Abstract
INTRODUCTION
Acute epididymo-orchitis is a common and increasing problem. This retrospective study reviewed whether the European Association of Urology guidelines for the management of acute epididymo-orchitis, which form the basis of this Trust's present inter-departmental guidelines, are being effectively implemented.
PATIENTS AND METHODS
Case notes of 53 patients attending the emergency department with acute epididymo-orchitis over a 6-month period were reviewed retrospectively. The hospital results' database was used to confirm the diagnostic tests requested on patients at the time of their initial presentation.
RESULTS
Of the study cohort, 26 patients were aged ≤ 35 years and 27 patients were aged > 35 years. The results demonstrated that a sexual history was documented in only 43.4% of cases. A mid-stream urine sample was sent for routine culture in 54.7% of cases whilst urine for the Chlamydia polymerase chain reaction (PCR) test was obtained in 17% and a urethral swab performed in 5.6%. Antibiotics were prescribed in 81% of cases. Of these patients, 46.5% received ciprofloxacin alone (mean age, 52 years; range, 18–87 years), 25.5% received doxycycline alone (mean age, 30 years; range, 18–45 years) and 21% received both ciprofloxacin and doxycycline (mean age, 33 years; range 18–49 years). In 26.4% of cases, verbal advice to attend a genito-urinary medicine clinic was given, whilst a formal telephone referral was made in only one case. Formal urological follow-up was arranged for only three out of 11 patients aged > 50 years.
CONCLUSIONS
Although a joint emergency department/urology clinical protocol for the investigation and treatment of acute epididymo-orchitis already exists within the Trust, our current management conforms to this in only a minority of cases. Many different strategies can be employed in the implementation of clinical practice guidelines and all are associated with variable degrees of success. The regular movement of junior staff through each department necessitates that the distribution of management protocols and guidelines occurs at frequent intervals throughout the year and that their implementation is continuously monitored so that, if necessary, further implementation strategies can be employed.
Keywords: Genital diseases, male; Guidelines; Clinical protocols; Medical audit
Acute epididymo-orchitis is a common and increasing problem with patients frequently presenting as GP or self-referrals via the emergency department. Epididymo-orchitis is predominantly an acute inflammatory process. However, if left untreated, chronic inflammation may develop with the sequelae of abscess formation, testicular infarction, testicular atrophy and infertility.1 In men aged > 35 years, the majority of cases are due to infection with common urinary pathogens and may involve other risk factors such as bladder outlet obstruction and urogenital malformations. In men aged ≤ 35 years who are sexually active, acute epididymo-orchitis may be associated with sexually transmitted organisms and infection of the consort.2,3 Infection by Chlamydia trachomatis remains the most common bacterial sexually transmitted disease (STD) in the UK and studies have shown that acute epididymo-orchitis in young males is frequently associated with C. trachomatis infection.4,5 The increasing incidence of acute epididymo-orchitis in this younger age group is occurring alongside a nation-wide increase in the transmission rates of C. trachomatis infection and is part of a wider public health crisis of spiralling STD rates in the UK population.6,7 Correct treatment of young men presenting with acute epididymo-orchitis is imperative in combating the spread of C. trachomatis infection and limiting the sequelae of both male and female infertility.
The European Association of Urology (EAU) guidelines on the management of urinary and male genital tract infections, published in 2001 and updated in March 2006, provide clearly defined diagnostic and therapeutic protocols based upon patient age and likely pathogens (Table 1).8 This retrospective study aimed to review whether the EAU guidelines, which form the basis of this Trust's present inter-departmental guidelines, were being implemented effectively in the treatment of men of all age groups presenting acutely via the emergency department, with particular emphasis on the treatment of men aged < 35 years.
Table 1.
EAU guidelines for investigation and treatment of acute epididymo-orchitis
| Aged ≤ 35 years | Aged > 35 years | ||
|---|---|---|---|
| Investigations | Prior to commencing antibiotic therapy:
|
||
| Antibiotics | • Fluoroquinolone (ofloxacin or levofloxacin) | • Fluoroquinolone (ofloxacin or levofloxacin) | |
| OR | |||
|
|||
| Therapy duration | 2 weeks |
Patients and Methods
A search of the computerised emergency department patient database for the terms ‘testicular’, ‘testicle’ or ‘scrotal’ included in the presenting complaint was performed. Case notes of all patients attending the emergency department with acute epididymo-orchitis over a 6-month period were reviewed. The notes were assessed for documentation regarding sexual history, previous or current antibiotic therapy, investigations employed, prescribed antibiotics and their regimens, referral to genitourinary medicine for contact tracing and formal urological follow-up. The hospital results' database was also searched to confirm the diagnostic tests requested on these patients at the time of their initial presentation.
Results
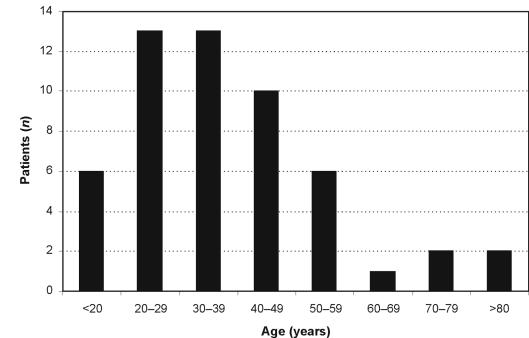
A total of 89 cases of acute epididymo-orchitis were identified over the 6-month period. Of these, only 53 sets of notes were available for review. The age range of patients was 18–87 years with an average age of 38 years (Fig. 1); of these, 26 patients were aged ≤ 35 years and 27 patients were aged > 35 years (11 patients were > 50 years of age).
Figure 1.
Age distribution of study population.
Of patients presenting to the emergency department, 28% had already been commenced on antibiotic therapy by their GP (Table 2). Investigations to identify causative pathogens included a mid-stream urine (MSU) sample for culture (54.7%), urine for Chlamydia polymerase chain reaction (PCR; 17%) and urethral swabs (5.6%).
Table 2.
Range of antibiotic therapy at time of presentation
|
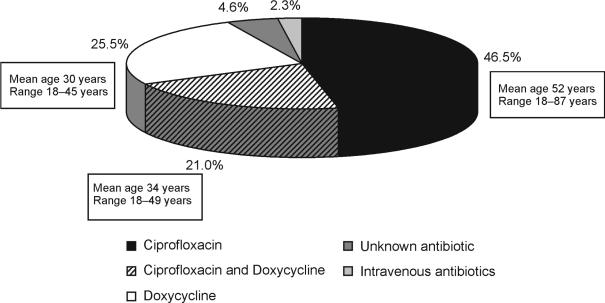
Oral antibiotics were prescribed in 81% of cases. Figure 2 summarises the pattern of prescription and the associated age range of the patients in each treatment group. Of all patients prescribed antibiotics, 46.5% were given ciprofloxacin alone (mean age, 52 years; range, 18–87 years), 25.5% of patients received doxycycline alone (mean age, 30 years; range, 18–45 years) and 21% received ciprofloxacin in combination with doxycycline (mean age, 32 years; range, 18–49 years). Documented dosing regimens and duration of treatment were also variable (Table 3).
Figure 2.
Antibiotic prescribing pattern.
Table 3.
Therapeutic regimens
| Antibiotic | Ciprofloxacin | Doxycycline |
| Dosing regimen | 500 mg bd | 100 mg od or 100 mg bd (200 mg first dose in 2 cases) |
| Duration of treatment | 10 days to 6 weeks | 1–8 weeks |
A sexual history of any form was documented in only 23 of the 53 cases studied (43.4%). Sexual history details were documented in 61.5% of men aged ≤ 35 years and in 25.9% of men aged > 35 years. Referral to genitourinary medicine was documented as made in the form of verbal advice to the patient in only 14 cases (26.4% of total cases), 11 of these in men aged ≤ 35 years (42.3% of men aged ≤ 35 years). A formal telephone referral was made in only one of the 53 cases reviewed (patient aged 40 years).
Formal out-patient urological follow-up was arranged for 14 patients in total. Of the 11 patients aged > 50 years, only three were subsequently referred for further urological assessment and investigation of possible risk factors such as bladder outlet obstruction.
Discussion
The effective management of acute epididymo-orchitis at the time of initial presentation is essential in reducing the risk of long-term sequelae in patients of all ages and imperative in preventing further increase in transmission rates of C. trachomatis infection among the younger population. The EAU guidelines provide an important and useful tool for any clinician involved in the management of patients with acute epididymo-orchitis.
The EAU guidelines recommend that both a urethral swab and an MSU specimen are obtained prior to the commencement of antibiotic therapy. In this study, investigations included an MSU for routine culture in 54.7% of cases, urine for Chlamydia PCR in 17% and a urethral swab in only 5.6% of cases. Chlamydia PCR is not yet widely available for routine clinical use but is rapidly becoming a gold standard test due to its high specificity and sensitivity.9 Interestingly, 28% of patients were already prescribed antibiotics at the time of presentation having attended a primary care centre prior to their attendance at the emergency department. The choice of antibiotics prescribed in the primary care setting was varied (Table 2). The EAU guidelines on empirical antibiotic therapy recommend that for sexually active men aged ≤ 35 years, where C. trachomatis is usually the causative organism, the fluoroquinolones ofloxacin and levofloxacin should be first choice due to their broad spectrum of action, activity against C. trachomatis and good penetration into urogenital tissues. In proven cases of C. trachomatis, treatment should be continued with doxycycline, 200 mg/day, for at least 2 weeks. In men aged ≥ 35 years, where enteric organisms are the likely cause, a fluoroquinolone or trimethoprim alone is recommended. In this study, oral antibiotics were prescribed in 81% of cases. The data show that the choice of antibiotic regimen appeared unrelated to patient age and included the use of ciprofloxacin and/or doxycycline (Fig. 2). In this study, ciprofloxacin was the most frequently prescribed antibiotic. While most fluoroquinolones have activity against C. trachomatis, the clinical efficacy of ciprofloxacin is variable with a potential for persistence of the organism following treatment. In cases where doxycycline was prescribed, both the dose and duration of treatment were seen to be variable (Table 3).
Rates of C. trachomatis infection continue to increase with data showing that between 2003 and 2004 diagnoses of C. trachomatis in the UK rose by 8.6%.6 Data also showed that 56% of all diagnoses in men were in young men. Some of the rise in infection rates may reflect the use of more acceptable and sensitive tests, such as polymerase chain reaction (PCR).10 However, we must consider that the reported incidence is likely to be an underestimate as many chlamydial infections are asymptomatic. If left untreated. C. trachomatis infection can have major medical, social and economic consequences for both men and women.4 In cases of acute epididymo-orchitis caused by Chlamydia infection, the EAU guidelines affirm the importance of contact-tracing and treatment of sexual partners in order to prevent reinfection of the patient. A study of young men with acute epididymitis demonstrated that up to 80% of female partners screened tested positive for Chlamydia.2 It is, therefore, concerning that, in this study, a sexual history was documented as having been taken in only two-thirds of men aged ≤ 35 years, and verbal advice to attend a genitourinary medicine clinic was documented as given to only 42.3% of men aged ≤ 35 years.
A further concern is the lack of formal urological follow-up for older patients in whom risk factors such as bladder outlet obstruction may play a significant role in the aetiology of acute epididymo-orchitis. Of the 11 patients aged > 50 years (age range, 53–87 years), only three men in their 50s were referred for out-patient follow-up.
Junior staff of both the urology and emergency medicine departments routinely undertake the management of patients presenting with acute epididymo-orchitis via the emergency department. The results of this study show that the management of patients conforms to the EAU guidelines in only a minority of cases. Although a joint emergency department/urology clinical protocol already exists within the Trust, with paper copies available in the emergency department, this study demonstrates a lack of familiarity with the protocol and highlights problems associated with its implementation.
Clinical guidelines are systematically developed statements designed to help doctors and patients make decisions regarding appropriate healthcare for specific circumstances.11 Numerous different methods can be used to promote behavioural change among healthcare professionals and the implementation of research-based recommendations for the delivery of clinical care.12 There is accumulating evidence that different strategies used in the implementation of guidelines are associated with highly variable degrees of success.12–14 In their review of the literature, Bero and colleagues14 concluded that the passive dissemination of information, which includes the distribution of clinical practice guidelines and the use of didactic teaching, was generally ineffective in altering clinical practice. Interestingly, passive approaches represent the most common form of guideline implementation methods used by healthcare organisations. Audit and feedback on clinical performance, together with local consensus processes, where participating doctors are involved in the development of local guidelines, were shown to be of variable effectiveness.14 Strategies found to be most effective in the implementation of guidelines include the use of manual or computerised reminders and interactive educational meetings.14 It has also been demonstrated that multifaceted intervention strategies, which include two or more of either audit and feedback, use of reminders and local consensus processes, are more effective than single interventions.13,15
In this study, the regular movement of junior staff through both the urology and emergency medicine departments was identified as one of the main issues impeding the successful implementation of clinical guidelines on the management of acute epididymo-orchitis. This regular movement of staff necessitates that the distribution of management protocols and clinical practice guidelines occurs at frequent intervals throughout the year and that their implementation is continuously monitored so that, if necessary, further interventional strategies can be employed.
Conclusions
The results of this study show that the management of men of all age groups presenting with acute epididymo-orchitis conforms to the EAU guidelines, which forms the basis of this Trust's established clinical protocol, in only a minority of cases. With the current emphasis on evidence-based practice, the development of local clinical practice guidelines has become prevalent. However, as this study demonstrates, the successful implementation of such guidelines can be difficult to achieve. The use of local rather than national guidelines, in conjunction with the peripatetic lives of clinicians, leads to difficulties in altering established clinical practice. Successful implementation of guidelines requires the knowledge and use of effective methods in the dissemination of information and recognition of the potential barriers to change.
References
- 1.Nistel M, Paniagua R. Testicular and epididymal pathology. New York: Thieme-Stratton; 1984. [Google Scholar]
- 2.Robinson AJ, Grant JBF, Spencer RC, Potter C, Kinghom GR. Acute epididymitis: why patient and consort must be investigated. Br J Urol. 1990;66:642. doi: 10.1111/j.1464-410x.1990.tb07200.x. [DOI] [PubMed] [Google Scholar]
- 3.Weidner W, Scheifer HG, Garbe C. Acute nongonococcal epididymitis. Aetiological and therapeutic aspects. Drugs. 1987;34(Suppl 1):111. doi: 10.2165/00003495-198700341-00024. [DOI] [PubMed] [Google Scholar]
- 4.Stephenson JM. Screening for genital chlamydial infection. Br Med Bull. 1998;54:891–902. doi: 10.1093/oxfordjournals.bmb.a011736. [DOI] [PubMed] [Google Scholar]
- 5.De Jong Z, Pontonnier F, Plante P, Gautier JR, Ioualalen A, Archambaud M, et al. The frequency of Chlamydia trachomatis in acute epididymitis. Br J Urol. 1988;62:76–8. doi: 10.1111/j.1464-410x.1988.tb04271.x. [DOI] [PubMed] [Google Scholar]
- 6.Health Protection Agency Centre for Infections. Mapping the issues, HIV and other Sexually Transmitted Infections in the United Kingdom: 2005. London: Health Protection Agency Centre for Infections; 2005. [Google Scholar]
- 7.Information and Statistics Division. Setting the Scene, Sexually Transmitted Infections, Including HIV, in Scotland, 2004. Edinburgh: Information and Statistics Division Scotland Publications; 2005. [Google Scholar]
- 8.Naber KG, Bergman B, Bishop MC, Bjerklund-Johansen TE, Botto H, Lobel B, et al. EAU guidelines for the management of urinary and male genital tract infections. Eur Urol. 2001;40:576–88. doi: 10.1159/000049840. [DOI] [PubMed] [Google Scholar]
- 9.Jalal H, Stephen H, Al-Suwaine A, Sonnex C, Carne C. The superiority of polymerase chain reaction over an amplified enzyme immunoassay for the detection of genital chlamydial infections. Sex Transm Infect. 2006;82:37–40. doi: 10.1136/sti.2005.015362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burckhardt F, Warner P, Young H. What is the impact of change in diagnostic test method on surveillance data trends in Chlamydia trachomatis infection? Sex Transm Infect. 2006;82:24–30. doi: 10.1136/sti.2004.011882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Field MJ, Lohr KN, editors. Guidelines for clinical practice. From development to use. Washington, DC: National Academy Press; 1992. [PubMed] [Google Scholar]
- 12.Lomas J, Anderson GM, Domnick-Pierre K, Vayda E, Enkin MW, Hannah WJ. Do practice guidelines guide practice? N Engl J Med. 1989;321:1306–11. doi: 10.1056/NEJM198911093211906. [DOI] [PubMed] [Google Scholar]
- 13.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance: a systematic review of the effect of continuing medical education strategies. JAMA. 1995;274:700–5. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- 14.Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson A. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. BMJ. 1998;317:465–8. doi: 10.1136/bmj.317.7156.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wensing M, Grol R. Single and combined strategies for implementing changes in primary care: a literature review. Int J Quality Health Care. 1994;6:115–32. doi: 10.1093/intqhc/6.2.115. [DOI] [PubMed] [Google Scholar]