Abstract
Background
A recent Cochrane meta-analysis did not confirm the benefits of fish and fish oil in the secondary prevention of cardiac death and myocardial infarction. We performed a meta-analysis of randomized controlled trials that examined the effect of fish-oil supplementation on ventricular fibrillation and ventricular tachycardia to determine the overall effect and to assess whether heterogeneity exists between trials.
Methods
We searched electronic databases (MEDLINE, EMBASE, The Cochrane Central Register of Controlled Trials, CINAHL) from inception to May 2007. We included randomized controlled trials of fish-oil supplementation on ventricular fibrillation or ventricular tachycardia in patients with implantable cardioverter defibrillators. The primary outcome was implantable cardioverter defibrillator discharge. We calculated relative risk [RR] for outcomes at 1-year follow-up for each study. We used the DerSimonian and Laird random-effects methods when there was significant heterogeneity between trials and the Mantel-Hanzel fixed-effects method when heterogeneity was negligible.
Results
We identified 3 trials of 1–2 years' duration. These trials included a total of 573 patients who received fish oil and 575 patients who received a control. Meta-analysis of data collected at 1 year showed no overall effect of fish oil on the relative risk of implantable cardioverter defibrillator discharge. There was significant heterogeneity between trials. The second largest study showed a significant benefit of fish oil (relative risk [RR] 0.74, 95% confidence interval [CI] 0.56–0.98). The smallest showed an adverse tendency at 1 year (RR 1.23, 95% CI 0.92–1.65) and significantly worse outcome at 2 years among patients with ventricular tachycardia at study entry (log rank p = 0.007).
Conclusion
These data indicate that there is heterogeneity in the response of patients to fish-oil supplementation. Caution should be used when prescribing fish-oil supplementation for patients with ventricular tachycardia.
There is a public perception that fish and fish oil can be recommended uniformly for the prevention of coronary artery disease.1–3 However, the scientific evidence is divided4,5 and official agencies have called for more research.6
It is estimated that 0.5% of patients with coronary heart disease, 1% of patients with diabetes or hypertension and 2% of the general population at low risk of coronary heart disease take fish-oil supplements.7 In 2004, the price of fish oils overtook that of vegetable oils, and in 2006, the price rose to US$750 per ton.8 The value of fish oil as a nutraceutical in the European market was US$194 million in 2004, and it is anticipated that the price will continue to rise as availability declines.8 Canada is both a consumer and an exporter of fish oil, and it exported 15 000 tons in 2006.9
The scientific debate over the clinical value of fish oil is highlighted by a recent Cochrane review, which concluded that long-chain omega-3 fatty acids (eicosapentaenoic acid and docosahexaenoic acid) had no clear effect on total mortality, combined cardiovascular events or cancer.4 Furthermore, another recent meta-analysis10 only showed a significant positive association between fish-oil consumption and prevention of restenosis after coronary angioplasty in a select subgroup after excluding key negative papers.11 Finally, the antiarrhythmic effect, which is proposed to be the principal mechanism of their benefit in cardiovascular disease, has not been demonstrated clearly in clinical trials.12–14
We therefore performed a meta-analysis of randomized controlled trials that examined the effect of fish-oil supplementation in patients with implantable cardioverter defibrillators who are at risk of ventricular arrhythmia to determine the overall effect of fish oils. We also sought to investigate whether there was significant heterogeneity between trials.
Methods
Data search
We searched the following electronic databases from inception to May 2007: MEDLINE, EMBASE, The Cochrane Central Register of Controlled Trials and CINAHL. The search terms were combined into a single phrase “fish and implantable cardioverter defibrillator and arrhythmia.” The search was restricted to English language articles; however, when the language restriction was removed, we did not identify any additional trials. The search was performed independently by 2 of us (A.R.J. and R.L.).
Selection
We included randomized controlled trials that evaluated fish-oil supplementation in patients with implantable cardioverter defibrillators to prevent the recurrence of ventricular arrhythmia. We included studies where the intervention was consumption of fish-oil capsules (any dose). We excluded nonrandomized trials, letters and reviews; studies of atrial fibrillation or tachycardia and ventricular arrhythmia that did not involve implantable cardioverter defibrillators; and studies of fish-oil given as infusions or consumed as fatty fish. We selected studies involving patients with implantable cardioverter defibrillators because these patients are at high risk for ventricular tachycardia and fibrillation and because these studies provide a good model to study the potential antiarrhythmic effects of fish oil. Furthermore, implantable cardioverter defibrillators allow data to be gathered under controlled conditions over extended periods of supplementation with fish oils and provide an accurate reading of time to first event because of the long-term storage of electrocardiographic data. In contrast, an arrhythmic cause of death is difficult to infer from the history of patients without implantable cardioverter defibrillators.
Validity assessment
We used the Jadad Score to assess the methodologic quality of the included studies,15 and the Cochrane Collaboration Scale to rate study validity.
Data extraction
Data were extracted independently and in duplicate by 2 of us (A.R.J., D.J.A.J.). Extraction was verified by the study statistician (J.B.). All disagreements were resolved by consensus.
Quantitative data synthesis
Two of the trials reported hazard ratios12,14 and 1 reported relative risk [RR];13 thus, we calculated RR for outcomes at 1-year follow-up. We synthesized the outcome data using RR as the effect measure, and we examined heterogeneity using the Q test and I2 statistic.16,17 A RR of 1.0 or less indicates a lower rate of an outcome among patients given fish 0il than among those in the control group. We used the DerSimonian and Laird random-effect method when important and statistically significant heterogeneity existed between trials. The Mantel-Hanzel fixed-effect method was adopted when heterogeneity was negligible. We used the Review Manger (RevMan 4.2.7) statistical software provided by the Cochrane Collaboration for statistical analyses. All tests of significance were 2-sided and statistical significance was defined as p < 0.05.
Results
Trial flow
We identified 8 articles, 5 of which were excluded: 1 because it was a study rationale,18 1 because it was a letter19 and 3 because they were review articles20–22 (Figure 1). The 3 remaining articles were randomized controlled trials and were included in our analysis.12–14

Figure 1: Selection of studies for meta-analysis.
Study characteristics
The 3 trials selected for analysis included patients who were similar in terms of age, sex and mean ejection fraction (Table 1). The patients included in each trial had received an implantable cardioverter defibrillator because of ventricular tachycardia or ventricular fibrillation. The trials by Leaf and colleagues13 and Brouwer and colleagues14 included patients taking sotalol and amiodarone; however, these drugs were part of the exclusion criteria for the trial by Raitt and colleagues.12 The study by Raitt and colleagues reported that digoxin was given to 29% of participants in the intervention group and 33% in the control group. The other 2 studies did not report digoxin use.
Table 1
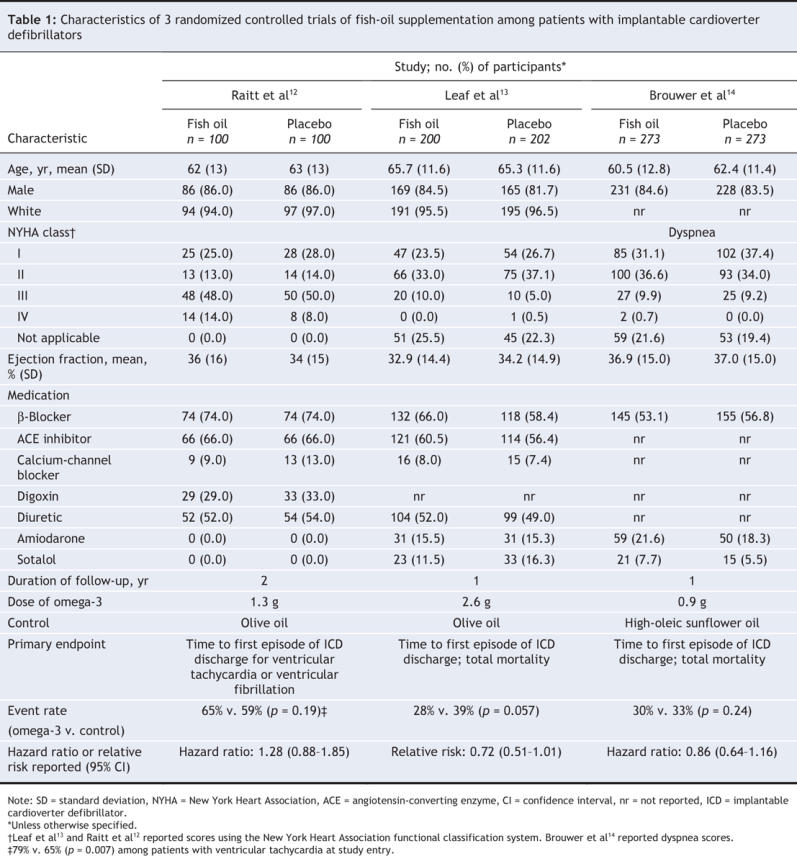
There were differences among the 3 studies in the number of participants and the duration of follow-up (Table 1). The fish-oil dose was 2.6 g/d fish oil in the study by Leaf and colleagues, 1.3 g/d in the study by Raitt and colleagues and 0.9 g/d in the study by Brouwer and colleagues. Brouwer and colleagues reported angina and dyspnea scores, and Leaf and colleagues and Raitt and colleagues reported scores using the New York Heart Association functional classification system. In the study by Raitt and colleagues, the extent of each patient's heart failure was specified; however, 20%–26% of participants' heart failure symptoms were not classified in the other 2 studies. In the study by Raitt and colleagues, 58% of participants in the intervention group and 62% of participants in the control group received a functional class score of III or IV. In contrast, Leaf and colleagues reported that 10% of participants in the intervention group and 6% of participants in the control group received this score, and Brouwer and colleagues reported that 11% of participants in the intervention group and 9% of participants in the control group received this score. The meaning of this difference is unclear, given the similarity in ejection fraction among all 3 studies (Table 1).
All 3 included trials were considered to be of high quality. Each trial received a Jadad Score of 5 out of 5.12–14 The Cochrane Collaboration Scale for rating study validity indicated a low risk of bias (score of A) for all studies.
Data synthesis
Meta-analysis of the 3 trials indicated a nonsignificant relative risk of implantable cardioverter defibrillator discharge during 1 year of fish-oil supplementation of (RR 0.93, 95% confidence interval [CI] 0.70–1.24, p = 0.63) (Figure 2). None of the 3 studies reported a benefit of fish oils in their primary analysis. However, when we recalculated relative risk based on the data available from the study by Leaf and colleagues, we found a significant benefit of fish oil (RR 0.74, 95% CI 0.56–0.98, p < 0.05).
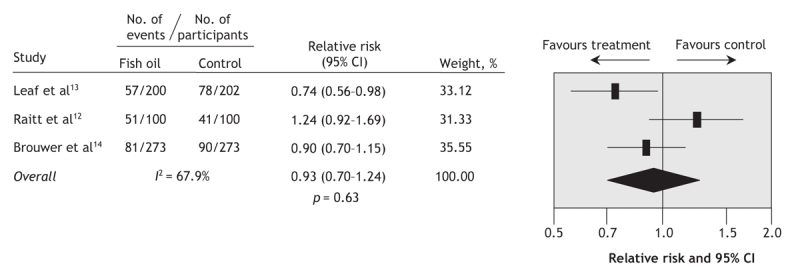
Figure 2: Meta-analysis of implantable cardioverter defibrillator discharge in studies of fish-oil supplementation. Significant heterogeneity was detected between trials (p = 0.04). Note: CI = confidence interval.
The meta-analysis of the 3 studies established significant heterogeneity (p = 0.04), therefore we also performed sensitivity analyses. We detected significant heterogeneity between the studies by Raitt and colleagues12 and Leaf and colleagues13 (p = 0.01). No significant heterogeneity was observed between the studies by Leaf and colleagues and Brouwer and colleagues14 (p = 0.30) or between the studies by Raitt and colleagues and Brower and colleagues (p = 0.10). Using a fixed-effects model to pool the studies by Leaf and colleagues and Brower and colleagues, we observed a significant positive effect of fish oil on implantable cardioverter defibrillator discharge (RR 0.83, 95% CI 0.69–0.99, p = 0.04) (Figure 3).

Figure 3: Sensitivity analysis of the trials by (A) Leaf et al13 and Brouwer et al14; (B) Raitt et al12 and Brouwer et al14; and (C) Raitt et al12 and Leaf et al.13 Significant heterogeneity was detected between the trials by Raitt et al12 and Leaf et al13 (p = 0.01). Note: CI = confidence interval. *Number of participants who experienced an implantable cardioverter defibrillator discharge.
We also performed a meta-analysis of all-cause mortality, which was an outcome common to all 3 studies (Figure 4). The follow-up period was 1 year for the studies by Leaf and colleagues and Brouwer and colleagues, and it was 2 years for the study by Raitt and colleagues. The overall RR for all-cause mortality was not significant (RR 0.70, 95% CI 0.42–1.15, p = 0.15). In addition, the confidence intervals for each study crossed the line of unity (Figure 4). Results of the test for heterogeneity were not significant (p = 0.29).

Figure 4: Meta-analysis of all-cause mortality in studies of fish-oil supplementation among patients with implantable cardioverter defibrillators. No significant heterogeneity was detected (p = 0.29). Note: CI = confidence interval.
Interpretation
Our meta-analysis suggests that there is significant heterogeneity in response to fish-oil supplementation among patients with implantable cardioverter defibrillators. This supports the theory that although some patients may benefit from supplementation with docosahexaenoic acid and eicosapentaenoic acid, others may not benefit or may be adversely affected.
The reason for the observed differences in 1-year recurrence-free survival among the 3 randomized controlled trials is not clear. However, the differences do not appear to be related to differences in cardiac status (Table 1). All patients received implantable cardioverter defibrillators for “secondary prophylaxis,” and the mean ejection fraction in the 3 studies was similar (Table 1). In 2 of the trials,12,13 patients with worse left-ventricular function who received fish oil appeared to have improved outcomes. A similar result was also found in a post-hoc analysis of the GISSI-Prevenzione trial.23
It is possible that drug–nutrient interactions may be, in part, responsible for the observed differences between studies. Of the 3 trials, the 2 that showed either a benefit of fish oil13 or no adverse events14 included a substantial number of patients who were taking antiarrhythmic drugs (sotalol and amiodarone). Potential drug–nutrient interactions have also been proposed as a reason for the differences in response to fish oil observed between the Diet and Reinfarction Trial (DART) and the Diet and Angina Randomization Trial (DART-2).24,25 In the Diet and Angina Randomization Trial, β-blockers and calcium-channel blockers (nifedipine) appeared to protect against myocardial infarction in men with angina who received fish or fish oil.25
Two recent meta-analyses failed to demonstrate a clear advantage of increased fish-oil consumption, either for secondary prevention of coronary heart disease or restenosis after angioplasty.4,10 In the first meta-analysis, the adverse events observed among patients with angina in the trial by Burr and colleagues24 contributed to an overall nonsignificant effect of fish oil on secondary prevention of coronary heart disease.4 In the second meta-analysis, despite a significant benefit in a clinical subgroup, which defined restenosis as recurrent stenosis of at least 50% in any vessel, no overall advantage was seen for fish oils in preventing restenosis after angioplasty.10 This result was consistent even when 1 major trial with a negative effect was omitted.11 Nevertheless, there are extensive positive pre-clinical data and some individual randomized controlled trials that suggest a benefit of fish-oil supplementation.13,26–28 Furthermore, a recent meta-analysis found a benefit of fish-oil supplementation and found no adverse effects related to contamination of fish.5 Despite these positive findings, recent meta-analyses of randomized controlled trials in all 3 areas related to coronary heart disease (secondary prevention, post-angioplasty restinosis, ventricular tachycardia and fibrillation) have not demonstrated a clear benefit for fish and fish oils but have shown significant between-study heterogeneity.4,10
The importance of randomized controlled trials of implantable cardioverter defibrillator and fish oils is that they explore a key mechanism by which omega-3 fatty acids have been suggested to confer cardiovascular benefit, namely, their direct antiarrhythmic effects.29,30 Trials have emphasized the early divergence of the Kaplan–Meier survival curves in secondary prevention of cardiovascular disease in studies of both fish oil and omega-3 vegetable oil.31,32 In these studies, the reduction in the number of coronary heart disease events started too soon after initiating supplementation to be caused by regression of arteriosclerotic lesions in coronary arteries. Furthermore, no changes were seen in serum lipids that would be predicted to reduce atheroma formation with the use of omega-3 fatty acids from fish or vegetables.
Some statin trials have shown early divergence of Kaplan– Meier curves by 1 year, and in this instance, the explanation may also not be related to atheroma regression but to plaque stabilization possibly because of statin's anti-inflammatory effects.33,34
A potential criticism of the implantable cardioverter defibrillator trials is that they collectively involved a relatively small number of patients compared to the GISSI-Prevenzione trial26 or the Japan EPA Lipid Intervention study,28 which included 11 324 and 18 645 participants respectively. The implantable cardioverter defibrillator trials included in our meta-analysis involved patients with pre-existing arrhythmia (secondary prophylaxis); however, the GISSI-Prevenzione trial and Japan EPA Lipid Intervention study were, in effect, studies of primary prophylaxis in which the mechanism of death may be quite different (e.g., ischemic ventricular fibrillation as opposed to scar-related ventricular tachycardia). In addition, in the GISSI-Prevenzione trial, early sudden death at 4 months (used as a marker for the potential anti-arrhythmic effects of fish oil) showed a significant difference favouring fish oil. However, the total number of participants at 4 months was not reported.31 At 3 months, there were 26 sudden deaths in the fish-oil group and 37 in the control group. In comparison, implantable cardioverter defibrillator discharge occurred in a total of 398 patients in the 3 implantable cardioverter defibrillator studies (fish oil, 189; control, 209; p = 0.63)12–14 and represents a substantially greater number of end-point events. Furthermore, the total number of all-cause deaths in these studies (n = 61) was of a similar order of magnitude to the sudden deaths in the GISSI-Prevenzione trial at 4 months, the time point at which significance was achieved.31
The discharge of implantable cardioverter defibrillators has also been used as a surrogate marker for sudden death. Leaf and colleagues reported deaths attributed directly to arrhythmia. They reported 3 deaths in the fish oil group and 1 in the control; thus, there were too few deaths for any conclusions to be made.13
Other studies have assessed the effect of fish-oil supplementation on cardiac rhythm in patients without implantable cardioverter defibrillators. In 2 studies that included patients with frequent premature ventricular complexes, fish-oil supplementation did not reduce the number of premature ventricular complexes.35,36 Among patients who had experienced myocardial infarction, fish-oil supplementation either did not reduce the number of ventricular extrasystoles37 or it increased heart-rate variability.38 Conclusive evidence for an antiarrhythmic benefit of fish oil in these studies is lacking; however, several studies suggest that fish oils decrease heart rate.35,39,40 Yet even among these studies, the data on changes in the electrocardiographic characteristics are inconsistent.36
Heterogeneity is an important issue in systematic reviews and meta-analyses. There are 2 main analytical approaches to dealing with heterogeneity: incorporating it into the analysis (using random-effects models) or explaining it (using meta-regression techniques or subgroup analyses, or both). Lau and colleagues41 have provided a useful flowchart that summarizes the ways that heterogeneity is being dealt with in the systematic-review literature, which includes ignoring heterogeneity completely (i.e., using a fixed-effects model) or not pooling the data. We chose to incorporate heterogeneity using a random-effects model, because we believed that the combined result was conservative and more honest (wider confidence intervals and larger p values), and that it reflected the uncertainty of the treatment effect. Furthermore, 1 of the studies included in our analysis appeared to be the main source of the observed heterogeneity, which led us to investigate the sensitivity of the meta-analysis results by excluding 1 study at a time. We also believed that the best approach to dealing with heterogeneity was to try to explain it using meta-regression techniques and subgroup analyses. However, because there were only 3 studies available for our meta-analysis, these approaches were not practical.
Fish oils have complex and pleiotropic effects that may affect the heart. These effects include blocking cardiac ion channels, reducing fibrosis in response to mechanical stress,42 decreasing blood coagulation, reducing serum triglycerides43 and possibly altering immune function. Studies in different patient populations with different pathophysiologies and therapeutic regimens have all produced divergent results. Early randomized controlled trials of secondary prevention suggested that supplementation with docosahexaenoic acid and eicosapentaenoic acid reduces cardiac events. However, more recent data suggest that caution should be exercised when analyzing data from certain subgroups, such as men with stable angina.24 The same may also be true for data from patients with implantable cardioverter defibrillators who have a history of ventricular tachycardia and who are not taking antiarrhythmic medications.12 The need for further research has been called for by official agencies.6 Large randomized controlled trials are needed to address the question of controlling ventricular arrhythmia with long-chain omega-3 fatty acids. Large trials are also needed to define the effects of long-chain omega-3 fatty acids in patients with heart failure and angina. These trials must be sufficiently large or selective to address the effects of cointerventions, especially the use of antiarrhythmic drugs. In view of the biochemical block in the conversion of eicosapentaenoic acid to docosahexaenoic acid44 and the environmental concerns over depletion of fish stocks, studies should include commercial docosahexaenoic acid from phytoplankton. This fatty acid is already being used in infant formula in Europe.45 The use of commercial fatty acids such as docosahexaenoic acid will allow the role of this specific fatty acid to be assessed, something that cannot be done using the current mixtures. In addition, comparisons should be made using α-linolenic acid, a shorter chain-length omega-3 fatty acid from vegetable sources, which has shown promise in preventing recurrence of coronary heart disease.32,46 At present, the use of fish oils in patients with implantable cardioverter defibrillators appears to warrant caution.
@ See related articles, pages 150, 177 and 181
Footnotes
Une version française de ce résumé est disponible à l'adresse www.cmaj.ca/cgi/content/full/178/2/157/DC1
This article has been peer reviewed.
Contributors: David Jenkins and Andrea Josse were responsible for the conception and acquisition of the data. David Jenkins, Andrea Josse, Joseph Beyene and Paul Dorian were responsible for the study design and drafted the manuscript. All of the authors contributed to the analysis and interpretation of data, revised the manuscript critically for important intellectual content and approved the version to be published.
Competing interests: None declared for Andrea Josse, Joseph Beyene, Paul Dorian, Michael Burr, Roxanne LaBelle, Cyril Kendall and Stephen Cunnane. David Jenkins has served on scientific advisory board, received consultants fees or has received honorarium from Barilla, Solae, Unilever, Haine Celestial, Loblaw's Supermarkets, Sanitarium Company, Herbalife International, Pacific Health Laboratories Inc., Metagenics/MetaProteomics, Bayer Consumer Care, Oldways Preservation Trust, The Almond Board of California, The California Strawberry Commission, Orafti, and Canola and Flax Councils.
Correspondence to: Dr. David J.A. Jenkins, Clinical Nutrition and Risk Factor Modification Centre, St. Michael's Hospital, 61 Queen St. East, Toronto ON M5C 2T2; fax 416 978-5310; cyril.kendall@utoronto.ca
REFERENCES
- 1.CBC News. Contaminated fish? Benefits outweigh the risks. Toronto: Canadian Broadcasting Corporation; 2007. Available: www.cbc.ca/news/background/foodsafety/fish.html (accessed 2007 Aug 15).
- 2.BBC.co.uk. Guidance on oily fish consumption. London (UK): BBC; 2004. Available: http://news.bbc.co.uk/1/hi/health/3834955.stm (accessed 2007 Aug 15).
- 3.Barton A. How flawed is your fish? Globe and Mail [Toronto] 2007. Available: www.theglobeandmail.com/servlet/story/RTGAM.20070516.wxlfish16/BNStory/GlobeSportsHockey/ (accessed 2007 Nov 20).
- 4.Hooper L, Thompson RL, Harrison RA, et al. Risks and benefits of omega-3 fats for mortality, cardiovascular disease and cancer: systematic review. BMJ 2006;332:752-60. [DOI] [PMC free article] [PubMed]
- 5.Mozaffarian D, Rimm EB. Fish intake, contaminants and human health: evaluating the risks and the benefits. JAMA 2006;296:1885-99. [DOI] [PubMed]
- 6.Kris-Etherton PM, Harris WS, Appel LJ. Fish consumption, fish oil, omega-3 fatty acids and cardiovascular disease. Circulation 2002;106:2747-57. [DOI] [PubMed]
- 7.Buettner C, Phillips RS, Davis RB, et al. Use of dietary supplements among United States adults with coronary artery disease and atherosclerotic risks. Am J Cardiol 2007;99:661-6. [DOI] [PubMed]
- 8.FOOD productiondaily.com. Global fish oil production down in 2005. France: Decision News Media; 2006. Available: www.foodproductiondaily.com/news/ng.asp?id=66435-fish-oil-omega (accessed 2007 Aug 15).
- 9.National Oceanic and Atmospheric Administration Fisheries: Office of Science and Technology. Quarterly fish meal and oil production (first quarter). Washington: US Census Bureau; 2007. Available: www.st.nmfs.gov/st1/market_news/doc76.txt (accessed 2007 Aug 15).
- 10.Balk EM, Lichtenstein AH, Chung M, et al. Effects of omega-3 fatty acids on coronary restenosis, intima-media thickness, and exercise tolerance: a systematic review. Atherosclerosis 2006;184:237-46. [DOI] [PubMed]
- 11.Leaf A, Jorgensen MB, Jacobs AK, et al. Do fish oils prevent restenosis after coronary angioplasty? Circulation 1994;90:2248-57. [DOI] [PubMed]
- 12.Raitt MH, Connor WE, Morris C, et al. Fish oil supplementation and risk of ventricular tachycardia and ventricular fibrillation in patients with implantable defibrillators: a randomized controlled trial. JAMA 2005;293:2884-91. [DOI] [PubMed]
- 13.Leaf A, Albert CM, Josephson M, et al. Prevention of fatal arrhythmias in high-risk subjects by fish oil n-3 fatty acid intake. Circulation 2005;112:2762-8. [DOI] [PubMed]
- 14.Brouwer IA, Zock PL, Camm AJ, et al. Effect of fish oil on ventricular tachyarrhythmia and death in patients with implantable cardioverter defibrillators: the Study on Omega-3 Fatty Acids and Ventricular Arrhythmia (SOFA) randomized trial. JAMA 2006;295:2613-9. [DOI] [PubMed]
- 15.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12. [DOI] [PubMed]
- 16.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [DOI] [PubMed]
- 17.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed]
- 18.Brouwer IA, Zock PL, Wever EF, et al. Rationale and design of a randomised controlled clinical trial on supplemental intake of n-3 fatty acids and incidence of cardiac arrhythmia: SOFA. Eur J Clin Nutr 2003;57:1323-30. [DOI] [PubMed]
- 19.I have an implantable cardioverter defibrillator (ICD), and I've been taking fish oil supplements because I had heard of their potential heart benefits. However, I recently read they might not be safe for people with ICDs. Should I stop taking them? Johns Hopkins Med Lett Health After 50 2005;17:8. [PubMed]
- 20.Brouwer IA, Geelen A, Katan MB. n-3 Fatty acids, cardiac arrhythmia and fatal coronary heart disease. Prog Lipid Res 2006;45:357-67. [DOI] [PubMed]
- 21.Jacobson TA. Secondary prevention of coronary artery disease with omega-3 fatty acids. Am J Cardiol 2006;98:61i-70i. [DOI] [PubMed]
- 22.Cleland JG, Coletta AP, Lammiman M, et al. Clinical trials update from the European Society of Cardiology meeting 2005: CARE-HF extension study, ESSENTIAL, CIBIS-III, S-ICD, ISSUE-2, STRIDE-2, SOFA, IMAGINE, PREAMI, SIRIUS-II and ACTIVE. Eur J Heart Fail 2005;7:1070-5. [DOI] [PubMed]
- 23.Macchia A, Levantesi G, Franzosi MG, et al. Left ventricular systolic dysfunction, total mortality, and sudden death in patients with myocardial infarction treated with n-3 polyunsaturated fatty acids. Eur J Heart Fail 2005;7:904-9. [DOI] [PubMed]
- 24.Burr ML, Ashfield-Watt PA, Dunstan FD, et al. Lack of benefit of dietary advice to men with angina: results of a controlled trial. Eur J Clin Nutr 2003;57:193-200. [DOI] [PubMed]
- 25.Burr ML, Dunstan FD, George CH. Is fish oil good or bad for heart disease? Two trials with apparently conflicting results. J Membr Biol 2005;206:155-63. [DOI] [PubMed]
- 26.GISSI-Prevenzione. Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto miocardico. Lancet 1999;354:447-55. [PubMed]
- 27.Burr ML, Fehily AM, Gilbert JF, et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet 1989;2:757-61. [DOI] [PubMed]
- 28.Yokoyama M, Origasa H, Matsuzaki M, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet 2007;369:1090-8. [DOI] [PubMed]
- 29.Leaf A. Prevention of sudden cardiac death by n-3 polyunsaturated fatty acids. Fundam Clin Pharmacol 2006;20:525-38. [DOI] [PubMed]
- 30.Leaf A. Omega-3 fatty acids and prevention of arrhythmias. Curr Opin Lipidol 2007;18:31-4. [DOI] [PubMed]
- 31.Marchioli R, Barzi F, Bomba E, et al. Early protection against sudden death by n-3 polyunsaturated fatty acids after myocardial infarction: time-course analysis of the results of the Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico (GISSI)-Prevenzione. Circulation 2002;105:1897-903. [DOI] [PubMed]
- 32.de Lorgeril M, Renaud S, Mamelle N, et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet 1994;343:1454-9. [DOI] [PubMed]
- 33.Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med 1995;333:1301-7. [DOI] [PubMed]
- 34.Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA 1998;279:1615-22. [DOI] [PubMed]
- 35.Geelen A, Brouwer IA, Schouten EG, et al. Effects of n-3 fatty acids from fish on premature ventricular complexes and heart rate in humans. Am J Clin Nutr 2005;81:416-20. [DOI] [PubMed]
- 36.Geelen A, Zock PL, Brouwer IA, et al. Effect of n-3 fatty acids from fish on electrocardiographic characteristics in patients with frequent premature ventricular complexes. Br J Nutr 2005;93:787-90. [DOI] [PubMed]
- 37.Hardarson T, Kristinsson A, Skuladottir G, et al. Cod liver oil does not reduce ventricular extrasystoles after myocardial infarction. J Intern Med 1989;226:33-7. [DOI] [PubMed]
- 38.Christensen JH, Gustenhoff P, Korup E, et al. Effect of fish oil on heart rate variability in survivors of myocardial infarction: a double blind randomised controlled trial. BMJ 1996;312:677-8. [DOI] [PMC free article] [PubMed]
- 39.Mozaffarian D, Geelen A, Brouwer IA, et al. Effect of fish oil on heart rate in humans: a meta-analysis of randomized controlled trials. Circulation 2005;112:1945-52. [DOI] [PubMed]
- 40.O'Keefe JH Jr, Abuissa H, Sastre A, et al. Effects of omega-3 fatty acids on resting heart rate, heart rate recovery after exercise, and heart rate variability in men with healed myocardial infarctions and depressed ejection fractions. Am J Cardiol 2006;97:1127-30. [DOI] [PubMed]
- 41.Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med 1997;127:820-6. [DOI] [PubMed]
- 42. Laurent G, Moe G, Hu X, et al. Long chain n-3 polyunsaturated fatty acids reduce atrial vulnerability in a novel canine pacing model. Cardiovasc Res 2007 Epub 2007 Oct 21 ahead of print. [DOI] [PubMed]
- 43.Bays H. Clinical overview of Omacor: a concentrated formulation of omega-3 polyunsaturated fatty acids. Am J Cardiol 2006;98:71i-6i. [DOI] [PubMed]
- 44.Plourde M, Cunnane SC. Extremely limited synthesis of long chain polyunsaturates in adults: implications for their dietary essentiality and use as supplements. Appl Physiol Nutr Metab 2007;32:619-34. [DOI] [PubMed]
- 45.Fleith M, Clandinin MT. Dietary PUFA for preterm and term infants: review of clinical studies. Crit Rev Food Sci Nutr 2005;45:205-29. [DOI] [PubMed]
- 46.Singh RB, Dubnov G, Niaz MA, et al. Effect of an Indo-Mediterranean diet on progression of coronary artery disease in high risk patients (Indo-Mediterranean Diet Heart Study): a randomized single-blind trial. Lancet 2002;360:1455-61. [DOI] [PubMed]


