Abstract
Background
Children aged 6–12 years are usually seen in primary care with an adult carer. It is a government and professional priority for doctors to try and involve these children in their medical consultations.
Aim
To ascertain the evidence available on the amount and type of involvement that children in the 6–12 year age group have in their primary care consultations when the consultation was held with a child, a GP, and an adult.
Design of the study
Literature review.
Method
Data sources included MEDLINE, CINAHL, EMBASE, and ERIC, The Cochrane library, PsychINFO, Web of Science and Wilson's Social Science abstracts, hand searching for references, and contact with authors.
Results
Twenty-one studies were selected for inclusion in the study. Children were found to have little quantitative involvement in their own consultations. They may take part during information gathering but are unlikely to participate in the treatment planning and discussion parts of the consultation.
Conclusion
Children in the 6–12 year age group have little meaningful involvement in their consultations.
Keywords: communication, consultation, general practice, paediatric, primary care, triadic
INTRODUCTION
The Institute of Public Policy Research has published a code of conduct in which children in partnership with their parents and health professionals can participate in decision making during their own medical consultations. A convincing evidenced based argument is presented, that children over the age of 5 years should be presumed competent to be involved in their own healthcare choices.1 Children in this age group are often capable of complex tasks such as playing chess or complicated homework.
The British Medical Association recommends that good practice for health professionals entails encouraging a child patient to express their views and participate in their health care.2 The National Service Framework for children puts the child at the centre of their care and states that: the child and parent should be actively involved in decisions made about the child's health, facilitated by appropriate information; that a child's consent where required should be sought, and also adds a reminder that it is difficult for a child to communicate about abusive experiences if they have had them.3 These policy directives assume that a child should have some involvement when he or she is the patient in the primary care consultation.
Qualitative studies commissioned by the Health Education Board for Scotland found that primary school children were both aware of, and understood, current health issues. These children were receptive to health messages such as the value of a healthy diet, exercise, and not smoking.4 Further evidence of the benefit of children's active involvement in their health care comes from a randomised controlled trial where children aged 8–12 years with asthma were included in a self-management programme. In the intervention group, games were used to teach children to recognise their symptoms and manage their illness. These children's asthma significantly improved compared with the control group.5
It has been suggested that guiding a child towards autonomy in managing their own health problem is practical: by school age children are spending increasing time away from their parents and may have to manage their own medication.6 When asked, some children indicate that they do not feel involved in their medical care and would like more say.7 At the older end of this age range there may be occasions when it is appropriate for the consultation to be held entirely with the child alone, if they are competent, and to do so is in their best interest.8 However, children aged 6–12 years are almost always seen with an adult carer and the consultations are triadic.9
It is known that children are not always treated as active participants in their medical encounters. For example, in a seminal research study on doctor–patient communication, which took place in a paediatric emergency clinic, the researchers stated that the patient in ‘paediatrics’ refers to the patient's parent.10
The child was similarly ignored in a major contribution to research on medical interaction, which produced a detailed analysis of 1020 paediatric encounters. The author explained in his report of the study why children did not feature.11
‘… the reason for my exclusion of children … is that they themselves are largely excluded from the consultation.’
These studies were conducted decades ago. Now there is more interest in children's active participation in medical consultations.12 Strides are being taken to develop means whereby children can evaluate their doctors, and where the children's opinion of their medical consultations matter.13
Consultation skills teaching has been shown to be an effective means of improving a doctor's skills at consulting.14 Specific training in consultation skills for paediatric encounters has been advocated.15
There are many examples of anecdotal writings where authors describe paediatric consultations and give advice on how a clinician should proceed.16,17
This study was carried out to discover more about the paediatric consultations based on research evidence. A literature search was conducted to ascertain the amount and type of involvement children in the 6–12 year age group have in their primary care consultations when the consultation was held with a child, a GP, and an adult.
How this fits in
There is evidence that if children directly participate in their health care it is beneficial for them. Children over 5 years old should be presumed competent to be involved in healthcare decisions concerning them, in partnership with their adult carer and/or parent and health professionals. This review demonstrates that pre-adolescent children have little meaningful involvement in their primary care consultations.
METHOD
Search strategy
The search was very broad because the words used to describe a child's part in the communication in medical consultations are general and appear in abstracts and keyword selection unrelated to the topic of this review. The procedure for finding eligible studies included searching the following databases, (search date 6 December 2006); MEDLINE, CINAHL, EMBASE, ERIC, the Cochrane library, PsychINFO, Web of Science, and Wilson's Social Science abstracts.
The keywords used for the search are shown in Box 1. These were entered into the electronic databases for searches and the strategy was adapted appropriately for the different databases.
Box 1. Keywords used in database search.
Child or children or paediatric or pediatric
Communication or talk or conversation or encounter or consulting or consultation
Primary care or general practice or doctor or general practitioner or GP or family practice or family practitioner
1 and 2 and 3
Methodological filters were not used. Results from the searches were manually searched to select possible studies for inclusion and this resulting list was then examined in more detail. Full text papers were looked at when appropriate. The search in PsychINFO and the Web of Science was adapted in line with the requirements of the database, keywords used were ‘communication,’ ‘doctor,’ and ‘children’.
The Cochrane Library was searched using the medical subject headings (Mesh) terms, communication and child. Books concerning communication with children were also examined. Relevant chapters found in books and articles yielded by the database searches were hand-searched for references.
Citation searches were run to find similar articles to those selected as appropriate for this study, as well as papers that had cited these articles as references. The following journals were hand-searched; British Medical Journal, British Journal of General Practice, Journal of Communication, Social Science and Medicine, and Communication and Medicine. Experts in the field were contacted to ask if they were aware of any further references.
Selection process
For inclusion the papers had to be relevant to communication with children in the primary care consultation but could also extend to settings outside primary care. The papers were required to mention all three members of the triad: adult, doctor and the child, and to report research on communication in this triad. Published and unpublished work was considered. Excluded were papers referring to children outside the 6–12–years age group, non-medical settings, or settings that were not considered relevant to primary care in the UK. There was no language restriction imposed when doing the searches. This review was initially undertaken prior to, and as part of, a study conducted investigating communication in the primary care paediatric consultation which is reported elsewhere in this journal.18 The results of this study are included in this review and discussed in detail in the article reporting the study.18
Data extraction and analysis
One reviewer conducted the search, selected the studies for inclusion, and extracted data, while a second reviewer checked and validated this. The reviewers discussed the appropriateness of the studies included and any disagreement was resolved by discussion.
There was no specific requirement for methodological type or rigour of studies to be included.
The studies found were very heterogeneous and meta-analysis was not applicable. A narrative and tabular summary of the results was made.
RESULTS
Search results
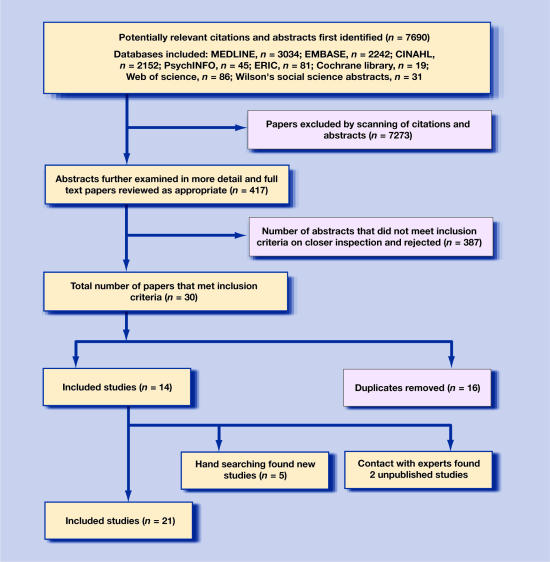
The results of the searches are presented in the flow chart in Figure 1. In total, 21 studies were included in this review. The final 21 studies are tabulated in Tables 1 and 2. (Table 1 for those set in primary care, and Table 2, for those set outside primary care).
Figure 1.
Flow chart of a summary of the study's inclusion and exclusion process.
Table 1.
Studies of paediatric consultations in primary care.
| Author, setting and country | Type of study | Findings: child's contribution to the consultation |
|---|---|---|
| Pantell et al19 Primary care university medical centre, US | Quantitative observational study of 115 videotaped paediatric consultations | The child's contribution, which was largely social, was 14.2% of the consultation. |
| Meeuwesen et al20 General practice, The Netherlands | Quantitative study of 95 videotapes of paediatric triadic consultations taken from an archived collection dating from 1975–1989 | Child's contribution was small, increasing slightly over the years. Child-doctor interaction was between 3–6% of turns. |
| Tates and Meeuwesen21 General practice, The Netherlands | Quantitative observational study of 106 video recordings of paediatric consultations from an archived collection | Turn allocation was examined. Children had 9.4% of turns. GPs tended to take child's age into account but parents did not. |
| Eminson et al22 General practice, UK. | Quantitative study using a triadic scale developed for the study to rate 66 GP consultations for involving the child in the consultation, before and after a teaching package was administered on triadic consultation skills | The GPs scored high at involving the child in the history and early stages of the consultation prior to the teaching. But after the teaching package, were better at involving the child in the later parts of the consultation than before the training. |
| Tates et ala23 General practice, The Netherlands | Qualitative study analysing 106 videotapes of paediatric consultations, from an achieved source. The participants' roles and identities were analysed | A child being invited to begin the consultation increased their involvement in problem formulation. All three participants jointly establish a situation where the consultations end up with the parent speaking for the child, this being a social co-construction where the norm is parents speaking for children. |
| Tates et alb24 General practice, The Netherlands | Quantitative study of 106 video recordings of paediatric consultations from an achieved source. Coded for instrumental versus affective behaviour of the participants | Child's contribution was 9.6% of the consultation. GPs accommodated for the child's age. Parents did not accommodate for age, 80% of advice given on treatment by the GP is directed towards the parent not the child. |
| Tates cet al25 General Practice, The Netherlands | Quantitative study of 105 videos of paediatric consultations taken from an archive coded for supportiveness of adults towards child involvement in the consultation and displays of child involvement | Children have limited involvement, especially at the end of the consultation. GPs and parents mostly assumed a non-supportive role in interaction with the child, 90% of consultations end with child non-participation. When the parents are not supportive towards the child's involvement the consultations are more likely to be doctor–adult dyads. |
| Cahill and Papageorgiou General practice, UK18 | A qualitative study of 31 paediatric primary care consultations | The child's contribution was 5.42%. Adult carers interrupted doctor–child talk when the adults had not had their concerns expressed early in the consultation. |
Table 2.
Papers on paediatric triadic consultations in settings outside primary care.
| Author, setting and country | Type of study | Children's involvement in consultations |
|---|---|---|
| Freemon et al26 Emergency children's hospital clinic, US | Quantitative descriptive study of 285 audiotaped consultations | Doctor–child communication was 12.5% of the total interaction units |
| Tannen and Wallat27,28 Child development centre/US | A series of qualitative analyses of a doctor examining Jody aged 9, in the presence of her mother | Jody's contribution is social, laughter and play Mother's questioning interrupts the examination |
| Aronsson and Rundstrom29 Allergy outpatient's clinic/Sweden | Quantitative study of 30 audiotaped consultations | The child has 8% of total discourse space. The parent has ultimate control, which doctors assist in enhancing. Doctors have control of the turn taking |
| Aronsson and Rundstrom30 Allergy outpatient's clinic, Sweden | Qualitative analysis 30 consultations audiotaped | Children spoken to in a direct or joking way by the doctors, at times to convey a message to parents |
| Van Dulmen31 Paediatric outpatients clinic/The Netherlands | Quantitative observational study, 302 consecutive videotaped consultations | Child's contribution was 4% of total utterance count. This increases with age of child and is at the expense of the parents |
| Tates and Meeuwesen (2001)32 | A review of literature on doctor–parent–child observational communication studies. | Most studies were doctor–parent dyads, not triadic. Children involved little in medical consultations |
| Runeson et al33 Paediatric hospital ward, Sweden. | Qualitative study of 140 critical incidents reported in paediatric triadic encounters | Children's protests were often ignored |
| Stivers34 Paediatric outpatients, US | Qualitative study of 291 videotaped consultations | Children said very little. Children regularly did not end up presenting the problem, even when invited to |
| Young et al35 Oncology clinic, UK | Qualitative study of 13 interviews with children and their parents | Parents described acting in an executive-like capacity with some children saying that they felt marginalised |
| Wassmer et al36 Paediatric outpatients, UK | Quantitative study of 51 audio-recorded consultations | Child's contribution to the conversation was 4.2%. The longer the child's contribution, the shorter the parent's was. Older children talked more than younger children |
| Van Dulmen37 Paediatric clinic/The Netherlands | Quantitative study analyses 846 videotapes of consultations | Children had very little say. They answered questions on medical information. Paediatricians talked to the child or the parent. No evidence of real multiparty talk. Older children were treated in a more child-centred way |
| Nova et al38 Paediatric clinic, Italy | Qualitative analysis of 10 videotaped consultation Content and discourse analysis | Quantitatively limited child contribution to the consultation |
Description of the studies
Eight studies were found that discussed triadic communication in the paediatric primary care consultation as described in Table 1.18–25 Thirteen papers on the paediatric triadic consultation in settings outside primary care, which met the criteria for inclusion, were found as shown in Table 2.26–38 They are diverse in terms of the methodology used to evaluate the consultations, settings, and study designs. Eleven quantitative studies, nine qualitative studies, and one literature review of triadic paediatric consultation were found. The studies came from a variety of countries including the Netherlands, Sweden, the US, Italy, and the UK.
Many studies on communication in paediatric consultations leave out the child's role
This literature review was undertaken to search for studies on communication in the paediatric consultation that reported on the child's part in the communication, as well as that of the adult and doctor. Studies on communication in paediatric consultations where the childs' participation was completely ignored were found, but as this was an exclusion criteria for this review, these studies were excluded.
Tates and Meeuwesen published a review of studies in 2001 on doctor–parent–child communication and comment on the lack of child participation in many of the research studies.32 At the time the study took place, authors found only three papers that were actually about triadic consultations with a doctor, child, and parent. This review was conducted to find studies on triadic paediatric consultations relevant to primary care. A paucity of research was identified on communication in paediatric consultations where the children's role in their own consultation is considered.
The quantitative amount of the child's involvement
Studies that quantify the percentage involvement of the child in their consultations estimate this to be from 3% to 14.2%.18–21,24,26,29,31,36 These studies use different methods to reach these estimates and so are not directly comparable with one another. However, they do show that the child has a limited quantifiable involvement in their own consultation. In addition these studies suggest that the child's involvement is not really meaningful.
Limited meaningful child involvement in these consultations
Some of the studies indicate that in terms of speaking, the children are mostly involved in their consultations in the form of social talk with the doctors.19,27–29,36
Although it has been shown that children can be involved in some of the business or instrumental behaviour in the consultation,24 Tates et al demonstrated that when children are participants in this way, doctor–child exchange is nearly always in the form of the child being an information giver and cooperating with the examination.24
Nova et al's study also showed that the child had limited quantifiable involvement in the consultation, but they found that the child participants express their subjective experience of their illness, which may be ignored.38
Towards the end of the consultation, the child is much less likely to have any involvement in the planning and decision making. This part takes place between the adults, with this distribution of child involvement seen in all the studies that reported this information.19,21,23–26,31,36
When a child was asked to present the problem for attendance, one of the studies suggested that this gave a child more opportunity to go on to have some participation in the latter part of the consultation.23 It has also been shown that if the doctor and child start talking together at the outset of the consultation without the adult carer having had their concerns expressed, this is likely to result in the adult interrupting doctor–child talk.18 However, it has also been shown that, even when prompted by the doctor, children do not generally present the problem themselves.34
Research exploring why the child has limited involvement
Some of the studies have attempted to discover reasons for limited child involvement in medical consultations. Aronsson and Rundstrom demonstrated how rules of politeness affect the doctor's behaviour in paediatric consultations.30 They found that triadic paediatric consultations are governed by politeness conventions; which suggests that doctors do not want to offend parents or challenge parental authority.30
In another analysis, the same authors illustrated how the doctor, who has institutional power, is in a position to invite a participant to speak and to allocate turns in the consultation.29 The adults, who in this study were the parents, have ultimate authority and executive power over the child. This research suggested that many parents act as self-appointed cultural brokers or translators for the child, and that the child is subordinate to both adults.29
Young et al also looked at the triadic consultation and found, as Aronsson and Rundstrom did,29 that parents acted in an executive-like capacity and managed information given to their children.35 Their work involved interviewing children attending an oncology clinic, and some of these children's parents. The aim was to discover more about the parent and the child's account of communication with their health workers. Children in an oncology clinic are likely to have serious illnesses, which has a great impact on the parent. Some of the children explained how they felt marginalised. The researchers were able to demonstrate that the reason behind the parental control of these consultations was a wish to protect the child and do their best for them. This would also be the reason why parents in Runeson et al's study helped staff conduct procedures on protesting children, such as venopuncture.33
Tates et al demonstrated that a child is more likely to speak in a consultation if the doctor is supportive of the child's involvement.25 The child is even more likely to be involved in consultations where both the adults are supportive towards them taking part.25 However, if the adult interrupts the doctor and child speaking together and is not supportive of the doctor and child talking, the consultation is very likely to become a doctor–adult dyad, with the child being excluded.18,20,24 It was found that doctors engaged more with the child the older they were, but parents did not make the same accommodation for the child's age.21
Interestingly, two of the studies showed that when the children did speak more in the consultations, the consultations were not longer, rather the child took up the adult's discourse space.31,36
Limitations of studies included in the review
A number of methodological limitations were identified in the studies found for this review.
Quantifying the consultation
To ‘measure’ the child's involvement in their medical encounters, quantitative researchers break the consultation into units and then code and count them. The difficulty with coding the sophisticated process of verbal and non-verbal communication between three people is that much of the complexity is lost. Silence and the use of non-verbal communication techniques can have an impact on a consultation.
Observational studies using audio recordings, which do not capture non-verbal communication, are limited in their capacity to comment fully on the communication during the consultation. Even studies using scales, which code for both verbal and non verbal interaction, are subject to inaccuracies as these rely on the coder's ability to reproduce the same standards from one consultation to the next. Some of the studies selected only consultations for inclusion if the child said something, which could give a misleadingly high child-contribution estimate.19,38 The estimation of child involvement should therefore be interpreted with caution, but since all the studies show very limited child involvement in their paediatric consultation, it could be argued that any inaccuracies in measuring this phenomenon would not alter the overall picture.
Sample bias
Finding a sample that is generalisable can be a problem when conducting observational research on communication in paediatric consultations, as not all clinicians and patients are comfortable having consultations analysed. The doctors and patients taking part in these studies were aware that their performance was being assessed which could lead to a selection bias. This bias needs to be considered when interpreting the studies but is probably unavoidable. In research, all participants must give fully informed consent and so are likely to have an idea of the area of research, if not the exact research question. For example, doctors may make an unusual effort to talk to the children, which would increase the percentage of involvement that children are estimated to have in the consultations.
Setting bias
Results from one study setting are not always transferable to another, especially if the settings are in different countries, cultures and healthcare systems.
DISCUSSION
Summary of the main findings
The available literature on children's communication in the consultation indicates that the child patient has little involvement in their consultations. They may have some input into the history and examination phases of the encounter, but much less involvement in the explanation and planning parts. Doctors are in a position to allocate turns in these consultations. If a doctor is talking with a child and a parent interrupts, the consultation is likely to revert to an adult–adult dyad. The adults dominate and control these consultations.
Limitations of the review
The studies included in this review are a very disparate collection in terms of research questions posed, results, and methodological rigour. This limits the ability to synthesise the results. However the wide diversity of these studies builds a broad picture of these consultations
Triadic consultation
The paediatric consultation is triadic. Three-way consultations are more complex for a doctor to conduct than when the consultation is a dyad. If a triadic consultation involves only adults, the relationship of the two parties visiting the doctor may not be immediately apparent and the doctor has to utilise their consultation skills to elucidate the situation, and is likely to talk directly with the patient. This is not the case in paediatric consultations, where a parent speaking for the child is the norm.23,25
The needs of the parent can take priority. This is illustrated in a US series of qualitative analyses of a doctor examining a child in the presence of the child's mother. The doctor deals sensitively with the needs of the parent while having to assess the child. The flow of the doctor's examination of the child is repeatedly interrupted to address the mother's worries, with the mother's anxieties taking precedence, over the child's issues.27,28
If a consultation was occurring for the parent's benefit, where the parent's agenda was being played out using the child's illness, the doctor would have a duty to the child to ensure he or she is being properly treated.
It has been suggested that some doctors elect to communicate with the parent, as it is only through the parent and/or carer that they can really treat an ill child.11 For example, a child may not be able to get to the doctor's surgery without her parent, or be able to access medication. Concordance in a paediatric situation involves both the child patient and their parent.6
Different levels of cognitive and emotional abilities will affect how much a child is involved in the communication process in their consultation, as will the topic under discussion. It can be presumed that not all children are going to want to talk directly with the doctor, and such a wish should be respected.2
Training implications
Tates et al demonstrated that a parent normally acts for the child in these consultations.23,25 It was also found that doctors tended to accommodate for the child's age more than the parents did.21,23 As a result of these observations, the suggestion was made that the doctor could actively provide clarity to the child and adult of the desirability of child participation in an age appropriate way. Eminson et al developed a teaching package which involves a series of simulated triadic consultations, guiding the learner on how such consultations could take place based on the recommendation of Tates and colleagues.22
Encounters with children make up a substantial part of general practice workload, yet the available literature on the involvement of children aged 6–12 years in their primary care consultation indicates that they play only a minor role in the communication process. The majority of dialogue occurs between the adult carer and the doctor.
Supplementary Material
Acknowledgments
We would like to thank Dr M Eminson at the Royal Bolton Hospital for reading and commenting on earlier versions of this paper
Supplementary information
Additional information accompanies this article at http://www.rcgp.org.uk/bjgp-suppinfo
Funding body
Not applicable
Competing interests
The authors have stated that there are none
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Alderson P, Montgomery J. Health care choices, making decisions with children. London: Institute for Public Policy Research; 1996. [Google Scholar]
- 2.BMA (British Medical Association) Consent, rights and choices in health care for children and young people. London: British Medical Journal books; 2000. [Google Scholar]
- 3.Department of Health. National Service Framework for children, young people and Maternity Services. London: Crown Copyright; 2004. [DOI] [PubMed] [Google Scholar]
- 4.Borland M, Laybourn A, Hill M, Brown J. Middle childhood. London: Jessica Kingsley; 1998. [Google Scholar]
- 5.Lewis C, Rachelefsky G, Lewis M, et al. Randomized trial of A.C.T. (Asthma Care Training) for kids. Pediatrics. 1984;74:478–86. [PubMed] [Google Scholar]
- 6.Sanz E. Concordance and children's use of medicine. BMJ. 2003;327:858–860. doi: 10.1136/bmj.327.7419.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boylan P. Children's voices project, feedback from children and young people about their experience and expectations of health care. England and Wales, Commission for Health Improvement: National Health Service; 2004. [Google Scholar]
- 8.Dimond B. Legal aspects of consent 8: children under the age of 16 years. Br J Nurs. 2001;10:797–799. doi: 10.12968/bjon.2001.10.12.5306. [DOI] [PubMed] [Google Scholar]
- 9.Eminson M, Coup W. GPs communication with children and adolescents. Context: the magazine for family therapy and systematic practice; thinking families. 2000;50:3. [Google Scholar]
- 10.Korsch B, Gozzi E, Francis V. Gaps in doctor–patient communication. Pediatrics. 1968;42:855–870. [PubMed] [Google Scholar]
- 11.Strong P. The ceremonial order of the clinic. London: Routledge and Kegan Paul; 1979. [Google Scholar]
- 12.Gabe J, Olumide G, Bury M. ‘It takes three to tango’: a framework for understanding patient partnership in paediatric clinics. Soc Sci Med. 2004;59:1071–1079. doi: 10.1016/j.socscimed.2003.09.035. [DOI] [PubMed] [Google Scholar]
- 13.Crossley J, Eiser C, Davies H. Children and their parents assessing the doctor–patient interaction: a rating system for doctors' communication skills. Med Educ. 2005;39:820–828. doi: 10.1111/j.1365-2929.2005.02230.x. [DOI] [PubMed] [Google Scholar]
- 14.Kurtz S, Silverman J, Draper J. The ‘why’: a rationale for communication skills teaching and learning in: teaching and learning communication skills in medicine. Oxford: Radcliffe Publishing; 2005. [Google Scholar]
- 15.Howells R, Davies H, Silverman J. Teaching and learning consultation skills for paediatric practice. Arch Dis Child. 2006;91:367–370. doi: 10.1136/adc.2005.073775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marino R, Kohen D. The power of words: communicating effectively with young patients. J Am Osteopath Assoc. 1996;96:410. [PubMed] [Google Scholar]
- 17.Lask B. Talking with children. Br J Hosp Med. 1992;47:688–690. [PubMed] [Google Scholar]
- 18.Cahill P, Papageorgiou A. A video analysis of the communication in paediatric consultations in primary care. Br J Gen Pract. 2007;57:866–871. doi: 10.3399/096016407782317838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pantell R, Stewart T, Dias J, et al. Physicians communication with children and parents. Pediatrics. 1982;70:396–402. [PubMed] [Google Scholar]
- 20.Meeuwesen L, Kaptein M. Changing interaction in doctor–parent–child communication. Psychol Health. 1996;11:787–795. [Google Scholar]
- 21.Tates K, Meeuwesen L. ‘Let Mum have her say’: turn taking in doctor–parent–child communication’. Patient Educ Counsel. 2000:151–162. doi: 10.1016/s0738-3991(99)00075-0. [DOI] [PubMed] [Google Scholar]
- 22.Eminson D. Children's consultations in primary care: teaching package development. 2001 The Research Findings Register Summary number 598 http://www.ReFeR.nhs.uk/ViewRecord.asp?ID=598 (accessed 10 Oct 2007)
- 23.Tates K, Meeuwesen L, Elber E, Bensing J. ‘I've come for his throat’: roles and identities in doctor–parent–child communication. Child Care Health Dev. 2002;28:109–116. doi: 10.1046/j.1365-2214.2002.00248.x. [DOI] [PubMed] [Google Scholar]
- 24.Tates K, Meeuwesen L, Bensing J, Elber E. Joking or decision making? affective and instrumental behaviour in doctor–patient parent communication. Psychol Health. 2002;17:281–295. [Google Scholar]
- 25.Tates K, Elber Ed, Meeuwesen L, Bensing J. Doctor–parent–child relationship: a ‘pas de trios’. Patient Educ Counsel. 2002;48:5–14. doi: 10.1016/s0738-3991(02)00093-9. [DOI] [PubMed] [Google Scholar]
- 26.Freemon B, Negrete V, Davies M, Korsch B. Gaps in doctor–patient communication: doctor–patient interaction analysis. Pediatric Research. 1971;5:298–311. [Google Scholar]
- 27.Tannen D, Wallat C. Doctor–mother–child communication: linguistic analysis of a pediatric interaction. In: Fisher S, Todd AD, editors. The social organisation of doctor–patient communication. Washington DC: Centre for Applied Linguistics; 1983. pp. 203–219. [Google Scholar]
- 28.Tannen D, Wallet C. Interactive frames and knowledge schemas in interaction: examples from a medical examination/interview. Social Psychology Quarterly. 1987;50:205–216. [Google Scholar]
- 29.Aronsson K, Rundstrôm B. Child discourse and parental control in pediatric consultations. Text. 1988;8:159–189. [Google Scholar]
- 30.Aronsson K, Rundstrôm B. Cats, dogs and sweets in the clinical negotiation of reality: on politeness and coherence in pediatric discourse. Language in Society. 1989;18:483–504. [Google Scholar]
- 31.Van Dulmen A. Children's contribution to pediatric outpatient encounters. Pediatrics. 1998;102:563–568. doi: 10.1542/peds.102.3.563. [DOI] [PubMed] [Google Scholar]
- 32.Tates K, Meeuwesen L. Doctor–parent–child communication. A (re) view of the literature. Soc Sci Med. 2001;52:839–851. doi: 10.1016/s0277-9536(00)00193-3. [DOI] [PubMed] [Google Scholar]
- 33.Runeson I, Enskar K, Elander G, Hermerén G. Professional's perception of children's participation in decision making in health care. J Clin Nurs. 2001;10:70–78. doi: 10.1046/j.1365-2702.2001.00433.x. [DOI] [PubMed] [Google Scholar]
- 34.Stivers T. Negotiating who presents the problem: next speaker selection in pediatric encounters. J Commun. 2001;51:252–282. [Google Scholar]
- 35.Young B, Dixon-Woods M, Windridge K, Heney D. Managing communication with young people who have a potentially life threatening chronic illness: qualitative study of patients and parents. BMJ. 2003;326:305. doi: 10.1136/bmj.326.7384.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wassmer E, Minnaar G, Abdel Aal N, et al. How do paediatricians communicate with children and parents? Acta Paeditricia. 2004;93:1501–1506. doi: 10.1080/08035250410015079. [DOI] [PubMed] [Google Scholar]
- 37.Van Dulman S. Pediatrician–parent–child communication: problem-related or not? Patient Educ Counsel. 2004;56:61–68. doi: 10.1016/s0738-3991(02)00250-1. [DOI] [PubMed] [Google Scholar]
- 38.Nova C, Vegni E, Moja E. The physician–patient–parent communication: a qualitative perspective on the child's contribution. Patient Educ Counsel. 2005;58:327–333. doi: 10.1016/j.pec.2005.02.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.