At Baylor University Medical Center, we have a very active patient safety program. Physicians can benefit from several of the safety, quality, and risk management initiatives—primarily by improving patient outcomes and reducing hassles and wasted time. In this article, I review some issues related to patient safety, medical errors, and features of high-reliability organizations and explain how physicians' efforts in teamwork and communication can improve safety. I also review key National Patient Safety Goals. My objective is to engage physicians in the safety program and help them better understand Baylor's culture and some legal opportunities and barriers that affect us in patient safety.
PATIENT SAFETY: BACKGROUND AND STATUS
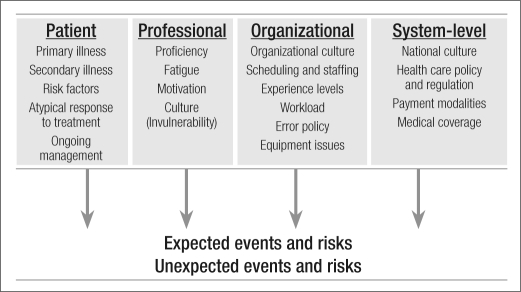
Patient safety can be defined as freedom from accidental injuries stemming from the processes of health care. In addition to the expected threats to safety that relate to the patient's illness, unexpected threats arise from professional, organizational, and system-level factors (Figure 1).
Figure 1.
Threats to safety in medicine. Proc (Bayl Univ Med Cent) 2008;21 (1):9–14
The title of a recent article stated: “Doctors say many obstacles block paths to patient safety” (1). This survey of 1155 physicians listed the top four obstacles: 1) a lack of resources and money; 2) patient compliance and awareness of healthy habits; 3) poor communication among physicians, nurses, and professionals; and 4) a desire to maintain the status quo. In addition, physicians have an attitude that bad things can't happen to them. They view catastrophic events as rare. They assume everything is safe, but they do not take steps to assure that everything is safe.
Patient safety issues became better recognized in 1999 when the Institute of Medicine published To Err Is Human, which indicated that 44,000 to 98,000 unnecessary deaths occur every year in US hospitals (2). In 2001, Crossing the Quality Chasm was published; its message was that the disconnect between the health care we have and the health care we could have is not just a gap but a chasm (3). Many other articles began showing up in newspapers, journals, and lay magazines. In 2004, a national survey examined the status of patient safety. In this survey, 33% of people reported personal or family experience with medical error; 55% were dissatisfied with the quality of health care (up from 44% 4 years earlier); 40% felt the quality of health care was worse than it was 5 years earlier (only 17% said it was better); and 50% were worried about the safety of their medical care (4). Thus, despite the public attention given to hospital safety, the health care community did not make improvements in the 4 years between an initial 2000 survey and the resurvey.
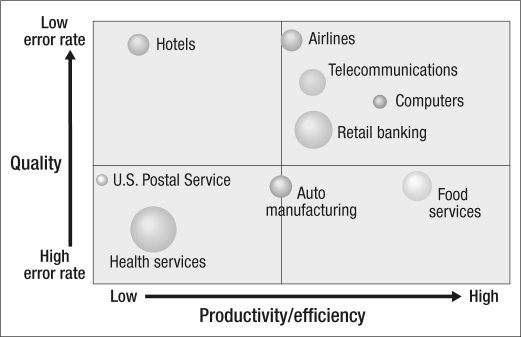
Neither does health care fare well when compared with other industries. Health services showed both a high error rate and low productivity, in contrast to highly reliable organizations, such as the airline, telecommunications, computer, and retail banking industries, for example (Figure 2). The book Managing the Unexpected listed characteristics of high-reliability organizations, characteristics that allow them to achieve their low error rates (Table 1) (5).
Figure 2.
A cross-industry comparison of quality and productivity, showing that health services is poor in both. From the Clinical Advisory Board 2005 National Meeting.
Table 1.
Characteristics of high-reliability organizations∗
| • Preoccupation with failure: when someone raises a concern, the problem exists until proven otherwise |
| • Reluctance to simplify: errors and close calls are reflections of deeper system flaws |
| • Commitment to resilience: knowing there will be problems and flaws, the job will get done |
| • Deference to expertise: the person who is most qualified does the job |
| • Sensitivity to operations: resources are flexed to deal with demand or workload |
∗From reference 5.
In 2006, a Time magazine cover story asked, “What scares doctors?” The answer was “being the patient” (6). We need to put ourselves in the patient's place. If we are aware of errors that can occur and see errors occurring with our patients, we need to take a step back and say, “What else can we do?” We need to focus on the patient rather than ourselves and do whatever we can to improve patient care and outcomes.
SYSTEM CHANGES AND THE SAFETY CULTURE
In the 1950s, health care was fairly simple, less effective, and inexpensive. In contrast, today health care is complex, highly effective, and costly. Because of this complexity, we get everything right only about 50% of the time, according to a report in the New England Journal of Medicine (7). Health care in the more limited 1950s era was safe. With the tests and procedures we do today and the complex system we work in, health care can be dangerous (Table 2).
Table 2.
System-related causes of medical errors∗
| • Interactions with technology |
| • Large number of staff providing care |
| • Poor communication between patients and staff and among staff |
| • Stress and fatigue |
| • Human factors |
| • Design factors |
| • Lack of appropriate education or training |
| • Higher acuity of illness |
| • Need for rapid decision making |
| • Reductions in staffing |
| • Lack of redundancies to prevent error |
∗From reference 8.
Medical errors can be errors of commission or omission. An error of commission involves doing something incorrectly, like misreading a label, and this happens about 3 times out of 1000. Errors of omission involve not doing something that should have been done;these errors occur 1 time in a 100. Although patients may be harmed in a variety of ways, fortunately only a fraction of errors actually result in harm. These errors range from accidents (such as falls in the hospital), equipment failures, and hospital-associated infections to procedure errors and the more common medication errors.
Clearly, humans make errors. Most errors do not result from individual recklessness. Rather, they are caused by faulty systems, processes, and other conditions that lead people to make mistakes or fail to prevent them (8). We can reduce the number of errors by redesigning the health care system at all levels to improve safety. From a broad perspective, this system must have procedures that address three goals: 1) preventing errors; 2) making errors visible when they do occur so that they may be intercepted; and 3) mitigating the adverse effects of errors when they are not detected and intercepted.
A culture of safety is required. In this environment, all workers accept responsibility for the safety of themselves, their coworkers, their patients, and visitors. They prioritize safety above financial and operational goals. Leaders encourage and reward the identification, communication, and resolution of safety issues. They ensure that the organization learns from accidents and provide the appropriate resources, structure, and accountability to maintain effective safety systems.
Such a culture represents a change. Medicine has traditionally been characterized by autonomy among physicians, a lack of teamwork, a lack of transparency about medical errors, and poor communication. Traditionally, health care institutions have approached medical errors by finding the individuals at fault, disciplining them, and then demanding retraining or establishing new policies. Rather than preventing human error, such an approach stifles discussion and the discovery of the causes of error (8).
The new safety culture focuses on learning each time an error occurs. The strategy is to identify system failures rather than individual failures within a nonpunitive environment that encourages occurrence reporting. At Baylor, we have started weekly safety walk rounds. A number of us go to one of the hospital floors and discuss with the front-line staff any safety issues that could affect patients as well as employees. We have support from the administration in correcting issues in order to make the institution safer and a more pleasant place to work.
In summary, the change in culture to become a highly reliable organization, where safety is the highest priority and transparency about errors is valued, demands a number of changes (Table 3). In the context of health care, reliability is defined as patients getting the intended tests, medications, information, and procedures at the appropriate time and in accordance with their values and preferences.
Table 3.
Changes required to achieve a safety culture
| Old culture | New culture |
| Total autonomy | Shared expectations |
| Organizational protection | Mutual accountability |
| Entitlement | Professional respect for all |
| Hierarchy | Everyone adds value |
| Silos | Collaboration and shared outcomes |
| Personal needs | Organizational needs |
WAYS TO IMPROVE PATIENT SAFETY
Several approaches can be used to improve patient safety and reduce errors and adverse effects. One approach is standardization, such as the use of order sets, protocols, and reminders. Some physicians believe that standardization compromises their ability to think. Instead, it is a way of reducing errors without conceding creativity or clinical acumen. Other approaches include designing safe systems and having prudent implementation of technology. As examples of the latter, Baylor has smart intravenous pumps that detect medication errors, as well as barcoding to ensure the five rights of medication administration (right patient, right route, right dose, right time, right medication).
Two other approaches to improve patient safety are teamwork and communication. Traditionally, physicians have been weak in these areas. Such approaches must be addressed, however, because they relate to the four areas of frustration or opportunity we have identified in our patient safety culture: 1) hand-offs and transitions, 2) teamwork across clinical units, 3) creation of a nonpunitive atmosphere, and 4) staffing concerns.
Teamwork
Baylor has begun teaching team resource management. When nurses and other clinical staff attend the training, they frequently say it was helpful but then ask: “Where are the doctors? These efforts are not going to work if we don't engage the doctors.”
Teamwork training has been shown to lead to more effective teams, which in turn lead to happier staff with higher retention rates and less turnover. This improves the safety culture and ultimately leads to fewer accidents and injuries to patients.
It has been estimated that over the next few years, the USA will face a shortage of up to a million nurses. The top three predictors of nursing turnover relate to these statements: “Doctors and nurses work as a team,” “I can speak up if I disagree with physicians,” and “Disagreements on this unit are resolved with what is right for the patient.” In contrast, one intensive care unit at Baylor University Medical Center had poor results for teamwork and communication in its employee survey (Table 4).
Table 4.
A sample of employee survey results showing the need for better teamwork
| Survey question | Response |
| Doctors, nurses, and other clinical staff work together as a highly coordinated team | 38% |
| Training that helps increase multidisciplinary teamwork is provided to caregivers | 36% |
| I feel respected by the doctors I commonly work with | 43% |
| I let doctors know when I feel their decisions may put a patient at increased risk | 48% |
Communication
According to data from the Joint Commission, breakdown of communication is an underlying cause in roughly 65% of sentinel events (9). Thus, improvement of communication is an essential strategy in patient safety. From a patient standpoint, communication failure can do more than hinder safety: it can delay diagnosis, create confusion regarding the plan of care, and increase the cost of care through repeated tests. Lack of effective communication creates frustration with patients and families and increases their anxiety when they are already anxious. It has a tendency to erode trust in the caregivers as well as the organization and thereby reduces patient satisfaction.
Some “routine” and “rescue” communication strategies have been identified. Among the routine strategies are “time-outs” before surgery or before other surgical interventions, such as insertion of a central line or aspiration of abscesses;prohibited abbreviations;read-backs of verbal orders and critical results;medication reconciliation;and a situational briefing model (SBAR, discussed below). Rescue communications include “stop the line”(discussed below), chain of command, rapid response teams, and disclosure. The first key in effective communication is for all parties to be knowledgeable of and in agreement about the respective communication expectations and responsibilities.
Health care professionals need to know how to assert themselves—even if that means speaking up to stop an action. Such a scenario requires psychologic safety, that is, an environment of respect. It also requires effective leadership: a flattened hierarchy, with sharing of the treatment plan and encouragement of all team members to participate in the conversation and to share questions or concerns. In the hospital, we often see groups of people walking down the hallway together, making multidisciplinary rounds. The group may look like a team, but teamwork is not always in play: the physicians are leading and talking among themselves, but the nurses, dietitians, physical therapists, and respiratory therapists are standing around and not interacting with the other participants. We need to engage all members of the team to create a team atmosphere.
Different styles of communication also come into play. Nurses have been trained to be narrative and descriptive, whereas physicians want to cut to the chase. National culture affects communication as well; in some cultures, female nurses do not want to speak up to male physicians. Additional factors relate to gender, hierarchy, and prior relationships. Regarding the latter, if a physician responded to a nurse by asking why she called and implying that she was harassing him, the nurse would be less likely to call that physician the next time a patient issue arises. The lines of communication that we are trying to open have already been shut down. Perceptions of teamwork depend on point of view: studies show that physicians rate nurses as high with respect to teamwork, but nurses rate physicians lower with respect to teamwork.
SBAR, situational briefing.
Baylor University Medical Center is teaching nurses to use a structured communication model called SBAR, which stands for situation, background, assessment, and recommendation (Table 5). This model has been used in the nuclear submarine service for concise and accurate communication. Nurses are being asked to change their style, to be less narrative and more to the point. Use of the model enhances predictability in the nurse and physician interaction and promotes critical thinking. In the past, nurses have not been asked to give an opinion or make a diagnosis. We need to encourage nurses to give their opinion. SBAR is very similar to the model many of us learned in medical school, with its focus on subjective, objective, assessment, and plan (SOAP).
Table 5.
The SBAR communication model
| Component | Explanation |
| S-Situation | What's the situation? Frame the conversation |
| B-Background | How did we get here? The context |
| A-Assessment | What do I think the problem is? |
| R-Recommendation | What are we going to do to fix it? When is that going to happen? |
Another way of looking at SBAR is for physicians to “Sit Back And Relax.” Nurses are making an effort to be prepared before they call physicians, so what physicians need to do is listen rather than interrupt. Nurses recognize that if they take a moment to get organized, it will make the communication even more effective.
“Stop the line.”
The stop the line initiative is being implemented at Baylor University Medical Center and across the country. The idea is that all those involved in a patient's care have the responsibility and authority to immediately intervene if they believe a patient's safety is at risk. The physician and the rest of the care team will immediately stop and respond to such a request by reassessing the patient's safety.
Although mistakes are inevitable, they are potentially reversible. Defects are mistakes that were not fixed soon enough and become permanent. It has been found that if you fix mistakes soon enough, your work will have zero defects. Mistakes are least harmful and easiest to fix the closer you get to the time and place they arise.
The basic strategy for stopping the line is to inspect, stop, and fix at the source. Every employee is an inspector. Every employee is empowered and can stop the line. The key phrase that we are spreading is “I need some clarity.” If you ever hear someone say, “I need some clarity,” then the right thing to do is to halt what you are doing and reevaluate. When you can't fix it on the spot, then you stop the procedure.
Disclosing errors to patients and their families.
A medical error should be disclosed to patients and their families whenever a mistake has clear or potential clinical significance or an unintended act or substance reaches the patient. Patients and their families want three things after a medical error: an honest explanation, an apology, and reassurance that it won't happen to anyone else. We respond accordingly by acknowledging the event, expressing regret, taking steps to minimize further harm to the patient, explaining what happens next to the patient or family, and committing to investigate to discover root causes for the error.
There has been some controversy as to whether or not we should apologize to patients. Most disclosure policies advocate an apology, because it shows the patient and family that you respect them. It shows that you are able to take responsibility for the situation. It demonstrates to others that you can be empathetic, and it helps dissipate anger. There are both pros and cons to the disclosure policy (Table 6). The “second victim” in disclosure can be the caregivers, whether physicians, nurses, or other health care professionals. These individuals may experience profound shame, guilt, and fear; they may have a compromised ability to deal with patients. The caregivers need support from colleagues.
Table 6.
Pros and cons of disclosure of medical errors
| Pros | Cons |
| What you would expect if it were you or your family | Fear of increased claims |
| May reduce lawsuits | Fear of negative reputation |
| Required by Joint Commission | Difficulty in assessing causality |
| Makes it okay to talk to other physicians about the event | Difficult emotionally to make disclosure and may not be in your skill set |
Several disclosure programs have been tried and have proved successful. One is COPIC Insurance Company's 3 R's program: Recognize, Respond, Resolve. In this program, physicians are encouraged to participate but are not required to do so. If they do participate, they are required to report within 24 hours if any error or harm has occurred or a patient or family is unhappy. In >1500 cases that were handled this way, the resolution rate was >99%—dealing directly with the patient and the family without attorneys. The average cost of settling a case was about $5000, and the settlement amount was not reportable to the National Practitioner Database. Disclosure was felt to be the right thing to do, as well as being advantageous to the physician and insurance company economically (10).
The Veterans Administration Hospital in Lexington, Kentucky, and the University of Michigan also have successful disclosure programs. In the Veterans Administration program, there were 88 claims in 7 years, with an average payout of $15,622—compared with a national average of $270,854 for settlement. The University of Michigan reported saving $2.2 million in defense costs in its first year of program implementation (10).
NATIONAL PATIENT SAFETY GOALS
Several of the Joint Commission's 2008 National Patient Safety Goals (11) relate to communication. One such goal is for patient identification: “Use at least two patient identifiers when providing care, treatment, or services.” At Baylor University Medical Center, nurses use full name and birth date. They check the identifiers before they give any medicines and draw any labs and before patients are transported for tests and procedures, for example.
The strategies of time-outs and read-backs of verbal orders and critical results are also among the National Patient Safety Goals:
Prior to the start of any invasive procedure, conduct a final verification process (such as a “time out”) to confirm the correct patient, procedure, and site, using active—not passive—communication techniques.
For verbal or telephone orders or for right, or both ears) telephonic reporting of critical test results, verify the complete order or test result by having the person receiving the information record and “read-back” the complete order or test result.
The Joint Commission has asked organizations to “standardize a list of abbreviations, acronyms, symbols, and dose designations that are not to be used.” Table 7 lists those abbreviations to be avoided within Baylor Health Care System. We have asked nurses on every floor to call physicians if they cannot read an order or if an unapproved abbreviation is used.
Table 7.
Abbreviations to be avoided in clinical documentation in hospitals of baylor health care System
| Unsafe term | Potential problem | Preferred term |
| AS, AD, AU (Latin abbreviations for left, right, or both ears) | Mistaken for OS, OD, and OU | Write “left ear,” “right ear,” or “both ears.” |
| HS | Mistaken for either half- strength or hour of sleep. “qHS” mistaken for every hour. | Write out “half-strength” or “at bedtime.” |
| IU (for International Unit) | Mistaken for IV (intravenous) or 10 (ten) | Write: “international unit.” |
| MS, MSO4, MgSO4 | Confused for one another. Can mean morphine sulfate or magnesium sulfate. | Write: “morphine sulfate” or “magnesium sulfate.” |
| QD, QOD (Latin abbreviations for once daily and every other day; upper or lower case, with or without periods) | Mistaken for each other. The period after the Q can be mistaken for an “I” and the “O” can be mistaken for an “I.” | Write: “daily” and “every other day.” |
| SQ or SC | Mistaken as SL for sublingual or “5 every” | Write “Sub-Q,” “subQ” or “subcutaneously” |
| U (for unit) | Mistaken as zero, four or cc | Write: “unit” (unit has no acceptable abbreviation) |
| Trailing zero (X.0 mg) (Note: Prohibited only for medication-related notations) Lacking a leading zero (.X mg) | Misreading of number | Never write a zero by itself after a decimal point (X mg) and always use a zero before a decimal point (0.X mg) |
Another goal relates to timeliness:
Measure, assess, and if appropriate, take action to improve the timeliness of reporting, and the timeliness of receipt by the responsible licensed caregiver, of critical tests and critical results and values.
Baylor's critical test result sheet has been modified to eliminate some test results that might not be critical. Everything on this new list is something physicians would want to know about, day or night. When a nurse calls with a critical test result, physicians need to respond with a verbal read-back. Then the nurse fills out a label, which is placed in the progress note, that gives the name of the patient, what the critical result was, who was notified, and whether the read-back was done. This procedure ensures compliance with the Joint Commission requirement about timeliness as well as the requirement for verification of critical laboratory results.
A final communication safety goal relates to hand-offs:
Implement a standardized approach to “hand off” communications, including an opportunity to ask and respond to questions.
Baylor is addressing hand-offs across the different areas of the hospital. The hand-off rule also applies to physicians. When one physician checks out patients to an associate, he or she is expected to provide some standard information. A hand-off is the transfer of information, along with authority and responsibility, during transitions in care across the continuum for the purpose of ensuring the continuity and safety of the patient's care. We're expected to exchange information about the patient's care, the treatment and services, the patient's current condition, and recent or anticipated changes. The hand-off must be interactive to allow the opportunity for questions. Many areas of the hospital are using a standardized approach to hand-offs, such as SBAR.
I also want to address three other National Patient Safety Goals: health care–associated infections, medication reconciliation, and the active involvement of patients.
The 2008 requirement for infections reads as follows: “Comply with current World Health Organization (WHO) hand hygiene guidelines or Centers for Disease Control and Prevention (CDC) hand hygiene guidelines.” Texas is one of a number of states that have mandated public reporting of infection rates. The simplest, cheapest, and most effective way to reduce hospital-related infections is to wash your hands. Our audits of hand-washing among different groups of hospital staff have shown that physicians are the least compliant (Table 8).
Table 8.
Handwashing compliance among different staff groups at Baylor University Medical Center
| Staff group | Observations (N) | Compliant (%) | Noncompliant (%) |
| Physicians | 153 | 37% | 63% |
| Nurses | 842 | 75% | 25% |
| Unit techs | 360 | 81% | 19% |
| Environmental services staff | 69 | 87% | 13% |
| Physical therapists | 73 | 82% | 18% |
| Pharmacists | 18 | 94% | 6% |
| Social workers | 10 | 60% | 40% |
| Respiratory therapists | 42 | 69% | 31% |
| Nutrition services staff | 14 | 79% | 21% |
| Patient transporters | 60 | 47% | 53% |
The medication reconciliation goal has two requirements:
There is a process for comparing the patient's current medications with those ordered for the patient while under the care of the organization.
A complete list of the patient's medications is communicated to the next provider of service when a patient is referred or transferred to another setting, service, practitioner or level of care within or outside the organization. The complete list of medications is also provided to the patient on discharge from the facility.
Some physicians think that the universal medication list is medication reconciliation, but it's not. Medication reconciliation is the whole process; filling out the list is only one part of that process. Although nurses and pharmacists can help fill out the universal medication list, physicians have ultimate responsibility for ensuring that medication reconciliation is done.
Patients should actively participate in their care. In this effort, patients need key points of information: the name of the nurse taking care of them, what is going to happen that day, and the plan for their care, both in and out of the hospital. Instead of reviewing these details, we often assume patients have them. A couple of sentences may alleviate patients' anxiety and reassure them.
ENGAGING PHYSICIANS IN A CULTURE OF SAFETY
Changing the health care culture and improving patient safety are not easy. Several barriers to these objectives exist. We work within a complex health care system that is specialized and often interdependent, and the culture of medicine emphasizes individualism and autonomy rather than teamwork. Physicians fear disclosure or admission of medical errors because of concerns about malpractice claims. In addition, there is a lack of strong safety measures for health care organizations to use as they try to change their systems. Finally, the reimbursement system inadvertently rewards errors by paying for additional costs due to error, without providing incentives to reduce recidivism and rework.
Despite the obstacles, improved patient safety is worth the effort involved. Beyond its obvious benefit to patients, patient safety has numerous other positive consequences. Many patient safety efforts conserve hospital resources and actually decrease costs. Measurable, documented improvement in patient safety has been shown to improve clinical outcomes and increase the staff's pride in the hospital system. Further, improved patient safety can be used as a powerful marketing tool, if handled appropriately. People are influenced by clinical outcomes and safety data. In the future, as pay for performance becomes more widespread, the hospital with a good safety culture will realize increased revenue, as will physicians.
However, all policies are useless without leadership support. Effective leaders model the values; their actions are consistent with their message. They tell front-line workers that safe care is important and their core business. They represent the difference between success and failure with many of the initiatives we spoke about.
So, for team training and patient safety, what's in it for you? Physicians have the potential of trapping errors, as well as an improved ability to do well with fewer delays and better outcomes. Nurses can realize better communication, leading to increased respect and being heard; administrators can see reduced staff turnover, fewer errors, and better data on potential hazards. Safety is the theme common to all groups, with fewer patient deaths and shorter hospital stays.
In conclusion, the organized medical staff is critical to many aspects of patient safety. Specific projects that achieve goals that are important to the medical staff are the key. Success occurs when the team is broadly based, with input from key physicians, administrators, nurses, and other hospital staff. Nearly all medical staffs and hospitals can benefit from such efforts.
Acknowledgments
I thank my wife for transcribing my grand rounds presentation.
Footnotes
Presented at internal medicine grand rounds, Baylor University Medical Center, on July 17, 2007.
References
- 1.Steiger B. Doctors say many obstacles block paths to patient safety. The Physician Executive 2007(May/June):6–14. Available at http://www.acpenet.org/MembersOnly/pejournal/2007/May_June/Steiger.pdf; accessed October 16, 2007. [PubMed]
- 2.Institute of MedicineKohn LT, Corrigan JM, Donaldson MS, editors. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 1999. [PubMed] [Google Scholar]
- 3.Institute of Medicine, Committee on Quality of Health Care in America . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 4.The Kaiser Family Foundation, Agency for Healthcare Research and Quality, Harvard School of Public Health. National Survey on Consumers' Experiences with Patient Safety and Quality Information, November 2004, Summary and Chart Pack Available at http://www.kff.org/kaiserpolls/upload/National-Survey-on-Consumers-Experiences-With-Patient-Safety-and-Quality-Information-Survey-Summary-and-Chartpack.pdf; accessed October 16, 2007.
- 5.Weick KE, Sutcliffe KM. Managing the Unexpected: Assuring High Performance in an Age of Complexity. San Francisco: Jossey-Bass; 2001. [Google Scholar]
- 6.Gibbs N, Bower A. What doctors hate about hospitals. Q: What scares doctors? A: Being the patient. Time, May 1, 2006. Available at http://www.time.com/time/magazine/article/0,9171,1186553,00.html; accessed October 16, 2007.
- 7.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 8.Leonard M, Frankel A, Simmonds T, Vega K. Achieving Safe and Reliable Healthcare: Strategies and Solutions. Chicago: Health Administration Press; 2004. [Google Scholar]
- 9.Joint Commission. Sentinel Event Statistics—June 30, 2007 Available at http://www.jointcommission.org/SentinelEvents/Statistics/; accessed October 17, 2007.
- 10.Leonard MW. Communicating unanticipated adverse events Presentation at the Patient Safety Officer Executive Development Program, Institute for Healthcare Improvement, March 12, 2007.
- 11.Joint Commission. 2008 National Patient Safety Goals Available at http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/; accessed October 17, 2007. [PubMed]