Abstract
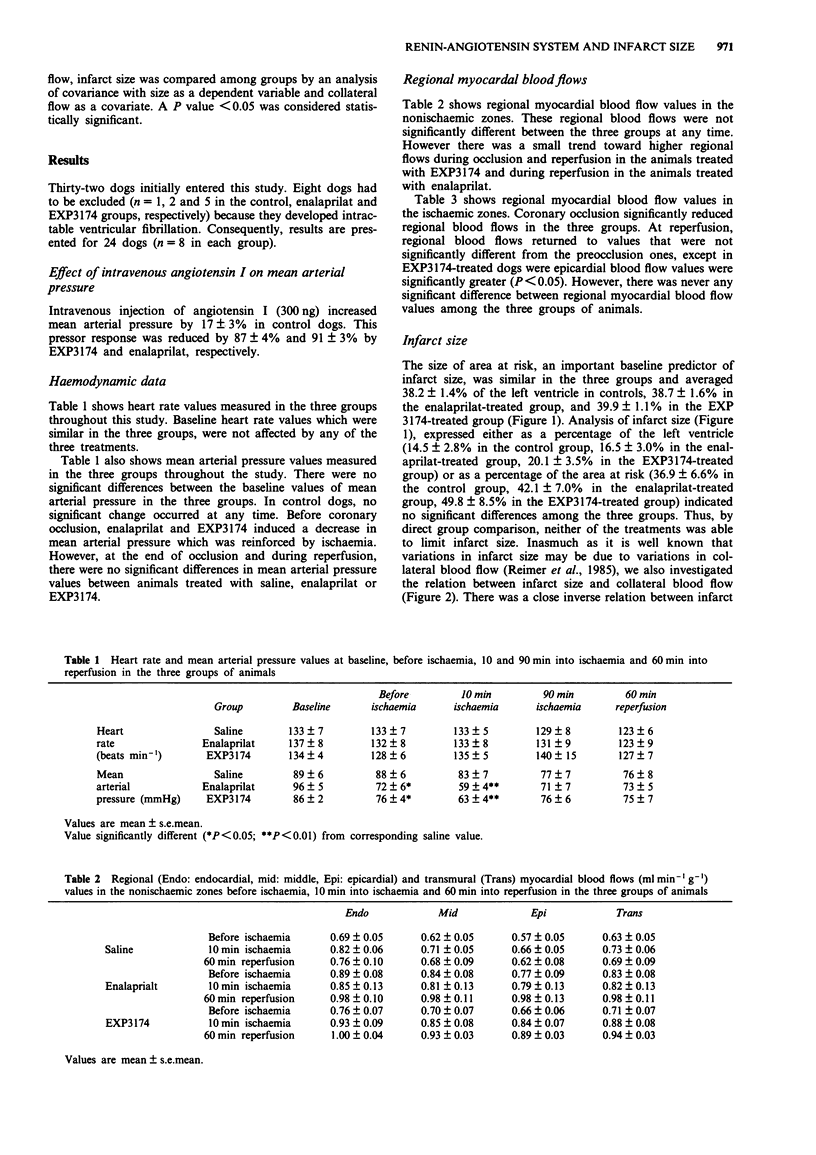
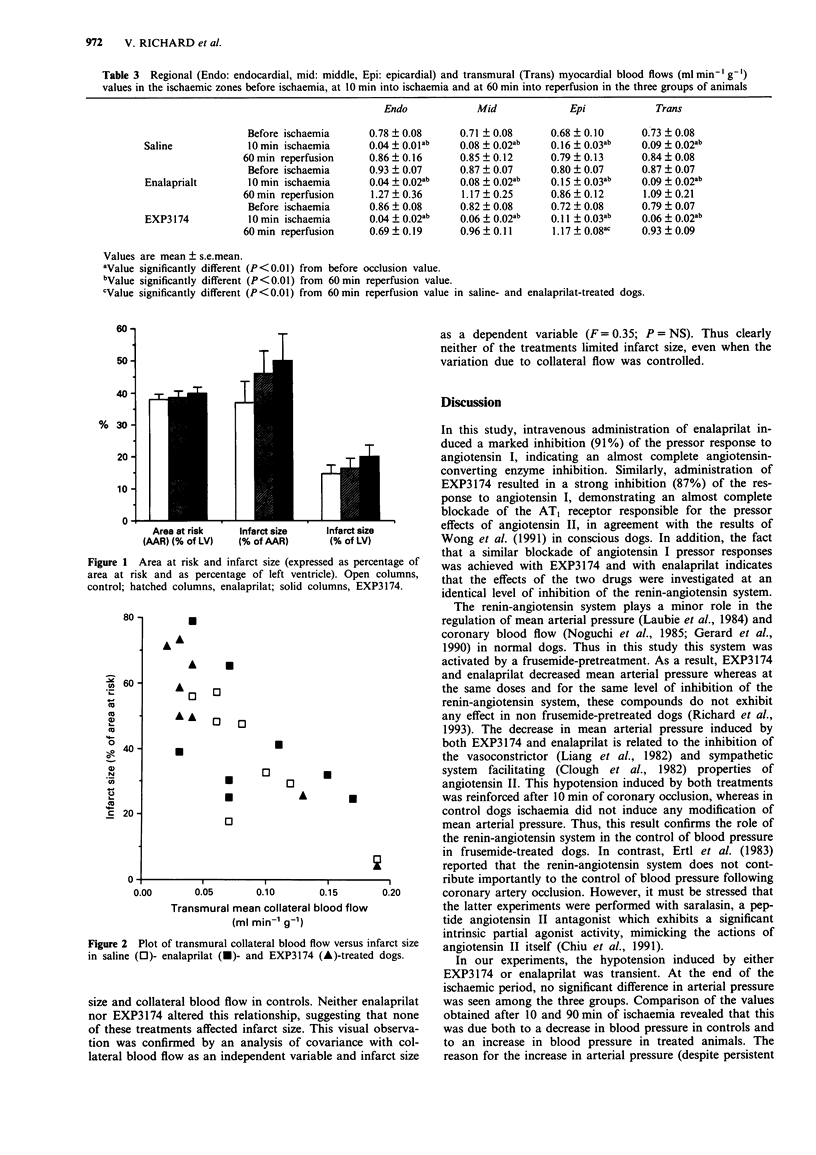
1. In order to determine whether the renin-angiotensin system is involved in myocardial ischaemia-reperfusion injury, we investigated and compared the effects on infarct size of two different drugs which interfere with this system, i.e., an angiotensin II (AT1) antagonist, EXP3174, and an angiotensin I-converting enzyme inhibitor (ACEI), enalaprilat in a canine model of ischaemia-reperfusion. 2. EXP3174 (0.1 mg kg-1, i.v. followed by 0.02 mg kg-1 h-1 for 5.5 h) and enalaprilate (0.3 mg kg-1, i.v. followed by 0.06 mg kg-1 h-1 for 5.5 h) were used in doses inducing a similar level of inhibition (87 +/- 4 and 91 +/- 3%, respectively) of the pressor responses to angiotensin I. Control animals received saline. 3. Infarct size and area at risk were quantified by ex vivo dual coronary perfusion with triphenyltetrazolium chloride and monastral blue dye. Regional myocardial blood flows (ischaemic and nonischaemic, endocardial, epicardial) were assessed by the radioactive microsphere technique. 4. Both EXP3174 and enalaprilat induced a decrease in mean arterial blood pressure. However, non significant changes in regional myocardial blood flows, whether ischaemic or nonischaemic, were observed after administration of either the ACEI or the AT1 antagonist. 5. The size of the area at risk was similar in the three groups. By direct comparison, there were no significant differences between infarct sizes in the three groups. Furthermore, there was a close inverse relationship between infarct size and transmural mean collateral blood flow in controls, and none of the treatments altered this correlation. Thus, neither EXP3174 nor enalaprilat limited infarct size.(ABSTRACT TRUNCATED AT 250 WORDS)
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ambrosioni E., Borghi C. Potential use of ACE inhibitors after acute myocardial infarction. J Cardiovasc Pharmacol. 1989;14 (Suppl 9):S92–S94. [PubMed] [Google Scholar]
- Baumgarten C. R., Linz W., Kunkel G., Schölkens B. A., Wiemer G. Ramiprilat increases bradykinin outflow from isolated hearts of rat. Br J Pharmacol. 1993 Feb;108(2):293–295. doi: 10.1111/j.1476-5381.1993.tb12797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker R. H., Linz W., Schölkens B. A. Pharmacological interference with the cardiac renin-angiotensin system. J Cardiovasc Pharmacol. 1989;14 (Suppl 4):S10–S15. [PubMed] [Google Scholar]
- Berdeaux A., Bonhenry C., Giudicelli J. F. Effects of four angiotensin I converting enzyme inhibitors on regional myocardial blood flow and ischemic injury during coronary artery occlusion in dogs. Fundam Clin Pharmacol. 1987;1(3):201–212. doi: 10.1111/j.1472-8206.1987.tb00558.x. [DOI] [PubMed] [Google Scholar]
- Chiu A. T., McCall D. E., Price W. A., Jr, Wong P. C., Carini D. J., Duncia J. V., Wexler R. R., Yoo S. E., Johnson A. L., Timmermans P. B. In vitro pharmacology of DuP 753. Am J Hypertens. 1991 Apr;4(4 Pt 2):282S–287S. doi: 10.1093/ajh/4.4.282s. [DOI] [PubMed] [Google Scholar]
- Chopra M., Beswick H., Clapperton M., Dargie H. J., Smith W. E., McMurray J. Antioxidant effects of angiotensin-converting enzyme (ACE) inhibitors: free radical and oxidant scavenging are sulfhydryl dependent, but lipid peroxidation is inhibited by both sulfhydryl- and nonsulfhydryl-containing ACE inhibitors. J Cardiovasc Pharmacol. 1992 Mar;19(3):330–340. doi: 10.1097/00005344-199203000-00005. [DOI] [PubMed] [Google Scholar]
- Clough D. P., Collis M. G., Conway J., Hatton R., Keddie J. R. Interaction of angiotensin-converting enzyme inhibitors with the function of the sympathetic nervous system. Am J Cardiol. 1982 Apr 21;49(6):1410–1414. doi: 10.1016/0002-9149(82)90352-6. [DOI] [PubMed] [Google Scholar]
- Daniell H. B., Carson R. R., Ballard K. D., Thomas G. R., Privitera P. J. Effects of captopril on limiting infarct size in conscious dogs. J Cardiovasc Pharmacol. 1984 Nov-Dec;6(6):1043–1047. [PubMed] [Google Scholar]
- Ertl G., Alexander R. W., Kloner R. A. Interactions between coronary occlusion and the renin-angiotensin system in the dog. Basic Res Cardiol. 1983 Sep-Oct;78(5):518–533. doi: 10.1007/BF01906463. [DOI] [PubMed] [Google Scholar]
- Ertl G. Coronary vasoconstriction in experimental myocardial ischemia. J Cardiovasc Pharmacol. 1987;9 (Suppl 2):S9–17. doi: 10.1097/00005344-198700002-00004. [DOI] [PubMed] [Google Scholar]
- Ertl G., Kloner R. A., Alexander R. W., Braunwald E. Limitation of experimental infarct size by an angiotensin-converting enzyme inhibitor. Circulation. 1982 Jan;65(1):40–48. doi: 10.1161/01.cir.65.1.40. [DOI] [PubMed] [Google Scholar]
- Grover G. J., Sleph P. G., Dzwonczyk S., Wang P., Fung W., Tobias D., Cushman D. W. Effects of different angiotensin-converting enzyme (ACE) inhibitors on ischemic isolated rat hearts: relationship between cardiac ACE inhibition and cardioprotection. J Pharmacol Exp Ther. 1991 Jun;257(3):919–929. [PubMed] [Google Scholar]
- Gérard J. L., Pussard E., Berdeaux A., Giudicelli J. F. Hemodynamic and cardiac effects of spiraprilat in normal and sodium depleted conscious dogs. Fundam Clin Pharmacol. 1990;4(5):547–558. doi: 10.1111/j.1472-8206.1990.tb00039.x. [DOI] [PubMed] [Google Scholar]
- Heusch G. Alpha-adrenergic mechanisms in myocardial ischemia. Circulation. 1990 Jan;81(1):1–13. doi: 10.1161/01.cir.81.1.1. [DOI] [PubMed] [Google Scholar]
- Heyndrickx G. R., Boettcher D. H., Vatner S. F. Effects of angiotensin, vasopressin, and methoxamine on cardiac function and blood flow distribution in conscious dogs. Am J Physiol. 1976 Nov;231(5 Pt 1):1579–1587. doi: 10.1152/ajplegacy.1976.231.5.1579. [DOI] [PubMed] [Google Scholar]
- Hock C. E., Ribeiro L. G., Lefer A. M. Preservation of ischemic myocardium by a new converting enzyme inhibitor, enalaprilic acid, in acute myocardial infarction. Am Heart J. 1985 Feb;109(2):222–228. doi: 10.1016/0002-8703(85)90587-3. [DOI] [PubMed] [Google Scholar]
- Kobayashi M., Furukawa Y., Chiba S. Positive chronotropic and inotropic effects of angiotensin II in the dog heart. Eur J Pharmacol. 1978 Jul 1;50(1):17–25. doi: 10.1016/0014-2999(78)90249-2. [DOI] [PubMed] [Google Scholar]
- Laubie M., Schiavi P., Vincent M., Schmitt H. Inhibition of angiotensin I-converting enzyme with S 9490: biochemical effects, interspecies differences, and role of sodium diet in hemodynamic effects. J Cardiovasc Pharmacol. 1984 Nov-Dec;6(6):1076–1082. [PubMed] [Google Scholar]
- Lefer A. M., Peck R. C. Cardioprotective effects of enalapril in acute myocardial ischemia. Pharmacology. 1984;29(2):61–69. doi: 10.1159/000137993. [DOI] [PubMed] [Google Scholar]
- Liang C. S., Gavras H., Black J., Sherman L. G., Hood W. B., Jr Renin-angiotensin system inhibition in acute myocardial infarction in dogs. Effects on systemic hemodynamics, myocardial blood flow, segmental myocardial function and infarct size. Circulation. 1982 Dec;66(6):1249–1255. doi: 10.1161/01.cir.66.6.1249. [DOI] [PubMed] [Google Scholar]
- Linder C., Heusch G. ACE inhibitors for the treatment of myocardial ischemia? Cardiovasc Drugs Ther. 1990 Oct;4(5):1375–1384. doi: 10.1007/BF02018265. [DOI] [PubMed] [Google Scholar]
- Martorana P. A., Kettenbach B., Breipohl G., Linz W., Schölkens B. A. Reduction of infarct size by local angiotensin-converting enzyme inhibition is abolished by a bradykinin antagonist. Eur J Pharmacol. 1990 Jul 3;182(2):395–396. doi: 10.1016/0014-2999(90)90301-l. [DOI] [PubMed] [Google Scholar]
- Noguchi K., Kato T., Ito H., Aniya Y., Sakanashi M. Effect of intracoronary captopril on coronary blood flow and regional myocardial function in dogs. Eur J Pharmacol. 1985 Mar 26;110(1):11–19. doi: 10.1016/0014-2999(85)90023-8. [DOI] [PubMed] [Google Scholar]
- Przyklenk K., Kloner R. A. Relationships between structure and effects of ACE inhibitors: comparative effects in myocardial ischaemic/reperfusion injury. Br J Clin Pharmacol. 1989;28 (Suppl 2):167S–175S. doi: 10.1111/j.1365-2125.1989.tb03592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reimer K. A., Jennings R. B., Cobb F. R., Murdock R. H., Greenfield J. C., Jr, Becker L. C., Bulkley B. H., Hutchins G. M., Schwartz R. P., Jr, Bailey K. R. Animal models for protecting ischemic myocardium: results of the NHLBI Cooperative Study. Comparison of unconscious and conscious dog models. Circ Res. 1985 May;56(5):651–665. doi: 10.1161/01.res.56.5.651. [DOI] [PubMed] [Google Scholar]
- Richard V., Berdeaux A., Giudicelli J. F. Systemic and coronary effects of the angiotensin II receptor antagonist EXP3174 in dogs. J Cardiovasc Pharmacol. 1993 Jul;22(1):52–57. doi: 10.1097/00005344-199307000-00009. [DOI] [PubMed] [Google Scholar]
- Schömig A., Dart A. M., Dietz R., Mayer E., Kübler W. Release of endogenous catecholamines in the ischemic myocardium of the rat. Part A: Locally mediated release. Circ Res. 1984 Nov;55(5):689–701. doi: 10.1161/01.res.55.5.689. [DOI] [PubMed] [Google Scholar]
- Wong P. C., Hart S. D., Duncia J. V., Timmermans P. B. Nonpeptide angiotensin II receptor antagonists. Studies with DuP 753 and EXP3174 in dogs. Eur J Pharmacol. 1991 Sep 24;202(3):323–330. doi: 10.1016/0014-2999(91)90274-t. [DOI] [PubMed] [Google Scholar]
- Wong P. C., Price W. A., Jr, Chiu A. T., Duncia J. V., Carini D. J., Wexler R. R., Johnson A. L., Timmermans P. B. Nonpeptide angiotensin II receptor antagonists. XI. Pharmacology of EXP3174: an active metabolite of DuP 753, an orally active antihypertensive agent. J Pharmacol Exp Ther. 1990 Oct;255(1):211–217. [PubMed] [Google Scholar]
- de Lorgeril M., Ovize M., Delaye J., Renaud S. Importance of the flow perfusion deficit in the response to captopril in experimental myocardial infarction. J Cardiovasc Pharmacol. 1992 Mar;19(3):324–329. doi: 10.1097/00005344-199203000-00004. [DOI] [PubMed] [Google Scholar]
- van Gilst W. H., Tio R. A., van Wijngaarden J., de Graeff P. A., Wesseling H. Effects of converting enzyme inhibitors on coronary flow and myocardial ischemia. J Cardiovasc Pharmacol. 1992;19 (Suppl 5):S134–S139. [PubMed] [Google Scholar]
- van Gilst W. H., van Wijngaarden J., Scholtens E., de Graeff P. A., de Langen C. D., Wesseling H. Captopril-induced increase in coronary flow: an SH-dependent effect on arachidonic acid metabolism? J Cardiovasc Pharmacol. 1987;9 (Suppl 2):S31–S36. [PubMed] [Google Scholar]


