Low socioeconomic position (SEP) is a known risk factor for many causes of death,1,2 even after adjustment for known biological risk factors,3 but the relative contributions of personal and contextual (i.e., neighbourhood) SEP have not been clearly established.4 Neighbourhood of residence may capture several long-term effects on health (such as lifetime changes in SEP and biological risk factors) as well as the current SEP (such as personally reported income); it is not clear how much additional information it provides over and above personally reported SEP and biological risk factors. Many analyses showing personal and contextual SEP to be independently predictive of health outcomes have not been adjusted for biological risk factors.
From 1973 to 1975, 12 866 men aged 35–57 years who were at high risk for coronary heart disease (CHD), but without diabetes, clinical CHD or other excessive mortality risks, were randomized into the Multiple Risk Factor Intervention Trial (MRFIT).5 Twenty-two urban clinical sites in 14 states participated. Baseline data included age, cigarettes smoked per day, blood pressure, serum cholesterol, race/ethnicity, identifying information, and home address. Men were asked, “What was your total family income last year before deductions and taxes? Include family income from all sources,” and selected from nine ranges; cut points were $4200, $7200, $10 000, $12 000, $15 000, $18 000, $22 500 and $35 000. Incomes were estimated as the range midpoint, except for the lowest and highest ranges, where $4200 and $45 000 were used. Home addresses were geocoded and matched to 1980 Census tracts.1,6
Men were randomized 1:1 to either usual care or a multifactor CHD intervention and monitored for seven years. The intervention included smoking cessation counselling, dietary counselling to lower blood cholesterol, and stepped-care drug treatment for hypertension. Mortality was ascertained through 2003 using clinic records, Social Security Administration files, and the National Death Index (NDI). Cause of death was coded from death certificates or obtained from the NDI-plus service.7
Proportional hazards regression models were stratified by clinical site (except where noted) and adjusted for baseline risk factors (age, cigarettes smoked per day, systolic blood pressure, and serum cholesterol), intervention group, and three racial/ethnic indicators: African-American (n=769), Hispanic-American (n=170), and Asian-American (n=120).4 Non-Hispanic whites (n=9756), Native Americans (n=13) and ‘Other’ (n=37) were the referent group. Income variables (family-level income and Census tract-level median household income from 4975 tracts) were then included, separately or together. Hazard ratios (HRs) and 95% confidence intervals were obtained from the models. Likelihood ratio tests were used to compare models, overall. Additional analyses examined the joint relationship of these income measures with mortality: age-adjusted mortality rates were computed for 16 groups defined by quartiles of the two income measures, and within quartiles of each income measure, adjusted HRs for the other income measure were computed and tested for categorical differences.
Of the 12 866 men randomized into the MRFIT, 10 865 had complete data, including a geocodable address. Tract-level median household income and family-level income had means (± standard deviation (SD)) of $21 920 (± $7242) and $21 709 (± $9572), and a correlation coefficient of 0.37.
Over an average follow-up of 30 years, 5094 (47%) participants died. Considered singly in risk-adjusted all-cause mortality models, family-level and tract-level income were each significant inverse mortality predictors, with the excess mortality from one SD less of family-level income (11%) being nearly three times as great as that from one SD less of tract-level income (4%) (Table 1). As the sole SEP variable in a model, each made an improvement in model fit, versus a model with risk factors alone (P=0.01 for tract-level income; P<0.0001 for family-level income). Adding tract-level income to a model with family-level income and risk factors did not meaningfully improve model fit (P=0.96) or the HR for family-level income. In contrast, adding family-level income to a model with tract-level income and risk factors improved model fit (P<0.0001) and completely attenuated the tract-level income effect. Similar relationships between the HRs for tract-level and family-level income were found for cause-specific mortality.
Table 1.
Census tract-based median household income and personally reported family income as risk-adjusted mortality predictors for 10 865 randomized men from the Multiple Risk Factor Intervention Trial (baseline 1973–75); mortality follow-up through 2003.
| Hazard ratio (95% confidence interval) associated with one standard deviation less income
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Cause of death | Number of deaths | Model 1 | Model 2 | Model 3 | Difference in −2log(partial likelihood) versus model 0a | |||
| Median Census tract household income (per $7242 less income) | Personally reported family income (per $9572 less income) | Median Census tract income (per $7242 less income) | Personally reported family income (per $9572 less income) | Model 1 | Model 2 | Model 3 | ||
| All-cause | 5094 | 1.04 (1.01–1.07) | 1.11 (1.08–1.15) | 1.00 (0.97–1.03) | 1.11 (1.08–1.15) | 6.0 | 53.1 | 53.1 |
| Cardiovascular diseases | 2422 | 1.07 (1.02–1.11) | 1.14 (1.10–1.19) | 1.02 (0.97–1.07) | 1.14 (1.09–1.19) | 8.2 | 39.0 | 39.7 |
| Coronary heart disease | 1657 | 1.04 (0.99–1.10) | 1.14 (1.08–1.20) | 1.00 (0.94–1.06) | 1.14 (1.08–1.21) | 2.7 | 26.3 | 26.3 |
| All cancer | 1567 | 1.01 (0.96–1.07) | 1.07 (1.02–1.13) | 0.99 (0.93–1.05) | 1.07 (1.02–1.13) | 0.2 | 6.7 | 6.9 |
| Lung cancer | 578 | 1.01 (0.93–1.11) | 1.09 (1.00–1.18) | 0.98 (0.89–1.08) | 1.09 (1.00–1.20) | 0.1 | 3.9 | 4.0 |
| Accident, injury and violence | 177 | 0.92 (0.78–1.08) | 1.02 (0.87–1.19) | 0.90 (0.76–1.07) | 1.05 (0.89–1.24) | 1.1 | 0.0 | 1.5 |
Model 0: Variables are age, cigarettes per day, serum cholesterol, systolic blood pressure, and three racial/ethnic indicators (African-American, Hispanic-American and Asian-American).
Model 1: Add median household income, by Census tract, to Model 0.
Model 2: Add personally reported family income to Model 0.
Model 3: Add both tract-based median household income and personally reported family income to Model 0.
In two nested models, the difference in −2log(partial likelihood) has a Chi-squared distribution and may be used to test for statistically significant improvements in a model fit.
To assess the influence of the risk factor adjustment on the association between each income measure and all-cause mortality, models with both income variables and various risk factor adjustments were considered. When adjusting for only age or age and randomization group, the estimated HR for tract-level income was 1.03 (95% CI 0.99–1.06); in a model adjusting for age and race/ethnicity, the estimated HR was 1.02, and in a fully adjusted model the HR was 1.00 (model 3 in Table 1). The estimated HR for family-level income remained nearly constant (range 1.10 to 1.11).
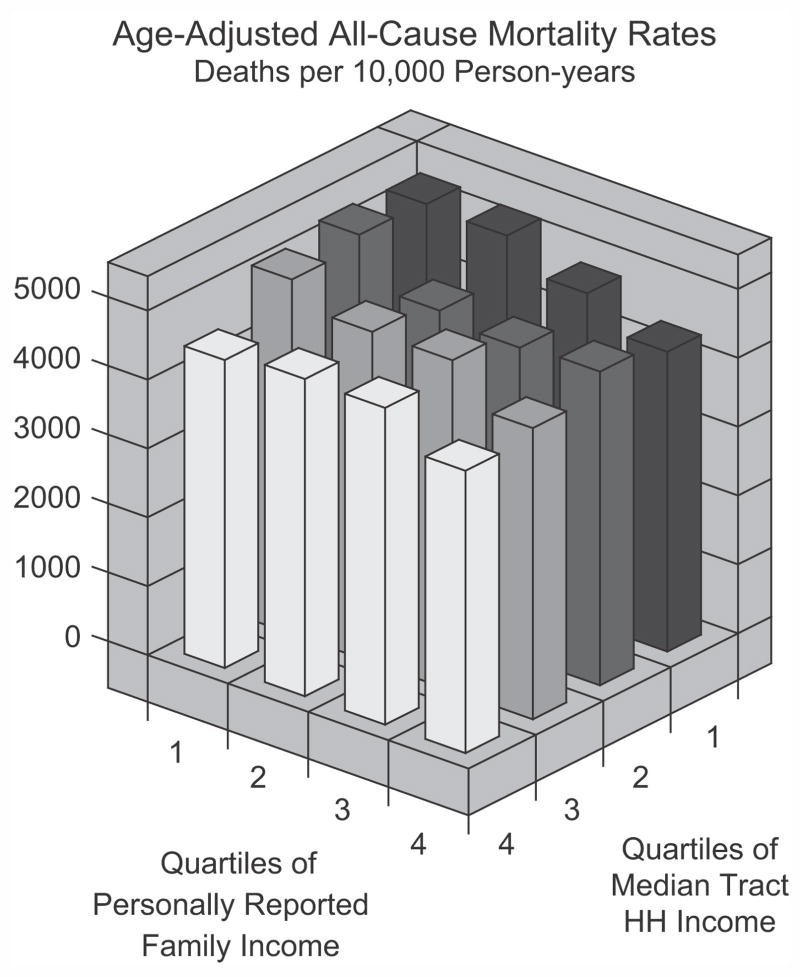
Within quartiles of tract-level income, family-level income was consistently inversely related to mortality (Fig. 1); across tract-level quartiles, risk-adjusted HRs for one SD less family-level income ranged from 1.06 to 1.16 (P-value for differences=0.10). Within quartiles of family-level income, a weaker inverse association between tract-level income and mortality was evident; risk-adjusted HRs for one SD less of tract-level income ranged from 0.99 to 1.05 (P-value for differences=0.68).
Figure 1.
Census-based and personally reported income measures as long-term risk-adjusted mortality predictors. The approximate quartiles of personally reported family income were as follows. Lowest quartile: 0–$14 999 (26% of participants); second quartile: $15 000–$17 999 (17% of participants); third quartile $18 000–$22 499 (23% of participants); and fourth quartile: $22 500 or higher (34% of participants). Quartile cut points for tract-based household income were $17 241, $21 196, and $25 887; each quartile contained 25% of participants.
Census tract-level and family-level income were both inverse mortality predictors in risk-adjusted models when used as stand-alone SEP estimators, though the area-based measure had a smaller effect per standard deviation (4% versus 11%). Age-adjusted mortality differences attributed to each income variable persisted across quartiles of the other income variable. In models containing both income variables, the estimated HR for tract-level income decreased from 1.03 (95% CI 0.99–1.06) to 1.00 as more risk factors were incorporated, suggesting that contextual SEP effects may reflect processes that are better captured by biological and behavioural risk factors.2 Many of the studies showing area-based and family-level incomes to be independent mortality predictors did not adjust for biological and behavioural risk factors;2,8–10 this may explain some of the differences between those results and ours. Other studies, with more life course SEP or biological risk factor adjustments, tend to show as we do that area-level SEP predictors are dominated by personally reported SEP.11
For 10 865 men randomized into the MRFIT in 1973–1975 and followed for 30 years, both family income and Census tract-based median household income were collected, permitting comparisons of each with mortality risks. Each income measure performed similarly as a stand-alone risk-adjusted mortality predictor. Census tract-level income added predictive value beyond family-level income only in models that excluded biological and behavioural risk factors, thus indicating that area-based SEP measures and conventional risk factors, both the result of long-term processes, are strongly overlapping mortality predictors. These patterns held across various causes of death, showing that the relationships between personal and contextual SEP and risk factors were not limited to any one disease.
Acknowledgments
The Multiple Risk Factor Intervention Trial was conducted under contract with the National Heart, Lung, and Blood Institute, Bethesda, MD, USA. This work was supported by National Heart, Lung, and Blood Institute Grants # R01-HL-43232 and # R01-HL-68140.
The authors would like to thank the current Multiple Risk Factor Intervention Trial Editorial Committee: Jerome Cohen, Saint Louis University School of Medicine; Jeffrey Cutler, NHLBI; Lynn Eberly, University of Minnesota; Greg Grandits, University of Minnesota; Richard Grimm, Hennepin County Medical Center, Minneapolis, MN; Lewis Kuller, University of Pittsburgh; James Neaton, University of Minnesota; Judith Ockene, University of Massachusetts Medical School; Ronald Prineas, Wake Forest University School of Medicine; Jeremiah Stamler, Northwestern University Medical School; and Avis Thomas, University of Minnesota.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tyroler HA. Socioeconomic status in the epidemiology and treatment of hypertension. Hypertension. 1989;13(5 Suppl):I94–7. doi: 10.1161/01.hyp.13.5_suppl.i94. [DOI] [PubMed] [Google Scholar]
- 2.Stamler J, Hazuda HP. Report of the conference on socioeconomic status and cardiovascular health and disease. National Heart, Lung and Blood Institute; National Institutes of Health; Bethesda, Maryland, USA: November 6–7, 1995. [Google Scholar]
- 3.Davey Smith G, Neaton JD, Wentworth D, Stamler R, Stamler J for the MRFIT Research Group. Mortality differences between black and white men in the USA: contribution of income and other risk factors among men screened for the MRFIT. Lancet. 1998;351:934–9. doi: 10.1016/s0140-6736(00)80010-0. [DOI] [PubMed] [Google Scholar]
- 4.Diez-Roux AV, Kiefe CI, Jacobs DR, Haan M, Jackson SA, Nieto FJ, Paton CC, Schulz R. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies. Ann Epidemiol. 2001;11:395–405. doi: 10.1016/s1047-2797(01)00221-6. [DOI] [PubMed] [Google Scholar]
- 5.Multiple Risk Factor Intervention Trial Research Group. Multiple risk factor intervention trial: risk factor changes and mortality results. JAMA. 1982;248:1465–77. [PubMed] [Google Scholar]
- 6.Thomas AJ, Eberly LE, Neaton JD, Davey Smith G for the Multiple Risk Factor Intervention Trial (MRFIT) Research Group. Latino risk-adjusted mortality in the men screened for the multiple risk factor intervention trial (MRFIT) Am J Epidemiol. 2005;162:569–78. doi: 10.1093/aje/kwi220. [DOI] [PubMed] [Google Scholar]
- 7.Thomas A, Eberly L, Davey Smith G, Neaton J, Stamler J for the MRFIT Research Group. Race/ethnicity, income, major risk factors and cardiovascular disease mortality. Am J Public Health. 2005;95:1417–23. doi: 10.2105/AJPH.2004.048165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robert S. Community-level socioeconomic status effects on adult health. J Health Soc Behav. 1998;39:18–37. [PubMed] [Google Scholar]
- 9.Robert S. Socioeconomic position and health: the independent contribution of community socioeconomic context. Annu Rev Sociol. 1999;25:489–516. [Google Scholar]
- 10.Winkelby M, Cubbin C, Ahn D. Effect of cross-level interaction between individual and neighborhood socioeconomic status on adult mortality rates. Am J Public Health. 2006;96:2145–53. doi: 10.2105/AJPH.2004.060970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naess O, Leyland A, Davey Smith G, Claussen B. Contextual effect on mortality of neighbourhood level education explained by earlier life deprivation. J Epidemiol Community Health. 2005;59:1058–9. doi: 10.1136/jech.2005.036822. [DOI] [PMC free article] [PubMed] [Google Scholar]