Abstract
Drawing upon the broader health, social, and political geography literature this paper outlines a framework for considering place-based processes through which syringe exchange availability may be understood. It is argued that the geographic distribution of syringe exchange programs (SEPs) in the United States is linked to the social and political conditions of particular localities through three place characteristics: (1) structural constraints; (2) social and spatial distancing of injection drug users; and (3) localized action. Although SEPs remain a controversial issue and face ongoing obstacles from the government, law enforcement and local communities, they continue to operate through the efforts of grassroots organizations and local activists. Action on this issue occurs locally, and the characteristics of place-based factors will affect whether particular areas adopt SEPs.
Keywords: syringe exchange programs, place, activism, injection drug use, HIV and hepatitis C prevention
Introduction
Injection drug use (IDU) has many public health implications, notably its role as a risk factor for infectious diseases such as HIV/AIDS, hepatitis B and C, and endocarditis, (Novick et al., 1997) and, increasingly the co-infection of HIV/AIDS and hepatitis C (Hagan et al., 2005). Preventing the spread of blood-borne pathogens through IDU requires a diversity of approaches, including treatment and detoxification programs, social services, primary health care, outreach, user involvement, and access to sterile syringes and injection equipment for people who are injecting (Brooner et al., 1998; Paone et al., 1999; Strathdee et al., 1999). In many parts of the world, syringe exchange programs (SEPs) have been adopted as a critical component of HIV and hepatitis C prevention for IDU. Injectors of heroin and other drugs have ready legal access to sterile syringes throughout much of Western Europe and Australia, as well as in many developing countries (e.g., Brazil and Nepal). In many of these countries, pharmacies sell syringes over the counter, and municipalities or other public bodies run SEPs. In contrast, the United States (U.S.) public health response to blood-borne infections among IDUs has been minimal and geographically uneven (Tempalski, 2005). In most parts of the U.S. legal access to syringes either through pharmacy sales or SEPs remains difficult, and is illegal is many places. Further, since 1998 the federal government has denied funding for SEPs. Understanding the geographic dimensions of SEPs is critically important because these programs have been shown to reduce transmission of HIV and, increasingly, hepatitis B and C, as well as to provide important medical and social services to IDUs (Hurley et al., 1997; MacDonald et al., 2003).
Although SEPs remain controversial and face ongoing obstacles from government and local communities and businesses, they continue to operate and expand through the efforts of grassroots organizations and local activists. Drawing on the broader public health and social and political geography literature, this paper outlines the effects of place characteristics through which geographic variation in SEP availability may be understood. It is hypothesized that the uneven geography of SEPs in the U.S. involves political, socioeconomic, and organizational characteristics of localities that affect service needs, resources, opposition, and localized action.
Place is understood in geography as space endowed with meaning(s) (Cooper et al, 2004; Cresswell, 2004; Kearns and Joseph, 1993), an idea that recognizes that society and space are mutually constituted (Massey, 1997; Soja, 1980; 1997). Central to this concept is that past and present interactions of social, political, and economic systems give shape to space, and that simultaneously, space configures social relations (Kearns and Joseph, 1993; Sibley, 1995). Geographers have been concerned with the role of power embedded in this configuration process, and the interactions between power and sites of resistance and opposition, and human agency (Castells, 1983; Pile, 1997; Smith, 1994). Castells argues that “resistance takes place as a result of demands around three basic structural issues: (1) collective consumption, such as housing, schools, welfare provision and so on; (2) the defense or expression of cultural identities; and (3) the working of the state and/or local government” (taken from Pile, 1997, pp. 9). Thus, economy, culture, and state must be accounted for in the geographical analysis of place.
The points at which power and resistance intersect are areas that shape and give rise to collective action (Martin and Miller, 2003). As Castells argues, Martin (2003) also suggests that resources have been a key to motivating action; this is most evident in the struggle over quality of life issues and the desire of identity groups to be acknowledged within the broader culture. Geographers thus argue that place provides an important mobilizing discourse and identity for collective action (Marston, 2003; Martin, 2003; Miller, 2000). People and groups organized into coalitions actively shape places, and the actions, driven by institutional structures, are never the same from place to place. Thus, people and institutions actively shape place, and simultaneously, place influences the structure of how resources are distributed to individuals and groups (Dear, 1988; Harvey, 1997; Johnston, 1991; Kearns and Joseph, 1993).
Examining the efforts to institute SEP in three U.S. metropolitan areas gives insight into how these forces configure grassroots and institutional response. Bluthenthal (1998) describes an example of collective action to establish SEPs, arguing that government inaction created the political opportunity structure that encouraged harm reduction activists in Oakland, California and elsewhere to set up SEPs. In other situations, strong support by local individuals can lead to wide support for SEPs, as the Tacoma case illustrates. The first publicly-funded SEP in the U.S., in Tacoma, Washington, resulted from the actions of Dave Purchase and others. Recognizing that many IDUs were dying of AIDS and lack of government response, Purchase set up a street-based SEP. Purchase's efforts strongly influenced local program adoption which led to the first publicly funded street-based SEP in the United States.
Yet, in other places, local direct action has been less successful. Attempts to set up SEPs in New Jersey point out political processes producing disconnects between need and services. Injection drug use is the most frequently reported risk behavior among HIV-positive individuals in New Jersey. In 2000, New Jersey reported over 19,000 cumulative IDU-related AIDS cases, and 2.3% of the Jersey City metropolitan area population was injecting drugs (State of New Jersey Department of Health and Senior Services (NJDHSS), 2002). However, the governor and city officials opposed distributing sterile syringes to IDUs, and they used arrests to suppress the state's only publicly visible SEP.
These examples from three places demonstrate different response to the HIV epidemic among IDUs. They illustrate varying philosophies and resource responses within each distinct place. Each one's social, economic and political context has shaped the general characteristics of place, and in turn, given shape and meaning to IDUs' health and access to HIV prevention services.
Thus, in this article, the concept of place allows us to engage the set of social and political relationships that create a spatial context in which differential responses to injection drug use–related HIV are structured. As such, this paper offers a context for understanding how place-specific processes—including need for services, local resources, opposition, and grassroots political action—affect the geographic distribution of SEPs in the United States. In this research, it is argued that the geographic distribution of SEPs in the United States is linked to the social and political conditions of particular localities through three place characteristics: (1) structural constraints, as they relate to disease vulnerability and service needs; (2) social and spatial distancing of IDUs and associated services; and (3) localized action concerning disease prevention and health service provision for stigmatized groups. These place-based processes are interrelated: the need for services may lead to activism, which can reduce stigma and ultimately lead to service provision.
This research directly and primarily contributes to geographic knowledge on HIV/AIDS prevention as it relates to health care needs, services, and activism. It also contributes to the broader literature that emphasizes how place-based political, social, and economic processes—such as local economic relations and inequalities, community responses, and grassroots activism—affect the geographies of health care services for people with HIV/AIDS and other stigmatized groups. Thus, this research improves our understanding of the geography of HIV/AIDS prevention services in the hidden and highly stigmatized population of IDUs.
This article expands our knowledge of how place-based political and social processes have led to variations in HIV/AIDS prevention-related services for IDUs, specifically SEPs. At the national level, the U.S. federal government's systematic denial of SEP funding influences the social and political environment of all U.S. localities under consideration. The conceptual framework discussed here shows how the lack of an association between the need for a program and the presence of a program implies that current U.S. political systems are not responding adequately to the important public health problem of infection-related disease. Response to this situation is a matter of local grassroots action, and the characteristics of place-based social and political processes will affect whether particular areas confront this and adopt an intervention.
Activism and Politics: Syringe Exchange Development in the U.S.
Whether the U.S. federal government should support the distribution of sterile syringes for injection drug use has been a highly controversial topic in the public policy discourse. In 1988, the U.S. Congress barred federal funding for SEPs, with the proviso that the ban could be lifted by the Surgeon General if he or she determined that such efforts could reduce the risk of HIV infection without encouraging illicit drug use. In 1997 an independent consensus panel convened by the National Institutes of Health concluded that SEPs reduce the spread of injection-related HIV and do not encourage illicit drug use (U.S. General Accounting Office, 1993). Moreover, at least 20 medical, scientific, and other professional associations have endorsed syringe exchange as an effective prevention strategy (Vlahov et al., 2001). Nonetheless, federal funding continues to be withheld.
In contrast, in many parts of the world, SEPs have been accepted as essential components of HIV prevention and other blood-borne diseases. The first SEP was developed in Amsterdam in 1983 as a method of reducing transmission of hepatitis B, another common blood-borne infection among IDUs. After the discovery of HIV infection among IDUs in Amsterdam, the exchange program was expanded and SEPs were implemented in other Dutch cities (Grund et al., 1991). Presently, throughout much of Europe, Australia, Canada, and New Zealand, users of heroin and other injection drugs have ready legal access to sterile syringes.
While syringe exchange was clearly taking on a public health role across European cities, it would remain only a radical idea in the United States for at least another two years. Then, beginning in November 1986, Jon Parker, a recovering IDU and student at Yale University School of Public Health, formed a group called the National AIDS Brigade and started the first underground needle exchange program1, distributing and exchanging needles on the streets of New Haven, Connecticut. By the late 1980's, needle exchange programs were operating in over a dozen cities – often in the face of harassment, arrests, and threats of violence. Some programs eventually came to operate with the support of local health authorities using public funds (e.g., Tacoma and New Haven). Other programs were supported and funded through private and charity funds and operated under the consent of the local authorities, as in San Francisco, California; Boulder, Colorado; and Portland, Oregon. Finally, other programs operated under the radar screen of local law enforcement and without official authorization.
By the year 2000, approximately 154 syringe exchange programs were operating in the United States (Beth Israel Medical Center, 2000). Figure 12 depicts the spatial distribution of SEPs across the largest 96 metropolitan statistical areas in the United States; high geographic clustering of programs is located in the northeast and northwestern and western regions; while the south and mid-western regions remain low in initiating SEPs.
Figure 1. Geographic Distribution of Syringe Exchange Programs in the US in 2000**.
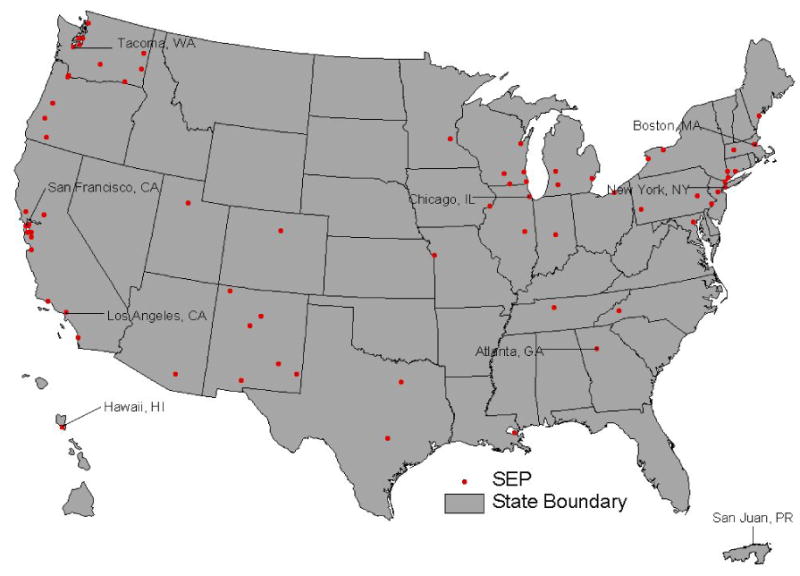
Source: 2000 National Survey of Syringe Exchange Programs from Beth Israel Medical Center, NY, NY.
**Only those SEPs that allowed data release are displayed on map.
Despite their proven effectiveness in HIV prevention and despite support from local public health authorities and research institutions, SEPs remain a controversial issue in the United States. They face ongoing obstacles in the form of legal challenges, funding constraints, disapproving attitudes of local residents or business associations, and police harassment of clients and service providers. In the absence of federal support for SEPs, responsibility for implementing this public health measure has fallen to state and local government entities; yet most state and local officials have been reluctant to authorize such programs, and public funding and regulation of syringe acquisition vary by state and locality. Additionally, in many states and localities, the acquisition and exchange of syringes are restricted under prescription and drug paraphernalia laws. Despite this variation, existing SEPs continue to expand and in some areas new programs are beginning; commonly this work is by citizens establishing “facts on the ground” and simply setting up SEPs on their own initiative. More than half the SEPs in the United States are run by nongovernmental organizations and were initiated by activists and local community members (Tempalski et al., 2003a; 2003b).
In the United States, the development and maintenance of services for IDUs—specifically, SEPs—have been linked to social movements (e.g., the harm reduction movement) and specific activist groups (e.g., AIDS Coalition to Unleash Power (ACT UP)). For example, in New York City and nearly half a dozen cities along the northeast corridor in 1989, the National AIDS Brigade and ACT UP established underground SEPs distributing 200,000–300,000 needles annually – members were regularly arrested for these acts of civil disobedience (Drucker, 1990).
These harm reduction efforts are built on the work of many other movements. In particular, ACT UP which used “direct political action” to successfully contest the stigmatization of people with AIDS by highlighting the underlying stigma rooted in homophobia. Many of the same players (i.e., harm reduction advocacy) then adopted a similar philosophy and used similar tactics to create and demand “direct HIV prevention services” for IDUs. Thus, many SEPs were started by AIDS activists from political groups motivated to challenge the treatment and marginalization of IDUs. Harm reduction advocates view the problems of illicit drug use and addiction as arising primarily from drug policies criminalizing the user, and they work toward minimizing the medical and social consequences of drug use. The harm reduction philosophy fosters alternative models to conventional health and human services, as well as drug treatment, while challenging traditional client–provider relationships.
Previous research has shown that political factors and local direct action may substantially influence SEP creation and sustainment (Tempalski et al., 2003b). Using the interpretive framework outlined in this paper, study results indicate that SEP formation, at least in the United States, is based not on relative need across localities, but on social and political factors—including active solidarity (ACT UP) and potential solidarity (large numbers of men who have sex with men (MSM) creating greater concern for HIV/AIDS issues)—that may help to form, defend, and possibly sustain SEPs. Hence, AIDS activism supported the harm reduction movement, and local efforts of groups such as ACT UP fostered the harm reduction philosophy and the U.S. expansion of SEPs.
The Relevance of Structural Constraints in IDU-related HIV Vulnerability
Research suggests that health differences across social class and population can be influenced by the social, economic, and political contexts of people's lives (Farmer, 1999; Krieger, 2001; Wallace and Wallace, 1998). For low income or “marginalized” populations, whose lives are narrowly circumscribed by inadequate resources and power, context has critically important effects on health. Prior research documents that social and economic conditions are related to a variety of health and social indicators although the directions of some relationships vary among studies. Ruhm (2000) found that economic good times are associated with worse physical health and with increases in alcohol consumption, though perhaps with better mental health. In a meta-analysis of studies during the 1980s and 1990s, Jin et al. (1997) found that higher unemployment rates are related to higher overall mortality, cardiovascular-related mortality, and suicide.
Thus, Krieger (2001) argues that the production and distribution of disease must be understood through constructs of social and economic relations characterized by inequalities and embedded in the larger social, economic, and political structures. She identifies two possible mechanisms of disease vulnerability. First, resources and harms are distributed along the lines of social and economic relations. Second, these relations condition behavior through factors such as relative and absolute deprivation.
The extent of relative deprivation within a society largely determines the degree of harm across particular groups. For example, spatial de-concentration of urban minority communities in New York City (caused by neglect and “planned shrinkage” policies spurred by white governmental fear of urban black revolution) fueled the reemergence of tuberculosis in the 1980's. Deteriorating living conditions, social decay, and reduced fire-fighting capacity contributed to an increased number of fires; the resultant destruction of housing stock dispersed South Bronx communities—and, consequently, multidrug-resistant tuberculosis and AIDS spread within and to adjacent neighborhoods (Wallace et al., 1997).
Although the U.S. HIV/AIDS epidemic has historically affected two groups—MSM and IDUs— in recent years the broadening impact of the epidemic across classes, races, genders, and sexual orientations indicates a growing need for a variety of educational, prevention and treatment services. Resources availability, for example, can vary greatly affecting where and when prevention and treatment services can be implemented. In seeking to understand the factors that shape the HIV/AIDS epidemic among IDUs, and ways in which societies and communities have responded to it, a growing body of research has focused on structural factors that facilitate HIV transmission and its concentration with particular geographic areas and populations (Farmer, 1999; Singer, 1998; Sumartojo, 2000; Taussig et al., 2000). Structural constraints are defined here as social, economic and political environments that shape and constrain individual, community, and societal health outcomes.
Previous research suggests HIV prevalence or incidence among IDUs in a locality is a function of policies about purchasing syringes (Friedman et al, 2001; 2000), syringe exchange (Des Jarlais et al, 1996; Hurley, 1997; MacDonald et al., 2003) urban development (Friedman et al., 1999) or urban “desertification” (Wallace and Wallace, 1998), and indicate that these policies might be altered to reduce HIV transmission. Structural constraints relating to syringe acquisition, which differ by state and locality, can significantly reduce the ability of IDUs to purchase and possess sterile syringes. State and local laws concerning the sale, distribution, and possession of syringes can prohibit any distribution of syringes. Policy processes and regulations governing syringe sales at the state and local levels (e.g., prescription and drug paraphernalia laws) influence the legality of syringe access, the conditions of syringe distribution, and the use of government funds to distribute syringes.
Taussig et al. (2000) look at the legal and regulatory barriers that restrict pharmacy sales of syringes to IDUs and discuss how reducing these barriers can facilitate access to sterile syringes for IDUs and reduce ones' vulnerability to HIV infection. Currently, fourteen states have prescription provisions3 (Burris, 2005), and twelve states4 and the District of Columbia have affirmatively authorized SEPs (Burris, 2002). Additionally, Friedman et al., (2001) research showed that restricting syringe access were associated with HIV transmission. The study indicated that MSAs with anti-over-the-counter-syringe laws had a higher mean HIV prevalence among IDUs than other MSAs (13.8% vs. 6.7%).
Economic and political variables may influence HIV rates among IDUs, and the degree of IDU stigmatization in a locality may be positively associated with HIV transmission. In the case of IDUs, metropolitan-level economic trends affect both their presence and HIV status. Friedman et al. (2004a) found the percent of the population in poverty was positively associated with the population density of injection drug use, HIV prevalence among IDUs, change in HIV prevalence among IDUs, and both black/White and Hispanic/White disparities in IDU population density. Additional research by Friedman et al. (2004b) showed increases in both unemployment and poverty rates between 1990 and 2000 were associated with a higher population density of IDUs in 1998.
The broader sociopolitical system of municipal governance can affect individual IDU behavior. For example, policing patterns and arrests can affect drug users' access to services, even in states where syringe access is legal. Cooper et al. (2005) found that particular drug-crackdown tactics by police affected IDUs' ability to safely inject. Drug-related arrests were also found to affect IDUs' use of health and treatment services. Research by Bluthenthal et al. (1997) determined that program participation declined following arrests of staff at illegal SEPs. Furthermore, Bluthenthal et al. (1999a) found that IDUs who feared arrest are at least twice as likely as other IDUs to borrow syringes and other injection equipment, perhaps because they hesitate to carry syringes. Bourgois et al. (1997) also found that impoverished or minority IDUs were especially fearful of arrest and therefore particularly reluctant to carry syringes increasing the risk of sharing injection equipment.
The mounting evidence of social and political structuring of race, class, gender and sexuality indicates the need for a variety of approaches to developing services and service provision strategies. Des Jarlais et al. (1995) work in five cities where both low HIV prevalence and incidence remained low among IDUs over a minimum of six years suggest three factors contributed to “public health control” over HIV transmission among IDUs: (1) beginning prevention efforts when prevalence was still low; (2) using community outreach to establish trusted communication between health workers and drug users; and (3) providing a ready supply of sterile injection equipment.
However, the design and implementation of HIV prevention strategies to meet the needs of IDUs—such as SEPs or methadone maintenance programs—face challenges to acceptability and feasibility at the local level. For example, while local residents may recognize the pervasiveness of drug use in their community, they may not welcome services for users into their neighborhood (Dear et al., 1997; Wilton, 2000). The reluctance to allow such services is partly attributable to local views of drug users and their behavior as deviant (Daker-White, 1997; Takahashi, 1998). This perception raises important questions relating to the marginalization and exclusion of populations based on gender, sexual orientation, race, and class. These social and political processes rooted in place result in a non-distribution of resources and goods to those in society with the greatest need[s] (e.g., mentally ill, homeless, or HIV-infected persons, prevention and treatment services for IDUs) and thus, largely determine the location of services.
Social and Spatial Distancing of IDUs: Implications for HIV Prevention Services for IDUs in the United States
To explain resistance to the provision of human service facilities social scientists turn to theories of social distancing embedded in concepts of difference: social distancing fuels the stigmatization of individuals, groups and places. Conceptualizations based on difference are rooted in moral beliefs closely related to local cultures; this is, the sense of one's moral responsibility for others decays as one becomes increasingly distanced from others (Smith, 1994). The social and moral distance created by such stigma can carry over to the location and establishment of many programs for services-dependent groups, including HIV-prevention services for IDUs. Syringe exchange programs, for example, can be difficult to establish even in communities hard-hit by injection drug use–related HIV transmission.
Stigma regarding drug use and HIV/AIDS involves not only the devalued individuals and groups but also the locations where such persons receive services; thus, the stigma is extended from person to place. According to Takahashi (1998), the built environment reflect the constructed stigma in society, resulting in a stigmatized landscape in which public and community spaces are viewed as less productive, more dangerous, and less desirable. Within this context, human services facilities can reinforce stigma, because the stigma of places is conditioned partly by the built environment and the types of services provided and clients served. Thus, Takahashi's (1998) research suggests these place-based factors maintain and enforce community boundary definitions, reinforcing current spatial relations of stigma.
During the HIV/AIDS epidemic of the 1980s and 1990s, changing epidemiological patterns and the effects of stigma varied among diverse populations (Farmer, 1992). Although some aspects of this stigma are shared by all HIV-infected persons, others are population-specific. Discrimination against persons with AIDS drew from and compounded preexisting stigmas (especially vis-à-vis MSM and IDUs). As a result, negative attitudes towards drug use enable the institutionalization of prejudices against drug users (Friedman, 1998), and people who have acquired HIV by injecting drugs are doubly stigmatized—for being HIV-positive and for being an “addict.”
Stigmatization associated with drug use and HIV/AIDS extends beyond the devaluation or punishment of individuals and groups and often becomes embodied in the location of services used and frequented by clients. This transfers stigma from persons to services and often the places where those services are located. In the United States, this transfer of stigma often embroils harm reduction focused services such as SEPs and can be embodied in community attitudes, law enforcement, and political opposition within various levels of the government (Tempalski, 2005).
The most powerful opposition to establishing SEPs in the United States has come from government authorities or law-enforcement representatives (e.g., district attorneys, police, and politicians) and community leaders (e.g., clergy and business association members). In fact, when these influential groups support SEPs, local resistance to SEPs is greatly weakened. However, the processes that lead to the establishment of SEPs are complex and reflect the social and historical circumstances in each place-based context. In some cases, SEP support was brought on by the direct actions of influential local individuals. For example5, the establishment of an SEP in Tacoma, Washington resulted from the direct action of a local activist, Dave Purchase, and others. After recognizing that many IDUs were dying of AIDS and that the government was doing nothing to help, Purchase set up a SEP in Tacoma in 1988. Purchase describes the situation in this way:
People were going to die. I had some time on my hands. I had some friends that did help out a lot and never got the credit they deserve. We started in the summer of '88 and every couple of years there's another brouhaha with the same old argument. The fact of the matter is that there have been enough local political people with backbone that have supported us and so has the health department, and so we've weathered attacks. And politics is still a number one problem. AIDS is all politics, it's not science and stuff like that, its all politics (Purchase, 2003).
Purchase's efforts in the late 1980s brought about political support in favor of SEPs and government funding for programs early on in the epidemic. Both are clearly very important for program adoption and sustainability and, in turn, for keeping HIV prevalence low. Efforts of political advocacy groups like ACT UP were just beginning to develop at the time Purchase was working toward gaining local support for a SEP. Thus, his efforts strongly influenced program adoption in Tacoma and led to the first publicly funded street-based SEP in the United States.
In another city, a pro-SEP client believed that the city council's view on syringe exchange was influenced by a very organized community group who managed to vote in city council members who believed that drug use was morally wrong and would oppose syringe exchange to maintain there consituents' support. He had this to say about the locate opposition in his city:
The Council members are saying it sends the wrong message: one person understands it and sees the health benefits but still feels it sends the wrong message to children, another person is adamantly opposed to anything like that and says all addicts should go into treatment and he actually prefers religiously-based treatment (we didn't even try talking to him he's just so outrageous), the Mayor feels it's a law enforcement issue and therefore you shouldn't declare a state of emergency to support an illegal activity and they can go into recovery and force recovery in the jail system…
Additionally, a different respondent in this city had this to say about trying to get SEP legalized in that city:
So we are trying to override that [city council vote] because you have basically politicians who are embedded in their conservative morality and that morality is driving politics not public interest or healthcare. So it's pretty scary.
Some AIDS advocacy groups and public health researchers argue that the conservative views of a local community, backed by a Republican majority in local government, can knock down any initiative to establish a legal SEP. In explaining why a SEP did not exist in his city, one local activist described the political environment in the following terms:
The majority of the city is run by the Republicans, and [the local law enforcement] are ultra-conservative… they can go wherever they want, whenever they want, and clean up what they wish. They make a show of cleaning up prostitutes…
Additionally, a shift in political leadership and SEP support/opposition are not uncommon. In this particular scenario the state legislators who had originally approved syringe exchange were replaced with new officials who did not sympathize with the SEP and turned against it. An SEP supporter described the situation in this way:
The police were educated about it [syringe exchange] and were very cooperative. This has changed within the last two years, when we've come under public attack and have had more problems with the police…. It's a nightmare. There are new legislators, new cops, everything's changed…. Now there are letters being written against us, we're in the papers and on TV and it's turned into this huge controversy.
Further opposition can result from on-going police harassment of service providers or difficult relations between police and programs stemming from the illegality of drug use and of distributing drug paraphernalia, such as syringes. A local harm reduction worker regarded law enforcement issues relating to drug paraphernalia laws as the biggest obstacle to trying to establish an SEP there:
There were attempts to set up a public program early on, about 8–10 years ago, but the police would not permit it. No one has made an attempt to do anything publicly in the last five years. It is not illegal to set up a syringe exchange, but it is illegal to carry drug paraphernalia. The police arrested everyone who tried to set up programs.
One SEP worker provided an example of police harassment of SEP employees and clients based the current state and local syringe law in that city:
If you work for it (the SEP) they arrest you. There's that kind of harassment. There are people being arrested all the time for possession of syringes. Even if they have a card…They can show a card and they're told that's no good here. I don't know of any workers going to jail, but I know participants have gone to jail for possession of syringes.
Repressive policies that influence local social and political environments can make program implementation very difficult. Institutional repression based on political policies such as the declaration of “war on drugs,” reinforced by local law enforcement policies, may prevent SEPs from being established. Still other forms of opposition lie in police harassment of service providers and clients, or difficult relations between police and programs created by state drug paraphernalia laws, for distributing or carrying syringes (Bluthenthal, 1999b). Thus, local activists often find it easier to implement underground SEPs than to fight difficult institutionalized policies.
In many localities, prejudice attached to drug use is reinforced by the illegal and covert nature of illicit drug use. Included in this prejudice is a negative perception of injection drug users (e.g., they are junkies and criminals) and IDUs with HIV are poor and non-white (Friedman, 1998). Additionally, in some communities, residents view HIV as a natural, acceptable consequence of deviant behavior (Alonzo and Reynolds, 1995), which intensifies the stigma and creates barriers to initiating HIV prevention services for IDUs. In this case, it is not a negative experience with syringe exchange that leads to opposition to these services, but the overall moral judgment that drug users are evil. For persons holding this view, opposition to SEPs results from an overall equation of HIV with immorality, more so than any personal experience with syringe exchanges. Thus, resistance to SEPs may arise even in the absence of adverse events, and such stigma-based resistance remains strong and likely to reoccur.
Localized Action: The Harm Reduction Movement as Disease Prevention
Public and sociopolitical responses prompted by the HIV/AIDS epidemic surpass previous response to past epidemics. Many factors throughout the epidemic (e.g., the “war on drugs,” characteristics of affected groups, criminalization of drug treatment, and racial fears) have influenced society's response. These elements of the epidemic have demanded new strategies of public health response to meet the needs of those stigmatized by the disease. Marginalization of specific groups and individuals has been countered by social movements in instances where the state is unwilling or unable to stem the widening health disparities due to HIV/AIDS.
Social movements sparked by grassroots activism have often represented the initial response to a health crises and significantly shaped public health policy (Bluthenthal, 1998; Hoffman, 2003; Szreter, 1988) and health service provision (Petchey et al., 1998). The great sanitary movement in late–18th century Britain, for example, was driven chiefly by local activists appalled by the living and working conditions of the urban poor (Porter, 1999). Other social movements and activism, from the feminist health movement to AIDS activism, have restructured health-related issues, including treatment services, health care reform, AIDS policy, and the destigmatization of particular groups (Banzhaf et al., 1992; Barnett and Barnett, 2003; DeMacro and Johnsen, 2003).
In the HIV/AIDS epidemic's first 20 years, numerous confrontational tactics by advocacy groups resulted in major policy changes. A primary goal of the AIDS movement has been the adoption of a multi-faceted strategy by the U.S. public health system. The AIDS movement grew from the result of the marginalization and exclusion of particular groups based on gender, sexual orientation, race, and class; resulting in widespread social and health disparities among these groups. Early in the epidemic, activists sharply criticized the government and drug companies for their complacency about HIV/AIDS. The emergence of political advocacy groups such as ACT UP, which began in 1987 in New York, and then spread to other U.S. cities, is important in lesbian/gay, AIDS, and medical history (Altman, 1994; Stoller, 1998).
Famous for its imaginative street theater, ACT UP, an offshoot from other community-based AIDS organizations, was a magnet for radical young gay men and women. It derived many of its political and cultural practices from a variety of sources as diverse as anarchism, the peace movement, the punk subculture, the feminist health movement, and gay liberation (Epstein, 1996). The success of some local chapters was the result of a natural outgrowth of radical politics (e.g. San Francisco) and/or predominantly gay, white male identity (e.g. New York City) (Epstein, 1997; Stoller, 1998). ACT UP chapters typically had no formal leaders, and in many cities, meetings were consensus based. Thus, direct action tactics of ACT UP chapters were place-specific and highly dependent on local epidemiological needs and local philosophy concerning the epidemic.
ACT UP, and the AIDS movement in general, effected changes in AIDS research, prevention, and treatment methods, ultimately challenging the paternalism of the Western biomedical model forcing traditional medical authorities to respond to “patient power” (Epstein, 1996, p.9), and its attendant demands for structural change and treatment advocacy. These achievements are significant because of their impact on an epidemic that public officials had been underemphasizing, and their influence on direct action tactics for other health concerns (e.g., breast cancer and harm reduction services).
The AIDS movement was successful for three reasons: (1) their approach often involved challenging mainstream medical and/or scientific knowledge and practice; (2) activists typically highlighted the embodied experience of people with the disease contesting current biomedical wisdom that the body is a mere vector of infection; and (3) activists involved in the movement typically engage in collaboration with medical and health researchers and professionals to help expand treatment and prevention, and research and funding.
The emergence and mobilization of advocacy for IDU-related HIV services has been built on the work of many other movements, among them: the medical marijuana movement (McQuie, 2003); community services for persons with HIV/AIDS by the Gay Men's Health Crisis6; ACT UP and others from the feminist health movement. Accordingly, the harm reduction movement and IDUs advocacy groups are built on the foundations of other movements and borrowed from their particular strengths, specifically the direct action philosophy of ACT UP.
The harm reduction movement, in particular, has successfully convinced clients who are generally put off by other kinds of public health approaches to participate in SEPs. It recognizes that abstinence for drug users is difficult to achieve, and views the problems of illicit drug use and addiction as arising primarily from drug policies that criminalize the user, and works toward minimizing the adverse medical and social consequences of drug use (Clear, 2003). Examples of “actions” associated with harm reduction include syringe exchange, supplying clean injection equipment (e.g. bleach kits, cookers, etc.) overdose training prevention, vein care, wound care, and safe injection space(s). Feasibility of implementing SEPs are subject to a variety of local place-based factors, including the presence of grassroots advocacy; in some cases, underground exchange programs; legal aid for activists who are prosecuted; legal action on behalf of programs working with IDUs; public and private funding for programs; the establishment of programs by public authorities and local community support.
Bluthenthal advocates it was government inaction that created the political opportunity structure that encouraged harm reduction activists in Oakland, California and elsewhere to set up SEPs. The development of an SEP in Oakland, Bluthenthal argues, emerged “through the mobilization of elements of impacted communities and their allies” (Bluthenthal 1998, p.1151), rather than any rational or sensible cost effective public health strategy designed by experts. Further advocating, it was the diversity of skills of its volunteers and board members embedded in a political environment that encouraged solidarity for the establishment of an SEP. These specific place-based factors contributed to conditions for the emergence of an activist-oriented SEP in Oakland.
In New Haven, Connecticut it would be another six years after Jon Parker's National AIDS Brigade first distributed and exchanged needles on the streets before an IDU in that city would have legal access to sterile syringes. After three years of lobbying from 1987-90, involving the Mayor's Task Force on AIDS and the New Haven Health Department a law was passed in the spring of 1990 amending state statutes that had made syringe purchase without a prescription illegal to allow legal possession of syringes for participants in a demonstration NEP, which was started in New Haven in November of 1990. The NEP officially opened on November 13, 1992 and has continued to this day. The program has since expanded statewide to include other cities such as Danbury, Bridgeport, and Stamford, and at the same time, made syringe purchases in pharmacies available (Kinzly, 2003).
In New Mexico, syringe exchange began on February 2, 1998. After a seven-year legislative struggle, The Harm Reduction Act of 1997 was passed; the Act made syringe exchange legal to programs approved by the New Mexico Department of Health throughout the state. Support came from both Department of Health and community activists – opposition from legislators has gradually waned over the years (McCague, 2004).
The philosophy of harm reduction, developed in Great Britain and the Netherlands, has fostered a global movement. Domestically, it has spread through a network of researchers, providers, and organizations creating health-oriented change at the local community level. National Harm Reduction Coalitions offer a variety of resources, information, and skills training for outreach workers and advocacy groups to work more effectively with drug users and build safer, healthier communities. The movement is broad based and diverse, ranging from grassroots activists, recovering drug users, AIDS activists, lawyers, substance use–HIV researchers, community health educators and service providers, many of whom volunteer at SEPs and have been arrested repeatedly for distributing syringes; it cuts across the various communities hard-hit by substance-abuse and by the HIV/AIDS epidemic, and includes gays and lesbians, IDUs, and many African-American and Latino communities.
The structuring of place processes for the success of implementing SEPs and other harm reduction services concerns the spatial distribution of local organized action including the efforts of individuals, organizations, and networks. In the United States, it is the combined efforts of local organized action that has led to the design and implementation of place-based HIV prevention programs for IDUs. As such, program design based on need is best determined by those braving the crisis, not by government policies based on fear and exaggeration. Grassroots efforts, such as those of the harm reduction movement, defy institutionalized public policies that serve dominant interests and work toward building solidarity for stigmatized groups. U.S. grassroots activists continue to influence HIV prevention efforts to help reduce injection drug use–related harm. Action associated with HIV prevention efforts occurs locally, which in turn affects whether particular areas adopt the intervention.
Discussion and Conclusion
This research suggests that response to IDU-related HIV is responsive to local characteristics as well as to broader factors. This perspective embraces the notion that interactions of social, political, and economic systems give shape to place (Soja, 1980) and, simultaneously, place configures the structure of how resources and harms are distributed. Despite the proven effectiveness of SEPs in preventing HIV transmission, and support for SEPs from local public health and research institutions, these programs remain controversial and face ongoing governmental opposition, inadequate funding, negative attitudes from local residents and business associations, and police harassment. For IDUs, the broader social and political issues attached to sterile syringe access have largely been viewed as issues relating to inequality, marginalization, discrimination, and drug use–associated stigma. These spatially-situated social and political processes have produced large gaps in basic services to vulnerable populations, particularly services to reduce drug-related harm (Tempalski et al, 2003b). An understanding of how these processes influence the availability of services is important because: (1) SEPs reduce HIV transmission and provide important medical and social services to IDUs, and (2) it may clarify the trajectory of U.S. syringe-exchange policy and the limitations of public health reform.
Structural constraints within a particular place are important in facilitating the establishment and operation of SEPs. Embedded in important political issues like the criminalization of drug use is whether the federal government should fund SEPs. Even if the U.S. federal funding ban were lifted, however, major state and local barriers to syringe access or exchange programs probably would remain in place. Public policies, particularly drug control policies, limit access to sterile syringes and injection equipment. State and local laws and regulations can prevent syringe distribution. The political processes and regulations at the state and local levels governing syringe sales (e.g., prescription and drug paraphernalia laws) determine the legality of syringe access, the conditions of syringe distribution, and the use of government funds to distribute syringes. Consequently, in localities with SEPs, the programs are often hampered by statutes outlawing syringe possession, and, as a result, many SEPs remain underground.
The dynamic of social and spatial distancing of IDUs, which is embedded in concepts of difference, is reflected in opposition to and rejection of service – dependent individuals. The processes of stigmatization based on the social production of difference help explain negative attitudes and prejudice toward specific individuals and groups. Examinations of the origins of stigmatization enhanced our understanding of how differences and exclusions are defined and play out at the local level. Several place characteristics are important in explaining the social and spatial distancing of IDUs, including the perceived “dangerousness” of users, the moral (and legal) transgression constituted by drug use, and the belief that people are to blame for their own predicament.
In many localities, these characteristics shape public opinion and heighten opposition to the presence of SEPs in the community, which, in turn, produces large gaps in basic services. Narratives revealed place-related social and political attitudes toward IDUs that might be important in understanding where SEPs are more likely to be established – in particular the attitude of local law enforcement, the political climate at the time of implementing programs and having exceptional political leadership willing to implement controversial programs.
Currently in the U.S., syringe exchange programs exist even though harm reduction activities distinctly contradict current U.S. drug policies and drug laws, which results in SEP activists and staff being arrested and charged with illegal, criminal activity. Pro-SEP harm reduction activists defend themselves as acting out of moral necessity and as being justified in handing out sterile syringes to avert greater harm. It is these places where power and resistance intersect giving rise to collective action and activism; in the case of SEPs – the harm reduction movement. The harm reduction approach, alternatively, emphasizes the dignity and rights of drug users and aims to limit or reduce the adverse health, social, economic, and legal consequences of drug use. Current harm reduction goals exist to minimize drug-related harms by making sure that users have access to sterile syringes and clean injection equipment through the direct services of SEPs.
Finally, the HIV/AIDS epidemic's impact has put new demands on state bureaucratic institutions, demands that have often been met by government inaction. The social and political complexities of designing new public health strategies around the epidemic gave rise to new social movements. These social movements and grassroots activism have influenced the establishment of health care services and provisions for stigmatized groups. For example, ACT UP has brought about political understanding and awareness of AIDS issues and harm reduction actions, such as the creation and expansion of prevention services, while counteracting discrimination and stigmatization of substance users. In the past, ACT UP's direct action campaigns successfully contested the stigmatization of people with AIDS by highlighting the influence of homophobia on popular conceptions of HIV. Many of the same players adopted a similar philosophy and tactics in creating and demanding primary health care and HIV prevention services for IDUs, starting “direct services” as a form of direct action (and often, civil disobedience). The emergence of the harm reduction movement and of organizations that work toward establishing and sustaining direct services demonstrates how health-related social movements innovate in disease prevention.
Continued place-based research on IDU-related HIV services is essential to identify areas in need. This is partly because locality is an important factor in determining whether an IDU are likely to become infected with HIV and where services for IDUs will be readily available. That is, an IDU living in a metropolitan area with high HIV prevalence (e.g., New York City, Jersey City, Baltimore) is more likely to become infected than one living in a low-prevalence area (e.g., Los Angeles, Tucson, or Dayton); and as such, the social and political characteristics of localities are likely to affect HIV prevalence levels and the types of interventions implemented.
To date, the debate in the United States has been driven not by science or public health concerns but by an ideology that sees drug use as “immoral and evil” and SEPs as abetting this antisocial behavior. This view has persisted in Congress, which has barred SEPs from receiving federal funds since 1988, despite clear evidence showing that these programs slow the spread of disease without creating new addicts. Currently in the U.S., syringe exchange programs exist even though harm reduction activities distinctly contradict current U.S. drug policies, which results in SEP activists and staff being arrested and charged with illegal, criminal activity. This conflict between federal policy and more local public health policies demonstrates why localized action, particularly grassroots action in the form of “direct services” is often the best and only means toward developing HIV prevention efforts and service provision for IDUs.
In this paper, place is seen as a process in which individual efforts by social movement activists and IDUs themselves, together with institutional and structural forces, actively shape the response to and patterns of IDU-related HIV transmission. For health services planners, whether officials or grassroots activists, understanding which place characteristics are related to the presence (and scope) of SEPs can be useful in determining how to facilitate the expansion of SEPs. This understanding of the influence of place-based processes on the development of SEPs and other services for IDUs, may help service providers and advocates overcome structural barriers and capitalize on facilitators to HIV prevention. Further research should follow these attempts to provide information to activists and draw on their experience to contribute to academic and scientific knowledge.
Acknowledgments
The research described in this paper is collaboration between Community Vulnerability and Response to IDU-Related HIV project at the National Development and Research Institutes., Inc. (supported by the National Institute of Drug Abuse grant # R01 DA13336) and National Survey of Syringe Exchange Programs (funded by American Foundation for AIDS Research) at Beth Israel Medical Center. Special thanks to Dr. Samuel R. Friedman and Dr. Don C. Des Jarlais for their support and use of data from the Community Vulnerability and Response project and Beth Israel Survey of Syringe Exchange Programs respectively; Dr. Sara McLafferty for her un-wilting support and intellectual feedback on the theory framework; Marie Keem and Risa Friedman for transcribing the interviews presented here; and Moriah M. McGrath for her editorial suggestions during the writing of this manuscript.
Footnotes
Syringe exchange and needle exchange programs are the same type of program; the terms are used interchangeably throughout the text.
For confidentiality reasons, reporting on the specific names of some cities or programs are prohibited.
California, Connecticut, Florida, Delaware, Illinois, Indiana, Maine, Massachusetts, New Hampshire, Nevada, New Jersey, New York, Pennsylvania, Virginia and Virgin Islands.
California, Connecticut, District of Columbia, Hawaii, Maine, Massachusetts, Maryland, New Hampshire, New Mexico, New York, Rhode Island, Vermont and Washington.
Interviews provided by the Community Vulnerability and Response to IDU-related HIV Project, Survey of Community Experts (funded by the National Institute on Drug Abuse, Grant# R01 DA13336).
GMHC was the first community-based response to the AIDS epidemic in New York City. It also started the world's first AIDS hotline to handle the public's fears and questions about the epidemic.
References
- Alonzo AA, Reynolds NR. Stigma, HIV, and AIDS: An exploration and elaboration of a stigma trajectory. Social Science and Medicine. 1995;41(3):303–315. doi: 10.1016/0277-9536(94)00384-6. [DOI] [PubMed] [Google Scholar]
- Altman D. Power and Community: Organizational and Cultural Responses to AIDS. London: Taylor & Francis Ltd; 1994. [Google Scholar]
- Banzhaf M, Morgan T, Ramspacher K. Reproductive rights and AIDS: The connections. In: Banzhaf M, et al., editors. Women, AIDS, and activism. Boston: South End Press; 1992. pp. 199–209. [Google Scholar]
- Barnett R, Barnett P. If you want to sit on your butts you'll get nothing!: Community activism in response to threats of rural hospital closure in southern New Zealand. Health and Place. 2003;9(2):59–71. doi: 10.1016/s1353-8292(02)00019-9. [DOI] [PubMed] [Google Scholar]
- Beth Israel Medical Center. Beth Israel National Survey of Syringe Exchange Programs. 2000. [Google Scholar]
- Bluthenthal RN. Syringe exchange as a social movement: A case study of harm reduction in Oakland, California. Substance Use and Misuse. 1998;33(5):1147–1171. doi: 10.3109/10826089809062212. [DOI] [PubMed] [Google Scholar]
- Bluthenthal RN, Kral AH, Lorvick J, Watters JK. Impact of law enforcement on syringe exchange programs: a look at Oakland and San Francisco. Medical Anthropology. 1997;18:61–83. doi: 10.1080/01459740.1997.9966150. [DOI] [PubMed] [Google Scholar]
- Bluthenthal RN, Lorvick J, Kral A, Erringer E, Kahn J. Collateral damage in the war on drugs: HIV risk behaviors among injection drug users. International Journal of Drug Policy. 1999a;10:25–38. [Google Scholar]
- Bluthenthal RN, Kral AH, Erringer EA, Edlin BR. Drug paraphernalia laws and injection-related infectious disease risk among drug injectors. Drug Issues. 1999b;22:1–16. [Google Scholar]
- Brooner R, Kidorf M, King V, Bielenson P, Svikis D, Vlahov D. A drug abuse treatment success among needle exchange participants. Public Health Reports. 1998;113(1):130–139. [PMC free article] [PubMed] [Google Scholar]
- Bourgois P, Lettiere M, Quesada J. Social misery and the sanctions of substance abuse: Confronting HIV risk among homeless heroin addicts in San Francisco. Social Problems. 1997;44:155–173. [Google Scholar]
- Burris S. Temple University Beasley School of Law; 2005. James E Beasley Professor of Law. Personal communication. [Google Scholar]
- Burris S, Vernick J, Ditzle A, Strathdee S. The legality of selling or giving syringes to injection drug users. Jones TS, Coffin PO, editors. Preventing blood-borne infections through pharmacy syringe sales and safe community syringe disposal. Journal of the American Pharmaceutical Association. 2002;42:S13–17. doi: 10.1331/1086-5802.42.0.s13.burris. [DOI] [PubMed] [Google Scholar]
- Castells M. The City and the Grassroots. Berkeley, CA: University of California Press; 1983. [Google Scholar]
- Clear A. New York: 2003. Executive director, Harm Reduction Coalition, New York City. Personal communication. [Google Scholar]
- Cooper H, Moore L, Gruskin S, Krieger N. Characterizing perceived police violence: Implication for public health. American Journal of Public Health. 2004;94(7):1109–1118. doi: 10.2105/ajph.94.7.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper H, Moore L, Gruskin S, Krieger N. The impact of a police drug crackdown on drug injectors' ability to practice harm reduction: a qualitative study. Social Science and Medicine. 2005;61:673–684. doi: 10.1016/j.socscimed.2004.12.030. [DOI] [PubMed] [Google Scholar]
- Cresswell T. Place: a short introduction. Blackwell Publishing; 2004. [Google Scholar]
- Curtis D. Looking for strengths in response to AIDS: Individual, group and public authority roles in strategy. Public Administration and Development. 2004;24:51–59. [Google Scholar]
- Daker-White G. Drug user's access to community-based services. Health and Place. 1997;3(4):217–228. [Google Scholar]
- Dear MJ. The postmodern challenge: Reconstructing human geography. Transactions of the Institute of British Geographers. 1988;13:262–274. [Google Scholar]
- Dear M, Wilton R, Gaber SL, Takahashi LM. Seeing people differently: The sociospatial construction of disability. Environment and Planning: Society and Space. 1997;15:455–480. [Google Scholar]
- Dee TS. Alcohol abuse and economic conditions: Evidence from repeated cross-sections of individual-level data. Health Economics. 2000;10:257–270. doi: 10.1002/hec.588. [DOI] [PubMed] [Google Scholar]
- DeMarco R, Johnsen C. Taking action in communities: Women living with HIV/AIDS lead the way. Journal of Community Health and Nursing. 2003;20(1):51–62. doi: 10.1207/S15327655JCHN2001_05. [DOI] [PubMed] [Google Scholar]
- Des Jarlais DC. Research, politics, and needle exchange. American Journal of Public Health. 2000;90(79):1392–1394. doi: 10.2105/ajph.90.9.1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC, Paone D, Friedman SR, Peyser N, Newman RG. Public health then and now: Regulating controversial programs for unpopular people: Methadone maintenance and syringe-exchange programs. American Journal of Public Health. 1995;85(11):1577–1584. doi: 10.2105/ajph.85.11.1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC, Marmor M, Paone D, Titus S, Shi Q, Perlis T, Friedman S. HIV incidence among syringe exchange participants in New York City. The Lancet. 1996;348:987–991. doi: 10.1016/s0140-6736(96)02536-6. [DOI] [PubMed] [Google Scholar]
- Downing M, Vernon K, Riess TH, Mulia N, McKnight C, Des Jarlais DC, Edlin BR. Community acceptance and implementation of HIV prevention interventions for injection drug users. AIDS Education and Prevention. 2005;17(1):68–78. doi: 10.1521/aeap.17.1.68.58688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drucker E, Lurie P, Wodak A, Alcabes P. Measuring harm reduction: The effects of needle and syringe exchange programs and methadone maintenance on the ecology of HIV. AIDS. 1998;12 A:S217–230. [PubMed] [Google Scholar]
- Drucker E. Notes from the drug wars, through the eye of the needle III: In a dark season, one million points of light. Drugtext: the Internet Center for Substance Use Related Risk Reduction. 1990 http://www.drugtext.org/library/articles/902304.htm.
- Epstein S. Impure science: AIDS, Activism, and the Politics of Knowledge. Berkeley, CA: University of California Press; 1996. [PubMed] [Google Scholar]
- Farmer P. AIDS and Accusation: Haiti and the Geography of Blame. Berkeley and Los Angeles, California: University of California Press; 1992. [Google Scholar]
- Farmer P. Infections and inequalities: The modern plagues. Berkeley, CA: University of California Press; 1999. [Google Scholar]
- Friedman SR. The political economy of drug-user scapegoating and the philosophy and politics of resistance. Drugs: Education, Prevention, and Policy. 1998;5(1):15–32. [Google Scholar]
- Friedman SR, Perlis T, Des Jarlais DC. Laws prohibiting over-the-counter syringe sales to injection drug users: Relations to population density, HIV prevalence, and HIV incidence. American Journal of Public Health. 2001;91(5):791–793. doi: 10.2105/ajph.91.5.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Perlis T, Lynch J, Des Jarlais DC. Economic inequality, poverty, and laws against syringe access as predictors of metropolitan area rates of drug injection and HIV infection. Proceedings of the Global Research Network Meeting, Durban, South Africa. 2000:147–149. [Google Scholar]
- Friedman SR, Tempalski B, Cooper H, Keen M, Friedman R, Flom PL, Des Jarlis DC. Structural analysis for structural intervention: Predictors of IDU population size and HIV prevalence among IDUs in U.S. cities. Oral presentation at the XV International AIDS Conference; 11-16 July 2004; Bangkok, Thailand. 2004a. [Google Scholar]
- Friedman SR, Tempalski B, Cooper H, Perlis T, Keem M, Friedman R, Flom PL. Estimating numbers of IDUs in metropolitan areas for structural analyses of community vulnerability and for assessing relative degrees of service provision for IDUs. Journal of Urban Health. 2004b;8(3):377–400. doi: 10.1093/jurban/jth125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Curtis R, Neaigus A, Jose B, Des Jarlais DC. Social networks, drug injectors' lives, and HIV. New York: Plenum; 1999. [Google Scholar]
- Grund J, Kaplan C, Adriaans N. Featuring high-risk behavior: Needle sharing in the Netherlands. American Journal of Public Health. 1991;81(12):1602–07. doi: 10.2105/ajph.81.12.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan H, Thiede H, Des Jarlais DC. HIV/hepatitis C virus co-infection in drug users: Risk behavior and prevention. AIDS. 2005;19 3:S199–S207. doi: 10.1097/01.aids.0000192090.61753.d4. [DOI] [PubMed] [Google Scholar]
- Harvey D. On the history and present condition of Geography: An historical materialist manifesto. In: Agnew J, Livingstone DN, Rogers A, editors. Human Geography: An Essential Anthology. Oxford: Blackwell Publishers, Ltd; 1996. [Google Scholar]
- Hoffman B. Health care reform and social movements in the United States. American Journal of Public Health. 2003;93(1):75–98. doi: 10.2105/ajph.93.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmberg S. The estimated prevalence and incidence of HIV in 96 large U.S. metropolitan areas. American Journal of Public Health. 1996;86(5):642–654. doi: 10.2105/ajph.86.5.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley SF, Jolley DJ, Kaldor JM. Effectiveness of needle-exchange programs for prevention of HIV infection. The Lancet. 1997;21:1797–1800. doi: 10.1016/S0140-6736(96)11380-5. [DOI] [PubMed] [Google Scholar]
- Jin RL, Shah CP, Svoboda TJ. The impact of unemployment on health: A review of the evidence. Journal of Public Health Policy. 1997;18:275–301. [PMC free article] [PubMed] [Google Scholar]
- Johnston RJ. A question of place: Exploring the practices of Geography. Oxford, England & Cambridge, MA: Blackwell Publishing Ltd; 1991. [Google Scholar]
- Kinzly M. New Haven, CT: 2003. Research Associate, Yale University, Department of Epidemiology and Public Health. Presonal communication. [Google Scholar]
- Kearns RA, Joseph AE. Space in its place: Developing the link in medical geography. Social Science and Medicine. 1993;37(6):711–717. doi: 10.1016/0277-9536(93)90364-a. [DOI] [PubMed] [Google Scholar]
- Krieger N. A glossary for social epidemiology. Journal of Epidemiology and Community Health. 2001;55:693–700. doi: 10.1136/jech.55.10.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marston SA. Mobilizing geography: Locating space in social movement theory. Mobilization: An International Journal. 2003;8(2):227–231. [Google Scholar]
- Martin DG, Miller B. Space and contentious politics. Mobilization: An International Journal. 2003;8(2):143–156. [Google Scholar]
- Martin DG. ‘Place-framing’ as place-making: constituting a neighborhood for organizing and activism. Annals of the Association of American Geographers. 2003;93(3):730–750. [Google Scholar]
- Massey D. A Global Sense of Place. In: Cresswell T, editor. Place a short introduction. Blackwell Publishing; 1997. pp. 63–70. [Google Scholar]
- McCague D. Albuquerque, New Mexico: 2004. Director, Health Care for the Homeless. Personal communication. [Google Scholar]
- MacDonald M, Law M, Kaldor J, Hales J, Dore G. Effectiveness of needle and syringe programmes for preventing HIV transmission. International Journal of Drug Policy. 2003;14:351–352. [Google Scholar]
- McQuie H. Campaign Coordinator to legalize the medical use of marijuana 2003. Personal communication.
- Miller BA. Geography and social movements: Comparing antinuclear activism in the Boston area. Minneapolis, MN: University of Minnesota Press; 2000. [Google Scholar]
- Novick DM, Haverkos HW, Teller DW. The medically ill substance abuser. In: Lowinson Joyce H, Ruiz Pedro, Millman Robert B, Landgrod John G., editors. Substance Abuse: A Comprehensive Textbook. Third. Baltimore: Williams & Wilkins; 1997. pp. 534–550. [Google Scholar]
- Paone D, Clark J, Shi Q, Purchase D, Des Jarlais DC. Syringe exchange in the United States, 1996: A national profile. American Journal of Public Health. 1999;89:43–46. doi: 10.2105/ajph.89.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petchey R, Williams J, Farnsworth B, Starkey K. A tale of two (low prevalence) cities: Social movement organizations and the local policy response to HIV/AIDS. Social Science and Medicine. 1998;47(9):1197–1208. doi: 10.1016/s0277-9536(97)10020-x. [DOI] [PubMed] [Google Scholar]
- Pile S, Keith M, editors. Geographies of resistance. London and New York: Routledge; 1997. [Google Scholar]
- Porter D. Health, civilization and the state: A history of public health from ancient to modern times. London and New York: Routledge; 1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purchase D. Director, Point Defiance AIDS Projects, and the North American Syringe Exchange Network 2003. Personal communication.
- Ruhm CJ. Are recessions good for your health? Quarterly Journal of Economics. 2000;115:617–650. [Google Scholar]
- Sibley D. Geographies of Exclusion. London, England: Routledge; 1995. [Google Scholar]
- Singer M. Forging a Political Economy of AIDS. In: Singer M, editor. The political economy of AIDS. Baywood Publishing Company, Inc.; Amityville, New York: 1998. [Google Scholar]
- Smith DM. Geography and Social Justice. Oxford, England & Cambridge, MA: Blackwell Publishers Ltd.; 1994. [Google Scholar]
- Soja EW. The Socio-spatial dialectic. Annals of the Association of American Geographers. 1980;70 [Google Scholar]
- Soja EW. Reassertions: Towards a Spatialized Ontology. In: Agnew J, Livingstone DN, Rogers A, editors. Human Geography: An Essential Anthology. Oxford, England & Cambridge, MA: Blackwell Publishers Ltd; 1997. pp. 623–635. [Google Scholar]
- State of New Jersey Department of Health and Senior Services (NJDHSS) Division of AIDS, HIV/AIDS Epidemiologic Profile for the State of New Jersey. 2002. [Google Scholar]
- Strathdee S, Celentano D, Shah N, Lyles C, Stambolis VS, Macalino G, Nelson K, Vlahov D. Needle exchange attendance and health care utilization promote entry into detoxification. Journal of Urban Health. 1999;76:448–460. doi: 10.1007/BF02351502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoller NE. Lessons from the damned: Queers, whores, and junkies response to AIDS. New York, NY: Routledge; 1998. [Google Scholar]
- Sumartojo E. Structural factors in HIV prevention: concepts, examples, amd implications for research. AIDS. 2000;14(S1):S3–S10. doi: 10.1097/00002030-200006001-00002. [DOI] [PubMed] [Google Scholar]
- Szreter S. The importance of social intervention in Britain's mortality decline c 1850-1914: A re-interpretation of the role of public health. The Society for the Social History of Medicine. 1988;1:1–37. [Google Scholar]
- Takahashi LM. Homelessness, AIDS, and Stigmatization The NIMBY Syndrome in the United States at the End of the Twentieth Century. Oxford: Clarendon Press; 1998. [Google Scholar]
- Taussig JA, Weinstein B, Burris S, Jones TS. Syringe laws and pharmacy regulations are structural constraints on HIV prevention in the US. AIDS. 2000;14(S1):S47–S51. doi: 10.1097/00002030-200006001-00007. [DOI] [PubMed] [Google Scholar]
- Tempalski B, Des Jarlais DC, Friedman SR, Burris S. Spatial variations of legality, funding and services among U.S. SEPs. The 14th International Conference on the Reduction of Drug Related Harm; 6-10 April 2003; Chiang Mai, Thailand. 2003a. Published abstract. [Google Scholar]
- Tempalski B, Friedman SR, Des Jarlais DC, McKnight C, Keem M, Friedman R. What predicts which metropolitan areas in the USA have syringe exchange programs? International Journal on Drug Policy. 2003b;14(56):417–424. Special Issue on syringe exchange and access. [Google Scholar]
- Tempalski B. The uneven geography of syringe exchange programs in the United States: Need, politics, and place. Dissertation, Department of Geography, University of Washington 2005 [Google Scholar]
- U.S. General Accounting Office. Needle Exchange Programs: Research Suggests Promise as an AIDS Prevention Strategy. Washington, DC: US General Accounting Office; 1993. [Google Scholar]
- Wallace D, Wallace R. A Plague on Your Houses. New York: Verso; 1998. [Google Scholar]
- Wallace R, Huang Y, Gould P, Wallace D. The hierarchical diffusion of AIDS and violent crime among U.S. metropolitan regions: inner-city decay, stochastic resonance and reversal of the mortality transition. Social Science and Medicine. 1997;44(7):935–947. doi: 10.1016/s0277-9536(96)00197-9. [DOI] [PubMed] [Google Scholar]
- Wilton RD. Grounding hierarchies of acceptance: The social construction of disability in NIMBY conflicts. Urban Geography. 2000;21(7):586–608. [Google Scholar]
- Vlahov D, Des Jarlais DC, Goosby E, Hollinger PC, Lurie PG, Shiver MD, Strathdee S. Needle exchange programs for the prevention of human immuno-deficiency virus infection: Epidemiology and policy. American Journal of Epidemiology. 2001;154(12):S70–S77. doi: 10.1093/aje/154.12.s70. [DOI] [PubMed] [Google Scholar]


