It has become commonplace in accounts of medicine in the second half of the twentieth-century to ascribe an “antibiotic revolution” to the years when penicillin became widely available from the early 1950s. However, to date there have been hardly any studies that demonstrate a major discontinuity in medical practices after mid-century, let alone that go on to specify their character.1 There would seem to be two key features of any “antibiotic revolution”: first and foremost that the treatment of diseases was transformed as doctors were able to cure illness caused by infections with specific drugs that eliminated causative bacteria; and second that the ambition of doctors to intervene with drugs in a number of diseases grew, as did the ability of the pharmaceutical industry to supply an increasing range of targeted and effective remedies.2 In this article we contribute towards an assessment of the first of these key features by discussing the changing management of acute bronchitis from the mid-1940s to the early 1960s. The disease was amongst the most prevalent and important of that period in Britain, being the single largest cause of consultations with general practitioners (GPs) through much of the 1950s. Bronchitis was also the subject of many high profile debates among doctors and health care agencies as concerns about its morbidity and mortality touched on such issues as smoke pollution, the costs of the National Health Service (NHS) and changes in the doctor–patient relationship. The evidence of contemporary studies shows that the treatment of acute bronchitis changed radically after the introduction of antibiotics, such that by the mid-1950s over 80 per cent of patients diagnosed with the condition were prescribed penicillin or another antibacterial drug—a shift that was not supported by any clinical trials or systematic evidence.3 How and why this change occurred are the questions we set out to answer.
As well as addressing the specific issue of the impact of antibiotic therapy on the management of a single disease, our analysis also illuminates three other larger themes. Firstly, the aetiology, pathology and management of acute bronchitis was already contested in the 1940s, and this situation was further destabilized by antibiotics, so we have necessarily explored the changing medical constructions of the disease. Secondly, the introduction and widespread use of antibiotics coincided with the establishment of the NHS, so we also consider the inter-relations between changes in clinical practice and the new health care structures and policies after 1948. Finally, our discussion is relevant to current clinical practice because chest illnesses, such as acute bronchitis, remain the commonest reason for GP consultation in Britain, and most cases continue to be treated with antibiotics, even though evidence suggests that these drugs do little to affect the natural history of the illness, which is normally self limiting.4 Thus, it is likely that the legacy of the use and probable overuse of antibiotics for acute bronchitis, which emerged so strongly during the 1950s, has contributed substantially to the current alarming problems of antibiotic resistance, as well to the proliferation of side effects and the rising costs of health care.5
We begin by discussing the prevalence and importance of acute bronchitis from the late 1940s to the early 1960s and highlight the fact that the British were a particularly “chesty” nation and that this chestiness was mainly attributed to climate and the urban industrial environment. In this context, it is important to recognize that acute bronchitis was seen as infective rather than infectious; that is, bacteria were understood to be opportunistic, secondary infective agents of bronchi that had been inflamed by other physical, chemical and biological agents. Our discussion then moves on to look briefly at the public profile of the disease and the advice given to the public by doctors and the press. We identify three phases in the changing advice offered to doctors in published sources: a pre-antibiotic period in the 1940s; a period from the late 1940s to the mid-1950s when antibiotics were recommended only for complications and serious disease; and finally a period from the late-1950s when antibiotics were recommended for all cases of the disease. Finally, we analyse the influence of three non-clinical factors on the management of the disease: the structures and policies of the NHS; the pharmaceutical industry; and public pressures.
Acute Bronchitis in Britain in the 1950s
Leading medical textbooks in the late 1940s and early 1950s characterized acute bronchitis as a common, self-limiting but inconvenient illness, arising as a result of exposure to cold or to sudden changes in temperature or inhalation of irritating dusts or vapours (including smog). Bacteria and their by-products were assumed to play a role in secondary infection, or less commonly as primary irritating agent.6 The illness often started with catarrh or common cold symptoms and progressed to constitutional upset, fever, irritating dry cough, wheezing and rawness in the throat, and retrosternal discomfort. After a few days sputum production developed, and became copious and often discoloured (purulent). Mild fever of 100–103°F was common and in the chest, bilateral wheezes and crackles were the main diagnostic indicators. The presence of variable bilateral signs in the chest was seen as important in differentiating the illness from pneumonia, when the signs were usually one-sided. The symptoms then gradually settled spontaneously, although the cough often extended for three or four weeks. Chronic bronchitis was distinguished from the acute form by the absence of fever and pain, and a persistent and distinctive daily pattern of coughing phlegm.7
Such descriptions reveal that the diagnosis of acute bronchitis was made not by X-ray or laboratory tests, but by clinical judgement, based on the presence of a constellation of common signs and symptoms—principally a cough—that were shared by many other syndromes such as the common cold, simple cough, influenza and upper respiratory infections. The Chief Medical Officer, Dr J A Charles, in his 1958 annual report, devoted a whole section to the importance of the common respiratory diseases and the difficulty of diagnosing clinical syndromes such as bronchitis, pneumonia, influenza and upper respiratory infections in primary care, stating:
The differentiation on clinical grounds of “influenza”, for example, from other acute febrile respiratory illnesses is often quite arbitrary. This arises not so much from any defect of clinical judgment in individual cases as from the very nature of this group of illnesses, which present many gradations and combinations of symptoms …8
The Research Committee of the College of General Practitioners noted there were over 150 synonyms of acute respiratory infections, and that any classification based on identifying specific causes or the seat of the disease was near impossible in general practice.9
In the late 1940s, respiratory illness, particularly bronchitis, was by far the commonest reason for consultations with GPs, accounting for 41 per cent in the winter and 21 per cent in the summer in one urban practice.10 There was concern amongst employers and the government about working days lost, for example, in 1950–51 bronchitis was surpassed only by influenza as the reason for absence.11 Bronchitis was the commonest reason for GPs to issue sickness certificates, with 29 per cent of all certificates in 1953 being due to respiratory diseases.12 When Drs John and Elizabeth Horder, a husband-and-wife partnership, recorded the reasons for consultation in their general practice in London in 1954, bronchitis topped the list in the winter ahead of the common cold.13 A study in 1956 estimated that there were one million sufferers of acute chest infections, including acute bronchitis, in Britain each year.14 Between 1950 and 1951, one north-west London general practice reported that between 20 and 40 per cent of the work of the practice consisted of acute respiratory infection; most cases were not serious, but three-quarters of them were given a prescription.15 Such studies showed that acute bronchitis affected not only the older patients, but was a surprisingly common cause of consultation in younger adults, especially women, with younger and middle-aged women consulting twice as often as men.16 This high consultation and prescription rate for acute bronchitis is perhaps unsurprising, as its cardinal feature is a cough, and coughs are very common and often irritating enough to trigger a visit to the GP. As late as 1974, a two-week random survey found that coughs and sputum affected one-third of British adults.17
The Public and Acute Bronchitis in the 1950s
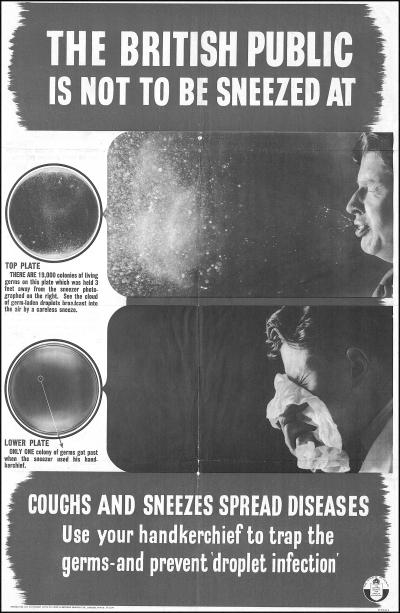
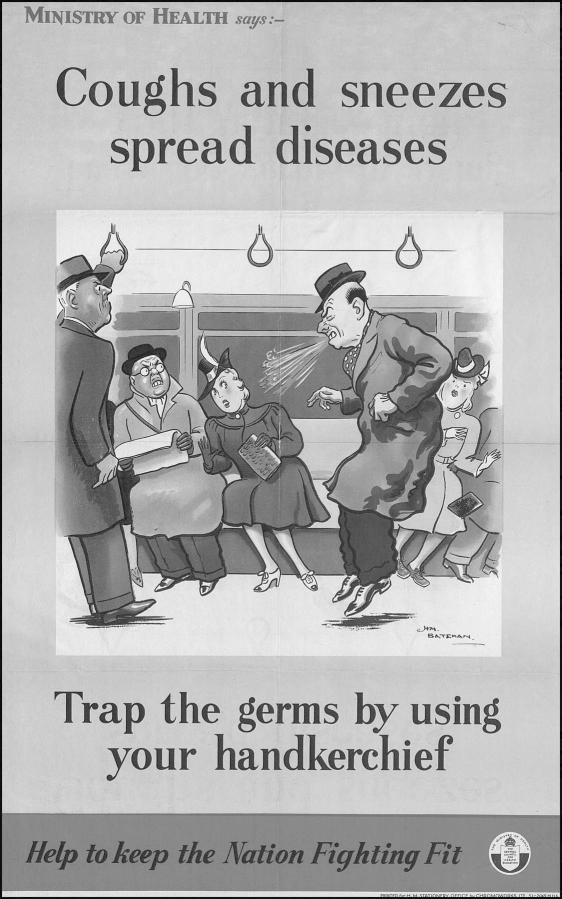
The profile of the disease was maintained in the public sphere by its frequent mention as a cause of illness in the rich and famous. Not infrequently, members of parliament or social figures were reported to be “consigned to bed with a sharp attack of bronchitis” in the Court Circular and News in Brief sections of The Times. The Maharaja of Indore was noted to be convalescing after a mild attack of bronchitis in July 1947 and Boo-Boo II, London Zoo's oldest chimpanzee died suddenly of acute bronchitis on 14 January 1949.18 Dr Fisher, the Archbishop of Canterbury was unable to take the service at the funeral of King George VI on 11 February 1952 being “confined to his room at Lambeth Palace with bronchitis”—the Archbishop of York presided instead.19 The public may also have been encouraged to see coughs as being caused by bacteria by the change in the Ministry of Health “coughs and sneezes spread diseases” poster campaign, with the medicalized 1951 version (Figure 1) showing culture plates covered in bacterial colonies from someone's cough and sneeze, compared with the more cartoon style one for 1941 (Figure 2).
Figure 1.
Ministry of Health poster, London, HMSO, 1951 (NA PRO BN10/218).
Figure 2.
Ministry of Health poster, London, HMSO, 1941 (NA PRO BN10/218).
The public were made aware of the potential seriousness of bronchitis by many authorities. In 1955, The Times echoed the views of the medical profession, indicating bronchitis, the common cold and influenza as three of the five conditions that caused the greatest burden “upon the individual, the employer, the community and the doctor”.20 Press reports during influenza outbreaks emphasized the significant death rate from bronchitis and pneumonia; for example, The Times reported that in Liverpool in January 1951 the death rate had quadrupled, mostly due to bronchitis and pneumonia after influenza.21 In 1954, the British Medical Association's (BMA) Family Doctor magazine published an article, responding to what doctors saw as unnecessary consultations, which discussed when a patient should see their GP when troubled by flu or a cough. The author suggested “don't bother him and make him more overworked. Far better to have the smug satisfaction of curing yourself.”22 The press also highlighted the dangers of bronchitis during the winter smogs.23 The Chief Medical Officer reported that the London fog of 5–8 December 1952 resulted in 3500 to 4000 excess deaths, mostly due to bronchitis, and in one week the bronchitis death rate increased ninefold.24
Advice on the Management of Acute Bronchitis
Acute bronchitis was mostly treated by GPs, with relatively few cases going to hospital. This situation highlighted a problem that the government and the profession wrestled with in the 1950s; namely, that hospital-based medical education did not prepare newly qualified doctors for general practice. There is no doubt that new GPs brought both more up-to-date knowledge and hospital habits to primary care, as subsequent studies showed younger GPs were more likely to prescribe antibiotics than their more experienced, older partners.25 However, young doctors entering general practice in the late 1940s and 1950 had not been taught to deal with the plethora of often mild, self-limiting and ill-defined illness seen in the consulting room. This was brought out in the damning report in March 1950 on the state of general practice in England by the Australian Dr Joseph Collings, which commented in particular on poor education, standards and morale.26 In one of many responses to the Lancet, Anthony Ryle, a newly qualified doctor, wrote: “At present, medical education fails to give a balanced view of the rôle of medicine. Taught entirely in well-equipped hospitals where patients, isolated from their homes and jobs, are analysed in fine detail, medical students are but distantly aware of the scope of general practice, and young doctors enter it ignorant of its problems and unprepared for the effort required to maintain professional standards.”27 The BMA's 1950 report on General practice and the training of the general practitioner, had recommended three postgraduate training years including a year as a trainee with an approved established general practitioner, but this was not instituted for several years.28 In 1953, only Manchester and Edinburgh medical schools had units teaching the principles of general practice to their medical students.29 Thus, newly qualified doctors entering general practice during the 1950s had to depend upon their hospital training and textbooks, and, because of the absence of professional updating, they, like their more experienced colleagues, also relied upon the medical press, prescribing formulae and information from pharmaceutical representatives to learn of new developments. Concerns about the inappropriate training of doctors going into general practice were highlighted as late as 1962 when a report in The Times, under the headline ‘Student doctor baffled by influenza. Training criticized’, reported the complaints of a GP that young doctors had never seen cases of bronchitis or influenza.30 This article tracks the changing ideas about the management of acute bronchitis through the many editions of widely used textbooks, the National Formulary and Prescribers’ Notes.31 Later we also discuss the nature and influence of pharmaceutical companies’ promotional activities. Clearly individual doctors made their own choices and there were wide variations in the extent to which they kept up with new treatments. Indeed this freedom was defended by GP leaders, the Council of the College of General Practitioners commenting to the Hinchcliffe Committee, “We believe it should be left to the doctor in change of a case to use his discretion concerning use of drugs”.32 However, they also recommended an independent body to assess new drugs and advise doctors on appropriate prescribing of these, and as a result all GPs were sent free the Prescribers’ Journal, an independent regular publication, as well as the National Formulary.33 Indeed the first eight editions of the Prescribers’ Journal included nine chapters on antibiotics and three on respiratory tract infections, emphasizing the importance that was increasingly given to appropriate antibiotic prescribing by GPs. In addition, the Medical Letter was produced by the Consumers’ Association of England from 1962 as a non-profit making publication with advice on drugs and therapeutics, but it cost GPs three guineas per year.
Before Antibiotics
The 1944 edition of the Textbook of medical treatment devoted eleven pages to acute bronchitis, concentrating on symptomatic management of the patient, with detailed advice on bed rest in a warm well-ventilated room, a light diet, the use of steam inhalations, local heat poultices to the chest, special woollen and flannel bed wear, medicines to suppress cough or aid expectoration, and sedatives.34 Oxygen and even blood-letting were suggested, with 10 to 20 oz of blood advised for more severe cases. Convalescence of two to four weeks before returning to work was recommended, and this was to include sunshine, a change of air and scenery, good nourishing food and breathing exercises morning and evening. Better-off patients were urged to take a holiday at the seaside. Such a regime demanded considerable commitment of time, effort and resources from the patient, his or her family and medical practitioner. The only specific therapy mentioned was the use of sulphonamides for treating complications. Doctors worried that acute bronchitis could lead to pneumonia, a condition greatly feared in the profession and by the public.35 The 1946 eighteenth edition of Black's medical dictionary warned of the potential for the inflammation to spread into the small bronchial tubes or the lung causing capillary bronchitis or pneumonia, particularly in the young, the elderly or those with underlying disease or “addicted to intemperance”.36 Sulphonamides were antibacterial chemotherapeutic agents that had been introduced in the mid-1930s. At that time, hopes for chemotherapy to treat infections were at a low ebb, science having failed to live up to Paul Ehrlich's prediction at the turn of the century that researchers should be able to produce “magic bullets” that would kill disease germs but leave host cells unharmed. Although sulphonamides were effective against a relatively small number of bacteria, such as those causing puerperal fever, erysipelas and pneumonia, where they had replaced serum therapy, they did alter the prospects for antibacterial therapy and were one factor that had prompted the search for new antibiotics in the late 1930s.37
Strict bed rest had been the traditional management for bronchitis for decades, but was criticized by Derek Dunlop, professor of therapeutics at Edinburgh University in his 1949 address to the Nottingham Medico-Chirurgical Society entitled ‘Modern concepts in therapeutics’.38 In attacking many of the fads and fashions of the previous fifteen years he asserted, “bed rest should be ordered with the same care as one would prescribe a dangerous drug”. Similarly Thomas Anderson, a Reader in infectious diseases at the University of Glasgow, stressed in 1952 the importance of early mobilization for the elderly with acute bronchitis as “it increases the depth of respiration, enhances the capacity to cough and so to clear the respiratory passages and, in most cases, produces a marked mental stimulation of the patient”.39
The National War Formulary of 1941 produced by the Ministry of Health to advise doctors on prescribing emphasized the importance of austerity in all aspects of drug use, commenting that use was “justified only if the drugs are required for essential medical purposes. Many important substances are available in but limited amounts for medicinal purposes. They are more urgently required for other branches of the nation's war effort”.40 By 1947 some relaxation was evident in the third edition, although caution in prescribing was required to “assist the nation's economic recovery”, which had been hit by a particularly severe winter.41
Antibiotics for Patients with Severe Disease
The 1949 edition of the Textbook of medical treatment advised the use of penicillin—the “miracle drug”—alongside sulphonamides, as the most important life-saving interventions in acute bronchitis. The wider therapeutic optimism regarding penicillin was reflected in the statement that it was “one of the most satisfying drugs in medicine … readily procurable at reasonable price on a doctor's or dentist's prescription. … there is no longer justification for withholding it in susceptible infections”.42 The first edition of Stanley Davidson's The principles and practice of medicine in 1952 devoted four pages to acute tracheo-bronchitis, with a sulphonamide (sulphadimidine) or injectable penicillin being recommended in the presence of fever, particularly in the elderly or those with other diseases.43 Similar advice had been given in the 1954 edition of Maurice Davidson's A practical manual of diseases of the chest. This provided detailed advice on symptomatic remedies, bed rest, fluid intake and diet—two hourly feeds of a mixture of milk, Bovril, raw egg, sugar and brandy; however, there was only one mention of antibiotics, “in some cases administration of the newer chemotherapeutic agents may be called for” in severe infection, when early venesection and oxygen therapy were also seen as being valuable.44
The Penicillin Act of 1947 had restricted penicillin supply to doctor prescription only but the variety of preparations on offer may have encouraged use by GPs, and the publicity surrounding penicillin raised patient expectations. The preferred mode of administration was by intramuscular injection, and, as penicillin was rapidly excreted from the body, these needed to be repeated several times each day. There were two oral forms available, but at this time these were poorly absorbed and could not be relied upon in serious conditions. Penicillin was also available as a powder or a solution for inhalation for treating chest infections (“Nebula penicillini”). The use of inhaled penicillin had become popular in general practice in the late 1940s, particularly in the USA, for treating sinusitis, bronchitis and pneumonia. In 1948 the Reader's Digest published an article which recommended penicillin mist as “the treatment by far the simplest, safest and most effective yet devised for sinus infections”.45 Dr A Christie recommended inhaled penicillin as the treatment of choice for acute bronchitis in a refresher course for GPs.46 However, providing a means of inhalation (by nebulizer, atomizer or pressured oxygen) was inconvenient for patient and doctor, and the problem of sore throat also saw its popularity wane. Local treatment was available using penicillin lozenges, toothpaste or chewing gum (with the trade name “Chulin”) for sore throats, different forms of penicillin ointment and cream for the skin, and drops for ear, nose and eye inflammation. Miscellaneous products included penicillin tulle, dusting powder, suppositories, pessaries and even penicillin earplugs, using cocoa butter as the base.
While acute bronchitis was typically regarded as a minor ailment—a “shower”—it was often seen as a precursor of pneumonia—a “storm”. The serious nature of pneumonia meant that many patients were hospitalized, hence, much of the expertise on the use of penicillins in such cases was held by hospital physicians. The 1951 Textbook of medicine emphasized the difficulties of making a diagnosis and noted most physicians were in favour of giving either penicillin or sulphonamides for at least forty-eight hours for chest infections, in case they were dealing with an undiagnosed pneumococcal or streptococcal infection, switching to chloramphenicol or a tetracycline if there was no improvement.47 This illustrates another feature of practice during the 1950s that the doctors would try first one and then a second antibiotic if recovery was not swift. This move to sequential prescribing was self-perpetuating for a condition, the symptoms and natural history of which were mostly uninfluenced by antibiotics. This may have been triggered by the description of the primary atypical pneumonia syndrome. This was an increasingly recognized entity by the early 1950s, being described in Davidson's The principles and practice of medicine in 1952 as presenting, not with the features of classic bacterial lobar pneumonia, but more like acute bronchitis with prominent cough and sparse signs on lung examination, and not responding to penicillin.48 This concern with primary atypical pneumonia as a common cause of chest infections highlights once again the anxieties about pneumonia and wider concerns about the dangers of lung diseases, although Professor Charles Stuart-Harris when speaking about pneumonia to the Nottingham Medico-Chirurgical Society on 13 February 1952 estimated that only a small number of cases were actually due to atypical infections.49 Similarly, John Fry reported having seen only fifty cases over a four-year period in general practice in spite of his keen interest in chest infections.50
The 1952 version of the National Formulary provided distinct encouragement to penicillin prescribing, commenting that “Penicillin is now freely available and relatively cheap … It is remarkably free from toxic side-effects although allergic reactions are not uncommon”.51 The cost had certainly dropped. In 1943 the price of a million units of penicillin was $200, by the time of the invasion of Europe in 1944 it was $35, and by 1950 it had dropped to 50 cents.52 Only two years later, the 1955 third edition of the National Formulary was much more cautious about antibiotic use and discussed its pros and cons with particular reference to the emerging problems of resistance, cost and side-effects.53 After an initial honeymoon period, side-effects were seen to be more of a problem with the newer antibiotics. Intestinal upsets and fungal and bacterial overgrowths were being reported with tetracyclines, with the effect on children's teeth being noted later. Chloramphenicol, initially seen as such a valuable drug, was now recommended only for serious conditions because of potentially fatal aplastic anaemia. The marked safety of penicillin had given doctors and the public a false sense of security about antibiotics in general, and there was some suggestion that knowledge about the side effects of new antibiotics took time to spread into general practice. In a review of chloramphenicol for the Practitioner in 1956, Professor Clifford Wilson from the London Hospital noted that, even though the enquiry the previous year had documented numerous deaths from aplastic anaemia, up to 6000 kilograms of the antibiotic were still being used in general practice.54 Erythromycin resistance were developing so rapidly that it was recommended only for penicillin-resistant staphylococcal infections. Injected penicillin, available in five formulations, was regarded as cheap and safe, and remained the preferred antibiotic for chest infections; whereas oral penicillin G was said to be poorly absorbed and was five to ten times more expensive.55
The reliance on administering penicillin by injection was significant. It meant that such treatments were easier to deliver with hospital patients and much more difficult in general practice because of the commitments required by doctor and patient. In 1955, John Fry linked the abuse of antibiotics to the growing availability of oral penicillins and advised that intramuscular injection was still the safest and most useful mode of administration in general practice, ensuring that it would be restricted to appropriate cases, “for in my opinion any case which needs penicillin also requires daily medical supervision”.56 Inconvenient it certainly was. Injections between two and five times a day were needed and strict guidelines were in place for sterilizing syringe and needle, and storing penicillin solution in a refrigerator.57 The injection was painful. One patient wrote to the Family Doctor recalling the pain of six hourly penicillin injections and commented, “the thought of future injections terrifies me”.58 Manufacturers of oral antibiotics exploited the inconvenience to the GP of prescribing a course of penicillin injections. An advert for penicillin G tablets in the British Medical Journal in 1953 contained the headline, “Freedom for a day!” and continued: “‘Come again tomorrow for another penicillin injection’ … tomorrow … tomorrow … how relentlessly those ‘tomorrows’ confine the doctor to a restricted programme … given a supply of tablets … the patient can easily carry out the treatment himself.”59 Other doctors saw oral penicillin as little more than a placebo.60 When speaking at a conference held at the Royal Society of Medicine in November 1954, Dr Lindsay Batten reported the use of oral penicillin as doubtful practice and an abuse, because of irregular absorption. She recommended, “the ‘penicillin umbrella’ should be reserved for real impending storms and not unfurled and hoisted at every threatened shower”.61
In the third edition of Davidson's Principles and practice in 1956, the new oral antibiotic tetracyclines, chloramphenicol or streptomycin were advised if clinical improvement had not occurred after forty-eight hours of starting penicillin injections.62 Sulphonamides were no longer mentioned. Penicillin was still mainly used for complications in severe cases, especially when fever was present and the aim was to “prevent” the extension of the infection.63 Older methods of treatment persisted in some contexts, for example, in 1958, Dr Kenneth Robson, a specialist from the Brompton Hospital, in a review on acute bronchitis in the Practitioner in 1958 recommended a “good old-fashioned steam tent … The tent should be a comprehensive affair going right to the foot of the bed, with a canopy like a fourposter”.64 He also commented that, “the sooner they [sufferers] give up work and accept the fact that getting well is going to be their whole-time occupation for a week or so, the better”.65
Antibiotics for All Patients
The 1954 fourth edition of A practical manual of diseases of the chest similarly cautioned, “It is … a wise policy not to regard any case [of acute bronchitis], even the mildest, too lightly, as the condition is potentially serious and may be followed by a more extensive involvement of the respiratory passages with severe constitutional disturbance.”66 At this time the aetiology of acute bronchitis and pneumonia were seen as quite similar, both developing as a result of secondary opportunistic bacterial infection of inflamed bronchial and lung tissues, hence treatment with antibiotics developed around the idea of nipping such infections in the bud. Such a preventative strategy became popular in general practice because accurate diagnosis, and differentiating bronchitis from early bronchopneumonia, was difficult. This probably resulted in the labelling of any cough or acute respiratory symptoms as acute bronchitis, with resultant over-diagnosis, particularly at times of heavy workload during the winter “chesty cough” season, when GPs were quick to diagnose bronchitis and offer an antibiotic prescription. An expert study group accepted the difficulty of differentiating uncomplicated influenza from influenzal pneumonia in the home during the 1957/58 influenza epidemic and recommended that patients over fifty and those with pre-existing cardiac or respiratory disease should all be given a broad spectrum antibiotic such as chlortetracycline.67 Dr Alastair Mackinnon, a GP from Leeds, when recommending early penicillin commented, “Today the general practitioner does not wait for the development of the classical signs of pneumonia, or seek in his treatment to discriminate between acute bronchitis and broncho-pneumonia … his aim must be, in Montgomery's language, to hit the invading germs for six with his most potent weapons.”68 Such a policy was recommended despite the evidence that only 7 per cent of patients with acute chest infections were admitted to hospital (which in turn meant that hospital doctors saw only a few severe cases) and that 88 per cent of illnesses ran an uncomplicated course.69
Two main changes occurred with the Formulary in 1957. It was re-named the British National Formulary and published in an alternative edition, produced by the Joint Formulary Committee of the BMA and the Pharmaceutical Society of Great Britain. Drugs were now grouped according to their purpose, to aid the GP in prescribing for individual conditions, rather than just listed alphabetically to aid dispensing. Preparations for the relief of cough featured prominently with fifteen mixtures and linctuses to suppress cough, four preparations for inhalation (mainly benzoin, menthol and eucalyptus mixtures) to aid expectoration, and seventeen to relieve any spasm.70 In the section on antibiotic therapy, official concerns about the indiscriminate use of antibiotics were aired and it was advised that, “In general it may be said that if the patient is ill enough to receive an antibiotic he is ill enough to be in bed. Penicillin is still the antibiotic with the fewest side-effects and should usually be the first choice.” It was also noted that “it is usually preferable to give penicillin by injection [for adults].”71 Follow-up treatment with tetracycline was recommended if patients with acute bronchitis (or pneumonia) did not respond to penicillin. This firm advice to treat only patients ill enough to be in bed was somewhat countered by the section on the respiratory system drugs which stated, “It should be remembered that many coughs have a background of infection, and chemotherapy with … antibiotics may be desirable.”72 This mixed message persisted in the 1960 edition which also indicated that oral therapy was becoming more acceptable and certainly easier; no less than twelve different proprietary preparations of oral penicillin were now available, mostly variants of phenoxymethylpenicillin.
The 1964 edition of the Textbook of medical treatment made a clear link between acute bronchitis and bacterial infection, stating “acute bronchitis is an acute inflammation of the mucous membrane of the trachea and bronchi caused by bacterial infection”, and now recommended the newly available range of oral antibiotics, even in the absence of fever.73 This contrasted with the second edition twenty years previously where acute bronchitis was described only as an inflammation of the mucous membranes of the bronchi, with predisposing causes including coryza and influenza.74 By the mid-1960s, the antibiotic options available to doctors had changed out of all recognition, with a choice of fifteen oral penicillin preparations including names such as econocil, stabillin, and tonsillin. Similarly, the 1966 edition of L S P Davidson's book described acute bronchitis as being caused by pyogenic bacteria, and antibiotics were firmly ensconced as appropriate treatment whatever the symptoms, with the expectation that the condition was “usually mild and of short duration, the patient recovering in two to three days if a suitable antibiotic is given”.75
GPs were mainly interested in whether to prescribe antibiotics or not, while hospital specialists were concerned with which antibiotic to use. This situation reflected the differences of both the clinical context and the doctor–patient relationship in general practice and in the hospital. In 1955 Anthony Batty Shaw and John Fry, both well known GPs with a special interest in the subject, summarized the GPs’ dilemma of whether or not to prescribe antibiotics:
The core of the problem of treatment of acute infective chest disease in general practice is deciding when antibacterial therapy should be given … it is not necessary or desirable to treat minor catarrhal infections which will recover without antibacterial agents, but a practitioner does not wish to prejudice his patient's recovery by failing to institute such treatment when necessary. It is therefore natural that the practitioner will err on the side of over-prescribing rather than under-prescribing …76
Robson, a hospital chest specialist, in his 1958 review of acute bronchitis advocated early antibiotics:
Some authorities state categorically that antibiotic treatment is not called for in this type of disorder. On the other hand bacterial invasion, if not a primary feature, is highly likely to come in as a secondary one and there is everything to be said for building up a blood level prophylactically. On the whole this consideration outweighs others and if the disturbance is a really acute and widespread one with fever, it is wise to get started with antibiotic treatment on the first or second day. One of the so-called “wide spectrum” preparations should be chosen … tetracycline and oxytetracycline are good first choices.77
This increased pressure to use antibiotics, even the newer ones, was also expressed in a discussion between the GPs John Horder and John Fry, and Neville Oswald, a hospital chest specialist, about the acute chest in 1963. Horder was asked about his policy with antibiotics for the acute chest, and responded:
I tend increasingly to give antibiotics … we … know that [patients] get better quicker if they have an antibiotic. One feels that giving an antibiotic may influence the likelihood of another attack … it is this that compels me to give antibiotics more and more regularly and earlier and earlier … I almost always use tetracycline … not penicillin.78
Evident here is the prophylactic as well as therapeutic use of antibiotics. Yet by 1971, the British National Formulary had firmly turned away from a widespread recommendation for antibiotic use. GPs were advised:
The enormous success of antibiotics has lead to such extensive use that … their value is … being lessened … doctors should not be obliged to give an antibiotic just because there are signs of infection. Many common illnesses are due to viruses for which antibiotics are useless—even if bacterial it may well be trivial and self-limiting.79
Such usage in the 1960s seems surprising given the long-running concern about the link between “over prescription” and the side effects, resistance and cost of antibiotics. Ironically, one important factor in the increased use of antibiotics was the perceived safety and doctors’ dependence on them for minor ills. This feeling was well summed up in the commentary which accompanied a symposium on antibiotics published in the Practitioner in 1956:
The exceptional safety of penicillin put us off our guard. The impression was created that antibiotic therapy could be applied with impunity. Time has shown that this is not so. Not a single antibiotic introduced subsequent to penicillin has rivalled it in non-toxicity. … If the community is to obtain the full benefit of the tremendous advantages bestowed upon humanity by the discovery and development of antibiotics, it is essential that these preparations should be used correctly and with circumspection.80
The problem of penicillin resistance had been apparent by the late 1940s and data from the USA illustrated the alarming rise in resistance to newer antibiotics, particularly amongst staphylococci.81 Over a two-year period from 1951, penicillin resistance for staphylococci was around 60 per cent, whilst streptomycin resistance rose from 48 per cent to 65 per cent, chlortetracycline resistance from 23 per cent to 63 per cent, and erythromycin resistance from zero to nearly 20 per cent in one year.82 This was brought to the public's attention by, for example, The Times’ headlines, “Doctors’ warnings on antibiotics. Organisms becoming resistant”, when reporting the condemnation of the indiscriminate use of antibiotics by the BMA in 1956.83
Debates amongst doctors in the 1940s related primarily to the value of the traditional management methods, and then in the 1950s switched to decisions about when to start antibiotics and which one to chose. The advice in textbooks and formularies shows a clear shift towards bacterial infection being seen as the treatable cause of acute bronchitis, with antibiotics as the treatment of choice. There was a move away from recommendations of regimens of bed rest, diet and fluids, symptomatic therapies and slow convalescence, first to the use of antibiotics in more serious cases to treat complications, and then to their early use to lessen the symptoms and prevent complications. Thus, acute bronchitis changed from a potentially dangerous condition with a slow recovery, to one where doctors and patients expected a safe and prompt recovery, brought on by antibiotics. The change in treatment protocols was likely to have been popular with the patient, his or her family and the doctor, as it would have been perceived to reduce the duration, labour and cost of the traditional regimens.84 The increasing use of oral antibiotics in the mid- and late 1950s, instead of the injections and inhalation that were the main forms of administration for the first decade of penicillin treatment for chest diseases, added further to the attraction of the antibiotic “quick fix”. It was not until the late 1950s that advances in laboratory techniques for identifying viruses showed that they were important causes of acute respiratory illness.85 The idea that viruses were implicated in many cases of colds and acute chesty coughs heralded a progressive shift of opinion in the 1960s that most acute respiratory illnesses were viral and not bacterial in origin and, as such, would not respond to antibiotics, which were largely unnecessary. Indeed, in the 1970s the thirteenth edition of the American Cecil–Loeb textbook of medicine acute bronchitis was no longer listed in the index as a distinct entity, instead it appeared as one syndrome of respiratory illness caused by a variety of viruses.86 A slower change of emphasis in aetiological thinking was also evident in British textbooks. In the twelfth edition of the Textbook of medical treatment in 1971, acute bronchitis was described as acute inflammation “caused by virus or bacterial infections”.87 However, by then, the habit of using antibiotics for acute bronchitis and acute respiratory symptoms had been acquired by both patients and GPs, and was not easily broken.
Issues in the Management of Acute Bronchitis
The shift towards prescribing antibiotics for all patients with acute bronchitis was not wholly shaped by clinical experience and research findings, it was affected by, and itself affected, wider trends in medicine in the post-war decades. Our research found that three factors were particularly important: the NHS, the pharmaceutical industry, and the emergence of the consumer-patient. In making these points, we show how the policies, organizational structures and dynamics between the NHS and the pharmaceutical industry identified at the national level by historians, affected specific local practices with a single disease.88
The NHS: Structures and Policies
Costs and work pressures were key factors influencing the use of antibiotics in general practice. The unexpected demand for services that followed the birth of the NHS resulted in an increased burden of work and a huge overspend on the estimated GP costs. When noting a 13 per cent rise in workload over the first two years of the Service, the Chief Medical Officer commented:
Reports received from all quarters [confirm] that the general public has not been backward in taking advantage of free consultation and free medicine. … Assuming that some of this increase is due to the opportunities presented to those whose faith in the virtue of the bottle of medicine or box of tablets is unbounded, there still remains the question whether it is in the general interest that more people should be taking their trivial ailments to the doctor with perhaps the risk of developing a disease-conscious frame of mind.89
The biggest increase in consultations was among women under the age of sixty-five, the very group which subsequent studies showed consulted more frequently for acute respiratory illness.90 This led GPs to develop strategies to cope with their new and excessive workload, whilst at the same time they were under pressure from the Ministry of Health to restrict expenditure on prescriptions. The drug bill was one of the greatest expanding costs of the new NHS, much of this from primary care prescribing. In June 1948, the last month of the National Health Insurance (NHI) scheme saw 6.8 million prescriptions being dispensed by chemists. By September 1948, this had doubled to 13.6 million.91 Patients expected to receive medicine. In 1956–57, J P Martin investigated why up to three-quarters of medical contacts resulted in a prescription; he found that there was an expectation on both sides, and from both NHI “panel” and private patients, “that the prescription frequency was … part of a response to ill-health … of doctor and patient when illness occurred”.92 However, the new factor was that now neither the patient nor the GP paid for the medicines, hence the removal of the financial barrier was of particular significance for the uptake of expensive antibiotic drugs. Antibiotics contributed substantially to the NHS costs, and by 1956 accounted for 22.7 per cent of the total prescription cost in England and Wales and a quarter of the total of all prescriptions by 1961.93 They were marketed almost exclusively in the more expensive proprietary form.94 The percentage of proprietary medicines prescribed was only 7 per cent of total prescriptions in 1947 under the NHI, 18 per cent in 1950, 40 per cent in 1956 and 48 per cent in 1957. In 1958, the Hinchcliffe Committee singled out proprietary antibiotics (and steroids) as being the major financial factor in the increasing drug costs for the NHS.95
GPs were put under increasing pressure by the Ministry of Health to restrict the prescription of expensive items, and exhortations were soon backed up by the threat of sanctions, though none of these proved particularly effective.96 In 1951 the Prescribing Investigations Unit was established to monitor prescribing. This led to about 900 GPs being visited each year by their Regional Medical Officer to enquire about their drug costs, and some GPs were fined up to £100 by their Local Medical Committee for excess prescribing.97 Another response to the rising drugs bill was to introduce prescription charges, which led to Bevan's resignation in 1951 and the removal of the post of Minister of Health from the Cabinet. However, we suggest it was not the introduction of the one shilling charge per script in 1952 that was critical in reshaping prescribing practice, but the intended cost-saving decision in 1956 to charge a shilling per item.98 Ironically, this seems to have encouraged the use of (expensive) antibiotics in the treatment of acute bronchitis. GPs had previously added antibiotics to the cheap symptomatic remedies on a multi-item script, now they chose what they saw as the single most effective medication (and also the most expensive). Given the medical and public concerns about pneumonia and the wish to avoid prolonged illness, it was predictable that an antibiotic became the treatment of choice. The move towards antibiotics and away from symptomatic prescriptions happened earlier in the USA. In 1952–1953, nearly 20 per cent of all prescriptions from the USA were for antibiotics compared with 8 per cent in England and Wales. The reverse was true for cough preparations, which amounted to only 5 per cent of prescriptions in the USA but over 17 per cent in England and Wales at that time.99 By 1959, only six years later, the number of prescriptions in England and Wales for antibiotics now matched almost exactly those for cough preparations, although the total cost of the cough mixtures was only 4.5 per cent of the total prescription budget compared with 28 per cent for antibiotics.100
List sizes and consultation rates increased after 1948 and work pressure on GPs was considerable.101 In 1953, Stephen Taylor found consultation rates of up to ten per listed person per year, particularly in industrial and urban areas, where list sizes and morbidity were also higher. Surgery consultations numbered between fifteen to fifty and home visits twelve to thirty per day with the average consultation time being less than five to six minutes.102 Thus, patient pressure was considerable and consultation time was short, particularly in the winter when bronchitis, coughs, colds and influenza were so common. It is unsurprising that antibiotics, which offered a quick fix, emerged as the preferred choice for a self-limiting condition such as acute bronchitis, when put against the time taken for the doctor to explain the traditional management and natural history of bronchitis with the somewhat complex regime of symptomatic care and convalescence. The capitation scheme introduced with the NHS, where the GP was paid by the size of his list (to a maximum of 5000 patients), put some financial pressure on the GP to keep list sizes high. This may also have contributed further to antibiotic prescribing for two reasons. Firstly, giving the new “miracle drugs” could have been a strategy to keep the patient happy and on the GP's list; secondly, large lists, which were common in urban practices, were associated with increased consultation rates per patient, less time per consultation and increased prescribing.103 Dr Lennox Johnston from Wallasey brought out the first issue in the Lancet in 1950, stating, “The most important factor in the debasement of general practice is … competition between general practitioners for goodwill. The patient can and often (I might almost say usually) does bring economic pressure to bear on his general practitioner, in order to secure the type of medical treatment he wants.”104 As Taylor put it in his book Good general practice, which surveyed life in general practice in 1954, “The doctor with the over-crowded surgery, who is always so rushed he never has time to examine properly any of his patients, is continually doling out placebos for improperly diagnosed conditions.”105 Dr Strong, a GP from Kent, put it another way in a letter to the Lancet in 1950, “At one end of the scale are the men with small practices, suffering financial hardship but trying to practice good medicine … at the other end are the four-thousand odd being given the best service that can be expected from overworked and harassed doctors. Quality brings bankruptcy: quantity has some financial reward.”106
In 1958, the Council of the College of General Practitioners, in submitting their report to the Hinchcliffe Committee on the cost of prescribing, forcefully made the point that undergraduate and newly qualified doctors did not receive adequate experience of the common, self-limiting conditions which made up the greater part of a family doctor's work.107 Unlike the situation nowadays, nationally agreed, clinical management guidelines for common conditions aimed specifically at general practitioners were not available. Acute bronchitis would have been a good example of such a common condition, one that hospital trained doctors had never seen during their training, but would treat, relying on a simple approach of “infection equals antibiotics”. Antibiotics were certainly commonly used by hospital doctors—in some hospitals up to 40 per cent of the drug budget was spent on them in 1954.108 However, in view of the vastly greater number of prescriptions used in general practice, the direct financial and ecological impact was much less then, and it is only relatively recently that hospital acquired “superbugs” have caused concern. In 1957, John Fry noted that £10 million a year were spent by GPs on antibiotics compared with only £2 million spent by hospitals.109
The Pharmaceutical Industry
Over the 1950s, the standard, proprietary products of the pharmaceutical industry displaced the individually made-up prescriptions by the dispensing chemist as the mainstay of medical treatments. Indeed, the rise in the cost of the proprietary medicines was the main cause of the spiralling NHS drug bill, especially for new antibiotics.110 For instance, the cost of a single day's treatment of chloramphenicol in 1951 was 22s 6d, about seven times the average cost of a prescription.111 In the House of Commons debate on the proposed prescription charge on 27 March 1952, Aneurin Bevan stated that the main reason for the rise in drug expenditure was the use of new and expensive antibiotics by the “ill-disciplined” medical profession. A Labour colleague Dr Edith Summerskill blamed “high powered salesmen, on behalf of the drug manufacturers … persuading doctors to prescribe expensive proprietary drugs for their more well-to-do patients … the most flagrant abuse … by the better-off section of the community at the expense of the worse-off”.112 GPs were certainly targeted by the drug companies. On average, each GP saw two to three representatives each week and received seven mailings of drug promotional literature every day, occupying over half of his total daily post delivery.113 Medical organizations had not escaped criticism either. When Dr Charles Brooke from Mottingham wrote to Aneurin Bevan on 10 November 1949 regarding “this Bevan bob business”, he blamed the BMA and the Medical Protection Union as “aiders and abetters in the racket [of drug sales in the UK]” due to the enormous revenues that they were getting through advertisements in their journals, noting that the latter would be ruined if it refused such advertisements.114
The changes in the number and type of advertisements carried by the British Medical Journal show the increase in the “information” targeted at doctors. In the four issues in January 1949, there were eight antibiotic advertisements, one being a full page, of which five were for penicillin, including three for penicillin chewing-gum. Over the four issues in December 1953 there were twenty-three antibiotic ads: fifteen of them whole pages and nine for non-penicillin preparations, mostly tetracyclines. For the same period in 1962 there were thirty-three whole page advertisements for antibiotics, with less than half for penicillin.
The annual reports of the Association of the British Pharmaceutical Industry (ABPI) show the industry's unhappiness about the criticism it received for excess expenditure on advertising and promotion. The first published figures from 1961 revealed that the industry spent just over 12 per cent of the revenue from home sales of prescription medicines on advertising and promotion. In 1963 this amounted to £8.9 million, with £4 million being spent on drug representatives, £1.3 million on advertising in medical journals, £2.0 million on mail shots, £0.9 million on other marketing activities and £0.8 million on free samples.115 The industry justified this large expenditure and answered the criticisms about its activities by presenting the pharmaceutical companies as an important source of medical information for the medical and pharmaceutical professions to ensure “the physician is given detailed scientific information on their proper use”.116 It recognized that the GP had great difficulty in keeping up to date with these advances, often being dependent on drug company representatives or promotional literature in the absence of any formal professionally organized postgraduate education.117
The doctors’ freedom to prescribe on the NHS whatever they considered best inevitably encouraged extravagant sales propaganda and pressure, much of it being seen as “undesirable”, particularly when the down side of the products was not mentioned. When Dr Batten reported to a meeting at the Royal Society of Medicine in 1955 that toxicity was being increasingly reported in the medical press for the newer antibiotics, she added, “though you would never think so from the advertisements”.118 Certain pharmaceutical company literature was not all promotional; for example, information sheets produced for the medical and pharmaceutical professions about penicillin, and about “coughs and colds” by Boots Pure Drug Company in 1950, gave no hint that antibiotics should be used for non-severe respiratory illnesses such as acute bronchitis.119 Companies also claimed that they needed good sales and profits to invest in research and development for tomorrow's drugs. However, subsequent annual reports show a change of emphasis and by 1966–67 the ABPI was seeking professional accreditation and legitimization for representatives.120
Patients or Consumers
That patients expected a prescription when visiting their doctor came partly from custom, partly from their pre-1948 role as purchasers of health care as insurance subscribers or private patients, and partly from the behaviour of the medical profession. The Council of the College of General Practitioners in its evidence to the Hinchcliffe Committee admitted that,
In many cases the patient's expectation that a medicine will be prescribed must be met … his sympathy and understanding must often be reinforced by the exhibition of a tangible token. Many patients would be generally disturbed by their doctor's failure to prescribe … even an intelligent patient, who in health will readily agree that drugs were inadvisable, when he falls sick will often feel much happier if his doctor gives him something.121
It is probable that from the late 1940s to the mid-1950s, many doctors prescribed the least effective oral penicillins and other oral antibiotics as these were less demanding of their time, and that they reserved injected penicillins for more serious illnesses that also demanded monitoring.
Public information on antibiotics was available from many other sources including health encyclopaedias and dictionaries, medical and government publications, articles in the popular press and magazines, and radio and television programmes. There was even a horse called “Aureomycin” which ran in the Hambleton Plate at Thirsk Racecourse on 14 April 1950.122 Encyclopaedias on family health would certainly have raised public expectations. For example, the 1956 Good Housekeeping's encyclopaedia of family health stated that, “antibiotics have given man almost complete mastery over disease caused by micro-organisms”; also commenting, “pure penicillin is so powerful that one grain in one thousand gallons of water is fatal to some bacteria, whereas a man could take half an ounce without the least harm”.123 However, neither this nor other popular family health books of the time specifically recommended antibiotics for treating acute bronchitis. Instead, they merely described the condition as one of potentially protracted duration, typically stating, “the course of the illness is variable from seven to fourteen days—though cough, expectoration and debility may last for several weeks”; and in The book of health, “It is possible for [the] symptoms to become much more severe and to last for three or four weeks or longer. It often follows the common cold.”124 This would have been depressing reading for those persons afflicted with the early symptoms, particularly when the advice was to seek bed rest, light diet, steam inhalations, the “bronchitis kettle”, aspirin and proprietary cough mixtures. Might such advice have encouraged patients to consult their GP to get one of the new wonder antibiotics in the hope of alleviating or shortening their distress?
The message in the information in publications produced by, or speaking for, the medical profession was, as one might expect, more measured. The 1955 edition of Black's medical dictionary, which was aimed at a medically-informed audience, advised penicillin or sulphonamides for troublesome bronchitis symptoms, while still recommending a steam kettle and bed rest in a warm room for mild acute bronchitis, accompanied with an illustration of the bronchitis tent.125 Another medically sanctioned publication, the Family Doctor, launched in April 1951 by the BMA to provide the public “in straight forward English the advice and guidance of doctors who know what they are talking about”, included items on “Is your medicine really necessary?” and “Are you a human medicine bottle?”, which appeared in the early editions. In the first of these articles, Dr W Edwards told the public, “Next time you have to consult your doctor, pay much more attention to the advice he gives you, and much less to the prescription form. Pin your faith on his experience … not on the coloured mixture.”126 Dr C Brogan, when seeking an explanation for “the frantic medicine tippling that has infected the National Health Service with financial dropsy”, argued that the public had come to value the “bottle” as a sign of interest from the doctor. Failure to prescribe was interpreted wrongly as an “unkindly hint that the patient was not really ill”.127
Articles on bronchitis that appeared in the 1952 and 1953 volumes of Family Doctor stressed that bed rest and not antibiotics was important.128 One article took the form of a dialogue between a patient with acute bronchitis and his GP, and gave an interesting insight into the consultation dynamics at that time. When asked whether he had been coughing much, the patient comments, “Yes … The wife was getting fed up on account of it—said I would have to come to see you.” The doctor recommends a few days in bed. The patient becomes concerned because of the effect on his job and asks, “You couldn't give me something to clear it up right away, doctor. I mean like one of those new drugs.” The GP retorted, “Most of these wonder drugs, as they call them, don't work at all on the sort of bronchitis you've got. You'll just have to nurse it and look after it. You take my advice and you'll be all right in a fortnight or three weeks… . if you go on … struggling to work, you'll end up with a really bad chest.”129
There is evidence of pressure from patients to prescribe antibiotics. Writing to the College of General Practitioners in 1956, Dr Byrne, a GP from Milnthorpe, placed the blame for increased prescribing on the direct advertising of drugs to the public, along with health education articles in the press and programmes on radio and television.130 Dr Ashworth from Manchester, by contrast, wrote, “I do not accept much pressure from patients … Doctors must be prepared to lose a few patients in order to preserve their proper ethical standards”.131 Such comments from individual doctors need to be treated with caution as the interaction between patient and doctor in this regard is known to be complex. 132 The Reader's Digest featured high on critics’ list of offending journals in this respect, possibly unfairly as, alongside articles praising the safety and efficacy of penicillin, there was, in July 1953, an article entitled “Are you overdosing with antibiotics?” This stated that, “Antibiotics are no cure-alls … too many of us summon these drugs against a mild self limiting disease …We use them to try and cure a feverish cold”. The author went on to warn about the development of resistance “you are hastening the day when the wonder drugs will have lost their punch”, and concluded, “your Doctor [is] more wary of their [antibiotic] indiscriminate use. Free of your prodding, he will be more selective and more accurate in his treatment”.133
A 1961 Foyle's Health Handbook on Coughs, colds and bronchitis by Dr Kenneth Hutchin described acute bronchitis as “an acute infection of the bronchial tubes”, often when a cold “has gone down on to the chest”. He added that, “When it does follow on from a cold it is most likely that the cause … is some germ which has been superimposed on the original cold infection, because bronchitis is usually due to a bacteria rather than a virus”. The author recommended “old-fashioned measures” of bed rest, nursing, and symptomatics (Friar's Balsam) comfort, which he said aided the effects of antibiotics. He justified the use of antibiotics (especially the oral administration of teramycin and achromycin) on the grounds that they reduced the number of cases that might eventually need hospital care and hence were the most cost-effective treatment. 134
Conclusion
In this article we have argued that there was a revolution in the treatment of acute bronchitis over the 1950s, as antibiotics rapidly replaced symptomatics as the primary form of treatment. We have shown that this change certainly did not occur because of the efficacy of the new drugs, as there was little evidence then or now that antibiotics significantly alter the course or duration of acute bronchitis for the majority of patients.135 Instead, we have shown that changes in the treatment of the disease were due to interrelated epidemiological, clinical, educational, social, political, economic and industrial pressures. The evidence presented here suggests that antibiotics were first adopted to treat or prevent secondary complications, such as pneumonia, rather than for the primary disease. Epidemiologically, acute bronchitis was amongst the most prevalent illnesses in the 1950s and one of the most common reasons for seeing the doctor, which gave it a high profile in debates about the problems and future of general practice. Clinically, there was a dialectical relationship between the changing understanding of the aetiology and pathology of acute bronchitis and available treatments, especially as the properties of antibiotics encouraged doctors to shift from a symptomatic to an aetiological definition of the condition. Indeed, it seems that the adoption of antibiotic therapy encouraged doctors to see bacteria as the primary cause of acute bronchitis, even though there were few studies of the role of specific bacteria and growing evidence pointing to a greater role for viruses. The structures of the new NHS and the fact that health care was free at the point of delivery meant that GPs saw more patients and hence more acute bronchitis than ever before. Increased work loads and unsocial long hours, along with poor pay and conditions led to low morale amongst GPs, who, while struggling to keep their heads above water were faced with wave after wave of innovations, with little opportunity to keep up to date with the rapidly changing therapeutic advances, except via pharmaceutical company promotions. In such circumstances, it seems that GPs were more susceptible to seek quick fix antibiotic remedies, both to treat patients presenting with infections and to prevent their return with persistent disease. Such practices would have also met patient demands, both for the traditional token of a prescription—the “bottle”—and for the most advanced and effective medicine of the day, and encouraged them to stay on the GP's list. Also, the political pressures to reduce costs led to a per script charging regime which paradoxically probably served to raise costs by leading doctors to prescribe what they and their patients saw as the single most effective drug.
What does the changing management of acute bronchitis tell us about the alleged “antibiotic revolution”? To begin with it is clear that antibiotics came to dominate the treatment of the disease, however, this change occurred in an evolutionary manner over a decade or so. Moreover, there were two stages to this takeover, with antibiotics used first to prevent and treat serious, secondary chest infections, before dominating as a treatment of primary disease. We have also demonstrated the often overlooked point that antibiotics were not a single stable commodity, their properties changed constantly as new entities and new modes of administration were introduced. Among the most important was the availability of oral administration which allowed a change in the doctor–patient relationship through the self-administration of antibiotics, and it was perhaps no accident that this coincided with the shift to “antibiotics for all disease”. Increasing choice of type also saw the practice of trying a second antibiotic if recovery was not fast enough with the first, cementing further the dependence on such treatment. We have also shown that changes in the use of antibiotics were closely linked to changes in NHS policies on prescription pricing. The most radical changes overall were perhaps the most general; namely, the way that the use of antibiotics led doctors to think aetiologically about acute bronchitis and progressively redefine it largely as a bacterial infection, amenable to single-fix, antibiotic treatments. This attitude persisted through habit by both doctors and patients, even after research identified viruses as the most common aetiological agents in the 1970s, and expert opinion and clinical guidance advised against the routine use of antibiotics for acute bronchitis.
The habit of prescribing antibiotics for acute bronchitis persists today. Patients still visit their GP in large numbers for common symptoms such as cough (with nearly two million consultations for acute bronchitis annually in England and Wales) and GPs cope by using a strategy of prescribing antibiotics for the majority of cases. In 1994, the Audit Commission judged antibiotic prescriptions in the community for respiratory tract infection to be the most important factor contributing to the increasing problems of antibiotic resistance, side effects and cost to the community.136 Ironically, a recent successful move to reduce GP antibiotic prescribing has been putatively linked to a rise in morbidity and mortality from respiratory infections, suggesting that the circle is beginning to turn back towards pre-antibiotic days and that we need to learn lessons from the 1950s on how to decide which patients need antibiotics—the older, those with underlying disease, those with localizing signs of pneumonia in the chest, and those ill enough to be in bed.137 It is interesting to note that this approach was recommended for the use of antibiotics during an influenza pandemic in the guidelines produced by the Chief Medical Officer in 2006, further evidence of a return to fifty-year-old practices for the appropriate and targeted use of antibiotics for acute chest infections.138
Acknowledgments
We would both like to thank the Wellcome Trust for their support; John Macfarlane for the short-term training fellowship which made this study possible, and Michael Worboys for the support of his personal research and of the Manchester Unit. We are grateful for help to Claire Jackson (Archivist, Royal College of General Practitioners); Lee Sands (Archivist, British Medical Association); Sophie Clapp (Company Archivist, Boots Group, plc); Jackie Ellis (Administrator, Nottingham Medico-Chirurgical Society); together with advice from Robert Bud, Flurin Condrau, Mark Jackson, Irvine Loudon and John Pickstone. We would also like to thank the referees for their constructive comments.
Footnotes
1 See for example, K Brown, Penicillin man: Alexander Fleming and the antibiotic revolution, Stroud, Sutton, 2004. In typical fashion, this book offers a few examples of previously life-threatening diseases that could be effectively treated with penicillin, e.g. endocarditis, meningitis, sepsis, and puerperal fever, p. 193. On changing drug therapies over the century, emphasizing evolutionary change, see M Weatherall, In search of a cure: a history of pharmaceutical discovery, Oxford University Press, 1990.
2 R Bud, ‘Penicillin and the new Elizabethans’, Br. J. Hist. Sci., 1998, 31: 305–33; D Masters, Miracle drug: the inner history of penicillin, London, Eyre & Spottiswoode, 1946; H M Böttcher, Miracle drugs: a history of antibiotics, London, Heinemann, 1963.
3 College of General Practitioners (CGP), ‘Acute chest infection in general practice. A group investigation by 55 general practitioners organized by the research committee of the council of the College of General Practitioners’, Br. med. J., 1956, i: 1516–20, p. 1518.
4 Scottish Intercollegiate Guidelines Network (SIGN), ‘Community management of lower respiratory tract infection in adults’, 2002, 59: 1–29. Accessed by http://www.sign.ac.uk/guidelines; Patient-Orientated Evidence that Matters (POEM), ‘Antibiotics are not needed for lower respiratory tract infection’, Br. med. J., 20 Aug. 2005, 331: 0NN.
5 M Woodhead, D Fleming, R Wise, ‘Antibiotics, resistance and clinical outcomes’, Br. med. J., 2004, 328: 1270–71.
6 The important contribution of viruses did not emerge until the 1960s.
7 Chronic bronchitis: an NAPT symposium, London, NAPT, 1958.
8 National Archives, Public Records Office (hereafter NA PRO) MH 132/48, Report of the Minister of Health for the year ending 1958. Part 11. On the state of the public health, being the annual report of the Chief Medical Officer, London, HMSO, Nov. 1959, p. 73.
9 CGP, op. cit., note 3 above, p. 1518.
10 J Pemberton, ‘Illness in general practice’, Br. med. J., 1949, i: 306–7.
11 The Times, 16 Sept. 1955, p. 7.
12 Anon., ‘Facts from general practice’, Lancet, 1953, ii: 978–9.
13 J Horder and E Horder, ‘Illness in general practice’, Practitioner, 1954, 173: 177–87, p. 186.
14 CGP, op. cit., note 3 above, p. 1518.
15 E M Backett, J A Heady, J C G Evans, ‘Studies of a general practice (II). A doctor's job in an urban area’, Br. med. J., 1954, i: 109–15, p. 113.
16 This pattern was confirmed by the General Register Office 1952–1954 study of 37,000 consultations.
17 J Fry, Common diseases: their nature, incidence, and care, Lancaster, Medical and Technical Publishing, 1974, ch. 2 ‘Influenza’, pp. 16–26.
18 The Times, 12 Jul. 1947, p. 6; 15 Jan. 1949, p. 3.
19 The Times, 11 Feb. 1952, p. 6.
20 The Times, 16 Sept. 1955, p. 7.
21 The Times,17 Jan. 1951, p. 2. Dr John Fry, a GP from Beckingham, who was a pivotal figure in the early days of primary care research and published widely on acute bronchitis and chest infections, put it another way, “‘flu’ can become a convenient garbage-can type of loose and imprecise diagnostic term that offers a quick and ready label for the victims of a multitude of common respiratory infections”. Fry, op. cit., note 17 above, p. 22.
22 ‘All about ‘flu’, Family Doctor, 1954, 4: 84–5, p. 84.
23 The Times, 31 Jan. 1953, p. 3.
24 NA PRO MH 132/36, Report of the Minister of Health for the year ending 31 Dec 1952. Part 11. On the state of the public health, being the annual report of the Chief Medical Officer for the year 1952, London, HMSO, Dec 1953, p. 76.
25 J G R Howie, I M Richardson, G Gill, D Durno, ‘Respiratory illness and antibiotic use in general practice’, J. R. Coll. General Practitioners, 1971, 21: 657–63.
26 J S Collings, ‘General practice in England today’, Lancet, 1950, i: 555–85.
27 Anthony Ryle, letter to the Lancet, 1950, i: 885.
28 British Medical Association, General practice and the training of the general practitioner, London, British Medical Association, 1950, pp. 82–4; P A Tyser, ‘Training for general practice’, Lancet, 1950, i: 1091.
29 G Rivett, From cradle to grave: fifty years of the NHS, London, King's Fund, 1998, p. 90.
30 The Times, 24 Oct. 1962, p. 15.
31 We have been unable to track down any extant copies of Prescribers’ Notes. It was produced between 1952 and 1958 and was the forerunner of the Prescribers’ Journal, which replaced it in 1961 on the recommendation of the Hinchcliffe Committee. See, Department of Health, Final report of the Committee on Cost of Prescribing, Hinchcliffe Committee report, London, HMSO, 1959, p. 49.
32 Royal College of General Practitioners, Archives (hereafter RCGPA), ACE J8–1, The cost of prescribing. A memorandum from the Council of the College of General Practitioners, 1958, p. 3.
33 Ibid., p. 4.
34 D M Dunlop, L S P Davidson, J W McNee, Textbook of medical treatment, 3rd ed., Edinburgh, Livingstone, 1944, pp. 861–71.
35 A B Christie, ‘Refresher course for general practitioners: acute bronchitis’, Br. med. J., 1951, i: 82–5.
36 J D Comrie, H A Clegg, Black's medical dictionary, 18th ed., London, Adam and Charles Black, 1946, pp. 145–9.
37 M Worboys, ‘Treatments for pneumonia in Britain, 1910–1940’, in I Löwy (ed.), Medicine and change: historical and sociological studies of medical innovation, Montrouge, John Libbey Eurotext; and Paris, INSERM, 1993, pp. 317–26; I Loudon, ‘Puerperal fever, the streptococcus, and the sulphonamides, 1911–1945’, Br. med. J., 1987, 295: 485–9.
38 Christie, op. cit., note 35 above, p. 84. University of Nottingham Hallward Library manuscripts and special collections material (hereafter UNHL) MCH 1/10/1, Minutes of the address by Professor Sir Derrick Dunlop to the Nottingham Medico-Chirurgical Society on ‘Modern concepts in therapeutics’, on 30 Nov. 1949, pp. 116–17.
39 T Anderson, ‘The newer antibiotics in respiratory infections’, Practitioner, 1952, 169: 589–95, p. 592.
40 Ministry of Health, National War Formulary, 1st ed., London, HMSO, 1941, p. 5.
41 Ministry of Health, National [War] Formulary, 2nd ed., London, HMSO, 1947, p. 5.
42 D M Dunlop, L S P Davidson, J W McNee (eds), Textbook of medical treatment, 5th ed., Edinburgh, Livingstone, 1949, pp. 86–8, on p. 86.
43 L S P Davidson, The principles and practice of medicine: a textbook for students and doctors, 1st ed., Edinburgh, Livingstone, 1952, pp. 58–61.
44 Maurice Davidson, A practical manual of diseases of the chest, London, Geoffrey Cumberlege, Oxford University Press, 1954, p. 117.
45 Miller, ‘Penicillin mist for sinus trouble’, Readers’ Digest, April 1948: 59–61.
46 See Christie op. cit., note 35 above, pp. 82–5.
47 R L Cecil, R F Loeb, A textbook of medicine, 8th ed., Philadelphia and London, Saunders, 1951, pp. 822–4.
48 Davidson, op. cit., note 43 above, pp. 58–61.
49 UNHL, MCH 1/11, Minutes of the address by Professor Stuart-Harris to the Nottingham Medico-Chirurgical Society, ‘Pneumonia’, on 13 Feb. 1952, p.21.
50 J Fry, ‘Primary atypical pneumonia’, Br. med. J., 1951, ii: 1217.
51 Ministry of Health, National Formulary, 2nd ed., London, HMSO, 1952, p. 16.
52 T I Williams, Howard Florey: penicillin and after, Oxford University Press, 1984, pp. 148–9.
53 Ministry of Health, National Formulary, 3rd. ed., London, HMSO, 1955.
54 C Wilson, ‘Chloramphenicol’, Practitioner, 1956, 176: 14–17, on p. 17.
55 K R Capper, ‘Preparations of penicillin’, Practitioner, 1955, 174: 12–20.
56 Joint Meeting of the Section of General Practice with the Section of Medicine, ‘Discussion on the use and abuse of antibiotics’, Proc. R.. Soc. Med., 1955, 48: 355–64, on p. 363.
57 NA PRO, MH 133/193, Standing Nursing Advisory Committee meeting 24 July 1951, p. 12.
58 ‘Doctor answers, “Painful injections”’, Family Doctor, 1960, 10: 128.
59 On crystapen tablets see, Br. med. J., 4 Apr. 1953, i: 7.
60 CGP, op. cit., note 3 above, p. 1518.
61 Joint Meeting, op. cit., note 56 above, p. 360.
62 L S P Davidson, The principles and practice of medicine: a textbook for students and doctors, 3rd ed., Edinburgh, Livingstone, 1956, pp. 272–5.
63 D M Dunlop, S Davidson, S Alstead (eds), Textbook of medical treatment, 7th ed., Edinburgh, Livingstone, 1958, pp. 653–5.
64 K Robson, ‘Acute bronchitis’, Practitioner, 1958, 181: 681–5, p. 684.
65 Ibid., p. 683.
66 M Davidson, op. cit., note 44 above, p. 106.
67 Combined Study Group, ‘Some aspects of the recent epidemic of influenza in Dundee’, Br. med. J., 1958, i: 908–13, p. 912.
68 A U Mackinnon, ‘Winter ailments in general practice’, Practitioner, 1960, 185: 764–9, on p. 768.
69 CGP, op. cit., note 3 above, pp. 1516–20.
70 The British Medical Association and the Pharmaceutical Society of Great Britain), British National Formulary (alternative edition), London, British Medical Association and the Pharmaceutical Society of Great Britain, 1957, pp. 151–61.
71 Ibid., pp. 106, 103.
72 Ibid., pp. 152.
73 D M Dunlop, L S P Davidson, S Alstead (eds), Textbook of medical treatment, 9th ed., Edinburgh, Livingstone, 1964, pp. 678–80, on p. 678.
74 D M Dunlop, L S P Davidson, J W McNee (eds), Textbook of medical treatment, 2nd ed., Edinburgh, E and S Livingstone, 1942, p. 817.
75 L S P Davidson, The principles and practice of medicine: a textbook for students and doctors, 8th ed., Edinburgh, Livingstone, 1966, pp. 341–3, on p. 342.
76 A Batty Shaw and J Fry, ‘Acute infections of the chest in general practice’. Br. med. J., 1955, ii: 1577–86, p. 1584.
77 Robson op. cit., note 64 above, pp. 684–5.
78 J Horder, N Oswald and J Fry, ‘The acute chest’, Medical World, Sept. 1963: 380–7, on p. 384.
79 Ministry of Health, British National Formulary, 9th ed., London, HMSO, 1971, pp. 108–9.
80 Anon., ‘The month’, Practitioner, 1956, 176: 1–2, commentary accompanying a symposium on antibiotics printed, pp. 5–65.
81 M Finland, ‘Changing patterns of resistance of certain pathogenic bacteria to antimicrobial agents’, N. Engl. J. Med., 1955, 252: 570–80.
82 Joint Meeting, op. cit., note 56 above, p. 361.
83 The Times, 16 July 1953, p. 3.
84 Dr A Christie of Fazakerley Hospital, Liverpool, in a review for GPs on acute bronchitis in 1951, noted that most cases would eventually clear up without specific treatment, but only, “at the cost of several weeks’ ambulant illness, during which time the patients are a nuisance and danger to themselves and to other people”. Christie, op. cit., note 35 above, p. 84.
85 NA PRO, MH 132/48, Report of the Minister of Health for the year ending 1958. Part 11. On the state of the public health, being the annual report of the Chief Medical Officer. HMSO, London, Nov. 1959, p. 73.
86 P B Beeson, Walsh McDermott (eds), Cecil–Loeb textbook of medicine, Philadelphia, W B Saunders, 1971, pp. 361–2.
87 S Alstead, A G Macgregor, R H Gridgwood (eds), Textbook of medical treatment, 12th ed., Edinburgh, E & S Livingstone, 1971, p. 193. The 1st to 11th editions were edited by D Dunlop and others.
88 C Webster, The health services since the war: Volume 1: Problems of health care: the National Health Service before 1957, London, HMSO, 1988; idem, The health services since the war: Volume 2: Government and health care: The National Health Service 1958–1979, London, HMSO, 1996; Rivett, op. cit., note 29 above; V Berridge and K Loughlin (eds), Medicine, the market and the mass media: producing health in the twentieth century, London, Routledge, 2005.
89 NA PRO MH 132/30, Report of the Minister of Health for the year ending 31. Mar. 1950 including the report of the Chief Medical Officer on the state of the public health, HMSO, London, Sept. 1951, pp. 24–5.
90 NA PRO MH128/283, Report of the Cohen Committee on General Practice under the National Health Service, London, HMSO, 1954, p. 9.
91 C Webster, The National Health Service: a political history, Oxford University Press, 1998, p. 46.
92 J P Martin, Social aspects of prescribing, London, Heinemann, 1957. p. 109.
93 The Times, 4 July 1962, p. 5.
94 The Times, 20 Apr. 1957, p. 3.
95 Department of Health, Final Report of the Committee on Cost of Prescribing, London, HMSO, 1959, pp. 28–33, esp. p. 31.
96 Webster, vol. 1, op. cit., note 88 above, pp. 222–3.
97 NA PRO MH 135/709, Ministry of Health, England, Joint Pricing Committee for England, ‘Prescribing Investigation Unit: formation and rates of pay’, 1949–1961; NA PRO MH 123/293, Department of Health, Scotland, Report of the Scottish Committee on Prescribing Costs, Edinburgh, HMSO, 1959.
98 The Times, 3 Jan. 1959, p. 7.
99 H Davis, ‘The National Health Service and pharmacy’, J. Pharm. Pharmacol., 1954, 6: 761–72.
100 NA PRO, MH 132/49, Report of the Minister of Health for the year ending 1959. Part 1. The National Health Service, London, HMSO, July 1960.
101 Webster, op. cit., note 88 above, vol. 2, pp. 349–57.
102 S Taylor, Good general practice, London, Nuffield Provincial Hospitals Trust, Oxford University Press, 1954, pp. 64–7.
103 Martin, op. cit., note 92 above, pp. 15–16, 30–1; Anon, ‘Five years pricing’, Pharmaceutical J., 1954, 173: 61–2; Taylor, op. cit., note 102 above pp. 64–5.
104 L Johnston, ‘Preparing for general practice’, Lancet, 1950, ii: 824. Italics in original.
105 Taylor, op. cit., note 102 above, p. 183.
106 G Strong, ‘General practice today’, Lancet, 1950, i: 928–9, on p. 928.
107 RCGPA, op. cit., note 32 above, p. 4–5.
108 NA PRO, MH132/39, Report of the Minister of Health for the year ended 31 Dec 1954. Part I. The National Health Service, London, HMSO, 1955, p. 117.
109 NA PRO, FD 23/1934, Proposed Therapeutic Trail of Antibiotics in General Practice. Correspondence between Dr J Fry and the Medical Research Council, 1957.
110 The Times, 21 Feb. 1955, p. 9.
111 See Martin, op. cit., 92 above, p. 11.
112 The Times, 28 March 1952, p. 4.
113 Association of British Pharmaceutical Industry (hereafter ABPI), Annual report. 1964–5, London, ABPI, 1965, p. 13.
114 NA PRO, MH 135/61, Letter from Dr Charles Brooke to Mr Aneurin Bevan, 10 Nov. 1949.
115 See ABPI op. cit., note 113 above, p. 13.
116 ABPI, Annual report. 1966–7, London, ABPI, 1967, p. 10.
117 RCGPA, op. cit., note 32 above, p. 3.
118 Joint Meeting, op. cit., note 56 above, p. 359.
119 Boots plc Archives (hereafter BA) 3322/85, ‘Boots Penicillin Oral Tablets’, for the information of the Medical Profession, Nottingham, Boots Pure Drug Company Limited, 1950c. BA A126/1, Boots Information Leaflet, No. 39, ‘Cold and coughs’, for the information of the Pharmaceutical Staff, Nottingham, Boots Pure Drug Company Limited, 1950c.
120 ABPI, Annual report 1966–7, London, ABPI, 1967, pp. 15–16.
121 RCGPA, op. cit., note 32 above, p. 3.
122 The Times, 15 Apr., 1950, p. 4.
123 Good Housekeeping's encyclopaedia of family health: a modern illustrated home doctor, London, National Magazine, 1956, pp. 57–8.
124 G Somerville (ed.), Newnes family health encyclopaedia, London, George Newnes, 1959, p. 112; R L Clark, R W Cumley (eds), The book of health: a medical encyclopedia for everyone, Princeton, Van Nostrand, 1962, p. 135.
125 W A R Thomson, Black's medical dictionary, 22nd ed., London, Adam and Charles Black, 1955, pp. 143–5.
126 W Edwards, ‘Is your medicine really necessary?’, Family Doctor, 1951, 1: 259–61, p. 261.
127 C Brogan, ‘Are you a human medicine bottle?’ Family Doctor, 1952, 2: 428–30, p. 429.
128 D Tavistock, ‘Family doctor speaking about bronchitis’, Family Doctor, 1952, 2: 600–1; ‘All about bronchitis’, Family Doctor, 1953, 3: 158–9.
129 Tavistock, ‘Family doctor speaking about bronchitis’, op. cit., note 128 above, pp. 600–1.
130 RCGPA, ACE J 8–1, Letter from Dr Byrne to the Council of the College of General Practitioners, 14 Oct. 1957.
131 Ibid., Letter from Dr Ashworth to the Council of the College of General Practitioners, 15 Oct. 1957.
132 J T Macfarlane, W F Holmes, R M Macfarlane, N Britten, ‘Influence of patients’ expectations on antibiotic management of acute lower respiratory tract illness in general practice: questionnaire study’, Br. med. J., 1997, 315: 1211–14.
133 A Lake, ‘Are you overdosing with antibiotics?’, Reader's Digest, July 1953, pp. 23–5.
134 K C Hutchin, Coughs, colds and bronchitis, London, W & G Foyle, 1961, pp. 59–64.
135 There were no studies or trials that demonstrated the efficacy of antibiotics in acute bronchitis, as there was with streptomycin and tuberculosis. A Yoshioka, ‘Use of randomisation in the Medical Research Council's clinical trial of streptomycin in pulmonary tuberculosis in the 1940s’, Br. med. J., 1998, 317: 1220–23.
136 B Arroll, T Kenealy, ‘Antibiotics for acute bronchitis’, Br. med. J., 2001, 322: 939–40, and Audit Commission, A prescription for improvement. Towards more rational prescribing in general practice, London, HMSO, 1994.
137 Woodhead, Fleming, Wise, op. cit., note 5 above, pp. 1270–71.
138 Committee of the British Thoracic Society and British Infection Society, Health Protection Agency acting on behalf of the Department of Health. Clinical guidelines for patients with an influenza-like illness during an influenza pandemic (http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4121753), Version 10.5, 5 March 2006.
Contributor Information
JOHN T MACFARLANE, Nottingham University Hospitals, City Hospital Campus, Hucknall Road, Nottingham, NG5 1PB, UK; e-mail: j.macfarlane@nuh.nhs.uk.
MICHAEL WORBOYS, Centre for the History of Science, Technology and Medicine and Wellcome Unit for the History of Medicine, University of Manchester, Oxford Road, Manchester, M13 9PL, UK; e-mail: michael.worboys@manchester.ac.uk.