Abstract
BACKGROUND
Patient satisfaction is increasingly recognized as a quality indicator and important outcome of care. Little is known about the clinical factors associated with satisfaction after myocardial infarction (MI).
OBJECTIVE
To assess the hypothesis that angina after MI is independently associated with lower treatment satisfaction.
METHODS
We evaluated 1,815 MI patients from 19 U.S. centers. Angina was measured at 1 and 6 months after MI using the Seattle Angina Questionnaire (SAQ). Treatment satisfaction was measured using the SAQ at 6 months. Multivariable regression was used to evaluate the association between 1- and 6-month angina and 6-month treatment satisfaction.
RESULTS
Sixty-two percent of patients had no angina at 1 and 6 months after MI, 14% had transient angina (angina at 1 month, no angina at 6 months), 11% had new angina (angina at 6 months only), and 13% had persistent angina (angina at both 1 and 6 months). In unadjusted analysis, the presence of angina at 6 months, whether new or persistent, was associated with lower treatment satisfaction (p < 0.001). In multivariable analysis, angina was associated with lower treatment satisfaction [relative risk (RR) 2.9, 95%confidence interval (CI) 2.4–3.5 patients with new angina; RR 3.1, 95%CI 2.5–3.9 patients with persistent angina, vs patients with no angina].
CONCLUSIONS
In conclusion, angina in the 6 months following MI is present in almost 1 in 4 patients and is strongly associated with lower treatment satisfaction. This suggests the importance of angina surveillance and management after MI as a possible target to improve treatment satisfaction and, thereby, quality of care.
KEY WORDS: angina, treatment satisfaction, myocardial infarction
BACKGROUND
Patient satisfaction is considered a marker of effectiveness of health care delivery and is often used as a benchmark of health system performance.1–4 Patient satisfaction has been shown to be influenced by physician communication skills, age and gender of the physician, patient expectations, and length of relationship with the physician.5,6 There is increasing interest in the potential influence of a patient’s clinical condition on their satisfaction with care.7,8
Little is known about what influences treatment satisfaction among patients who have experienced an acute myocardial infarction (MI). One important aspect of a patient’s clinical condition post-MI is the presence of angina. A previous study conducted in the Veterans Health Administration in 1998–1999 found that current angina symptoms were associated with current treatment satisfaction after controlling for baseline patient characteristics,8 thus suggesting that a potential target for improving satisfaction includes better angina management. Recurrent or persistent angina symptoms post-MI may be viewed by patients as having received less than optimal care. Because the association between angina in the months following MI and patient treatment satisfaction in contemporary practice is unknown, we sought to investigate whether active angina symptoms in the months after MI are associated with decreased treatment satisfaction.
The objectives of this study were to describe the prevalence of active angina symptoms (angina symptoms over the previous 4 weeks) after MI and to evaluate whether the presence of angina in the months following MI was associated with treatment satisfaction in a multicenter cohort. Our hypothesis was that active angina after MI is independently associated with lower treatment satisfaction after adjustment for baseline patient characteristics, MI treatment, and site. Because angina is potentially treatable, the results of this study may suggest that improved angina management after MI is a target for improving patient treatment satisfaction.
METHODS
Study Population
The patient population for this study was from the “Prospective Registry Evaluating Myocardial Infarction: Events and Recovery” (PREMIER) study, which included consecutive patients hospitalized with AMI from 19 U.S. hospitals between January 1, 2003, and June 28, 2004. Patients with a positive troponin test or elevated creatine phosphokinase-MB fractions were screened for study inclusion. Eligibility requirements included age ≥18 years, elevated cardiac biomarkers, and presentation to the enrolling institution (or transferred) within the first 24 hours of symptom onset. Exclusion criteria included incarcerated patients and patients without a preexisting MI whose elevated cardiac biomarkers were followed by a revascularization procedure.9 The total enrollment consisted of 2,498 patients, of whom 2,481 survived their hospitalization. Of these, 102 patients died prior to the 6-month assessment, 164 patients were too ill or refused to be interviewed, 349 patients were lost to follow-up, and 68 did not have complete data on angina frequency or treatment satisfaction at follow-up. After excluding such patients, the cohort for this study was comprised of 1,815 patients. Institutional Research Board approval was obtained at each participating institution.
Variables
Angina frequency and patient treatment satisfaction were measured using the Seattle Angina Questionnaire (SAQ). The SAQ was administered at 1 month and 6 months after MI hospitalization. The SAQ is a 19-item self-administered disease-specific questionnaire that is valid, reliable, sensitive to clinical changes, and prognostic of clinical events in patients with coronary artery disease.10,11 The SAQ measures anginal stability, physical limitation, and disease perception, in addition to the principal variables of interest in this study, angina frequency and treatment satisfaction. The SAQ angina frequency scale is scored 0–100, with higher scores indicating less angina. The scale asks patients to report the average frequency of their angina over the preceding 4 weeks. The SAQ treatment satisfaction scale is scored from 0 to 100, with higher scores indicating higher satisfaction with treatment. The scale incorporates patients’ ratings of satisfaction with explanations from their doctor, satisfaction that everything possible is being done, how bothersome is it to take their medications as prescribed, and overall satisfaction with current treatment.
Statistical Analysis
For this analysis, SAQ angina frequency scores were dichotomized as angina present versus absent based upon the distribution of scores in the study population at 6 months (daily angina 1.8%, weekly angina 8.0%, monthly angina 17.1%, and no angina 73.%). Then, a variable representing angina status (present or absent) at 1 and 6 months post-MI was created as follows: (1) no angina during follow-up (no angina at 1 and 6 months), (2) transient angina (angina at 1 month, not at 6 months), (3) new angina (no angina at 1 month, angina at 6 months), and (4) persistent angina (angina at both 1 and 6 months). In the primary analysis, the SAQ treatment satisfaction score was dichotomized as dissatisfied [those in the lowest quartile (<87.5)] versus satisfied [those in the upper 3 quartiles (>=87.5)]. As a secondary analysis, the treatment satisfaction score was also modeled as a continuous variable. The results of this analysis were similar to the primary analysis and are therefore not presented in this manuscript. Additionally, we repeated the analysis using only the question about overall treatment satisfaction, measured on a 5-point ordinal scale, comparing those who responded “completely satisfied” (76% of patients) with patients responding anything less than completely satisfied (24% of patients). Finally, we modeled each individual measure of treatment satisfaction as outcomes. Risk adjustment variables included the demographic, cardiac, noncardiac, hospitalization, and discharge medication variables listed in Table 1. For modeling, the scales of the continuous variables were converted for ease of interpretation. Those that were normally distributed were scaled per 1 standard deviation increase, creatinine was left as per 1 mg/dL increase, peak troponin is per +100 μg/mL, and patient health questionnaire score was scaled to +5 points, which denotes a 1-step increase in severity classification.
Table 1.
Characteristics of the Study Population
| Angina type (angina at 1/6 mo) | p value | ||||
|---|---|---|---|---|---|
| No angina (no/no) n = 1125 | Transient angina (yes/no) n = 258 | New angina (no/yes) n = 201 | Persistent angina (yes/yes) n = 231 | ||
| Demographic | |||||
| Age (mean +/− SD), years | 62.4 +/− 12.3 | 59.6 +/− 13.2 | 59.5 +/− 12.2 | 55.8 +/− 11.1 | <0.001 |
| Male gender (%) | 69.2 | 65.9 | 68.2 | 61.5 | 0.134 |
| Non-white race (%) | 17.3 | 24.3 | 26.5 | 26.4 | <0.001 |
| BMI (mean +/− SD) | 29.3 +/− 6.1 | 28.9 +/− 5.4 | 29.6 +/− 6.2 | 29.6 +/− 6.9 | 0.567 |
| Cardiac | |||||
| Prior MI (%) | 17.4 | 20.5 | 19.9 | 25.5 | 0.034 |
| Prior PCI (%) | 14.3 | 20.9 | 23.4 | 25.5 | <0.001 |
| Prior CABG (%) | 9.2 | 12.4 | 18.4 | 21.6 | <0.001 |
| CHF (%) | 8.5 | 5.8 | 10.9 | 10.8 | 0.149 |
| Noncardiac | |||||
| Diabetes mellitus (%) | 25.3 | 24.8 | 30.3 | 28.6 | 0.368 |
| Smoking status (%) | <0.001 | ||||
| Current (<30 d) | 28.6 | 39.1 | 35.0 | 40.8 | |
| Former (>=30 d) | 39.6 | 35.3 | 32.5 | 39.0 | |
| Never | 31.9 | 25.6 | 32.5 | 20.2 | |
| Hypertension (%) | 60.1 | 62.4 | 67.2 | 62.3 | 0.281 |
| Hypercholesterolemia (%) | 48.1 | 51.9 | 56.2 | 54.5 | 0.073 |
| Peripheral arterial disease (%) | 6.7 | 6.2 | 5.5 | 8.2 | 0.693 |
| Prior CVA/TIA (%) | 7.1 | 7.0 | 8.0 | 9.1 | 0.741 |
| PHQ depression score (mean +/− SD) | 4.4 +/− 4.8 | 5.8 +/− 5.0 | 6.3 +/− 5.4 | 8.8 +/− 6.3 | <0.001 |
| Hospitalization | |||||
| Presentation heart rate mean +/− SD | 80.2 +/− 22.1 | 77.5 +/− 16.2 | 79.4 +/− 19.3 | 80.3 +/− 19.5 | 0.266 |
| Presentation systolic blood pressure (mean +/− SD), mm Hg | 139.6 +/− 30.8 | 138.7 +/− 29.2 | 141.0 +/− 34.3 | 135.5 +/− 29.1 | 0.247 |
| Presentation diastolic blood pressure (mean +/− SD), mmHg | 78.4 +/− 19.0 | 76.1 +/− 18.8 | 79.1 +/− 19.9 | 76.6 +/− 18.1 | 0.171 |
| Initial creatinine (mean +/− SD), mg/dL | 1.5 +/− 1.4 | 1.4 +/− 1.6 | 1.5 +/− 1.7 | 1.3 +/− 1.0 | 0.464 |
| MI type | 0.052 | ||||
| STEMI | 48.2 | 51.6 | 45.3 | 39.8 | |
| NSTEMI | 51.8 | 48.4 | 54.7 | 60.2 | |
| TIMI STEMI risk score (mean +/− SD) | 3.3 +/− 2.2 | 3.0 +/− 2.0 | 3.2 +/− 2.2 | 2.8 +/− 1.8 | 0.251 |
| TIMI NSTEMI risk score (mean +/− SD) | 3.2 +/− 1.3 | 3.3 +/− 1.4 | 3.3 +/− 1.5 | 3.1 +/− 1.4 | 0.759 |
| Peak troponin (mean +/− SD) μg/mL | 90.1 +/− 236.6 | 75.9 +/− 227.9 | 63.8 +/− 171.4 | 53.0 +/− 164.9 | 0.084 |
| Cardiac catheterization (%) | 91.6 | 90.7 | 90.0 | 91.8 | 0.863 |
| Revascularization type (%) | <0.001 | ||||
| None | 21.1 | 23.3 | 25.9 | 33.8 | |
| PCI | 65.4 | 67.8 | 59.7 | 61.9 | |
| CABG surgery | 13.5 | 8.9 | 14.4 | 4.3 | |
| ICD (%) | 2.8 | 0.4 | 2.5 | 2.2 | 0.100 |
| Discharge medications | |||||
| Beta blocker (%) | 88.3 | 89.9 | 89.1 | 84.4 | 0.260 |
| ACE/ARB (%) | 74.1 | 74.8 | 70.1 | 80.1 | 0.117 |
| Statin (%) | 82.8 | 84.9 | 81.6 | 83.5 | 0.803 |
| Aspirin/antiplatelet (%) | 94.4 | 97.7 | 95.0 | 93.9 | 0.164 |
p values for comparison to no angina. Trend p < 0.001
ACE/ARB = angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers; BMI = body mass index; CABG = coronary artery bypass graft; CHF = chronic heart failure; CVA/TIA = cerebral vascular accident/transient ischemic attacks; ICD = implantable cardioverter–defibrillator; MI = myocardial infarction; NSTEMI = non-ST-segment elevation myocardial infarction; PCI = percutaneous coronary intervention; PHQ = patient health questionnaire; STEMI = ST-segment elevation myocardial infarction; TIMI = thrombolysis in myocardial infarction; no angina = no angina at 1 or 6 months; transient angina = angina at 1 month, not at 6 months; new angina = no angina at 1 month, angina at 6 months; persistent angina = angina at 1 and 6 months; SAQ = Seattle Angina Questionnaire
The baseline characteristics of patients with no angina at 1 or 6 months were compared to those with transient angina, new angina, and persistent angina. Next, the bivariate association between angina status and patient treatment satisfaction was analyzed using chi-squared or Fisher’s exact tests for categorical variables and t tests or Mann–Whitney tests for continuous variables. Multivariable regression models were then developed to determine whether angina status was independently associated with patient treatment satisfaction. Because the outcome (lowest quartile of the SAQ Treatment Satisfaction scale) was by definition not a rare event, relative risks (RRs) were modeled directly using modified Poisson regression models, rather than approximated using odds ratios from logistic regression.12 A series of models was created to assess the association between angina and treatment satisfaction with incremental adjustment for demographic, cardiac, noncardiac, hospitalization, and discharge medications variables as listed in Table 1. Site was included in the models as a random effect. Confidence intervals (CI) adjusted for multiple comparisons were used to evaluate the independent relationship between the 3 angina categories (transient, new, and persistent) and patient treatment satisfaction compared with the reference category (no angina at both 1 and 6 months). The adjustment for multiple comparisons was done using a simulation-based method that estimates the multivariate distribution of joint tests, thereby taking correlations between tests into account.13 In addition, a first-level interaction between depression and angina was evaluated in the multivariate model based on prior evidence of the association between depression and angina.14
Approximately 17% of patients were missing 1 or more baseline covariate values (only 3% were missing more than 1 value). Multiple imputation methods were used in the primary analysis to impute these covariate values on the basis of observed data and to account for missingness in statistical inferences.15,16 In addition, multiple imputation methods were also used in a secondary analysis to examine potential bias because of lost follow-up, imputing baseline covariate values as well as missing follow-up SAQ angina frequency and treatment satisfaction scores. The imputation model included all Table 1 variables; SAQ scores at baseline, 1 month, and 6 months; and whether patients were hospitalized or died during follow-up. These analyses were virtually identical to the primary results, suggesting that the results observed were applicable to the overall study population. All analyses were done using SAS version 9.1 (SAS Institute, Cary, NC, USA).
RESULTS
Of the 1,815 patients in the study, 62% had no angina at 1 or 6 months, 14% had transient angina, 11% had new angina, and 13% had persistent angina after MI. Thus, 24% of the cohort had active angina symptoms 6 months after the MI hospitalization. Patients with no angina at 1 month or 6 months were more likely to be older, to be white, and to have been revascularized during the index hospitalization. They were less likely to have had prior MI, to have had prior PCI, to have had prior CABG, to be a current smoker, and to have severe depression (Table 1). Treatment satisfaction scores averaged 91.5 and ranged from 12.5 to 100. The median treatment satisfaction score was 100, and the lower quartile was 87.5.
Unadjusted Association
Figure 1 demonstrates the association between post-MI angina and treatment satisfaction. First, there was a significant trend toward worse treatment satisfaction with a greater presence of angina (p < 0.001). Patients with no angina or transient angina averaged treatment satisfaction scores of 95 and 93, whereas those with new angina had an average score of 84 and persistent angina, 80. A change of 5 points or more is considered clinically significant.10 Second, the presence of active angina at 6 months, whether new or persistent, was associated with significantly worse treatment satisfaction (p < 0.001).
Figure 1.
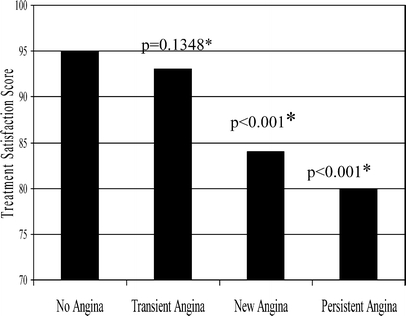
Angina versus SAQ treatment satisfaction score
Risk-Adjusted Associations
Prior to adding angina, a treatment satisfaction model was developed with the demographic, cardiac, noncardiac, hospitalization, and discharge medication variables listed in Table 1. Being younger and of non-white race and having a prior PCI, a more severe depression score, and a higher systolic blood pressure at hospital presentation were significantly associated with worse treatment satisfaction. After adding angina status, having a prior PCI, more severe depression, and higher systolic blood pressure at hospital presentation remained significant in the model; however, their magnitude of association was smaller than angina status during follow-up. The RRs for the angina types for each incremental model are presented in Table 2. In the final multivariable model, after adjustment for patient demographic, clinical and treatment variables, and site, patients with transient angina were 1.2 times (RR 95%CI, 0.8–1.8) more likely to be dissatisfied, patients with new angina were 2.9 times (RR 95%CI, 2.4–3.5) more likely to be dissatisfied, and patients with persistent angina were 3.1 times (RR 95% CI, 2.5–3.9) more likely to be dissatisfied as compared to patients with no angina. The interaction term between depression and angina was not significant in the model, indicating that the association between angina and patient treatment satisfaction was not modified by depression. The results of the secondary analysis, which included modeling the single question about overall treatment and modeling each individual measure of satisfaction, showed a similar pattern to that of the primary analysis. Specifically, patients with persistent angina were 2.7 (2.3–3.2) times more likely to be dissatisfied that everything possible is being done for them; were 2.3 (1.9–2.6) times more likely to report dissatisfaction with the explanations given; were 3.0 (2.4–3.7) times more likely to report dissatisfaction with current treatment; and, finally, were 2.1(1.6–2.7) times more likely to report that it was bothersome for them to take their pills.
Table 2.
Multivariable Risk Models
| Angina status | Unadjusted RRs | RRs adjusted for baseline demographic and clinical characteristics | RRs adjusted for demographic, clinical and treatment characteristics | RRs adjusted for demographic, clinical, treatment characteristics and site adjustment |
|---|---|---|---|---|
| No angina (ref.) | – | – | – | – |
| Transient angina | 1.3 (0.9–1.8) | 1.1 (0.8–1.6) | 1.1 (0.8–1.6) | 1.2 (0.80–1.8) |
| New angina | 3.2 (2.5–3.9) | 3.0 (2.3–3.7) | 3.0 (2.3–3.7) | 2.9 (2.4–3.5) |
| Persistent angina | 3.7 (3.1–4.4) | 3.3 (2.6–4.4) | 3.3 (2.6–4.0) | 3.1 (2.5–3.9) |
DISCUSSION
The objectives of this study were to describe the prevalence of angina in the months following MI and to evaluate whether the presence of active angina after MI was associated with patient treatment satisfaction. We found that, as the presence of angina increased from transient (angina at 1 month, not at 6 months) to new (no angina at 1 month, angina at 6 months) to persistent angina (angina at both 1 and 6 months), patients were at incrementally higher risk of being dissatisfied with their treatment. This association between angina and treatment satisfaction persisted after risk adjustment for a wide range of patient demographic, cardiac, noncardiac, hospitalization, and discharge medication variables.
These results expand the previous literature in several ways. First, little is known about the prevalence of angina in the months after acute MI. In this study, nearly one-quarter of patients had angina 6 months after MI discharge. This finding is consistent with prior studies suggesting chronic angina is undertreated in clinical practice.17,18 However, it is surprising that the prevalence of angina is so high so soon after hospitalization for a cardiac event in an era of early invasive treatment. Angina has been shown to be predictive of subsequent mortality and cardiac events and is associated with diminished functional status and quality of life.19–21 Moreover, angina is treatable through a wide range of pharmacologic treatments, as well as coronary revascularization. In practice, angina symptoms need to be identified through communication between the patient and physician, and the physician needs to have a full understanding of treatments available. The results of this study suggest the need for improved post-MI surveillance and treatment of recurrent or persistent angina.
This study broadens our understanding of the correlates of patient treatment satisfaction after MI, which are poorly understood despite the fact that the Institute of Medicine and others have suggested the importance of patient satisfaction as a marker of healthcare quality.22–24 Whereas some health care systems, such as Kaiser Permanente and the Veterans Health Administration, routinely assess patient satisfaction as a quality indicator,25,26 little information exists about patient factors associated with greater or lesser satisfaction after an MI. One previous study performed in 1998–1999 reported a cross-sectional association between angina and patient satisfaction 7 months after ACS in a cohort of veterans.8 However, that study was cross-sectional and performed prior to the era of early intervention, reporting PCI rates of 12.6% during hospitalization versus the in-hospital PCI rates in the current study cohort of 64.5%. The current study, which had a broader representation of patients and longitudinal assessment of angina, provides evidence that active angina is a strong correlate of patient treatment satisfaction. Furthermore, we found that depression was independently associated with treatment satisfaction, but did not modify the relationship between angina and treatment satisfaction. Prior studies have found that depression post-MI was associated with higher mortality, rehospitalization, and more frequent angina,27,28 thus highlighting the need for further investigation of the possible interrelationship between angina symptoms, depressive symptoms, and treatment satisfaction. Overall, these findings contribute to the broader patient satisfaction literature, adding evidence that patients’ clinical condition is a key driver of their satisfaction with care.
Understanding the association between angina and patient treatment satisfaction may have implications for improvement of other aspects of care. For example, prior studies have found that satisfied patients are more likely to stay within a health care system, more likely to remain enrolled in the same HMO, and more likely to maintain a relationship with their physician.5,6,29,30 Thus, improving patient satisfaction may lead to better longitudinal care and management of patients. The results of this study suggest the importance of symptom management after MI with regard to patient treatment satisfaction.
The directionality of association between angina and patient treatment satisfaction found in this study cannot be conclusively determined. As was our a priori hypothesis, it is possible that active angina symptoms lead to decreased treatment satisfaction, which has been supported in the satisfaction literature showing associations between clinical factors and satisfaction.7,8 Conversely, it is possible that dissatisfied patients are less compliant with their medical therapy, potentially including antianginal medications, with dissatisfaction thereby leading to more angina. It has been shown that interventions to improve patient satisfaction, such as greater patient involvement in treatment plans, can improve patient adherence to medications.31,32 However, among this cohort, satisfied and dissatisfied patients 6 months posthospitalization reported equal antianginal medication use. Furthermore, when 6-month medication variables (beta-blockers, angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers, aspirin, nitrates, calcium-channel blockers, and statins) were added to the final model, none were significant and the association between angina and treatment satisfaction remained strong. In addition, patients who were revascularized during their index hospitalization had less angina and were more satisfied. This latter fact must be interpreted with caution given probable selection bias in who undergoes revascularization. Taken together, however, all of these factors support that active angina leads to lower satisfaction.
There are several potential limitations of the study. First, as with all observational studies, there is a possibility of unmeasured confounding. However, we were able to adjust for a wide array of demographic, cardiac, noncardiac, hospitalization, and discharge medication variables. Second, there is potential selection bias from those who did return follow-up surveys. However, the survey completion rate was >70%, and multiple imputation methodology was employed to evaluate for potential bias, without evidence of any such bias having been introduced. Still, because multiple imputation has limitations, such as assuming that missingness of a variable is unrelated to its value, the results of this investigation should be replicated in other studies. It should also be noted that this study was focused on patient satisfaction with treatment for their heart disease. The findings may therefore have limited generalizability to broader constructs of patient satisfaction.
In conclusion, this study found that angina in the 6 months after MI is prevalent and a strong correlate of patient treatment satisfaction. Increased surveillance for angina may be an important aspect of post-MI care. Future studies should evaluate whether improved angina recognition and treatment after MI can improve both traditional clinical outcomes and patient satisfaction, and thereby improve quality of care.
Acknowledgement
This project was principally supported by CV Therapeutics and R-01 HS11282-01 from the Agency for Healthcare Research and Quality. Dr. Barry is supported by National Institute on Aging training grant T32AG019134.
Conflict of Interest None disclosed.
References
- 1.Aharony L, Strasser S. Patient satisfaction: what we know about and what we still need to explore. Med Care Rev. 1993;50:49–79. [DOI] [PubMed]
- 2.Dean Beaulieu N, Epstein AM. National Committee on Quality Assurance health-plan accreditation: predictors, correlates of performance, and market impact. Med Care. 2002;40:325–37. [DOI] [PubMed]
- 3.Wolosin RJ. The voice of the patient: a national, representative study of satisfaction with family physicians. Qual Manag Health Care. 2005;14:155–64. [PubMed]
- 4.Spoeri RK, Ullman R. Measuring and reporting managed care performance: lessons learned and new initiatives. Ann Intern Med. 1997;127:726–32. [DOI] [PubMed]
- 5.Forrest CB, Shi L, von Schrader S, Ng J. Managed care, primary care, and the patient–practitioner relationship. J Gen Intern Med. 2002;17:270–7. [DOI] [PMC free article] [PubMed]
- 6.Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients’ trust in their physicians: effects of choice, continuity, and payment method. J Gen Intern Med. 1998;13:681–6. [DOI] [PMC free article] [PubMed]
- 7.Fan VS, Reiber GE, Diehr P, Burman M, McDonell MB, Fihn SD. Functional status and patient satisfaction. J Gen Intern Med 2005;20:452–9. [DOI] [PMC free article] [PubMed]
- 8.Beinart SC, Sales AE, Spertus JA, Plomondon ME, Every NR, Rumsfeld JS. Impact of angina burden and other factors on treatment satisfaction after acute coronary syndromes. Am Heart J. 2003;146:646–52. [DOI] [PubMed]
- 9.Spertus JA, Peterson ED, Rumsfeld JS, Jones PG, Decker C, Krumholz H. Cardiovascular Outcomes Research Consortium. The Prospective Registry Evaluating Myocardial Infarction: Events and Recovery (PREMIER)—evaluating the impact of myocardial infarction on patient outcomes. Am Heart J. 2006;151:589–97. [DOI] [PubMed]
- 10.Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Fihn SD. Monitoring the quality of life in patients with coronary artery disease. Am J Cardiol. 1994;74:1240–4. [DOI] [PubMed]
- 11.Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonell M, Fihn SD. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–41. [DOI] [PubMed]
- 12.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. [DOI] [PubMed]
- 13.Westfall P, Tobias R, Rom D, Wolfinger R, Hochberg Y. Multiple Comparisons and Multiple Tests Using SAS. Cary: SAS; 1999.
- 14.Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA 2003;290:215–21. [DOI] [PMC free article] [PubMed]
- 15.Rubin D. Multiple Imputation for Non-response in Surveys. New York: Wiley; 1987.
- 16.Taylor JM, Cooper KL, Wei JT, Sarma AV, Raghunathan TE, Heeringa SG. Use of multiple imputation to correct for nonresponse bias in a survey of urologic symptoms and African-American men. Am J Epidemiol. 2002;156:774–82. [DOI] [PubMed]
- 17.Carasso S, Markiewicz W. Medical treatment of patients with stable angina pectoris referred for coronary angiography: failure of treatment or failure to treat. Clin Cardiol. 2002;25:436–41. [DOI] [PMC free article] [PubMed]
- 18.Wiest FC, Bryson CL, Burman M, McDonell MB, Henikoff JG, Fihn SD. Suboptimal pharmacotherapeutic management of chronic stable angina in the primary care setting. Am J Med. 2004;117:234–41. [DOI] [PubMed]
- 19.Kim J, Henderson RA, Pocock SJ, Clayton T, Sculpher MJ, Fox KA. Health-related quality of life after interventional or conservative strategy in patients with unstable angina or non-ST-segment elevation myocardial infarction: one-year results of the third Randomized Intervention Trial of unstable Angina (RITA-3). J Am Coll Cardiol. 2005;45:221–8. [DOI] [PubMed]
- 20.Dougherty CM, Dewhurst T, Nichol WP, Spertus J. Comparison of three quality of life instruments in stable angina pectoris: Seattle Angina Questionnaire, Short Form Health Survey (SF-36), and Quality of Life Index—Cardiac Version III. J Clin Epidemiol. 1998;51:569–75. [DOI] [PubMed]
- 21.Spertus JA, Jones P, McDonell M, Fan V, Fihn SD. Health status predicts long-term outcome in outpatients with coronary disease. Circulation. 2002;106:43–9. [DOI] [PubMed]
- 22.Institute of Medicine. To Err is Human: Building a Safer Health System. Washington DC: National Academy Press; 2006.
- 23.Schneider EC, Zaslavsky AM, Landon BE, Lied Tr, Sheingold S, Cleary PD. National quality monitoring of Medicare health plans: the relationship between enrollees’ reports and the quality of clinical care. Med Care. 2001;39:1313–25. [DOI] [PubMed]
- 24.Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician–patient interactions on the outcomes of chronic disease. Med Care. 1989;27:S110–27. [DOI] [PubMed]
- 25.Holsclaw SL, Olson KL, Hornak R, Denham AM. Assessment of patient satisfaction with telephone and mail interventions provided by a clinical pharmacy cardiac risk reduction service. J Manag Care Pharm. 2005;11:403–9. [DOI] [PMC free article] [PubMed]
- 26.National Veterans Satisfaction; Office of Quality and Performance. National Survey of Veterans. Available at: http://www1.va.gov/vetdata/docs/survey_final.htm. Assessed July 16, 2007.
- 27.Parashar S, Rumsfeld JS, Spertus JA, Reid KJ, Wenger NK, Krumholz HM, Amin A, Weintraub WS, Lichtman J, Dawood N, Vaccarino V. Time course of depression and outcome of myocardial infarction. Arch Intern Med. 2006;166(18):2035–43 [DOI] [PubMed]
- 28.Rumsfeld JS, Magid DJ, Plomondon ME, Sales AE,Grunwald GK, Every NR, Spertus JA. History of depression, angina, and quality of life after acute coronary syndromes. Am Heart J 2003;145(3):493–9. [DOI] [PubMed]
- 29.Ware JE, Jr., Wright WR, Snyder MK, Chu GC. Consumer perceptions of health care services: implications for academic medicine. J Med Educ. 1975;50:839–48. [DOI] [PubMed]
- 30.Hulka BS, Cassel JC, Kupper LL, Burdette JA. Communication, compliance, and concordance between physicians and patients with prescribed medications. Am J Public Health. 1976;66:847–53. [DOI] [PMC free article] [PubMed]
- 31.Irwin RS, Richardson ND. Patient-focused care: using the right tools. Chest. 2006;130:73S–82S. [DOI] [PubMed]
- 32.Loghman-Adham M. Medication noncompliance in patients with chronic disease: issues in dialysis and renal transplanation. Am J Manag Care. 2003;9:155–71. [PubMed]


