Abstract
This review evaluated the effect of complementary and alternative medicine on pain during labor with conventional scientific methods using electronic data bases through 2006 were used. Only randomized controlled trials with outcome measures for labor pain were kept for the conclusions. Many studies did not meet the scientific inclusion criteria. According to the randomized control trials, we conclude that for the decrease of labor pain and/or reduction of the need for conventional analgesic methods: (i) There is an efficacy found for acupressure and sterile water blocks. (ii) Most results favored some efficacy for acupuncture and hydrotherapy. (iii) Studies for other complementary or alternative therapies for labor pain control have not shown their effectiveness.
Keywords: acupuncture, biofeedback, complementary and alternative medicine, delivery, homeopathy, hydrotherapy, hypnosis, labor, labor pain, manual healing, pain, sophrology, sterile water blocks, stimulation, transcutaneous electrical nerve stimulation, yoga
Introduction
Even though delivery is a natural phenomenon, it has been demonstrated that the accompanying pain is considered severe or extreme in more than half of cases. Besides conventional approaches, such as epidural analgesia, many complementary or alternative methods have been reported to reduce pain during labor and delivery. Complementary or Alternative Medicine (CAM) can be defined as theories or practices that are not part of the dominant or conventional medical system. Some of them have been reclassified as part of conventional medicine when supported by clinical experience or scientific data (1).
These methods are popular because they emphasize the individual personality, and the interaction between mind, body and environment (2). They are attractive to people who want to be more involved in their own care and feel that such therapies are more in harmony with their personal philosophies. The conventional medical community usually offers traditional choices of analgesia, such as epidural and intravenous drugs. Patients may have access to alternative methods, but will generally be obliged to do the relevant research themselves beforehand. Those seeking alternatives are not necessarily dissatisfied with conventional medicine, but attempt to supplement rather than replace traditional care. Quite often, users of complementary medicine do not inform the practitioners in charge of their pregnancy and delivery. There are also different expectations for the management of pain during labor according to the category of professionals. Physicians are expected to provide pharmacological therapy, whereas midwives, nurses and other auxiliaries are required to assist patients with psychological methods, and in fact use alternative approaches more often. The theoretical bases for many alternative methods derive from Eastern tradition or philosophy.
After a description of labor pain, we shall mention the conventional treatments and describe the different complementary methods applicable to labor pain.
Nature of Pain During Labor and Delivery
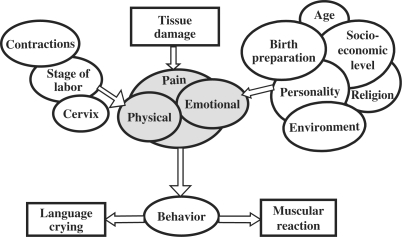
A scientific definition of pain is ‘an unpleasant sensory and emotional experience associated with actual or potential tissue damage’ (3). Acute pain such as labor pain has two dimensions: a sensory or physical dimension, with the transmission of information, the pain stimuli, to the brain, and an affective dimension due to interpretation of these stimuli through the interaction of a wide variety of emotional, social, cultural and cognitive variables unique to the individual (Fig. 1).
Figure 1.
Components of pain (6).
For the management of pain, conventional medicine focuses more on the physical side, while alternative methods deal mainly with emotional considerations. In the laboring patient, the two stages of labor correspond to different types of pain and routes of transmission. During dilatation (first stage), visceral pain predominates, due to mechanical distention of the cervix and of the lower part of the uterus. These stimuli are transmitted to the spinal cord at the level of the tenth thoracic to the first lumbar root. Uterine contractions may be felt as back pain because the nerves that supply the uterus also supply the skin on the lower back or lumbosacral area. During the descent phase (second stage), pain is also caused by distension and stretching of the pelvic floor and perineum. These stimuli are transmitted via the pudendal nerve to the second to fourth sacral nerves.
Even though pain is a personal experience, it can be analyzed by means of quantitative pain measures. Verbal reports using standardized instruments, such as the McGill Pain Questionnaire and the Visual Analogue Scale (VAS), have been the most common methods of pain assessment both in clinical practice and research (4).
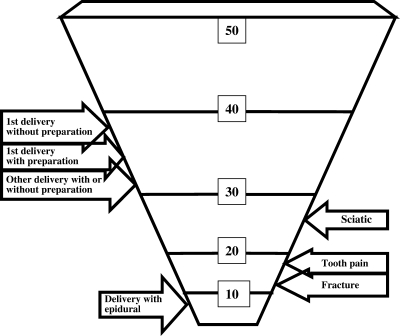
A Canadian study comparing different pain syndromes found that average labor pain scores were higher in both nulliparous (first delivery) and multiparous women than the average scores previously recorded for out-patients with sciatic pain, toothache and fracture pain (5,6) (Fig. 2). However, whereas the average score is higher, its exact value differs greatly from one woman to another. Bonica found that labor pain was mild in 15% of cases, moderate in 35%, severe in 30% and extreme in 20% (7).
Figure 2.
Pain scores (4–6).
Some factors are associated with increased pain: first delivery, history of dysmenorrhea (painful periods), fear of pain, a religious practice. Some factors diminish pain: childbirth preparation classes, complications during pregnancy, wish to breast feed, high socio-economic status, older age (5).
To evaluate the efficiency of the different therapies, we have applied conventional scientific methods to published studies. In other words, do these studies report a statistically significant reduction in labor pain? As we shall see, few publications in the field of CAM meet these standards. However, we should consider that pain, which can now be quantified, is only one component of a woman's overall experience of labor and birthing. Personal satisfaction is not always correlated with the level of pain and although difficult to quantify should be included in the evaluations. Note that the term analgesia means pain relief without total loss of sensation, while anesthesia is defined as pain relief with total loss of sensation.
Conventional Treatments
Regional Analgesia: Epidural
An epidural involves the introduction of a local anesthetic agent to the sensitive nerves conducting the pain messages on their way to the spine. A catheter (fine flexible tube) is usually placed in the epidural space, allowing intermittent or continuous infusion throughout the delivery.
The epidural is the most efficient way of reducing labor pain (Fig. 2). A total of 85–95% of women report complete relief of pain during the two phases of delivery: cervical dilatation and descent of the baby (8). Complete failure is rare and usually due to technical problems, as when the epidural space cannot be reached with the catheter. Delivery pain relief can be partial. The painful feeling of contractions persists, but at a lower intensity. Sometimes the area of analgesia is incomplete. For example, the pain can be felt laterally in half of the abdomen. When the lower nerves are not, or are insufficiently, dulled, pain may develop during the second phase of labor. One of the main advantages of the epidural is that it is efficient regardless of the cultural context, with few side effects. But it is not always available.
Injected Drugs
Morphine-like drugs (opioids) can be given continuously or in intermittent doses at the patient's request or via patient-controlled administration. Recent reports suggest that the analgesic effect of these agents in labor is limited and that the primary mechanism of action is heavy sedation, which means that consciousness is reduced during delivery. Such drugs may also have some effect on the newborn, with rare but possible breathing difficulties that may require assistance. Few studies have dealt with efficiency. Most were done in the 1960s and provide information on patient satisfaction (generally good in about half of the cases), but without quantitative evaluation of pain reduction.
Nitrous Oxide
Nitrous oxide gas is given for inhalation at subanesthetic concentrations. Despite being used for more than 100 years, there is no clear quantitative evidence of the efficacy of nitrous oxide in relieving labor pain. The subjective feelings of mothers giving birth suggest, however, that nitrous oxide is beneficial in many cases. Many women report significant analgesia with it, and many would choose it again for another delivery.
Alternative Approaches
Complementary and alternative methods applicable to labor pain can be divided into mind–body interventions, alternative systems of medical practice, manual healing, bioelectromagnetic and physical methods, and alternative medication (1).
Mind–Body Interventions
Mind–body interventions are based on the interconnectedness of mind and body and on the power of each to affect the other. Many mind–body interventions are applied to chronic illness, but this technique also appears to be applicable to the acute situation of delivery.
Psychoprophylactic Methods
Grantly Dick-Read introduced ‘natural childbirth’ in 1933. He believed that childbirth pain was a pathologic response produced by fear, apprehension and tension. He felt it essential to teach women the anatomic and physiologic facts of childbirth, and to instruct them in physical and mental relaxation. Both approaches are alleged to diminish pain by familiarizing the pregnant woman with the process of childbirth and by creating an atmosphere of confidence.
Fernand Lamaze introduced his method in France in 1951 after a visit to Russia. This method was first optimistically called ‘painless childbirth’, but later the more appropriate term ‘fearless childbirth’ was applied. It is based on the Pavlovian concept of conditioned reflex training. By focusing on certain breathing patterns or concentration points such as a mark on a nearby wall, it should be possible to block pain messages to the brain.
Bradley's method emphasizes natural childbirth, with the parents working as a team. Students of this method are taught about deep abdominal breathing and an understanding of the labor and delivery process. Rather than trying to block out pain, Bradley's method encourages concentrated awareness that works through the pain.
These methods are expected to provide better information about the process of delivery, reduce fear, give greater satisfaction with a sense of achievement and happiness, and create a better child–mother relationship. The importance of a good relationship between the patient and the care-giving team is also emphasized. Of these approaches, we have only found an evaluation of the Lamaze method: a study by Melzack in 1984 (5) using the McGill pain scale found a slight decrease in average pain score in patients using the Lamaze method, but this was not statistically significantly different from the control group (Fig. 2).
This study also showed that the average pain score is slightly higher at the first delivery, compared with subsequent deliveries, but the difference is not statistically significant.
Leboyer's Method
Frédéric Leboyer described his method in France in 1974 in his book ‘Birth without violence’. Inspired by Indian yoga, this method focuses on providing a better welcome for the newborn. In contrast to the usual environment, with too much light and noise stressing the baby, Leboyer proposes calm for mother, father and professionals, and darkness, little noise and a warm bath for the newborn. For the comfort of the mother during delivery, Leboyer considers that serenity obtained through attention to the baby raises the pain threshold. There has been no specific evaluation of the effects on labor pain. However, couples express a high degree of satisfaction. Although Leboyer's method is rarely used now as described in the 1970s, many birth practitioners still consider it to have a positive effect, with gentle and heightened attention for the newborn.
Hypnosis
The word hypnosis originates from the Greek ‘hypnos’ meaning ‘sleep’. In fact, it is not sleep but a state of focused concentration in which the patient can be relatively unaware, but not completely blind to her surroundings (2). During hypnosis, suggestions may be made, focusing on diminishing awareness of pain, fear and anxiety. The woman is prepared with initial hypnotic experiences that include three steps: absorption of the words or images presented by the therapist, dissociation, a suspension of critical judgment, and responsiveness. A few comparative studies have evaluated the efficiency of hypnosis.
In 1962, Davidson (9) compared 70 patients who had six lessons of autohypnosis with 70 who had received Dick-Read's training and with 71 who had no special antenatal training. The study was not randomized as patients were allowed to choose their group. A statistically significant reduction in the duration of the first stage of labor was found in the hypnosis group as compared with the two other groups. Autohypnosis was effective on labor pain: 59% of this group required no analgesia, compared with 1.4% in the control group. All patients required analgesia in the Dick-Read training group. The subjective impression of labor was much more pleasant in the autohypnosis group. In 1990, Harmon et al. (10) completed a randomized study showing shorter stage 1 labor, less medication and higher pain thresholds in the hypnosis group than in the control group. In 1995, Mairs (11) compared 29 primigravida women who chose to join ‘hypnosis for childbirth’ classes and 29 in a control group. The trained group reported statistically significantly lower ratings of both pain and anxiety. However, there was no statistically significant difference between the two groups in their drug usage during labor.
A few negative effects of hypnosis have been reported, including mild dizziness, nausea and headache. These seem to be associated with failure to dehypnotize the patient properly. Caution should be used in patients vulnerable to psychotic decompensation.
To summarize, hypnosis seems to reduce fear, tension and pain during labor and to raise the pain threshold. It reduces the need for chemical analgesia. Patients have a greater sense of control over painful contractions. Hypnosis, therefore, can be considered as a helpful adjunct during the course of labor and delivery.
Biofeedback
Biofeedback uses monitoring instruments to provide feedback to patients, i.e. physiological information of which they are normally unaware. Electrodes feed information to a monitoring box that registers the results by a sound or a visual meter that varies as the monitored function increases or decreases. For women in labor, several biofeedback-assisted relaxation techniques have been introduced.
Duchene (12) completed in 1989 a prospective randomized trial in which tension of the abdominal muscles was monitored. As uterine contractions occurred the women focused on relaxing the abdominal muscles. The reports of pain using VASs and verbal description scales showed significantly lower pain values in the biofeedback group and less medication. In 1992, Bernat et al. (13) used a fingertip thermometer. When the patient relaxes, vasodilation occurs and the finger temperature increases. However, none of the experimental subjects attempted to use fingertip temperature control as a coping technique during labor. The authors concluded that a lack of hospital staff support may have contributed to this study's outcome.
In conclusion, biofeedback-assisted relaxation techniques applied to pain control yield contradictory results. Their efficiency is certainly contingent on strong support from caregivers to facilitate the use of the technique.
Yoga
Yoga, a method of Indian origin, proposes control of mind and body. Between the different types of yoga, ‘energy yoga’ can be applied to pregnancy and delivery. Through special training of breathing, it achieves changes in levels of consciousness, relaxation, receptivity to the world and inner peace. According to professionals who use this technique for delivery, yoga shortens the duration of labor, decreases pain and reduces the need for analgesic medication. However, we have not found any scientific confirmation of these assertions.
Sophrology
The word sophrology derives from two Greek words, ‘sos’ harmony or serenity and ‘phren’ conscience or spirit. This technique derived from Indian yoga was introduced in Europe during the 1960s. Its purpose is to improve the control of body and spirit through three degrees of dynamic relaxation: concentration, contemplation and meditation. Applied to obstetrics, better control of the delivery process is expected. Patients individually report a high degree of satisfaction with this experience of relaxation during prenatal classes and delivery, but there is no controlled evaluation in the literature.
Haptonomy
Derived from the Greek words ‘hapsis’ affectivity and ‘nomos’ knowledge, haptonomy can be defined as the science of affectivity. This approach was proposed by Frans Vedman (14) in the Netherlands during the 1940s. Specific zones of affectivity are reported to improve the contact between father, mother and baby and to help to share emotions. In practice, haptonomy is appreciated by couples during pregnancy, but it seems to be used irregularly during labor, particularly because teams in charge of delivery are not always aware of its existence. Practitioners expect a quicker and easier delivery as well as a better relationship between parents and newborn. There is no published evaluation of haptonomy and in fact such an assessment should not be expected because, as the specialists of this method say, ‘affectivity cannot be put into numbers’.
Music Therapy
Music addresses many of the physical and psychological needs of patients. In obstetrics, a slow and restful type of music may be used as a sedative to promote relaxation during the early stage of labor. Music with a steady beat may be used as a stimulant to promote movement during the latter stages. The literature findings are discordant.
In Austin, Texas, a music program is used during the third trimester of pregnancy (15). The prospective mother and her partner are allowed to select the kind of music they like for the different stages of labor. After a study of 30 deliveries, only one half of the women who had listened to music required analgesia. However, in a randomized study Durham and Collins (16) could not demonstrate the value of music in reducing the need for analgesic medication. But the subjective sense of satisfaction appeared to be higher in the group that listened to music. In a randomized controlled trial by Phumdoung and Good (17), 110 primiparous women, during the active phase of labor, were assigned to a soft music group for 3 h (n = 55) or a control group (n = 55). Dual VAS were used to measure the sensation of pain before starting the study and every three hours. The results indicate that in the music group women had significantly less sensation of pain (P < 0.001). After these contradictory results concerning the effects of music therapy there is a need for further scientific analyses.
Alternative Systems of Medical Practice
Acupuncture
Acupuncture has been used in China for more than 2000 years. Specific anatomic parts of the body are stimulated for therapeutic purposes. This can be done in the usual way with needles, but practitioners may also use heat, pressure, impulse of magnetic energy, burning by a preparation of the herb Artemia vulgaris, electrical stimulation or surface electrodes at acupuncture loci.
Acupuncture is based on the balance between Yin and Yang. Treatment is aimed at reconstituting the normal movement between these two opposites. The meridians are considered as energy channels. Most treatments of obstetrical and gynecological problems involve the use of points on different meridians: spleen-pancreas located on the inside of the ankle bone, conception, governing or penetrating vessel.
Acupuncture may produce effects through several different mechanisms. One hypothesis is that acupuncture points have electrical properties that, when stimulated, may alter the level of chemical neurotransmitters in the body. Another hypothesis is that endorphins are released due to activation of the hypothalamus. The effects of acupuncture have also been attributed to alterations in the natural electrical currents or electromagnetic fields in the body.
The use of acupuncture for pain relief has given equivocal results. Wallis et al. (18) in San Francisco in 1974 found that 19 of 21 patients had inadequate pain relief based on pain scores and none of the 21 subjects was judged by investigators to have adequate analgesia. Abouleish and Depp (19) in the USA in 1970 used electroacupuncture and described relief of pre-existing pain in 7 of 12 participants. The investigators, who found the technique time-consuming, cited some disadvantages: inconsistency, unpredictability and lack of completeness. Hyodo and Gega (20) in Japan in 1977 in a study of subjective and objective relief of labor pain in 32 women described an improvement in ∼60% of 16 primiparous women and 90% of 16 multiparous women. However, all patients received systemic sedation. The authors concluded that acupuncture is useful for delivery because of its safety, despite erratic and less potent results than conventional analgesic techniques. In Nigeria in 1986, 19 of 30 women (63.3%) given sacral acupuncture by Umeh (21) indicated that they had adequate pain relief by responses on a visual scale and did not request another form of analgesia. Yanai et al. (22) in Israel in 1987 evaluated electroacupuncture during the labor of 16 parturients. Fifty-six percent of the women reported mild to good pain relief and 81% described increased relaxation. The perceived positive effects led the authors to believe that acupuncture should be pursued as an additional method of pain control. In 1999, Lyrenas et al. (23) in Sweden studied 31 primiparous women who had received repeated acupuncture compared with untreated women. Pain assessed on a VAS was not reduced in women treated with acupuncture, and the acupuncture did not reduce the need for analgesics during labor. In 2002 Ramnero et al. (24) in Sweden reported a randomized, controlled study in 90 parturients, 46 of whom received acupuncture during labor as a complement or alternative to conventional analgesia. Acupuncture significantly reduced the need for epidural analgesia (12% vs. 22%). Patients in the acupuncture group reported a significantly greater degree of relaxation compared with the control group. The authors considered these results to suggest that acupuncture could be a good alternative or complement for women who seek an alternative to pharmacological analgesia in childbirth, but further trials are required to clarify whether the main effect of acupuncture during labor is analgesic or relaxing. In the trial by Skilnand et al. (25), 210 parturients were randomly assigned to receive either real acupuncture or false acupuncture. Real acupuncture consisted of a treatment protocol from the Norwegian School of Acupuncture. The same type and number of needles were used not on the classic meridians. Pain was assessed using a linear VAS (rated 0–10) recorded at 30, 60 and 120 min after treatment. There were significantly lower pain scores at 30, 60, 120 min after treatment (P < 0.001), and significantly less need for epidural analgesia and intramuscular pethidine (P = 0.01 et P < 0.001, respectively). Qu and Zhou (26) compared in a prospective randomized study 20 primipara with electro-acupuncture and 19 as controls. The electro-acupuncture group was found to exhibit a lower pain intensity and a better degree of relaxation than the control group (P = 0.018 and 0.031).
To summarize, acupuncture studies are difficult to conduct and analyze for several reasons, including lack of standardization with use of multiple acupuncture points, and the difficulty of choosing a control group. Within the control group the needles might be correctly placed but not stimulated, or needles could be placed in inappropriate sites. There were no reported complications in any of the studies but there is a potential risk of infection. To achieve a good analgesic effect during labor, a relatively long induction period may be required. It is difficult for a woman in labor to remain still for 15–30 min, and some patients felt discomfort because of the restrictions in movement.
Overall, a beneficial therapeutic effect on labor pain of acupuncture is not certain. Better designed studies need to be completed with, if possible, standardization of the points used, and better control groups. However, it should be recognized that the procedure is time-consuming, and that the required training of patients and personnel may be considerable.
Acupressure Systems
Acupressure is a descendant of Chinese manipulative therapy in which points are stimulated by pressure, using hands, fingers and thumbs (27). Acupressure supposedly promotes the circulation of blood, the harmony of yin and yang and the secretion of neurotransmitters, thus maintaining the normal functions of the human body and enhancing well being. Some midwives use acupressure to release the pain of labor. Pressure is applied simultaneously to both sides of the spine in the lower back. Pressure against spots that are sensitive can be particularly efficacious. Force is initially applied during contractions and then continuously.
The purpose of the study of Chung et al. (28) is to determine the effect of L14 and BL67 acupressure on labor pain during the first stage of labor. A total of 127 parturient women were randomly assigned to three groups. Each group received only one of the following treatments: L14 and BL67 acupressure, light skin stroking or no treatment. There was a significant difference in decreased labor pain in the first group compared with the two others.
A study of Lee et al. (29) evaluated the effects of SP6 acupressure on labor pain. 75 women in labor were randomly assigned to either the SP6 acupressure (n = 36) or SP6 touch control (n = 39) group using double-blinded method. Labor pain was measured four times using VAS. There were significant differences between the groups in pain scores at all times following the intervention: immediately after the intervention (P = 0.012), 30 min after the intervention (P = 0.021) and 60 min after the intervention (P = 0.012). The total labor time (3 cm of dilatation to delivery) was significantly shorter in the SP6 acupressure intervention group than in the control group (P = 0.006).
Homeopathy
Homeopathy involves the use of diluted substances that cause symptoms in their undiluted form. According to homeopathic theory, remedies stimulate the self-healing mechanism. The amount of medicine prescribed is so small that it often cannot be measured in molecular amounts (30). We found no studies evaluating the effect of homeopathic treatment on labor pain. Smith (31) has reviewed cervical ripening and labor induction by “caulophyllum”. There were no differences between the homeopathy and control groups in a randomized, controlled trial involving 40 women.
Manual Healing
Manual healing methods used today during delivery include therapeutic touch and massage therapy.
Therapeutic Touch
The purpose of therapeutic touch in labor is to communicate caring and reassurance. Painful contractions of the uterus can be treated by the application of pressure with the hands to the woman's back, abdomen, hips, thighs, sacrum or perineum. Whether touch is perceived as positive or not is dependent on who is touching the patient: in one study, touching was perceived positively by 94% of patients when they were touched by a relative or friend, 86% by their husbands, 73% by a nurse and 21% by a physician (32). Anxiety is reported to be reduced in patients who receive reassuring touch. In a retrospective study of 30 patients, 77% experienced ‘less pain’ when they were touched during labor, and 40% reported less need for pain medication.
Massage Therapy
The practice of massage varies from the tickling massage of ‘kung fu’ to a firm massage. The effect of a gentle massage of the periumbilical area by their partner was studied in nine women compared with six who received no massage (33). There was no significant difference between the two groups in pain evaluated by means of visual scale, and no difference in the time of use of epidural analgesia for labor.
In a randomized controlled study by Chang et al. (34), 60 primiparous women expected to have a normal childbirth were randomly assigned to either the experimental (n = 30) or the control (n = 30) group. The experimental group received massage intervention comprising abdominal effleurage, sacral pressure and shoulder/back kneading during labor. In the massage group, the woman received a 30-min massage during uterine contractions first by the researcher and then by the partner during each of the three phases of labor. The intensity of pain between the two groups was compared in the latent phase (cervix dilated 3–4 cm), active phase (5–7 cm) and transitional phase (8–10 cm). A t-test demonstrated that the massage group had significantly lower pain reactions in the latent, active and transitional phases.
Bioelectromagnetic Applications and Physical Methods
Transcutaneous Electrical Nerve Stimulation
TENS involves administration of low voltage electrical stimuli through flat electrodes applied to the skin. TENS units consist of a stimulator and two pairs of electrodes. The upper electrodes are taped at the level of the tenth thoracic to the first lumbar root and the lower pair at the level of the second to fourth sacral nerves. The stimulator has two channels for the two pairs of electrodes. Initial reports were encouraging. Augustinson et al. (1977) (35) found that among 147 women, 44% rated pain relief as good or very good and 44% as moderate. Bundsen et al. (36) found TENS to be especially beneficial for labor pain localized in the back. However, a meta-analysis by Carroll et al. (37) of 10 randomized, controlled trials in 877 women, 436 receiving TENS and 441 as controls, revealed no significant difference in pain and the use of additional analgesic interventions was not different between the two groups.
Sterile Water Blocks
Counter-irritation is the process by which localized pain may be relieved by irritating the skin in the same dermatomal distribution. For example, the uterus is supplied by the lower thoracic spinal cord segments. Some of these receive stimuli from the skin of the lower back and the sacrum. Labor analgesia may be produced by counter-irritation of this area. Irritation can be achieved by intracutaneous injection of sterile water papules over the sacrum with a fine needle. Lytzen et al. (38) in Sweden noted instant and complete relief of lower back pain in the first stage of labor in 83 women. Pain relief lasted as long as 3 h. In some women, the block was repeated. Half of the women required no other form of analgesia. Martensson and Wallin (39) compared in a randomized study pregnant women with severe labor pain treated by injections of water intracutaneously and isotonic saline subcutaneously injections (placebo). Labor pain was significantly lower in the first group compared with the placebo group (P = 0.002 and 0.006). Labrecque et al. (40) compared water blocks with TENS for the treatment of lower back pain during labor. Women who received the sterile water injections rated the intensity of pain lower than did women in the TENS group. Intracutaneous water injections are associated with a sharp injection pain that lasts between 20 and 30 sec, which some women find less acceptable than lower back pain. This method may be an alternative for women who have lower back pain during labor but wish to avoid epidural analgesia.
Hydrotherapy
The popularity of undergoing part of labor in water has increased dramatically around the world. The expected benefits include pain relief and decreased use of analgesia and anesthesia. Several studies have reported use of analgesia for women undergoing labor in water, but others have found no difference from control groups. In a 1987 non-randomized, prospective, controlled study, Lenstrup et al. (41) evaluated the effect of a warm bathtub on 88 parturients, and found that cervical dilatation rate and pain relief could be improved in patients who had a bath during the first stage of labor. In 1988, independent midwives used hydrotherapy in which a clean bathtub was filled with warm water. The clinical impression of practitioners who use hydrotherapy is that their patients experience shorter and less painful labor. Burn and Greenish (42) studied 302 women who used a labor pool. Fifty percent of the primigravidas in the pool group used pain medication, compared with 76% in the control group. Rush et al. (43) found in a randomized study in 785 women that the tub group required fewer pharmacological agents than the control group (66% vs. 59%, P = 0.06). Cammu et al. (37) in a prospective randomized trial using a VAS showed that absolute values of labor pain were not significantly different between hydrotherapy and control groups.
In the Cochrane Pregnancy and Childbirth register (45), eight randomized controlled trials (2939 women) comparing bath tub/pool with no immersion during pregnancy, labor or birth were selected. Women who used water immersion during the first stage of labor reported statistically significant less pain than those not laboring in water. There was a statistically significant reduction in the use of epidural/spinal/paracervical/analgesia/anaesthesi among women allocated to water immersion during the first stage of labor compared with those not allocated to water immersion. There were no significant differences incidence of an Apgar score less than 7 at 5 min, neonatal unit admissions or neonatal infection rates.
Maternal satisfaction with this birth experience has been measured and women report increased levels of satisfaction, self-esteem, pain relief and relaxation with immersion. Ruptured membranes have been discussed as a potential problem in the use of hydrotherapy, although in the study of Lenstrup et al. they were not considered a contraindication. Odent (46) reported no infectious complications in patients who gave birth in water, even if the membranes were already ruptured.
Alternative Medications
Herbal Medicine
Herbal medicine is described as the use of plant materials in medicine and food for therapeutic purposes. Various herbal remedies are used during the prenatal period to ‘prepare’ the uterus and cervix for childbirth and ease pain during labor and delivery.
In a study of the practice of a group of independent midwives in Utah (27), specific herbs were used because of their perceived actions and properties, in particular a ‘5-week formula’ which is a combination of 10 herbs used during the last 5 or 6 weeks of pregnancy. This is said to facilitate birth. Some herbal remedies are used as the principal method of managing pain and enhancing endurance during delivery. Practitioners observed that these herbal formulas had a calming and relaxing effect. Labor pain can also be treated specifically with motherwort. The effect of raspberry leaf in facilitating labor in 192 multiparous women was studied by Simpson et al. (47) in a double-blind, randomized, placebo-controlled trial in Australia. Raspberry leaf was consumed in tablet form from 32 weeks of gestation until labor. Contrary to popular belief, it did not shorten the first stage of labor but rather the second (mean difference 9.59 min), and also lowered the rate of forceps deliveries (19.3% vs. 30.4%). The difficulty with herbal remedies is that few have undergone scientific scrutiny, chemical isolation, or extraction to identify the pharmacologically active agent or to enable toxicity testing.
Aromatherapy
Aromatherapy uses essential oils extracted from aromatic botanical sources to treat and balance the mind, body and spirit (30). It combines the physiological effects of massage with the use of essential oils. One of the purposes of this method is to relieve anxiety and stress and to help relaxation. Massage around the lower back with jasmine, juniper, geranium, clary sage, rose and lavender have been reported to provide subjective benefit in labor.
Conclusion
Complementary and alternative medicine can be defined as methods that are not currently part of the dominant or conventional medical system. CAM exists because conventional medicine can be limited in its ability to provide relief and to meet patients’ needs. CAM and conventional medicine share the responsibility for applying evidence-based practice and for seeking scientific proof to justify a planned intervention, as well as the obligation to avoid harmful or useless practices.
For labor pain, most studies demonstrate the greatest benefit during the beginning of the dilatation phase. When women enter the active phase of dilatation or during delivery itself, there is more need for additional conventional analgesics. This suggests that complementary medicine may be useful for the early onset of pain or as a distracter, diverting women's attention from the source of pain. In some cases the number of parturients who successfully use alternative methods is greater than what would be expected from a placebo effect. In a few cases the amount of pain medication was reduced but this was not consistently true. The degree of success of a method is correlated with the availability of support staff in both educational and trial phases of the studies, and necessarily in clinical practice. Whereas physicians do not need to be experts in the management of alternative therapies, they should at least possess some basic knowledge of complementary medicine. In the future, the demand for complementary medicine will probably continue to rise. Care providers have to facilitate informed choices through discussion of their own experience and knowledge. One of the difficulties for the physician is to identify studies sufficiently well-designed to help them guide their patients.
This article is an update of a chapter in the book complementary and alternative approaches to biomedicine with permission of the publisher (48).
References
- 1.Chez RA, Jonas WB. The challenge of complementary and alternative medicine. Am J Obstet Gynecol. 1997;177:1156–61. doi: 10.1016/s0002-9378(97)70033-4. [DOI] [PubMed] [Google Scholar]
- 2.Gentz BA. Alternative therapies for the management of pain in labor and delivery. Clinical Obstet Gynecol. 2001;44:704–35. doi: 10.1097/00003081-200112000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Lowe NK. The nature of labor pain. Am J Obstet. 2002;186:16–24. doi: 10.1067/mob.2002.121427. [DOI] [PubMed] [Google Scholar]
- 4.Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1:277–99. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- 5.Melzack R. The myth of painless childbirth. Pain. 1984;19:321–37. doi: 10.1016/0304-3959(84)90079-4. [DOI] [PubMed] [Google Scholar]
- 6.Cardin H, Moisson Tardieu MT, Tournaire M. La péridurale. Paris: Balland; 1986. [Google Scholar]
- 7.Bonica JJ. Textbook of Pain. Edinburgh: Churchill-Livingstone; 1984. [Google Scholar]
- 8.Brownridge P, Cohen S. Neural Blockade in Clinical Anesthesia and Management of Pain. Philadelphia: J. P. Lippincott Company; 1988. Neural blockade for obstetrics and gynecologic surgery. [Google Scholar]
- 9.Davidson JA. An assessment of the value of hypnosis in pregnancy and labor. Br Med J. 1962;2:951–3. doi: 10.1136/bmj.2.5310.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harmon TM, Hynan MJ, Tyre TE. Improved obstetric outcomes using hypnotic analgesia and skill mastery combined with childbirth education. J Consult Clin Psychol. 1990;58:525–30. doi: 10.1037//0022-006x.58.5.525. [DOI] [PubMed] [Google Scholar]
- 11.Mairs D. Hypnosis and Pain in Childbirth. Contemp Hypnosis. 1995;12:111–18. [Google Scholar]
- 12.Duchene P. Effects of biofeedback on childbirth pain. J Pain Symptom Manage. 1989;4:117–23. doi: 10.1016/0885-3924(89)90004-3. [DOI] [PubMed] [Google Scholar]
- 13.Bernat SH, Wooldridge PJ, Marecki M, Snell L. Biofeedback-assisted relaxation to reduce stress in labor. J Obstet Gynecol Neonatal Nurs. 1992;21:295–303. doi: 10.1111/j.1552-6909.1992.tb01740.x. [DOI] [PubMed] [Google Scholar]
- 14.Veldman F. Haptonomy science de l’affectivité. Paris: Presse Universitaire de France; 1989. [Google Scholar]
- 15.Marwick C. Leaving concert hall for clinic, therapists now test music's “charms”. Jama. 1996;275:267–8. [PubMed] [Google Scholar]
- 16.Durham L, Collins M. The effect of music as a conditioning aid in prepared childbirth education. J Obstet Gynecol Neonatal Nurs. 1986;15:268–70. doi: 10.1111/j.1552-6909.1986.tb01396.x. [DOI] [PubMed] [Google Scholar]
- 17.Phumdoung S, Good M. Music reduces sensation and distress of labor pain. Pain Manag Nurs. 2003;2:54–61. doi: 10.1016/s1524-9042(02)54202-8. [DOI] [PubMed] [Google Scholar]
- 18.Wallis L, Shnider SM, Palahniuk RJ, Spivey HT. An evaluation of acupuncture analgesia in obstetrics. Anesthesiology. 1974;41(6):596–601. doi: 10.1097/00000542-197412000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Abouleish E, Depp R. Acupuncture in obstetrics. Anesth Analg. 1975;54:82–8. doi: 10.1213/00000539-197501000-00017. [DOI] [PubMed] [Google Scholar]
- 20.Hyodo M, Gega O. Use of Acupuncture Anesthesia for Normal Delivery. Am J Chin Med. 1977;5:63–9. doi: 10.1142/s0192415x77000075. [DOI] [PubMed] [Google Scholar]
- 21.Umeh B. Sacral acupuncture for pain relief in labor: initial clinical experience in Nigerian women. Acupunct Electrother Res. 1986;11:147–51. doi: 10.3727/036012986816359120. [DOI] [PubMed] [Google Scholar]
- 22.Yanai N, Shalev E, Yagudin E, Zuckerman H. The use of acupuncture during labor. Am J Acupunct. 1987;15:311–12. [Google Scholar]
- 23.Lyrenas S, Lutsch H, Hetta J, Nyberg F, Willdeck-Lundh G, Lindberg B. Acupuncture before delivery: effect on Pain Perception and the Need for Analgesics. Gynecol Obstetric Invest. 1999;29(2):118–24. doi: 10.1159/000293316. [DOI] [PubMed] [Google Scholar]
- 24.Ramnero A, Hanson V, Kihlgren M. Acupuncture treatment during labour. A randomised controlled trial. BJOG. 2002;109:637–44. [PubMed] [Google Scholar]
- 25.Skilnand E, Fossen D, Heiberg E. Acupuncture in the management of pain in labor. Acta Obstet Gynecol Scand. 2002;81:943–8. doi: 10.1034/j.1600-0412.2002.811008.x. [DOI] [PubMed] [Google Scholar]
- 26.Qu F, Zhou J. Electro-acupuncture in relieving Labor Pain. ECam J. 2007 doi: 10.1093/ecam/nel053. (in press) (Advance access published on August 17, 2006) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sakala C. Content of care by independent midwives: assistance with pain in labor and birth. Soc Sci Med. 1988;26:1141–58. doi: 10.1016/0277-9536(88)90190-6. [DOI] [PubMed] [Google Scholar]
- 28.Chung UL, Hung LC, Kuo SC, Huang CL. Effects of L14 and BL67 acupressure on labor pain and uterine contractions in the first stage of labor. J Nurs Res. 2003;4:251–60. doi: 10.1097/01.jnr.0000347644.35251.c1. [DOI] [PubMed] [Google Scholar]
- 29.Lee MK, Chang SB, Kang DH. Effects of SP6 acupressure on labor pain and length of delivery time in women during labor. J Altern Complement Med. 2004;10:959–65. doi: 10.1089/acm.2004.10.959. [DOI] [PubMed] [Google Scholar]
- 30.Allaire AD. Complementary and alternative medicine in the labor and delivery suite. Clinical Obstet Gynecol. 2001;44:681–91. doi: 10.1097/00003081-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Smith CA. Homeopathy for induction of labour. Cochrane Database Sys Rev. doi: 10.1002/14651858.CD003399. CD 003399:2001. [DOI] [PubMed] [Google Scholar]
- 32.Penny KS. Postpartum perceptions of touch received during labor. Res Nurs Health. 1979;2:9–16. doi: 10.1002/nur.4770020103. [DOI] [PubMed] [Google Scholar]
- 33.Hedstrom LW, Newton N. Touch in labor: a comparison of cultures and eras. Birth. 1986;13:181–6. doi: 10.1111/j.1523-536x.1986.tb01041.x. [DOI] [PubMed] [Google Scholar]
- 34.Chang M, Wang S, Chen C. Effects of massage on pain and anxiety during labour: a randomized controlled trial in Taiwan. J Adv Nurs. 2002;38:68–73. doi: 10.1046/j.1365-2648.2002.02147.x. [DOI] [PubMed] [Google Scholar]
- 35.Augustinsson LE, Bohlin P, Bundsen P, Carlsson CA, Forssman L, Sjoberg P, et al. Pain relief during delivery by transcutaneous electrical nerve stimulation. Pain. 1977;4(1):59–65. doi: 10.1016/0304-3959(77)90087-2. [DOI] [PubMed] [Google Scholar]
- 36.Bundsen P, Peterson LE, Selstam U. Pain relief labor by transcutaneous electrical nerve stimulation, a prospective matched study. Acta Obstet Gynecol Scand. 1981;60:459–468. doi: 10.3109/00016348109155461. [DOI] [PubMed] [Google Scholar]
- 37.Carroll D, Moore RA, Tramer MR, Mc Quay HJ. Transcutaneous electrical nerve stimulation does not relieve labor pain: updated systematic review. Contemp, Rev Obstet Gynecol. 1997:; 195–205. [Google Scholar]
- 38.Lytzen T, Cederberg L, Moller Nielsen J. Relief of low back pain in labor by using intracutaneous nerve stimulation (INS) with sterile water papules. Acta Obstet Gynecol Scand. 1989;6:341–3. doi: 10.3109/00016348909028669. [DOI] [PubMed] [Google Scholar]
- 39.Martensson L, Wallin G. Labour pain treated with cutaneous injections of sterile water: randomized controlled trial. Br J Obstetric Gynaecology. 1999;106:633–7. doi: 10.1111/j.1471-0528.1999.tb08359.x. [DOI] [PubMed] [Google Scholar]
- 40.Labrecque M, Nouwen A, Bergeron M, Rancourt JF. A randomized controlled trial of nonpharmacologic approaches for relief of low back pain during labor. J Fam Pract. 1999;48(4):259–63. [PubMed] [Google Scholar]
- 41.Lenstrup, Schantz A, Berget A, Feder, Roseno H, Hertel J. Warm tub bath during delivery. Acta Obstet Gynecol Scand. 1987;66:709–12. doi: 10.3109/00016348709004148. [DOI] [PubMed] [Google Scholar]
- 42.Burn E, Greenish K. Water birth. Pooling information. Nurs Times. 1993;89:47–9. [PubMed] [Google Scholar]
- 43.Rush J, Burlock S, Lambert K, Loosley-Millman M, Hutchison B, Enkin M. The effects of whirlpool baths in labor: a randomized controlled trial. Birth. 1996;23:136–43. doi: 10.1111/j.1523-536x.1996.tb00474.x. [DOI] [PubMed] [Google Scholar]
- 44.Cammu H, Clasen K, Van Wettere L, Derde M. “To bathe or not to bathe” during the first stage of labor. Acta Obstet Gynecol Scand. 1994;73:468–72. doi: 10.3109/00016349409013433. [DOI] [PubMed] [Google Scholar]
- 45.Cluett E, Nikodem V, McCandlish R, Burns E. Immersion in water in pregnancy, labour and birth. Cochrane Database Syst Rev. 2004;2:CCD000111. doi: 10.1002/14651858.CD000111.pub2. [DOI] [PubMed] [Google Scholar]
- 46.Odent M. Birth under water. Lancet. 1983;2(8365–6):1476–7. doi: 10.1016/s0140-6736(83)90816-4. [DOI] [PubMed] [Google Scholar]
- 47.Simpson M, Parsons M, Grenwood J, Wade K. Raspberry leaf in pregnancy: its safety and efficacy in labor. J Midwifery Womens Health. 2001;46:51–9. doi: 10.1016/s1526-9523(01)00095-2. [DOI] [PubMed] [Google Scholar]
- 48.Tournaire M. Alternative approaches to pain relief during labor and delivery. In: Cooper E, Yamaguchi N, editors. Complementary and Alternative Approaches to Biomedicine. New-York: Kluwer Academic/Plenum publishers; 2004. pp. 193–206. [Google Scholar]