Abstract
Adequate data on the incidence, prevalence, natural history, and clinical course of temperomandibular disorders (TMD) and other chronic pain conditions are largely lacking, though the need to derive such basic data is recognized by clinicians, researchers, and public health agencies. This paper discusses challenges to the epidemiologic study of TMD diagnosis. These challenges include:
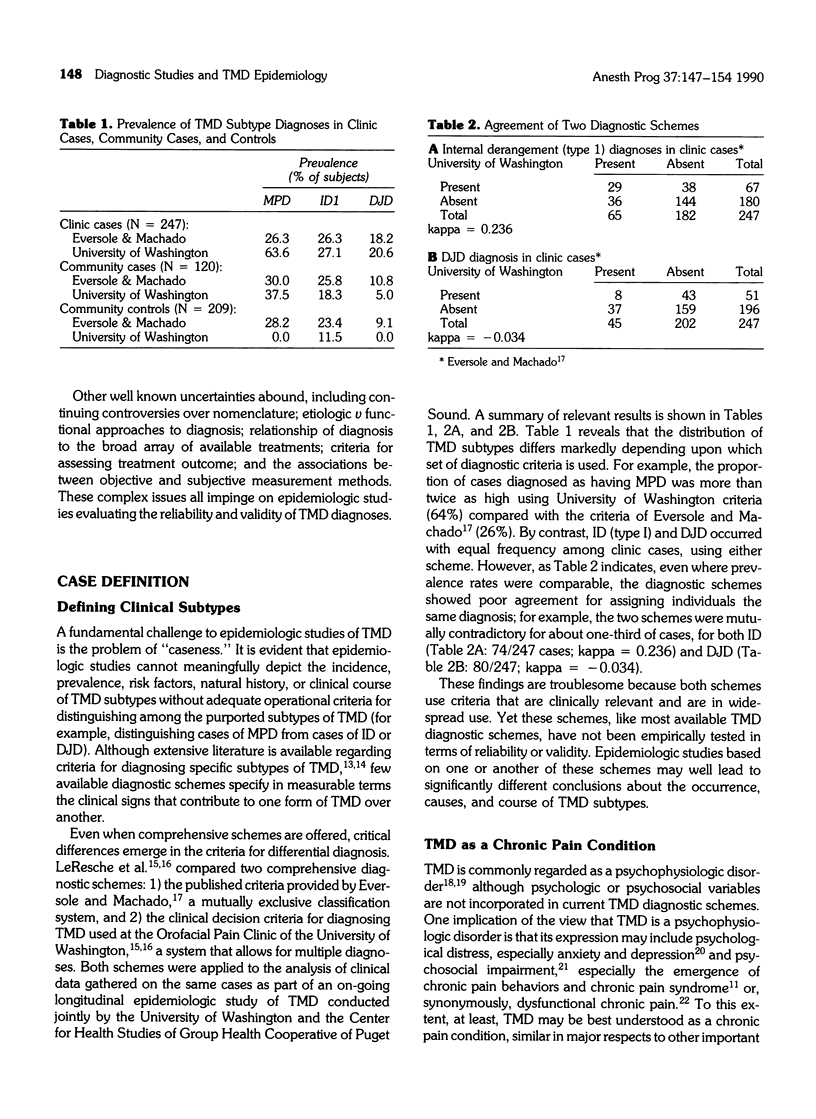
• Case definition: There is currently poor agreement regarding which combinations of clinical and psychosocial findings differentially define cases of TMD
• Differentiation of normal variation v pathophysiologic signs: To what extent do commonly gathered clinical measurements constitute pathophysiologic signs of TMD v reflect normal biologic variation
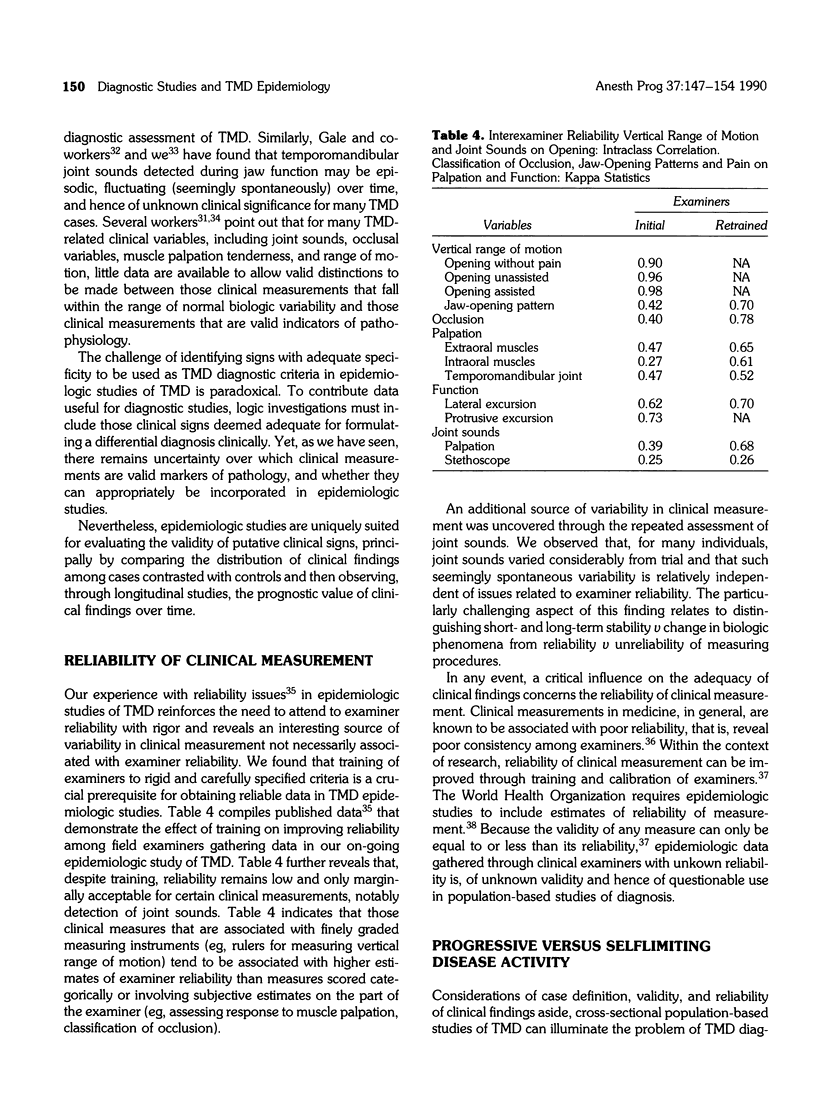
• Reliability of clinical measurement: Factors influencing reliability of clinical signs and reliability of examiners have not been adequately assessed
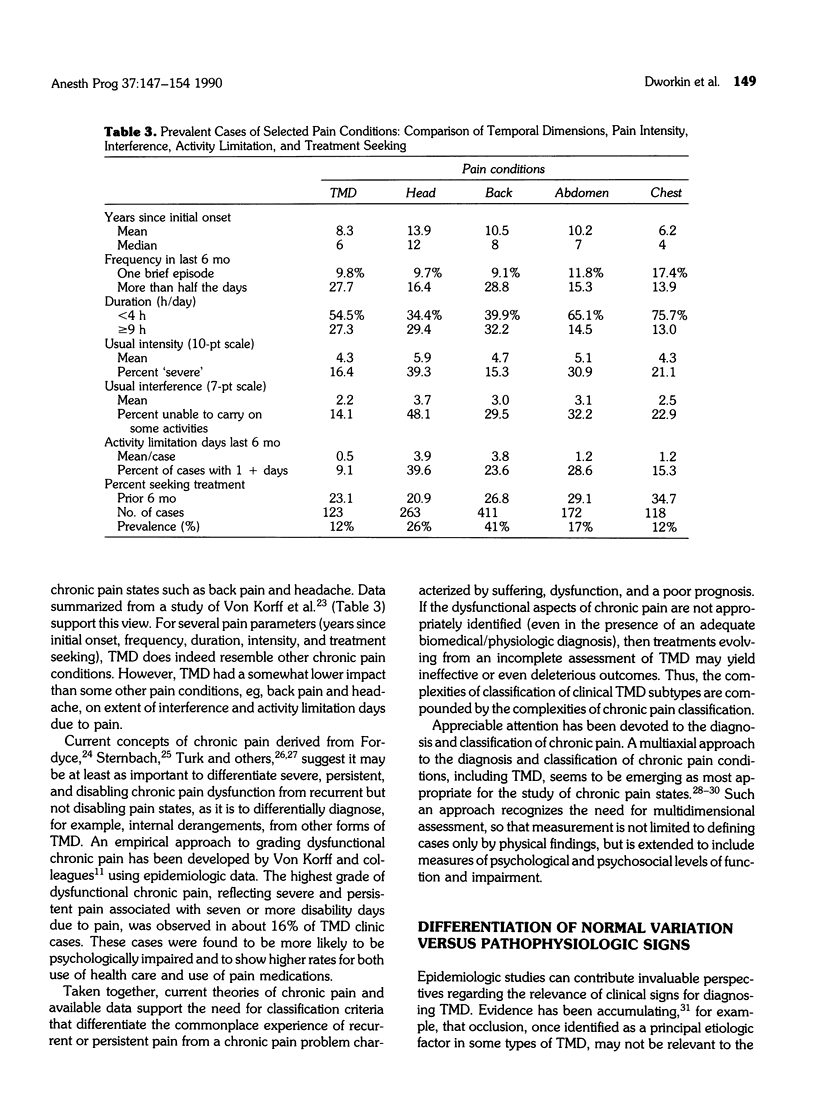
• Progressive v self-limiting disease activity: Do TMD subtypes represent a continuum of pathologic disease activity, or nonmutually exclusive categories describing largely symptomatic pain conditions that are selflimiting or stable.
It is recommended that epidemiologic studies not be constrained by a priori definitions of TMD subtypes, but continue to gather data on clinical signs and symptoms that have theoretical and clinical relevance to mandibular dysfunction and psychosocial status. An approach is proposed for development of reliable and valid criteria of TMD subtypes suitable for epidemiologic research.
Full text
PDF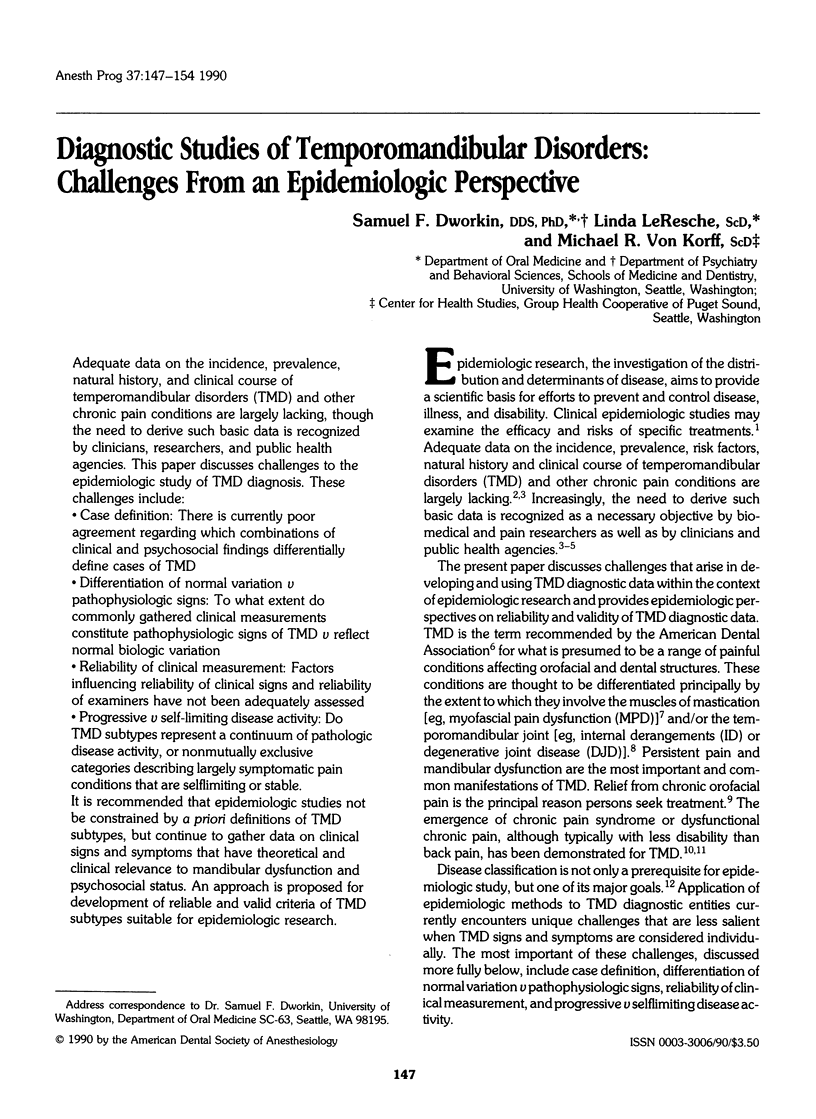
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bouckoms A. J. Recent developments in the classification of pain. Psychosomatics. 1985 Aug;26(8):637-42, 645. doi: 10.1016/S0033-3182(85)72808-3. [DOI] [PubMed] [Google Scholar]
- Eversole L. R., Machado L. Temporomandibular joint internal derangements and associated neuromuscular disorders. J Am Dent Assoc. 1985 Jan;110(1):69–79. doi: 10.14219/jada.archive.1985.0283. [DOI] [PubMed] [Google Scholar]
- Farrar W. B. Characteristics of the condylar path in internal derangements of the TMJ. J Prosthet Dent. 1978 Mar;39(3):319–323. doi: 10.1016/s0022-3913(78)80103-6. [DOI] [PubMed] [Google Scholar]
- Fricton J. R., Schiffman E. L. The craniomandibular index: validity. J Prosthet Dent. 1987 Aug;58(2):222–228. doi: 10.1016/0022-3913(87)90181-8. [DOI] [PubMed] [Google Scholar]
- Greene C. S., Marbach J. J. Epidemiologic studies of mandibular dysfunction: a critical review. J Prosthet Dent. 1982 Aug;48(2):184–190. doi: 10.1016/0022-3913(82)90110-x. [DOI] [PubMed] [Google Scholar]
- Helöe B., Heiberg A. N., Krogstad B. S. A multiprofessional study of patients with myofascial pain-dysfunction syndrome. I. Acta Odontol Scand. 1980;38(2):109–117. doi: 10.3109/00016358009003487. [DOI] [PubMed] [Google Scholar]
- Koran L. M. The reliability of clinical methods, data and judgments (first of two parts). N Engl J Med. 1975 Sep 25;293(13):642–646. doi: 10.1056/NEJM197509252931307. [DOI] [PubMed] [Google Scholar]
- Laskin D. M., Block S. Diagnosis and treatment of myofacial pain-dysfunction (MPD) syndrome. J Prosthet Dent. 1986 Jul;56(1):75–84. doi: 10.1016/0022-3913(86)90287-8. [DOI] [PubMed] [Google Scholar]
- Laskin D. M. Etiology of the pain-dysfunction syndrome. J Am Dent Assoc. 1969 Jul;79(1):147–153. doi: 10.14219/jada.archive.1969.0234. [DOI] [PubMed] [Google Scholar]
- Marbach J. J., Lipton J. A. Aspects of illness behavior in patients with facial pain. J Am Dent Assoc. 1978 Apr;96(4):630–638. doi: 10.14219/jada.archive.1978.0121. [DOI] [PubMed] [Google Scholar]
- McNeill C. Craniomandibular (TMJ) disorders--the state of the art. Part II: accepted diagnostic and treatment modalities. J Prosthet Dent. 1983 Mar;49(3):393–397. doi: 10.1016/0022-3913(83)90284-6. [DOI] [PubMed] [Google Scholar]
- Rudy T. E., Turk D. C., Zaki H. S., Curtin H. D. An empirical taxometric alternative to traditional classification of temporomandibular disorders. Pain. 1989 Mar;36(3):311–320. doi: 10.1016/0304-3959(89)90090-0. [DOI] [PubMed] [Google Scholar]
- Rugh J. D., Solberg W. K. Oral health status in the United States: temporomandibular disorders. J Dent Educ. 1985 Jun;49(6):398–406. [PubMed] [Google Scholar]
- Rugh J. D., Solberg W. K. Psychological implications in temporomandibular pain and dysfunction. Oral Sci Rev. 1976;7:3–30. [PubMed] [Google Scholar]
- Scientific approach to the assessment and management of activity-related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine (Phila Pa 1976) 1987 Sep;12(7 Suppl):S1–59. [PubMed] [Google Scholar]
- Turk D. C., Flor H. Pain greater than pain behaviors: the utility and limitations of the pain behavior construct. Pain. 1987 Dec;31(3):277–295. doi: 10.1016/0304-3959(87)90158-8. [DOI] [PubMed] [Google Scholar]
- Turk D. C., Rudy T. E. Toward an empirically derived taxonomy of chronic pain patients: integration of psychological assessment data. J Consult Clin Psychol. 1988 Apr;56(2):233–238. doi: 10.1037//0022-006x.56.2.233. [DOI] [PubMed] [Google Scholar]
- Turk D. C., Rudy T. E. Towards a comprehensive assessment of chronic pain patients. Behav Res Ther. 1987;25(4):237–249. doi: 10.1016/0005-7967(87)90002-7. [DOI] [PubMed] [Google Scholar]
- Von Korff M., Dworkin S. F., Le Resche L. Graded chronic pain status: an epidemiologic evaluation. Pain. 1990 Mar;40(3):279–291. doi: 10.1016/0304-3959(90)91125-3. [DOI] [PubMed] [Google Scholar]
- Von Korff M., Dworkin S. F., Le Resche L., Kruger A. An epidemiologic comparison of pain complaints. Pain. 1988 Feb;32(2):173–183. doi: 10.1016/0304-3959(88)90066-8. [DOI] [PubMed] [Google Scholar]


