Abstract
The goal of this study was to more fully understand readiness for treatment in a pre-treatment sample of 446 substance abusers. Structural Equation Modeling (SEM) was used to: (1) examine the relationships between readiness factors identified in the Pre-Treatment Readiness Scale; and (2) identify the effects of predisposing, illness, and inhibiting determinants on the factors. As with in-treatment samples, Problem Recognition was found to influence Treatment Readiness, although through a different intervening factor, Desire for Change rather than Desire for Help. A fourth factor, Treatment Reluctance, was also influenced by the Desire for Change factor. Fixed characteristics such as age and gender had minimal influences on readiness factors, as did inhibiting characteristics that reflected recent functioning. Illness characteristics including drug severity and perceived treatment barriers had a more robust influence on readiness factors. This study provides an increased understanding of readiness for treatment among pre-treatment substance abusers and also supported the construct validity of the Pre-Treatment Readiness Scale.
Keywords: Substance abuse, motivation for treatment, treatment readiness
INTRODUCTION
Although substance abuse treatment is widely available in the United States, rates of treatment entry are low and many substance users who need treatment services have never been in treatment (1,2). Substance abusers not following through with treatment is almost universally attributed to poor motivation in both community-based drug treatment (3-5) and in criminal justice settings (6).
Motivation for treatment is frequently characterized as “treatment readiness” when substance abusers’ decisions to enter treatment are considered. Motivation, or readiness, may be viewed as an individual’s personal considerations, commitments, reasons, and intentions that lead to the performance of certain behaviors (7). The elements of treatment readiness have usually been examined among in-treatment substance abuse populations and found to be comprised of well-defined components that include problem recognition and desire for help (3,5). Motivation, or readiness, has not been examined in substance abusers immediately after their assessment but before treatment entry. This period is a critical juncture in the treatment continuum of care whether the assessment takes place at a treatment program or a community-wide centralized intake unit.
The present study seeks to expand our understanding of treatment readiness in a pre-treatment population of substance abusers who were evaluated at a centralized intake unit in Dayton, Ohio. The Pre-Treatment Readiness Scale (PRS) (9) was re-examined using an increased sample of substance abusers who had just been assessed but had not yet entered treatment. Structural equation modeling (SEM) was used to examine the factor structure of the PRS and how the factors influence one another. Three groups of predictor variables were tested to examine their potential influence on separate readiness factors as well as the overall process of readiness.
BACKGROUND
Treatment Readiness
Constructs such as Problem Recognition, Desire for Help, and Treatment Readiness are generally used in describing substance abusers’ attitudes about their substance use and need to get help (5,10). The Stages of Change, Readiness, and Treatment Eagerness Scale (SOCRATES) presents three components of readiness, including problem recognition, taking steps, and ambivalence, as well as sub-tasks associated with stages of change such as contemplation (10). The Circumstances, Motivation, Readiness, and Suitability Scale (CMRS) was developed with substance abusers in long-term therapeutic communities (3). The CMRS identified two separate dimensions of motivation–circumstances surrounding substance use and an individual’s perceptions of the suitability of a treatment program.
Attempts to assess motivational factors in out-of-treatment populations have frequently started with the Treatment Motivation Assessment (TMA), a scale originally developed with in-treatment methadone patients (5). The TMA’s three scales–Problem Recognition, Desire for Help, and Treatment Readiness–were tested as a measure of motivation among substance abusers at two inner-city soup kitchens (8). Path models demonstrated that readiness for treatment is influenced by Desire for Help as an intervening factor but no direct relationship was found between Problem Recognition and Treatment Readiness. Two items constituting negativity toward treatment were deleted as being incompatible with the overall motivational model.
Treatment readiness has also been represented as a single dimension, rather than as separate but related factors. A single cumulative score representing the additive values of Problem Recognition, Desire for Help, and Treatment Readiness was tested to determine its ability to differentiate treatment acceptors from treatment deniers (11). In multivariate results the combined measure, along with the Addiction Severity Index drug composite score, successfully predicted acceptors from deniers. Similar attempts to produce a single readiness score from constituent factors have resulted in counter-intuitive findings about the relationship between readiness, retention and improved outcomes (12-14).
Our research team (9) developed the Pre-Treatment Readiness Scale (PRS) to identify motivational constructs in substance abusers who had been assessed and referred at a centralized intake unit, but had not yet entered treatment. Factor analyses and structural equation modeling revealed both similarities and differences when compared to scales developed with in-treatment samples. Problem Recognition and Treatment Readiness factors were present in both in-treatment and pre-treatment populations. However, unlike in-treatment substance abusers the pre-treatment sample identified a Desire for Change, a subtle but important difference from Desire for Help. Treatment Reluctance, the conceptual opposite of readiness, was also a distinct factor.
Influences on Treatment Readiness
A more thorough understanding of the process whereby substance abusers enter treatment has come from examining the influence of individual characteristics on treatment readiness. Andersen’s model of health care utilization is a useful paradigm for considering three groups of individual characteristics–predisposing, illness, inhibiting–that may influence treatment readiness and its constituent factors (15).
Predisposing Characteristics
Predisposing characteristics are static, unchangeable attributes of individuals, such as gender, race/ethnicity, age, and treatment history. Although not always considered as such, these variables may be composites of more complex phenomena that can greatly influence readiness. Gender, for example, has been widely considered for its relationship to readiness. Out-of-treatment female crack users were shown to be less ready for treatment than their male counterparts (16), although other studies found that women were more motivated than men (5,13,17-20). Women also scored higher on motivation measures across three sub-scales including Problem Recognition, Desire for Help, and Treatment Readiness (5). Similarly, being male was negatively related to Desire for Help, one component of overall treatment readiness (13). Other research, however, has not found any relationship between gender and readiness (11,21,22).
The link between race/ethnicity and treatment readiness is also not consistent. Long shore and colleagues found that African-Americans and Hispanics who were daily substance users were less likely than Whites to report a need for treatment (20). Whites who were opioid addicts were found to have higher scores than Non-Whites on all three readiness constructs–Problem Recognition, Desire for Help, and Treatment Readiness (5). Using the same readiness scale, however, being African American was positively associated with treatment readiness, although not with problem recognition and desire for help (13). African-Americans were more likely than Whites to be in the action stage of change, a construct similar to readiness, after completing an assessment (19). Other studies, however, have not identified race/ethnicity as a significant predictor of motivation (11,22).
Prior history of substance abuse treatment is one of the more consistently cited predictors of treatment readiness. Prior treatment was positively associated with three readiness factors–Problem Recognition, Desire for Help, and Treatment Readiness among out-of-treatment substance abusers (8) and a positive predictor of Desire for Help among crack users (13). Prior treatment has also been associated with decreased odds of wanting treatment among crack users (16) although the lack of influence may be conditional on other factors. Two or more previous treatment admissions were required to positively influence readiness in injection drug users, although one previous treatment experience did not (23). Substance abusers who related that they had a successful prior treatment experience were also more likely to re-enter treatment (24). In other studies, no association was found between prior treatment history and readiness to change (18,25).
Illness Factors
Several personal and environmental characteristics have been directly related to decisions about treatment. As such, these illness factors may have a stronger and clearer impact on readiness than do predisposing characteristics (26). They include overall health beliefs and perceived value of getting treatment, as well as tangible barriers such as lack of transportation and inability to pay for care. Crack users who described themselves as being ready for treatment were more likely to report lack of transportation and inability to pay as barriers to treatment compared with crack users not ready for treatment (16). No significant difference was found between groups when considering another tangible barrier, childcare (16). However, Nwakeze (8) noted that childcare responsibilities were a significant predictor of treatment readiness in substance abusers at a soup kitchen.
Readiness for treatment is generally higher among substance abusers with more severe substance abuse problems. A positive relationship between substance use problem severity indicators and the recognition factor in the Stages of Change Readiness and Treatment Scale (SOCRATES) was found for a large sample (N = 1,672) of problem drinkers (10). Higher scores on the Addiction Severity Index drug and alcohol composites were positive predictors of higher levels of Problem Recognition, Desire for Help, and Treatment Readiness (11,13). Other characteristics of drug use, such as frequency and intensity, have also been associated with readiness (8,16,23). However, the relationship between substance use factors and motivation is not consistently found (27,28).
Involvement in the legal system is a relevant, though unlikely illness factor, when considering substance abuse treatment. Perceived legal pressure was twice as common among ready for treatment substance abusers than in substance abusers who were not ready for treatment (16). Further, substance abusers entering treatment as a result of legal coercion were over three times more likely to indicate that they engaged in recovery oriented behavior following admission (18). Similar conclusions were drawn by other researchers who found that higher readiness for change was positively associated with legal coercion (12). Legal problems, as measured by Addiction Severity Index legal composite scores, not only predicted external motivation as might be expected, but also internalized, self-driven motivation (22).
Inhibiting Factors
Inhibiting factors are circumstances in the substance abusers’ overall environment that interfere with health related actions. These mutable, or changeable, characteristics are general in nature and include functioning in critical areas such as physical and mental health, social relationships, and employment.
Depression, in particular, is frequently associated with measures of readiness. Substance abusers’ depression was positively correlated with three measures of motivation–internal, external and interpersonal help-seeking (22,29). Higher levels of depression have also been positive predictors of treatment readiness and problem recognition (8,16). Despite the possible positive relationship between depression and improved readiness to enter treatment, depression has also been also associated with poorer treatment outcomes (30,31).
Social support and familial influences impact treatment motivation in various ways. In a sample of individuals entering outpatient cocaine treatment, 31% cited social and family pressures as a reason for entering treatment (32); social encouragement was cited as a common reason to seek treatment among problem drinkers (33). The influence of social group may also be more subtle and less predictable. Having a peer group that encourages risk-taking or a dysfunctional family was positively correlated with problem recognition (5). The positive relationship between higher levels of family and social problems and readiness may indicate that when individuals do not feel supported by their social group they seek assistance elsewhere. No significant relationships were found between characteristics of the social network like network size and frequency of contact, and help-seeking (34).
Having a trade and/or job skills has been negatively associated with problem recognition, suggesting that as long as employment is intact substance abusers may feel less in need of treatment (8). Similarly, unemployment was a positive predictor of help-seeking among male problem drinkers (34). Being unemployed was related to a higher composite motivation score in a sample of 133 crack cocaine users, primarily through the treatment readiness factor (13).
METHODS
This study was conducted as part of Reducing Barriers to Substance Abuse Treatment Services, a National Institute on Drug Abuse funded clinical trial. Substance abusers who receive an assessment and referral at a centralized intake unit (CIU) are randomly assigned to: (1) a standard of care group; (2) one session of motivational interviewing; or (3) five sessions of strengths-based case management. The study is located at Samaritan Crisis Care, a centralized intake unit (CIU) in Dayton, Ohio. The CIU is the county’s only point of entry for uninsured individuals seeking treatment for substance abuse and mental health problems.
Eligibility requirements for the clinical trail included: Substance abusers who meet the following criteria are referred to the Reducing Barriers Project: (1) over 18 years of age; (2) diagnosed as having a substance abuse and/or dependence disorder using criteria from the Diagnostic and Statistical Manual (American Psychiatric Association, 2001) (subjects who were diagnosed only with alcohol abuse or dependence were not eligible); (3) not diagnosed with schizophrenia or any other psychotic disorder; and (4) referred to either residential or outpatient substance abuse services.
Eligible subjects are referred to RBP research staff by CIU assessment therapists. RBP research assistants provide a summary of the project, and if an individual is interested an informed consent approved by a university’s institutional review board is read to them. The confidential nature of the study is stressed as is the fact that refusal to participate does not affect CIU services for which an individual is otherwise eligible. Individuals who wish to enter the study then participate in a baseline interview lasting about 1 1/2 hours. Most interviews take place immediately following a clinical assessment, although some potential subjects are scheduled to return at a later time. Follow-up interviews are conducted at three and six months following baseline. Subjects are paid a $30 stipend for their time spent answering questions on each interview.
The Pre-Treatment Readiness Scale (PRS) was developed to assess readiness for treatment in substance abusers assessed and referred to treatment but not yet in treatment (9). PRS items came from the Texas Christian University Treatment Motivation Assessment (TMA) made up of three factors: Problem Recognition, Desire for Help, and Treatment Readiness (5). The scale consists of twenty-three items which make up the three constructs: (a) Problem Recognition (PR; 9 items) assesses an individual’s attitude toward their drug use (e.g., “Your drug use is causing problems in thinking or doing your work”); (b) Desire for Help (DH; 6 items) gauges the need for assistance (e.g., “You need help in dealing with your drug use”); and (c) Treatment Readiness (TR; 8 items) measures the level of readiness for seeking treatment (e.g., “Treatment may be your last chance to solve your drug problems”). Subjects were asked to respond to the items based on a five-point Likert-type scale that included: (1) strongly disagree, (2) disagree, (3) neutral, (4) agree, (5) strongly agree. Raw scores on negatively worded items, e.g., “Treatment will not be very helpful to you” were reversed to ensure intended relationships among items.
Exploratory and confirmatory factor analyses and difference tests demonstrated that a four factor model represented a significant improvement over the original three factor model. As in the original TMA, Problem Recognition and Treatment Readiness constructs were present. A Desire for Change scale was identified in this pre-treatment sample indicating a willingness to make changes rather than a willingness to get help. A Treatment Reluctance factor indicated ambivalence and negativity about entering treatment.
An extensive baseline questionnaire contain questions that are designed to gather lifetime, six month and 30 day information from subjects relative to gender, age, education level, marital status, drug use, housing, employment patterns, HIV risk behaviors, treatment history, and critical life events. The interview included all items from the Addiction Severity Index (ASI), Version 5 (35). The ASI is a widely used instrument for assessing the severity of drug addiction problems in seven life areas–alcohol use, drug use, legal, family/social, medical, employment, and psychiatric. Composite scores from each of the seven ASI areas are based on items representing functioning during the 30 days before the interview.
The 59-item Barriers to Treatment Inventory was used to represent barriers that substance abusers identified prior to treatment (36). The scores from each of the factors representing internal barriers–Absence of Problem, Negative Social Support, Fear of Treatment, and Privacy Concerns–were used in this analysis. The internal barrier constructs include: (a) Absence of Problem (AP; 6 items) assesses an individual’s attitude toward their drug use (e.g., “I do not think I have a problem with drugs); (b) Negative Social Support (NSS; 5 items) gauges the belief of family and peers that there is no need for treatment (e.g., “Friends tell me not to go to treatment’’); (c) Fear of Treatment (FT; 4 items) measures individuals’ concerns about being in treatment (e.g., “I am afraid of what might happen in treatment”); and (d) Privacy Concerns (PC; 3 items) representing individuals’ reticence to talk about themselves (e.g., I hate being asked personal questions). The BTI is read to subjects by a research assistant, taking an average of 15 minutes to complete. Subjects are asked to indicate on a five-point scale how much they believe that each barrier would affect their entry into treatment. The five point scale includes: (1) disagree strongly, (2) disagree, (3) uncertain, (4) agree, and (5) agree strongly.
ANALYSIS
Confirmatory Factor Analysis (CFA) and Structural Equation Modeling (SEM) were conducted using the structural equation-modeling software, AMOS (Analysis of Moment Structures) (37). Several fit indices were examined in evaluating CFAs. The primary criterion for evaluating the fit of each model was the Comparative Fit Index (CFI) (38). This index is determined by comparing the fit of the model and the fit of the independent model. CFI values range from 0 to 1 and values above 0.90 represent a good fit. The Tucker-Lewis coefficient (TLI) (39), Root Mean Squared Error of Approximation (RMSEA) (40), and Probability of Close Fit (p Close) are three other indicators that measure the fit between the model and the observed data. RMSEA is one of the most sensitive indices for models with mis-specified factor loadings (41). RMSEA values of less than 0.05 indicate a close fit and less than 0.08 a reasonable fit (42,43). P Close is a significance value for testing the null hypothesis that the difference between the model and population is not greater than 0.05; non-significant values indicate better goodness of fit.
Variables representing Andersen’s three categories of individual characteristics associated with health care utilization were tested to examine their influence on the treatment readiness process. Predisposing characteristics included ethnicity, gender, age, education level, and previous treatment experience. Illness variables included court referral, subjects’ preference for residential treatment, ASI composite scores for alcohol and drug functioning, and four treatment specific internal barriers–Absence of Problem, Negative Social Support, Fear of Treatment, and Privacy Concerns. ASI composite scores for alcohol and drug use were also viewed as illness related. Five ASI life areas were used to represent inhibiting characteristics in health, psychiatric, work, employment, and social functioning. Dummy coding was used with categorical variables: being male, White, having previous treatment experience, being court referred and preferring residential treatment were all coded as “1.”
RESULTS
Descriptive Statistics
Table 1 presents descriptive statistics for the sample. Among the 446 participants, 63.0% were male, and 47.3% were Black. The mean age of subjects was 34.09 years (S.D. 10.96, range 18-64). The participants had completed a mean of 11.3 years of secondary education (S.D. 1.9, range 6-16). Almost two-thirds (63.5%) of the sample identified crack cocaine as their primary drug problem and about seventy percent (70.5%) of the sample (males 64.3% and females 35.7%) had been previously treated for alcohol or drug abuse.
Table 1.
Selected Sample Characteristics (N = 446)
| n | % | |
|---|---|---|
| Ethnicity | ||
| African American | 211 | 47.3 |
| Caucasian | 235 | 52.7 |
| Gender | ||
| Male | 281 | 63.0 |
| Female | 165 | 37.0 |
| Age groups (in years) | Mean = 34.09 | SD = 10.96 |
| 18-24 | 106 | 23.8 |
| 25-34 | 152 | 34.1 |
| 35-44 | 89 | 20.0 |
| >45 | 99 | 22.2 |
| Eucation (highest grade completed) | Mean = 11.26 | SD = 1.92 |
| 1 to 8 | 32 | 7.2 |
| 9 to 12 | 319 | 71.5 |
| 13+ | 95 | 21.3 |
| Primary drug | ||
| Crack/cocaine | 33 | 63.5 |
| Heroin/opiates | 16 | 30.7 |
| Marijuana | 3 | 5.8 |
| Previous treatment history (in times) | Mean = 0.46 | SD = 2.31 |
| Yes | 314 | 70.4 |
| No | 132 | 29.6 |
| Court-referred | ||
| Yes | 123 | 27.6 |
| No | 323 | 72.4 |
| Residential, inpatient or therapeutic treatment needed | ||
| Yes | 151 | 33.9 |
| No | 295 | 66.1 |
| ASI composite score | ||
| Medical status | Mean = 0.23 | SD = 0.34 |
| Employment status | Mean = 0.81 | SD = 0.23 |
| Alcohol use | Mean = 0.12 | SD = 0.21 |
| Drug use | Mean = 0.21 | SD = 0.16 |
| Legal status | Mean = 0.19 | SD = 0.21 |
| Family/Social status | Mean = 0.31 | SD = 0.20 |
| Psychiatric status | Mean = 0.27 | SD = 0.25 |
note: four cases in “other” ethnic group were omitted from our analyses.
Confirmatory Factor Analyses
Results of exploratory (EFA) and confirmatory factor analyses (CFA) with 446 substance abusers confirmed the factor structure present in our previous study (9). All factor loadings were significant, with standardized loadings ranging from .370 to .876. Table 2 shows the inter-correlations of the four-factors, all of which were strongly related and significant (p < .001). As reported elsewhere, scale inter-correlations were stronger between theoretically adjacent stages, suggesting a possible linear progression between factors (5,6). Problem Recognition-Desire for Change and Desire for Change-Treatment Readiness showed stronger associations than nonadjacent stages, Problem Recognition and Treatment Readiness. As expected, Treatment Reluctance was negatively correlated with all factors: Problem Recognition (r = −0.55), Desire for Change (r = −0.67) and Treatment Readiness (r = −0.67).
TABLE 2.
Intercorrelations among factors derived from pre-treatment population
| Factors | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. Problem Recognition (PR) | 1.000 | .778*** | .616*** | −.553*** |
| 2. Desire for Change (DC) | 1.000 | .718*** | −.665*** | |
| 3. Treatment Readiness (TRd) | 1.000 | −.670*** | ||
| 4. Treatment Reluctance (TRl) | 1.000 |
note: 1. all coefficients are standardized coefficients; 2. *** p < 0.001.
Path Analyses of Treatment Readiness Process
Path analyses using SEM (Figure 1) showed a strong positive and statistically significant relationship between Problem Recognition and Desire for Change. In turn, Desire for Change had a strong positive relationship with Treatment Readiness and an equally strong negative relationship with Treatment Reluctance. Treatment Readiness and Treatment Reluctance represent opposite views about entering treatment and had a negative relationship.
FIGURE 1.
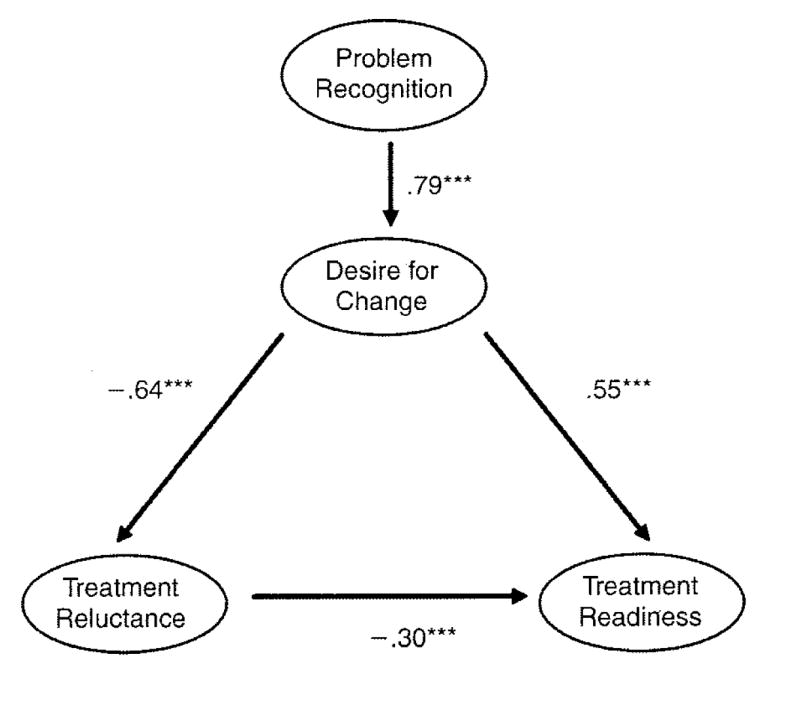
Structural equation modeling estimating the causal relationship between problem recognition, desire for change, treatment readiness, and treatment reluctance. Chi-square = 490.88, df = 165, CFI = .914, TLI = .901, RMSEA = .066, PCIOSE = .000. *** p < .001
Path Analyses of the Treatment Readiness Process with Individual Characteristics
The addition of individual characteristics to the four factor model changed the relationship between some factors (Figure 2). The previously non-existent relationship between Problem Recognition and Treatment Reluctance became a moderately strong relationship (beta = 0.36; p < .001) in an unexpected direction. It seemed that the more that a problem was recognized, the more reluctant substance abusers were to enter treatment. The relationship between Treatment Readiness and Treatment Reluctance was no longer evident.
FIGURE 2.
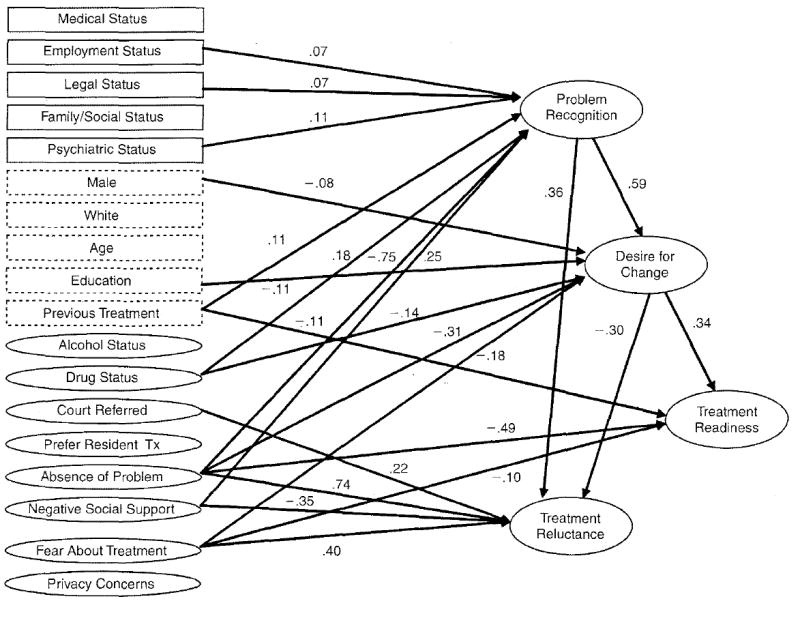
Structural equation modeling estimating the causal relationship between predisposing (dash box), inhibiting (solid boxes) and illness (oval) characteristics and PRS scales. Estimates of model fit: Chi-square = 2391.87, Df = 1229, CFI = .866, TLI = .856, RMSEA = .046, PCLOSE = .985. All values are significant at p < .001.
Predisposing characteristics did not play a strong role in predicting any of the factors of the Pre-Treatment Readiness Scale. Only previous treatment influenced more than one of the four PRS factors, predicting higher Problem Recognition (beta = 0.11; p < .001) but lower Treatment Readiness (beta = −0.11; p < .001). Being male and having a relatively lower level of education negatively influenced Desire for Change, although both influences were weak. Neither race/ethnicity nor age predicted any readiness factor.
Inhibiting characteristics represented by ASI composite scores also had a minimal influence on readiness factors. Higher levels of dysfunction in three areas–employment, legal status, and psychiatric status–predicted increased Problem Recognition.
As a group, illness factors exerted the strongest influence on the four PRS factors. Absence of Problem as a barrier to treatment had a strong to moderate negative relationship with Problem Recognition (beta = −0.75; p < .001), Desire for Change (beta = −0.31; p < .001) and Treatment Readiness (beta = −0.49; p < .001). Fear of Treatment was negatively predictive of substance abusers’ desire to change and their readiness to enter treatment. The perception that there was no problem, having a fear of treatment, and being referred for an assessment by the criminal justice system predicted increased reluctance to enter treatment.
An unexpected relationship occurred between Negative Social Support and both Problem Recognition and Treatment Reluctance. A higher level of negative support from friends and family actually predicted more problem recognition and less reluctance to enter treatment. The relationship between the Addiction Severity Index drug composite score and desire for change was negative but weak, suggesting that the more extensive that one’s drug use is, the lower the desire for change becomes.
DISCUSSION
Readiness Process
Exploratory and confirmatory factor analyses with 446 substance abusers confirmed the factor structure of the Pre-Treatment Readiness Scale from an earlier study and SEM clarified the relationship between readiness components. Our results provide both similarities and contrasts with readiness scales developed with substance abusers already in treatment. Problem Recognition was confirmed as a distinct factor, suggesting that substance abusers, whether in treatment or considering treatment, must first assess whether there is a problem or not before moving further in the readiness process. Treatment Readiness was also identified as a distinct factor, a consistent finding in most other readiness scale studies.
The overall process of developing readiness for treatment differed in two distinct ways from in-treatment samples. First, pre-treatment substance abusers identified a desire to change rather than a desire to seek help. Change items reflected substance abusers’ willingness to alter their current lifestyle by giving up drugs as well as drug using friends and places. Items in the PRS that represented help, rather than change, did not form a distinct factor. The structure of the change, or help, factor has been inconsistent in the past, perhaps reflecting the context-sensitive nature of the factor (5). It is also possible that help-related items from the original Treatment Motivation Assessment do not accurately describe getting help among substance abusers who are just beginning the treatment continuum. New items should be tested to determine whether a stable help factor may be present in addition to the change factor.
The Treatment Reluctance factor found here is both clinically and conceptually valuable. Conceptually, treatment reluctance is similar to constructs such as pre-contemplation (University of Rhode Island Change Assessment) and ambivalence (SOCRATES) (10,44). These related constructs may indicate a lower degree/level of readiness or a separate and distinct construct in the readiness process. Operationalizing the view that reluctance is just less readiness, has been arrived at by subtracting treatment negative factors such as pre-contemplation from the summed scores of factors that represented willingness to go to treatment–contemplation, preparation, and action (45). This, and similar attempts to quantify the readiness measure resulted in counter-intuitive findings about the relationship between readiness and treatment attendance and retention (12,14).
Alternatively, reluctance can be treated as a distinct construct that is related to readiness, not merely a lower degree of readiness. A four item resistance construct was tested to clarify the relationship between the factor and treatment readiness (46). Results suggested that readiness/motivation and resistance should be viewed as separate constructs, each adding valuable information to the understanding of treatment readiness.
Our results seem to favor the separate construct view. When examining the readiness process before predictor variables were considered, reluctance was modeled as a next step beyond desire for change and a precursor to readiness. After the introduction of individual determinants, a significant relationship developed between Problem Recognition and Treatment Reluctance. This finding raises the possibility that when substance abusers recognize the extent of their substance abuse problem, hesitancy about entering treatment may develop.
Clinically, the reluctance factor represents the uncertainty that many substance abusers have about going to treatment. Further, it can serve as a reminder to treatment professionals that some reluctance to enter treatment might be present even if there is also some readiness for treatment present. Motivational interventions that help substance abusers clarify their reasons for entering treatment and role induction techniques to improve understanding of the treatment process may be particularly beneficial for substance abusers who are still uncertain about their next steps.
Influence of Individual Characteristics on Readiness
Testing the effect of individual determinants in the structural equation model altered the relationship between readiness factors. Prior to their introduction, the effect of problem recognition on treatment reluctance was mediated by the desire for change. The introduction of predisposing, illness, and inhibiting measures led to a direct relationship between identifying a problem and treatment reluctance. This result may represent a clinical reality for some substance abusers: once they fully appreciate the specific evidence of a problem they become overwhelmed and reluctant to enter treatment.
Predisposing characteristics selected for inclusion in the analysis were relatively unimportant in influencing the treatment readiness process. The characteristics that were tested here, e.g., ethnicity, may not have a prominent relationship with substance abusers’ considerations about entering treatment. Also, the measures used to describe predisposing characteristics may not be adequately sensitive to the phenomenon underlying the measure. Being African American, for example, may represent obvious factors such as income or geographic location as well as more subtle themes such as: strength of ethnic identity, perceptions of racism, cultural biases in the health care delivery system, and lack of culturally appropriate treatment programs (47). Understanding and testing the important core elements of static characteristics such as gender, age, ethnicity, and employment level will allow researchers to more fully assess the impact of these characteristics on the readiness process.
Addiction Severity Index composite scores are aggregate measures that represent several major areas of functioning. For example, the medical composite is made up of three aspects of current functioning–days of medical problems, concern over medical problems, and importance of treatment. Because these measures are multidimensional and may be consequences of substance use it was expected that there would be a stronger connection between them and the readiness process. This was not the case as three of the composites–psychiatric, employment, legal–were only weakly related to Problem Recognition and not at all to other readiness factors.
Illness factors had the most robust influence on the four PRS factors. This is not surprising since illness factors by definition are closely associated with an illness and the utilization of services. The finding that the ASI drug composite was positively associated with Problem Recognition is to be expected, although its negative relationship with Desire to Change is somewhat counterintuitive. Some substance abusers that have an increased awareness of problems may be overwhelmed and have a fatalistic view of their situation, minimizing the desire to change or attempt to enter treatment.
Fear of treatment represented by items such as “I’m afraid of what might happen in treatment” was associated with three of the four readiness factors. Fear items focused on seeking and being in treatment. Its effect was shown through a reduced desire to change and less treatment readiness, although not associated with the first step of recognizing a problem. Fear’s strongest association was, not surprisingly, related to Treatment Reluctance.
Although not a specific goal of this study, analyses provided support for the factor structure of both the Pre-Treatment Readiness Scale (PRS) and the Barriers to Treatment Inventory (BTI). Most of the relationships between factors in the two instruments were in expected directions. Absence of Problem (a factor in the BTI) had a very strong to moderate negative relationship with Problem Recognition, Desire for Change and Treatment Readiness, all part of the PRS. Fear of Treatment (BTI) was negatively predictive of the desire to change and readiness to enter treatment (PRS). The perception that there was no problem and the fear of treatment influenced Treatment Reluctance in an expected direction. Privacy Concerns and Time Conflict factors from the Barriers to Treatment Inventory were associated only with desire for change, perhaps because these two issues were only salient if substance abusers were considering change and help in the first place.
Limitations
Generalizing the results of this study to other populations of substance abusers must be done cautiously. The substance abusers that participated in this study represent a convenience sample that may not be representative of all substance abusers, potentially limiting the usefulness of the Pre-Treatment Readiness Scale. Subjects in this study were recruited at a centralized intake unit indicating that they are eligible for public financial support when they attend treatment. It is possible that their level of motivation may be different than that of substance abusers who have not been assessed or who have private insurance. Further, the substance abusers that agreed to participate in this study may represent a subset of particularly motivated CIU clients.
Although there did not appear to be any incentive for study participants to exaggerate or fabricate their responses to items relating to motivation, there is always the possibility that responses are biased, either over- or under-representing the presence of motivation. Studies of self-reported drug use suggested that self-report data from such samples tend to be reasonably reliable (17,48,49).
Implications
Factors representing treatment ambivalence and desire for change are not usually identified among in-treatment samples of substance abusers. This may reflect the settled attitude that in-treatment substance abusers have about treatment: their ambivalence is resolved and ostensibly their desire for change is represented within the desire for help. In this pre-treatment population both desire for change and treatment reluctance were distinct factors in the readiness process.
Our findings provide a useful message for professionals interacting with substance abuses during the critical assessment period. The ability to help clients become ready to enter treatment (treatment readiness) may be facilitated not by directly promoting treatment (desire for help), but by assisting clients to identify personal reasons for change. Clinical staff might emphasize change rather than the need for help, at least in marginally motivated individuals. Motivational interventions emphasize this point, encouraging substance abusers to become more aware of discrepancies between their current drug-using lifestyle and their view of how they want their life to be. Strengths-based case management (SBCM), one of the interventions being tested in this trial, may also be useful in improving treatment readiness. As with motivational interviewing SBCM engages individuals in a non-confrontive relationship and assists them in resolving barriers that can interfere with treatment linkage (31).
The Pre-Treatment Readiness Scale has not been evaluated for its ability to predict important aspects of the treatment process, including treatment linkage and engagement. A larger sample size in the Reducing Barriers Project will make this possible. In addition, we will use the PRS to study the impact of the two study interventions–motivational interviewing and strengths-based case management–on motivation for treatment at three and six months following assessment.
Acknowledgments
This study was supported by a grant from the National Institute on Drug Abuse (Grant No. DA 15690) and the administrative and clinical staff at Samaritan CrisisCare, Sue McGatha director.
References
- 1.Brown BS, Needle RH. Modifying the process of treatment to meet the threat of AIDS. International Journal of Addictions. 1994;29(13):1739–1752. doi: 10.3109/10826089409047959. [DOI] [PubMed] [Google Scholar]
- 2.Sobell LC, Sobell MB, Toneatto T. Recovery from alcohol problems without treatment. In: Heather N, Miller WR, Greeley JE, editors. Self-control and the addictive behaviors. New York: Maxwell MacMillan; 1992. pp. 198–242. [Google Scholar]
- 3.De Leon G, Jainchill N. Circumstance, motivation, readiness and suitability as correlates of treatment tenure. Journal of Psychoactive Drugs. 1986;18:203–208. doi: 10.1080/02791072.1986.10472348. [DOI] [PubMed] [Google Scholar]
- 4.De Leon G, Hawke J, Jainchill N, Melnick G. Therapeutic communities. Enhancing retention in treatment using “senior professor” staff. Journal of Substance Abuse Treatment. 2000;19(4):375–382. doi: 10.1016/s0740-5472(00)00124-0. [DOI] [PubMed] [Google Scholar]
- 5.Simpson DD, Joe GW. Motivation as a predictor of early dropout from drug abuse treatment. Psychotherapy: Theory, Research, Practice, Training. 1993;30(2):357–368. [Google Scholar]
- 6.Hiller ML, Knight K, Leukefeld C, Simpson DD. Motivation as a predictor of therapeutic engagement in mandated residential substance abuse treatment. Criminal Justice & Behavior. 2002;29(1):56–75. [Google Scholar]
- 7.Cunningham JA, Sobell LC, Sobell MB, Agrawal S, Toneatte T. Barriers to treatment: Why alcohol and drug abusers delay or never seek treatment. Addictive Behaviors. 1993;18(3):347–353. doi: 10.1016/0306-4603(93)90036-9. [DOI] [PubMed] [Google Scholar]
- 8.Nwakeze PC, Magura S, Rosenblum A. Drug problem recognition, desire for help, and treatment readiness in a soup kitchen population. Substance Use and Misuse. 2002;37(3):291–312. doi: 10.1081/ja-120002480. [DOI] [PubMed] [Google Scholar]
- 9.Rapp RC, Xu J, Carr C, Lane DT, Wang J, Carlson RG. Development of a motivation assessment in a pre-treatment population of substance abusers. American Journal of Drug and Alcohol Abuse. In Press. [Google Scholar]
- 10.Miller WR, Tonigan JS. Assessing drinkers’ motivations for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) Psychology of Addictive Behaviors. 1996;10(2):81–89. [Google Scholar]
- 11.Boyle K, Polinsky ML, Hser Y. Resistance to drug abuse treatment: A comparison of drug users who accept or decline treatment referral assessment. Journal of Drug Issues. 2000;30(3):555–574. [Google Scholar]
- 12.Blanchard KA, Morgenstern J, Morgan TJ, Labouvie E, Bux DA. Motivational subtypes and continuous measures of readiness for change: Concurrent and predictive validity. Psychology of Addictive Behaviors. 2003;17(1):56–65. doi: 10.1037/0893-164x.17.1.56. [DOI] [PubMed] [Google Scholar]
- 13.Rapp RC, Li L, Siegal HA, DeLiberty RN. Demographic and clinical correlates of client motivation among substance abusers. Health and Social Work. 2003;28(2):107–115. doi: 10.1093/hsw/28.2.107. [DOI] [PubMed] [Google Scholar]
- 14.Stotts AL, Schmitz JM, Grabowski J. Concurrent treatment for alcohol and tobacco dependence: Are patients ready to quit both? Drug and Alcohol Dependence. 2003;69(1):1–7. doi: 10.1016/s0376-8716(02)00227-2. [DOI] [PubMed] [Google Scholar]
- 15.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- 16.Zule WA, Lam WKK, Wechsberg WM. Treatment readiness among out-of-treatment African-American Crack Users. Journal of Psychoactive Drugs. 2003;35(4):503–510. doi: 10.1080/02791072.2003.10400498. [DOI] [PubMed] [Google Scholar]
- 17.Freyer J, Tonigan JS, Keller S, Rumpf H, John U, Hapke U. Readiness for change and readiness for help-seeking: A composite assessment of client motivation. Alcohol & Alcoholism. 2005;40(6):540–544. doi: 10.1093/alcalc/agh195. [DOI] [PubMed] [Google Scholar]
- 18.Gregoire TK, Burke AC. The relationship of legal coercion to readiness to change among adults with alcohol and other drug problems. Journal of Substance Abuse Treatment. 2004;26:337–343. doi: 10.1016/s0740-5472(03)00155-7. [DOI] [PubMed] [Google Scholar]
- 19.Hile MG, Adkins RE. The impact of substance abusers’ readiness to change on psychological and behavioral functioning. Addictive Behaviors. 1998;23(3):365–370. doi: 10.1016/s0306-4603(98)00016-1. [DOI] [PubMed] [Google Scholar]
- 20.Longshore D, Hsieh S, Anglin MD. Ethnic and gender differences in drug users’ perceived need for treatment. International Journal of the Addictions. 1993;28(6):539–558. doi: 10.3109/10826089309039646. [DOI] [PubMed] [Google Scholar]
- 21.Florentine R, Anglin MD. Perceiving need for drug treatment: A look at eight hypotheses. International Journal of the Addictions. 1994;29(14):1835–1854. doi: 10.3109/10826089409128260. [DOI] [PubMed] [Google Scholar]
- 22.Ryan RM, Plant RW, O’Malley SS. Initial motivations for alcohol treatment: Relations with patient characteristics, treatment involvement, and dropout. Addictive Behaviors. 1995;20(3):279–297. doi: 10.1016/0306-4603(94)00072-7. [DOI] [PubMed] [Google Scholar]
- 23.Zule WA, Desmond DP, Vogtsberger KN. Injecting drug users who want treatment. American Journal of Drug and Alcohol Abuse. 1997;23(4):507–522. doi: 10.3109/00952999709016892. [DOI] [PubMed] [Google Scholar]
- 24.Hser YI, Maglione M, Polinsky ML, Anglin MD. Predicting drug treatment entry among treatment-seeking individuals. Journal of Substance Abuse Treatment. 1998;15(3):213–220. doi: 10.1016/s0740-5472(97)00190-6. [DOI] [PubMed] [Google Scholar]
- 25.Hubbard RL, Craddock SG, Anderson J. Overview of 5-year follow-up outcomes in the drug abuse treatment outcome studies (DATOS) Journal of Substance Abuse Treatment. 2003;25:125–134. doi: 10.1016/s0740-5472(03)00130-2. [DOI] [PubMed] [Google Scholar]
- 26.Isenhart CE. Motivational subtypes in an inpatient sample of substance abusers. Addictive Behaviors. 1994;19(5):463–475. doi: 10.1016/0306-4603(94)90002-7. [DOI] [PubMed] [Google Scholar]
- 27.Carney MM, Kivlahan JR. Motivational subtypes among veterans seeking substance abuse treatment: Profiles based on stages of change. Psychology of Addictive Behaviors. 1995;9(2):135–142. [Google Scholar]
- 28.Carpenter KM, Miele GM, Hasin DS. Does motivation to change mediate the effect of DSM-IV substance use disorders on treatment utilization and substance use? Addictive Behaviors. 2002;27(2):207–225. doi: 10.1016/s0306-4603(00)00178-7. [DOI] [PubMed] [Google Scholar]
- 29.Cahill MA, Adinoff B, Hosig H, Muller K, Pulliam C. Motivation for treatment preceding and following a substance abuse program. Addictive Behaviors. 2003;28:67–79. doi: 10.1016/s0306-4603(01)00217-9. [DOI] [PubMed] [Google Scholar]
- 30.Dodge R, Sindelar JSR. The role of depression symptoms in predicting drug abstinence in outpatient substance abuse treatment. Journal of Substance Abuse Treatment. 2005;28(2):189–196. doi: 10.1016/j.jsat.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 31.Rapp RC, Siegal HA, Li L, Saha P. Predicting post-primary treatment services and drug use outcome: A multivariate analysis. American Journal of Drug and Alcohol Abuse. 1998;24(4):603–615. doi: 10.3109/00952999809019610. [DOI] [PubMed] [Google Scholar]
- 32.Marlowe DB, Kirby KC, Bonieskie LM, Glass DJ, Dodds LD, Husband SD, Platt JJ, Festinger DS. Assessment of coercive and non-coercive pressures to enter drug abuse treatment. Drug and Alcohol Dependence. 1996;42:77–84. doi: 10.1016/0376-8716(96)01261-6. [DOI] [PubMed] [Google Scholar]
- 33.Tucker JA, Vuchinich RE, Rippens PD. A factor analytic study of influences on patterns of help-seeking among treated and untreated alcohol dependent persons. Journal of Substance Abuse Treatment. 2004;26:237–242. doi: 10.1016/S0740-5472(03)00209-5. [DOI] [PubMed] [Google Scholar]
- 34.Hajema K, Knibbe RA, Droop MJ. Social resources and alcohol-related losses as predictors of help seeking among male problem drinkers. Journal on Studies of Alcohol. 1999;60:120–129. doi: 10.15288/jsa.1999.60.120. [DOI] [PubMed] [Google Scholar]
- 35.McLellan AT. The fifth edition of the addiction severity index. Journal of Substance Abuse Treatment. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 36.Rapp RC, Xu J, Carr C, Lane DT, Wang J, Carlson RG. Factor analysis of treatment barriers identified by substance abusers following assessment at a centralized intake unit. Journal of Substance Abuse Treatment. 2006;30:227–235. doi: 10.1016/j.jsat.2006.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arbuckle JL. AMOS user’s guide. Chicago: Small-Waters; 1997. [Google Scholar]
- 38.Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 39.Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88(3):588–606. [Google Scholar]
- 40.Steiger JH. Tests for comparing elements of a correlation matrix. Psychological Bulletin. 1980;87:245–251. [Google Scholar]
- 41.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- 42.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- 43.Marsh HW, Balla JR, Hau KT. An evaluation of incremental fit indices: A clarification of mathematical and empirical process. In: Marcoulides GA, Schumacker RE, editors. Advanced structural equation modeling techniques. Hillsdale, NJ: Erlbaum; 1996. pp. 315–353. [Google Scholar]
- 44.McConnaughy EA, DiClemente CC, Prochaska JO, Velicer WF. Stages of change in psychotherapy: A follow-up report. Psychotherapy: Theory, Research, Practice, Training Win. 1989;26(4):494–503. [Google Scholar]
- 45.Pantalon MV, Swanson AJ. Use of the University of Rhode Island Change Assessment to measure motivational readiness to change in psychiatric and dually diagnosed individuals. Psychology of Addictive Behaviors. 2003;17:91–97. doi: 10.1037/0893-164x.17.2.91. [DOI] [PubMed] [Google Scholar]
- 46.Longshore D, Teruya C. Treatment motivation in drug users: A theory-based analysis. Drug and Alcohol Dependence. 2006;81:179–188. doi: 10.1016/j.drugalcdep.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 47.Longshore D. Help-seeking by African American drug users: A prospective analysis. Addictive Behaviors. 1999;24(5):683–686. doi: 10.1016/s0306-4603(98)00111-7. [DOI] [PubMed] [Google Scholar]
- 48.Adair EBG, Craddock SG, Miller HG, Turner CF. Assessing consistency of responses to questions on cocaine use. Addiction. 1995;90:1497–1502. doi: 10.1046/j.1360-0443.1995.901114978.x. [DOI] [PubMed] [Google Scholar]
- 49.Siegal HA, Falck RS, Wang J, Carlson RG. Predictors of drug abuse treatment entry among crack-cocaine smokers. Drug and Alcohol Dependence. 2002;68(2):159–166. doi: 10.1016/s0376-8716(02)00192-8. [DOI] [PubMed] [Google Scholar]


