Abstract
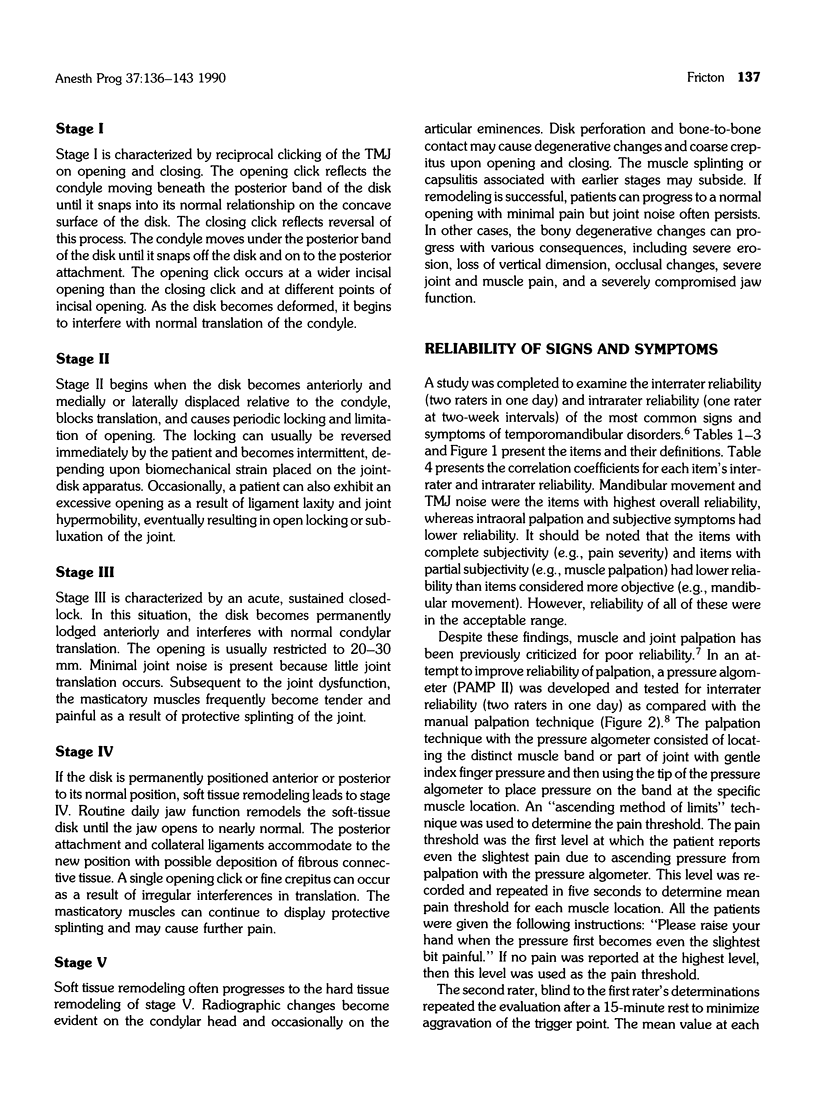
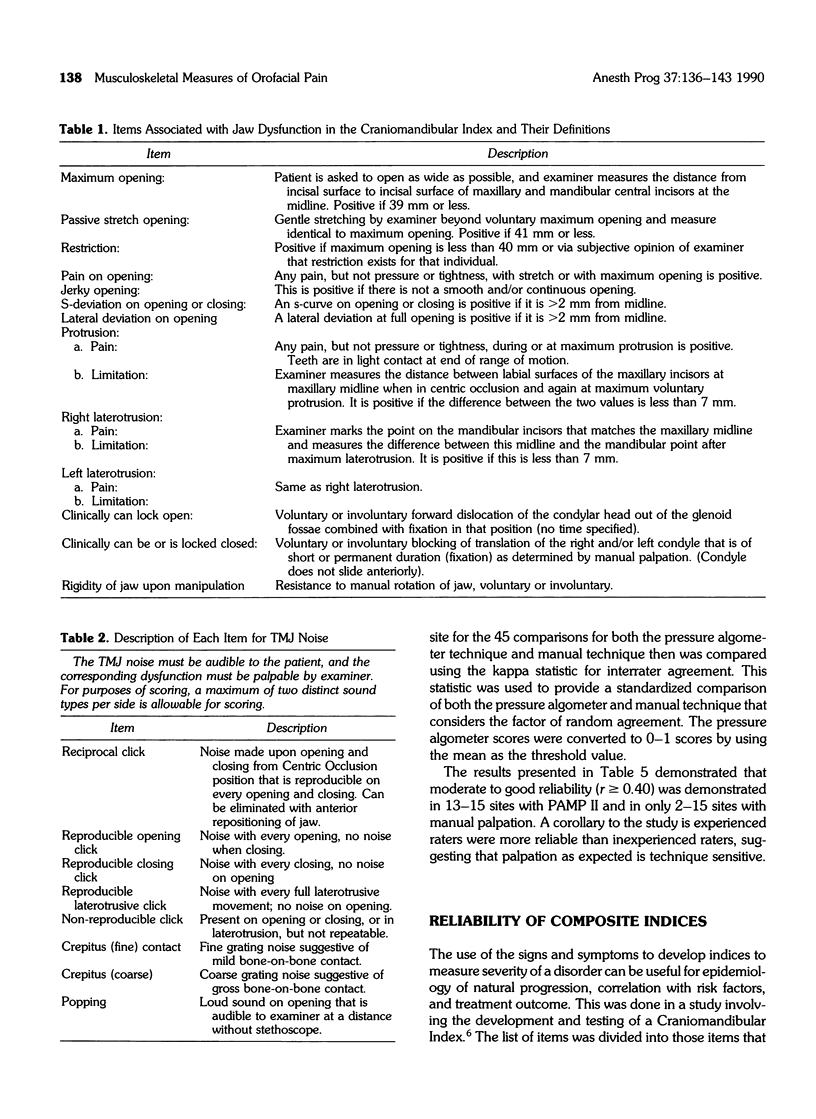
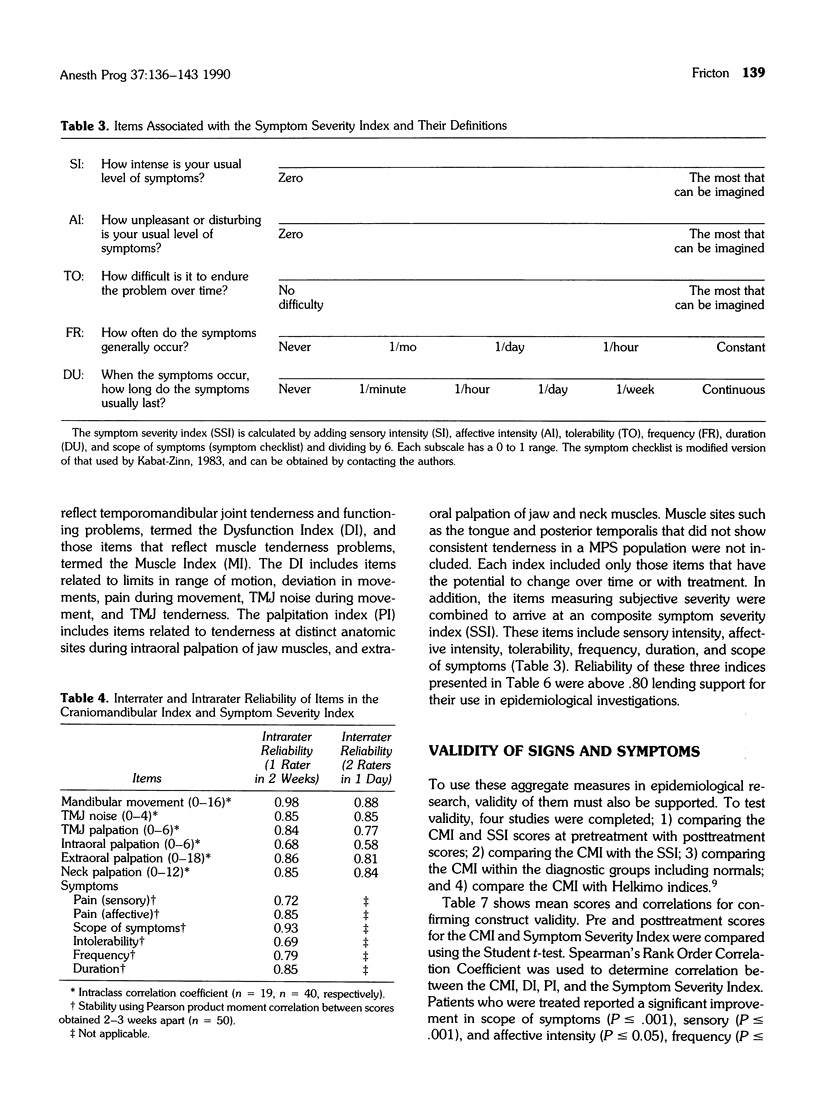
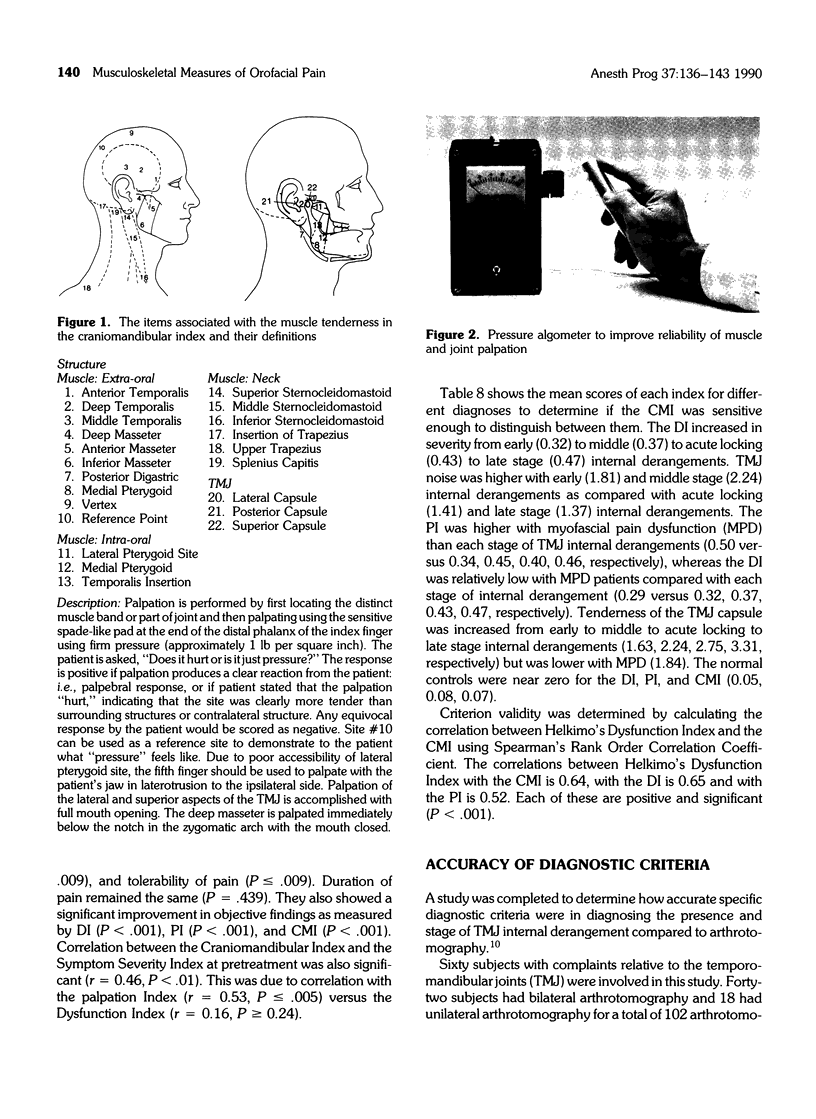
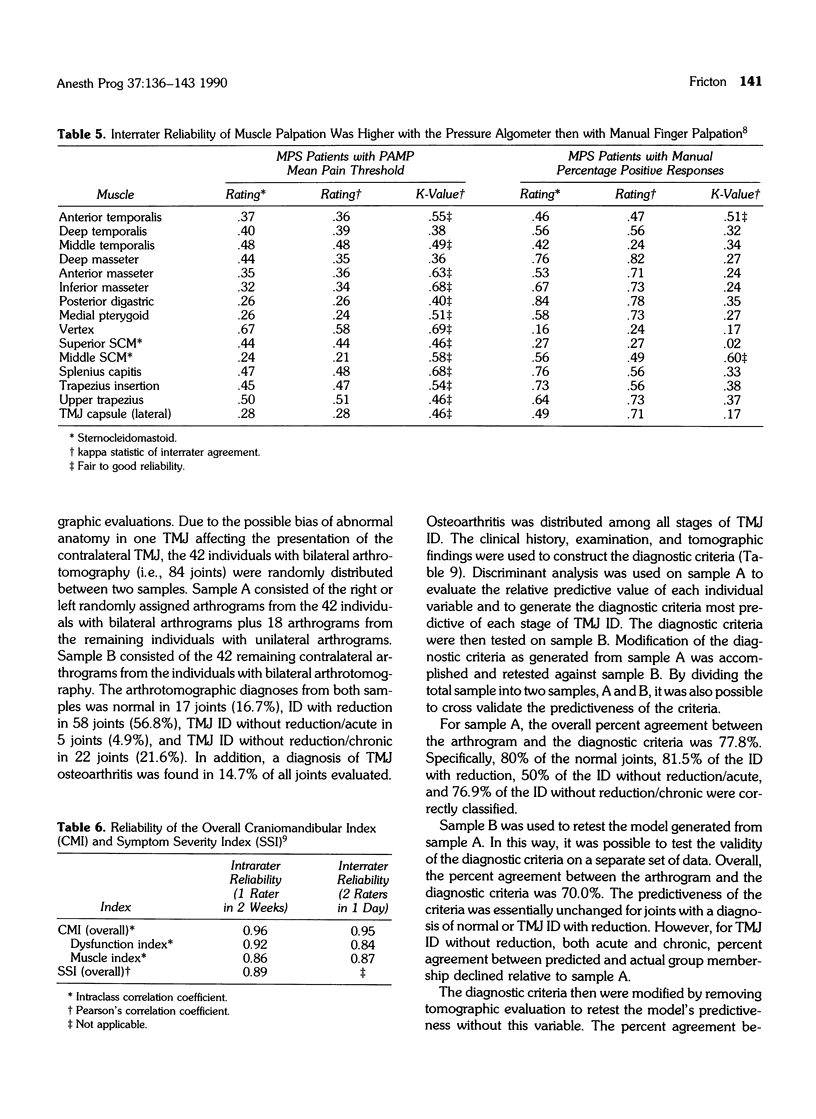
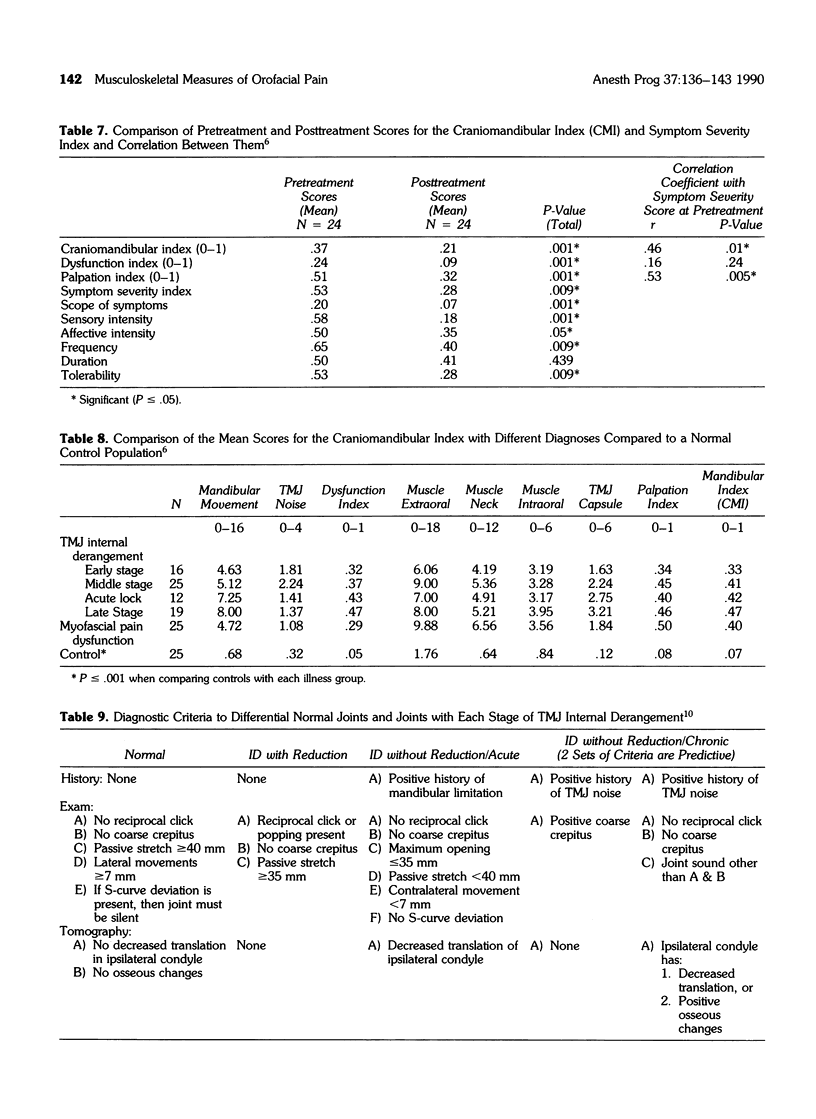
Musculoskeletal disorders of the stomatognathic system comprise the majority of diagnoses responsible for chronic orofacial pain. The most common signs for these disorders include tenderness, limitation in range of motion, deviation in range of motion, and joint noise. Although these signs are used routinely for diagnosis, the reliability, validity, and accuracy of their use as diagnostic criteria or outcome measures has not been established. A series of clinical studies on a Craniomandibular Index (CMI) was completed to examine these issues. Interrater and intrarater reliability of the grouped items in the CMI ranged from 0.58-0.98, with an overall correlation coefficient of 0.95 and 0.96, respectively. Pressure algometry improved reliability of muscle and joint palpation for tenderness. Tenderness, but not dysfunction, was correlated with symptom severity. Both tenderness and dysfunction improved with treatment but did not become normal. The percent agreement of these signs as diagnostic criteria for the presence and stage of a temperomandibular joint (TMJ) internal derangement was about 80% compared with arthrotomography. These studies suggest that these clinical characteristics can be used with adequate reliability and validity to diagnose and measure severity if standardized methods are used.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Eversole L. R., Machado L. Temporomandibular joint internal derangements and associated neuromuscular disorders. J Am Dent Assoc. 1985 Jan;110(1):69–79. doi: 10.14219/jada.archive.1985.0283. [DOI] [PubMed] [Google Scholar]
- Fricton J. R., Kroening R., Haley D., Siegert R. Myofascial pain syndrome of the head and neck: a review of clinical characteristics of 164 patients. Oral Surg Oral Med Oral Pathol. 1985 Dec;60(6):615–623. doi: 10.1016/0030-4220(85)90364-0. [DOI] [PubMed] [Google Scholar]
- Fricton J. R., Schiffman E. L. The craniomandibular index: validity. J Prosthet Dent. 1987 Aug;58(2):222–228. doi: 10.1016/0022-3913(87)90181-8. [DOI] [PubMed] [Google Scholar]
- Fricton J. R., Schiffman E. L. The craniomandibular index: validity. J Prosthet Dent. 1987 Aug;58(2):222–228. doi: 10.1016/0022-3913(87)90181-8. [DOI] [PubMed] [Google Scholar]
- Friedman M. H., Weisberg J. Pitfalls of muscle palpation in TMJ diagnosis. J Prosthet Dent. 1982 Sep;48(3):331–331. doi: 10.1016/0022-3913(82)90022-1. [DOI] [PubMed] [Google Scholar]
- Rasmussen O. C. Description of population and progress of symptoms in a longitudinal study of temporomandibular arthropathy. Scand J Dent Res. 1981 Apr;89(2):196–203. doi: 10.1111/j.1600-0722.1981.tb01671.x. [DOI] [PubMed] [Google Scholar]
- Report of the president's conference on the examination, diagnosis, and management of temporomandibular disorders. J Am Dent Assoc. 1983 Jan;106(1):75–77. doi: 10.14219/jada.archive.1983.0020. [DOI] [PubMed] [Google Scholar]



