Short abstract
The authors of this review discuss the changing role of vascular surgery and the impact of developments such as endovascular interventions and new techniques for treating varicose veins
Vascular surgery has come of age over the past two decades. The specialty has increasingly separated from general surgery as evidence accrues that outcomes for patients are better when arterial operations are done by a specialist.1 In the United Kingdom, this has meant an increasing number of consultant posts for purely vascular surgery being advertised. As a result of the expanding ageing population and historical under-provision of vascular intervention in the United Kingdom, vascular workload is expected to rise and the need for specialists will grow.2
Recognition of the multisystem nature of vascular disease has increased integration of vascular surgery into multidisciplinary teams of allied specialties. Surgical decisions are now often made jointly with the input of the renal physician, diabetologist, radiologist, cardiologist, neurologist, and specialist nurse. As a result, the role of the vascular surgeon as a sole player within hospital medicine is changing.
Sources and selection criteria
To identify emerging trends in vascular surgery, we searched Medline and the Cochrane database and discussed developments with surgical colleagues. We also reviewed published abstracts of presentations from the Vascular Surgical Society of Great Britain and Ireland, the European Society of Vascular and Endovascular Surgery, and the Society for Vascular Surgery (USA) in the past two years.
Abdominal aortic aneurysm
Endovascular aortic repair
Endovascular repair of abdominal aortic aneurysms was introduced a decade ago. This operation involves radiographically guided intraluminal placement of a prosthetic graft on a wire mesh into the abdominal aorta. This is done via a small groin incision, thus avoiding the morbidity and mortality associated with major open abdominal surgery. As with conventional repair, the goal of endovascular treatment is to prevent further expansion by excluding flow within the aneurysm, thus reducing the risk of rupture. As this method involves less perioperative blood loss and fewer cardiovascular complications, the recovery period is shorter.3 The procedure can be done under local anaesthetic.
Summary points
Vascular surgery is becoming a distinct specialty, with fewer general surgeons in the United Kingdom doing vascular procedures
Endovascular interventions are being used in all anatomical areas; although the relative merits are not yet clear, we will probably see a huge increase in endoluminal interventions in the near future
National randomised studies of abdominal aortic aneurysms and carotid stenting are being undertaken in the United Kingdom and will inform practice in the medium term
The multicentre aneurysm screening study proved that screening for abdominal aortic aneurysms in men aged over 65 is clinically beneficial and economically viable
Subintimal angioplasty will probably replace peripheral bypass surgery as first line treatment for ischaemia of the leg
Less invasive techniques are emerging to replace the standard procedure of flush ligation, stripping, and multiple avulsions used in the treatment of varicose veins
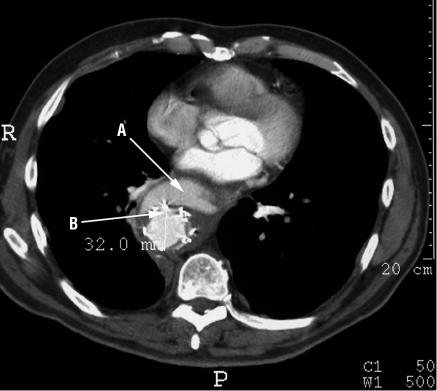
The shape of the aneurysm and its relation to other vessels determines suitability for endovascular repair and the type of graft used. However, recognised complications with endovascular repair make the technique controversial. These include graft movement within the aneurysm sac, fracture of the supporting wires, and, the most common problem, endoleak (fig 1). This is the continued pressurisation of the aneurysm sac by blood leaking outside the graft. Endoleak puts the patient at risk of aortic rupture. These problems mean that at least 10% of patients need further intervention in the first year after stent grafting.4
Fig 1.
Computed tomography scan of the thoracic aorta showing a stent graft (A) with an associated endoleak (B)
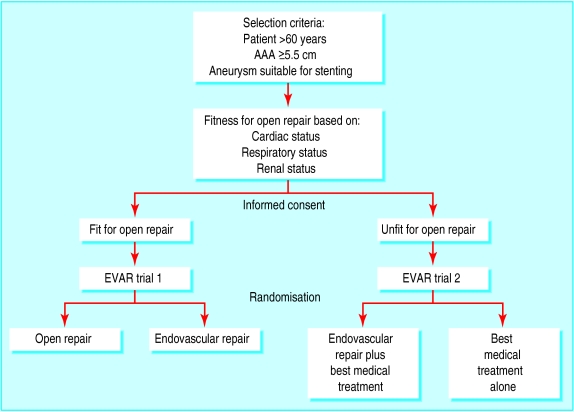
Two national multicentre randomised prospective trials are ongoing (fig 2). Endovascular aneurysm repair trial (EVAR) 1 and EVAR 2 started in 1999 and aim to define the role of endovascular surgery in the management of abdominal aortic aneurysms (table). EVAR 1 compares endovascular repair with standard open repair in patients considered fit enough for open repair. EVAR 2 compares endovascular repair combined with best medical treatment with best medical treatment alone in patients considered unfit for open repair.5 The results evaluating mortality, durability and safety, costs, and health related quality of life for patients with endovascular repair are awaited. Data published so far, however, have shown that endovascular services can be introduced into general hospitals in the United Kingdom, not only into referral centres.6 Other preliminary evidence has shown that an endovascular repair has a credible role for ruptured abdominal aortic aneurysms, as outcome may be superior to open repair with a reduction in perioperative mortality.7
Fig 2.
Trial protocol for endovascular aneurysm repair (EVAR) trials 1 and 2. AAA=abdominal aortic aneurysm
Table 1.
Recent and ongoing trials in vascular surgery
| Name of trial | Summary |
|---|---|
| Endovascular aneurysm repair trial 1 (EVAR 1) |
Compares endovascular repair with standard open repair in patients considered fit enough for open repair (results awaited) |
| Endovascular aneurysm repair trial 2 (EVAR 2) |
Compares endovascular repair combined with best medical treatment with best medical treatment alone in patients considered unfit for open repair (results awaited) |
| Multicentre aneurysm screening study (MASS) |
Showed that screening for abdominal aortic aneurysms in men over 65 is clinically beneficial and economically viable |
| Asymptomatic carotid atherosclerosis study (ACAS) |
Established that the long term risk of ipsilateral stroke in fit asymptomatic patients with a ≥60% carotid stenosis was reduced by carotid endarterectomy |
| Asymptomatic carotid surgery trial (ACST) |
Measured stroke-free survival time in patients with asymptomatic carotid stenosis (results awaiting publication) |
| Carotid and vertebral transluminal angioplasty study (CAVATAS) |
Compared carotid endarterectomy with endovascular treatment and reported a similar major risk and effectiveness for stenting and carotid endarterectomy |
| Stenting and angioplasty with protection in patients at high-risk for endarterectomy (SAPPHIRE) |
Interim findings show that outcomes for stenting are similar to those for carotid endarterectomy |
| Heart protection study (HPS) | Showed effectiveness of simvastatin 40 mg/day in reducing total mortality and cardiovascular mortality in patients with peripheral vascular disease |
Exciting advances have been made in the repair of the thoracic aorta with endovascular grafts (fig 3). Thoracic aortic aneurysms and thoracic dissections are conditions that are often managed conservatively, because of perceived poor outcome with conventional surgical reconstruction.8 The thoracic aorta is a “straight” tube (unlike the abdominal aorta, which has a bifurcation) and anatomically is very amenable to endovascular approaches. Endovascular repair may even have a role in the treatment of thoraco-abdominal aortic aneurysms, which have a high mortality for standard repair. Preliminary results from a series of operations at St Mary's Hospital, where open surgery was combined with endovascular stenting, have shown great potential, and information on long term outcome is eagerly awaited.9
Fig 3.
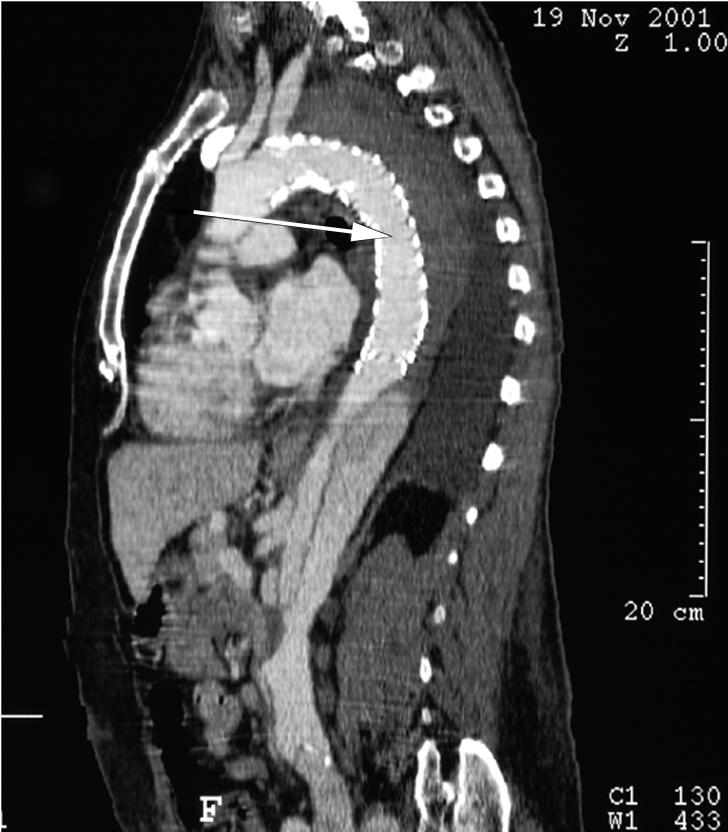
Sagittal computed tomography scan of thoracic stent graft
Screening
Until rupture occurs, most abdominal aortic aneurysms are asymptomatic. Rupture is estimated to have 85% mortality and causes 2% of deaths in men over the age of 65 in the United Kingdom.10,11 As an accessible, sensitive, and specific test is available for detecting abdominal aortic aneurysms (ultrasound can detect an aneurysm in 99% of cases), screening may be of value.12 Surgery for standard elective repair carries a mortality of 6%, after which life expectancy returns to near normal.13 The results of a United Kingdom based, multicentre randomised controlled trial—the multicentre aneurysm screening study—showed a clinical benefit from screening with ultrasound scanning.10 In the screened arm of the trial, comprising 33 839 men, 47 fewer deaths occurred than in the control arm. Overall, screening decreased the risk of dying from a ruptured aneurysm by 42%. A secondary endpoint, the quality of life of participants who had an aneurysm detected, was unchanged. In addition, the cost effectiveness of screening for abdominal aortic aneurysms was calculated to be at the margin of acceptability according to current thresholds (comparable to breast screening) and would improve with time.14 A separate trial showed no clinical indication or economic viability for screening women for abdominal aortic aneurysm.15
Estimates indicate that the annual cost of a screening programme for abdominal aortic aneurysms in the United Kingdom would be less than £15 million, falling to £5 million within 10 years.11 This means that screening for abdominal aortic aneurysms is likely to be cheaper than existing screening programmes.16
When is carotid endarterectomy effective?
When to do a carotid endarterectomy is a controversial question among vascular surgeons; practices vary in different countries. Large multicentre trials show that surgery for high grade carotid stenoses is beneficial in patients with symptoms.17 Patients who have transient ischaemic attacks will benefit greatly from carotid endarterectomy (the risk of stroke is greatest in the weeks after an attack); however, death due to the complications of ischaemic heart disease is the most common outcome in patients with transient ischaemic attacks.18
In the patients with atherosclerotic disease, examination of the carotid arteries is of prime importance. A duplex scan is suitable, and a carotid endarterectomy can be done based solely on the findings of a duplex scan.19 The most contentious question, however, is whether to operate on asymptomatic patients.
The North American asymptomatic carotid atherosclerosis study established that the long term risk of ipsilateral stroke in fit asymptomatic patients with a ≥ 60% carotid stenosis was reduced by carotid endarterectomy.20 Following this, the European asymptomatic carotid surgery trial was set up to measure stroke-free survival time in patients with asymptomatic carotid stenosis.21 It compared the outcome of carotid endarterectomy done in conjunction with best medical treatment with that of best medical treatment alone. Preliminary results indicate that patients with high grade asymptomatic carotid stenosis should be operated on.
Carotid angioplasty and stenting
A minimally invasive alternative to carotid endarterectomy is angioplasty and stenting of a carotid stenosis. However, this carries risks, particularly of cerebrovascular damage secondary to thromboemboli. A randomised controlled trial—the carotid and vertebral transluminal angioplasty study—compared carotid endarterectomy with endovascular treatment. It reported a similar rate of adverse events for stenting and carotid endarterectomy, although the risk of stroke with surgery was unusually high in this study compared with other studies in the literature.22 Findings from another trial—the stenting and angioplasty with protection in patients at high-risk for endarterectomy study—recently showed that outcomes are similar (verbal report, AHA, 19 November 2002).
The use of distal cerebral protection devices is becoming widespread during stenting. These devices are used to prevent plaque debris entering the cerebral circulation, and preliminary studies have shown them to be effective at decreasing postoperative morbidity in the short term.23,24 Furthermore, variation in carotid atherosclerotic plaque morphology has been shown to change plaque susceptibility to distal embolisation and subsequent complications.25 Also, duplex characterisation of carotid plaque preoperatively may determine the risk of cerebral complications during carotid endovascular intervention.26
Arterial disease in the leg
Most patients with lower limb arterial disease are treated conservatively and do not reach the stage at which surgical intervention is needed. The heart protection study clearly showed the benefit of statin (simvastatin 40 mg once daily) treatment for patients with peripheral arterial disease; apart from improving peripheral vascular symptoms, it reduced coronary events by 20%.27,28 For patients with severe ischaemia, peripheral arterial bypass surgery improves walking distance and quality of life significantly over other approaches.29,30
Minimally invasive techniques are now available to treat lower limb ischaemia. Subintimal angioplasty is a radiological technique in which the angioplasty guide wire enters the extraluminal (subintimal) space within the vessel wall and dissection is done with radiographic guidance. The angioplasty balloon is then inflated within this subintimal space. This redirects the blood flow inside the wall of the artery, bypassing the occlusion, and back into the lumen beyond, leaving the atheroma core in situ with a new channel created around it. The procedure carries a low risk of complications and has a high initial technical success rate.31 It is used chiefly for long femoral and popliteal artery occlusions in which an intraluminal angioplasty guide wire cannot be passed. Although short term patency rates are excellent, long term patency is not as good as with bypass surgery.32 The technique may, however, have an important role as first line treatment for patients with both claudication and limb threatening ischaemia and those deemed unfit for surgery.
In some centres, endovascular stents have been used to improve patency after angioplasty in patients with peripheral arterial insufficiency. Often a stent is implanted if the angioplasty result is suboptimal or an arterial dissection occurs or for a restenosis. However, results of short term and long term follow up differ in the literature; overall, stents seem to have little role in treating peripheral arterial disease.33
New treatments for varicose veins
Varicose veins are present in up to 40% of the population and are a common indication for surgical intervention, now often done as a day case procedure.34,35 Alternatives to the current operative techniques are being introduced to avoid the need for general anaesthesia and to improve cosmetic outcome. Endovenous obliteration using radiofrequency (diathermy) or laser has been devised to close the long saphenous vein, an alternative to the traditional “stripping.” Another new technique that obviates the need for multiple “phlebectomies” to avulse calf varicosities, thus giving a more cosmetically favourable outcome, is “powered phlebectomy.” This minimally invasive approach uses an illuminator under the skin to accurately target the vein, which is removed by suction under direct vision (fig 4). This leaves the patient without multiple stab incision scars and potentially lowers the risk of postoperative infection.36 Trials show that both these novel techniques are acceptable alternative treatments.37,38
Fig 4.

Transilluminated powered phlebectomy, showing resector and illuminator placed under the skin either end of the varicosity
Additional educational resources
Books
Donnelly R, London NJM. ABC of vascular surgery. London: BMJ Publishing, 2001
Beard J, Gaines P. Vascular and endovascular surgery. 2nd ed. London: W B Saunders, 2001
Selected papers
Endovascular versus surgical treatment in patients with carotid stenosis in the carotid and vertebral artery transluminal angioplasty study (CAVATAS): a randomised trial. Lancet 2001;357: 1729-37
Cusi C, Candelise L. Is carotid endarterectomy effective and safe in asymptomatic patients with carotid stenosis? Neuroepidemiology 2003;22: 153-4
Ashton HA, Buxton MJ, Day NE, Kim LG, Marteau TM, Scott RA, et al. The multicentre aneurysm screening study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial. Lancet 2002;360: 1531-9
Cheshire N, Elias SM, Keagy B, Kolvenbach R, Leahy AL, Marston W, et al. Powered phlebectomy (TriVex) in treatment of varicose veins. Ann Vasc Surg 2002;16: 488-94
Websites for doctors
European Journal of Vascular and Endovascular Surgery (www.elsevierhealth.com/journals/ejvs)—official journal of the European Society of Vascular Surgery
Journal of Vascular Surgery (www.sciencedirect.com/science/journal/07415214)—provides recent information on vascular surgery for vascular, cardiothoracic, and general surgeons
National Coordinating Centre for Health Technology Assessment (www.ncchta.org)—coordinates the health technology assessment programme under contract from the Department of Health's research and development division
Surgery (www.medicinepublishing.co.uk)—monthly journal that builds into an updated textbook of surgical practice
Websites for patients
Veins1 (www.veins1.com)—source of information on vein care for patients
American College of Phlebology (www.phlebology.org/brochure.htm)—source of the latest information on phlebology for patients and health professionals
Vascular Disease Foundation (www.vdf.org)—information on all aspects of vascular disease
Health World (healthy.net/library/Books/Healthyself/varicoseveins.htm)—tips on self care for varicose veins
What the future holds
Data from the United Kingdom Office for National Statistics indicate that the number of people aged 60 and over will rise from 12 million in 2001 to 18.6 million in 2031. During this period, the number of people with chronic diseases and disabilities will increase threefold.39 The shifting face of vascular surgery reflects the needs of an increasingly frail elderly population. These changes have important consequences for vascular specialist training and the number of trainees entering the field. Important political considerations also exist; many of the “endovascular” techniques described above are not currently used by vascular surgeons but rather by cardiologists and interventional radiologists. This alters the dynamics not just of vascular specialist training and training post numbers but also between medical specialties and ultimately the provision of vascular services. In the near future, vascular surgeons will need to learn these skills. They will have to work alongside colleagues with similar interests in order to provide appropriate care for the changing population.
The question of a “turf war” between vascular surgeons and allied specialties is a frequent topic for discussion at vascular meetings throughout the United Kingdom, but the answer may not be as controversial or as difficult as at first thought. This is because not all general or vascular surgeons wish to convert wholly to vascular or endoluminal practice. Moreover, interventional radiologists have many other areas of clinical practice, including a growing endo-urological commitment and combined hepatobiliary and upper gastrointestinal work with gastroenterologists. In addition, rates of intervention for many arterial procedures are much lower in the United Kingdom than in northern Europe or North America. Thus the United Kingdom will probably need a combined and sustained “effort” from vascular surgeons and radiologists working together if the new endoluminal revolution is to provide sufficient intervention for the increasing ageing population.
Contributors: Authors contributed equally to researching and writing the review.
Competing interests: None declared.
References
- 1.Tu JV, Austin PC, Johnston KW. The influence of surgical specialty training on the outcomes of elective abdominal aortic aneurysm surgery. J Vasc Surg 2001;33: 447-52. [DOI] [PubMed] [Google Scholar]
- 2.Stanley JC, Barnes RW, Ernst CB, Hertzer NR, Mannick JA, Moore WS. Vascular surgery in the United States: workforce issues. Report of the Society for Vascular Surgery and the International Society for Cardiovascular Surgery, North American Chapter, Committee on Workforce Issues. J Vasc Surg 1996;23: 172-81. [DOI] [PubMed] [Google Scholar]
- 3.Jordan WD, Alcocer F, Wirthlin DJ, Westfall AO, Whitley D. Abdominal aortic aneurysms in “high-risk” surgical patients: comparison of open and endovascular repair. Ann Surg 2003;237: 623-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laheij RJ, Buth J, Harris PL, Moll FL, Stelter WJ, Verhoeven EL. Need for secondary interventions after endovascular repair of abdominal aortic aneurysms: intermediate-term follow-up results of a European collaborative registry (EUROSTAR). Br J Surg 2000;87: 1666-73 [DOI] [PubMed] [Google Scholar]
- 5.Greenhalgh RM, Brown LC. Status of the UK randomized EVAR trials in standard. risk and high risk patient groups: will they yield answers? 29th Global Conference in Vascular and Endovascular Issues, Techniques and Horizons, New York, November 2002: Abstract XVI.
- 6.Karkos CD, Vimalachandran D, Lavelle JM, Wilson P, Abraham JS. Endovascular abdominal aortic aneurysm repair outside a tertiary referral centre: feasibility and impact upon workload. Cardiovasc Surg 2003;11: 6-11. [DOI] [PubMed] [Google Scholar]
- 7.Hinchliffe RJ, Braithwaite BD, Hopkinson BR. The endovascular management of ruptured abdominal aortic aneurysms. Eur J Vasc Endovasc Surg 2003;25: 191-201. [DOI] [PubMed] [Google Scholar]
- 8.Criado FJ, Clark NS, Barnatan MF. Stent graft repair in the aortic arch and descending thoracic aorta: a 4-year experience. J Vasc Surg 2002;36: 1121-8. [DOI] [PubMed] [Google Scholar]
- 9.Robless P, Cheshire N, Kerle M, Cowling M, Clark M, Wolfe J. Combined endovascular and open surgical techniques in the treatment of complex thoraco-abdominal aortic aneurysms. Br J Surg 2003;90(suppl 1).
- 10.Ashton HA, Buxton MJ, Day NE, Kim LG, Marteau TM, Scott RA, et al. The multicentre aneurysm screening study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial. Lancet 2002;360: 1531-9. [DOI] [PubMed] [Google Scholar]
- 11.Beard JD. Screening for abdominal aortic aneurysm. Br J Surg 2003;90: 515-6. [DOI] [PubMed] [Google Scholar]
- 12.Lindholt JS, Vammen S, Juul S, Henneberg EW, Fasting H. The validity of ultrasonographic scanning as screening method for abdominal aortic aneurysm. Eur J Vasc Endovasc Surg 1999;17: 472-5. [DOI] [PubMed] [Google Scholar]
- 13.UK Small Aneurysm Trial Participants. Mortality results for randomised controlled trial of early elective surgery or ultrasonographic surveillance for small abdominal aortic aneurysms. Lancet 1998;352: 1649-55. [PubMed] [Google Scholar]
- 14.Multicentre Aneurysm Screening Study Group. Multicentre aneurysm screening study (MASS): cost effectiveness analysis of screening for abdominal aortic aneurysms based on four year results from randomised controlled trial. BMJ 2002;325: 1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scott RA, Bridgewater SG, Ashton HA. Randomised clinical trial of screening for abdominal aortic aneurysm in women. Br J Surg 2002;89: 283-5. [DOI] [PubMed] [Google Scholar]
- 16.Lee TY, Korn P, Heller JA, Kilaru S, Beavers FP, Bush HL, et al. The cost-effectiveness of a “quick-screen” program for abdominal aortic aneurysms. Surgery 2002;132: 399-407 [DOI] [PubMed] [Google Scholar]
- 17.Rothwell PM, Gutnikov SA, Warlow CP, European Carotid Surgery Trialist's Collaboration. Reanalysis of the final results of the European carotid surgery trial. Stroke 2003;34: 514-23. [DOI] [PubMed] [Google Scholar]
- 18.Hennessy MJ, Britton TC. Transient ischaemic attacks: evaluation and management. Int J Clin Pract 2000;54: 432-6. [PubMed] [Google Scholar]
- 19.Logason K, Karacagil S, Hardemark HG, Bostrom A, Hellberg A, Ljungman C. Carotid artery endarterectomy solely based on duplex scan findings. Vasc Endovascular Surg 2002;36: 9-15. [DOI] [PubMed] [Google Scholar]
- 20.Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. Endarterectomy for asymptomatic carotid artery stenosis. JAMA 1995;273: 1421-8. [PubMed] [Google Scholar]
- 21.Halliday AW, Thomas D, Mansfield A. The asymptomatic carotid surgery trial (ACST): rationale and design. Eur J Vasc Surg 1994;8: 703-10 [DOI] [PubMed] [Google Scholar]
- 22.Endovascular versus surgical treatment in patients with carotid stenosis in the carotid and vertebral artery transluminal angioplasty study (CAVATAS): a randomised trial. Lancet 2001;357: 1729-37. [PubMed] [Google Scholar]
- 23.Angelini A, Reimers B, Della Barbera M, Sacca S, Pasquetto G, Cernetti C, et al. Cerebral protection during carotid artery stenting: collection and histopathologic analysis of embolized debris. Stroke 2002;33: 456-61. [DOI] [PubMed] [Google Scholar]
- 24.Reimers B, Corvaja N, Moshiri S, Sacca S, Albiero R, Di Mario C, et al. Cerebral protection with filter devices during carotid artery stenting. Circulation 2001;104: 12-5. [DOI] [PubMed] [Google Scholar]
- 25.Bicknell CD, Cheshire NJ. The relationship between carotid atherosclerotic plaque morphology and the embolic risk during endovascular therapy. Eur J Vasc Endovasc Surg 2003;26: 17-21. [DOI] [PubMed] [Google Scholar]
- 26.Biasi GM, Ferrari SA, Nicolaides AN, Mingazzini PM, Reid D. The ICAROS registry of carotid artery stenting: imaging in carotid angioplasties and risk of stroke. J Endovasc Ther 2001;8: 46-52. [DOI] [PubMed] [Google Scholar]
- 27.Burns P, Lima E, Bradbury AW. What constitutes best medical therapy for peripheral arterial disease? Eur J Vasc Endovasc Surg 2002;24: 6-12. [DOI] [PubMed] [Google Scholar]
- 28.Collins R, Peto R, Armitage J. The MRC/BHF heart protection study: preliminary results. Int J Clin Pract 2002;56: 53-6. [PubMed] [Google Scholar]
- 29.Gelin J, Jivegard L, Taft C, Karlsson J, Sullivan M, Dahllof AG, et al. Treatment efficacy of intermittent claudication by surgical intervention, supervised physical exercise training compared to no treatment in unselected randomised patients I: one year results of functional and physiological improvements. Eur J Vasc Endovasc Surg 2001;22: 107-13. [DOI] [PubMed] [Google Scholar]
- 30.Taft C, Karlsson J, Gelin J, Jivegard L, Sandstrom R, Arfvidsson D, et al. Treatment efficacy of intermittent claudication by invasive therapy, supervised physical exercise training compared to no treatment in unselected randomised patients II: one-year results of health-related quality of life. Eur J Vasc Endovasc Surg 2001;22: 114-23. [DOI] [PubMed] [Google Scholar]
- 31.Tisi PV, Mirnezami A, Baker S, Tawn J, Parvin SD, Darke SG. Role of subintimal angioplasty in the treatment of chronic lower limb ischaemia. Eur J Vasc Endovasc Surg 2002;24: 417-22. [DOI] [PubMed] [Google Scholar]
- 32.Laxdal E, Jenssen GL, Pedersen G, Aune S. Subintimal angioplasty as a treatment of femoropopliteal artery occlusions. Eur J Vasc Endovasc Surg 2003;25: 578-82 [DOI] [PubMed] [Google Scholar]
- 33.Bachoo P, Thorpe P. Endovascular stents for intermittent claudication. Cochrane Database Syst Rev 2003;(1): CD003228. [DOI] [PubMed]
- 34.Golledge J, Quigley FG. Pathogenesis of varicose veins. Eur J Vasc Endovasc Surg 2003;25: 319-24. [DOI] [PubMed] [Google Scholar]
- 35.Dimakakos P, Vlahos L, Papadimitriou J. Surgery of varicose veins on ambulatory basis: early and late results. Int Surg 1995;80: 267-70. [PubMed] [Google Scholar]
- 36.Arumugasamy M, McGreal G, O'Connor A, Kelly C, Bouchier-Hayes D, Leahy A. The technique of transilluminated powered phlebectomy—a novel, minimally invasive system for varicose vein surgery. Eur J Vasc Endovasc Surg 2002;23: 180-2. [DOI] [PubMed] [Google Scholar]
- 37.Sybrandy JE, Wittens CH. Initial experiences in endovenous treatment of saphenous vein reflux. J Vasc Surg 2002;36: 1207-12. [DOI] [PubMed] [Google Scholar]
- 38.Cheshire N, Elias SM, Keagy B, Kolvenbach R, Leahy AL, Marston W, et al. Powered phlebectomy (TriVex) in treatment of varicose veins. Ann Vasc Surg 2002;16: 488-94. [DOI] [PubMed] [Google Scholar]
- 39.Khaw KT. How many, how old, how soon? BMJ 1999;319: 1350-2. [DOI] [PMC free article] [PubMed] [Google Scholar]