Abstract
The original description of M-mode echocardiography in 1953, by Inge Edler (1911–2001) and his physicist friend Hellmuth Hertz, marked the beginning of a new diagnostic noninvasive technique. Edler used this technique primarily for the preoperative study of mitral stenosis and diagnosis of mitral regurgitation. His work was carried forward by cardiologists all over the world, who developed Doppler, 2-dimensional, contrast, and transesophageal echocardiography. These are now standard in cardiologic examinations. Edler also influenced neurologists and obstetricians at Lund University (Sweden) to use ultrasound in their fields. For his landmark discovery, Edler is recognized as the “Father of Echocardiography.”
Key words: Biography; echocardiography/history; Edler I; Hertz CH; history, 20th cent.; mitral valve stenosis/history; pericardial effusion/ultrasonography; ultrasonics/history
Known as the Father of Echocardiography,1 Inge Edler had an impact on the field of diagnostic imaging similar to that of Hounsfield on the development of computed tomography.2 Echocardiography is now the most rapidly growing medical imaging technique, projected by many to become more important than the x-ray itself.3
Early Developments in Echocardiography
The importance of echo reflection, the concept behind echocardiography, was first demonstrated by Lazzaro Spallanzani4 (1729–1799), when he showed that reflected echoes of inaudible sound enabled bats to navigate. With the discovery of piezoelectricity by the Curies in 1880 came the ability to create ultrasonic waves.5 Lewis Richardson's suggestion, in 1912, that an echo-ranging technique could be used to detect underwater objects was followed by the development of the SONAR (Sound Navigation and Ranging) system by Langevin in 1915,4 in time to be used for detecting enemy submarines during World War I. By 1941, in time for World War II, the U.S. Navy was using reflected radio waves to detect the presence of airplanes, a technology that they termed RADAR (Radio Detection and Ranging). The ultrasonic pulse-echo technique was first used for nonmilitary purposes by Sergei Sokolov in 1937,6 and then by Floyd Firestone in 1942,7 for the detection of flaws in metals.
Inspired by the success of RADAR, French physiotherapist André Denier, in 1946, proposed that ultrasound might be used to visualize the internal organs of the human body.8 The Americans, leaders in the field of advanced electronics at that time, were the first to begin experimentation. However, their early investigations were very general and did not have any practical applications.8 An Austrian neurologist, Karl Theo Dussik,9 in association with his physicist brother, was probably the first (1941) to apply ultrasound to medical diagnosis, when he used transmission ultrasound to outline the ventricles of the brain. However, after a decade of work, his efforts were not fruitful, due to the great attenuation and reflection of ultrasonic waves by the bony structure of the cranium. In the late 1940s, the German physicist, Wolfe Dieter Keidel, envisioned the use of transmitted continuous ultrasound for recording the rhythmic volume variations of the heart. Unfortunately, he was not able to make his method quantitative and concluded that the “immense technical problems compared with the crude diagnostic possibilities” rendered the work hardly worthwhile.8 Both Dussik and Keidel eliminated the possibility of using reflected ultrasound, for theoretical reasons; they never performed any practical experiments with reflected ultrasound.
Birth of a Legend
On 17 March 1911, Inge Edler was born in Burlöv, Malmöhus county (now Malmö county), at the southern tip of Sweden. His parents, Carl and Sophia Edler, were teachers in a primary school in the vicinity.1 He was the youngest of 3 siblings. From early childhood, he was interested in technology, nature, and geography. Edler was adventurous. He enjoyed, for example, doing advanced acrobatics on his bicycle, which he continued to do until he was about 75 years of age—performing shows for his grandchildren. As an amateur sportsman, he at one time held a local record for the 100-meter sprint. As an amateur magician, he performed for his family and even traveled to conferences of magicians all over Europe, quite unaware of the magic that he would create in the years to come.*
Edler graduated from his local high school, Hegre Allmanna Laroverket, in 1930. In spite of a keen interest in physics, in particular micronics (the study of the physical phenomena associated with small geometrical structures), he at first chose dentistry, having been influenced by his older sister, who was a dentist. As fate would have it, Edler attempted too late in the year to enter dental school, so he enrolled in medical school at Lund University, merely as a stopgap.
Medicine captivated this quiet thinker, and he went on to receive his medical degree in 1943.1 In 1939, he met the love of his life, Karin Jungebeck, a medical student at the same university, and they married. His wife was a great motivating force, helping him in every possible way, from housework to the proofreading of manuscripts.* Their marriage was blessed with 4 children.
Medicine as a Profession
At the outset of his career in general practice, Edler soon joined the Department of Internal Medicine at Malmö General Hospital. Because his interest lay in cardiology, he served there as director of the Laboratory for Heart Catheterization from 1948 until 1950. For the decade thereafter, he worked as head of the Department of Internal Medicine and as director of the Cardiovascular Laboratory at the University Hospital of Lund. It was at this time that he conceived an idea that the Royal Physiological Society of Sweden would later call, in giving Edler the Lund Award, a “scientific work of extraordinary significance.”3
The Problem
During the late 1940s, surgery of the heart was started in Lund by Drs. Helge Wulff and Phillip Sandblom, both pioneers in the field. They set out to alleviate mitral stenosis in adults, dilating the constricted valve by inserting a finger. Most patients got better after this procedure. However, Wulff and Sandblom encountered some patients whose condition worsened postoperatively. They realized that the symptoms of these patients arose not simply from a small valve opening (mitral stenosis) but from valve incompetence (mitral regurgitation).10 The only way of knowing this condition preoperatively was through elaborate cardiac catheterization.
This was where Dr. Inge Edler stepped in. As the director of the Cardiovascular Laboratory, he was responsible for the preoperative evaluation of valvular heart disease, to enable appropriate referral for closed mitral commissurotomy. Unhappy with the inadequacies of cardiac catheterization imaging techniques at that time, he set his focus immediately on the possibility of making a quantitative diagnosis of mitral stenosis and determining the existence of mitral regurgitation, through noninvasive means.10
Early in his career, Edler was interested in exploring the possibility of using rheocardiography (the recording of changes in electrical impedance in the thorax during heart cycles) as a tool to evaluate the degree of regurgitation.8 Although unsuccessful, his procedure suggested that the left atrium expanded when blood regurgitated from the left ventricle back to the left atrium. This hint was enough to arouse his inquisitive mind. Could this expansion be measured by an echo method? Edler, who found orienteering through uncharted forests with maps and compass a wonderful pastime,** was now in a similarly unexplored field of cardiology, with a mystery to unravel and an ingenious idea to help him.
With fresh knowledge of the recent military experience of RADAR in World War II, Edler read a book on RADAR engineering and wondered if it would be possible to generate frequencies high enough for use in measuring short distances.
Inge Edler and Carl Hellmuth Hertz
Faced with this problem, Edler contacted his nurse's husband, Jan Cedurlund, a physicist. Cedurlund, in turn, put the doctor's query to his physicist friend, Carl Hellmuth Hertz. Hertz's father, Gustav, was a Nobel Prize winner in physics, and his uncle, Heinrich Hertz, had lent his name to the unit of frequency.11 Having won a 1-year scholarship to Lund University in 1947, the young Hellmuth Hertz had so impressed everyone that he had stayed on as a junior assistant in physics. His reply to Edler's query was that such high frequencies could not be generated. However, the problem intrigued Hertz, who during his recent training had plodded his way through the “bible of ultrasound,” Der Ultraschall, by Ludwig Bergman. He thought that ultrasound might be the solution to Dr. Edler's problem. After a couple of days, Hertz contacted Cedurlund, asking him who the doctor was.10
Having inherited the “hertzonian” genes, this boy wonder set out with the quiet thinker, Dr. Edler, towardsfinding a solution to “visualizing the heart.” Thus was born a memorable collaboration between the young graduate physicist and the 42-year-old cardiologist, a team of contrasting personalities—Hertz, impulsive and insistent upon the immediate trial of new ideas, and Edler, reflective and more practical than scientific in his orientation.10 This team (Fig. 1) would bring about, in the words of Pamela S. Douglas, then president of the American Society of Echocardiography, “one of the truly groundbreaking and remarkable innovations of the 20th century.”12
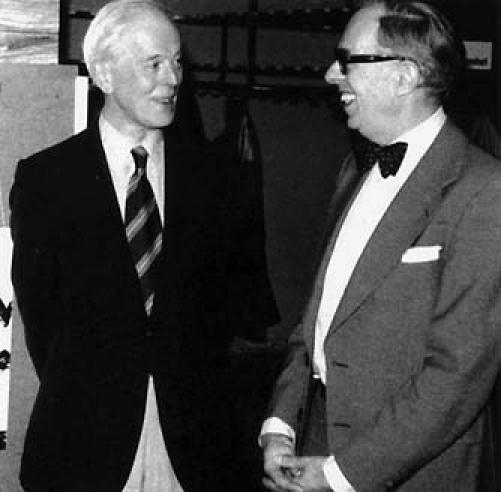
Fig. 1 Inge Edler (left) and Carl Hellmuth Hertz, the cardiologist-physicist team that gave the world echocardiography, at a symposium in Lund, Sweden, 1977.(Photo from the private collection of Dr. Lars Edler, published by permission.)
At that time, Hertz estimated that there was a 50% possibility that reflected ultrasound could be used for measuring the expansion of the left atrium.8 This was good enough for Edler and Hertz to take a chance. Unaware of other experimental attempts to use ultrasound as a medical diagnostic tool, they decided to perform practical experiments without benefit of theoretical groundwork.
The 1st ultrasonic reflectoscope was delivered to Tekniska Rontgencentralen AB, a company that specialized in nondestructive testing10 at Kockum's shipbuilding yard in Malmö. Hertz visited the company in May 1953 and, while there, applied the transducer to his precordium and observed pulsatile echo signals. Could this have been the 1st ultrasonic image of the heart? Unaware of the implications, the manager of the company was kind enough to lend Hertz the reflectoscope for the weekend—a small act of consideration that set the stage for a path-breaking discovery. At the cardiac laboratory at Lund University, Edler and Hertz put the ultrasonic probe over the latter's heart and, to their fascination, saw an echo moving back and forth along the X-axis of the oscilloscope screen at a depth of 8 to 9 cm from the chest wall.13
Because neither man held a Swedish PhD, Edler and Hertz were not entitled to apply for the research grant that would have been necessary to buy an ultrasonic reflectoscope.8 Luck again played its part. Hertz found out that the Siemens Corporation was building an ultrasonic reflectoscope. Hertz's father, Prof. Gustav Hertz, had served as the director of one of the Siemens laboratories before World War II, so he was able to contact Wolfgang Gellinek, director of the Siemens medical branch in Erlangen, Germany. Just married, the younger Hertz arrived in Germany for his honeymoon; but he left his wife, Birgit, long enough to demonstrate his discoveries at the factory laboratory in Erlangen. Immediately able to grasp the importance that this work could have for cardiology, Gellinek ordered that a Siemens reflectoscope be sent to Lund on loan for 1 year, although a regular customer would have to wait. As it happened, this equipment was never to be returned.13
After getting their reflectoscope, Edler and Hertz had to dispel the long-standing notion that the small difference in impedance between heart muscle and blood was not significant enough to be detected by reflected ultrasonic waves. This required an exacting choice of ultrasonic frequency—a frequency that would have enough penetration without compromising resolution. Hertz chose 2.5 MHz as optimal for this purpose, and the initial experiments on isolated, transected hearts (excised from the thorax and filled with water) showed the desired muscle–fluid interface. Edler and Hertz were also able to measure the thickness of the cardiac walls and the interventricular septum.8 However, these initial A-mode (amplitude-mode) images were crude and gave little information beyond telling the distance between the transducer surface and the echo-giving structure. In order to record continuously the changing depth of the echoes from moving cardiac structures, Edler devised the recording technique that is now known as the time-motion, or M-mode, technique. In his original M-mode system, the output was photographed by film that was exposed as it passed in front of the oscilloscope screen at a constant speed. The echoes from non-moving structures appeared on the film as straight lines, while those from moving structures changed position in parallel with the motion of the structures from which they were reflected.14
Then, on 29 October 1953, equipped with the “Ultraschall Impulsgerät” (the Siemens Ultrasound Reflectoscope), Inge Edler and Hellmuth Hertz recorded the 1st moving pictures of the heart, thus inaugurating the field of “ultrasound cardiography,” UCG for short. The 1st echoes, recorded via M-mode, were from the posterior wall of the left ventricle and from anotherstructure thought to be the anterior wall of the left atrium. An article titled “The use of ultrasonic reflecto-scope for continuous recording of the movements of heart valves” was published in the proceedings of the Royal Physiological Society in Lund in 1954.14
Master Magician at Work
Edler, during the course of his subsequent ultrasonic cardiograms, realized that a characteristic pattern of echo signals was obtained in patients who displayed mitral stenosis, from some structure that lay at a depth of 6 to 8 cm from the chest wall and 2 to 4 cm anterior to the rearmost echo from the heart, a pattern that varied with pressure changes in the left atrium.15 Determined to find the origin of these signals, he performed experiments on calf hearts behind the closed doors of a kitchen in the non-surgical ward of his hospital (Fig. 2).

Fig. 2 Inge Edler is seen experimenting on calf hearts. With these, he proved that echoes—at first thought to be from the anterior wall of the left atrium—were actually from the mitral valve. This information was subsequently used by Edler in the diagnosis of valvular heart disease, one of the earliest applications of echocardiography. (Photo from the private collection of Dr. Lars Edler, published by permission.)
Subsequently, to verify his observations, Edler devised and conducted ingenious UCG examinations on dying patients. Upon completion of an exam, he marked the direction of the ultrasonic beam on the patient's chest. After the patient died, he passed an ice pick through the chest wall in the direction taken by the ultrasonic beam. On postmortem examination, Edler found that the needle had pierced the anterior wall of the right ventricle, had passed through the right ventricular outflow tract, the interventricular septum, and the upper part of the left ventricle, and, as a rule, had entered the left atrium via the mitral valve. Edler realized that this anterior cusp of the mitral valve was responsible for the echo signal in question.15
During the course of subsequent examinations, Edler observed that the typical UCG finding from the anterior wall of the left atrium of patients with mitral stenosis was different from that recorded in patients with mitral regurgitation. The movement of the echo signal in regurgitation had a high speed in early ventricular diastole, whereas it was very slow throughout the entire diastole in patients with a predominantly stenotic valve. After closed commissurotomy, this motion (termed diastolic downstroke) increased. The original goals that had spurred the development of this technique had been met: in addition to establishing a diagnostic distinction between stenosis and regurgitation, echocardiography made it possible to determine the severity of the stenosis. A correlation had been found between the speed of diastolic downstroke and the size of the mitral ostium.16
The 1st clinical application of diagnostic cardiac ultrasound was actually in the diagnosis and follow-up of patients with pericardial effusion. With experience, Edler's proficiency increased still more: as early as 1956, when the comparatively primitive quartz-based ultrasonic transducers were still in use, he was able to make the rare diagnosis of atrial myxoma when a patient with mitral stenosis was referred to him to rule out thrombosis.17
Edler and Hertz also attempted transesophageal echocardiography8; however, they faced difficulties in obtaining acoustic coupling between the transducer and the esophageal wall. This feat was first accomplished by Frazin and associates in 1976,18 more than 2 decades after the attempt by Edler and Hertz.
Other early applications of M-mode echocardiography included the demonstration of atrial wall motion during atrial flutter and the recording (after the introduction of the more sensitive barium titanate crystal) of the locations, amplitudes, and motion patterns of all the cardiac valves.
“Great Things Happen over Lunch”
Edler and Hertz's work stimulated other research scientists in Lund to develop ultrasonic imaging techniques, in neurology, obstetrics, and gynecology. Lars Leksell, head of the Department of Neurosurgery, borrowed Edler's equipment and his expert advice to detect displacement of the midline of the brain in patients with intracranial masses.19 Alf Stovall, Professor of Obstetrics and Gynecology, became interested in this technique after a luncheon conversation with Drs. Edler and Leksell and encouraged its use for the evaluation of early pregnancy, which eventually culminated in the world's 1st ultrasonic pictures of twins, taken by his young resident Bertie Sundén.20 Pediatric cardiologist Niles-Rune Lindstrom also understood the potential of this entirely noninvasive technique when investigating illness in children.21 The University Hospital of Lund provided the ideal atmosphere for the interdisciplinary exchange of research results, because its small size meant that the entire faculty took their lunch in a single hall.
When the Literati Became Illiterate
During the early years of echocardiography, cardiologists showed little interest in Edler and Hertz's inventive ultrasonic technique. When famed Harvard cardiologist Paul Dudley White visited Lund University in September 1956, Edler got the opportunity to demonstrate his technique. Dr. White uttered a polite dismissal: “an ingenious method.” Later in the same year, Edler had the opportunity to present the technique to André F. Cournand, who was visiting Lund after receiving the Nobel Prize in Stockholm for his early work in heart catheterization. “He will definitely understand,” thought Edler. However, Dr. Cournand also showed no interest in this noninvasive technique.8 This callous attitude on the part of the scientific community resulted in ignorance of this important work in most parts of the world, albeit for a short while. Edler felt let down by his international colleagues and was now hesitant to publish. He was unwilling, even, to write his doctoral thesis. Even when his chief, Dr. Naquin Mambos, encouraged him with the offer of his own department, Edler flatly refused. For him, the ceremonies connected with the conferral of a doctoral degree were equivalent to the awarding of prizes at a horse show. He then moved to a smaller county hospital.*
Hertz, meanwhile, created new techniques for 2-dimensional echocardiography and for using the Doppler effect to measure the rate of blood flow. However, he was given no support in the form of grants from the Swedish Board of Technical Development, because the Board's advisors believed that the method lacked “medical” and “commercial” interest. Disappointed, he left the field of cardiac ultrasound and directed his attention to the development of inkjet printing, after having been named the founding professor of the Department of Electrical Measurements at Lund University.10 Edler continued his work in cardiac imaging. Finally, in 1961, he defended his thesis (Fig. 3) and returned to Lund University as chairman of cardiology.
Fig. 3 Inge Edler defends his thesis, 1961.(Photo from the private collection of Dr. Lars Edler, published by permission.)
“From Sweden, with Love…”: A World Premiere
Edler's work was reviewed in a scientific film shown atthe 3rd European Congress of Cardiology in Rome in 196022 and was summarized in a review article in Acta Medica Scandinavia in 196115—an article that remained the most extensive review of this field for the next 10 years.
Over the course of that decade, the world began to have a better understanding of echocardiography's potential. Director Gellinek of Siemens invited Hertz to encourage German doctors to use the method. These physicians—prominent among them Dr. Sven Effert23 —were sent to Edler at Lund University to learn the technique. The Japanese24 and the Chinese25 were starting their own experiments. A similar story was unfolding in the United States, with Dr. Harvey Feigenbaum in the lead.
Echocardiography in the United States: The Feigenbaum Story
Echocardiography had been introduced in the United States by John Wild and John Reid, who had examined excised hearts ultrasonically as early as 1952.26 However, since neither was a physician, their work was hardly noticed. It was not until a decade after Edler and Hertz's discovery of “cardiac ultrasound” that the 1st American article on the cardiac use of diagnostic ultrasound in mitral stenosis, a duplication of Edler's work, was published by John Reid and Claude Joyner.27 The American effort was carried forward by Harvey Feigenbaum, who, in 1963, sought answers in ultrasound because he was “frustrated with the tediousness and inaccuracies of using the catheterization techniques to measure the cardiac output, volumes and pressures.”11 He borrowed an ultrasonic instrument that neurologists were using to study the deviation of the midline of the brain and proceeded to identify pericardial effusion.28 Still, America was skeptical of the new technology, having witnessed, a few decades back, a promising discovery in ballistocardiography fall into disfavor.
Knowing that one of his shortcomings was the lack of a proper instrument for further work, Feigenbaum collaborated in 1968 with Harold Dodge at the University of Alabama, whose laboratory at that time had the greatest expertise in measuring angiographic volumes. Together, Feigenbaum and Dodge applied the M-mode technique to the measurement of ventricular dimensions—which today is one of the most common uses of echocardiography. Yet their work was rejected by every major cardiology journal at that time, because reviewers were unable to comprehend the method.11 Max Planck once said, “A new scientific truth does not triumph by convincing its opponents and making them see the light, but rather because its opponents eventually die, and a new generation grows up that is familiar with it.” Accordingly, Harvey Feigenbaum proceeded to train young fellows in the field. The 1st course dedicated solely to cardiac ultrasound was taught in Indianapolis in 1968, and among the faculty was the pioneer himself, Dr. Inge Edler.11 Two of the students, B.L. Troy and J.F. Popp, proceeded to repeat the work that Feigenbaum and coworkers had done in 1968 and obtained the same results.29,30 This time, when the reports were sent for publication, the reviewer was Feigenbaum himself, who happily accepted them. These and other discoveries—that left ventricular wall thickness,31 internal dimensions,32 stroke volume,33 ejection fraction,29 and valvular regurgitation30 could all be measured by ultrasonography—proved to be the necessary catalyst for the growth of that diagnostic method in the United States. Ultrasonography also came to be used in the diagnosis of hypertrophic subaortic stenosis, aortic insufficiency, and mitral valve prolapse.
Feigenbaum is credited with giving UCG its present name, “echocardiography,” which arose from neurologists' use of “echoencephalography” in application to a similar technique for the ultrasonic examination of the cranium. He also gave the world the 1st nonphysician “cardiac sonographer” when he hired and trained Charles Haine, a high-school dropout, to record echocardiograms to ease the burden on physicians.11
New Dimensions in Echocardiography
Edler and Hertz set off a remarkable chain of events that today has made echocardiography the “virtual stethoscope.” Scientists all over the world became interested in the new technology.
Yet an M-mode echocardiogram was not a “picture” of the heart: it was a diagram that showed how the position of its structures changed during the course of the cardiac cycle.34 In the early 1970s, Reggie Eggleton35 put a Sunbeam® electronic toothbrush to an innovative use and gave the world its 1st commercially successful 2-dimensional echocardiogram, which enabled the visualization of actual images of the heart. In 1973, S.L. Johnson,36 with an engineer friend, went a step further when he combined 2-dimensional with pulsed Doppler imaging to enable the detection of flow signals from specific locations within the heart or great vessels; thus was born duplex scanning.
Simultaneously, another major breakthrough in Doppler came in 1979, when Holen37 and then Hatle38 noted that a modified Bernoulli equation could be used to detect pressure gradients across stenotic valves and demonstrated that hemodynamic data could be accurately determined with Doppler ultrasound—the long-standing notion that cardiologists learn hemodynamics in the catheterization laboratory was suddenly changed.
In an effort to attain a better visualization “window,” Frazin and his colleagues,18 in 1976, accomplished transesophageal echocardiography. Early in the 1980s, cardiothoracic surgeons added echocardiography to their armamentarium when Marcus and associates39 developed the use of the epicardial Doppler crystal, which could be affixed to a coronary artery at the time of cardiac surgery to evaluate the physiologic significance of coronary stenosis in human beings. This technique, together with transesophageal echocardiography, was subsequently used for the intraoperative monitoring of the repair and replacement of heart valves, for the assessment of corrected congenital defects, and for the monitoring of wall-motion abnormalities. The field of echocardiography is of course still evolving.
Inge Edler: The Father of Echocardiography
To create a new and revolutionary diagnostic technique requires extraordinary qualities of interdisciplinary thinking, good judgment, and patience. Inge Edler, it seems, had all of these. The world recognized Edler's contributions only after his retirement.
In that year (1977), the Albert and Mary Lasker Foundation awarded Edler and Hertz the Clinical Medicine Research Prize, often regarded as the American equivalent of the Swedish Nobel in Medicine. As a recipient of the Lasker Award, Edler joined the ranks of André Cournand (1949), Alfred Blalock and Helen Taussig (1954), and C.W. Lillehei (1955).40 The 1977 Lasker Award was given “for pioneering the clinical application of ultrasound as a noninvasive tool in the medical diagnosis of abnormalities of the heart, probably the most important noninvasive tool for cardiac diagnosis since the electrocardiography machine.”
In 1983, Edler received the Rotterdam Echocardiography Award for his pioneering work in applying ultrasound as a diagnostic tool in cardiology. In 1984, he was awarded the Lund Award by the Royal Physiological Society of Sweden. In recognition of his pioneering contributions to ultrasonic imaging, Lund University, in 1987, bestowed upon him the title of Professor H.C.1 (“Honoris Causa”). In 1988, he received the Medical Ultrasound Pioneer Award from the American Institute of Ultrasound in Medicine, the World Federation of Ultrasound in Medicine and Biology, and the Medical Sciences Division of the National Museum of American History. Edler was also awarded the Aachener und Münchner Preis für Technik und angewandte Naturwissenschaften in 1988 and the Erik K. Fernström Foundation's Nordic Prize in 1991. His last scientific award was in 2000, when he was designated “the Swedish Cardiologist of the Twentieth Century” after a vote by members of the Swedish Society of Cardiology.3
The Father of Echocardiography, however, was never concerned about his personal recognition. He was proud not of his contribution to medicine, but of the advances to which his work had led. He always downplayed his contributions, crediting those persons who were inspired by his work and continued on his path.41 After his retirement, he spent quite a lot of his time helping young biomedical engineering students at the Lund Institute of Technology.3 Harry Rakowski, former president of the American Society of Echocardiography, recalls an incident in 1977, when he journeyed to Lund as a research fellow, on the eve of Dr. Edler's retirement: “I flew to Copenhagen and then took the hydrofoil to Malmö, a town near Lund. To my immense surprise and embarrassment, Inge and his wonderful wife, Karin, met my wife, Elaine, and me at the station and took us to our hotel. It was not something that I would expect the most famous cardiologist in Sweden to do for a research fellow.”41 This act was typical of Edler, who was kindhearted and affable. Those who were fortunate enough to know Edler found in him a great amount of humanity, cordiality, and good humor, together with a natural curiosity about many different subjects.3
Edler's explorations continued late into his life. At the age of 81, Edler undertook an adventure in the company of his wife, an attempt to travel the Silk Road from Islamabad to Peking, including the treacherous Khunjerab Pass, 4,733 meters above sea level. This attempt was thwarted by an avalanche, which trapped the couple in a remote military camp in northern Pakistan for almost a week, before they could return to Islamabad by climbing over ravines and destroyed roads. After this aborted trip, Edler, with his characteristic determination and love of adventure, returned for a 2nd attempt; this time, he completed his journey, alone and 5 years older.3
Inge Edler died on 7 March 2001, just 10 days short of his 90th birthday, in peace, in his sleep at home.
Conclusion
Edler's pioneering work has prolonged and improved the lives of millions of patients. The echocardiogram is the true stethoscope, for it permits us to see what occurs beneath the surface of the skin.11 Today, more than 25 million echocardiograms are performed each year throughout the world.12 According to Prof. Petros Nihoyannopoulos,42 “Never before has the pace of innovations in echocardiography been so swift…. technological innovations are put into clinical practice at such a speed that it has become very difficult to follow, even for dedicated echocardiographers.” Handheld ultrasonographic devices are becoming smaller and smaller, and have highly superior image qualities and functions; there are new methods to study ventricular function with very high temporal resolution, which far exceed the capabilities of cardiac magnetic resonance imaging; contrast echocardiography is now used worldwide for myocardial perfusion studies and may soon become a means of drug delivery43; and 3-dimensional echocardiography is now a reality. “Academic echocardiologists” are now devoting their time to teaching and research in the rapidly expanding field. Although Edler's original M-mode technique has largely been replaced by new and improved imaging modes, it remains an important part of the complete ultrasonic examination of the heart—its superior local-target sensitivity enables better detection of small pericardial effusions, and its higher effective sampling rate (in comparison with 2-dimensional echocardiography) is useful for the precise timing of cardiac events.
Acknowledgments
We sincerely thank Dr. Lars Edler, son of the late Dr. Inge Edler, for providing us valuable insight into his father's personal life and for allowing us to publish photographs from his private collection.
Footnotes
*Personal communication: Dr. Lars Edler (son of Inge Edler) with Siddharth Singh via e-mail on 26 March 2006.
*Personal communication: Dr. Kirsten Brauer (Lund University) with Siddharth Singh via e-mail on 15 May 2006.
**Personal communication: Dr. Lars Edler with Siddharth Singh via e-mail on 28 April 2006.
Address for reprints: Abha Goyal, House No. 1039, Sector 4, Panchkula, Haryana 134112, India. E-mail: abhagoyal@gmail.com
Mr. Singh and Ms Goyal are students at All India Institute of Medical Sciences, New Delhi, India. This paper is runner-up in the 8th and final Texas Heart Institute Award for Undergraduate Writing in the History of Cardiovascular Medicine and Surgery. The winning papers were published in June and September 2007.
References
- 1.Acierno LJ, Worrell LT. Inge Edler: father of echocardiography. Clin Cardiol 2002;25:197–9. [DOI] [PMC free article] [PubMed]
- 2.Hounsfield GN. Computerized transverse axial scanning (tomography). 1. Description of system. Br J Radiol 1973;46: 1016–22. [DOI] [PubMed]
- 3.Holmer NG, Lindstrom K, Lundstrom N-R, Marsal K, Olsson B, Pettersson H, Persson HW. In memoriam: Inge Edler–the father of echocardiography. Eur J Ultrasound 2001; 13:179–82.
- 4.Feigenbaum H. History of echocardiography [monograph on the Internet; cited 2005 Jul 21]. Available from: http://www.asecho.org/freepdf/FeigenbaumChapter.pdf
- 5.Curie P, Curie J. Developpement, par pression de l'electricite polaire dans les cristaux hemiedres a faces inclinees. Comptes Rendus 1880;91:291–5.
- 6.Sokolov SY, inventor. Means for indicating flaws in materials. United States patent US 2164125. 1937.
- 7.Firestone FA, inventor. Flaw detecting device and measuring instrument. United States patent US 1280226. 1942.
- 8.Edler I, Lindstrom K. The history of echocardiography. Ultrasound Med Biol 2004;30:1565–644. [DOI] [PubMed]
- 9.Dussik KT. On the possibility of using ultrasound waves as a diagnostic aid. Neurol Psychiat 1942;174:153–68.
- 10.Nilsson J, Westling H. Ultrasound in Lund–three world premieres. Clin Physiol Funct Imaging 2004;24:137–40. [DOI] [PubMed]
- 11.Feigenbaum H. Evolution of echocardiography. Circulation 1996;93:1321–7. [DOI] [PubMed]
- 12.Siemens celebrates 50th anniversary of echocardiography[news release on the Internet]. PR Newswire Association LLC; c1996-2007 [2003 Mar 30; cited 2005 Jul 23]. Available from: http://www.prnewswire.com/cgi-bin/stories.pl?ACCT=104&STORY=/www/story/03-30-2003/0001916398&EDATE
- 13.Woo JSK. A short history of the development of ultrasound in obstetrics and gynecology [homepage on the Internet]. c1998-2002 [updated 2006 Nov; cited 2005 Jul 23]. Available from: http://www.ob-ultrasound.net/ingehertz.html
- 14.Edler I, Hertz CH. The use of ultrasonic reflectoscope for the continuous recording of the movements of heart walls. 1954. Clin Physiol Funct Imaging 2004;24:118–36. [DOI] [PubMed]
- 15.Edler I. The use of ultrasound as a diagnostic aid, and its effects on biological tissues. Continuous recording of the movements of various heart-structures using an ultrasound echo-method. Acta Med Scand Suppl 1961;370:7–65. [PubMed]
- 16.Edler I, Gustafson A. Ultrasonic cardiogram in mitral stenosis; preliminary communication. Acta Med Scand 1957;159:85–90. [DOI] [PubMed]
- 17.Gustafson A, Edler I, Dahlback O, Kaude J, Persson S. Left atrial myxoma diagnosed by ultrasound cardiography. Angiology 1973;24:554–62. [DOI] [PubMed]
- 18.Frazin L, Talano JV, Stephanides L, Loeb HS, Kopel L, Gunnar RM. Esophageal echocardiography. Circulation 1976;54: 102–8. [DOI] [PubMed]
- 19.Leksell L. Echo-encephalography. 1. Detection of intracranial complications following head injury. Acta Chir Scand 1956; 110:301–15. [PubMed]
- 20.Sundén B. On the diagnostic value of ultrasound in obstetrics and gynaecology. Acta Obstet Gynecol Scand 1964;43(Suppl 6):1–191. [PubMed]
- 21.Lundstrom N-R, Edler I. Ultrasoundcardiography in infants and children. Acta Paediatr Scand 1971;60:117–28. [DOI] [PubMed]
- 22.Edler I, Gustafson A, Karlefors T, Christensson B. The movements of aortic and mitral valves recorded with ultrasonic echo techniques. Scientific film at 3rd European Congress of Cardiology; Rome, Italy; September 1960.
- 23.Effert S, Domanig E. Diagnosis of intra-auricular tumors & large thrombi with the aid of ultrasonic echography [in German]. Dtsch Med Wochenschr 1959;84:6–8. [DOI] [PubMed]
- 24.Kikuchi Y, Uchida R, Tanaka K, Wagai T. Early cancer diagnosis through ultrasonics. J Acoust Soc Amer 1957;29:824–33.
- 25.An S, Wang TH, An SY, Chu SL, Wu HH, Hsu CC, Yu KJ. The use of pulsed ultrasound in clinical diagnosis. Chin Med J 1962;81:315–25. [PubMed]
- 26.Wild JJ, Crawford HD, Reid JM. Visualization of the excised human heart by means of reflected ultrasound of echography; preliminary report. Am Heart J 1957;54:903–6. [DOI] [PubMed]
- 27.Joyner CR Jr, Reid JM, Bond JP. Reflected ultrasound in the assessment of mitral valve disease. Circulation 1963;27(4 Pt 1):503–11. [DOI] [PubMed]
- 28.Feigenbaum H, Waldhausen JA, Hyde LP. Ultrasound diagnosis of pericardial effusion. JAMA 1965;191:711–4. [DOI] [PubMed]
- 29.Pombo JF, Troy BL, Russel RO Jr. Left ventricular volumes and ejection fraction by echocardiography. Circulation 1971; 43:480–90. [DOI] [PubMed]
- 30.Popp RL, Harrison DC. Ultrasonic cardiac echography for determining stroke volume and valvular regurgitation. Circulation 1970;41:493–502. [DOI] [PubMed]
- 31.Feigenbaum H, Popp RL, Chip JN, Haine CL. Left ventricular wall thickness measured by ultrasound. Arch Intern Med 1968;121:391–5. [PubMed]
- 32.Popp RL, Wolfe SB, Hirata T, Feigenbaum H. Estimation of right and left ventricular size by ultrasound. A study of the echoes from the interventricular septum. Am J Cardiol 1969; 24:523–30. [DOI] [PubMed]
- 33.Feigenbaum H, Zaky A, Nasser WK. Use of ultrasound to measure left ventricular stroke volume. Circulation 1967;35: 1092–9. [DOI] [PubMed]
- 34.Echo in Context [homepage on the Internet]. Durham, NC: Duke University Medical Center; c2000 [updated 2000 Nov 11; cited 2005 Jul 28]. Basic echo: two-dimensional echocardiography in the normal heart [page 1]. Available from: http://www.echoincontext.com/begin/skillB_02.asp
- 35.Wann LS, Weyman AE, Feigenbaum H, Dillon JC, Johnston KW, Eggleton RC. Determination of mitral valve area by cross-sectional echocardiography. Ann Intern Med 1978;88: 337–41. [DOI] [PubMed]
- 36.Johnson SL, Baker DW, Lute RA, Dodge HT. Doppler echocardiography: the localization of cardiac murmurs. Circulation 1973;48:810–22. [DOI] [PubMed]
- 37.Holen J, Simonsen S. Determination of pressure gradient in mitral stenosis with Doppler echocardiography. Br Heart J 1980;41:529–35. [DOI] [PMC free article] [PubMed]
- 38.Hatle L, Angelsen BA, Tromsdal A. Non-invasive assessment of aortic stenosis by Doppler ultrasound. Br Heart J 1979;43: 284–92. [DOI] [PMC free article] [PubMed]
- 39.Marcus M, Wright C, Doty D, Eastham C, Laughlin D, Krumm P, et al. Measurements of coronary velocity and reactive hyperemia in the coronary circulation of humans. Circ Res 1981;49:877–91. [DOI] [PubMed]
- 40.Lasker Foundation [homepage on the Internet]. New York: Lasker Medical Research Network [cited 2005 Aug 1]. Former winners. Available from: http://www.laskerfoundation.org/awards/former.html
- 41.Rakowski H. Lives lived: Inge Edler [presidential address]. Raleigh, NC: American Society of Echocardiography; c2007 [2001 May; cited 2005 Jul 23]. Available from: http://www.asecho.org/Archives/Presidents_Message/body_may01.php
- 42.Nihoyannopoulos P. Happy birthday echocardiography: where do we go from here? Hellenic J Cardiol 2003;44:363–5.
- 43.Skyba DM, Price RJ, Linka AZ, Skalak TC, Kaul S. Direct in vivo visualization of intravascular destruction of microbubbles by ultrasound and its local effect on tissue. Circulation 1998; 98:290–3. [DOI] [PubMed]


