Abstract
INTRODUCTION
Appendicectomy is by far the commonest major emergency general surgical operation and laparoscopic appendicectomy is now becoming common. The question of whether a normal-looking appendix should be removed laparoscopically is more pertinent than ever before.
PATIENTS AND METHODS
A retrospective study was undertaken to review the histopathology results and compare macroscopic with microscopic descriptions of all patients who underwent an appendicectomy, either by open surgery or laparoscopically, over a 1-year period from 1 September 2004 to 31 August 2005.
RESULTS
A total of 199 appendicectomies were carried out in the year of which histopathology results for 190 could be retrieved. Of the 190 who had an appendicectomy, 110 (57.9%) were female and 80 (42.1%) were male. While appendicitis was confirmed histologically in 65 of 80 (81.2%) male patients, it could only be confirmed histologically in 57 of 110 (51.8%) female patients. However, in a large number of female patients in whom macroscopically normal appendices had been removed, other findings were noted including fibro-obliterative changes in 10, luminal inflammation in 6, serositis in 5, lymphoid hyperplasia in 3, feacoliths in 2, and pinworm in 1, making another abdominal pathology a possibility.
CONCLUSIONS
The number of macroscopically normal appendices removed was much larger in female patients. However in 27 of 49 normal looking appendices in females, findings such as serositis, luminal inflammation, lymphoid hyperplasia, etc. were noted on histology, suggesting that another abdominal pathology may have been missed or the appendix may still have been the cause for pain. On the basis of these findings, we suggest that diagnostic laparoscopy should be performed at least in all female patients before an appendicectomy; if no other findings are noted on laparoscopy, it is likely to be worthwhile to remove the appendix.
Keywords: Appendicitis, Laparoscopy, Histology
Appendicectomy is by far the commonest major emergency general surgical operation. All surgeons have at some stage in their careers faced the prospect of a normal-looking appendix following appendicectomy incision. After struggling to identify any other possibility by trying to catch a glimpse of the tubes and ovaries, and extruding the bowel through that incision, the diagnostic dilemma has remained, whether to remove that appendix or not. Although studies exist both supporting1,2 and opposing3 the removal of a macroscopically normal appendix, it has largely remained the surgeon's predilection. Now that laparoscopic appendicectomy is in vogue, the question becomes more pertinent than ever before – should a normal looking appendix be removed laparoscopically or not? The aim of this study was to attempt an answer to this question.
Patients and Methods
A retrospective study was undertaken to review the histopathology results and compare macroscopic with microscopic descriptions of all patients who underwent an appendicectomy whether carried out by open surgery or laparoscopically over a 1-year period from 1 September 2004 to 31 August 2005. The data for male and female patients were tabulated separately.
Results
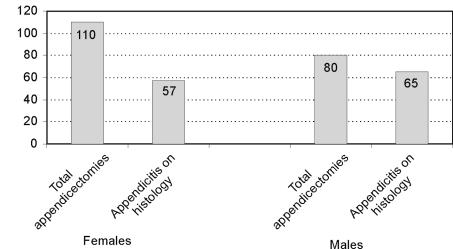
A total of 199 appendicectomies were carried out in the year, from which histopathology results for 190 could be retrieved. Of the 190 patients who had an appendicectomy, 110 (57.9%) were female and 80 (42.1%) were male (Fig. 1)
Figure 1.
Summary of the 190 patients who had an appendicectomy and for whom histopathology results could be retrieved.
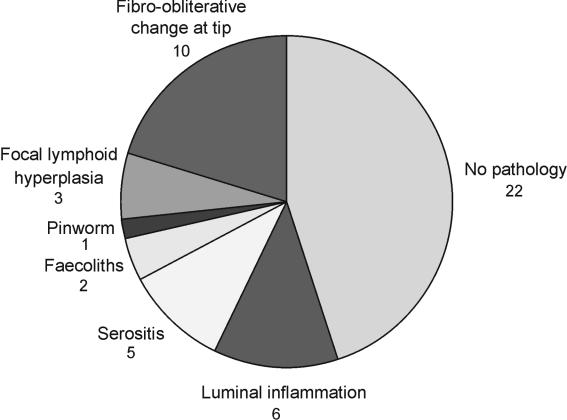
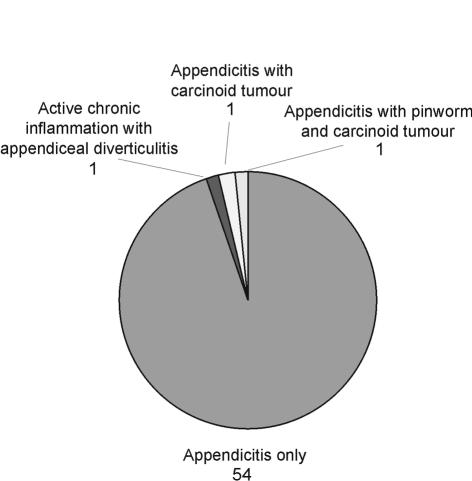
While appendicitis was confirmed histologically in 65 of 80 (81.2%) male patients, it was confirmed histologically in only 57 of 110 (51.8%) female patients. However, in a large number of female patients in whom macroscopically normal appendices had been removed, other findings were noted including fibro-obliterative changes in 10, luminal inflammation in 6, serositis in 5, lymphoid hyperplasia in 3, feacoliths in 2, and pinworm in 1 (Fig. 2). In all female patients in whom appendicitis was noted macroscopically, the appendix was inflamed histologically as well, with 1 patient having appendicitis with a carcinoid tumour, 1 with both carcinoid tumour and a pin-worm, and 1 showing active chronic inflammation within appendiceal diverticulitis (Fig. 3).
Figure 2.
Distribution of histology in macroscopically normal appendices in females.
Figure 3.
Distribution of histology in macroscopically inflamed appendices in females.
The age distribution of female patients with macroscopically normal appendices did not confirm to any particular age group with two exceptions – lymphoid hyperplasia (seen only in teenagers) and fibro-obliterative changes occurring more often in an older age group (Table 1).
Table 1.
Age distribution of microscopic findings in normal-looking appendices in females
| Microscopic finding | n | Age range (years) | Mean age (years) | SD |
|---|---|---|---|---|
| No pathology | 22 | 14–60 | 25.18 | 13.07 |
| Luminal inflammation | 6 | 13–49 | 23 | 14.08 |
| Serositis | 5 | 15–55 | 40 | 17.06 |
| Faecoliths | 2 | 16–52 | 34 | 25.4 |
| Pinworm | 1 | 16 | 16 | |
| Focal lymphoid hyperplasia | 3 | 14–19 | 16 | 2.64 |
| Fibro-obliterative change | 10 | 22–68 | 39.1 | 13.2 |
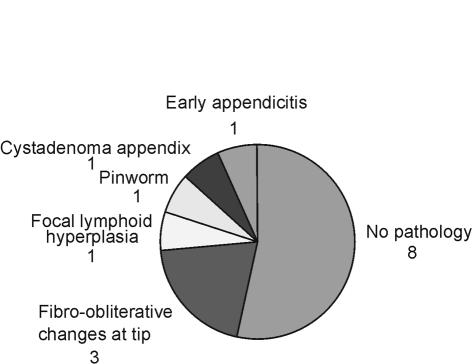
Of the 15 male patients in whom the appendix was noted to be macroscopically normal, 1 had early appendicitis on histology, and 6 had other findings with fibro-obliterative change in 3, focal lymphoid hyperplasia in 1, a cystadenoma in 1, and a pin-worm in 1 (Fig. 4). In all 64 male patients who were noted to have appendicitis macroscopically, appendicitis was confirmed on histology as well with 2 patients having pinworms in addition, and 1 having a mucinous adenocarcinoid tumour (Fig. 5).
Figure 4.
Distribution of histology in macroscopically normal appendices in males.
Figure 5.
Distribution of histology in macroscopically inflamed appendices in males.
Of note, the age distribution of male patients with macroscopically normal appendices again had focal lymphoid hyperplasia in a 12-year-old, and fibro-obliterative changes occurring in a relatively older age group (Table 2).
Table 2.
Age distribution of microscopic findings in normal-looking appendices in males
| Microscopic finding | n | Age range (years) | Mean age (years) | SD |
|---|---|---|---|---|
| No pathology | 8 | 16–66 | 27.8 | 16 |
| Fibro-obliterative changes at tip | 3 | 28–41 | 33.6 | 6.6 |
| Focal lymphoid hyperplasia | 1 | 12 | 12 | |
| Pinworm | 1 | 16 | 16 | |
| Cystadenoma appendix | 1 | 57 | 57 | |
| Early appendicitis | 1 | 24 | 24 |
Discussion
The number of macroscopically normal appendicectomies was much larger in female patients as has been noted in other studies.4 However, in 27 of 49 (55.1%) normal-looking appendices in females, there were other findings on histology. While 6 patients had luminal inflammation, 5 had serositis, making another abdominal pathology a good possibility. Serositis or peri-appendicitis has been noted to occur in numerous other studies1,5 and is thought to represent extra-appendicular sepsis.6 Although one should be wary of Crohn's disease in cases with just luminal inflammation, Crohn's is seen to have differential characteristics on histology.7
A large number of patients including 10 females and 3 males were found to have fibro-obliterative changes, often at the tip of the appendix. The significance of fibro-obliterative change of the appendix remains uncertain although it has been reported to occur with acute appendicitis in a few case series.1,5 In our study, fibro-obliterative change on histology was found in a relatively older age group, with a mean age of 39.1 years in females and 33.6 years in males, respectively. However, little data exist to define this entity. Lymphoid hyperplasia was found in 3 female patients and 1 male patient on histology in macroscopically normal appendices. Lymphoid hyperplasia has been noted to occur in up to 25% of patients with acute appendicitis8 and appendicectomy in patients having just lymphoid hyperplasia on histology has been seen to relieve pain.1,2,9
In our study, pinworm was found to occur in teenage children both with and without evidence of acute appendicitis. Pinworm has been reported to occur on histology in some large series ranging from 1.4–4.1%,10–12 with evidence to suggest that it may be the cause of abdominal pain mimicking appendicitis without causing appendicitis. Similarly, luminal obstruction with faecoliths, etc. is known to occur in the aetiology of appendicitis.2,8
In our study, appendicitis was noted to occur in association with a carcinoid tumour in 2 patients, and a mucinous adeno-carcinoid tumour in 1 patient. Up to 12% of carcinoid tumours occur in the appendix,13 although carcinoid in itself remains a small cause of appendicitis and has been noted to have a good prognosis with up to 98% 5-year survival after an appendicectomy13,14 There have been few case reports of adenocarcinomas of the appendix since it is a rarely seen tumour 15.
While the on-table diagnostic accuracy of surgeons in diagnosing appendicitis has been noted to be low16 and studies show that, especially in children, appendiceal colic is likely to occur,17 data from our study further questions the wisdom of leaving behind a normal-looking appendix if no other pathology is evident.
Conclusions
On the basis of our findings, we suggest that a diagnostic laparoscopy should be performed, at least in all female patients, before an appendicectomy; if no other findings are noted on laparoscopy, it is likely to be worthwhile to remove the appendix. However, larger studies are needed to support this view.
References
- 1.Lyons TL, Winer WK, Woo A. Appendectomy in patients undergoing laparoscopic surgery for pelvic pain. J Am Assoc Gynecol Laparosc. 2001;8:542–4. doi: 10.1016/s1074-3804(05)60618-4. [DOI] [PubMed] [Google Scholar]
- 2.Panchalingam L, Driver C, Mahomed AA. Elective laparoscopic appendicectomy for chronic right iliac fossa pain in children. J Laparoendosc Adv Surg Tech A. 2005;15:186–9. doi: 10.1089/lap.2005.15.186. [DOI] [PubMed] [Google Scholar]
- 3.Schreiber HW, Otto HF, Koch G, Kortmann KB. Surgical diseases of the veri-form appendix. Chirurg. 1978;49:679–83. [PubMed] [Google Scholar]
- 4.Chang AR. An analysis of the pathology of 3003 appendices. Aust NZ J Surg. 1981;51:169–78. doi: 10.1111/j.1445-2197.1981.tb05932.x. [DOI] [PubMed] [Google Scholar]
- 5.Harris RS, Foster WG, Surrey MW, Agarwal SK. Appendiceal disease in women with endometriosis and right lower quadrant pain. J Am Assoc Gynecol Laparosc. 2001;8:536–41. doi: 10.1016/s1074-3804(05)60617-2. [DOI] [PubMed] [Google Scholar]
- 6.Mukherjee A, Schlenker E, LaMasters T, Johnson M, Brunz J, Thomas E. Periappendicitis: is it a clinical entity? Am Surg. 2002;68:913–6. [PubMed] [Google Scholar]
- 7.Stangl PC, Herbst F, Birner P, Oberhuber G. Crohn's disease of the appendix. Virchows Arch. 2002;440:397–403. doi: 10.1007/s004280100532. [DOI] [PubMed] [Google Scholar]
- 8.Babekir AR, Devi N. Analysis of the pathology of 405 appendices. East Afr Med J. 1990;67:599–602. [PubMed] [Google Scholar]
- 9.Jona JZ, Belin RP, Burke JA. Lymphoid hyperplasia of the bowel and its surgical significance in children. J Pediatr Surg. 1976;11:997–1006. doi: 10.1016/s0022-3468(76)80080-2. [DOI] [PubMed] [Google Scholar]
- 10.Arca MJ, Gates RL, Groner JI, Hammond S, Caniano DA. Clinical manifestations of appendiceal pinworms in children: an institutional experience and a review of the literature. Pediatr Surg Int. 2004;20:372–5. doi: 10.1007/s00383-004-1151-5. [DOI] [PubMed] [Google Scholar]
- 11.Budd JS, Armstrong C. Role of Enterobius vermicularis in the aetiology of appendicitis. Br J Surg. 1987;74:748–9. doi: 10.1002/bjs.1800740834. [DOI] [PubMed] [Google Scholar]
- 12.Wiebe BM. Appendicitis and Enterobius vermicularis. Scand J Gastroenterol. 1991;26:336–8. doi: 10.3109/00365529109025051. [DOI] [PubMed] [Google Scholar]
- 13.Modlin IM, Kidd M, Latich I, Zikusoka MN, Shapiro MD. Current status of gas-trointestinal carcinoids. Gastroenterology. 2005;128:1717–51. doi: 10.1053/j.gastro.2005.03.038. [DOI] [PubMed] [Google Scholar]
- 14.Zeng QA, Pan HY, Xiong DF, Mo HS. Clinical features and treatment principles of appendix carcinoid tumor: a report of 13 cases. Ai Zheng. 2004;23(Suppl):1582–4. [PubMed] [Google Scholar]
- 15.Smejkal P, Pazdro A, Smejkal M, Pafko P, Frantlova M. The cystadenocarcinoma of the appendix. Rozhl Chir. 2005;84:33–6. [PubMed] [Google Scholar]
- 16.Shum CF, Lim JF, Soo KC, Wong WK. On-table diagnostic accuracy and the clinical significance of routine exploration in open appendectomies. Asian J Surg. 2005;28:257–61. doi: 10.1016/S1015-9584(09)60356-0. [DOI] [PubMed] [Google Scholar]
- 17.Gorenstin A, Serour F, Katz R, Usviatsov I. Appendiceal colic in children: a true clinical entity? J Am Coll Surg. 1996;182:246–50. [PubMed] [Google Scholar]