Committee of the VU University Medical Centre approved the study protocol (number 03/155)
Competing interests
The authors have stated that there are none
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Huibers MJ, Beurskens AJ, Bleijenberg G, van Schayck CP. The effectiveness of psychosocial interventions delivered by general practitioners. Cochrane Database Syst Rev. 2003;(2) doi: 10.1002/14651858.CD003494. CD003494. [DOI] [PubMed] [Google Scholar]
- 2.Bijl RV, van Zessen G, Ravelli A. Psychiatric morbidity among adults in the Netherlands: the NEMESIS-Study. II. Prevalence of psychiatric disorders. Netherlands Mental Health Survey and Incidence Study. (In Dutch) Ned Tijdschr Geneeskd. 1997;141(50):2453–2460. [PubMed] [Google Scholar]
- 3.Mynors-Wallis L, Davies I, Gray A, et al. A randomised controlled trial and cost analysis of problem-solving treatment for emotional disorders given by community nurses in primary care. Br J Psychiatry. 1997;170:113–119. doi: 10.1192/bjp.170.2.113. [DOI] [PubMed] [Google Scholar]
- 4.Zantinge EM, Verhaak PF, Bensing JM. The workload of GPs: patients with psychological and somatic problems compared. Fam Pract. 2005;22(3):293–297. doi: 10.1093/fampra/cmh732. [DOI] [PubMed] [Google Scholar]
- 5.Terluin B, Van Heest FB, van der Meer K, et al. Dutch College of General Practitioners guidelines for anxiety disorders (first revision). (In Dutch) Huisarts Wet. 2004;47(1):26–37. [Google Scholar]
- 6.Van Marwijk HWJ, Bijl D, Van Gelderen M, et al. Dutch College of General Practitioners guideline for depression, first revision [NHG-Standaard Depressieve stoornis (depressie). Eerste herziening. Huisarts Wet. 2003;46:614–623. [Google Scholar]
- 7.Chilvers C, Dewey M, Fielding K, et al. Antidepressant drugs and generic counselling for treatment of major depression in primary care: randomised trial with patient preference arms. BMJ. 2005;322(7289):772–775. doi: 10.1136/bmj.322.7289.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Schaik DJ, Klijn AF, van Hout HP, et al. Patients' preferences in the treatment of depressive disorder in primary care. Gen Hosp Psychiatry. 2004;26(3):184–189. doi: 10.1016/j.genhosppsych.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Cardol M, van Dijk L, De Jong JD, et al. Utrecht, Bilthoven: Nivel, Rijksinstituut voor Volksgezondheid en Milieu; 2004. General practice care: what does the gate-keeper do? Second National Study of diseases and procedures in general practice (In Dutch) [Google Scholar]
- 10.The MaGPIe Research Group. The treatment of common mental health problems in general practice. Fam Pract. 2006;23(1):53–59. doi: 10.1093/fampra/cmi097. [DOI] [PubMed] [Google Scholar]
- 11.Kendrick T, Simons L, Mynors-Wallis L, et al. A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study. Health Technol Assess. 2005;9(37):1–104. iii. doi: 10.3310/hta9370. [DOI] [PubMed] [Google Scholar]
- 12.Mynors-Wallis L. Problem-solving treatment for anxiety and depression. A practical guide. 1st edn. Oxford: Oxford University Press; 2005. [Google Scholar]
- 13.Schreuders B, van Oppen P, Van Marwijk HWJ, et al. Frequent attenders in general practice: problem solving treatment provided by nurses [ISRCTN51021015] BMC Fam Pract. 2005;6:42. doi: 10.1186/1471-2296-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koeter MWJ, Ormel J. General Health Questionnaire. Lisse: Swets, Test Services; 1991. Dutch version, manual (in Dutch) [Google Scholar]
- 15.Dowrick C, Dunn G, Ayuso-Mateos JL, et al. Problem solving treatment and group psychoeducation for depression: multicentre randomised controlled trial. Outcomes of Depression International Network (ODIN) Group. BMJ. 2000;321(7274):1450–1454. doi: 10.1136/bmj.321.7274.1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kendrick T, Simons L, Mynors-Wallis L, et al. Cost-effectiveness of referral for generic care or problem-solving treatment from community mental health nurses, compared with usual general practitioner care for common mental disorders: randomised controlled trial. Br J Psychiatry. 2006;189:50–59. doi: 10.1192/bjp.bp.105.012435. [DOI] [PubMed] [Google Scholar]
- 17.Mynors-Wallis L. Problem-solving treatment: evidence for effectiveness and feasibility in primary care. Int J Psychiatry Med. 1996;26(3):249–262. doi: 10.2190/0HVY-CD2F-0KC7-FVTB. [DOI] [PubMed] [Google Scholar]
- 18.D'Zurilla TJ, Goldfried MR. Problem solving and behavior modification. J Abnorm Psychol. 1971;78(1):107–126. doi: 10.1037/h0031360. [DOI] [PubMed] [Google Scholar]
- 19.Mynors-Wallis LM, Gath DH, Lloyd-Thomas AR, Tomlinson D. Randomised controlled trial comparing problem solving treatment with amitriptyline and placebo for major depression in primary care. BMJ. 1995;310(6977):441–445. doi: 10.1136/bmj.310.6977.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 21.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 22.Maydeu-Olivares A, D'Zurilla TJ. Social Problem Solving Skills Inventory-Revised (SPSI-R): a factor analytic study of the Social-Problem Solving Inventory: an integration of therapy and data. Cognitive theory and research. 1996;20(2):115–133. [Google Scholar]
- 23.Aaronson NK, Muller M, Cohen PD, et al. Translation, validation, and norming of the Dutch language version of the SF-36 health survey in community and chronic disease populations. J Clin Epidemiol. 1998;51(11):1055–1068. doi: 10.1016/s0895-4356(98)00097-3. [DOI] [PubMed] [Google Scholar]
- 24.Crawford J, Henry J, Crombie C, Taylor E. Normative data for the HADS. Br J Clin Psych. 2001;40(4):429–434. doi: 10.1348/014466501163904. [DOI] [PubMed] [Google Scholar]
- 25.Altman DG. Practical statistics for medical research. London: Chapman & Hall; 1991. [Google Scholar]
- 26.Olsson I, Mykletun A, Dahl A. The Hospital Anxiety and Depression Rating Scale: a cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry. 2005;5:46. doi: 10.1186/1471-244X-5-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spinhoven PH, Ormel J, Sloekers PPA, et al. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27(2):363–370. doi: 10.1017/s0033291796004382. [DOI] [PubMed] [Google Scholar]
- 28.Lin EHB, Katon W, Tang L, et al. Effect of improving depression care on pain and functional outcomes among older adults with arthritis: a randomized controlled trial. JAMA. 2003;290(18):2428–2429. doi: 10.1001/jama.290.18.2428. [DOI] [PubMed] [Google Scholar]
- 29.Mynors-Wallis L. Does problem-solving treatment work through resolving problems? Psychol Med. 2002;32(7):1315–1319. doi: 10.1017/s0033291702006025. [DOI] [PubMed] [Google Scholar]
- 30.Bower P, Rowland N. Effectiveness and cost effectiveness of counselling in primary care. Cochrane Database Syst Rev. 2006;3 doi: 10.1002/14651858.CD001025.pub2. CD001025. [DOI] [PubMed] [Google Scholar]
- 31.Verheij RA, Schellevis FC, Hingstman L, de Bakker DH. General practitioner care: how large is the use and from what does it exist? Public Health Future explorations, the National Public Health Compass (in Dutch) Bilthoven: RIVM; 2006. [Google Scholar]
- 32.Spijker J, de Graaf R, Bijl RV, et al. Duration of major depressive episodes in the general population: results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Br J Psychiatry. 2002;181:208–213. doi: 10.1192/bjp.181.3.208. [DOI] [PubMed] [Google Scholar]