Abstract
INTRODUCTION
Carpal tunnel decompression is the most commonly performed surgical procedure within a hand unit. Although very effective, the complications following the procedure can be significant. In an attempt to identify the causes of such complications, we assessed whether seniority of the surgeon impacts on outcome for open carpal tunnel decompression.
PATIENTS AND METHODS
Data were jointly and prospectively gathered from two units from either side of the Atlantic – the Pulvertaft Hand Center, UK and the Curtis Hand Center, USA. The aim of the study was to assess outcome following carpal tunnel decompression. Completed data were gathered following open carpal tunnel decompression on 352 hands. Surgeons of a consultant grade had performed 123 of these procedures whilst surgical trainees had performed 229 of the procedures. Assessment was by Levine Katz questionnaire results, Semmes-Weinstein testing, grip strength and pinch grip strength testing performed both preoperatively and 6 months' postoperatively. Complications following the procedure were also recorded.
RESULTS
Mean results were found to be better in those patients where the surgeon was of a consultant grade. However, this was only found to be of statistical significance on Semmes-Weinstein testing. Complications following the procedure were also noted to be higher in the group of patients operated on by trainee grades.
CONCLUSIONS
Our results show the carpal tunnel decompression performed by a surgeon of consultant grade offers slightly better results in objective neurological testing when compared with those performed by a more junior grade.
Keywords: Carpal tunnel syndrome, Decompression, Surgical, Medical education
Carpal tunnel decompression is the most commonly performed surgical procedure of the hand. While surgical decompression is a popular and effective means of treatment, complications following carpal tunnel decompression have been reported in 12–20% of cases.1 Data gathered from a joint cross-Atlantic study to assess outcome after carpal tunnel surgery was reviewed to see if grade of surgeon performing the carpal tunnel decompression had any bearing on outcome. This allowed us the opportunity to analyse data on a large number of patients who had undergone carpal tunnel decompression.
Patients and Methods
Data were reviewed from the Curtis Hand Center, Baltimore USA and the Pulvertaft Hand Center, Derby UK. The data arose from a prospective study to assess outcome following carpal tunnel decompression. All patients diagnosed with carpal tunnel syndrome by means of clinical evaluation and had persistent symptoms despite a period of splintage were recruited into the study. EMG studies were only performed in those patients in whom diagnosis was uncertain. The patients from the UK limb of the study underwent standard open carpal tunnel decompression performed by either a hand surgeon at registrar grade (unsupervised) or at consultant grade. In contrast all patients who received treatment in the US limb of the study underwent carpal tunnel decompression performed by a consultant hand-surgeon.
The data were then reviewed retrospectively to assess whether outcome from this procedure differed according to grade of operator.
Assessment
Data on age, sex and body mass index (BMI) were recorded for each patient. All patients underwent objective and subjective assessment of symptom severity and functional disability. These assessments were performed pre-operatively and 6 months' postoperatively in all patients. Outcome measures included assessment using a Levine-Katz questionnaire, assessment of grip strength, pinch grip strength and Semmes-Weinstein monofilament testing.2,3 The tests were used at each assessment stage.
All complications were also documented including scar tenderness, pillar pain and persistent symptoms
Data
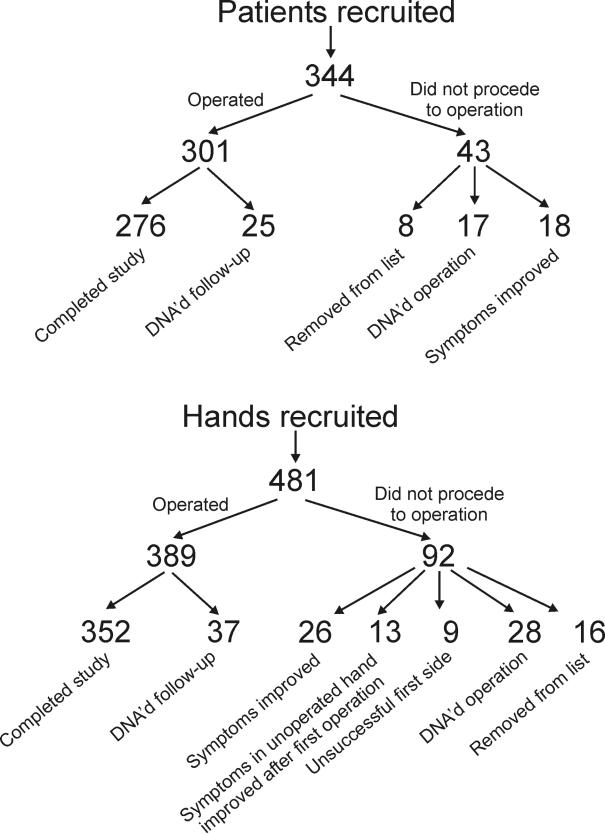
A total of 389 hands in 301 consecutive patients who were recruited into the study underwent standard open carpal tunnel decompression. From these patients, we were able to collect 352 completed data sets from 276 patients. Of the 344 patients initially recruited, 43 dropped out prior to surgery and 25 were lost to follow-up (Fig. 1). Consultant surgeons performed 123 operations, 57 of which were performed in the UK and 66 preformed in the US. The registrars performed 229 procedures. Five different consultant surgeons and three registrars of varying experience from 2–4 years of registrar experience in orthopaedics were involved in performing the procedures. Two of these were specialist registrar trainees whilst the remaining registrar was a clinical fellow; all three were on a 1-year placement in the department.
Figure 1.
Outcome of patients booked for theatre.
The data collected were then analysed by comparing the changes in measurements between before and after carpal tunnel decompression. A statistical analysis was performed using the Mann-Whitney non-parametric test.
Results
The mean age for those patients operated on by trainee grades was 54 years and 59 years for those patients operated on by consultants. The mean BMI was 30 kg/m2 and 31 kg/m2, respectively, for each group the difference being statistically insignificant (P > 0.05). The results of the outcome measures showed that those patients operated on by surgeons at a consultant grade had higher levels of mean improvement in all but grip strength testing. Despite the means being higher, the only tests which showed a statistically significant difference was the Semmes-Weinstein testing (P < 0.001) and Levine Katz Symptom Severity score (P = 0.03; Table 1).
Table 1.
Changes in scores from pre-operatively to 6-months' postoperatively following carpal tunnel decompression
| Improvement in | Surgeon grade | n | Mean | SD | Significance |
|---|---|---|---|---|---|
| Levine Katz Symptom Severity Score | Consultant | 123 | 1.51 | 0.83 | 0.031 |
| Registrar | 229 | 1.39 | 0.83 | ||
| Levine Katz Functional Score | Consultant | 123 | 0.84 | 0.90 | 0.115 |
| Registrar | 229 | 0.61 | 0.86 | ||
| Semmes-Weinstein score | Consultant | 123 | 0.674 | 0.863 | < 0.001 |
| Registrar | 229 | 0.251 | 0.927 | ||
| Grip Strength Score | Consultant | 123 | 0.520 | 8.61 | 0.155 |
| Registrar | 229 | 1.80 | 8.10 | ||
| Pinch Grip Score | Consultant | 123 | 0.617 | 5.54 | 0.173 |
| Registrar | 229 | 1.797E-02 | 2.72 |
We found no statistical difference in outcome between the patients operated on by different registrars. This was also true when comparing outcomes between different consultants.
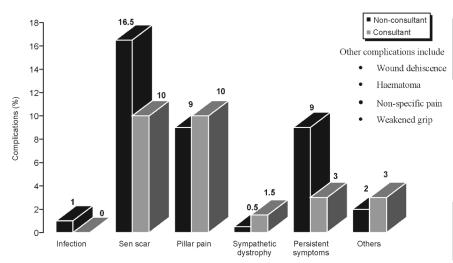
Complications from surgery occurred in 33% of patients. Complications occurred in 37% of patients operated on by trainee grades and in 28% of patients operated on by consultant grades. The complication of scar tenderness was noted to be higher in the group of patients operated on by trainee grades (Fig. 2).
Figure 2.
Complication rates following carpal tunnel decompression.
Discussion
Carpal tunnel decompression is a successful technique for dealing with patients complaining of symptoms of carpal tunnel syndrome, which have not responded to conservative methods. Complications following carpal tunnel decompression vary from scar tenderness to incomplete division of the transverse carpal ligament or even division of the median nerve and studies report complication rates up to 12–20%.1 This frequency combined with the large number of patients who undergo carpal tunnel decompression amount to a significant total morbidity.
A variety of different surgical approaches have been used, in an attempt to reduce the morbidity from the procedure. Dawson et al.4 suggested that the grade of surgeon performing the carpal tunnel decompression might have an impact on outcome, with higher complication rates and lower patient satisfaction in patients where a trainee had performed the procedure.
Our study also demonstrated differences in outcome dependent on grade of operating surgeon. However, these differences were subtle and in specific areas.
In our cohort of patients, the BMI was similar for both groups; however, in the group operated on by consultants, the patients were on average 6 years older. The results of the post-operative assessment revealed that the outcome was better in the group operated on by consultant grades in all but one of the measures we used, despite these patients being slightly older. However, the only tests to show statistically significant differences in outcome were the Semmes Weinstein monofilament testing (P < 0.001) and the Levine Katz Symptom Severity score (P = 0.03). Greater recovery noted on objective neurological testing may point to a more thorough external neurolysis having been performed in this group of patients.
The overall complication rate was 33%, which is higher than in other series;1,5 however, the pattern of complications also differs considerably as a majority of our complications were due to scar tenderness, which accounted for 42% of all the complications. Persistent symptoms, which could suggest intraneural fibrosis or incomplete division of the transverse carpal ligament, occurred in only 7% of cases, which is lower than in other series.6,7 We observed higher rates of scar tenderness and persistent symptoms in the group operated on by registrars (Fig. 1). Overall complications were also noted to be higher in patients operated on by trainee grades.
The study also revealed that 20% of hands booked for theatre did not proceed to have surgery – 28% of these were due to symptom resolution prior to surgery and 14% were inpatients with bilateral symptoms with resolution of symptoms in the non-operated side after the first side had been decompressed. This illustrates, clearly, the characteristic fluctuating presence and degree of symptomatology experienced by patients suffering with carpal tunnel syndrome. In the US, where the time to surgery was considerably shorter allowing less time for fluctuations in symptoms, the cancellations due to symptom resolution were zero.
Conclusions
The study has demonstrated that, even in a routinely performed procedure such as carpal tunnel decompression, differences in outcome do occur dependent on grade of surgeon performing the operation. The differences are, however, slight and may be attributed specifically to certain parts of the procedure. These findings may permit identification of weaknesses in technique that can be improved upon. Scar tenderness can be reduced by more careful dissection to expose the transverse carpal ligament8 and improving sensory restoration can be achieved by a full decompression and a thorough external neurolysis.
Our findings are particularly relevant in a period when training times for surgeons are becoming ever shorter. Those involved in supervision and training of surgeons should, therefore, be alert to these points in the operation where a greater degree of guidance and supervision may be required. These finding should also guide those departments involved in developing models for surgical simulators for the purpose of training.
References
- 1.Louis DS, Greene TL, Noellert RC. Complications of carpal tunnel surgery. J Neurosurg. 1985;62:352–6. doi: 10.3171/jns.1985.62.3.0352. [DOI] [PubMed] [Google Scholar]
- 2.Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75:1585–92. doi: 10.2106/00004623-199311000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Weinstein S, Semmes J, Ghent L, Teuber HL. Roughness discrimination after penetrating brain injury in man: analysis according to locus of lesion. J Comp Physiol. 1958;51:269–75. doi: 10.1037/h0047187. [DOI] [PubMed] [Google Scholar]
- 4.Dawson MJ, Holmes S, Kuczyc R, Gibb PA. Does surgical grade affect outcome of open carpal tunnel release. Ann R Coll Surg Engl (Suppl) 2001;83:261. [Google Scholar]
- 5.Macdonald RI, Lichtman DM, Hanlon JJ, Wilson JN. Complications of surgical release for carpal tunnel syndrome. J Hand Surg. 1978;3:70–6. doi: 10.1016/s0363-5023(78)80118-x. [DOI] [PubMed] [Google Scholar]
- 6.Brown RA, Gelberman RH, Seiler JG, Abrahamsson SO, Weiland AJ, Urbaniak JR, et al. Carpal tunnel release: a prospective, randomized assessment of open and endoscopic methods. J Bone J Surg Am. 1993;75:1265–75. doi: 10.2106/00004623-199309000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Kluge W, Simpson RG, Nicol AC. Late complications after open carpal tunnel decompression. J Hand Surg Br. 1996;21:205–7. doi: 10.1016/s0266-7681(96)80098-2. [DOI] [PubMed] [Google Scholar]
- 8.Ahcan U, Arnez ZM, Bajrovic FF, Hvala A, Zorman P. Nerve fibre composition of the palmar cutaneous branch of the median nerve and clinical implications. Br J Plast Surg. 2003;56:791–6. doi: 10.1016/j.bjps.2003.08.012. [DOI] [PubMed] [Google Scholar]