Abstract
Background and purpose:
Pharmacological inhibition of beta-amyloid (Aβ) induced reactive gliosis may represent a novel rationale to develop drugs able to blunt neuronal damage and slow the course of Alzheimer's disease (AD). Cannabidiol (CBD), the main non-psychotropic natural cannabinoid, exerts in vitro a combination of neuroprotective effects in different models of Aβ neurotoxicity. The present study, performed in a mouse model of AD-related neuroinflammation, was aimed at confirming in vivo the previously reported antiinflammatory properties of CBD.
Experimental approach:
Mice were inoculated with human Aβ (1–42) peptide into the right dorsal hippocampus, and treated daily with vehicle or CBD (2.5 or 10 mg kg−1, i.p.) for 7 days. mRNA for glial fibrillary acidic protein (GFAP) was assessed by in situ hybridization. Protein expression of GFAP, inducible nitric oxide synthase (iNOS) and IL-1β was determined by immunofluorescence analysis. In addition, ELISA assay of IL-1β level and the measurement of NO were performed in dissected and homogenized ipsilateral hippocampi, derived from vehicle and Aβ inoculated mice, in the absence or presence of CBD.
Key results:
In contrast to vehicle, CBD dose-dependently and significantly inhibited GFAP mRNA and protein expression in Aβ injected animals. Moreover, under the same experimental conditions, CBD impaired iNOS and IL-1β protein expression, and the related NO and IL-1β release.
Conclusion and implications:
The results of the present study confirm in vivo anti-inflammatory actions of CBD, emphasizing the importance of this compound as a novel promising pharmacological tool capable of attenuating Aβ evoked neuroinflammatory responses.
Keywords: cannabidiol, Aβ, reactive gliosis, GFAP, IL-1β, iNOS, mice
Introduction
Alzheimer's disease (AD) is the most common age-related neurodegenerative disorder (Koo et al., 1999) whose specific hallmarks are neurofibrillary tangles (Terry, 1963) and senile plaques (Braak and Braak, 1997). While neurofibrillary tangles result from the deposition of hyperphosphorylated tau proteins (Lee et al., 1991), senile plaques represent more complex extracellular lesions composed of a core of β-amyloid (Aβ) aggregates, surrounded by activated astrocytes and dystrophic neuritis (Itagaki et al., 1989; Cotman et al., 1996). At present, although biochemical events leading to Aβ neurotoxicity still remain unclear, proposed mechanisms include production of oxygen free radicals (Behl et al., 1994), changes in cytosolic calcium homeostasis (Ueda et al., 1997; Mattson, 2002) and activation of Wnt pathway as well as of the transcription nuclear factor NF-κB (Green and Peers, 2002; Caricasole et al., 2003). In addition to cytotoxic mechanisms directly affecting neurons, Aβ-induced glial cell activation, triggering inflammatory responses with subsequent release of neurotoxic cytokines, is present in the AD brain, contributing to the pathogenesis of disease (Craft et al., 2006). The possibility of interfering with this detrimental cycle by pharmacologically inhibiting reactive gliosis has been proposed as a novel rationale to develop drugs able to blunt neuronal damage and consequently slow the course of disease.
Cannabidiol (CBD), the main non-psychotropic component of the glandular hairs of Cannabis sativa, exhibits a plethora of actions including anti-convulsive, sedative, hypnotic, anti-psychotic, anti-nausea, anti-inflammatory and anti-hyperalgesic properties (Mechoulam et al., 2002; Costa et al., 2007). CBD has been proved to exert in vitro a combination of neuroprotective effects in Aβ-induced neurotoxicity, including anti-oxidant and anti-apoptotic effects (Iuvone et al., 2004), tau protein hyperphosphorylation inhibition through the Wnt pathway (Esposito et al., 2006a), and marked decrease of inducible nitric oxide synthase (iNOS) protein expression and nitrite production in Aβ-challenged differentiated rat neuronal cells (Esposito et al., 2006b).
In spite of the large amount of data describing the significant neuroprotective and anti-inflammatory properties of CBD in vitro, to date no evidence has been provided showing similar effects in vivo. To achieve this, the present study investigated the potential anti-inflammatory effect of CBD in a mouse model of AD-related neuroinflammation induced by the intrahippocampal injection of the human Aβ (1–42) fragment.
Methods
Animal care
Experiments were conducted in 3–5-months old C57BL/6J mice (35–40 g) (Harlan, Udine, Italy). Animals were housed under controlled illumination (12 h light/12 h dark cycle; light on 0600h) and standard environmental conditions (ambient temperature 20–22°C, humidity 55–60%) for at least 1 week before starting experiments. Food and water were available ad libitum. All surgery and experimental procedures were performed during the light cycle and were made according to the National Institutes of Health guidelines for the care and use of laboratory animals and to those of the Italian Ministry of Health (DL 116/92), and were approved by the local Institutional Animal Care and Use Committees. All efforts were made to reduce both animal number and suffering during the experiments.
Surgical preparation
Mice were anaesthetized with halothane (1–3%), placed in a stereotaxic frame, and injected with 10 ng of Aβ (1–42) (Tocris Cookson, Bristol, UK) or vehicle artificial cerebrospinal fluid (aCSF) into the right dorsal hippocampus, using the following coordinates relative to the bregma: AP=+2.0 mm; ML=−1.8 mm; DV=−2.3 mm. The flow was maintained at a constant value of 0.5 μl min−1, using a microdialysis pump and the needle was left in place for additional 5 min to allow for diffusion. Animals were kept on a warming pad until they had fully recovered from the anaesthetic and were kept in individual cages to prevent damage to the scalp sutures until they were killed for tissue processing.
Starting on the third day after surgery, mice were intraperitoneally (i.p.) treated daily with vehicle (Tocrisolve 100, Tocris Cookson) or CBD (Tocris Cookson) (2.5 or 10 mg kg−1) for 7 days. The doses of the drug were selected according to previous literature (Mechoulam et al., 2002), whereas the i.p. administration route was derived from the author's experience in such animal model of AD. Animals for in situ hybridization analysis were killed by cervical dislocation and brain were removed, snap-frozen on dry-ice, and stored at −80°C. Brains were mounted on Tissue Tek (Polysciences, PA, USA), and 14-μm-thick coronal sections were cut on a cryostat Microtome HM560 (Microm, Walldorf, Germany). Sections were mounted onto frozen SuperFrost/Plus slides (Fisher Scientific, Schwerte, Germany), dried on a 42°C warming plate, and stored at −20°C until used. Animals for immunofluorescence analysis were killed and perfused with HEPES buffer containing protease inhibitors; brains were rapidly frozen in liquid N2. Tissue was cut on a freezing sliding microtome (Leica SM 2000 R, Milan, Italy) to obtain 30 μm sections collected in a 15 mM NaN3 phosphate-buffered saline (PBS) solution and stored at 4°C. For enzyme-linked immunosorbent assay (ELISA) experiments brains were bisected down the sagittal sulcus and the hippocampus was dissected out of the right side and quickly frozen in liquid N2.
In situ hybridization
Sections were fixed in ice-cold 4% paraformaldehyde for 20 min, rinsed in PBS, quenched for 15 min in 1% H2O2 methanol solution, rinsed in PBS, quenched for 8 min in 0.2 M HCl, rinsed in PBS, treated with proteinase K 20 μg ml−1 (Roche Molecular Diagnostics, Milan, Italy) in 50 mM Tris-HCl, 5 mM ethylene diamine tetra acetic acid (EDTA) (pH 8.0) for 10 min, rinsed in PBS, fixed in ice-cold 4% paraformaldehyde, incubated for 10 min in 0.1 M triethanolamine (pH 8.0) to which 1.2 ml acetic anhydride was added dropwise, rinsed in PBS, washed with 0.9% NaCl for 5 min, dehydrated in graded series of ethanol and air-dried. Hybridization was carried out in 100 μl of hybridization buffer containing specific sense or antisense 35S-labelled riboprobe for glial fibrillary acidic protein (GFAP; 70 000–100 000 c.p.m. μl−1). Hybridization buffer consisted of 50% deionized formamide, 20 mM Tris-HCl (pH 8.0), 0.3 M NaCl, 5 mM EDTA (pH 8.0), 10% dextran sulphate (Sigma, Milan, Italy), 0.02% Ficoll 400 (Sigma), 0.02% polyvinylpyrrolidone (PVP 40; Sigma), 0.02% bovine serum albumin (BSA; Sigma), 0.5 mg ml−1 tRNA (Roche Molecular Diagnostics), 0.2 mg ml−1 fragmented herring sperm DNA and 200 mM dithiothreitol. Before applying to the tissue the hybridization cocktail was denatured for 2 min at 95°C. Slides were incubated overnight at 54°C in a humidified chamber. Four high-stringency washes were carried out at 62°C with 5 × saline sodium citrate (SSC)/0.05% Tween-20 (Sigma), then with 50% formamide/2 × SSC/0.05% Tween-20, with 50% formamide/1 × SSC/0.05% Tween-20 and finally with 0.1 × SSC/0.05% Tween-20. Slides were dehydrated in graded ethanol series, air-dried and exposed to Biomax MR film (Scientific Imaging Systems, NY, USA). GFAP mRNA expression was semi-quantified by densitometric scanning of the Biomax film with a GS 700 imaging densitometer (Bio-Rad Laboratories, CA, USA) and a computer programme (Molecular Analyst, IBM, Milan, Italy).
Immunofluorescence
Brain coronal sections (30 μm) were fixed for 30 min in 4% paraformaldehyde, washed with PBS, and blocked for 15 min with 10% BSA. Sections were then incubated for 2 h with one of the following primary antibodies: monoclonal anti-GFAP (1:200, Lab Vision, CA, USA), monoclonal anti-IL-1β (1:100, Sigma) and monoclonal anti-iNOS (1:100, Sigma). Following PBS washing, sections were incubated in the dark for half an hour with Texas Red-conjugated or fluorescein isothiocyanate (FITC)-conjugated secondary antibody (1:200; AbCam, Cambridge, UK). After final PBS washing, sections were analysed with a Zeiss LSM 410 microscope equipped with a krypton/argon laser, dichroic beam splitters and barrier emission filters needed for triple labelling. Texas Red was excited at a wavelength of 568 nm and collected through a long pass filter (590LP). FITC was excited with a wavelength of 488 nm and collected with a narrow band filter (515–540BP). Texas Red and FITC were assigned to the red and green channels respectively of the generated RGB image.
Nitrite assay
NO was measured as nitrite (NO2−) accumulated in the inoculated ipsilateral hippocampi. A spectrophotometer assay based on the Griess reaction was used (Di Rosa et al., 1990). Briefly, Griess reagent (1% sulphanilamide, 0.1% naphthylethylenediamine in H3PO4) was added to an equal volume of homogenized tissue supernatant and the absorbance at 550 nm was measured after 10 min. The NO2− concentration was thus determined using a standard curve of NaNO2 and referred to μg of homogenized hippocampal protein content according to BioRad assay method.
IL-1β assay
ELISA was used to quantify the presence of IL-1β in the supernatant of homogenized hippocampi ipsilateral to the inoculation site. A mouse IL-1β ELISA kit (R&D System, MN, USA) was used according to the manufacturer's recommendations. Briefly, 50 μl of standard, control buffer, or sample was combined with 50 μl of assay buffer in IL-1β antibody-coated wells on the ELISA plate and incubated at room temperature for 2 h. Wells were washed five times before the addition of 100 μl of the appropriate horseradish peroxidase conjugate and incubated for 2 h more. After a second wash cycle, 100 μl of hydrogen peroxide/tetramethylbenzidine substrate solution was added per well, and the plate was incubated for 30 min at room temperature in the dark. The reaction was stopped by addition of the hydrochloric acid solution provided in the kit. The absorbance at 450 nm was measured with a microreader (Bio-Rad Laboratories, 3550-UV) with wavelength correction at 570 nm.
Statistical analysis
Results were expressed as mean±s.e.m. of experiments. Statistical analysis was performed using analysis of variance, and multiple comparisons were performed by Bonferroni's test, with P<0.05 considered significant.
Results
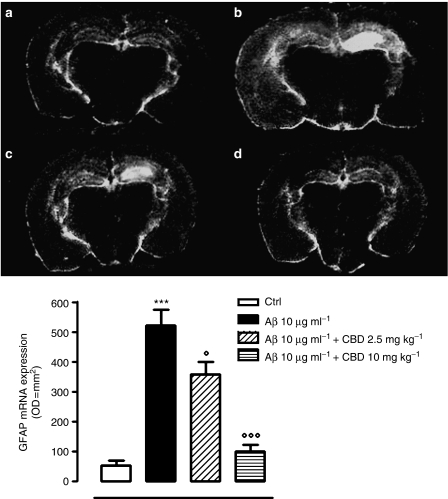
CBD effects on GFAP mRNA expression in Aβ inoculated mice
The induction of mRNA for GFAP protein 10 days following intrahippocampal injection of Aβ (1–42) (10 μg ml−1) was examined. As shown in Figure 1, GFAP mRNA, as measured by densitometry, was significantly increased by Aβ treatment in comparison with mice hippocampi injected with vehicle (+883±12%). CBD (2.5 or 10 mg kg−1) dose-dependently and significantly inhibited (−31.3±4.1 and −81±6.7% respectively) GFAP mRNA expression versus Aβ-injected animals i.p. treated with vehicle. Negligible or no increase in GFAP mRNA was observed following treatment with Aβ (42–1) reverse peptide or CBD alone (data not shown).
Figure 1.
Effects of cannabidiol (CBD) (intraperitoneal (i.p.) treatment for 7 consecutive days) on glial fibrillary acidic protein (GFAP) mRNA in mouse hippocampus. Upper panel: Dark-field photomicrographs showing the distribution of GFAP mRNA as detected by in situ hybridization in (a) vehicle-inoculated mice (control), (b) Aβ inoculated mice, (c) Aβ inoculated and cannabidiol (CBD) (2.5 mg kg−1) i.p. treated mice, (d) Aβ inoculated and CBD (10 mg kg−1) i.p. treated mice. Lower panel: Quantification of GFAP mRNA by densitometry. Data are shown as mean±s.e.m. of five experiments. ***P<0.001 versus control; °P<0.05 and °°°P<0.001 versus Aβ inoculated mice.
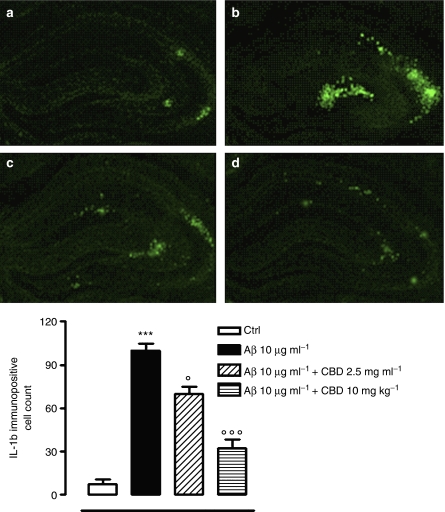
CBD effects on GFAP, iNOS and IL-1β protein expression in Aβ inoculated mice
Immunofluorescence analysis was aimed at estimating the effect of CBD treatment on the expression of inflammatory proteins 10 days following Aβ (1–42) (10 μg ml−1) injection into mouse hippocampi. As shown in Figures 2, 3 and 4, the number of GFAP, iNOS and IL-1β-positive cells was significantly increased by Aβ (+407±34, +1025±68, and +1288±16% respectively) versus vehicle-inoculated hippocampi. CBD (2.5 or 10 mg kg−1) treatment dose-dependently and significantly inhibited the number of cells positive for GFAP (−30±3.12 and −64.14±6.2% respectively), iNOS (−33.3±5.2 and −61.5±4.25% respectively) or IL-1β (−30.5±5.7 and −68±4.23% respectively), in comparison with animals given Aβ and injected with CBD vehicle. Also in this case, negligible or no increase in GFAP, iNOS and IL-1β was observed following treatment with Aβ (42–1) reverse peptide or CBD alone (data not shown).
Figure 2.
Effects of cannabidiol (CBD) (intraperitoneal (i.p.) treatment for 7 consecutive days) on glial fibrillary acidic protein (GFAP) in mouse hippocampus. Upper panel:Representative photomicrographs showing GFAP immunoreactive cells in: (a) vehicle inoculated mice (control), (b) Aβ inoculated mice, (c) Aβ inoculated and CBD (2.5 mg kg−1) i.p. treated mice, (d) Aβ inoculated and CBD (10 mg kg−1) i.p. treated mice. Lower panel: Quantification of immunoreactivity expressed as the number of cells immunostained with anti-GFAP antibody. Data are shown as mean±s.e.m. of five experiments. ***P<0.001 versus control; °P<0.05, and °°°P<0.001 versus Aβ inoculated mice.
Figure 3.
Effects of cannabidiol (CBD) (intraperitoneal (i.p.) treatment for 7 consecutive days) on inducible nitric oxide synthase (iNOS) in mouse hippocampus. Upper panel: Representative photomicrographs showing iNOS immunoreactive cells in: (a) vehicle inoculated mice (control), (b) Aβ inoculated mice, (c) Aβ inoculated and CBD (2.5 mg kg−1) i.p. treated mice, (d) Aβ inoculated and CBD (10 mg kg−1) i.p. treated mice. Lower panel: Quantification of immunoreactivity expressed as the number of cells immunostained with anti-iNOS antibody. Data are shown as mean±s.e.m. of five experiments. ***P<0.001 versus control; °P<0.05, and °°°P<0.001 versus Aβ inoculated mice.
Figure 4.
Effects of cannabidiol (CBD) (intraperitoneal (i.p.) treatment for 7 consecutive days) on IL-1β in mouse hippocampus. Upper panel: Representative photomicrographs showing IL-1β immunoreactive cells in: (a) vehicle inoculated mice (control), (b) Aβ inoculated mice, (c) Aβ inoculated and CBD (2.5 mg kg−1) i.p. treated mice, (d) Aβ inoculated and CBD (10 mg kg−1) i.p. treated mice. Lower panel: Quantification of immunoreactivity expressed as the number of cells immunostained with anti- IL-1β antibody. Data are shown as mean±s.e.m. of five experiments. ***P<0.001 versus control; °P<0.05, and °°°P<0.001 versus Aβ inoculated mice.
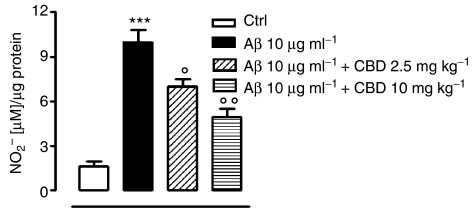
CBD effects on NO release in hippocampal homogenates
The release of NO was evaluated by measurement of its stable metabolite (NO2−) in homogenized ipsilateral hippocampi 10 days after Aβ (1–42) (10 μg ml−1) injection. As shown in Figure 5 NO2− levels were significantly increased by Aβ injection in comparison with vehicle-inoculated hippocampi (+525±30%). CBD (2.5 or 10 mg kg−1) treatment dose dependently and significantly inhibited NO2− release in tissue homogenates (−30±1 and −51±3.71% respectively) compared with those from mice injected with vehicle.
Figure 5.
Effects of cannabidiol (CBD) (2.5 or 10 mg kg−1 intraperitoneal (i.p.) for 7 consecutive days) on nitrite (NO2−) level in mouse hippocampal homogenates 10 days after Aβ (1–42) (10 μg ml−1) injection into mouse hippocampi. Data are shown as mean±s.e.m. of five experiments. ***P<0.01 versus control; °P<0.05, and °°P<0.01 versus Aβ inoculated mice.
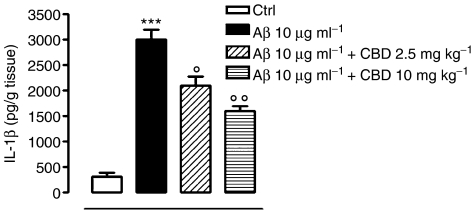
CBD effects on IL-1β levels in hippocampal homogenates
ELISA assay was performed on homogenized ipsilateral hippocampi 10 days following Aβ (1–42) (10 μg ml−1) injection to evaluate the effect of CBD treatment on IL-1β release. As shown in Figure 6, IL-1β level was significantly increased by Aβ injection in comparison with vehicle-inoculated hippocampi (+900±60%). Treatment with CBD (2.5 or 10 mg kg−1) dose-dependently and significantly inhibited IL-1β release in tissue homogenates (−30±3 and −46.7±4% respectively) when compared with homogenates derived from vehicle-treated animals.
Figure 6.
Effects of cannabidiol (CBD) (2.5 or 10 mg kg−1 intraperitoneal (i.p.) for 7 consecutive days) on IL-1β level in hippocampal homogenates 10 days after Aβ (1–42) (10 μg ml−1) injection into mouse hippocampi. Data are shown as mean±s.e.m. of five experiments. ***P<0.01 versus control; °P<0.05, and °°P<0.01 versus Aβ inoculated mice.
Discussion and conclusions
The urgent need for novel strategies for AD is apparent with the realization that the currently approved therapies are only palliative without significant and substantial disease modifying effects (Turner, 2006). In contrast, the present study suggests that CBD, here investigated with a primary focus on glial pathways, exhibits a potential to delay effectively the onset and progression of Aβ neurotoxicity. Actually, the current results provide evidence that CBD causes a clear-cut reduction of the transcription and expression of glial pro-inflammatory molecules in the hippocampus of an in vivo model of Aβ-induced neuroinflammation. They suggest CBD may be regarded as a promising tool able to affect the course of Aβ-related neuropathology, by reducing Aβ-generated reactive gliosis and subsequent neuroinflammatory responses, in addition to the previously demonstrated protective effects directly affecting neurons (Iuvone et al., 2004; Esposito et al., 2006a, 2006b). Indeed, the increasing body of immunohistological and molecular findings, showing that inflammatory processes are pre-eminent and constant aspects of the neuropathology generated by the Aβ toxicity, supports the notion that the previously under-appreciated glial activation plays a critical role in the pathogenesis of brain lesions subsequent to Aβ deposition (Craft et al., 2006). Although acute activation of glial cells may have important beneficial effects in the recovery of the CNS from a variety of insults, it is believed that a persistent activation amplifies inflammatory responses leading to a worsening of the consequences of injury (Ralay Ranaivo et al., 2006). In the scenario of reactive gliosis, the main features are astrocytic hypertrophy and proliferation, along with a marked overexpression of the intermediate filament proteins, such as GFAP, the best known hallmark of activated astrocytes (O'Callaghan and Sriram, 2005).
The present investigation focuses the ability of this phytocannabinoid, CBD, to negatively modulate GFAP transcription and expression as well as to significantly reduce IL-1β and iNOS upregulation, which importantly contribute to disease progression, through the propagation of inflammation and oxidative stress. Among the many active substances produced by Aβ stimulated microglia, IL-1β has proved to be substantially implicated in the cytokine cycle of cellular and molecular events responsible for the neurodegenerative consequences (Griffin et al., 1998). These include synthesis and processing of amyloid precursor protein (Buxbaum et al., 1992; Mrak and Griffin, 2000), as well as astrocyte activation with a subsequent iNOS overexpression and excessive production of NO (Das and Potter, 1995; Sheng et al., 1996). Increasing amounts of NO, a short-lived and diffusible free radical involved in all reported neuroinflammatory and neurodegenerative conditions (Murphy, 2000), accelerate neuronal protein nitration and cause a marked increase in tau protein hyperphosphorylation (Saez et al., 2004), encouraging the detrimental progression of Aβ-related pathology (Nathan et al., 2005).
Therefore, in this context where inflammatory pathways are believed to play relevant roles as driving forces of the Aβ-induced injury, they are identified as potential modulators of the neuronal damage and are reported as neuronal targets for effective therapeutic interventions. The present investigation provides the first evidence that substantial components of the neuroinflammatory response, set in motion by Aβ deposition and allowing for progression of neuropathology, are suppressed in vivo by CBD. The current data confirm and further reinforces the view that CBD can exhibit protective effects in models of neuroinflammation/neurodegeneration.
The seminal work describing CBD neuroprotective properties demonstrated its ability to protect cortical neurons in culture against glutamate-induced neurotoxicity. Such effects were found to be not antagonized by the established CB1 antagonist SR141716A, suggesting that they were independent of CB1 cannabinoid receptor involvement. Later CBD was shown to prevent Aβ-induced toxicity in PC12 pheocromocytoma cells, increasing survival while decreasing reactive oxygen species production, lipid peroxidation, caspas-3 levels, DNA fragmentation and intracellular calcium (Iuvone et al., 2004). In addition to this combination of anti-oxidant, anti-inflammatory and anti-apoptotic effects, subsequent studies, carried out under the same experimental conditions, demonstrated that CBD was able to operate as a Wnt/β-catenin pathway rescuer, inhibiting Aβ-induced tau protein hyperphosphorylation while attenuating iNOS protein expression and NO production (Esposito et al., 2006b). Such a wide range of effects on pathophysiological processes implicated in neuroinflammatory/neurodegenerative diseases appears truly intriguing and encourages the clinical applicability of CBD for therapeutic use.
Its antioxidant and neuroprotective actions are presumably related in part to a potential as a scavenger of free radicals due to its structural characteristics (Hampson et al., 2000), although there is room for alternative mechanisms. Ruling out the possibility that transient receptor potential vanilloid type 1 channels may be involved in the suppression of reactive gliosis exerted by CBD (personal data), a potential involvement of the CB2 receptor might be taken into account. The recently provided in vitro evidence that CBD can display CB2 receptor inverse agonist properties (Thomas et al., 2007) might offer an explanation of the anti-neuroinflammatory effects we have shown here. In Aβ neurotoxicity, several results have related CB2 receptors to events involved in the progression of brain damage by affecting reactive gliosis at neuroinflammatory lesion sites (Walter and Stella, 2004). Further, we have recently reported that, in a rodent model of Aβ-induced reactive gliosis, CB2 receptors were overexpressed (van der Stelt et al., 2006), paralleling the changes in cannabinoid receptor expression occurring in AD brain, where, in astrocyte-associated plaques, CB2 receptors were also found to be up-regulated (Ramirez et al., 2005). Interestingly, some of our recent unpublished results suggest that pharmacological interactions at glial CB1 and CB2 receptors result in a marked and opposite regulation of reactive astroglial response, with CB2 receptor blockade suppressing astroglial activation. These findings would imply a function for CB2 receptors in the regulation of CBD actions and would encourage further study of how pharmacological interactions at this receptor could influence the effects of CBD. Although more research will be needed to elucidate fully the molecular mechanisms implicated in the CBD actions described in this paper, the current data showed that the early administration of CBD markedly attenuated in vivo the reactive gliosis induced by Aβ injury. The relevance of these results stems from the fact that a proper control of glial cell function, which is compromised by the persistence of inflammatory events, is critical to provide an environment capable of ensuring neuronal survival and function. For this reason, on the basis of the present results, CBD, a drug well tolerated in humans, may be regarded as an attractive medical alternative for the treatment of AD, because of its lack of psychoactive and cognitive effects.
Acknowledgments
This work was supported by FIRB2006.
Abbreviations
- Aβ
beta amyloid
- AD
Alzheimer's disease
- CBD
cannabidiol
- i.p.
intraperitoneally
- GFAP
glial fibrillary acidic protein
- iNOS
inducible nitric oxide synthase
- IL-1β
interleukin 1 beta
- ELISA
enzyme linked immunosorbent assay
Conflict of interest
The authors state no conflict of interest.
References
- Behl C, Davis JB, Lesley R, Shubert D. Hydrogen peroxide mediates amyloid beta protein toxicity. Cell. 1994;77:817–827. doi: 10.1016/0092-8674(94)90131-7. [DOI] [PubMed] [Google Scholar]
- Braak H, Braak E. Frequency of stages of Alzheimer-related lesions in different age categories. Neurobiol Aging. 1997;18:351–357. doi: 10.1016/s0197-4580(97)00056-0. [DOI] [PubMed] [Google Scholar]
- Buxbaum JD, Oishi M, Chen HI, Pinkas-Kramarski R, Jaffe EA, Gandy SE, et al. Cholinergic agonists and interleukin 1 regulate processing and secretion of the Alzheimer beta/A4 amyloid protein precursor. Proc Natl Acad Sci USA. 1992;89:10075–10078. doi: 10.1073/pnas.89.21.10075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caricasole A, Copani A, Caruso A, Caraci F, Iacovelli L, Sortino MA, et al. The Wnt pathway, cell-cycle activation and beta-amyloid: novel therapeutic strategies in Alzheimer's disease. Trends Pharmacol Sci. 2003;24:233–238. doi: 10.1016/s0165-6147(03)00100-7. [DOI] [PubMed] [Google Scholar]
- Costa B, Trovato AE, Comelli F, Giagnoni G, Colleoni M. The non-psychoactive cannabis constituent cannabidiol is an orally effective therapeutic agent in rat chronic inflammatory and neuropathic pain. Eur J Pharmacol. 2007;556:75–83. doi: 10.1016/j.ejphar.2006.11.006. [DOI] [PubMed] [Google Scholar]
- Cotman CW, Tenner AJ, Cummings BJ. Amyloid converts an acute phase injury response to chronic injury responses. Neurobiol Aging. 1996;17:723–731. doi: 10.1016/0197-4580(96)00117-0. [DOI] [PubMed] [Google Scholar]
- Craft JM, Watterson DM, Van Eldik LJ. Human amyloid beta-induced neuroinflammation is an early event in neurodegeneration. Glia. 2006;53:484–490. doi: 10.1002/glia.20306. [DOI] [PubMed] [Google Scholar]
- Das S, Potter H. Expression of the Alzheimer amyloid-promoting factor antichymotrypsin is induced in human astrocytes by IL-1. Neuron. 1995;14:447–456. doi: 10.1016/0896-6273(95)90300-3. [DOI] [PubMed] [Google Scholar]
- Di Rosa M, Radomski M, Carnuccio R, Moncada S. Glucocorticoids inhibit the induction of nitric oxide synthase in macrophages. Biochem Biophys Res Commun. 1990;172:1246–1252. doi: 10.1016/0006-291x(90)91583-e. [DOI] [PubMed] [Google Scholar]
- Esposito G, De Filippis D, Carnuccio R, Izzo AA, Iuvone T. The marijuana component cannabidiol inhibits beta-amyloid-induced tau protein hyperphosphorylation through Wnt/beta-catenin pathway rescue in PC12 cells. J Mol Med. 2006a;84:253–258. doi: 10.1007/s00109-005-0025-1. [DOI] [PubMed] [Google Scholar]
- Esposito G, De Filippis D, Maiuri MC, De Stefano D, Carnuccio R, Iuvone T. Cannabidiol inhibits inducible nitric oxide synthase protein expression and nitric oxide production in beta-amyloid stimulated PC12 neurons through p38 MAP kinase and NF-kappaB involvement. Neurosci Lett. 2006b;15:91–95. doi: 10.1016/j.neulet.2006.01.047. [DOI] [PubMed] [Google Scholar]
- Green KN, Peers C. Divergent pathways account for two distinct effects of amyloid beta peptides on exocytosis and Ca(2+) currents: involvement of ROS and NF-kappaB. J Neurochem. 2002;81:1043–1051. doi: 10.1046/j.1471-4159.2002.00907.x. [DOI] [PubMed] [Google Scholar]
- Griffin WS, Sheng JG, Royston MC, Gentleman SM, McKenzie JE, Graham DI, et al. Glial-neuronal interactions in Alzheimer's disease: the potential role of a cytokine cycle in disease progression. Brain Pathol. 1998;8:65–72. doi: 10.1111/j.1750-3639.1998.tb00136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampson AJ, Grimaldi M, Lolic M, Wink D, Rosenthal R, Axelrod J. Neuroprotective antioxidants from marijuana. Ann N Y Acad Sci. 2000;899:274–282. [PubMed] [Google Scholar]
- Itagaki S, McGeer PL, Akiyama H, Zhu S, Selkoe D. Relationship of microglia and astrocytes to amyloid deposits of Alzheimer desease. J Neuroimmunol. 1989;24:173–182. doi: 10.1016/0165-5728(89)90115-x. [DOI] [PubMed] [Google Scholar]
- Iuvone T, Esposito G, Esposito R, Santamaria R, Di Rosa M, Izzo AA. Neuroprotective effect of cannabidiol, a non-psychoactive component from Cannabis sativa, on beta-amyloid-induced toxicity in PC12 cells. J Neurochem. 2004;89:134–141. doi: 10.1111/j.1471-4159.2003.02327.x. [DOI] [PubMed] [Google Scholar]
- Koo EH, Lansbury PT, Kelly JW. Amyloid diseases: abnormal protein aggregation in neurodegeneration. Proc Natl Acad Sci USA. 1999;96:9989–9990. doi: 10.1073/pnas.96.18.9989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee VMY, Balin BJ, Otvos L, Trojanowski JQ. A68: a major subunit of paired helical filaments and derivatized forms of normal tau. Science. 1991;251:675–678. doi: 10.1126/science.1899488. [DOI] [PubMed] [Google Scholar]
- Mattson MP. Oxidative stress, perturbed calcium homeostasis, and immune dysfunction in Alzheimer's disease. J Neurovirol. 2002;8:539–550. doi: 10.1080/13550280290100978. [DOI] [PubMed] [Google Scholar]
- Mechoulam R, Parker LA, Gallily R. Cannabidiol: an overview of some pharmacological aspects. J Clin Pharmacol. 2002;42:11S–19S. doi: 10.1002/j.1552-4604.2002.tb05998.x. [DOI] [PubMed] [Google Scholar]
- Mrak RE, Griffin WS. IL-1 and the immunogenetics of Alzheimer's disease. J Neuropath Exp Neurol. 2000;59:471–476. doi: 10.1093/jnen/59.6.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy S. Production of nitric oxide by glial cells: regulation and potential roles in the CNS. Glia. 2000;29:1–13. doi: 10.1002/(sici)1098-1136(20000101)29:1<1::aid-glia1>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Nathan C, Calingasan N, Nezezon J, Ding A, Lucia MS, La Perle K, et al. Protection from Alzheimer's-like disease in the mouse by genetic ablation of inducible nitric oxide synthase. J Exp Med. 2005;202:1163–1169. doi: 10.1084/jem.20051529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Callaghan JP, Sriram K. Glial fibrillary acidic protein and related glial proteins as biomarkers of neurotoxicity. Expert Opin Drug Saf. 2005;4:433–442. doi: 10.1517/14740338.4.3.433. [DOI] [PubMed] [Google Scholar]
- Ralay Ranaivo H, Craft JM, Hu W, Guo L, Wing LK, Van Eldik LJ, et al. Glia as a therapeutic target: selective suppression of human amyloid-beta-induced upregulation of brain proinflammatory cytokine production attenuates neurodegeneration. J Neurosci. 2006;26:662–670. doi: 10.1523/JNEUROSCI.4652-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez BG, Blazquez C, Gomez del Pulgar T, Guzman M, de Ceballos ML. Prevention of Alzheimer's disease pathology by cannabinoids: neuroprotection mediated by blockade of microglial activation. J Neurosci. 2005;25:1904–1913. doi: 10.1523/JNEUROSCI.4540-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saez TE, Pehar M, Vargas M, Barbeito L, Maccioni RB. Astrocytic nitric oxide triggers tau hyperphosphorylation in hippocampal neurons. In vivo. 2004;3:275–280. [PubMed] [Google Scholar]
- Sheng JG, Mrak RE, Rovnaghi CR, Kozlowska E, Van Eldik LJ, Griffin WS. Human brain S100 beta and S100 beta mRNA expression increase with age: pathogenetic implications for Alzheimer's disease. Neurobiol Aging. 1996;17:359–363. doi: 10.1016/0197-4580(96)00037-1. [DOI] [PubMed] [Google Scholar]
- Terry RD. The fine structure of neurofibrillary tangles in Alzheimer's disease. J Neuropathol Exp Neurol. 1963;22:629–642. doi: 10.1097/00005072-196310000-00005. [DOI] [PubMed] [Google Scholar]
- Thomas A, Baillie GL, Phillips AM, Razdan RK, Ross RA, Pertwee RG. Cannabidiol displays unexpectedly high potency as an antagonist of CB(1) and CB(2) receptor agonists in vitro. Br J Pharmacol. 2007;150:613–623. doi: 10.1038/sj.bjp.0707133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RS. Alzheimer's disease. Semin Neurol. 2006;26:499–506. doi: 10.1055/s-2006-951622. [DOI] [PubMed] [Google Scholar]
- Ueda K, Shinohara S, Yagami T, Asakura K, Kawasaki K. Amyloid β-protein potentiates Ca2+ influx through 1-type voltage-sensitive Ca2+ channels: a possible involvement of free radicals. J Neurochem. 1997;68:265–271. doi: 10.1046/j.1471-4159.1997.68010265.x. [DOI] [PubMed] [Google Scholar]
- van der Stelt M, Mazzola C, Esposito G, Matias I, Petrosino S, De Filippis D, et al. Endocannabinoids and beta-amyloid-induced neurotoxicity in vivo: effect of pharmacological elevation of endocannabinoid levels. Cell Mol Life Sci. 2006;63:1410–1424. doi: 10.1007/s00018-006-6037-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter L, Stella N. Cannabinoids and neuroinflammation. Br J Pharmacol. 2004;141:775–785. doi: 10.1038/sj.bjp.0705667. [DOI] [PMC free article] [PubMed] [Google Scholar]