Abstract
Background
Researchers have not examined relationships between perception of physical functional disability and demographic, clinical, and psychological variables at 5-10 years after heart transplantation. Therefore, the purposes of this study were to describe physical functional disability over time and identify predictors of physical functional disability from 5 to 10 years after heart transplantation.
Methods
Five hundred fifty-five patients who were between 5-10 years post heart transplant enrolled in our study (age = 54 ± 9 years, 78% male, 88% white, 79% married). Patients completed six instruments that measure physical functional disability and factors that may impact physical functional disability. Statistical analyses included calculation of frequencies, means ± standard deviation (plotted over time), Pearson correlation coefficients, and multiple regression coupled with repeated measures.
Results
Between 5-10 years after heart transplantation, physical functional disability was low, and 34-45% of patients reported having no functional disability. More physical functional disability was associated with having more symptoms; having depression / mood / negative affect / and lower use of negative coping strategies; having more co-morbidities and more specific co-morbidities (ex., more orthopedic problems and diabetes); higher NYHA class; having more acute rejection, infection, or cardiac allograft vasculopathy; being female, older, less educated, and unemployed; higher BMI; and more hospital readmissions (explaining 46% of variance [F=84.75, p<0.0001]).
Conclusions
Demographic, clinical, and psychological factors were significantly related to physical functional disability. Knowledge of these factors provides the basis for development of therapeutic plans of care.
Perception of improvement in physical function from before to after heart transplantation has been reported through 5 years after transplant1-5. Researchers have also determined that perception of improvement in physical function has been greater than perception of improvement in either psychological status or social functioning after heart transplantation6, 7. However, there is also evidence of reduced physical activity8, functional limitations9, and physical functional disability2, 5, 10 at 1-2 years after heart transplantation.
A few cross-sectional studies have examined perception of physical function ≥ 5 years after heart transplant. These studies revealed no more than mild limitations in activities of daily living11, reduced physical activity12, and conflicting data regarding perceived physical function as compared to a general population13, 14, 15.
Multivariate analyses have also been conducted to examine physical function long-term after heart transplantation. Demographic, clinical, and psychosocial factors have been found to be predictors of physical function at 5-6 years after heart transplantation16, 17 as well as at ≥ 10 years after transplant13, 14. Researchers have not examined predictors of physical functional disability at 5-10 years post transplant.
Therefore, the purposes of this study were to describe physical functional disability over time and identify predictors of physical functional disability from 5 to 10 years after heart transplantation. We defined physical functional disability as a heart transplant recipient's perception of his/her inability to perform activities (as related to health status) in three areas of function: mobility, ambulation, and body care/movement.
Methods
Sample
Patients were from a large, prospective, longitudinal, multi-site study of quality of life, long-term after heart transplantation who were transplanted between July 1, 1990 and June 30, 1999 at four medical centers in the United States. Eight hundred eighty-four patients were potentially eligible to participate in our study. Patients were included in the study if they were ≥ 4.5 years post orthotopic heart transplantation, ≥ 21 years, fluent and literate in English, and physically able to participate. Five hundred ninety-seven patients who met inclusion criteria volunteered to participate in our study, and 555/597 patients completed one or more booklets of quality of life instruments. Thus, our final sample size was 555 patients who were between 5-10 years post transplant. Reasons for patient non-enrollment have been discussed previously18.
Instruments
Patients completed six instruments that measure physical functional disability and factors that may impact physical functional disability in < 1 hour. These self-report instruments were selected for this study based on their relevance to long-term heart transplant recipients and the purpose of our study. Instruments included the Sickness Impact Profile19, Heart Transplant Symptom Checklist20, Jalowiec Coping Scale21, Assessment of Problems with the Heart Transplant Regimen22, Positive and Negative Affect Schedule – Expanded version23-25, and Cardiac Depression Scale26. Table 1 provides additional information about each instrument; only those instrument subscales used for these analyses were included. Instruments were combined into a booklet of questionnaires, and the order of instruments was varied for each time period in order to control for response bias, fatigue, and sensitization.
Table 1.
Self-report Instruments Used to Measure Physical Functional Disability and to Measure Factors Impacting on Physical Functional Disability
| Instruments/authors | Number of items used | Sub-scales used | Scoring |
|---|---|---|---|
| Sickness Impact Profile (Bergner et al, 1981)18 | 45 | Body care/movement | Yes/No |
| Mobility | Yes responses are weighted by amount of disability indicated | ||
| Ambulation | |||
| Heart Transplant Symptom Checklist (Grady, Jalowiec, & Grusk, 1988)19 [modified, 1999] | 75 | Cardiopulmonary | Yes/No |
| Gastrointestinal | Presence of symptoms | ||
| Genitourinary | |||
| Neurological/muscular | |||
| Dermatological/soft tissue | |||
| Jalowiec Coping Scale (Jalowiec, 1987)20 | 25 | Evasive | Use of coping strategy: |
| Fatalistic | 0-3 | ||
| Emotive | 0 = never used | ||
| Palliative | 3 = often used | ||
| Assessment of Compliance with Transplant Regimen (Grady, Grusk, & Jalowiec, 1988)21 [modified, 1999] | 2 | Difficulty with compliance (exercise) | Difficulty: 1-4 |
| Actual compliance (exercise) | 1 = no difficulty | ||
| 4 = a lot of difficulty | |||
| Compliance 1-4 | |||
| 1 = all of the time | |||
| 4 = hardly ever | |||
| Positive and Negative Affect Schedule (Watson & Clark, 1991)22 | 10 | Negative affect | 1-5 |
| 1 = very slightly or not at all | |||
| 5 = extremely | |||
| Cardiac Depression Scale (Hare, 1993)25 | 16 | Sleep | 1-7 |
| Uncertainty | Agreement or disagreement with individual anchors for each question | ||
| Mood | |||
| Hopelessness |
Physical functional disability was a composite score (composed of 45 items from three subscales) of the Sickness Impact Profile19. The subscales are ambulation (12 questions, ie., I walk more slowly and I do not use stairs at all); mobility (10 questions, ie., I stay away from home only for short periods of time and I stay home most of the time); and body care and movement (23 questions, ie., I have trouble getting shoes or stockings on and I make difficult moves with help such as getting into or out of cars).
Reliability and validity have previously been demonstrated to be adequate for the instruments (Sickness Impact Profile19, 27, 28, Heart Transplant Symptom Checklist20, 29, Jalowiec Coping Scale21, Assessment of Problems with the Heart Transplant Regimen22, Positive and Negative Affect Schedule23, and Cardiac Depression Scale26). The adequacy of psychometric support has been demonstrated in patients with chronic illnesses and associated therapies, including heart failure and heart transplantation.
Chart review data (including demographic data and clinical data) were collected from patient medical records (including both inpatient and outpatient records) and a large heart transplant registry (the Cardiac Transplant Research Database [CTRD]).
Procedures
Institutional Review Board approval was received by all 4 institutions for conduct of this study and the CTRD. Patients who were ≥ 4.5 years post heart transplantation were informed about the study, and patients who volunteered to enroll in the study signed a written informed consent form. Enrollees were subsequently given a booklet of questionnaires to complete every 6 months (based on the date of their heart transplant) from 5 to 10 years post transplantation. All booklets and chart reviews were screened and cleaned at Rush University and sent to the University of Alabama at Birmingham for data entry.
Statistics
Data were analyzed using SAS version 8.2 (Cary, NC). Data were converted to standardized scores (range=0.00 – 1.00) for items, subscales, and total scale scores by dividing the items, subscales, and total scale scores by the maximum possible score for most questionnaires. Statistical analyses included calculation of frequencies, means ± standard deviation (plotted over time), Pearson correlation coefficients, and multiple regression coupled with repeated measures.
Four separate regression analyses were run with the following four dependent variables: physical functional disability (the composite score for the subscales of ambulation, mobility, and body care / movement), and each of the three subscales of ambulation, mobility, and body care / movement. Correlations with the dependent variable were examined and correlations were generally ≤ .50. Inter-item correlations among the independent variables were also examined, and multicollinearity was identified among < 0.001% of variables and therefore was not a problem. Thirty-four independent variables were entered into each of the regression analyses in groups in the following order: seven demographic variables, eighteen clinical variables, and nine psychological / behavioral variables. While the ratio of cases to independent variables (16:1) was generally acceptable for multiple regression30, we also conducted a post-hoc power analysis. A sample size of 555 would achieve 99% power to detect an R-Squared of 0.3 (the R2 ranged from 0.31 to 0.45 in our regression models) attributed to 34 independent variables using an F-Test with a significance level (alpha) of 0.05. Thus, our sample should provide adequate statistical power. All subjects were retained in the analyses as no influential outliers were identified. The model fit was tested and acceptable. The level of significance was set at p=0.05 for all analyses.
Results
Descriptive analyses
Demographic and clinical characteristics
At time of transplant, patients (n=555) were primarily middle aged, white, married males who were fairly well educated (59% > high school education and mean = 14 ± 3 years). See table 2. The etiology of heart failure was primarily ischemic and dilated cardiomyopathy. At time of transplant, 61% of patients were United Network for Organ Sharing (UNOS) status 1 (ie., 1A or 1B). Patients had 5 ± 3 co-morbidities as listed in Table 2. Between 5 and 10 years after transplant, 14% of patients experienced ≥ 1 episode of hospitalization. Cumulative rates of acute rejection were 2.2 ± 2.0 episodes, and rates of infection were 0.8 ± 1.3 episodes. During this time period, 42% of patients showed evidence (via coronary angiography) of cardiac allograft vasculopathy.
Table 2.
Characteristics of enrolled patients
| Characteristics | Enrolled in Study (n=555) |
|---|---|
| Demographic Characteristics | |
| Age at transplant (years) (mean ± SD) | 53.8 ± 9.9 |
| Gender (%) | |
| male | 78% |
| female | 22% |
| Race/ethnicity (%) | |
| White | 88% |
| Black | 9% |
| Hispanic | 1% |
| Other | 2% |
| Marital Status (%) | |
| Married | 79% |
| Divorced/separated | 11% |
| Single | 6% |
| Widowed | 4% |
| Current Employment (%) | |
| Working | 32% |
| Not Working | 68% |
| BMI (kg/m2) (mean ± SD) | 29 ± 5.3 |
| Clinical Characteristics | |
| Co-morbidities (%) | |
| Hypertension | 87% |
| Hyperlipidimia | 78% |
| Renal dysfunction | 37% |
| Cancer (including skin cancer) | 27% |
| Diabetes | 27% |
| Orthopedic problems | 26% |
| Gastrointestinal problems | 22% |
| Gout | 18% |
| Genitourinary problems | 12% |
Patterns of physical functional disability at 5-10 years after transplant
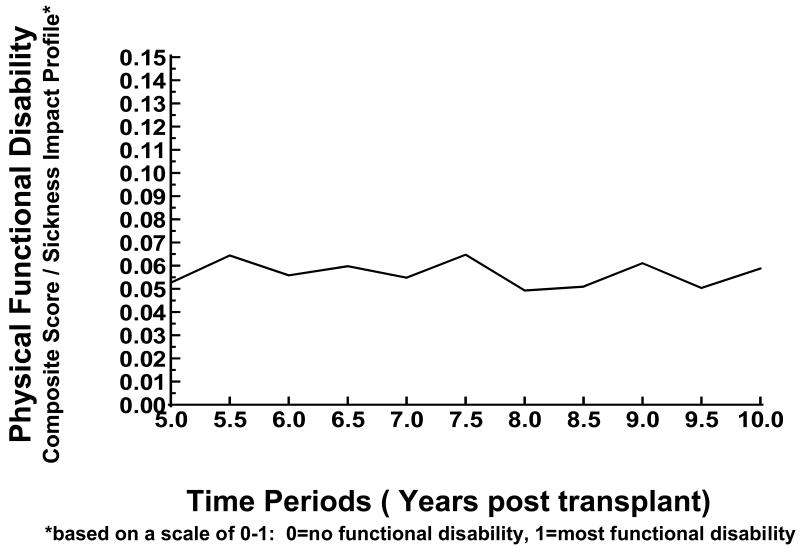
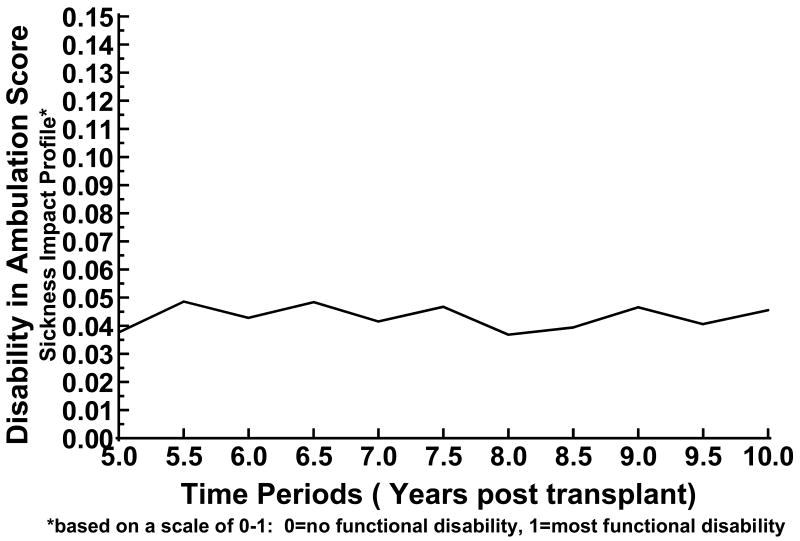
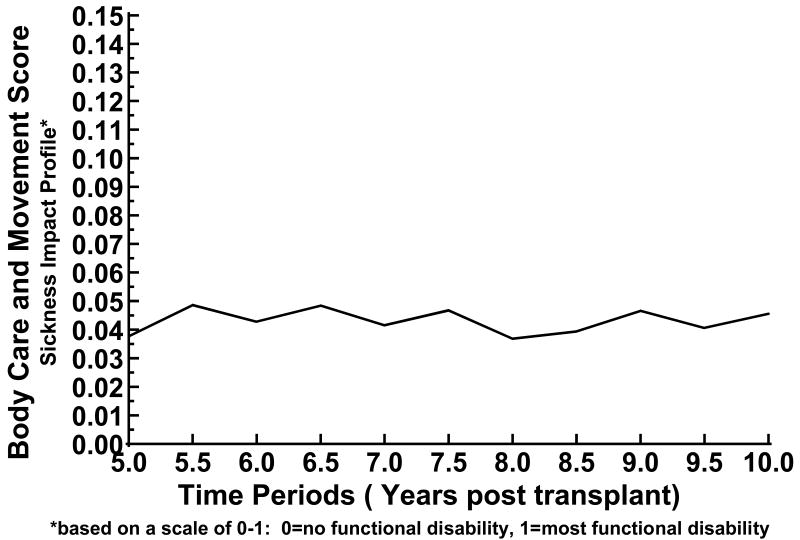
Between 5-10 years after heart transplantation, physical functional disability was low (mean=0.06 ± 0.09, 0 = no functional disability and 1 = most functional disability), and 34-45% of patients reported having no functional disability. See table 3 and figure 1. Similarly, from 5 to 10 years after heart transplantation, functional disability was low related to the subscales of ambulation, mobility, and body care / movement. Patients reported no disability as follows: ambulation, 50-59% (mean= 0.09 ± 0.14); mobility, 62-79% (mean=0.05 ± 0.11); and body care / movement, 49-59% (mean=0.04 ± 0.08), (0 = no functional disability to 1 = most functional disability for all subscales). When these patterns of disability were examined over time, there were no significant changes, except for mobility, for which there was a trend that suggested that patient mobility decreased further from the date of transplant. See table 3 and figures 2-4.
Table 3.
Percent of Patients with no Physical Functional Disability from 5-10 years after Heart Transplantation
| Target Time (years) | Physical Function Composite Score (%) | Ambulation Score (%) | Mobility Score (%) | Body Care and Movement Score (%) |
|---|---|---|---|---|
| 5.0 | 45 | 59 | 69 | 59 |
| 5.5 | 34 | 54 | 62 | 49 |
| 6.0 | 39 | 59 | 68 | 50 |
| 6.5 | 36 | 53 | 67 | 49 |
| 7.0 | 45 | 57 | 68 | 55 |
| 7.5 | 40 | 50 | 70 | 56 |
| 8.0 | 44 | 57 | 79 | 56 |
| 8.5 | 40 | 51 | 68 | 54 |
| 9.0 | 38 | 50 | 65 | 54 |
| 9.5 | 39 | 55 | 71 | 55 |
| 10.0 | 37 | 52 | 70 | 51 |
from the Sickness Impact Profile
Figure 1.
Physical Functional Disability at 5-10 years after Heart Transplantation
Figure 2.
Disability in Ambulation at 5-10 years after Heart Transplantation
Figure 4.
Disability in Body Care and Movement at 5-10 years after Heart Transplantation
Multivariate analyses
Four separate multivariate analyses, adjusted for time, were conducted with physical functional disability, ambulation, mobility, and body care / movement as dependent variables. Thirty-four independent variables were entered into each regression analysis in the following order: demographic variables, clinical variables, and psychological / behavioral variables. For physical functional disability, 20 candidate variables were significant and explained 46% of variance (F=84.75, p<0.0001). Thus, more physical functional disability was associated with having more symptoms (neurological / muscular, genito-urinary, and cardiopulmonary); depression / mood / negative affect / and lower use of negative coping strategies; having more co-morbidities and more specific co-morbidities (more orthopedic problems and diabetes, and fewer genitourinary problems and malignancies); higher NYHA class; having more acute rejection, infection, or cardiac allograft vasculopathy; being female, older, less educated, and unemployed; higher BMI; and more hospital readmissions. See table 4.
Table 4.
Predictors of Physical Functional Disability
| Variable | Beta
Weights |
Partial
R-Square |
Model
R-Square |
F Value | P Value |
|---|---|---|---|---|---|
| Neuro-muscular symptoms | 0.12 | 0.317 | 0.317 | 932.74 | < .0001 |
| Depression | 0.001 | 0.032 | 0.350 | 99.32 | < .0001 |
| Number of co-existing illnesses | 0.003 | 0.020 | 0.370 | 64.75 | < .0001 |
| NYHA class | 0.02 | 0.016 | 0.390 | 53.26 | < .0001 |
| Transplant event | 0.003 | 0.012 | 0.400 | 39.93 | < .0001 |
| Male | -0.02 | 0.008 | 0.407 | 28.33 | < .0001 |
| Employment | -0.01 | 0.006 | 0.413 | 20.61 | < .0001 |
| Body mass index | 0.002 | 0.006 | 0.418 | 19.60 | < .0001 |
| Orthopedic problems | 0.02 | 0.006 | 0.424 | 20.81 | < .0001 |
| Mood | -0.06 | 0.005 | 0.429 | 16.60 | < .0001 |
| Negative affect | 0.07 | 0.006 | 0.435 | 19.25 | < .0001 |
| Genitourinary symptoms | 0.04 | 0.005 | 0.439 | 16.23 | < .0001 |
| Number of readmissions | 0.01 | 0.004 | 0.443 | 12.97 | 0.0003 |
| Cardiopulmonary symptoms | 0.04 | 0.003 | 0.446 | 10.60 | 0.001 |
| Age at transplant | 0.001 | 0.003 | 0.449 | 12.32 | 0.0005 |
| Cumulative malignancies | -0.005 | 0.003 | 0.452 | 11.75 | 0.0006 |
| Education | -0.002 | 0.003 | 0.455 | 10.90 | 0.001 |
| Diabetes mellitus | 0.009 | 0.002 | 0.458 | 7.93 | 0.005 |
| Genitourinary/urological problems | -0.01 | 0.001 | 0.459 | 5.17 | 0.02 |
| Use of negative coping | -0.02 | 0.001 | 0.460 | 5.13 | 0.02 |
NYHA= New York Heart Association
Transplant Event = composite score of acute rejection, infection and cardiac allograft vasculopathy
Similar candidate variables that were related to physical functional disability were also related to disability regarding ambulation, mobility, and body care / movement. Twenty-two variables explained 40% of variance in disability related to ambulation (F=60.03, p<0.0001). These variables were identical to variables associated with physical functional disability, except that two additional variables were associated with disability related to ambulation: less compliance with an exercise regimen and renal dysfunction.
For mobility and body care / movement, candidate variables that were similar to those that predicted physical functional disability were noted, but there were more differences. Sixteen candidate variables were related to mobility (F=56.18, p<0.0001), explaining 31% of variance. See table 5. Lastly, 16 candidate variables explained 38% of variance in body care / movement (F=76.45, p<0.0001). See table 6.
Table 5.
Predictors of Disability in Ambulation
| Variable | Beta
Weights |
Partial
R-Square |
Model
R-Square |
F Value | P Value |
|---|---|---|---|---|---|
| Neuro-muscular symptoms | 0.16 | 0.245 | 0.245 | 652.26 | < .0001 |
| Number of co-existing illnesses | 0.004 | 0.029 | 0.274 | 80.05 | < .0001 |
| NYHA class | 0.04 | 0.022 | 0.296 | 62.85 | < .0001 |
| Depression | 0.001 | 0.017 | 0.313 | 49.32 | < .0001 |
| Transplant event | 0.006 | 0.120 | 0.325 | 35.41 | < .0001 |
| Body mass index | 0.004 | 0.010 | 0.335 | 29.53 | < .0001 |
| Orthopedic problems | 0.03 | 0.009 | 0.345 | 28.75 | < .0001 |
| Employment | -0.02 | 0.008 | 0.352 | 23.08 | < .0001 |
| Cardiopulmonary symptoms | 0.08 | 0.009 | 0.361 | 27.66 | < .0001 |
| Following a schuled exercise program | 0.01 | 0.006 | 0.367 | 18.55 | < .0001 |
| Diabetes mellitus | 0.02 | 0.004 | 0.371 | 13.56 | 0.0002 |
| Male | -0.03 | 0.005 | 0.376 | 15.07 | 0.0001 |
| Age at transplant | 0.001 | 0.004 | 0.380 | 13.52 | 0.0002 |
| Genitourinary symptoms | 0.07 | 0.003 | 0.383 | 10.77 | 0.001 |
| Mood | -0.07 | 0.004 | 0.387 | 12.75 | 0.0004 |
| Cumulative malignancies | -0.006 | 0.003 | 0.390 | 8.08 | 0.005 |
| Negative affect | 0.07 | 0.002 | 0.392 | 7.42 | 0.007 |
| Genitourinary/urological problems | -0.02 | 0.002 | 0.394 | 6.06 | 0.01 |
| Number of readmission | 0.01 | 0.002 | 0.396 | 5.65 | 0.02 |
| Use of negative coping | -0.03 | 0.001 | 0.397 | 4.77 | 0.03 |
| Renal problems | 0.01 | 0.001 | 0.398 | 4.56 | 0.03 |
| Education | -0.002 | 0.001 | 0.400 | 4.07 | 0.04 |
NYHA= New York Heart Association
Transplant Event = composite score of acute rejection, infection and cardiac allograft vasculopathy
Table 6.
Predictors of Disability in Mobility
| Variable | Beta
Weights |
Partial
R-Square |
Model
R-Square |
F Value | P Value |
|---|---|---|---|---|---|
| Depression | 0.001 | 0.186 | 0.186 | 458.33 | <.0001 |
| Neuromuscular symptoms | 0.08 | 0.042 | 0.228 | 109.93 | <.0001 |
| Male | -0.02 | 0.018 | 0.246 | 47.39 | <.0001 |
| Number of readmissions | 0.01 | 0.012 | 0.258 | 32.24 | <.0001 |
| NYHA class | 0.03 | 0.010 | 0.268 | 26.67 | <.0001 |
| Caucasian | -0.03 | 0.008 | 0.276 | 21.87 | <.0001 |
| Education | -0.003 | 0.006 | 0.282 | 17.15 | <.0001 |
| Negative affect | 0.09 | 0.005 | 0.287 | 15.14 | 0.0001 |
| Mood | -0.08 | 0.006 | 0.293 | 15.62 | <.0001 |
| Transplant event | 0.003 | 0.004 | 0.297 | 11.51 | 0.0007 |
| Genitourinary symptoms | 0.04 | 0.004 | 0.301 | 10.94 | 0.001 |
| Employment | -0.01 | 0.002 | 0.306 | 5.40 | 0.02 |
| Diabetes mellitus | 0.01 | 0.002 | 0.308 | 4.84 | 0.03 |
| Cumulative malignancies | -0.004 | 0.002 | 0.308 | 4.53 | 0.03 |
| Following a scheduled exercise program | -0.006 | 0.002 | 0.310 | 4.97 | 0.03 |
| Number of co-existing illnesses | 0.002 | 0.001 | 0.311 | 4.16 | 0.04 |
NYHA= New York Heart Association
Transplant Event = composite score of acute rejection, infection and cardiac allograft vasculopathy
Post-hoc correlational analyses
Post-hoc correlational analyses were run between each of the 29 items of the neuromuscular subscale (regarding presence or absence of the symptom) in the Heart Transplant Symptom Checklist and three of the four dependent variables (physical functional disability, ambulation, and body care / movement) since the neuromuscular subscale accounted for the most variance in these outcomes. The symptoms that were significantly correlated at r ≥ 0.30 for all three outcomes were weakness in the whole body, arms, and legs. In addition, problems with taste, fatigue, blurred or unclear eyesight, trouble speaking, and confusion or disorientation were correlated at r ≥ 0.30 for physical functional disability, and blurred or unclear eyesight and confusion or disorientation were correlated at r ≥ 0.30 for body care / movement.
Discussion
Demographic, clinical, and psychological / behavioral factors were significantly related to all four dependent variables in our regression equations: physical functional disability, ambulation, mobility, and body care / movement. Three factors (neuromuscular symptoms, higher NYHA class, and depression) explained more than 1% of variance in the four dependent variables; four factors (having more co-morbidities, orthopedic problems, negative affect, and increased BMI) explained more than 1% variance in three of the four dependent variables, and four factors (having acute rejection, infection, or cardiac allograft vasculopathy; mood, female, and lack of employment) explained 1% variance in two of the four dependent variables. Despite low levels of functional disability, (also reported by other researchers2, 5, 17, 31 ≤ 5 year post heart transplant) these findings have important therapeutic implications.
Neuromuscular symptoms were highly related to physical functional disability, ambulation, mobility, and body care / movement. Symptom frequency and distress have been described after heart transplantation5, 15, 20, 31-35. Specifically, neuromuscular symptoms have been previously described within 2 years after heart transplant (ie., fatigue5, 20, 31, 32, weakness20, 32, restlessness20, insomnia20, 31, concentration and memory disorders31, 32, and tremors31) and similarly at more than 2 years after transplant (fatigue33-35, weakness15, 35, insomnia15, 33, 35, concentration and memory disorders33, and tremors33). These symptoms, as a unique subset, have not previously explained variance in physical disability. Thus, our findings strengthen support for persistence of these symptoms and their strong association with physical dysfunction long-term after heart transplantation. It is incumbent upon clinicians to serially assess these symptoms, and depending upon etiology, develop a plan of care.
Higher NYHA class has not been previously reported as significantly related to physical functional disability, ambulation, mobility, and body care / movement in patients after heart transplantation; although increased NYHA class has previously been correlated with reduced exercise capacity36. This relationship may suggest possible cardiac pathology, given that higher NYHA class reflects the impact of worsening symptoms of heart failure on activities of daily living. This relationship has been demonstrated in the findings of Butler et al.16 regarding the relationship of acute rejection and / or allograft vasculopathy with physical functional disability, as well as the findings of Schwaiblmair et al.37 demonstrating the influence of vasculopathy on exercise capacity.
Psychological status was also strongly related to limitations in physical function. Psychological symptoms, depression, and anxiety disorders have been well documented during the first few years after heart transplantation, with evidence of improvement over time20, 31, 33, 38-40. Findings of long-term psychological dysfunction have also been reported4, 14, 41, 42. Only a few researches have reported a relationship between psychological dysfunction and physical disability5, 14, 17, 43, 44. More recently, Type D personality has been reported to be related to impaired physical functioning45. This “mind-body” connection demonstrates the need for expanded assessment when considering therapeutic approaches. Patients with serious physical limitations may well have concurrent psychological problems, and both areas of dysfunction may need to be addressed.
The relationship between physical functional disability, ambulation, and body care / movement with increased number of co-morbidities (specifically orthopedic problems and increased BMI) provides a focus for treatment as well. We have previously reported that orthopedic problems were related to limitations in ambulation at 5 years post heart transplant17 and Rosenblum et al.35 have reported a relationship between musculoskeletal-neurological impairment and worse physical function up to 10 years post heart transplantation. This small, but compelling body of evidence suggests the need for evaluation of orthopedic problems and tailoring of treatment plans including surgical intervention, physical therapy, and occupational therapy.
Obesity is a common problem after heart transplantation. Pre-operative obesity has been found to be a risk factor for morbidity and mortality after heart transplantation46, while postoperative obesity has been associated with poor clinical outcomes47 and poor functional outcomes16. Obesity was noted by Butler et al.16 to directly impact functional performance, while increased BMI was reported by Leung et al.48 to be correlated with reduced exercise capacity. Thus, considering our current findings and those of other researchers, post transplant obesity confers significant physical risk. If any modicum of success in weight reduction and maintenance of weight loss is to be gained, behavioral therapies, dietary programs, and exercise must be individualized and incorporated into a patient's lifestyle.
Lastly, being female and unemployed explained a significant amount of variance in overall physical functional disability, ambulation, and / or mobility. These findings have been supported in reports of perception of physical functional disability earlier after heart transplantation5, 17. In addition, Evangelista et al.8 have previously reported that 85% of female heart transplant recipients engage in low or minimal levels of physical activity, and Renlund et al.49, and Leung et al.48 have reported that female gender is related to worse exercise capacity after heart transplantation. The evidence suggests that female transplant recipients have limitations in physical function. Therefore, careful screening for disability and appropriate treatment and referral (perhaps for occupational therapy and / or physical therapy) may be indicated.
The relationship between unemployment and physical disability has been reported by other researchers after heart transplantation12, 13, 50. Rates of unemployment have varied from 22% to 86% over time after transplant9, 35, 51-54. Given the extent and yet variability of post transplant unemployment, it is incumbent upon clinicians to determine reasons for not working and provide assistance to patients who desire to return to work. Clearly, this area requires further research given its significant impact on patients, families, and society.
Our study has limitations. While our sample size was large and geographically diverse, we none-the-less studied patients who survived long enough to consider enrollment in our study, met study criteria, enrolled in our study, and were willing to complete booklets of questionnaires. This limitation may result in underestimation of physical functional disability (ie., not including patients who were too sick to enroll) or overestimation of physical functional disability (ie., not including patients who met criteria and did not enroll in our study because they were active and too busy). Also, our study sample was composed of primarily older, white, married men. We attempted to enroll all eligible patients, but were constrained by the imposed limits of patients who were transplanted 5 – 10 years earlier at the four institutions. Lastly, while our intention was to study long-term post-transplant physical functional disability, we did not have baseline pre transplant data.
Conclusion
We have demonstrated a low rate of perceived physical functional disability in patients from 5 – 10 years after heart transplantation. We have further identified strong relationships between physical functional disability and demographic, clinical, and psychological factors. Knowledge of these factors provides the basis for development of therapeutic plans of care that uses a holistic approach to heart transplant patient management.
Figure 3.
Disability in Mobility at 5-10 years after Heart Transplantation
Table 7.
Predictors of Disability in Body Care/Movement
| Variable | Beta
Weights |
Partial
R-Square |
Model
R-Square |
F Value | P Value |
|---|---|---|---|---|---|
| Neuromuscular symptoms | 0.12 | 0.283 | 0.283 | 792.92 | <.0001 |
| Depression | 0.0006 | 0.021 | 0.304 | 59.67 | <.0001 |
| Number of co-existing illness | 0.003 | 0.018 | 0.322 | 52.90 | <.0001 |
| NYHA class | 0.01 | 0.007 | 0.329 | 20.75 | <.0001 |
| Cumulative rejections | 0.004 | 0.008 | 0.337 | 24.99 | <.0001 |
| Orthopedic problems | 0.12 | 0.008 | 0.345 | 24.09 | <.0001 |
| Negative affect | 0.06 | 0.005 | 0.350 | 15.75 | <.0001 |
| Mood | -0.05 | 0.005 | 0.356 | 16.49 | <.0001 |
| Body mass index | 0.002 | 0.006 | 0.361 | 17.31 | <.0001 |
| Age at transplant | 0.0008 | 0.004 | 0.365 | 12.77 | 0.0004 |
| Cardiopulmonary symptoms | 0.03 | 0.004 | 0.369 | 13.30 | 0.0003 |
| Education | -0.002 | 0.004 | 0.373 | 11.87 | 0.0006 |
| Number of readmissions | 0.009 | 0.003 | 0.376 | 9.52 | 0.002 |
| Caucasian | -0.01 | 0.002 | 0.378 | 6.04 | 0.01 |
| Male | -0.008 | 0.001 | 0.379 | 4.58 | 0.03 |
| Dermatologic symptoms | 0.02 | 0.001 | 0.381 | 4.12 | 0.04 |
NYHA= New York Heart Association
Acknowledgments
This research was funded by the NIH (National Institute of Nursing Research, R01 #NR005200); a grant-in-aid from the College of Nursing, Rush University; and intramural funding from the Rush Heart Institute, Rush University Medical Center.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kathleen L. Grady, Northwestern Memorial Hospital, Chicago, IL.
David C. Naftel, University of Alabama Medical Center, Birmingham, AL.
James B. Young, The Cleveland Clinic Foundation, Cleveland, OH.
Dave Pelegrin, The Cleveland Clinic Foundation, Cleveland, OH.
Jennifer Czerr, The Cleveland Clinic Foundation, Cleveland, OH.
Robert Higgins, Rush University Medical Center, Chicago, IL.
Alain Heroux, Loyola University Medical Center, Maywood, IL.
Bruce Rybarczyk, Virginia Commonwealth University, Richmond, VA.
Mary McLeod, Rush University Medical Center, Chicago, IL.
Jon Kobashigawa, UCLA Medical Center, Los Angeles, CA.
Julie Chait, UCLA Medical Center, Los Angeles, CA.
Connie White-Williams, University of Alabama Medical Center, Birmingham, AL.
Susan Myers, University of Alabama Medical Center, Birmingham, AL.
James K. Kirklin, University of Alabama Medical Center, Birmingham, AL.
References
- 1.Caine N, Sharples L, English T, et al. Prospective study comparing quality of life before and after heart transplantation. Transplant Proc. 1990;22:1437–9. [PubMed] [Google Scholar]
- 2.Fisher DC, Lake KD, Reutzel TJ, et al. Changes in health-related quality of life and depression in heart transplant recipients. J Heart Lung Transplant. 1995;14(2):373–81. [PubMed] [Google Scholar]
- 3.Streiff N, Feurer I, Speroff T, et al. The effects of rejection episodes, obesity, and osteopenia on functional performance and health-related quality of life after heart transplantation. Transplant Proc. 2001;33:3533–5. doi: 10.1016/s0041-1345(01)02424-1. [DOI] [PubMed] [Google Scholar]
- 4.Bunzel B, Laederach-Hofmann K. Long-term effects of heart transplantation: The gap between physical performance and emotional well-being. Scand J Rehab Med. 1999;31:214–222. doi: 10.1080/003655099444380. [DOI] [PubMed] [Google Scholar]
- 5.Jalowiec A, Grady K, White-Williams C. Functional status one year after heart transplant. J Cardiopulm Rehab. doi: 10.1097/01.hcr.0000265029.25392.6e. in press. [DOI] [PubMed] [Google Scholar]
- 6.Bunzel B, Grundbock A, Laczkovics A, et al. Quality of life after orthotopic heart transplantation. J Heart Lung Transplant. 1991;10:455–9. [PubMed] [Google Scholar]
- 7.Packa D. Quality of life of adults after a heart transplant. J Cardiovasc Nurs. 1989;3:12–22. doi: 10.1097/00005082-198902000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Evangelista L, Dracup K, Doering L, Moser D, Kobashigawa J. Physical activity patterns in heart transplant women. J Cardiovasc Nurs. 2005;20(5):334–9. doi: 10.1097/00005082-200509000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Brann WM, Bennett LE, Keck BM, Hosenpud JD. Morbidity, functional status, and immunosuppressive therapy after heart transplantation: An analysis of the joint International Society for Heart and Lung Transplantation/ United Network for Organ Sharing Thoracic Registry. J Heart Lung Transplant. 1998;17:374–82. [PubMed] [Google Scholar]
- 10.White-Williams C, Jalowiec A, Grady K. Who returns to work after heart transplantation? J Heart Lung Transplant. 2005;24:2251–61. doi: 10.1016/j.healun.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Mulcahy D, Fitzgerald M, Wright C, et al. Long term follow-up of severely ill patients who underwent urgent cardiac transplantation. British Med J. 1993;306:98–101. doi: 10.1136/bmj.306.6870.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salyer J, Flattery M, Joyner P, et al. Lifestyle and quality of life in long-term cardiac transplant recipients. J Heart Lung Transplant. 2003;22:309–21. doi: 10.1016/s1053-2498(02)00552-1. [DOI] [PubMed] [Google Scholar]
- 13.Politi P, Piccinelli M, Poli FP. Ten years of extended life: Quality of life among heart transplant survivors. Transplantation. 2004;78:257–63. doi: 10.1097/01.tp.0000133537.87951.f2. [DOI] [PubMed] [Google Scholar]
- 14.Fusar-Poli P, Martinelli V, Klersy C, et al. Depression and quality of life in patients living 10-18 years beyond heart transplantation. J Heart Lung Transplant. 2005;24:2269–78. doi: 10.1016/j.healun.2005.06.022. [DOI] [PubMed] [Google Scholar]
- 15.DeCampli WM, Luikart H, Hunt S, et al. Characteristics of patients surviving more than ten years after cardiac transplantation. J Thorac Cardiovasc Surg. 1995;109:1103–15. doi: 10.1016/S0022-5223(95)70194-X. [DOI] [PubMed] [Google Scholar]
- 16.Butler J, McCoin N, Feurer ID, et al. Modeling the effects of functional performance and post-transplant comorbidities on health-related quality of life after heart transplantation. J Heart Lung Transplant. 2003;22:1149–56. doi: 10.1016/s1053-2498(02)01188-9. [DOI] [PubMed] [Google Scholar]
- 17.Grady KL, Naftel DC, Kirklin JK, et al. Predictors of physical functional disability at 5 to 6 years after heart transplantation. J Heart Lung Transplant. 2005;24:2279–85. doi: 10.1016/j.healun.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 18.Grady KL, Naftel DC, Kobashigawa J, et al. Patterns and predictors of quality of life at 5-10 years after heart transplantation. J Heart Lung Transplant. 2007;26:535–43. doi: 10.1016/j.healun.2007.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bergner M, Bobbitt RA, Carter WB, et al. The Sickness Impact Profile: Development and final revision of a health status measure. Med Care. 1981;19:787–806. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Jalowiec A, Grady KL, White-Williams C. Symptom distress three months after heart transplantation. J Heart Transplant. 1997;16:604–14. [PubMed] [Google Scholar]
- 21.Jalowiec A. The Jalowiec Coping Scale. In: Strickland OL, Dilorio C, editors. Measurement of nursing outcomes. 2nd. Vol. 3. New York: Springer; 2003. pp. 71–87. Self care and coping. [Google Scholar]
- 22.Grady KL, Jalowiec A, White-Williams C. Patient compliance at one year and two years after heart transplantation. J Heart Lung Transplant. 1998;17:383–94. [PubMed] [Google Scholar]
- 23.Watson D, Clark LA. The PANAS-X: Preliminary manual for the positive and negative affect schedule-expanded form. Southern Methodist University; Dallas, TX: 1991. pp. 2–35. [Google Scholar]
- 24.Watson D. Intraindividual and interindividual analyses of positive and negative affect: Their relation to health, compliance, perceived stress, and daily activities. J Pers Soc Psychol. 1988;54:1020–30. doi: 10.1037//0022-3514.54.6.1020. [DOI] [PubMed] [Google Scholar]
- 25.Watson D. The viscitudes of mood measurement: Effects of varying descriptors, time frames, and response formats on measures of positive and negative affect. J Pers Soc Psychol. 1988;55:128–41. doi: 10.1037//0022-3514.55.1.128. [DOI] [PubMed] [Google Scholar]
- 26.Hare DL, Davis CR. Cardiac Depression Scale: Validation of a new depression scale for cardiac patients. J Psychosom Res. 1996;40(4):379–86. doi: 10.1016/0022-3999(95)00612-5. [DOI] [PubMed] [Google Scholar]
- 27.Bergner M, Bobbitt RA, Pollard WE, Martin DP, Gilson BS. The Sickness Impact Profile: Validation of a health status measure. Med Care. 1976;14:57–67. doi: 10.1097/00005650-197601000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Pollard WE, Bobbitt RA, Bergner MB, Martin DP, Gilson GP. The Sickness Impact Profile: Reliability of a health status measure. Med Care. 1976;14:146–55. doi: 10.1097/00005650-197602000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Grady KL, Jalowiec A, Grusk BB, et al. Symptom distress in cardiac transplant candidates. Heart Lung. 1992;21(5):434–9. [PubMed] [Google Scholar]
- 30.Stevens J. Applied Multivariate Statistics for the Social Sciences. Lawrence Earlbaum Assoc; New Jersey: 1986. [Google Scholar]
- 31.Baumann L, Young C, Egan J. Living with a heart transplant: Long-term adjustment. Transplant Int. 1992;5:1–8. doi: 10.1007/BF00337181. [DOI] [PubMed] [Google Scholar]
- 32.Angermann C, Bullinger M, Spes C, Zellner M, Kemkes B, Theisen K. Quality of life in long-term survivors of orthotopic heart transplantation. Karldiologie. 1992;81:411–17. [PubMed] [Google Scholar]
- 33.Lough M, Lindsey A, Shinn J, Stotts N. Impact of symptom frequency and symptom distress on self-reported quality of life in heart transplant recipients. Heart Lung. 1987;16:193–200. [PubMed] [Google Scholar]
- 34.Reyes CJ, Evangelista LS, Doering L, Dracup K, Cesario DA, Kobashigawa J. Physical and psychological attributes of fatigue in female heart transplant recipients. J Heart Lung Transplant. 2004;23:614–9. doi: 10.1016/S1053-2498(03)00310-3. [DOI] [PubMed] [Google Scholar]
- 35.Rosenblum D, Rosen M, Pine Z, Rosen S, Borg-Stein J. Health status and quality of life following cardiac transplantation. Arch Phys Med Rehabil. 1993;74:490–3. doi: 10.1016/0003-9993(93)90111-m. [DOI] [PubMed] [Google Scholar]
- 36.Chang AC, Shyr Y, Groves J, et al. The utility of exercise testing after cardiac transplantation in older patients. J Surg Res. 1999;81(1):48–54. doi: 10.1006/jsre.1998.5484. [DOI] [PubMed] [Google Scholar]
- 37.Schwaiblmair M, von Scheidt W, Uberfuhr P, Reichart B, Vogelmeier C. Lung function and cardiopulmonary exercise performance after heart transplantation: Influence of cardiac allograft vasculopathy. Chest. 1999;116(2):332–9. doi: 10.1378/chest.116.2.332. [DOI] [PubMed] [Google Scholar]
- 38.Dew MA, Kormos RL, DiMartini AF, et al. Prevalence and risk of depression and anxiety-related disorders during the first three years after heart transplantation. Psychosomatics. 2001;42:300–13. doi: 10.1176/appi.psy.42.4.300. [DOI] [PubMed] [Google Scholar]
- 39.Shapiro PA, Kornfeld DS. Psychiatric outcomes of heart transplantation. Gen Hosp Psychiatry. 1989;11:352–7. doi: 10.1016/0163-8343(89)90123-0. [DOI] [PubMed] [Google Scholar]
- 40.Evangelista LS, Dracup K, Moser DK, Westlake C, Erickson V, Hamilton MA, Fonarow GC. Two-year follow-up of quality of life in patients referred for heart transplant. Heart Lung. 2005;34:187–93. doi: 10.1016/j.hrtlng.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 41.Bunzel B, Laederach-Hofman K, Grimm M. Survival, clinical data, and quality of life 10 years after heart transplantation: A prospective study. Zeitschrift Kardiol. 2002;91:319–27. doi: 10.1007/s003920200033. [DOI] [PubMed] [Google Scholar]
- 42.Dobbels F, De Geest S, Martin S, et al. Prevalence and correlates of depression symptoms at 10 years after heart transplantation: continuous attention required. Transplant Int. 2004;17:424–31. doi: 10.1007/s00147-004-0732-5. [DOI] [PubMed] [Google Scholar]
- 43.Dew MA, Kormos RL, Roth LH, Murali S, DiMartini A, Griffith BP. Early post-transplant medical compliance and mental health predict physical morbidity and mortality one to three years after heart transplantation. J Heart Lung Transplant. 1999;18:549–62. doi: 10.1016/s1053-2498(98)00044-8. [DOI] [PubMed] [Google Scholar]
- 44.Leedham B, Meyerowitz BE. Positive expectations predict health after heart transplantation. Health Psychol. 1995;14(1):74–9. doi: 10.1037//0278-6133.14.1.74. [DOI] [PubMed] [Google Scholar]
- 45.Pedersen SS, Holkamp PG, Caliskan K, van Domburg RT, Erdman R, Balk A. Type D personality is associated with impaired health-related quality of life 7 years following heart transplantation. J Psychosom Res. 2006;61:791–5. doi: 10.1016/j.jpsychores.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 46.Grady KL, White-Williams C, Naftel D, Costanzo MR, Pitts D, Rayburn B, VanBakel A, Jaski B, Bourge R, Kirklin J. Are preoperative obesity and cachexia risk factors for post heart transplant morbidity and mortality: A multi-institutional study of preoperative weight-height indices. J Heart Lung Transplant. 1999;18:750–63. doi: 10.1016/s1053-2498(99)00035-2. [DOI] [PubMed] [Google Scholar]
- 47.Grady KL, Naftel D, Pamboukian SV, Frazier OH, Hauptman P, Herre J, Eisen H, Smart F, Bourge R. Post-operative obesity and cachexia are risk factors for morbidity and mortality after heart transplant: Multi-institutional study of post-operative weight change. J Heart Lung Transplant. 2005;24:1424–30. doi: 10.1016/j.healun.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 48.Leung TC, Ballman KV, Allison TG, et al. Clinical predictors of exercise capacity 1 year after cardiac transplantation. J Heart Lung Transplant. 2003;22(1):16–27. doi: 10.1016/s1053-2498(02)00475-8. [DOI] [PubMed] [Google Scholar]
- 49.Renlund DG, Taylor DO, Ensley RD, et al. Exercise capacity after heart transplantation: Influence of donor and recipient characteristics. J Heart Lung Transplant. 1996;15(1 pt1):16–24. [PubMed] [Google Scholar]
- 50.White-Williams C, Jalowiec A, Grady KL. Who returns to work after heart transplantation? J Heart Lung Transplant. 2005;24:2255–61. doi: 10.1016/j.healun.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 51.Paris W, Woodbury A, Thompson S, et al. Return to work after heart transplantation. J Heart Lung Transplant. 1993;12:46–54. [PubMed] [Google Scholar]
- 52.Kavanaugh T, Yacoub MH, Kennedy J, Austin PC. Return to work after heart transplantation: 12 year follow-up. J Heart Lung Transplant. 1999;18:846–51. doi: 10.1016/s1053-2498(99)00049-2. [DOI] [PubMed] [Google Scholar]
- 53.Harvison A, Jones BM, McBride M, et al. Rehabilitation after heart transplantation: The Australian experience. J Heart Lung Transplant. 1988;7:337–41. [PubMed] [Google Scholar]
- 54.Meister ND, McAleer MJ, Meister JS, Riley JE, Copeland JG. Returning to work after heart transplantation. J Heart Lung Transplant. 1986;5:154–61. [PubMed] [Google Scholar]