Abstract
The first 25 consecutive patients with high occlusal plane angulation, dysfunction, and pain who were treated with temporomandibular joint (TMJ) total joint prostheses and simultaneous maxillomandibular counterclockwise rotation were evaluated before surgery (T1), immediately after surgery (T2), and at the longest follow-up (T3) for surgical movements and long-term stability. Subjective ratings were used for patients' facial pain/headache, TMJ pain, jaw function, diet, and disability, and objective functional changes were determined by measuring maximum incisal opening and lateral excursive movements. Results showed that the areas of greatest surgical change included an average decrease in the occlusal plane of 13.3 degrees with advancement at point B of 13.4 mm and at the genial tubercles of 16.3 mm. At longest follow-up, relapse was 0.7 degrees, 0.8 mm, and 1.2 mm, respectively, with no statistically significant changes. Significant subjective pain and dysfunction improvements were observed (P ≤ 0.001). Maximum incisal opening increased, but lateral excursion decreased. Those who had two or more previous TMJ surgeries showed greater levels of dysfunction at T1 and T3 than those who had one or no previous surgeries, but otherwise patients presented similar amounts of absolute changes. In conclusion, end-stage TMJ patients can achieve significant improvement in their pain, dysfunction, dentofacial deformity, and airway problems in one operation with TMJ reconstruction and mandibular advancement using TMJ custom-made total joint prostheses and simultaneous maxillary osteotomies for maxillomandibular counter-clockwise rotation.
End-stage degeneration and destruction of the temporomandibular joint (TMJ) can occur as a result of trauma, osteoarthritis, reactive arthritis, failed previous surgeries, infection, ankylosis, idiopathic condylar resorption, connective tissue/autoimmune diseases (CTAD; e.g., rheumatoid arthritis, psoriatic arthritis, lupus, scleroderma, Sjogren's disease, ankylosing spondylitis), and other pathological TMJ conditions. The joint structures also can be destroyed from alloplastic implants such as Proplast-Teflon (Vitek Inc, Houston, TX), Silastic (Dow-Corning Inc, Midland, MO), acrylic, and bone cements (1–4). These TMJ pathologies can result in retrusion of the mandible, loss of vertical height of the ramus secondary to condylar resorption, anterior open bite, Class II malocclusion, increased occlusal and mandibular plane angulations, limited jaw function, masticatory dysfunction, alteration of speech, decreased oropharyngeal airway, sleep apnea, and mild, moderate, or severe pain.
In some patients, multiple TMJ procedures have failed, usually related to inappropriate selection of surgical procedures for the existing TMJ pathology. Some patients who have repeated orthognathic surgery in an attempt to correct the malocclusion and jaw deformity experience later relapses because of unrecognized or ignored TMJ pathology, resulting in further TMJ degenerative and destructive changes. Patients with two or more previous failed TMJ surgical procedures, inflammatory TMJ pathology (i.e., CTAD, reactive arthritis), or foreign body giant cell reactions (FBGCR) (related to failed alloplastic implants) have a very high failure rate with TMJ reconstruction using autogenous tissues (1, 5, 6). In such patients with end-stage TMJ pathologies, custom-made total joint prostheses may be indicated for simultaneous TMJ reconstruction and correction of the functional and aesthetic problems associated with the mandible (1, 5, 7). A coexisting maxillary deformity can be corrected at the same operation by performing maxillary osteotomies to optimize functional and aesthetic outcomes.
The custom-made total joint prostheses used in this study were originally developed in 1989 by Techmedica Inc. (Camarillo, CA) and since 1996 have been manufactured by TMJ Concepts Inc. (Ventura, CA). These prostheses are CAD/CAM devices (computer-assisted design/computer-assisted manufacture), designed to fit the specific anatomical requirements for each patient. The characteristics important for TMJ total joint prostheses to be successful as well as the design and composition of these prostheses have been previously reported (8–15).
Patients requiring the type of surgical treatment presented in this paper usually have 1) nonsalvageable TMJ pathology, 2) major retrusion of the mandible, 3) retrusion of the maxilla, 4) anterior vertical maxillary excess and/or posterior vertical maxillary deficiency, 5) high occlusal plane angulation, 6) TMJ and jaw dysfunction, and 7) pain and headaches. In addition, patients may have a Class II occlusion, anterior open bite, and decreased oropharyngeal airway causing sleep apnea in the more severe cases.
In 1990, Wolford (1, 5) developed the treatment philosophy, surgical techniques, and protocol applied in this study. Custom-made total joint prostheses were used for simultaneous TMJ reconstruction and mandibular advancement with concomitant maxillary osteotomies at the same operation for counter-clockwise rotation of the maxillomandibular complex to optimize the functional and aesthetic outcomes as well as reduce pain. The purpose of this study was to evaluate patient outcomes utilizing this treatment protocol.
PATIENTS AND METHODS
This prospective study had three inclusion criteria: 1) counter-clockwise rotation of the maxillomandibular complex with a mandibular occlusal plane angle surgical change of ≥5 degrees; 2) TMJs reconstructed and mandible advanced with custom-made TMJ Concepts/Techmedica total joint prostheses; and 3) simultaneous maxillary osteotomies. Twenty-five consecutive patients (24 women and 1 man) with 49 joints (1 patient had a unilateral prosthesis and a mandibular ramus sagittal osteotomy on the opposite side) who met these requirements were analyzed to determine outcome results and long-term stability.
The average age at surgery was 36.2 years (range, 15 to 56 years), and postsurgical follow-up averaged 2.64 years (range, 1 to 4.6 years). All patients were operated on by the same surgeon (LMW), and all procedures were performed at one operation. Fat grafts were placed around the TMJ prostheses in five patients.
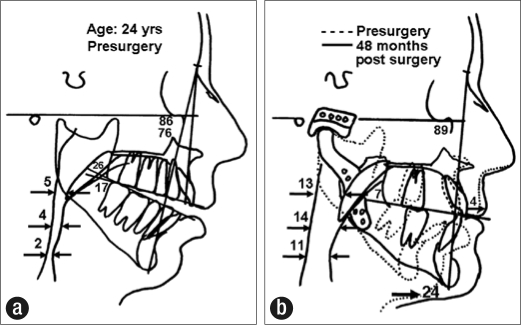
Lateral cephalometric radiographs at T1 (before surgery), T2 (immediately after surgery), and T3 (longest follow-up) were traced for analysis. Superimposition of the radiographic tracings on the stable cranial base structures was used to determine surgical change (T2 – T1) and long-term stability (T3 – T2). Specific anatomical points were identified to determine the following: 1) occlusal plane angle change, 2) anteroposterior change of point A, 3) anteroposterior change of point B, 4) anteroposterior change of the genial tubercles, 5) anteroposterior change of upper incisor, 6) vertical change of upper incisor, 7) anteroposterior change of upper first molar, and 8) vertical change of upper first molar (Figure 1). All cephalometric tracings were performed by one individual (ORM), who was not involved in any way with patient care.
Figure 1.
Cephalometric tracings included cranial base structures and nine anatomical landmarks for specific analysis.
Objective functional results were determined by measuring the maximum incisal opening (MIO) and lateral excursive movements at T1 and T3. MIO measurements were taken with the jaws at maximum opening without assistance, measuring from incisor tips of the lower and upper incisors. In cases of anterior open bite, the amount of open bite was subtracted from the maximal opening value to calculate the actual opening. In patients with anterior overbites, the amount of vertical dental overlap was added to the opening to calculate the actual opening. Pain assessment was subjectively analyzed, using a numerical pain intensity scale (0 = no pain, 10 = worst pain imaginable), before surgery and at the latest follow-up evaluation. A paired t test was applied to determine the level of significance (P < 0.05) for subjective changes.
Patients were divided into two groups according to the number of previous surgeries: group 1 had no more than one previous surgery (n = 10), and group 2 had two or more previous surgeries (n = 15).
Surgical technique
Three patients required a preliminary surgical stage to remove previously placed, failed total joint prostheses that contained metal, so that an accurate computed tomography (CT) scan could be taken. Metal in the TMJ and/or ramus can cause interference in the CT scan imaging data and significantly distort the three-dimensional plastic model on which the custom-made total joint prostheses are made. The CT scan extended from superoposterior to the TMJ to anterior to the chin, maxilla, and inferior orbital rim areas.
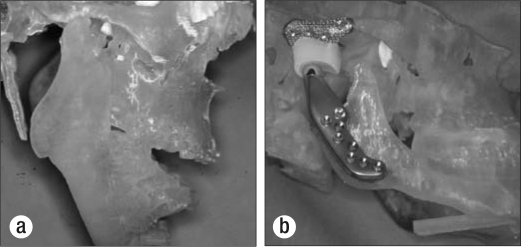
A three-dimensional CAD/CAM plastic model was then created (Figure 2a). A surgical prediction tracing was developed from a presurgical lateral cephalometric radiograph to determine the desired final position of the maxilla and mandible. The CAD/CAM model was mounted on an anatomical articulator, and precise model surgery was performed to reposition the mandible to the desired postsurgical position relative to the unoperated maxilla. Once the mandibular position was achieved, the mandible was secured to the maxilla by placing quick-cure acrylic interocclusally to lock in the position of the mandible. The condyles were cut off and, if indicated, bony recontouring of the fosse and lateral aspect of the rami was completed. Any recontouring on the CAD/CAM model had to be accurately duplicated on the patient at the time of surgery. The custom-made total joint prostheses were then manufactured from the CAD/CAM model to fit the patient's specific anatomical requirements (Figure 2b).
Figure 2.
(a) A CAD/CAM model of the patient's TMJs and jaws was generated for subsequent manufacturing of the TMJ Concepts/Techmedica custom-made total joint prosthesis. (b) The mandible on the model was repositioned to its predetermined position relative to the unoperated maxilla. Fosse and rami were recontoured if necessary, and a custom-made total joint prosthesis was manufactured.
Immediately prior to surgery, the mandibular movements done on the CAD/CAM model were accurately duplicated on anatomically mounted dental models, and an intermediate splint was constructed to aid in repositioning the mandible (16). At surgery, an endaural or preauricular approach was used to perform the condylectomy, joint debridement, coronoidectomy to release the temporalis muscle, and, if indicated, accurate bony recontouring of the fossa as dictated by the recontouring done on the CAD/CAM model. In some cases, the lateral pterygoid muscle was to be reattached to the prosthesis, so a 2-0 monofilament nylon suture or braided polyester suture was passed in a multiple mattress fashion through the lateral pterygoid muscle, prior to placement of the prosthesis components, for later securing of the muscle to the prosthetic condylar neck.
Through a submandibular approach, the pterygomasseteric sling was reflected off the mandibular ramus and lateral recontouring completed as indicated from the CAD/CAM model. The mandible was then mobilized and repositioned using the intermediate splint, and intermaxillary fixation was applied. The fossa component was inserted through the endaural/preauricular incision and stabilized to the zygomatic arch with three to four 2-mm diameter bone screws. The mandibular prosthetic component was inserted through the submandibular incision and stabilized to the ramus with eight to twelve 2-mm diameter bone screws. The suture previously placed through the lateral pterygoid muscle was looped around the neck of the mandibular component to secure the muscle to the prosthesis. In five patients, fat grafts were harvested from the abdomen and packed around the articulating area of the prosthesis to help prevent fibrosis and heterotopic/reactive bone formation after surgery (17). The incisions were closed.
Multiple maxillary osteotomies were then performed to establish the best possible functional and aesthetic result, since before surgery the maxilla was usually retruded anteroposteriorly as well as had anterior vertical maxillary excess and/or posterior vertical maxillary deficiency with a high occlusal plane angulation. The maxilla was stabilized with bone plates and porous block hydroxyapatite grafts (PBHA, Interpore 200, Interpore Inc, Irvine, CA) (17–19). After surgery, light interarch elastics were used to help support the mandible, since the muscles of mastication were reflected from the mandible and were initially nonfunctional. Postoperative elastics were generally discontinued following adequate functional return of the pterygomasseteric musculature (usually 2 to 4 weeks after surgery), unless required for finishing orthodontic mechanics. Passive physical therapy was used on all patients beginning approximately 6 to 8 weeks after surgery. Patients were instructed to open and close their jaws and begin shifting their jaws from side to side four to five sessions per day for 10 to 15 minutes each session.
When indicated, procedures such as genioplasty, turbinectomies, nasoseptoplasty, and rhinoplasty were performed at the same surgery. Many of these patients, particularly those with significant retrognathia, had moderate to severe presurgical sleep apnea symptoms because of the decreased oropharyngeal airway. The suprahyoid muscles were not deliberately detached from the genial tubercles in any of the cases. Alloplastic materials such as PBHA or HTR (Hard Tissue Replacement, Walter Lorenz Inc, Jacksonville, FL) were used for augmentation genioplasties.
RESULTS
For the 25 patients in this study, the average decrease in the occlusal plane angle was 13.3 degrees, with a long-term stability change of 0.7 degrees, for a comparative change relative to the surgical change of 5.3%. The average advancement at point B was 13.4 mm, with a long-term stability change of 0.8 mm, for a comparative change of 5.9%. The average mandibular advancement at the genial tubercles was 16.3 mm, with a long-term stability change of 1.2 mm, for a comparative change of 7.4%. There were no statistically significant changes in any of these parameters from the immediate postsurgery period to the date of longest follow-up. Changes in maxillary and dental positions were mixed with combinations of superior, inferior, forward, and/or backward movements, creating smaller numerical values for averaged movements. Specific changes can be seen in Table 1, denoting overall good stability.
Table 1.
Surgical and long-term positional changes in 25 patients after treatment with custom-made TMJ prostheses and maxillomandibular counter-clockwise rotation
| Variable | Surgical change (T3 − T1) | Long-term change (T3 − T2) | Comparative change |
| Occlusal plane angle alteration: degrees (range) | 13.3 (6 to 28) | 0.7 (−2 to 2.5) | 5.3% |
| Anteroposterior change of point A: mm (range) | 2.2 (−2 to 6) | −0.1 (−1 to 1) | 4.5% |
| Anteroposterior change of point B: mm (range) | 13.4 (4 to 25) | 0.8 (−2 to 3) | 5.9% |
| Anteroposterior change of genial tubercles: mm (range) | 16.3 (7 to 29) | 1.2 (−3 to 5) | 7.4% |
| Anteroposterior change of upper incisor: mm (range) | 5.2 (1 to 10) | 0.2 (−2 to 2) | 3.8% |
| Vertical change of upper incisor: mm (range) | 1.7 (−6 to 7) | 0.5 (−1 to 2) | 29.4% |
| Anteroposterior change of upper first molar: mm (range) | 5.2 (1 to 12) | 0.5 (−2 to 2) | 9.6% |
| Vertical change of upper first molar: mm (range) | 2.8 (−2 to 10) | −0.3 (−2 to 1) | 10.7% |
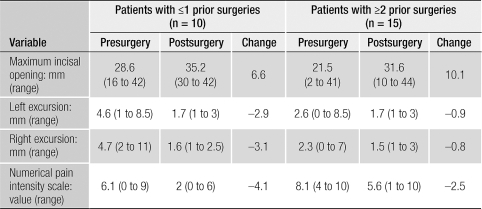
The patients were divided into two groups for function and pain results: group 1 had 0 to 1 previous TMJ surgeries (n = 10), and group 2 had ≥2 previous TMJ surgeries (n = 15). The average MIO for group 1 was 28.6 mm at T1 and 35.2 mm at T3, for an increase of 6.6 mm. One third of group 2 patients presented some degree of ankylosis. The average MIO for group 2 was 21.5 mm at T1 and 31.6 mm at T3, for an increase of 10.1 mm. For group 1, the average left lateral excursion was 4.6 mm at T1 and 1.7 mm at T3; the average right lateral excursion was 4.7 mm at T1 and 1.6 mm at T3. For group 2, the average left lateral excursion was 2.6 mm at T1 and 1.7 mm at T3; the average right lateral excursion was 2.3 mm at T1 and 1.5 mm at T3. The average pain level for group 1 was 6.1 at T1 and 2 at T3, an average decrease of 4.1 points. The average pain level for group 2 was 8.1 at T1 and 5.6 at T3, an average decrease of 2.5 points (Table 2). Significant subjective pain and dysfunction improvements were observed (P < 0.001) for both groups. All patients were satisfied with the aesthetic and airway results.
Table 2.
Function and pain changes after treatment with custom-made TMJ prostheses and maxillomandibular counter-clockwise rotation, comparing patients based on number of prior surgeries
CASE REPORTS
Case 1
A 24-year-old woman was referred after previous failed bilateral TMJ surgery, maxillary osteotomies, and genioplasty (Figures 3a, 3b, 4a, 4b, 5a). She reported problems with other joints, and a nonspecific CTAD was diagnosed during a rheumatology evaluation. Magnetic resonance imaging showed severe condylar resorption and a reactive pannus surrounding the TMJ articular discs. Her surgical diagnoses included 1) severe bilateral condylar resorption, 2) maxillary anteroposterior and posterior vertical hypoplasia, 3) severe anteroposterior mandibular hypoplasia, 4) Class II occlusion with severe apertognathia (7 mm), 5) decreased oropharyngeal airway causing sleep apnea, 6) severe masticatory dysfunction, and 7) severe TMJ and myofascial pain.
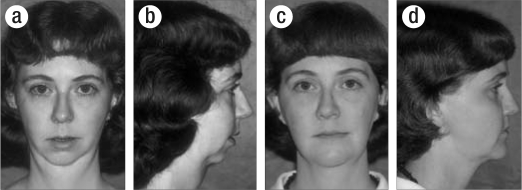
Figure 3.
Case 1. (a) This 24-year-old woman with nonspecific connective tissue/autoimmune disease had previous failed TMJ and orthognathic surgery, with a resultant significant dentofacial deformity. (b) The maxilla was anteroposteriorly deficient and the mandible was severely retruded. (c, d) Four years after surgery, this patient demonstrated good facial balance.
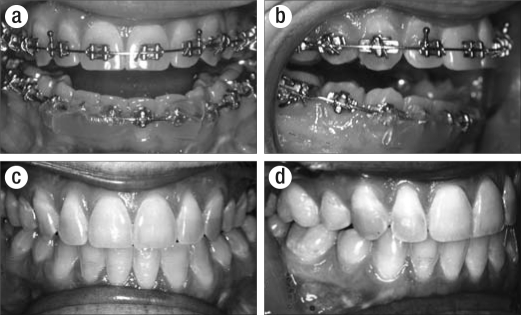
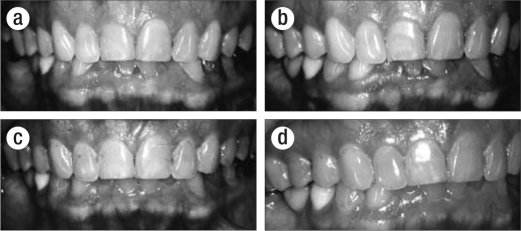
Figure 4.
Case 1. (a, b) This patient had a large anterior open bite (7 mm) and Class II end-on occlusion with only the second molars occluding. (c, d) Four years after surgery, this patient maintained a good Class I occlusion.
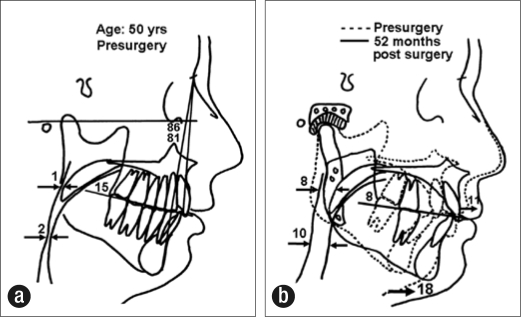
Figure 5.
Case 1. (a) Presurgical cephalometric analysis showed skeletal and occlusal Class II anterior open bite (7 mm), a high occlusal plane angle, and a significantly reduced oropharyngeal airway. (b) Four years after surgery, the analysis showed improved facial balance, elimination of the anterior open bite, and a significantly increased oropharyngeal airway. The counter-clockwise rotation of the maxillomandibular complex and chin implant advanced pogonion 24 mm.
Four surgical procedures were performed: 1) bilateral TMJ reconstruction and mandibular advancement in a counterclockwise direction utilizing the TMJ Concepts/Techmedica custom-made total joint prostheses with the rami lengthened 17 mm and the chin (pogonion) advanced 24 mm; 2) bilateral coronoidectomies; 3) multiple maxillary osteotomies with the maxillary incisor tips advanced 7 mm and the posterior maxilla inferiorly positioned 5 mm stabilized with bone plates and PBHA grafts; and 4) PBHA chin augmentation. The mandibular occlusal plane was surgically decreased 19 degrees.
At 4 years postsurgery, the patient maintained a stable facial balance and occlusion (Figures 3c, 3d, 4c, 4d, 5b). Her incisal opening improved from 24 mm before surgery to 42 mm after surgery. Pain levels decreased from 9 at T1 to 1 at T3. The sleep apnea was resolved, and the patient could eat relatively normally. Because this patient had had only one previous TMJ surgery and had no Proplast-Teflon or Silastic implants placed in her TMJs, her postsurgical prognosis and result were predictably very good.
Case 2
A 50-year-old woman had a preexisting retrusion of the maxilla and mandible, but her TMJ problems began following an automobile accident. She was referred after four failed bilateral TMJ surgeries, including the placement of Proplast-Teflon TMJ interpositional implants. She had severe sleep apnea associated with her retruded mandible and maxilla (Figures 6a, 6b, 7a, 7b, 8a). Although a direct correlation could not be proven in this case, following her exposure to Proplast-Teflon, she developed multiple sclerosis, polyarthralgia, fibromyalgia, seizure disorder, and severe dysfunction of her immune system. She had bilateral TMJ arthritis and a significant TMJ FBGCR but had relatively minimal condylar resorption. Her surgical diagnoses included 1) bilateral TMJ arthritis and Proplast-Teflon interpositional implants, 2) mandibular hypoplasia, 3) maxillary anteroposterior and posterior vertical hypoplasia, 4) TMJ pain, 5) headaches, 6) myofascial pain, 7) decreased oropharyngeal airway causing severe sleep apnea, and 8) severe masticatory dysfunction.
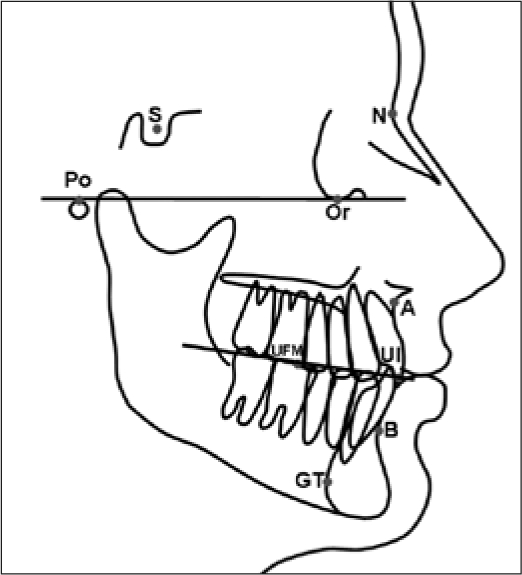
Figure 6.
Case 2. (a, b) This 50-year-old woman had four failed bilateral TMJ surgeries, including Vitek Proplast-Teflon implants. In addition, she had severe sleep apnea related to the retruded maxilla and mandible. (c, d) Improved facial balance was evident 4½ years after surgery.
Figure 7.
Case 2. (a, b) The patient had a Class I occlusion before surgery. (c, d) At 4½ years after surgery, the patient maintained a good occlusion.
Figure 8.
Case 2. (a) Cephalometric analysis showed retrusion of the maxilla and mandible, a high occlusal plane angle, and a severely decreased oropharyngeal airway. (b) The counter-clockwise rotation of the maxillomandibular complex advanced pogonion 18 mm. The oropharyngeal airway opened 8 to 10 mm, eliminating her severe sleep apnea.
Four surgical procedures were performed at one operation: 1) bilateral TMJ removal of Proplast-Teflon implants, condylectomies, and extensive debridement; 2) bilateral TMJ reconstruction and mandibular advancement utilizing the TMJ Concepts/Techmedica custom-made total joint prostheses with the rami lengthened 12 mm and the chin (pogonion) advanced 18 mm; 3) bilateral coronoidectomies; and 4) multiple maxillary osteotomies with the incisor tips advancing 11 mm and the posterior maxilla inferiorly positioned 4 mm. The occlusal plane was decreased 7 degrees.
The patient was followed for 4½ years after surgery with good stable occlusion and facial balance (Figures 6c, 6d, 7c, 7d, 8b). Her incisal opening improved from 22 mm at T1 to 35 mm at 1 year postsurgery, but at longest follow-up, the incisal opening was 28 mm. Pain levels decreased from 9 at T1 to 5 at T3. The sleep apnea was completely resolved, and the patient could eat better. Because this patient had four previous bilateral TMJ surgeries, including Proplast-Teflon implants placed in her TMJs, her postsurgical prognosis and results are predictably compromised relative to pain and jaw function (1, 5).
DISCUSSION
Previous reports have documented the effectiveness of custom-made total joint prostheses for TMJ reconstruction (5, 7, 15). Wolford, Cottrell, and Henry (5) presented a study of 56 consecutive patients, with 100 reconstructed TMJs, using the Techmedica custom-made total joint prostheses, with follow-up that averaged 30 months (range, 16 to 46 months). The outcome groups were categorized as good, fair, or poor, based on clinical assessment criteria for stability, function, and pain. Outcomes were good in 35 patients (63%), fair in 13 patients (23%), and poor in 8 patients (14%). Among patients with 0 or 1 previous TMJ surgeries, 86% had good results, 14% fair, and 0% poor. For patients with 2 or more previous surgeries, 55% had good results, 26% fair, and 19% poor. Thirty percent of the patients (17/56) received further operations for joint debridement because of heterotopic bone formation, fibrosis, calcification, inflammation, and/or pain, which occurred predominantly in patients who had several prior operations and/or had previous Proplast-Teflon or Silastic implants. The TMJ Concepts/Techmedica total joint prostheses remained in position. The continued pain was associated predominantly with the poor outcome group, which may be related to problems associated with the Proplast-Teflon, Silastic, and acrylic implants or other factors causing conditions such as continued FBGCR, cervical neuropathy, polyneuropathy, reflex sympathetic dystrophy, residual inflammatory or immunological reaction to alloplastic particles (i.e., Proplast-Teflon, Silastic, acrylic), fibrosis, calcification, heterotopic bone, and CTAD (20).
When Proplast-Teflon or Silastic implants are placed in the TMJ, extensive particulization occurs. Microscopic particles are disseminated throughout the TMJ and adjacent hard and soft tissues, causing a localized but often proliferative FBGCR that can destroy the affected hard and soft tissues. Destruction of the condyles by the FBGCR often causes the mandible to become more retruded, with a tendency to develop a Class II occlusion and anterior open bite. Proplast-Teflon implants generally create a far greater FBGCR reaction than Silastic implants. The extensive dissemination of the particles and the FBGCR make it impossible to completely remove this pathology during the TMJ debridement portion of the surgery (4, 20–23). Therefore, the FBGCR remains in the region following TMJ reconstruction, causing a continued inflammatory reaction and invasion of the local neurological innervation, contributing to the continued postsurgical pain (1, 20, 21).
Mercuri et al (7) reported a multicenter study of 215 patients (202 women and 13 men), with an average age at reconstruction of 40.9 years (range, 15 to 77 years). There were 363 total joint prostheses placed: 296 bilateral and 67 unilateral. The patients had presurgical TMJ problems for an average of 10.3 years (range, 1 to 44 years). The number of previous unsuccessful TMJ surgeries averaged 5.4 (range, 0 to 28). Postsurgery data were collected for up to 48 months, and the results revealed a statistically significant decrease in pain, increase in function, and improvement in diet (P < 0.0001) as well as increase in incisal opening. The number of previous surgeries was a strong predictor of postsurgery pain, function, diet scores, and MIO. The life table analysis indicated good durability of the prostheses over time.
Wolford, Chemello, and Hilliard (24, 25) previously reported on alteration of the occlusal plane to maximize functional and aesthetic results in patients with healthy and stable TMJs. Twenty-seven patients underwent double-jaw surgery for counter-clockwise rotation of the maxillomandibular complex. The mean follow-up was 21 months, with an average occlusal plane change of 8.8 degrees. Point B and pogonion advanced an average of 8 mm and 10 mm, respectively. The maxilla moved superiorly an average of 3 mm at point A, and the maxillary first molars showed no significant vertical movement. The immediate postsurgical changes compared with long-term follow-up demonstrated no statistically significant horizontal movement of the mandible. There were statistically significant but clinically undetectable changes for the horizontal position of point A (–0.5 mm average change), and the posterior maxilla settled superiorly an average of 1 mm. This study confirmed good long-term stability when decreasing the occlusal plane angulation by counter-clockwise rotation of the maxillomandibular complex in the presence of healthy and stable TMJs (26).
This current study demonstrates good stability with the use of the TMJ Concepts/Techmedica custom-made total joint prostheses to provide advancement and counter-clockwise repositioning of the maxillomandibular complex as well as reconstruction of the TMJs. Pain level improvement was less striking as the number of previous TMJ surgical procedures increased. Patients who had 0 or 1 previous surgeries did significantly better relative to pain levels as well as incisal opening. The reason for this finding may be multifactorial. Only 2 of the 10 patients in group 1 had alloplastic materials such as Proplast-Teflon or Silastic in their joints, whereas in group 2, 11 of the 15 patients had previous exposure to Proplast-Teflon and/or Silastic TMJ implants. The implants were in the form of inter-positional disc implants or Vitek-Kent total joint prostheses. Exposure of patients to these materials precludes the ability to completely eliminate pain because of FBGCR, inflammation, reactive heterotopic bone formation, sympathetic neuropathy, autoimmune polyneuropathy, and multiple chemical sensitivity (1, 5, 20, 21). Genetic predisposition to connective tissue and autoimmune diseases may make some of these patients more reactive to alloplastic material, including intractable pain problems (20, 21).
The incisal opening was greater at T1 and also at T3 for group 1 compared with group 2. However, overall, group 2 showed greater improvement in the amount of incisal opening gained, which may be attributed to the fact that a third of group 2 patients had a presurgical component of bony ankylosis. Although excursive movements at T1 were greater in group 1 compared with group 2, the T3 excursive movements decreased significantly and were almost identical between the two groups. It is expected that there will be limited excursive movements postsurgery, with a range of approximately 1 to 3 mm. This is related to the total joint prostheses, muscle detachments, and fibrosis around the joints and is not related to the alteration of the occlusal plane angle. Attachment of the lateral pterygoid muscle to the prostheses did not improve excursive movements, and thus we no longer include the muscle reattaching procedure.
As these significant counter-clockwise rotations are performed, particularly when the position of the ramus is elongated vertically, the muscles of mastication must be reflected from the ramus of the mandible and a coronoidectomy performed to release the temporalis muscle. These procedures allow the ramus of the mandible to rotate inferiorly and advance forward to increase the vertical length and anteroposterior position of the ramus. Following placement of the prosthesis, the pterygomasseteric sling is repositioned down towards the inferior border of the ramus and sutured into the best position. The muscles usually reattach at a level higher on the ramus than their original position. No functional testing of the masticatory abilities after these procedures has yet been done, although dietary self-regulation in some patients seems more related to functional pain than to lack of muscular strength. The mechanical leverage in many of these cases has been significantly altered, but the effects of this have not been studied.
Only 5 of the 25 patients in this study had fat grafts placed in the TMJs around the prostheses. The sample size was too small for statistical analysis of this factor in this study. However, Wolford and Karras (17) reported improved pain levels and jaw function with the use of fat grafts. Their comparative study with closely matched patient samples of nongrafted patients (n = 20) and fat-grafted patients (n = 15) revealed that 30% of the nongrafted patients required additional surgery for heterotopic bone formation and fibrosis, whereas none of the fat-grafted patients required further surgery by the end of the study. Fat grafts packed around the articulating area of the TMJ prostheses can eliminate dead space, preventing blood clot formation. Blood clots can provide a matrix for fibrous ingrowth and pluripotential cell migration into the area, which could lead to development of bone and dense fibrotic tissues (27). Also, in patients with previous Proplast-Teflon or Silastic implants, the fat grafts block out large areas in which FBGCR could redevelop (17). A subsequent study will follow incorporating this technique.
CONCLUSIONS
Custom-made TMJ total joint prostheses, with proper design and use of materials well proven in orthopedic prostheses, can be used to simultaneously reconstruct the TMJs and advance the mandible in a counter-clockwise direction. Maxillary osteotomies may also be required to establish optimal functional and aesthetic outcomes and can be performed at the same operation. With these procedures, patients can expect a decrease in pain and increase in incisal opening, but a decrease in lateral excursive movements. Patients with multiple prior TMJ operations have poorer outcomes relative to pain and function; the higher the number of prior operations, the greater the decline in outcome. Patients who had previous alloplasts in the TMJs, including Proplast-Teflon and Silastic implants, may have significantly compromised outcomes, although they still see improvement.
References
- 1.Henry CH, Wolford LM. Treatment outcomes for temporomandibular joint reconstruction after Proplast-Teflon implant failure. J Oral Maxillofac Surg. 1993;51(4):352–358; discussion 359–360. doi: 10.1016/s0278-2391(10)80343-x. [DOI] [PubMed] [Google Scholar]
- 2.Acton C, Hoffman G, McKenna H, Moloney F. Silicone-induced foreign-body reaction after temporomandibular joint arthroplasty. Case report. Aust Dent J. 1989;34(3):228–232. doi: 10.1111/j.1834-7819.1989.tb00675.x. [DOI] [PubMed] [Google Scholar]
- 3.Florine BL, Gatto DJ, Wade ML, Waite DE. Tomographic evaluation of temporomandibular joints following discoplasty or placement of polytetrafluoroethylene implants. J Oral Maxillofac Surg. 1988;46(3):183–188. doi: 10.1016/0278-2391(88)90080-8. [DOI] [PubMed] [Google Scholar]
- 4.Timmis DP, Aragon SB, van Sickels JE, Aufdemorte TB. Comparative study of alloplastic materials for temporomandibular joint disc replacement in rabbits. J Oral Maxillofac Surg. 1986;44(7):541–554. doi: 10.1016/s0278-2391(86)80094-5. [DOI] [PubMed] [Google Scholar]
- 5.Wolford LM, Cottrell DA, Henry CH. Temporomandibular joint reconstruction of the complex patient with the Techmedica custom-made total joint prosthesis. J Oral Maxillofac Surg. 1994;52(1):2–10. doi: 10.1016/0278-2391(94)90003-5. [DOI] [PubMed] [Google Scholar]
- 6.Bradrick JP, Indresano AT. Failure rates of repetitive temporomandibular joint surgical procedures. J Oral Maxillofac Surg. 1992;50(Suppl 3):145. [Google Scholar]
- 7.Mercuri LG, Wolford LM, Sanders B, White RD, Hurder A, Henderson W. Custom CAD/CAM total temporomandibular joint reconstruction system: preliminary multicenter report. J Oral Maxillofac Surg. 1995;53(2):106–115. doi: 10.1016/0278-2391(95)90381-x. [DOI] [PubMed] [Google Scholar]
- 8.Black J, Sholtes V. Biomaterial aspects of surface replacement arthroplasty of the hip. Orthop Clin North Am. 1982;13(4):709–728. [PubMed] [Google Scholar]
- 9.Williams DF. Tissue reaction to metallic corrosion products and wear particles in clinical orthopaedics. In: Williams DF, editor. Biocompatibility of Orthopedic Implants. I. Boca Raton, FL: CRC; 1981. pp. 231–248. [Google Scholar]
- 10.Hastings GW. Biocompatibility of polyethylenes and polypropylene. In: Williams DF, editor. Biocompatibility of Clinical Implant Materials. II. Boca Raton, FL: CRC; 1981. pp. 43–58. [Google Scholar]
- 11.Williams DF. The properties and clinical uses of cobalt-chromium alloys. In: Williams DF, editor. Biocompatibility of Clinical Implant Materials. I. Boca Raton, FL: CRC; 1981. pp. 99–127. [Google Scholar]
- 12.Williams DF. Titanium and titanium alloys. In: Williams DF, editor. Biocompatibility of Clinical Implant Materials. I. Boca Raton, FL: CRC; 1981. pp. 9–44. [Google Scholar]
- 13.Mercuri LG. The TMJ Concepts patient fitted total temporomandibular joint reconstruction prosthesis. Oral Maxillofac Surg Clin North Am. 2000;12(1):73–91. [Google Scholar]
- 14.Mercuri LG. The use of alloplastic prostheses for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 2000;58(1):70–75. doi: 10.1016/s0278-2391(00)80020-8. [DOI] [PubMed] [Google Scholar]
- 15.Wolford LM, Pitta MC, Reiche-Fischel O, Franco PF. TMJ Concepts/Techmedica custom-made TMJ total joint prosthesis: 5-year follow-up study. Int J Oral Maxillofac Surg. 2003;32(3):268–274. doi: 10.1054/ijom.2002.0350. [DOI] [PubMed] [Google Scholar]
- 16.Cottrell DA, Wolford LM. Altered orthognathic surgical sequencing and a modified approach to model surgery. J Oral Maxillofac Surg. 1994;52(10):1010–1020. doi: 10.1016/0278-2391(94)90164-3. [DOI] [PubMed] [Google Scholar]
- 17.Wolford LM, Karras SC. Autologous fat transplantation around temporomandibular joint total joint prostheses: preliminary treatment outcomes. J Oral Maxillofac Surg. 1997;55(3):245–251. doi: 10.1016/s0278-2391(97)90535-8. [DOI] [PubMed] [Google Scholar]
- 18.Wolford LM, Wardrop RW, Hartog JM. Coralline porous hydroxylapatite as a bone graft substitute in orthognathic surgery. J Oral Maxillofac Surg. 1987;45(12):1034–1042. doi: 10.1016/0278-2391(87)90160-1. [DOI] [PubMed] [Google Scholar]
- 19.Wardrop RW, Wolford LM. Maxillary stability following downgraft and/or advancement procedures with stabilization using rigid fixation and porous block hydroxyapatite implants. J Oral Maxillofac Surg. 1989;47(4):336–342. doi: 10.1016/0278-2391(89)90333-9. [DOI] [PubMed] [Google Scholar]
- 20.Wolford LM, Henry CH, Nikaein A, Newman JT, Namey TC. The temporomandibular joint alloplastic implant problem. In: Sessle BJ, Bryant PS, Dionne RA, editors. Temporo-mandibular Disorders and Related Pain Conditions. Seattle, WA: IASP Press; 1995. pp. 443–447. [Google Scholar]
- 21.Wolford LM. Temporomandibular joint devices: treatment factors and outcomes. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83(1):143–149. doi: 10.1016/s1079-2104(97)90105-0. [DOI] [PubMed] [Google Scholar]
- 22.Ryan DE. Alloplastic implants in the temporomandibular joint. Oral Maxillofac Surg Clin North Am. 1989;1:427–441. [Google Scholar]
- 23.Yih WY, Merrill RG. Pathology of alloplastic interpositional implants in the temporomandibular joint. Oral Maxillofac Surg Clin North Am. 1989;1:415–426. [Google Scholar]
- 24.Wolford LM, Chemello PD, Hilliard FW. Occlusal plane alteration in orthognathic surgery. J Oral Maxillofac Surg. 1993;51(7):730–740. doi: 10.1016/s0278-2391(10)80410-0. [DOI] [PubMed] [Google Scholar]
- 25.Wolford LM, Chemello PD, Hilliard F. Occlusal plane alteration in orthognathic surgery—Part I: Effects on function and esthetics. Am J Orthod Dentofacial Orthop. 1994;106(3):304–316. doi: 10.1016/S0889-5406(94)70051-6. [DOI] [PubMed] [Google Scholar]
- 26.Chemello PD, Wolford LM, Buschang PH. Occlusal plane alteration in orthognathic surgery—Part II: Long-term stability of results. Am J Orthod Dentofacial Orthop. 1994;106(4):434–440. doi: 10.1016/S0889-5406(94)70066-4. [DOI] [PubMed] [Google Scholar]
- 27.Thomas BJ. Heterotopic bone formation after total hip arthroplasty. Orthop Clin North Am. 1992;23(2):347–358. [PubMed] [Google Scholar]