Abstract
Bipolar disorder is a highly recurrent and debilitating illness. Research has implicated the role of psychosocial stressors, including high expressed-emotion (EE) attitudes among family members, in the relapse–remission course of the disorder. This article explores the developmental pathways by which EE attitudes originate and predict relapses of bipolar disorder. Levels of EE are correlated with the illness attributions of caregivers and bidirectional patterns of interaction between caregivers and patients during the postepisode period. Although the primary treatments for bipolar disorder are pharmacological, adjunctive psychosocial interventions have additive effects in relapse prevention. Randomized controlled trials demonstrate that the combination of family-focused therapy (FFT) and pharmacotherapy delays relapses and reduces symptom severity among patients followed over the course of 1 to 2 years. The effectiveness of FFT in delaying recurrences among adolescents with bipolar disorder and in delaying the initial onset of the illness among at-risk children is currently being investigated.
Keywords: family-focused treatment, expressed emotion, psychosocial treatment, pharmacotherapy, childhood-onset bipolar disorder
By the year 2020, bipolar disorder will be the sixth leading cause of disability worldwide among all medical illnesses (Murray & Lopez, 1996). Persons with the disorder vary between the extremes of mania (a highly energized, elated, or irritable state) and depression (a deflated, withdrawn, morose, and often suicidal state). The Diagnostic and Statistical Manual of Mental Disorders (4th ed., American Psychiatric Association, 1994) defines two primary types of bipolar disorder: Bipolar I (at least one episode of mania or mixed disorder) and Bipolar II (episodes of hypomania alternating with severe periods of depression). Over 2% of the US population has Bipolar I or II disorder, and another 2.4% has the disorder in its various subclinical (or subsyndromal) forms (Merikangas et al., 2007).
The illness is highly recurrent, with 60% of patients experiencing recurrences of mania or depression within 2 years and up to 75% experiencing recurrences within 5 years. Patients experience significant symptoms during approximately half of the weeks of their lives and have multiple impairments in school, at work, and in relationships (Judd et al., 2002). Up to 15% die by suicide, and as many as 50% attempt suicide one or more times (Miklowitz & Johnson, 2006).
Mood stabilizers and atypical antipsychotics have a substantial success record in hastening recovery from episodes and decreasing risk of recurrence. However, these medications do not fully prevent recurrences of the disorder, nor do they eliminate the significant residual symptoms—notably depression—that many patients experience between episodes.
The family environment is an important context for understanding the development and maintenance of severe psychopathology (Repetti, Taylor, & Seeman, 2002) and mood disorders in particular (Hooley & Parker, 2006; Miklowitz, 2004). This article concerns the role of family relationships as risk or protective processes in the course of bipolar illness and the role of family-focused therapy (FFT) as an adjunct to drug therapy during the postepisode period.
THE ROLE OF THE FAMILY IN THE COURSE OF BIPOLAR ILLNESS
Current thinking about the relapse–remission course of bipolar disorder emphasizes a biopsychosocial model that incorporates the interactive roles of genetic vulnerability, biological predispositions, family or life events stress, and psychological vulnerability. The illness is clearly heritable, and there is substantial evidence for dysfunction of the neurotransmitter systems (notably dopamine and serotonin) and of the limbic–cortical system. Specifically, elevated activity in the amygdala and diminished activity of the frontal-cortical regions may interfere with the capacity to regulate emotion (for review, see Miklowitz & Johnson, 2006).
Family stress has been operationalized as whether or not the patient resides with relatives characterized by high expressed-emotion (EE) attitudes (Brown, Birley, & Wing, 1972). High EE refers to high levels of criticism, hostility, and/or emotional overinvolvement from a caregiving relative (typically a parent or spouse) during or immediately following a patient’s acute episode of illness. It is typically assessed through the Camberwell Family Interview, although briefer alternative assessments with acceptable reliability and validity are available (Hooley & Parker, 2006). Patients with schizophrenia, bipolar disorder, or recurrent major depressive disorder who return home to high-EE families following an acute episode are two to three times more likely to relapse in the subsequent 9 months than are patients who return to low-EE families (Barrowclough & Hooley, 2003; Miklowitz, 2004).
A Developmental Psychopathology Approach to Expressed Emotion
Research on the mechanisms underlying the association between EE and relapse have addressed two questions: (a) How do caregiving relatives become high-EE? (b) What variables mediate the association between EE and patients’ relapses? A developmental psychopathology framework for understanding the causal and reactive roles of parental EE in mood disorders (Miklowitz, 2004) begins with a child who has temperamental disturbances (e.g., irritability, low frustration tolerance, mood instability, high anxiety) or compromised cognitive functioning. These early disturbances partially reflect the child’s genetic vulnerability to bipolar, schizophrenic, or other psychiatric disorders. The child is paired with a parent who, by virtue of his or her own neurobiology and social history, reacts to the child’s behavior with frustration and hostility (expressed as frequent criticisms of the child) or with guilt and anxiety (expressed in overly protective behaviors). Repeated exposure to criticisms, anxiety, or overinvolvement during the period when a child is developing a sense of identity may contribute to self-doubt, self-criticism, and core beliefs about relationships as aversive and conflict-ridden. These schemata for the self may interfere with the child’s acquisition of emotional self-regulatory skills, as reflected in depression, anxiety, aggression, and the inability to tolerate negative states of affect. In turn, his or her negative counterreactions fuel high-EE attitudes and behaviors in parents, which recursively contribute to the child’s emotional and cognitive vulnerabilities. The model in Figure 1 clarifies how similar recursive processes may maintain high-EE attitudes and contribute to relapse in families in which patients have already had episodes of bipolar disorder.
Fig. 1.
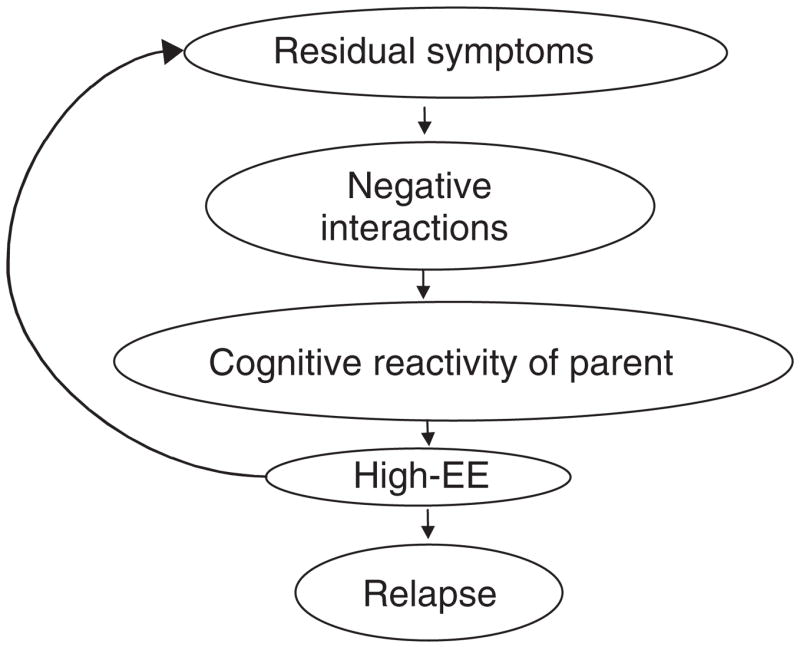
Bidirectional relationship between parental expressed emotion (EE) and patients’ mood symptoms. The pathway begins with unresolved residual symptoms in the patient (e.g., depression, irritability, mild delusional thinking, withdrawal, hypomania) that contribute to the intensity of the patient’s reactions to caregivers. Escalating negative interactions reduce the threshold for caregivers to react with fear, frustration, and hopelessness; remember and exaggerate negative experiences from prior illness episodes; and make attributions of controllability and negative predictions about the future (e.g., “She’s doing this to hurt me”; “I’ll always have to take care of him”). This “cognitive reactivity” of the caregiver may fuel his or her expression of high-EE attitudes toward the patient, resulting in temporary exacerbations of the patient’s residual symptoms and a worsening pattern of dyadic interaction. In combination with biological and genetic vulnerability factors, repeated exposure to negative family interactions may contribute to the patient’s overall liability to early relapse.
Research on Pathways to EE
Although the pathway in Figure 1 is hypothetical, it is supported by cross-sectional research on the correlates of EE among relatives of psychiatric patients. Notably, high-EE relatives are more likely to attribute the negative behaviors of patients to personal and controllable factors (i.e., personality, lack of effort) than are low-EE relatives, who are more likely to attribute the behaviors to uncontrollable factors (i.e., illness or external stressors; Barrowclough & Hooley, 2003). Several studies find that high-EE relatives and patients are more likely than low-EE relatives and patients to be engaged in negative cycles of verbal and nonverbal interaction during the postepisode period (for review, see Miklowitz, 2004).
A study of family interactions among patients with schizophrenia is particularly relevant to this hypothesized pathway (Rosenfarb, Goldstein, Mintz, & Nuechterlein, 1995). During the period following a hospitalization for psychosis, patients with schizophrenia from high-EE families showed significantly more odd and disruptive behaviors with parents during laboratory-based family interactions than did patients from low-EE families. High-EE parents were more likely than low-EE parents to respond with a criticism to the first unusual thought expressed by the patient with schizophrenia, which increased the probability that the patient would express a second unusual thought. A study with similar methodology in a small sample of bipolar patients found that there was a strong correlation (r = .53) between relatives’ harsh criticisms and patients’ “odd and grandiose thinking” during family interactions, but only among patients who relapsed in the subsequent 9 months (Rosenfarb et al., 2001). The correlation was low (r = .12) among patients who did not subsequently relapse.
The pathways from high-EE attitudes in caregivers to relapses among patients may be mediated by patients’ biological and psychological vulnerabilities. Hooley, Gruber, Scott, Hiller, and Yurgelun-Todd (2005) examined neural activation (as measured by functional magnetic resonance imaging) among college students with and without a history of depression while they listened to tapes of their mothers expressing critical, supportive, or neutral statements. In students with a prior history of depression, the dorsolateral prefrontal cortex failed to activate in response to maternal criticism, although activation in response to criticism was observed among students with no depression history. The dorsolateral prefrontal cortex plays a major role in working memory, problem-solving, affective expression, interpersonal effectiveness, and the conscious control of behavior.
These and other cognitive vulnerabilities of patients may affect their processing of critical comments from relatives and may contribute to their overall levels of distress. A longitudinal study found that bipolar patients who reported being more emotionally distressed by criticisms from relatives had higher depression scores and fewer days well during a 1-year prospective period than did patients who reported less distress from criticisms (Miklowitz, Wisniewski, Miyahara, Otto, & Sachs, 2005). Patients who become especially distressed by signs of interpersonal rejection from family members may internalize the content of criticisms, which may contribute to their subsequent mood dysregulation.
Thus, high-EE attitudes emerge through a complex interplay between historical events, personal variables, attributional styles, and current relationship factors. Family interventions should therefore consider (a) the developmental processes by which high-EE attitudes originated, (b) the ways in which patients process and react to negative affect from parents or other caregivers, (c) the cognitive reactivity of relatives, (d) the ability of patients to manage stressful family interactions, and (e) the behaviors of patients that provoke negativity among caregivers.
FAMILY INTERVENTION FOR BIPOLAR DISORDER
Family interventions for bipolar disorder are psychoeducational in orientation, meaning that families (spouses, parents) and patients are taught to recognize the signs and symptoms of bipolar disorder, develop strategies for intervening early with new episodes, and assure consistency with medication regimens (see Box 1). The psychoeducational approach recognizes that lack of information about the disorder, along with uncertainties about the future, fuel patients’ denial of the diagnosis and contribute to caregivers’ high-EE attitudes. Thus, in addition to providing prescriptive information, clinicians address the patients’ and family members’ affective reactions to the illness, its prognosis, and its expected treatments and assist them in developing coping strategies relevant to their individual situation.
BOX 1 Key Features of Family-Focused Treatment.
Commences shortly after an acute episode of mania, depression, or mixed disorder
Involves the patient and one or more relatives (spouse, parents, siblings)
Conducted in 21 sessions over 9 months (weekly for 3 months, biweekly for 3 months, monthly for 3 months)
-
Consists of three consecutive modules:
Psychoeducation: didactic information and interactive discussion about the symptoms of bipolar disorder, early warning signs, relapse prevention plans, roles of risk and protective factors, and the importance of medication adherence (7 sessions)
Communication enhancement training: behavioral rehearsal of effective speaking, listening, and negotiating skills, with homework practice (7–10 sessions)
Problem-solving skills training: identify and define specific family problems, brainstorm solutions, evaluate the advantages and disadvantages of each solution, choose one or a combination of solutions, develop implementation plans; homework between sessions (4–5 sessions)
Booster sessions as needed
The first randomized trial of FFT (Miklowitz, George, Richards, Simoneau, & Suddath, 2003) involved 101 bipolar patients (mean age = 36 years; mean prior episodes = 6.4) who had had an acute episode of mania or depression in the 3 months prior to the trial. Of the 101 patients, 82 began the trial in the hospital. Patients were randomly assigned as outpatients to FFT and drug therapy or to a comparison crisis-management treatment consisting of two sessions of family psychoeducation, crisis-intervention sessions as needed over a period of 9 months, and drug therapy. Over a 2-year follow-up, patients in FFT were more likely to survive the full follow-up without relapsing (52%) than were patients in crisis management (17%) and also had less severe depressive and manic symptoms (Miklowitz et al., 2003; see Fig. 2).
Fig. 2.
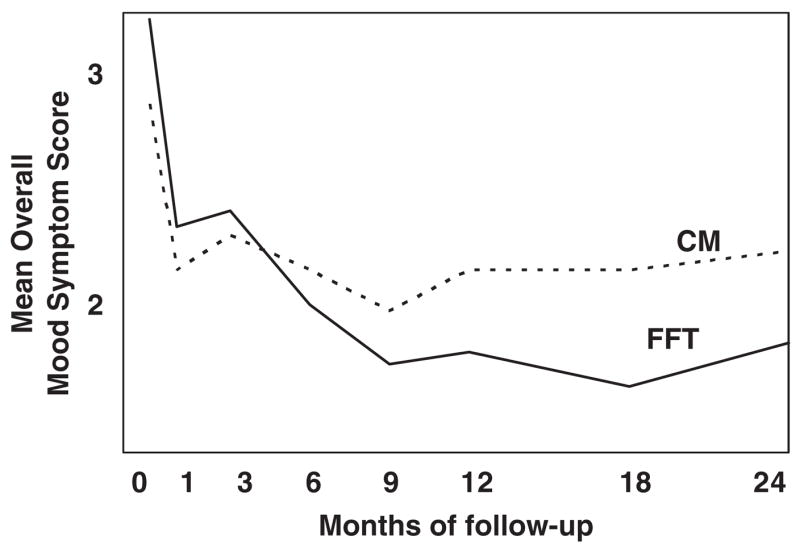
Results of a 2-year randomized trial (N = 101) showing that family-focused treatment (FFT; n = 31) and medications improve bipolar patients’ mood symptoms more than crisis management (CM; n = 70) and medications. From “A Randomized Study of Family-Focused Psychoeducation and Pharmacotherapy in the Outpatient Management of Bipolar Disorder,” by D.J. Miklowitz, E.L. George, J.A. Richards, T.L. Simoneau, and R.L. Suddath, 2003, Archives of General Psychiatry, 60, p. 909.
A second trial (Rea et al., 2003) compared FFT and pharmacotherapy with an individual psychoeducational therapy of identical duration and intensity (21 sessions over 9 months) and equivalent drug therapy. Over a period of 2 to 3 years, patients in FFT had longer periods of stability prior to recurrence than did patients in individual therapy. In the 1- to 2-year period after treatment ended, only 12% of the FFT patients were rehospitalized, compared to 60% of the individual therapy patients.
The multisite Systematic Treatment Enhancement Program for Bipolar Disorder contrasted the effectiveness of FFT and other psychotherapies to a brief psychosocial intervention across 15 U.S. treatment centers (Miklowitz et al., 2007). Acutely depressed bipolar patients (N = 293) were randomly assigned to one of three intensive (30 sessions) psychotherapies with drug therapy—FFT, interpersonal and social-rhythm therapy (therapy focused on interpersonal problem solving and the regulation of daily routines and sleep–wake cycles), or cognitive-behavioral therapy—or to a minimal (3 sessions) “collaborative care” (CC) psychoeducational treatment and drug therapy. Over the course of 1 year, all three intensive psychotherapies were associated with more rapid recoveries (mean = 169 days) from bipolar depression in comparison with the recoveries of those assigned to CC (mean = 279 days). The rates of recovery were 64% for patients in intensive treatment (77% for FFT, 65% for interpersonal therapy, 60% for cognitive-behavioral therapy) and 52% for those in CC. Patients in the intensive treatments were also more likely to stay well during any given study month than were patients in CC. Differences among the three 30-session treatments were nonsignificant. The Systematic Treatment Enhancement Program concluded that intensive therapies developed in academic settings (including FFT) can be successfully exported to community settings in which clinicians have had minimal previous exposure to manual-based interventions.
TREATMENT MECHANISMS FOR FFT
The Miklowitz et al. (2003) trial identified two variables that mediated the effects of FFT on mania and depression, respectively: improvements in medication adherence and augmentation of positive family communication. Patients in FFT were more likely to adhere to lithium or anticonvulsant drug regimens than were patients in crisis management, and adherence was associated with less severe mania symptoms over the course of 2 years. Patient–relative interactions were more positively toned after FFT than they were after crisis management, and improvements in patient–relative interaction were correlated with improvements in depressive symptoms among patients over the course of 1 year. Negative communication did not change in either treatment condition. Thus, FFT may enhance the protective qualities of family relationships rather than directly reducing the frequency of criticisms or aversive patterns of family interaction.
CONCLUSIONS
Episodes of bipolar disorder are strongly associated with family discord, criticism, and conflict. There is increasing evidence that family psychoeducational treatments are effective in relapse prevention and symptom control when combined with standard drug treatment.
Much remains to be learned about the subpopulations of patients most likely to benefit from family interventions. It is not clear, for example, whether only patients with high-EE families should be given FFT, and whether patients who do not report significant family conflicts or who are disengaged from their families would be better suited to individual or group approaches. The mediating mechanisms by which family interventions achieve their effects—which may include enhancing medication adherence, family communication and problem-solving, or the family’s ability to recognize and intervene with early warning signs of recurrence—deserve further examination in randomized trials that measure mediators at systematically controlled intervals.
Longitudinal high-risk studies should clarify which family risk or protective processes operate among children who are genetically at risk for bipolar disorder. Specifically, investigators should identify early childhood temperamental or symptom attributes that bear a resemblance to manic or depressive symptoms (e.g., extreme moodiness or impulsiveness), clarify the circumstances under which these attributes evoke criticism or overprotectiveness among parents, and determine which of these children actually develop bipolar disorder in adulthood. It will be important in such studies to measure the psychiatric background of parents, as well as protective factors (e.g., a supportive secondary parent) that may reduce the likelihood that the child develops the disorder under conditions of high genetic risk.
Two uncontrolled treatment trials found that FFT alone or the combination of FFT and cognitive-behavioral therapy helped stabilize the course of bipolar disorder in adolescent and school-aged children, respectively (Miklowitz, Biuckians, & Richards, 2006; Pavuluri et al., 2004). Early preventative interventions involving the family are currently being developed (Miklowitz et al., 2006). Notably, teaching communication, problem-solving, and emotional self-regulation skills to at-risk children and their parents may help ameliorate stress within the family and contribute to delaying the onset of full manic episodes. Early-intervention studies involving high-risk populations should be a central focus for the next generation of research on bipolar disorder.
Acknowledgments
Preparation of this article was supported in part by National Institute of Mental Health Grant MH073871, a grant from the Robert Sutherland Foundation, and a Faculty Fellowship from the University of Colorado’s Council on Research and Creative Work.
Footnotes
Recommended Reading
Jamison, K.R. (1995). (See References)
Johnson, S.L., & Emery, R. (2003). (See References)
Miklowitz, D.J. (2002). (See References)
Miklowitz, D.J. & Goldstein, M.J. (1997). (See References)
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Barrowclough C, Hooley JM. Attributions and expressed emotion: A review. Clinical Psychology Review. 2003;23:849–880. doi: 10.1016/s0272-7358(03)00075-8. [DOI] [PubMed] [Google Scholar]
- Brown GW, Birley JLT, Wing JK. Influence of family life on the course of schizophrenic disorder. British Journal of Psychiatry. 1972;121:241–258. doi: 10.1192/bjp.121.3.241. [DOI] [PubMed] [Google Scholar]
- Hooley JM, Gruber SA, Scott LA, Hiller JB, Yurgelun-Todd DA. Activation in dorsolateral prefrontal cortex in response to maternal criticism and praise in recovered depressed and healthy control participants. Biological Psychiatry. 2005;57:809–812. doi: 10.1016/j.biopsych.2005.01.012. [DOI] [PubMed] [Google Scholar]
- Hooley JM, Parker HA. Measuring expressed emotion: An evaluation of the shortcuts. Journal of Family Psychology. 2006;20:386–396. doi: 10.1037/0893-3200.20.3.386. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Archives of General Psychiatry. 2002;59:530–537. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RMA, Petukhova M, Kessler RC. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Archives of General Psychiatry. 2007;64:543–552. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ. The role of family systems in severe and recurrent psychiatric disorders: A developmental psychopathology view. Development and Psychopathology. 2004;16:667–688. doi: 10.1017/s0954579404004729. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Biuckians A, Richards JA. Early-onset bipolar disorder: A family treatment perspective. Development and Psychopathology. 2006;18:1247–1265. doi: 10.1017/S0954579406060603. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, George EL, Richards JA, Simoneau TL, Suddath RL. A randomized study of family-focused psychoeducation and pharmacotherapy in the outpatient management of bipolar disorder. Archives of General Psychiatry. 2003;60:904–912. doi: 10.1001/archpsyc.60.9.904. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Johnson SL. The psychopathology and treatment of bipolar disorder. Annual Review of Clinical Psychology. 2006;2:199–235. doi: 10.1146/annurev.clinpsy.2.022305.095332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Wisniewski SR, Kogan JN, et al. Psychosocial treatments for bipolar depression: A 1-year randomized trial from the Systematic Treatment Enhancement Program. Archives of General Psychiatry. 2007;64:419–427. doi: 10.1001/archpsyc.64.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Wisniewski SR, Miyahara S, Otto MW, Sachs GS. Perceived criticism from family members as a predictor of the 1-year course of bipolar disorder. Psychiatry Research. 2005;136:101–111. doi: 10.1016/j.psychres.2005.04.005. [DOI] [PubMed] [Google Scholar]
- Murray CL, Lopez AD. The global burden of disease: A comprehensive assessment of mortality and disability from disease, injuries, and risk factors in 1990 projected to 2020. Boston: Harvard University Press; 1996. [Google Scholar]
- Pavuluri MN, Graczyk PA, Henry DB, Carbray JA, Heidenreich J, Miklowitz DJ. Child and family-focused cognitive behavioral therapy for pediatric bipolar disorder: Development and preliminary results. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:528–537. doi: 10.1097/00004583-200405000-00006. [DOI] [PubMed] [Google Scholar]
- Rea MM, Tompson M, Miklowitz DJ, Goldstein MJ, Hwang S, Mintz J. Family focused treatment vs. individual treatment for bipolar disorder: results of a randomized clinical trial. Journal of Consulting and Clinical Psychology. 2003;71:482–492. doi: 10.1037/0022-006x.71.3.482. [DOI] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–366. [PubMed] [Google Scholar]
- Rosenfarb IS, Goldstein MJ, Mintz J, Nuechterlein KH. Expressed emotion and subclinical psychopathology observable within the transactions between schizophrenic patients and their family members. Journal of Abnormal Psychology. 1995;104:259–267. doi: 10.1037//0021-843x.104.2.259. [DOI] [PubMed] [Google Scholar]
- Rosenfarb IS, Miklowitz DJ, Goldstein MJ, Harmon L, Nuechterlein KH, Rea MM. Family transactions and relapse in bipolar disorder. Family Process. 2001;40:5–14. doi: 10.1111/j.1545-5300.2001.4010100005.x. [DOI] [PubMed] [Google Scholar]


