Abstract
There is growing evidence that yoga may offer a safe and cost-effective intervention for Type 2 Diabetes mellitus (DM 2). However, systematic reviews are lacking. This article critically reviews the published literature regarding the effects of yoga-based programs on physiologic and anthropometric risk profiles and related clinical outcomes in adults with DM 2. We performed a comprehensive literature search using four computerized English and Indian scientific databases. The search was restricted to original studies (1970–2006) that evaluated the metabolic and clinical effects of yoga in adults with DM 2. Studies targeting clinical populations with cardiovascular disorders that included adults with comorbid DM were also evaluated. Data were extracted regarding study design, setting, target population, intervention, comparison group or condition, outcome assessment, data analysis and presentation, follow-up, and key results, and the quality of each study was evaluated according to specific predetermined criteria. We identified 25 eligible studies, including 15 uncontrolled trials, 6 non-randomized controlled trials and 4 randomized controlled trials (RCTs). Overall, these studies suggest beneficial changes in several risk indices, including glucose tolerance and insulin sensitivity, lipid profiles, anthropometric characteristics, blood pressure, oxidative stress, coagulation profiles, sympathetic activation and pulmonary function, as well as improvement in specific clinical outcomes. Yoga may improve risk profiles in adults with DM 2, and may have promise for the prevention and management of cardiovascular complications in this population. However, the limitations characterizing most studies preclude drawing firm conclusions. Additional high-quality RCTs are needed to confirm and further elucidate the effects of standardized yoga programs in populations with DM 2.
Keywords: blood pressure, cardiovascular disease, coagulation, glycemia, insulin resistance, lipids, lung function, oxidative stress, sympathetic activity
Introduction
Type 2 Diabetes mellitus (DM 2) is a leading cause of death and disability in the United States (US) and other industrialized nations (1–3) as well as in a growing number of developing countries (4–6). In the United States, newly diagnosed cases of DM 2 have increased ∼50% in the past 10 years alone (2). As of 2002, DM 2 was estimated to affect ∼16 million Americans, with 1.3 million new cases diagnosed each year (2). An additional 41 million or more people have impaired glucose tolerance or impaired fasting glucose, collectively referred to as prediabetes, a powerful predictor of clinical DM 2 (1,2,7). Both diabetes and prediabetes dramatically increase risk for cardiovascular disease (CVD) and stroke, and for death due to CVD-related causes (2,7,8). Leading to premature morbidity and mortality, and to prevene disability and work loss, DM 2 is clearly of pressing clinical and economic significance, with direct medical expenditures for DM 2 in the United States totaling over $92 billion in 2002 alone (1,2).
While diabetes is a glycemic disorder, diagnosed on the basis of elevated blood glucose levels, it is a complex condition characterized by multiple, underlying and interrelated metabolic abnormalities linked to insulin resistance (3,9,10). These alterations, together comprising the insulin resistance or metabolic syndrome, collectively and independently predict the development of DM 2 (1,9–11) and related vascular disorders, including atherosclerosis and CVD (1,9,11–16). Core features of the insulin resistance syndrome (IRS) are glucose intolerance, insulin resistance, atherogenic dyslipidemia, visceral adiposity and high blood pressure (12,14,16,17). Other abnormalities associated with the IRS and linked to the pathogenesis and progression of DM 2 (10,18–21) include hypercoagulation (10,14,20,21), chronic inflammation (8,14,16,17,19,21), endothelial dysfunction (8,10,14,20–22), oxidative stress (18,22) and impaired lung function (23–25). Increased sympathetic activity, enhanced cardiovascular reactivity and reduced parasympathetic tone have also been implicated in the pathogenesis of IRS (14,21,26–30) and in the development and progression of DM 2 and related cardiovascular complications (21,31,32). In addition, there is mounting evidence that chronic psychological stress and negative mood states are strongly associated, in a bidirectional manner, with insulin resistance (33–37), glucose intolerance (34,38), central obesity (39–41) dyslipidemia (34,37,42), hypertension (43–47) and other components of the IRS (33,39,48–54). Likewise, prospective studies have shown depression, a common comorbidity in diabetic populations (55,56) and a powerful predictor of CVD morbidity and mortality (45,52,57–62), to increase risk for developing DM 2 by 2- to 3-fold (56,63,64).
Clearly, there is a need to identify cost-effective prevention and management strategies for DM 2 that address the multiple interrelated factors underlying this complex, devastating and increasingly common disorder. In light of the strong influence of psychosocial factors on the development of IRS and DM 2, the role of sympathetic activation in the pathogenesis of insulin resistant states, and the bi-directional relationships of these and other IRS-related risk factors, mind–body therapies may hold particular promise for both the prevention and treatment of DM 2. Of particular interest in this regard is yoga, an ancient mind–body discipline that has been widely used in India for the management of diabetes, hypertension and related chronic insulin resistance conditions (65–69).
Originating in India over 4000 years ago, the practice of yoga has been rising steadily in the United States and other industrialized countries during recent decades (70–72). Of the seven major branches of Hindu yoga, Hatha (or forceful) yoga, Raja (Royal or classical) yoga, and Mantra yoga are perhaps the best known and most commonly practiced forms. Mantra yoga, emphasizing the use of specific sounds or chants to achieve mental and spiritual transformation, was popularized in the West by Maharishi Mahesh Yogi, the founder of Transcendental Meditation (TM). Raja yoga, Patanjali's eight limb system of meditation, contemplation and renunciation, seeks self-realization and transformation through progressive control of the mind (73). Hatha yoga, the branch of yoga most widely practiced in the Western industrialized world, approaches self-realization and healing through the physical body and its energetic (pranic/etheric) template, with a focus on breath control (pranayama) and specific postures (asanas), including both active and relaxation poses (73). Hatha yoga also incorporates mental concentration (dharana), and meditation (dhyana), mantras or chants, cleansing exercises (kriyas), and specific hand gestures (mudras) (74). With no appreciable side effects and multiple collateral lifestyle benefits (70,72,75,76), yoga appears safe, is simple to learn, and can be practiced by even ill, elderly or disabled individuals (77). Yoga is also easy and inexpensive to maintain, requiring little in the way of equipment or professional personnel, with some studies indicating excellent long-term adherence and benefits (78–80). Notably, there is growing evidence that yoga practice may aid in the prevention and management of DM 2, reduce IRS-related risk factors associated with DM 2, and may improve the prognosis and attenuate signs of those with clinical DM 2 (69,81–85).
In this paper, we critically review the published scientific literature regarding the influence of yoga on metabolic perturbations of DM 2 and on related clinical outcomes, taking into account the major limitations and biases of these studies. Relevant findings from non-diabetic populations regarding observed effects of yoga on IRS-related risk factors for CVD and associated clinical outcomes, reviewed in depth in a previous publication (82), are also summarized, and the implications of these findings for the primary and secondary prevention of DM 2 are discussed.
Methods
We conducted a thorough search of the published medical literature to identify studies regarding the effects of yoga in adults with diabetes. The search was restricted to English language articles published after 1970 and available in US libraries, and to original studies specifically evaluating the effects of yoga (alone or in combination with other interventions) on metabolic, anthropometric or clinical profiles of adults with DM. Because DM is so often associated with CVD (9,10), studies targeting populations with or at risk for cardiovascular disorders that explicitly included adults with DM were also evaluated. Original studies were included in the review if they reported outcome data and evaluated the effects of yoga and yoga-based interventions on clinical measures of insulin resistance, lipid profiles, body weight or composition, blood pressure, oxidative stress, coagulation/fibrinolytic profiles, lung function, or on markers of sympathetic activation and cardiovagal function. We also included studies assessing the influence of yoga and yoga-based programs on relevant clinical outcomes, including medication use, DM- or CVD-related events and hospitalizations, and measures of CVD progression.
Since the etiology and management for Type 1 diabetes differs from that of type 2 diabetes, studies targeting only populations with type 1 diabetes were excluded. Case studies, abstracts from conference proceedings and anecdotal reports were also eliminated, as were studies with intervention group sizes of less than four subjects. Articles were identified using MEDLINE, PubMED and psycINFO, three commercially indexed, scientific databases. Because the majority of studies investigating the effects of yoga therapy have been conducted in the Indian subcontinent and these databases offer only incomplete capture of articles published in Indian medical journals, IndMED, a bibliographic database of over 75 major Indian biomedical journals, was also searched. Search words included yoga, yogic, relaxation, mind–body and meditation. In addition, the citation sections of all identified articles, including review papers, were scanned to identify relevant papers not indexed in PsycINFO, PubMED, MEDLINE or IndMED.
Each eligible study (i.e. each study identified that met our inclusion criteria) was classified into one of three design categories: randomized controlled trials (RCTs), non-randomized controlled trials (NRCTs) and uncontrolled (pre-post) trials. In RCTs, an investigator randomly allocates a yoga or yoga-based program to one group (the experimental or yoga group) and no intervention, usual care, or another intervention to one or more other groups (controls). Both groups are then evaluated to determine change over time in specific indices of CVD risk. In NRCT, the experimental design and analytic strategy are similar to that of RCTs, but the allocation to a given treatment is not performed randomly. In uncontrolled (pre–post) studies, all subjects participate in a yoga or yoga-based program, and change over time (baseline to post-intervention) in specific indices of CVD risk is evaluated.
Study quality was evaluated using criteria based on those utilized in recent systematic reviews regarding the effects of yoga (82) and other popular mind–body therapies (86,87). Criteria included (i) adequate sample size; (ii) explicit eligibility criteria and/or adequate description of study population; (iii) single, well-defined intervention; (iv) appropriate control group(s) or comparison condition(s); (v) randomization of treatment allocation; (vi) blinding of outcome assessment; (vii) adequate accounting for confounders; (viii) statistical methods well described and appropriate; (ix) outcome measures well-defined and point estimates and measures of variability presented; (x) adequate follow-up/drop-out rate reported; and (xi) conclusions supported by findings.
Clinical measures and outcomes evaluated were categorized into several different domains (Table 2). For each domain, we summarized findings from relevant studies. Due to the heterogeneity of study designs, settings, interventions and outcomes, we did not conduct a meta-analysis.
Table 2.
Characteristics and relevant measures and outcomes of eligible studies
| Reference, location | Sample size (yoga, controls) | Duration | Study population | Comparison group/ condition | Intervention | Clinical measures | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IR indices | Lipids | Body size/ comp | BP | Coagulation | Oxidative stress | SNS/PSN activity | Lung function | Other clinical outcomes | ||||||
| Studies targeting adults with Diabetes mellitus† | ||||||||||||||
| Uncontrolled clinical trials | ||||||||||||||
| (92), India | 52 | 6+ months, 45 min per day | Adults 17–70 years with uncomplicated DM for 3+ years (11 DM 1, 38 obese) | Ss own controls | Yoga (AS, SH); obese also on low cal diet | X+ | X+ | X+ | ||||||
| (93), India | 14 (7 DM; 7 normal) | 6 months 40 min per day | White collar men aged 25–63, white collar, 7/10 with hx of DM for 6 months to 11 years (3 drop out first 2 weeks; 6 DM 2, 1 DM 1 complete study); 7 non-DM | Ss own controls | Yoga (AS, SH, PR) | X+ | X+ | |||||||
| (109), India | 32 (5–8 per group) | 10–12 weeks, 45–60 min day | 27 men, 5 women with DM; avg 47.5 (M), 43 years (F); randomized to 5 different yoga routines | Ss own controls | Yoga training (AS, PR, SH) | X+ | ||||||||
| (65), India | 16 | 28 days | Adults with DM assigned to 1 of 3 yoga routines | Ss own controls | Yoga AS | X+ | ||||||||
| (91), India | 35 | Not stated | Adults with DM (31 DM 2, 4 DM 1) | Ss own controls | Yoga PR | X+ | X+ | |||||||
| (94), India | 9 (2 DM 1, 7 DM 2) | 5 weeks, 1 h 2× per day | 9 hospital pts 25–50 years (DM 5–10 years) naïve to yoga; 4 on insulin, others on oral drugs | Ss own controls | Resid. yoga training (AS, PR, KR, SH) +low cal, fat diet | X+ | X+ | X+ | X+ | |||||
| (95), India | 20 (10 DM, 10 normal) | 6 months | I. 10 non-DM men 30–35 years, 10 DM men 32–37 years, on oral meds and special diet. Analyses stratified by DM status | Ss own controls | Yoga training and practice (AS, SH/R) | X+ | ||||||||
| (96), India | 20 (10 DM, 10 normal) | 6 months | I. 10 non-DM men 34–37 years, 10 non-obese DM men 34–37 years, on oral meds and special diet. Separate analyses | Ss own controls | Yoga training and practice (AS, SH/R) | X+ | ||||||||
| (99), India | 149 | 40 days, 2.5 h per day | 149 outpatients with DM 2, avg 45.9 years, 22–23 BMI | Ss own controls | Residential (hosp-ital) yoga AS, KR, PR, SH+ veg diet | X+ | X+ | X+ | ||||||
| (100), India | 30 | 40 days | Hospitalized men with DM 2; 22 on oral drugs, mean 59.5 years, 17 years DM duration, 22.5 BMI | Ss own controls | Residential (hosp-ital) yoga AS, KR, PR, SH+ veg diet | X+ | X+ | X+ | ||||||
| (97), India | 19 | 40 days, 2.5 h per day | Non-smoking adults 30–60 years w/uncomplicated DM 2?, on drug and diet control | Ss own controls | Yoga (AS, PR, M) | X+ | X+ | |||||||
| (98), India | 24 | 40 days, 30–40 min per day | Adults 30–60 years old; with un-complicated DM 2 (0–10 years) | Ss own controls | Supervised yoga AS, SH, PR | X+ | ||||||||
| (83), India | 24 | 40 days | Adults 30–60 years with un-complicated DM 2 (1–10 years) on meds, diet | Ss own controls | Yoga (AS, SH): 13 poses in standard sequence | X+ | X+ | X+ | X+ | |||||
| Non-randomized controlled trials | ||||||||||||||
| (103), India | 20, 20 | 40 days | 30–60 years; DM 2 for 0–10 years; controls similar age, DM severity | Medication, light-moderate exercise | Supervised yoga AS, PR, SH+ medication, diet | X+ | ||||||||
| (102), India | 80 (20,20,20,20) | 3 months, 2× per day, 25–35 min | 60 patients from Indore diabetic clinics (intervention), 20 non-DM matched on age, sex; 40–70 years on vegetarian diet | No intervention (non-DM adults); Strict diet alone (20 DM adults) | (i) Yoga AS,SH only center(ii) Yoga +strict diet | X+ | X+ | X+ | ||||||
| Randomized controlled trials | ||||||||||||||
| (101), UK | 21 (11,10) | 12 weeks, 90 min 1–5× per week | Uncomplicated type 2 DM controlled with meds (n = 13; 8 Yoga group) or diet (n = 8); 45–67 years, avg 53 (Y), 57 (C) | Usual care (continue on medication, diet) | Yoga classes (PR, AS, SH) + usual care | X+ | X+ | |||||||
| (84), UK | 37* | 16 weeks | Poorly controlled insulin-treated DM (14 with DM 1) from Hospital DM clinic, avg 60–61 years | Education, simple exercise | Education, Hatha yoga classes | X+ | X+ | X- | X+ | |||||
| Studies including but not targeting adults with DM 2 | ||||||||||||||
| Uncontrolled clinical trials | ||||||||||||||
| (68), India | 20 | 78 sessions, 1 h per day | Adults with mild to moderate hypertension, 35–55 years. Include 4 Ss with DM (age 39–50 years) | Ss own controls | Yoga (AS, PR, M,SH) +education | X+ | X+ | X+ | X+ | X+ | ||||
| (88), India | 98 (20 with DM) | 8 days, 3–4 h per day with weekend off | 67 male, 31 female clinic out-patients aged 20–74 (avg 46) years with CV disorders, DM, obesity or other chronic condition | Ss own controls | Yoga (AS, SH, M, PR)+ education, advice, group support, stress management | X+ | X+ | |||||||
| Non-randomized controlled trials | ||||||||||||||
| (111), Germany | 154 (118,36)¥ | 3 months | Lifestyle program participants (58 men, 48 women 18–64 years); analyses incl. 36–72 Ss; Ss with DM included, N unknown | Non-participants matched on age, gender, specific risk factors | Residential program: Kriya yoga+ vegetarian diet | X+ | X+ | X+ | X+ | X+ | ||||
| (112), US | 333 (194,139), 62 with DM | 12 months, 72 4 h sessions | Adults with confirmed CAD, eligible for revascularization; 263 men, 70 women | Usual care | Usual care +Session: 1h each: stress management (incl Yoga AS, M); exercise, group support, meal | X+ | X+ | X+ | ||||||
| (106), US | 440 (91 with DM)**; 342 complete | 12 months | Adults with confirmed CAD, eligible for revascularization. 347 men, 93 women in intervention arm (68 women, 274 men complete); mean age 58 (men)-59 (F) y. 55 men, 36 women with DM at baseline | Usual care** | 1 h per day stress management: Yoga AS, R, M + low fat vegetarian diet, group support 2× per week, exercise 3+h per week+usual care | X+ | X+ | X+ | X+ | |||||
| (104), India | 113 (71,42) | 12 months, 21 sessions | Adults 30–70 years with confirmed CAD, incl. 33 with DM 2. 71/80 in yoga group, 42/60 controls complete study | Usual care: AHA diet, moderate exercise, medication (incl statins) | Yoga + medication (except statins), low fat diet, walking, stress management | X+ | X+ | X+ | X+ | |||||
| Randomized controlled trials | ||||||||||||||
| (90), USA | 43 (20,9,14) 15 high risk (6,3,6) | 12 months | Adults 65+ y, avg 74 years; complete reliable data for 43 of original 57 Ss; high risk group includes Ss with DM (N not stated) | (1) Usual care; (2) Usual care+ diet,exercise, education, supplements | Yoga M, AS + walking, diet | X+ | X+ | X+ | ||||||
| (79), India | 42 (21,21) (7,5 with DM 2) | 4 days training+ 1 year | Men with CAD & chronic stable angina, 32–72 years. Yoga and control groups similar in age, weight, lesion severity | Usual care:AHA diet, moderate exercise; regular evaluations | Yoga: (PR, AS, K, M)+ diet, exercise, regular evaluations | X+ | X+ | X+ | ||||||
Under each category, a plus indicates a beneficial change in at least one measure; a negative sign indicates no change in any of the measures in a specific category.
AHA, American Heart Association; AS, yoga asanas or postures; avg, average; BF, biofeedback; BP, blood pressure; CAD, coronary artery disease; cal, calorie; Clin, clinical; comp, composition; comp, composition; d, day, DM, Diabetes mellitus; F, female; h, hour; IR, insulin resistance (markers of); KR, kriyas or cleansing exercises; M, meditation; MBSR, mindfulness-based stress-reduction program; mo, month; PMR, progressive muscle relaxation; PR, pranayama or yogic breathing exercises; R, relaxation poses (non-specified); Resid, residential; SH, shavasana or corpse pose, a traditional yoga relaxation pose; SNS/PNS, markers of sympathetic/parasympathetic activation, including heart rate and catecholamine levels; Ss, subjects; veg, vegetarian; week, week; y, year.
†Excluding studies exclusively targeting Type 1 Diabetes mellitus.
*N's for each group not given.
**Data for intervention group only presented in this study; number with DM 2 completing study not stated, although drop-outs similar to completers in medical risk factors.
¥36–72 analyzed in matched analyses.
Results and Discussion
The literature search identified a total of 25 eligible studies investigating the influence of yoga-based interventions on physiologic/anthropometric indices of DM 2 and/or related clinical outcomes, including 15 uncontrolled clinical trials, 6 NRCTs and 4 RCTs (Table 1). Of these studies, 13 uncontrolled studies, 2 NRCTs, and 2 RCTs specifically targeted adults with DM. A majority (77%) of identified studies were published between 1990 and 2006, and most were small in size, with over 40% having study populations numbering under 25 subjects. Seventy-nine percent of total eligible studies, and almost 90% of those specifically investigating diabetic populations were conducted in India (Table 1). Yoga-based interventions used in these studies ranged in duration from 8 days to 12 months. Some studies evaluated the effects of single (n = 2) or multiple components of yoga practice (n = 12) alone, while others assessed comprehensive yoga-based programs that included a special diet, lifestyle education, non-yogic exercise, stress management or other interventions (n = 11) (Table 1). Table 2 lists the characteristics of eligible studies identified. The findings of these studies regarding the effects of yoga-based interventions on specific IRS-related physiologic and anthropometric indices and relevant clinical outcomes are reviewed below.
Table 1.
Characteristics of eligible studies investigating the effects of yoga-based programs in adults with Diabetes mellitus (DM)
| Uncontrolled clinical trial | Non-randomized controlled trial | Randomized controlled trial | Totals | |||||
|---|---|---|---|---|---|---|---|---|
| Yoga alone | Multiple interventions | Yoga alone | Multiple interventions | Yoga alone | Multiple interventions | n | % | |
| Target population: adults with DM | ||||||||
| DM 2 only | 3 | 2 | 1 | 1 | 7 | 41.2 | ||
| DM 1 and 2 | 2 | 2 | 1 | 5 | 29.4 | |||
| Unspecified DM | 4 | 1 | 1* | 5 | 29.4 | |||
| Total targeting DM | 9 | 4 | 1 | 1 | 2 | 17 | ||
| Sample size | ||||||||
| <25 | 7 | 1 | 1 | 9 | 52.9 | |||
| 25–40 | 2 | 2 | 1 | 1 | 6 | 35.3 | ||
| 41–60 | 0 | 0.0 | ||||||
| >60 | 1 | 1 | 1* | 2 | 11.8 | |||
| Location | ||||||||
| India | 9 | 2 | 1 | 1 | 13 | 76.5 | ||
| US | 0 | 0.0 | ||||||
| Europe | 2 | 2 | 11.8 | |||||
| Year published | ||||||||
| 2000–05 | 3 | 1 | 1 | 5 | 29.4 | |||
| 1990–99 | 1 | 2 | 1 | 1* | 1 | 5 | 29.4 | |
| 1980–89 | 5 | 1 | 6 | 35.3 | ||||
| 1970–79 | 1 | 1 | 5.9 | |||||
| 17 | ||||||||
| Target population: adults with CAD/hypertension and/or various chronic illnesses including | ||||||||
| DM 2 | 1 | 1 | 1 | 3 | 42.9 | |||
| Unspecified DM | 1 | 3 | 1 | 5 | 71.4 | |||
| DM N not stated | 1 | 1 | 2 | 28.6 | ||||
| Total | 2 | 4 | 2 | 8 | ||||
| Sample size | ||||||||
| <25 | 1 | 1 | 14.3 | |||||
| 25–40 | 0 | 0.0 | ||||||
| 41–60 | 2 | 2 | 28.6 | |||||
| >60 | 1 | 4 | 5 | 71.4 | ||||
| Location | ||||||||
| India | 2 | 1 | 1 | 4 | 57.1 | |||
| US | 2 | 1 | 3 | 42.9 | ||||
| Europe | 1 | 1 | 14.3 | |||||
| Year published | ||||||||
| 2000–05 | 2 | 2 | 2 | 6 | 85.7 | |||
| 1990–99 | 2 | 2 | 28.6 | |||||
| 1980–89 | 0 | 0.0 | ||||||
| 1970–79 | 0 | 0.0 | ||||||
| Sample size | ||||||||
| <25 | 7 | 2 | 0 | 0 | 1 | 0 | 10 | 41.7 |
| 25–40 | 2 | 2 | 0 | 1 | 1 | 0 | 6 | 25.0 |
| 41–60 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 8.3 |
| >60 | 0 | 2 | 1 | 4 | 0 | 0 | 7 | 29.2 |
| Location | ||||||||
| India | 9 | 6 | 1 | 2 | 0 | 1 | 19 | 79.2 |
| US | 0 | 0 | 0 | 2 | 0 | 1 | 3 | 12.5 |
| Europe | 0 | 0 | 0 | 1 | 2 | 0 | 3 | 12.5 |
| Year published | ||||||||
| 2000–05 | 3 | 2 | 0 | 3 | 1 | 2 | 11 | 45.8 |
| 1990–99 | 1 | 2 | 1 | 2 | 1 | 0 | 7 | 29.2 |
| 1980–89 | 5 | 1 | 0 | 0 | 0 | 0 | 6 | 25.0 |
| 1970–79 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 4.2 |
| Totals | 9 | 6 | 1 | 5 | 2 | 2 | 25 | |
CAD, coronary artery disease; DM 1, Type 1 Diabetes mellitus; DM 2, Type 2 Diabetes mellitus.
*Two yoga-based interventions tested within same study (100).
Influence of Yoga on Core Indices of the IRS
Twenty-five eligible published studies from four countries have investigated the potential influence of yoga and yoga-based programs on one or more core indices of the IRS, including measures of insulin resistance and glucose metabolism, lipid profiles, body weight and composition, and blood pressure. Of these studies, 20 examined the influence of yoga-based interventions on clinical markers of insulin resistance (including 14 uncontrolled clinical trials, 3 NRCTs and 3 RCTs), 12 evaluated the influence of yoga on blood lipid profiles (including 4 uncontrolled clinical trials, 5 NRCTs and 3 RCTs), and 10 assessed the influence of yoga on body weight or composition (including 4 uncontrolled trials, 5 NRCTs and 1 RCT). In addition, we identified six eligible studies evaluating the effects of yoga on blood pressure, including three uncontrolled analyses, two non-randomized controlled studies and one RCT. Findings of these are summarized in Tables 2–4 and are discussed briefly below.
Table 3.
Summarized findings of studies (1970–2006) investigating the effects of yoga-based programs on insulin resistance, lipid profiles, and body size and composition, and blood pressure, stratified by study design and intervention (yoga alone versus in combination with other interventions)
| Findings, by clinical measure | Study design | |||||
|---|---|---|---|---|---|---|
| Uncontrolled clinical trials | Non-randomized controlled clinical trials | Randomized clinical trials | ||||
| Yoga alone | Multiple interventions | Yoga alone | Multiple interventions | Yoga alone | Multiple interventions | |
| Measures of insulin resistance | ||||||
| Fasting glucose | ||||||
| Reduced | (65,83,91,95–98) | (68,88,94, 99,100) | (102)* | (103,104)† | (101) | |
| No change | (90)* | |||||
| Post-prandial glucose | ||||||
| Reduced | (65,83,91–93,95–98) | (94,99) | ||||
| No change | (90) | |||||
| Reduced fructosamine | (102) | |||||
| Reduced fasting insulin | (90) (NS) | |||||
| Reduced OGT maximum/AIT | (99,100) | |||||
| Fasting glycated hemoglobin | ||||||
| Reduced | (83,97,98) | (100) | (101) (84) (NS) | |||
| No change | (90) | |||||
| Blood lipid profiles | ||||||
| Total cholesterol | ||||||
| Reduced | (109) | (68,88,100) | (102) | (104,106,111,112) | (84) | (79) (90) (NS) |
| Unchanged | ||||||
| Triglycerides | ||||||
| Reduced | (109) | (88,100) | (79) (90) (NS) | |||
| Unchanged | (106,112) | (84) | ||||
| Low density lipoprotein (LDL) | ||||||
| Reduced | (109) | (88) | (104,106,111,112) | (84) | (79) (90) (NS) | |
| High density lipoprotein (HDL) | ||||||
| Increased | (109) | (68,88) | (84) | |||
| Unchanged | (106,112) | (79,90) | ||||
| Reduced very LDL | (109) | (88) | ||||
| Reduced cholesterol/HDL ratio | (84) | |||||
| Reduced LDL/HDL ratio | (88) | (79) | ||||
| Anthropometric measures | ||||||
| BMI | ||||||
| Reduced | (111) | |||||
| Unchanged | (99,100)¥ | |||||
| Body weight | ||||||
| Reduced | (92,93) | (102)+ | (104)¶ (106) ¶¶(112) | (79) | ||
| Unchanged | (99,100)¥ | |||||
| Body composition | ||||||
| Reduced waist, hip circumference/ratio | (100) | |||||
| ↓% body fat, ↑% lean mass | (112) | |||||
| Blood Pressure | ||||||
| Reduced systolic and/ or diastolic pressure | (83) | (68,94) | (106)¶¶ | (90) | ||
| No change in systolic or diastolic pressure | (84) | |||||
| Systolic blood pressure | ||||||
| Reduced | (83) | (68,94) | (106)¶¶ | (90)†† | ||
| Unchanged | (84) | |||||
| Diastolic blood pressure | ||||||
| Reduced | (83) | (68,94) | (106)¶¶ | (90) | ||
| Unchanged | (84) | |||||
Studies demonstrating beneficial effects are in boldface.
*Described only as reduced plasma glucose.
+No statistics given; reduction greater than that with diet alone but similar to yoga + diet.
†In Ss with DM 2 (n = 33) ¥Baseline BMI average 22–23.
¶In overweight Ss.
¶¶Data presented only for intervention group.
†† p = 0.08 (n = 6 in yoga-based intervention).
Table 4.
Observed percent change with yoga in selected metabolic and anthropometric measures among adults with diabetes and/or other chronic disorders*
| Findings, by clinical measure and study population | Uncontrolled clinical trials | Non-randomized controlled clinical trials | Randomized clinical trials |
|---|---|---|---|
| Measures of insulin resistance | |||
| Reduced fasting glucose | |||
| Adults with diabetes/hyperglycemia | 9.1–33.4% (83,88,91,94–100) | 23.4–34.4% (102) | 6.9% (101)†† |
| Adults with hypertension/CVD or other chronic condition** | 6.1–6.2% (68,88) | ||
| Reduced post-prandial glucose | |||
| Adults with diabetes | 23.9–32.8% (65,83,92–94,97) | ||
| Reduced glucose (tolerance test) | |||
| Adults with diabetes | |||
| 1 h post-load | 10.1–32% (94–96) | ||
| 2 h post-load | 15.8–19.2% (94–96) | ||
| Area under the curve (AUC) | 16.5–29.5% (99,100) | ||
| Reduced fasting insulin | |||
| Adults at risk for CVD | 19.2% (90) | ||
| Reduced fasting glycated hemoglobin | |||
| Adults with diabetes | 13.3–27.3% (83,97,98,100) | 3.3–15.5% (84,101) | |
| Blood lipid profiles | |||
| Reduced total cholesterol | |||
| Adults with diabetes | 5.9–7.2% (100,109) | 8.3–19.9% (102) | |
| Adults with hypertension/CVD or other chronic condition** | 5.7†-7.5% (68,88) | 8.7–25.2% (104,106,112) | 5.8–21% (79,90) |
| Reduced triglycerides | |||
| Adults with diabetes | 8.9–11.9% (100,109) | ||
| Adults with/at risk for hypertension/CVD or other chronic condition** | 8.0%-12.4† (68,88) | 8.3% (111) | 14.1–23.7% (79,90) |
| Reduced low density lipoprotein (LDL) | |||
| Adults with diabetes | 7.5% (109) | ||
| Adults with hypertension/CVD or other chronic condition** | 5.1%† (88) | 13.7–26.0% (104,106,111,112) | 6.8–24.4% (79,90) |
| Reduced very LDL (VLDL) | |||
| Adults with diabetes | 14.5% (109) | ||
| Adults with DM, HT, or other chronic condition** | 17.7%† (88) | ||
| Increased high density lipoprotein | |||
| Adults with diabetes | 4.2% (109) | ||
| Adults with/at risk for hypertension/CVD or other chronic condition** | 3.5†-5.7% (68,88) | 33.3% (111) | |
| Anthropometric markers | |||
| Reduced body weight | |||
| Adults with diabetes | 8.2% (93) | 3.5% (102) | |
| Adults with hypertension/CVD** | 3.4–5.0% (106,112) | 7.8% (79) | |
| Blood pressure | |||
| Reduced diastolic BP | |||
| Adults with diabetes | 6.7–12.9% (83,94) | ||
| Adults with or at risk for CVD** | 15.8% (68) | 5.8% (106) | 9.3% (90) |
| Reduced systolic BP | |||
| Adults with diabetes | 11.1–11.3% (83,94) | ||
| Adults with or at risk for CVD** | 13.9% (68) | 3.9% (106) | 4.4% (90) |
| Reduced baseline heart rate | |||
| Adults with diabetes | 10.2% (83) | ||
| Adults with hypertension/CVD** | 5.7% (106) |
CVD, Cardiovascular disease
*Including studies reporting improvement in these indices; studies not reporting point estimates or presenting insufficient data to allow reliable calculation of point estimates were excluded.
**Including adults with diabetes mellitus †Ss with cholesterol ≥200 mg dl−1 (n = 43) (88).
††18.9% mean difference relative to controls (101).
Markers of Insulin Resistance
Of the 20 eligible studies evaluating the effects of yoga on markers of insulin resistance, all but one documented significant, post-intervention improvement in one or more clinical measures following the practice of yoga either alone or in combination with other therapies (Tables 3 and 4). Interventions ranged in length from 8 days (88) to 12 months (89,90), and all but one (91) incorporated yoga asanas or poses. All 14 uncontrolled studies targeting adults with DM 2 (65,83,91–101), hypertension (68) and/or other chronic conditions (88) reported significant improvement post-intervention in indices of insulin resistance relative to baseline values. Documented changes included reductions in fasting (65,68,83,88,91,94–100) and post-prandial glucose (65,83,91–99), and in fasting glycated hemoglobin (83,97,98,100) (Table 2). Likewise, non-randomized controlled studies of adults with diabetes (102,103) or confirmed coronary artery disease (CAD) (89) reported reductions in fasting glucose (89,102,103) and fructosamine (102) among subjects receiving a yoga-based intervention versus controls receiving enhanced usual care (89), a low fat vegetarian diet alone (102) or a light to moderate exercise program that included walking (103). In a small RCT of British adults with DM 2, Monro et al. (101) demonstrated significant declines in both fasting glucose and glycated hemoglobin (HbA1c) among participants attending structured yoga classes relative to usual care controls. In a second RCT of 37 adults with poorly controlled DM, of whom 14 had type 1 diabetes, those attending biweekly yoga classes for 16 weeks demonstrated similar, but non-significant declines in HbA1c (84). In contrast, in a small RCT of American seniors, a subanalysis of those at risk for CVD did not demonstrate significant reductions in HbA1c, fasting glucose or fasting insulin in those completing a comprehensive integrative medicine program relative to controls receiving usual care or an active exercise and diet intervention. However, sample sizes in this analysis of seniors were very small (n = 6, 3 and 3, respectively) (90). Overall, yoga practice was associated with a 6.1–34.4% reduction in fasting glucose, 23.9–32.8% reductions in post-prandial glucose and 10.5–27.3% reduction in HbA1c, with the percentages varying by study population and design (Table 4).
While the evidence for a beneficial effect of yoga on indices of insulin resistance appears generally consistent across studies, most studies (60%) had no comparison groups (65,68,83,88,91–100), and many had small sample sizes (65,68,83,84,93–98,101) or reduced power due to stratified analyses (65,90,99,102). Others lacked detailed information on eligibility criteria or study population characteristics (65,83,92,95–98,100,102–104), including type of diabetes (90,95,96,105–107). Blinding of the outcome assessment was reported in only one (90). The study sample selection process was unclear in several studies (83,93,95–98,100,102,103), and in others, potential selection bias (93,97), loss to follow-up (89,93–96) and uncontrolled confounding factors such as demographic, anthropometric and lifestyle characteristics (65,83,88,91,92,95–97,99,100) may have been influential. The intervention was not well-described (65,91,93,95) or appeared to vary in duration or intensity (91–94,101) in some studies; others included multiple interventions (68,79,88–90,94,99,100,103,105), rendering detection of the effect of a specific component difficult. Most studies did not adequately detail the analytic methods used (68,92,97–99,101,103,108), some presented no statistical analysis for some or all of the outcome measures (68,91,92,99,103), and many appeared to suffer other methodological deficiencies, including lack of adequate point estimates for key outcome measures (68,88,92,94,103,104), failure to adjust for multiple comparisons (68,83,84,88,90–92,94,97,98,100,102), confusing data presentation (65,68,91) and other potential analytic problems (65,90,95). Among the controlled studies, additional limitations included lack of randomization (89,102,103), failure to describe treatment allocation methods (89) or adjust for differing baseline characteristics (79,102) and/or absence of intergroup comparisons (103,107).
Blood Lipid Profiles
Of the 12 identified studies that assessed the potential effects of yoga on blood lipid concentrations, all suggested that the practice of yoga and yoga-based programs may improve lipid profiles (Table 3). Four uncontrolled studies targeting adults with diabetes (100,109) and/or other chronic conditions (68,88), demonstrated significant positive changes in blood lipid levels following yoga-based interventions that ranged from 8 days (109) to 3 months (109) in duration. Observed improvements in blood lipid fractions included reductions in cholesterol (68,88,100,109), triglycerides (88,100,109), low-density lipoprotein (LDL) (88,109), and very LDL levels (88,109), increases in high density lipoprotein (HDL) levels (68,109), and reduced LDL/HDL ratio (88) relative to baseline levels and/or control values (89,110,111). Similarly, five controlled, non-randomized studies (102,104,106,112,113) and two RCTs (79,84) investigating the effects of yoga alone (102) or in combination with diet (79,102,106,112,113), education (84), stress management (89,106,113) and other therapies (79,89,106,113) demonstrated significant improvement in lipid profiles relative to controls receiving enhanced usual care, exercise and/or dietary interventions (Tables 2 and 3). Although findings varied among studies, all documented significant changes in at least two measures of dyslipidemia. The most consistently and frequently reported improvements included reductions in total cholesterol and LDL (Table 3). Data from a third RCT of American seniors at risk for CVD also suggested improvement in several lipid indices following a yoga-based intervention. However, changes did not reach statistical significance, likely due to small sample sizes (n = 6 in the yoga-based intervention group) (90).
Controlled studies ranged in length from 3 (102,112) to 12 months (79,104,106,113) and included investigations of both diabetic (84,100,102,109) and other at risk populations (68,79,88,90,104,106,112,113). Among those studies demonstrating significant changes in specific lipid indices, completion of yoga-based interventions were associated with a 5.7–25.2% decrease in total cholesterol, 8.0–23.7% reduction in triglycerides, a 5.1–26.0% reduction in LDL, a 14.5–17.7% decrease in VLDL and a 4.2–33.3% increase in HDL, with the observed magnitude of the effects differing by population and design (Table 5).
Table 5.
Clinical trials investigating the effects of yoga and yoga-based programs on specific clinical outcomes, stratified by study design and intervention (yoga, including yoga-based meditation, alone versus in combination with other interventions)
| Findings, by outcome | Study design | |||||
|---|---|---|---|---|---|---|
| Uncontrolled clinical trials | Non-randomized controlled trials | Randomized controlled trials | ||||
| Yoga alone | Multiple interventions | Yoga alone | Multiple interventions | Yoga alone | Multiple interventions | |
| Clinical outcomes | ||||||
| Reduced need for medication | ||||||
| Hypertension/CAD | (68) | (104) | ||||
| Diabetes | (65,83,92,93) | (99) (68) | (84,101) | |||
| Studies targeting adults with CVD | ||||||
| Reduced revascularization procedures related complications | (112) | (79) | ||||
| Reduction in anginal episodes | (112) | (79) | ||||
| Reduced carotid intimal media thickness | (90) | |||||
| Reduced progression of CAD | (104) | (79) | ||||
| Increased regression of CAD | (104) | (79) | ||||
| Reduced number of serious coronary events | (112) | |||||
| Reduced number of hospitalizations | (104) | |||||
Studies reporting beneficial effects are in boldface. CAD, coronary artery disease; CVD, cardiovascular disease.
Again, published data from both uncontrolled and controlled studies suggest that the practice of yoga may have a positive influence on blood lipid profiles. However, most of the studies have methodological or other limitations that hinder interpretation of findings. These include absence of comparison groups or conditions (68,88,100,109), low power due to small sample sizes (68), stratified analyses (68,90,102,109,112) or other factors (84), lack of evidence for blinded outcome assessment [all but one study (90)], potential selection bias (88,111,113), differential loss to follow-up (89,106), lack of randomization (102,104,106,112,113) or information on the randomization process (79), multiple interventions (68,79,88–90,100,105), inadequate description of populations (89,102) or of the sampling or treatment allocation process (89). Other methodological concerns include unclear statistical analyses (68,109,111), possible uncontrolled confounding factors (88,100,109,111) and lack of adequate point estimates (68,88,104,111), intergroup comparisons (106,107) or adjustment for multiple comparisons (68,84,88,90,100,102,109,111).
Anthropometric Measures
Ten published clinical trials in four countries examined the effects of yoga on anthropometric indices of CVD risk in populations that included adults with Type 2 diabetes (Table 3). All utilized interventions incorporating active yoga asanas. Three of the four uncontrolled clinical trials (92,93,100) and all five non-randomized controlled studies identified reported declines in body weight (102,104,106,112,113), reductions in waist/hip ratio (100), and/or improvements in body composition (113) following yoga-based interventions ranging from 40 days (100) to 12 months (104,106,113). Similarly, a 12 month RCT in Indian men with CAD (79) demonstrated improvement in body weight relative to usual care (79). Results reporting improvement in anthropometric characteristics included investigations targeting adults with diabetes (92,93,100,102), as well as those with CAD (79,104,106,113) and/or other chronic conditions (112). Of these, completion of yoga-based programs was associated with a 3.5–8.2% reduction in body weight (Table 4). Only two studies reported no change in body weight (99,100), likely in part reflecting the participants' low BMI values at baseline.
Limitations include lack of control groups (92,93,99,100), reduced power due to low number of subjects (93) or other factors (102,112), possible selection bias (79,93,102,105,111), uncontrolled confounding (92,99,100,111) or floor effects (99,100), lack of appropriate statistical analyses or presentation (92,99,104,111), multiple comparisons (92,102,111), inadequate description of analytic methods (92,93,99,111), population (92,93,100,102), intervention (93), treatment allocation (89), or sample selection process (93,100,102,112), loss to follow-up (89,93) and multiple interventions (79,89,99,100,105). Among controlled studies, additional limitations included failure to compare control and intervention groups (106,107) and lack of randomization (102,104,112,113) or description of randomization methods (79). Blinded outcome assessment was not detailed in any of the 10 studies.
Blood Pressure
We identified seven eligible studies that assessed the effects of yoga-based interventions on blood pressure. Six of these studies reported significant improvement in both systolic and diastolic blood pressure as compared to baseline values (68,83,94,106,112), or to controls receiving enhanced usual care (90). One study, a small British RCT of poorly controlled insulin-treated diabetic adults, showed no change in blood pressure despite significant improvement in other indices of CVD risk (Table 3) (84). Research reporting positive results included three uncontrolled trials targeting Indian adults with diabetes (83,94) or hypertension (68), one NRCT in US adults with CAD (106), one NRCT of German community-dwelling adults (112) and one RCT in US seniors (90). Interventions ranged from 40 days (83) to 1 year (90,106) in duration, and all incorporated active asanas. Reductions in systolic and diastolic blood pressures varied from 3.9 to 13.9% and 5.8 to 15.8%, respectively, depending on design and population (Table 4).
However, the potential biases and limitations characterizing most of these studies again hinder interpretation of findings. These include absence of comparison groups (68,83,94), small sample sizes (68,83,94), reduced power due to stratified analyses (68,90) or other factors (84), possible selection bias or confounding by lifestyle or other factors (83,94), absence of detailed information regarding the population (83), statistical methods (68,83,94,111) or subject selection process (83,112), potential uncontrolled variation in exposure to the intervention (94) or loss to follow-up (94). Only one reported blinding of outcome assessment (90), and most studies used yoga in combination with other interventions (68,89,90,106,112), making it difficult to isolate an effect specific to yoga. Other methodological limitations are lack of randomization (106,111) and inadequacies in statistical analyses or presentation, including lack of appropriate point estimates (68,94,111), adjustment for multiple comparisons (68,83,84,90,94,111) and appropriate comparisons between (106) or within (68) groups.
Influence of Yoga on Other Indices
Eligible data suggest that yoga-based interventions may also have beneficial effects on coagulation profiles and oxidative stress, sympathetic activation and lung function in adults with DM 2, although investigations including diabetic populations are few. For example, recent uncontrolled trials targeting Indian adults with uncomplicated diabetes mellitus (97) or hypertension (68) reported significant reductions in malonyldialdehyde (MDA), an estimate of lipid oxidative damage, following a 40 day yoga training course (97) and a 12 week yoga lifestyle intervention (68). These findings suggest a decrease in oxidative damage with yoga. Data from a non-randomized controlled study of German adults (including an unspecified number with diabetes) suggest that yoga may also improve coagulation profiles. Compared to relative to community controls matched on age, gender and baseline fibrinogen levels, participants who completed a 3 month residential Kriya yoga program showed a significant decline in fibrinogen among participants (n = 76 subjects, including 38 controls) (111). These findings are consistent with those of uncontrolled (114–116) and controlled studies (117,118) in healthy adults (114–116,118) and in adults with other related chronic disorders (115,117). Recently, reviewed by Innes et al. (82), these reports showed significant improvement in measures of oxidative damage (115–118) and coagulopathy (114) following yoga-based interventions ranging from 10 weeks (118) to 5 months (116). Procoagulant changes and damage due to oxidative stress are thought to mediate many of the atherosclerotic and thrombotic changes associated with IRS (119–123) and to play a central role in the pathogenesis and progression of diabetes (18) and CVD (119–121,123).
Although many investigations have examined the effect of yoga on markers of sympathetic/parasympathetic activation and cardiovagal function (82), our search identified only four that included adults with diabetes, including two uncontrolled studies (68,83) and two NRCTs (106,112); only one of them specifically targeted patients with DM 2 (83) (Table 2). Relative to baseline (68,83,106) or to controls receiving no intervention (112), participants who completed a yoga program showed significant reductions in heart rate (83,106) and catecholamine levels (68,112). In agreement with these findings, results from over 35 in other populations, including healthy and hypertensive adults, suggest that yoga promotes a reduction in sympathetic activation, enhancement of cardio vagal function and a shift in autonomic nervous system balance from primarily sympathetic to parasympathetic (82). Documented changes have included significant reductions in respiratory and heart rate, in cortisol concentrations, catecholamine levels, and renin activity, in skin conductance, and in cardiovascular response to stress, as well as significant increases in heart rate variability and baroreflex sensitivity (82).
Impaired lung function is both an important complication (23,24) and a significant predictor (25) of type 2 diabetes, and has been inversely associated with insulin resistance (23) and glycemic exposure (24,124). Recent research in adults with DM 2 suggests that yoga may improve pulmonary function in this population (98). In an uncontrolled (pre–post) study of 24 Indian adults with an established diagnosis of DM 2, participants demonstrated significant increases in forced expiratory volume, forced vital capacity, peak expiratory flow rate and maximum voluntary ventilation following completion of a 40 day yoga program (98). Other research using healthy adults have yielded similar findings (125–129), although only one of them included controls (128).
While limited, available data support a possible beneficial influence of yoga on oxidative stress and coagulation profiles, sympathetic activation and pulmonary function in adults with DM 2. Limitations of existing research include lack of appropriate comparison groups (68,97,98,106), small sample sizes (68,97,98), possible selection bias or uncontrolled confounding by lifestyle and other factors (97,111), lack of randomization (111), inadequate information regarding the population (97,98), subject selection (97,98,112), or analytic methods (68,97,98,111), multiple interventions (68,101,111), and problems with data analysis or presentation (68,97,98,111). In addition, blinding of outcome assessment was not well-reported in any identified studies.
Influence of Yoga on Clinical Outcomes
Several studies in Indian (68,79,89,92,99), European (84,101) and American populations (90) have suggested that yoga may also improve specific clinical outcomes in patients with type 2 diabetes and other IRS-related chronic conditions. Twelve eligible studies evaluated the influence of yoga and yoga-based interventions on medication use and cardiovascular outcomes, including six uncontrolled trials, two non-randomized controlled studies and four RCTs (Table 5). In uncontrolled studies of Indian adults with hypertension (68) and/or diabetes (65,68,83,92,93,99), completion of a simple (65,83,92,93) or comprehensive yoga program (68,99) was associated with a reduced need for medication relative to baseline. In agreement with these findings, controlled studies of adults with diabetes (84,101) and/or CAD (89) showed a decline in medication requirements among those enrolled in a yoga-based intervention compared to controls receiving usual care (101), usual care plus intensive education and exercise (84), or usual care plus a diet and exercise program (89). Controlled studies in Indian (79) and American (90,113) populations also suggest that yoga may help reduce complications and improve the prognosis of those with frank or underlying disease. For example, in an RCT of Indian men with CAD, those enrolled in a 12 month comprehensive yoga program showed retardation of coronary atherosclerosis, increased regression and reduced progression of vascular lesions, and reduced anginal episodes relative to usual care controls (79). Two other non-randomized controlled studies of CAD patients in India (89) and the United States (113) yielded similar results (Table 5). In an RCT in American seniors, participants completing a 12 month comprehensive yoga-based program demonstrated a decline in carotid intimal media thickness, an indicator of carotid atherosclerosis, relative to those receiving usual care or a comprehensive medical, diet and exercise intervention (90). The reduction was inversely correlated with adherence to the yoga program, suggesting a direct relation between practice of this program and atherosclerotic change.
Although promising, several of these studies have methodological and other limitations, including absence of control groups (65,68,83,92,93,99), small sample sizes (65,68,93,101), lack of randomization (89,113), loss of participants at follow-up (89), possible uncontrolled confounding factors (92,99,101), unclear statistical analyses (65,68,83,92) or absence of intergroup comparisons (101), lack of adjustment for multiple comparisons (68,90,92) and multiple interventions (68,79,83,89,90,99,101,113). Several lacked adequate descriptions of the study population (83,89,92,93), sample selection process (83,93), intervention (65,93,101), treatment allocation (89) or statistical methods (68,92,99,101). Only one study presented information of blinding with outcome assessment (90). In addition, reporting bias may have resulted in omission of negative findings, possibly inflating the apparent positive effect of yoga on clinical outcomes.
Yoga, Psychosocial Risk Factors for Diabetes and CVD, and Possible Underlying Mechanisms
While methodological and other limitations preclude drawing firm conclusions, the published research reviewed above nonetheless offer evidence that yoga may improve risk profiles and clinical outcomes in adults with type 2 diabetes. In addition, although studies that specifically target diabetic populations are lacking, investigations in healthy adults (66,130–134) and in other chronically ill populations (135–142) suggest that yoga therapy may reduce psychosocial risk factors for the development and progression of diabetes as well. Yoga has been reported to decrease perceived stress (134,143,144) and reactivity to stressors (133), enhance stress-related coping (137,138), reduce symptoms of depression (130,132,136,140,142,145) and anxiety (66,88,130,132,135,137,138,141), decrease anger, tension and fatigue (130,135), enhance psychological well-being (66,68,88,94,130–133,137,138), and reduce sleep disturbance (134,139).
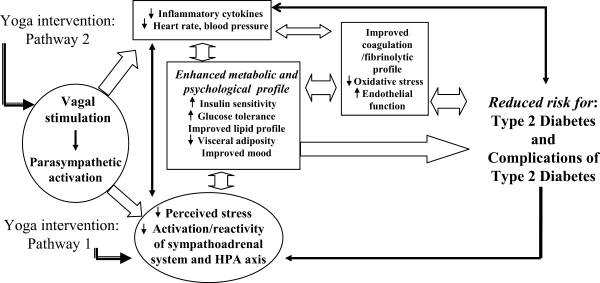
Mechanisms underlying the beneficial effects of yoga practice on diabetes-related risk profiles are not yet well understood. However, the observed changes may occur via at least two major pathways. First, by reducing the activation and reactivity of the sympathoadrenal system and the hypothalamic pituitary adrenal (HPA) axis and promoting feelings of well-being, yoga may alleviate the effects of stress and foster multiple positive downstream effects on neuroendocrine status, metabolic function and related systemic inflammatory responses (Fig. 1, Pathway 1) (74,146,147). Second, by directly stimulating the vagus nerve, yoga may enhance parasympathetic activity and lead to positive changes in cardiovagal function, in mood and energy state, and in related neuroendocrine, metabolic and inflammatory responses (Fig. 1, Pathway 2) (74,146,147). In addition, yoga may both indirectly (by encouraging healthy lifestyle changes) and directly lead to weight loss and reduced visceral adiposity. Weight loss itself lowers risk for DM 2 and CVD complications (148,149).
Figure 1.
Hypothesized pathways by which yoga intervention may reduce risk for Type 2 Diabetes mellitus (DM 2) and for complications related to DM 2.
In addition to physiologic improvements, yoga may provide a positive source of social support, a factor strongly associated with reduced risk for CVD (34,58), and may aid in improving health-related attitudes and lifestyle choices, in part by enhancing psychological well-being (34), and in this way also play an important role in diabetes management and prevention of cardiovascular complications (34).
Summary and Conclusions
In summary, a growing number of studies suggest that yoga may improve indices of risk in adults with type 2 diabetes, including glucose tolerance and insulin sensitivity, lipid profiles, anthropometric characteristics and blood pressure. Limited data also indicate that yoga may reduce oxidative damage, improve coagulation profiles and pulmonary function, and decrease sympathetic activation in adults with diabetes and related chronic disorders. Yoga may also be useful in reducing medication requirements in patients with diabetes and could help prevent and manage cardiovascular complications in this population.
However, despite the apparent therapeutic promise of yoga for diabetes management, rigorous, systematic studies regarding the effects of yoga on physiological, anthropometric and psychological profiles in adults with diabetes are few, and those in western populations are even fewer. Over 85% of published clinical trials (1970–2006) investigating the therapeutic applications and psychophysiological effects of yoga practice in diabetic populations have been conducted in India, where yoga forms a central part of long-standing spiritual and cultural traditions. Interpretation of existing studies is limited by small sample sizes, selection bias, lack of appropriate control groups, failure to adjust for baseline anthropometric characteristics, lifestyle factors, and other potential confounders, exposure to multiple interventions, and other methodological limitations. In addition, considerable variation in design, duration, intensity and delivery methods of yoga-based interventions renders comparison across studies problematic. Publication bias may also contribute to the selective reporting of positive results (150), particularly in non-Western countries, where yoga is more widely accepted and more likely to be incorporated into medical care. While existing RCTs have produced results consistent overall with those of non-randomized and uncontrolled studies, suggesting that the positive findings of these latter studies do not simply reflect poor study design, clearly, additional high-quality RCTs are warranted. Specifically, rigorous studies are needed to clarify the effects of specific yoga therapies on measures of DM 2 risk and related clinical outcomes, especially in American and other Western populations that remain underrepresented in existing research.
Acknowledgments
This work was made possible in part by the University of Virginia Institute on Aging and the National Center for Complementary and Alternative Medicine (NCCAM, Grant numbers R21AT002982 and S-T32-AT00052). The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the University of Virginia, NCCAM or the National Institutes of Health.
REFERENCES
- 1.Rizvi AA. Type 2 diabetes: epidemiologic trends, evolving pathogenetic [corrected] concepts, and recent changes in therapeutic approach. [see comment] [erratum appears in South Med J 2005;98:4] South Med J. 2004;97:1079–87. doi: 10.1097/01.smj.0000125108.06314.25. [DOI] [PubMed] [Google Scholar]
- 2.National Center for Chronic Disease Prevention and Health Promotion. National Diabetes Fact Sheet (2002). Centers for Disease Control. Available at: http://www.cdc.gov/diabetes/pubs/estimates.htm. [Google Scholar]
- 3.Douaihy K. Prediabetes & atherosclerosis: what's the connection? Nurse Pract. 2005;30:24–35. doi: 10.1097/00006205-200506000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Posner B, Franz M, Quatromoni P. Nutrition and the global risk for chronic diseases: the INTERHEALTH Nutrition Initiative. Nutr Rev. 1994;52:210–07. doi: 10.1111/j.1753-4887.1994.tb01421.x. [DOI] [PubMed] [Google Scholar]
- 5.Correa-Rotter R, Naicker S, Katz IJ, Agarwal SK, Herrera Valdes R, Kaseje D, et al. Demographic and epidemiologic transition in the developing world: role of albuminuria in the early diagnosis and prevention of renal and cardiovascular disease. Kidney Int Suppl. 2004;92:S32–7. doi: 10.1111/j.1523-1755.2004.09208.x. [DOI] [PubMed] [Google Scholar]
- 6.Lerman-Garber I, Villa AR, Caballero E. Diabetes and cardiovascular disease. Is there a true Hispanic paradox? Rev Invest Clin. 2004;56:282–96. [PubMed] [Google Scholar]
- 7.American Diabetes Association. American Diabetes Association: clinical practice recommendations. Diabetes Care. 2004;27:S1–9. [Google Scholar]
- 8.Cosentino F, Assenza GE. Diabetes and inflammation. Herz. 2004;29:749–59. doi: 10.1007/s00059-004-2635-8. [DOI] [PubMed] [Google Scholar]
- 9.Caglayan E, Blaschke F, Takata Y, Hsueh WA. Metabolic syndrome-interdependence of the cardiovascular and metabolic pathways. Curr Opin Pharmacol. 2005;5:135–42. doi: 10.1016/j.coph.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Rennert NJ, Charney P. Preventing cardiovascular disease in diabetes and glucose intolerance: evidence and implications for care. Prim Care. 2003;30:569–92. doi: 10.1016/s0095-4543(03)00035-6. [DOI] [PubMed] [Google Scholar]
- 11.McVeigh GE, Cohn JN. Endothelial dysfunction and the metabolic syndrome. Curr Diab Rep. 2003;3:87–92. doi: 10.1007/s11892-003-0059-0. [DOI] [PubMed] [Google Scholar]
- 12.Grundy S. Hypertriglyceridemia, insulin resistance, and the metabolic syndrome. Am J Cardiol. 1999;83:25F–9F. doi: 10.1016/s0002-9149(99)00211-8. [DOI] [PubMed] [Google Scholar]
- 13.Ginsberg H. Insulin resistance and cardiovascular disease. J Clin Invest. 2000;106:453–8. doi: 10.1172/JCI10762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Isomaa B. A major health hazard: the metabolic syndrome. Life Sci. 2003;73:2395–11. doi: 10.1016/s0024-3205(03)00646-5. [DOI] [PubMed] [Google Scholar]
- 15.Watkins LO. Epidemiology and burden of cardiovascular disease. Clin Cardiol. 2004;;27 doi: 10.1002/clc.4960271503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reilly M, Rader D. The metabolic syndrome: more than the sum of its parts? Circulation. 2003;108:1546–51. doi: 10.1161/01.CIR.0000088846.10655.E0. [DOI] [PubMed] [Google Scholar]
- 17.Reaven G, Abbasi F, McLaughlin T. Obesity, insulin resistance, and cardiovascular disease. Recent Prog Horm Res. 2004;59:207–23. doi: 10.1210/rp.59.1.207. [DOI] [PubMed] [Google Scholar]
- 18.Maritim A, Sanders R, Watkins Diabetes, oxidative stress, and antioxidants: a review. J Biochem Mol Toxicol. 2003;17:24–38. doi: 10.1002/jbt.10058. [DOI] [PubMed] [Google Scholar]
- 19.Wellen KE, Hotamisligil GS. Inflammation, stress, and diabetes. J Clin Invest. 2005;115:1111–9. doi: 10.1172/JCI25102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schiekofer S, Balletshofer B, Andrassy M, Bierhaus A, Nawroth PP. Endothelial dysfunction in diabetes mellitus. Semin Thromb Hemost. 2000;26:503–11. doi: 10.1055/s-2000-13206. [DOI] [PubMed] [Google Scholar]
- 21.Stas SN, El-Atat FA, Sowers JR. Pathogenesis of hypertension in diabetes. Rev Endocr Metab Disord. 2004;5:221–5. doi: 10.1023/B:REMD.0000032410.75638.da. [DOI] [PubMed] [Google Scholar]
- 22.Wheatcroft SB, Williams IL, Shah AM, Kearney MT. Pathophysiological implications of insulin resistance on vascular endothelial function. Diabet Med. 2003;20:255–68. doi: 10.1046/j.1464-5491.2003.00869.x. [DOI] [PubMed] [Google Scholar]
- 23.Lawlor DA, Ebrahim S, Smith GD. Associations of measures of lung function with insulin resistance and Type 2 diabetes: findings from the British Women's Heart and Health Study. Diabetologia. 2004;47:195–203. doi: 10.1007/s00125-003-1310-6. [DOI] [PubMed] [Google Scholar]
- 24.Davis WA, Knuiman M, Kendall P, Grange V, Davis TM. Glycemic exposure is associated with reduced pulmonary function in type 2 diabetes: the Fremantle Diabetes Study. Diabetes Care. 2004;27:752–7. doi: 10.2337/diacare.27.3.752. [DOI] [PubMed] [Google Scholar]
- 25.Ford ES, Mannino DM. Prospective association between lung function and the incidence of diabetes: findings from the National Health and Nutrition Examination Survey Epidemiologic Follow-up Study. Diabetes Care. 2004;27:2966–70. doi: 10.2337/diacare.27.12.2966. [DOI] [PubMed] [Google Scholar]
- 26.Beske SD, Alvarez GE, Ballard TP, Davy KP. Reduced cardiovagal baroreflex gain in visceral obesity: implications for the metabolic syndrome. Am J Physiol Heart Circ Physiol. 2002;282:H630–5. doi: 10.1152/ajpheart.00642.2001. [DOI] [PubMed] [Google Scholar]
- 27.Bjorntorp P, Holm G, Rosmond R. Hypothalamic arousal, insulin resistance and Type 2 diabetes mellitus. [see comment] Diabet Med. 1999;16:373–83. doi: 10.1046/j.1464-5491.1999.00067.x. [DOI] [PubMed] [Google Scholar]
- 28.Egan BM. Insulin resistance and the sympathetic nervous system. Curr Hypertens Rep. 2003;5:247–54. doi: 10.1007/s11906-003-0028-7. [DOI] [PubMed] [Google Scholar]
- 29.Esler M, Rumantir M, Wiesner G, Kaye D, Hastings J, Lambert G. Sympathetic nervous system and insulin resistance: from obesity to diabetes. Am J Hypertens. 2001;14:304S–9S. doi: 10.1016/s0895-7061(01)02236-1. [DOI] [PubMed] [Google Scholar]
- 30.Palatini P. Sympathetic overactivity in hypertension: a risk factor for cardiovascular disease. Curr Hypertens Rep. 2001;3(Suppl 1:):S3–9. doi: 10.1007/s11906-001-0065-z. [DOI] [PubMed] [Google Scholar]
- 31.Esler M, Rumantir M, Wiesner G, Kaye D, Hastings J, Lambert G. Sympathetic nervous system and insulin resistance: from obesity to diabetes. Am J Hypertens. 2001;14:304S–9S. doi: 10.1016/s0895-7061(01)02236-1. [DOI] [PubMed] [Google Scholar]
- 32.Perin PC, Maule S, Quadri R. Sympathetic nervous system, diabetes, and hypertension. Clin Exp Hypertens. 2001;23:45–55. doi: 10.1081/ceh-100001196. [DOI] [PubMed] [Google Scholar]
- 33.Bjorntorp P. Body fat distribution, insulin resistance, and metabolic diseases. Nutrition. 1997;13:795–803. doi: 10.1016/s0899-9007(97)00191-3. [DOI] [PubMed] [Google Scholar]
- 34.Vitaliano PP, Scanlan JM, Zhang J, Savage MV, Hirsch IB, Siegler IC. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosom Med. 2002;64:418–35. doi: 10.1097/00006842-200205000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Weber B, Schweiger U, Deuschle M, Heuser I. Major depression and impaired glucose tolerance. Exp Clin Endocrinol Diabetes. 2000;108:187–90. doi: 10.1055/s-2000-7742. [DOI] [PubMed] [Google Scholar]
- 36.Okamura F, Tashiro A, Utumi A, Imai T, Suchi T, Tamura D, et al. Insulin resistance in patients with depression and its changes during the clinical course of depression: minimal model analysis. Metab Clin Exp. 2000;49:1255–60. doi: 10.1053/meta.2000.9515. [DOI] [PubMed] [Google Scholar]
- 37.Raikkonen K, Matthews KA, Kuller LH. The relationship between psychological risk attributes and the metabolic syndrome in healthy women: antecedent or consequence? Metab Clin Exp. 2002;51:1573–7. doi: 10.1053/meta.2002.36301. [DOI] [PubMed] [Google Scholar]
- 38.Chan O, Inouye K, Riddell MC, Vranic M, Matthews SG. Diabetes and the hypothalamo-pituitary-adrenal (HPA) axis. Minerva Endocrinol. 2003;28:87–102. [PubMed] [Google Scholar]
- 39.Nelson TL, Palmer RF, Pedersen NL, Miles TP. Psychological and behavioral predictors of body fat distribution: age and gender effects. Obes Res. 1999;7:199–207. doi: 10.1002/j.1550-8528.1999.tb00702.x. [DOI] [PubMed] [Google Scholar]
- 40.Rosmond R. Stress induced disturbances of the HPA axis: a pathway to Type 2 diabetes? Med Sci Monit. 2003;9:RA35–9. [PubMed] [Google Scholar]
- 41.Drapeau V, Therrien F, Richard D, Tremblay A. Is visceral obesity a physiological adaptation to stress? Panminerva Med. 2003;45:189–95. [PubMed] [Google Scholar]
- 42.Chen CC, Lu FH, Wu JS, Chang CJ. Correlation between serum lipid concentrations and psychological distress. Psychiatry Res. 2001;102:153–62. doi: 10.1016/s0165-1781(01)00231-1. [DOI] [PubMed] [Google Scholar]
- 43.Lucini D, Norbiato G, Clerici M, Pagani M. Hemodynamic and autonomic adjustments to real life stress conditions in humans. Hypertension. 2002;39:184–8. doi: 10.1161/hy0102.100784. [DOI] [PubMed] [Google Scholar]
- 44.Levenstein S, Smith M, Kaplan G. Psychosocial predictors of hypertension in men and women. Arch Intern Med. 2001;161:1341–6. doi: 10.1001/archinte.161.10.1341. [DOI] [PubMed] [Google Scholar]
- 45.Pickering T, Clemow L, Davidson K, Gerin W. Behavioral cardiology—has its time finally arrived? Mt Sinai J Med. 2003;70:101–12. [PubMed] [Google Scholar]
- 46.Davidson K, Jonas B, Dixon K, Markovitz J. Do depression symptoms predict early hypertension incidence in young adults in the CARDIA study? Coronary Artery Risk Development in Young Adults. [Multicenter Study] Arch Intern Med. 2000;160:1495–500. doi: 10.1001/archinte.160.10.1495. [DOI] [PubMed] [Google Scholar]
- 47.Ariyo A, Haan M, Tangen C, Rutledge J, Cushman M, Dobs A, et al. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans. Cardiovascular Health Study Collaborative Research Group. Circulation. 2000;102:1773–91. doi: 10.1161/01.cir.102.15.1773. [DOI] [PubMed] [Google Scholar]
- 48.Spieker LE, Hurlimann D, Ruschitzka F, Corti R, Enseleit F, Shaw S, et al. Mental stress induces prolonged endothelial dysfunction via endothelin-A receptors. Circulation. 2002;105:2817–20. doi: 10.1161/01.cir.0000021598.15895.34. [DOI] [PubMed] [Google Scholar]
- 49.Cannon RO., 3rd Role of nitric oxide in cardiovascular disease: focus on the endothelium. [erratum appears in Clin Chem 1998;44:2070] Clin Chem. 1998;44:1809–19. [PubMed] [Google Scholar]
- 50.Sherwood A, Johnson K, Blumenthal JA, Hinderliter AL. Endothelial function and hemodynamic responses during mental stress. Psychosom Med. 1999;61:365–70. doi: 10.1097/00006842-199905000-00017. [DOI] [PubMed] [Google Scholar]
- 51.Eaton W, Armenian H, Gallo J, Pratt L, Ford D. Depression and risk for onset of type II diabetes. A prospective population-based study. [comment] Diabetes Care. 1996;19:1097–102. doi: 10.2337/diacare.19.10.1097. [DOI] [PubMed] [Google Scholar]
- 52.Black PH, Garbutt LD. Stress, inflammation and cardiovascular disease. J Psychosom Res. 2002;52:1–23. doi: 10.1016/s0022-3999(01)00302-6. [DOI] [PubMed] [Google Scholar]
- 53.von Kanel R, Mills PJ, Fainman C, Dimsdale JE. Effects of psychological stress and psychiatric disorders on blood coagulation and fibrinolysis: a biobehavioral pathway to coronary artery disease? Psychosom Med. 2001;63:531–44. doi: 10.1097/00006842-200107000-00003. [DOI] [PubMed] [Google Scholar]
- 54.Goodman E, Whitaker R. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 55.Lustman PJ, Clouse RE. Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes Complicat. 2005;19:113–22. doi: 10.1016/j.jdiacomp.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 56.Musselman D, Betan E, Larsen H, Phillips L. Relationship of depression to diabetes types 1 and 2: epidemiology, biology, and treatment. Biol Psychiatry. 2003;54:317–29. doi: 10.1016/s0006-3223(03)00569-9. [DOI] [PubMed] [Google Scholar]
- 57.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. [comment] Circulation. 1999;99:2192–217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 58.Bunker SJ, Colquhoun DM, Esler MD, Hickie IB, Hunt D, Jelinek VM, et al. “Stress” and coronary heart disease: psychosocial risk factors. Med J Aust. 2003;178:272–6. doi: 10.5694/j.1326-5377.2003.tb05193.x. [DOI] [PubMed] [Google Scholar]
- 59.Greenwood DC, Muir KR, Packham CJ, Madeley RJ. Coronary heart disease: a review of the role of psychosocial stress and social support. J Public Health Med. 1996;18:221–31. doi: 10.1093/oxfordjournals.pubmed.a024483. [DOI] [PubMed] [Google Scholar]
- 60.Kop WJ. The integration of cardiovascular behavioral medicine and psychoneuroimmunology: new developments based on converging research fields. Brain Behav Immun. 2003;17:233–7. doi: 10.1016/s0889-1591(03)00051-5. [DOI] [PubMed] [Google Scholar]
- 61.Todaro JF, Shen BJ, Niaura R, Spiro A, 3rd, Ward KD. Effect of negative emotions on frequency of coronary heart disease (The Normative Aging Study) Am J Cardiol. 2003;92:901–6. doi: 10.1016/s0002-9149(03)00967-6. [DOI] [PubMed] [Google Scholar]
- 62.Carney RM, Freedland KE, Miller GE, Jaffe AS. Depression as a risk factor for cardiac mortality and morbidity: a review of potential mechanisms. J Psychosom Res. 2002;53:897–902. doi: 10.1016/s0022-3999(02)00311-2. [DOI] [PubMed] [Google Scholar]
- 63.Everson-Rose SA, Meyer PM, Powell LH, Pandey D, Torrens JI, Kravitz HM, et al. Depressive symptoms, insulin resistance, and risk of diabetes in women at midlife. Diabetes Care. 2004;27:2856–62. doi: 10.2337/diacare.27.12.2856. [DOI] [PubMed] [Google Scholar]
- 64.Palinkas LA, Lee PP, Barrett-Connor E. A prospective study of Type 2 diabetes and depressive symptoms in the elderly: the Rancho Bernardo Study. Diabet Med. 2004;21:1185–91. doi: 10.1111/j.1464-5491.2004.01315.x. [DOI] [PubMed] [Google Scholar]
- 65.Sahay B. Yoga and diabetes. J Assoc Physicians India. 1986;34:645–8. [PubMed] [Google Scholar]
- 66.Telles S, Naveen K. Yoga for rehabilitation: an overview. Indian J Med Sci. 1997;51:123–7. [PubMed] [Google Scholar]
- 67.Pandya D, Vyas V, Vyas S. Mind-body therapy in the management and prevention of coronary disease. Compr Ther. 1999;25:283–93. doi: 10.1007/BF02944271. [DOI] [PubMed] [Google Scholar]
- 68.Damodaran A, Malathi A, Patil N, Shah N, Suryavansihi Marathe S. Therapeutic potential of yoga practices in modifying cardiovascular risk profile in middle aged men and women. [comment]. [Clinical Trial] J Assoc Physicians India. 2002;50:633–40. [PubMed] [Google Scholar]
- 69.Sahay B, Sahay R. Lifestyle modification in management of diabetes mellitus. J Indian Med Assoc. 2002;100:178–80. [PubMed] [Google Scholar]
- 70.Garfinkel M, Schumacher HJ. Yoga. Rheum Dis Clin North Am. 2000;26:125–32. doi: 10.1016/s0889-857x(05)70126-5. [DOI] [PubMed] [Google Scholar]
- 71.Chandler K. The emerging field of yoga therapy. Hawaii Med J. 2001;60:286–7. [PubMed] [Google Scholar]
- 72.Raub J. Psychophysiologic effects of Hatha Yoga on musculoskeletal and cardiopulmonary function: a literature review. J Altern Complement Med. 2002;8:797–812. doi: 10.1089/10755530260511810. [DOI] [PubMed] [Google Scholar]
- 73.Feuerstein G. The Deeper Dimension of Yoga: Theory and Practice. Boston: Shambhala Publications; 2003. [Google Scholar]
- 74.Innes K, Bourguignon C, Taylor A. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: a systematic review. J Am Board Fam Pract. 2005;18:491–519. doi: 10.3122/jabfm.18.6.491. [DOI] [PubMed] [Google Scholar]
- 75.Labarthe D, Ayala C. Nondrug interventions in hypertension prevention and control. Cardiol Clin. 2002;20:249–63. doi: 10.1016/s0733-8651(01)00003-0. [DOI] [PubMed] [Google Scholar]
- 76.Gimbel M. Yoga, meditation, and imagery: clinical applications. Nurse Pract Forum. 1998;9:243–55. [PubMed] [Google Scholar]
- 77.Wood C. Mood change and perceptions of vitality: a comparison of the effects of relaxation, visualization and yoga. J R Soc Med. 1993;86:254–8. [PMC free article] [PubMed] [Google Scholar]
- 78.Miller J, Fletcher K, Kabat-Zinn J. Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. Gen Hosp Psychiatry. 1995;17:192–200. doi: 10.1016/0163-8343(95)00025-m. [DOI] [PubMed] [Google Scholar]
- 79.Manchanda S, Narang R, Reddy K, Sachdeva U, Prabhakaran D, Dharmanand S, et al. Retardation of coronary atherosclerosis with yoga lifestyle intervention. [Randomized Controlled Trial] J Assoc Physicians India. 2000;48:687–94. [PubMed] [Google Scholar]
- 80.Patel C, Marmot M, Terry D, Carruthers M, Hunt B, Patel M. Trial of relaxation in reducing coronary risk: four year follow-up. Br Med J. 1985;290:1103–6. doi: 10.1136/bmj.290.6475.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jayasinghe SR. Yoga in cardiac health (a review) Eur J Cardiovasc Prev Rehabil. 2004;11:369–75. doi: 10.1097/01.hjr.0000206329.26038.cc. [DOI] [PubMed] [Google Scholar]
- 82.Innes KE, Bourguignon C, Taylor AG. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: a systematic review. J Am Board Fam Pract. 2005;18:491–519. doi: 10.3122/jabfm.18.6.491. [DOI] [PubMed] [Google Scholar]
- 83.Singh S, Malhotra V, Singh KP, Madhu SV, Tandon OP. Role of yoga in modifying certain cardiovascular functions in type 2 diabetic patients. J Assoc Physicians India. 2004;52:203–6. [PubMed] [Google Scholar]
- 84.Kerr D, Gillam E, Ryder J, Trowbridge S, Cavan D, Thomas P. An Eastern art form for a Western disease: randomised controlled trial of yoga in patients with poorly controlled insulin-treated diabetes. Pract Diabetes Intern. 2002;19:164–6. [Google Scholar]
- 85.Elder C. Ayurveda for diabetes mellitus: a review of the biomedical literature. Altern Ther Health Med. 2004;10:44–50. [PubMed] [Google Scholar]
- 86.Wang C, Collet JP, Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: a systematic review. Arch Intern Med. 2004;164:493–501. doi: 10.1001/archinte.164.5.493. [DOI] [PubMed] [Google Scholar]
- 87.Verhagen AP, Immink M, van der Meulen A, Bierma-Zeinstra SM. The efficacy of Tai Chi Chuan in older adults: a systematic review. Fam Pract. 2004;21:107–13. doi: 10.1093/fampra/cmh122. [DOI] [PubMed] [Google Scholar]
- 88.Bijlani RL, Vempati RP, Yadav RK, Ray RB, Gupta V, Sharma R, et al. A brief but comprehensive lifestyle education program based on yoga reduces risk factors for cardiovascular disease and diabetes mellitus. J Altern Complement Med. 2005;11:267–74. doi: 10.1089/acm.2005.11.267. [DOI] [PubMed] [Google Scholar]
- 89.Yogendra J, Yogendra H, Ambardekar S, Leie R, Shetty S, Dave M, et al. Beneficial effects of yoga lifestyle on reversibility of ischaemic heart disease: Caring Heart Project of International Board of Yoga. JAPI. 2004;52:283–9. [PubMed] [Google Scholar]
- 90.Fields JZ, Walton KG, Schneider RH, Nidich S, Pomerantz R, Suchdev P, et al. Effect of a multimodality natural medicine program on carotid atherosclerosis in older subjects: a pilot trial of Maharishi Vedic Medicine. Am J Cardiol. 2002;89:952–8. doi: 10.1016/s0002-9149(02)02245-2. [DOI] [PubMed] [Google Scholar]
- 91.Sahay B. Yoga and diabetes. J Assoc Physicians India. 1986;34:645–8. [PubMed] [Google Scholar]
- 92.Divekar M, Bhat M, Mulla A. Effect of yoga therapy in diabetes and obesity. J Diabet Assoc India. 1978;17:75–8. [Google Scholar]
- 93.Shembakar A, Kate S. Yogic exercise in the management of diabetes mellitus. J Diabet Assoc India. 1980;20:167–71. [Google Scholar]
- 94.Gore M. Yogic treatment for diabetes. Yoga Mimamsa. 1988;26:130–45. [Google Scholar]
- 95.Mukherjee A, Bandyopadhyay S, Benerjee S, Maity A. The influence of yogic exercise on blood sugar level in normal and diabetic volunteers. Indian J Physiol Allied Sci. 1989;43:105–12. [Google Scholar]
- 96.Mukherjee A, Banerjee S, Bandyopadhyay S, Mukherjee P. Studies on the interrelationship between insulin tolerance and yoga. Indian J Physiol Allied Sci. 1992;46:110–5. [Google Scholar]
- 97.Singh S, Malhotra V, Singh K, Sharma S. A preliminary report on the role of yoga asanas on oxidative stress in non-insulin dependent diabetes. Indian J Clin Biochem. 2001;16:216–20. doi: 10.1007/BF02864866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Malhotra V, Singh S, Singh K, Gupta P, Sharma S, Madhu S, et al. Study of yoga asanas in assessment of pulmonary function in NIDDM patients. Indian J Physiol Pharmacol. 2002;46:313–20. [PubMed] [Google Scholar]
- 99.Jain S, Uppal A, Bhatnagar S, Talukdar B. A study of response pattern of non-insulin dependent diabetics to yoga therapy. Diabetes Res Clin Pract. 1993;19:69–74. doi: 10.1016/0168-8227(93)90146-v. [DOI] [PubMed] [Google Scholar]
- 100.Jain S, Talukdar B. Role of yoga in control of hyperglycemia in middle aged patients of non-insulin dependent diabetes mellitus. Indian J Clin Biochem. 1995;10:62–5. [Google Scholar]
- 101.Monro R, Power J, Coumar A, Dandona P. Yoga therapy for NIDDM: a controlled trial. Complement Med Res. 1992;6:66–8. [Google Scholar]
- 102.Khare K, Jain D. Effect of yoga on plasma glucose and serum fructosamine level in NIDDM. Yoga Mimamsa. 1999;33:1–9. [Google Scholar]
- 103.Malhotra V, Singh S, Tandon O, Madhu S, Prasad A, Sharma S. Effect of Yoga asanas on nerve conduction in type 2 diabetes. Indian J Physiol Pharmacol. 2002;46:298–306. [PubMed] [Google Scholar]
- 104.Yogendra J, Yogendra H, Ambardekar S, Leie R, Shetty S, Dave M, et al. Beneficial effects of yoga lifestyle on reversbility of ischaemic heart disease: Caring Heart Project of International Board of Yoga. J Assoc Physicians India. 2004;52:283–9. [PubMed] [Google Scholar]
- 105.Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, et al. Intensive lifestyle changes for reversal of coronary heart disease. [see comment] [erratum appears in JAMA 1999;281:1380] JAMA. 1998;280:2001–7. doi: 10.1001/jama.280.23.2001. [DOI] [PubMed] [Google Scholar]
- 106.Koertge J, Weidner G, Elliott-Eller M, Scherwitz L, Merritt-Worden TA, Marlin R, et al. Improvement in medical risk factors and quality of life in women and men with coronary artery disease in the Multicenter Lifestyle Demonstration Project. Am J Cardiol. 2003;91:1316–22. doi: 10.1016/s0002-9149(03)00320-5. [DOI] [PubMed] [Google Scholar]
- 107.Khare K, Rai S. Study of lipid profile in post myocardial infarction subjects following yogic lifestyle intervention. Indian Pract. 2002;55:369–73. [Google Scholar]
- 108.Sahay BK, Sadasivudu B, Yogi R, Bhaskaracharyulu C, Raju PS, Madhavi S, et al. Biochemical parameters in normal volunteers before and after yogic practices. Indian J Med Res. 1982;76(Suppl:):144–8. [PubMed] [Google Scholar]
- 109.Bhaskaracharyulu C, Sitarama Raju P, Girija Kumari D, Sahay B, Annapurna M, Madhavi S, et al. The effect of yoga on lipo protein profile in diabetics. J Diabetes Assoc India. 1986;26:120–4. [Google Scholar]
- 110.Naruka J, Mathur R, Mathur A. Effect of pranayama practices on fasting blood glucose and serum cholesterol. Indian J Med Sci. 1986;40:149–52. [PubMed] [Google Scholar]
- 111.Schmidt T, Wijga A, Von Zur Muhlen A, Brabant G, Wagner T. Changes in cardiovascular risk factors and hormones during a comprehensive residential three month kriya yoga training and vegetarian nutrition. [Clinical Trial] Acta Physiol Scand Suppl. 1997;640:158–62. [PubMed] [Google Scholar]
- 112.Schmidt T, Wijga A, Von Zur Muhlen A, Brabant G, Wagner T. Changes in cardiovascular risk factors and hormones during a comprehensive residential three month kriya yoga training and vegetarian nutrition. Acta Physiol Scand Suppl. 1997;640:158–62. [PubMed] [Google Scholar]
- 113.Ornish D. Avoiding revascularization with lifestyle changes: The Multicenter Lifestyle Demonstration Project. Am J Cardiol. 1998;82:26. doi: 10.1016/s0002-9149(98)00744-9. [DOI] [PubMed] [Google Scholar]
- 114.Chohan IS, Nayar HS, Thomas P, Geetha NS. Influence of yoga on blood coagulation. Thromb Haemost. 1984;51:196–7. [PubMed] [Google Scholar]
- 115.Yadav RK, Ray RB, Vempati R, Bijlani RL. Effect of a comprehensive yoga-based lifestyle modification program on lipid peroxidation. Indian J Physiol Pharmacol. 2005;49:358–62. [PubMed] [Google Scholar]
- 116.Sharma H, Sen S, Singh A, Bhardwaj NK, Kochupillai V, Singh N. Sudarshan Kriya practitioners exhibit better antioxidant status and lower blood lactate levels. Biol Psychol. 2003;63:281–91. doi: 10.1016/s0301-0511(03)00071-1. [DOI] [PubMed] [Google Scholar]
- 117.Jatuporn S, Sangwatanaroj S, Saengsiri A, Rattanapruks S, Srimahachota S, Uthayachalerm W, et al. Short-term effects of an intensive lifestyle modification program on lipid peroxidation and antioxidant systems in patients with coronary artery disease. Clin Hemorheol Microcirc. 2003;29:429–36. [PubMed] [Google Scholar]
- 118.Bhattacharya S, Pandey U, Verma N. Improvement in oxidative status with yogic breathing in young healthy males. Indian J Physiol Pharmacol. 2002;46:349–54. [PubMed] [Google Scholar]
- 119.Dhalla N, Temsah R, Netticadan T. Role of oxidative stress in cardiovascular diseases. J Hypertens. 2000;18:655–73. doi: 10.1097/00004872-200018060-00002. [DOI] [PubMed] [Google Scholar]
- 120.Lee KU. Oxidative stress markers in Korean subjects with insulin resistance syndrome. Diabetes Res Clin Pract. 2001;54(Suppl 2:):S29–33. doi: 10.1016/s0168-8227(01)00332-1. [DOI] [PubMed] [Google Scholar]
- 121.Juhan-Vague I, Morange PE, Alessi MC. The insulin resistance syndrome: implications for thrombosis and cardiovascular disease. Pathophysiol Haemost Thromb. 2002;32:269–73. doi: 10.1159/000073579. [DOI] [PubMed] [Google Scholar]
- 122.Ginsberg HN, Huang LS. The insulin resistance syndrome: impact on lipoprotein metabolism and atherothrombosis. J Cardiovasc Risk. 2000;7:325–31. doi: 10.1177/204748730000700505. [DOI] [PubMed] [Google Scholar]
- 123.Kohler HP. Insulin resistance syndrome: interaction with coagulation and fibrinolysis. Swiss Med Wkly. 2002;132:241–52. doi: 10.4414/smw.2002.09856. [DOI] [PubMed] [Google Scholar]
- 124.McKeever TM, Weston PJ, Hubbard R, Fogarty A. Lung function and glucose metabolism: an analysis of data from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2005;161:546–56. doi: 10.1093/aje/kwi076. [DOI] [PubMed] [Google Scholar]
- 125.Tran MD, Holly RG, Lashbrook J, Amsterdam EA. Effects of hatha yoga practice on the health-related aspects of physical fitness. Prev Cardiol. 2001;4:165–70. doi: 10.1111/j.1520-037x.2001.00542.x. [DOI] [PubMed] [Google Scholar]
- 126.Telles S, Nagarathna R, Nagendra HR, Desiraju T. Physiological changes in sports teachers following 3 months of training in Yoga. Indian J Med Sci. 1993;47:235–8. [PubMed] [Google Scholar]
- 127.Joshi L, Joshi V, Gokhale L. Effect of short term ‘Pranayam’ practice on breathing rate and ventilatory functions of lung. Indian J Physiol Pharmacol. 1992;36:105–8. [PubMed] [Google Scholar]
- 128.Harinath K, Malhotra AS, Pal K, Prasad R, Kumar R, Kain TC, et al. Effects of Hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med. 2004;10:261–8. doi: 10.1089/107555304323062257. [DOI] [PubMed] [Google Scholar]
- 129.Birkel DA, Edgren L. Hatha yoga: improved vital capacity of college students. Altern Ther Health Med. 2000;6:55–63. [PubMed] [Google Scholar]
- 130.Berger B, Owen D. Mood alteration with yoga and swimming: aerobic exercise may not be necessary. Percept Mot Skills. 1992;75(3 Pt 2):1331–43. doi: 10.2466/pms.1992.75.3f.1331. [DOI] [PubMed] [Google Scholar]
- 131.Malathi A, Damodaran A, Shah N, Patil N, Maratha S. Effect of yogic practices on subjective well being. [Clinical Trial] Indian J Physiol Pharmacol. 2000;44:202–6. [PubMed] [Google Scholar]
- 132.Ray U, Mukhopadhyaya S, Purkayastha S, Asnani V, Tomer O, Prashad R, et al. Effect of yogic exercises on physical and mental health of young fellowship course trainees. [Randomized Controlled Trial] Indian J Physiol Pharmacol. 2001;45:37–53. [PubMed] [Google Scholar]
- 133.Schell F, Allolio B, Schonecke O. Physiological and psychological effects of Hatha-Yoga exercise in healthy women. [Clinical Trial. Controlled Clinical Trial. Journal Article] Int J Psychosom. 1994;41:46–52. [PubMed] [Google Scholar]
- 134.Sahajpal P, Ralte R. Impact of induced yogic relaxation training (IYRT) on stress-level, self-concept and quality of sleep among minority group individuals. J Indian Psychol. 2000;18:66–73. [Google Scholar]
- 135.Lavey R, Sherman T, Mueser KT, Osborne DD, Currier M, Wolfe R. The effects of yoga on mood in psychiatric inpatients. Psychiatr Rehabil J. 2005;28:399–402. doi: 10.2975/28.2005.399.402. [DOI] [PubMed] [Google Scholar]
- 136.Janakiramaiah N, Gangadhar B, Naga Venkatesha Murthy P, Harish M, Subbakrishna D, Vedamurthachar A. Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: a randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000;57:255–9. doi: 10.1016/s0165-0327(99)00079-8. [DOI] [PubMed] [Google Scholar]
- 137.Nespor K. Twelve years of experience with yoga in psychiatry. Int J Psychosom. 1993;40:105–7. [PubMed] [Google Scholar]
- 138.Shannahoff-Khalsa DS, Ray LE, Levine S, Gallen CC, Schwartz BJ, Sidorowich JJ. Randomized controlled trial of yogic meditation techniques for patients with obsessive compulsive disorders. CNS Spectr Intern J Neuropsychiatric Med. 1999;4:34–46. doi: 10.1017/s1092852900006805. [DOI] [PubMed] [Google Scholar]
- 139.Cohen L, Warneke C, Fouladi RT, Rodriguez MA, Chaoul-Reich A. Psychological adjustment and sleep quality in a randomized trial of the effects of a Tibetan yoga intervention in patients with lymphoma. Cancer. 2004;100:2253–60. doi: 10.1002/cncr.20236. [DOI] [PubMed] [Google Scholar]
- 140.Mishra M, Sinha RK. Effect of yogic practices on depression and anxiety. J Project Psychol Mental Health. 2001;8:23–7. [Google Scholar]
- 141.Woolery A MH, Sternlieb B, Zeltzer L. A yoga intervention for young adults with elevated symptoms of depression. Altern Ther Health Med. 2004;10:60–3. [PubMed] [Google Scholar]
- 142.Jorm A, Christensen H, Griffiths K, Rodgers B. Effectiveness of complementary and self-help treatments for depression. Med J Aust. 2002;176(Suppl:):S84–96. doi: 10.5694/j.1326-5377.2002.tb04508.x. [DOI] [PubMed] [Google Scholar]
- 143.Latha, Kaliappan K. Yoga, pranayama, thermal biofeedback techniques in the management of stress and high blood pressure. J Indian Psychol. 1991;9:36–46. [Google Scholar]
- 144.Walia IJ, Mehra P, Grover P, Earnest C, Verma SK. Sanjeev Health status of nurses and yoga. IV. Experiment and results. Nurs J India. 1992;83:27–8. [PubMed] [Google Scholar]
- 145.Ernst E, Rand J, Stevinson C. Complementary therapies for depression: an overview. Arch Gen Psychiatry. 1998;55:1026–32. doi: 10.1001/archpsyc.55.11.1026. [DOI] [PubMed] [Google Scholar]
- 146.Innes K, Vincent H, Taylor A. Chronic stress and insulin-resistance-related indices of cardiovascular disease risk: Part II. A potential role for mind-body therapies. Altern Ther Health Med. 2006 in press. [PubMed] [Google Scholar]
- 147.Innes K, Vincent H, Taylor A. Chronic stress and insulin-resistance-related indices of cardiovascular disease risk: Part I. Neurophysiologic responses and pathologic sequellae. Altern Ther Health Med. 2006 in press. [PubMed] [Google Scholar]
- 148.Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 149.Norris SL, Zhang X, Avenell A, Gregg E, Schmid CH, Lau J. Long-term non-pharmacological weight loss interventions for adults with prediabetes. Cochrane Database Syst Rev. 2005;;2 doi: 10.1002/14651858.CD005270. CD005270. [DOI] [PubMed] [Google Scholar]
- 150.Vickers A, Goyal N, Harland R, Rees R. Do certain countries produce only positive results? A systematic review of controlled trials. Control Clin Trials. 1998;19:159–66. doi: 10.1016/s0197-2456(97)00150-5. [DOI] [PubMed] [Google Scholar]