Abstract
Lipopolysaccharide (LPS) is lethal to animals because it activates cytokine release, causing septic shock and tissue injury. Early proinflammatory cytokines (e.g., tumor necrosis factor [TNF] and interleukin [IL]-1) released within the first few hours of endotoxemia stimulate mediator cascades that persist for days and can lead to death. High mobility group 1 protein (HMG-1), a ubiquitous DNA-binding protein, was recently identified as a “late” mediator of endotoxin lethality. Anti–HMG-1 antibodies neutralized the delayed increase in serum HMG-1, and protected against endotoxin lethality, even when passive immunization was delayed until after the early cytokine response. Here we examined whether HMG-1 might stimulate cytokine synthesis in human peripheral blood mononuclear cell cultures. Addition of purified recombinant HMG-1 to human monocyte cultures significantly stimulated the release of TNF, IL-1α, IL-1β, IL-1RA, IL-6, IL-8, macrophage inflammatory protein (MIP)-1α, and MIP-1β; but not IL-10 or IL-12. HMG-1 concentrations that activated monocytes were within the pathological range previously observed in endotoxemic animals, and in serum obtained from septic patients. HMG-1 failed to stimulate cytokine release in lymphocytes, indicating that cellular stimulation was specific. Cytokine release after HMG-1 stimulation was delayed and biphasic compared with LPS stimulation. Computer-assisted image analysis demonstrated that peak intensity of HMG-1–induced cellular TNF staining was comparable to that observed after maximal stimulation with LPS. Administration of HMG-1 to Balb/c mice significantly increased serum TNF levels in vivo. Together, these results indicate that, like other cytokine mediators of endotoxin lethality (e.g., TNF and IL-1), extracellular HMG-1 is a regulator of monocyte proinflammatory cytokine synthesis.
Keywords: HMG-1, tumor necrosis factor, monocyte activation, septic shock, lipopolysaccharide
Introduction
High mobility group 1 protein (HMG-1), named for its rapid migration properties on electrophoretic gels, is a member of the nonhistone chromatin-associated proteins. HMG-1 is translated as a 214–amino acid protein, and extensively modified posttranslationally, by glycosylation, acylation, methylation, and phosphorylation 1 2. The primary structure is evolutionarily conserved, with 100% amino acid sequence homology between rat and mouse, and 99% homology between rodents and humans 3 4. HMG-1 is dipolar, bearing an acidic COOH terminus with a 30–amino acid stretch of glutamic and aspartic acid residues, and at least two basic structural units termed HMG domains 5. Intracellular HMG-1 has been studied previously for its roles in binding DNA; stabilizing nucleosome formation; as a general transcription factor for nucleolar and mitochondrial RNA polymerases; and as a gene- and tissue-specific transcriptional regulator that can enhance transcription and/or replication 5 6 7 8 9 10.
Extracellular HMG-1 was recently implicated as a “late” mediator of delayed endotoxin lethality, because murine and human macrophages/monocytes release large amounts of a 30-kD form of HMG-1 when stimulated by exposure to bacterial endotoxin 11. During lethal endotoxemia in mice, serum HMG-1 levels accumulated 16–36 h after LPS administration 11. Passive immunization of mice with anti–HMG-1 antibodies attenuated LPS-induced lethality, even when antibody administration was delayed until after the onset of the early proinflammatory cytokine response (2 h after endotoxin administration). Purified rHMG-1 was lethal to both LPS-responsive (C3H/HeN, Balb/c) and LPS-resistant (C3H/HeJ) mice, indicating that HMG-1 mediates lethal toxicity in the absence of LPS signal transduction 11. HMG-1 levels were increased significantly in critically ill patients with sepsis: the highest serum HMG-1 levels were observed in patients that succumbed 11. HMG-1 levels were also significantly increased in the serum of an uninfected patient with hemorrhagic shock, suggesting that extracellular HMG-1 might play a mediator role in the setting of inadequate tissue perfusion 12.
Recently, we observed that toxic doses of HMG-1 were associated with the development of fever, weight loss, piloerection, shivering, and microthrombi formation in the lungs and liver 11. Other proinflammatory mediators of endotoxemia that mediate similar pathological effects (e.g., TNF and IL-1) also function as potent stimulators of monocyte cytokine release in order to amplify and extend the “cytokine cascade” 13 14 15 16 17. Accordingly, we considered it plausible that HMG-1 might also function to stimulate monocytes to release TNF and other proinflammatory cytokines. We tested this hypothesis in cultured monocytes and macrophages.
Materials and Methods
Reagents.
Rat rHMG-1 was expressed in Escherichia coli and purified to homogeneity as described previously 11. rHMG-1 preparations were tested routinely for LPS content by the chromogenic Limulus amebocyte lysate assay (Endochrome; Charles River); preparations contained 600 pg or less of endotoxin per microgram of rHMG-1.
Blood Donors and Cell Cultures.
PBMCs were isolated by endotoxin-free Ficoll-Paque™ PLUS centrifugation (Amersham Pharmacia Biotech) from buffy coats obtained from healthy adult blood donors at the Karolinska Hospital. The PBMCs were cultured at a cell concentration of 106 cells/ml in RPMI 1640 medium (GIBCO BRL) supplemented with 5% heat-inactivated human AB serum.The cells were cultured alone or in the presence of indicated concentrations of rHMG-1 or LPS (E. coli 055:B5, Department of Bacteriology, Karolinska Institutet) or rTNF (NordicBioSite). Cultures were supplemented routinely with polymyxin B (10 μg/ml, 70 U/ml, Polymyxin B Sulphate; Sigma-Aldrich) to inhibit contaminating endotoxin. The polymyxin B dose was determined from separate experiments to neutralize a concentration of 100 ng/ml of LPS from E. coli 055:B5; this polymyxin B dose was neither toxic nor stimulating for cytokine production in control experiments with rTNF-α and human PBMCs (data not shown).
Trypsin Digestion of HMG-1.
A solution of purified recombinant HMG-1 (200 μg/ml, in PBS) was mixed with one volume of type I bovine trypsin (2 μg/ml, cat. no. T8003; Sigma-Aldrich) and incubated at 20°C for 12 h. Degradation was confirmed by electrophoresis on a 4–20% SDS-polyacrylamide gel. The degraded rHMG-1 was added to the cultures of human PBMCs, and TNF released into the conditioned supernatant was determined by ELISA.
TNF ELISA.
Purified rHMG-1 was administered intraperitoneally into Balb/c mice (male, 6–7 wk, 20–23 g) at indicated doses, and serum was collected 6 h later. TNF levels were determined by ELISA (R&D Systems). TNF released by human monocytes was determined using another human-specific TNF ELISA.
TNF Production in C3H/HeJ Cultured Macrophages.
Resident peritoneal macrophages were obtained by peritoneal lavage with 5 ml Hepes-buffered RPMI in C3H/HeJ mice. The macrophages were then cultured for 2 h with indicated doses of rHMG-1 or vehicle in DMEM (cat. no. 31331-028; GIBCO BRL) supplemented with 10% fetal bovine serum in pyrogene-free 48-well flat-bottomed cell culture plates (Costar Corp.).
RNase Protection Assay.
Human PBMCs tested for TNF mRNA expression were cultured in OPTI-MEM I medium. Total RNA was extracted from cells using RNAzol B reagent following the manufacturer's instructions (Tel-Test “B”, Inc.) and electrophoresed on 1.2% agarose/17% formaldehyde gel to verify RNA integrity. The levels of TNF-α (287 bp) and glyceraldehyde 3-phosphate dehydrogenase (GAPDH) mRNA (97 bp) were measured using an RNase Protection assay kit (cat. no. hck3; BD PharMingen). The antisense RNA probes were labeled with [α-32P]UTP (800 μCi/mMol; Amersham Pharmacia Biotech) using T7 RNA polymerase. Relative RNA levels were quantified with an Instant Imager (Packard Instruments).
Antibodies.
Antibodies specific to cytokines were used for indirect immunocytochemistry. TNF-α (AF-210), IL-1α (AF-200), IL-1RA (AF-280), IL-6 (AF-206), IL-8 (AF-208), IL-12 (AF-219), macrophage inflammatory protein (MIP)-1α (BAF-270), and MIP-1β (BAF-271) were antigen affinity-purified goat IgG antibodies from R&D Systems; TNF-α (mAb1+mAb11, mouse IgG1 mAb) was from BD PharMingen, IL-1β (2.D.8+1437.96-15 mouse IgG1 mAb) was from Immunokontakt). IL-10 (19.F.1+12.G.8 rat IgG2a mAb; BD PharMingen), and mouse TNF were detected using goat anti-mTNF (AF-410) from R&D Systems. The cytokine-specific antibodies were used at a final concentration of 2–5 μg/ml. Monocytes were identified by an anti–calprotectin-1 mAb (DAKO-MAC387, mouse IgG1; Dako) diluted 1:600. Secondary antibodies for immunocytochemistry included Fab2-fragmented biotinylated donkey anti–goat IgG (cat. no. 705-066-147; Jackson ImmunoResearch Laboratories) diluted 1:1,000; biotinylated goat anti–mouse IgG1 (cat. no. M32115; Caltag Laboratories) diluted 1:600; or biotinylated goat anti–rat IgG (cat. no. BA9400; Vector Laboratories) diluted 1:500.
Cytokine Detection by Indirect Immunocytochemistry.
Cytokines were detected in human mononuclear cells using computerized cell staining techniques that have been described previously 18 19 20. Cell-associated cytokines were detected with a three-step immunostaining procedure using a primary cytokine-specific antibody, a secondary biotinylated cytokine-specific antibody, and a developing step with Oregon Green–avidin D (cat. no. A6374; Molecular Probes) for UV microscopy or avidin-biotin–horseradish peroxidase (Vectastain Elite PK-6100; Vector Laboratories) followed by diaminobenzidine (DAB peroxidase substrate kit SK-4100; Vector Laboratories) for conventional microscopy. Finally, the cells were counterstained with hematoxylin, washed, dried, and mounted with buffered glycerol.
Computer-assisted Image Analysis for Quantification of Cytokine-producing Cells.
The stained cells were examined on a Polyvar 2 microscope (Reichert-Jung) equipped with a 3CCD color camera (DXC-750P; Sony Corp.) and a monochrome CCD videocamera for UV light detection (RS-170; Cohu). Images were assessed using software as described previously (Quantimet 550S; Leica Cambridge Instruments) 18 19 20.
Statistical Analysis.
Student's unpaired t test was used to compare differences between HMG-1– and LPS-stimulated cultures.
Results
HMG-1 Induces TNF Release by Cultured Human PBMCs.
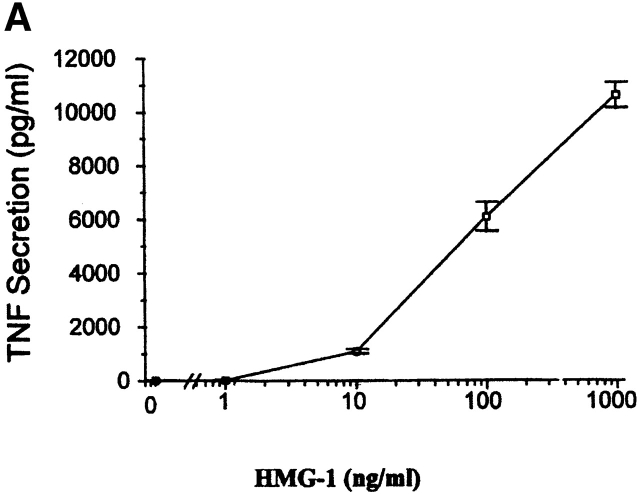
TNF is one of the earliest cytokines released by activated macrophages, and occupies a pivotal role in the pathogenesis of inflammation, endotoxic shock, and tissue injury 14 21. We measured TNF in supernatants conditioned by hPBMCs exposed to rHMG-1 for 4 h, and observed an HMG-1 dose–dependent stimulation of TNF (Fig. 1). HMG-1 concentrations as low as 10 ng/ml significantly increased TNF release. This TNF-stimulating effect of HMG-1 was observed even in the presence of polymyxin B at concentrations neutralizing >100-fold the amount of contaminating LPS. Proteolytic degradation of HMG-1 with trypsin eliminated the TNF-stimulating activity of rHMG-1 (data not shown), indicating that the induction of increased TNF synthesis by HMG-1 requires intact rHMG-1. In contrast, trypsinization of endotoxin did not destroy the TNF-stimulating activity of endotoxin (not shown), giving additional evidence that HMG-1 specifically mediated TNF release. To fully exclude the possibility that the insignificant amounts of LPS present in the experimental conditions mediated the TNF-stimulating effects of HMG-1, we added HMG-1 as a stimulating agent to primary peritoneal macrophages derived from C3H/HeJ mice. These mice are resistant to endotoxin signal transduction because of a mutation in the TLR4 endotoxin receptor 22. TNF synthesis in C3H/HeJ macrophages was increased significantly by addition of rHMG-1 (Table ), indicating that HMG-1 activation of cytokine synthesis in macrophages/monocytes occurs independently of LPS signal transduction.
Figure 1.
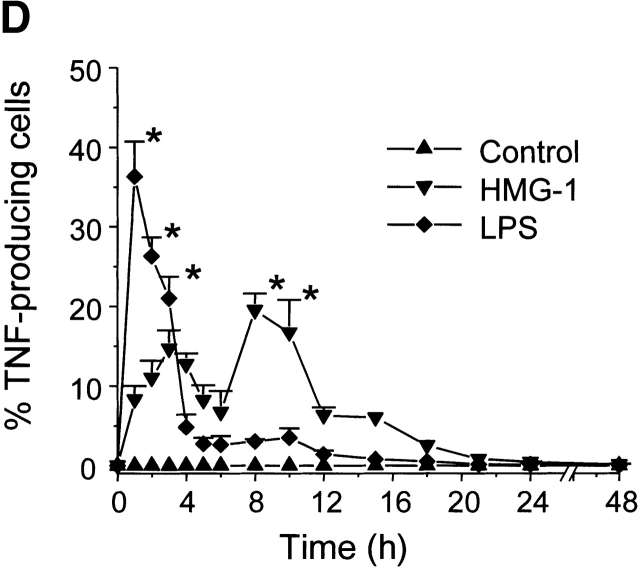
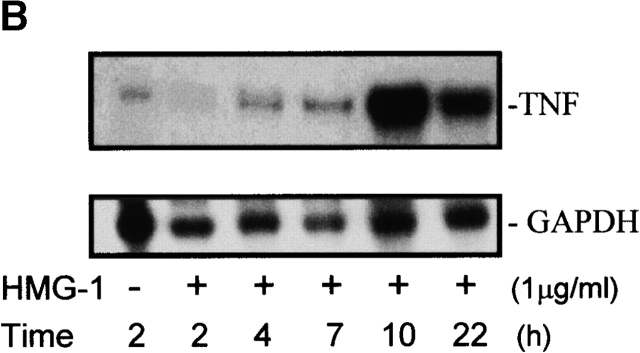
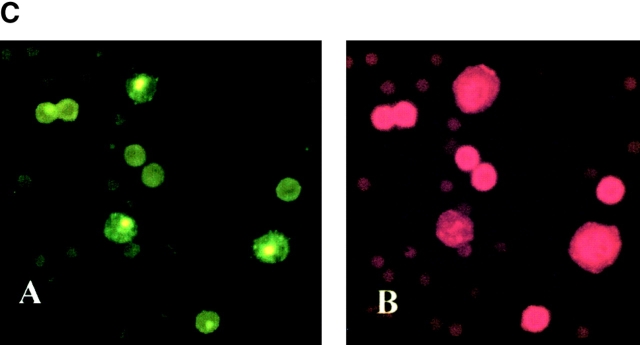
(A) HMG-1 stimulates release of TNF from cultured human PBMCs. Ficoll-separated human PBMCs were stimulated with purified rHMG-1 (0.001–1 μg/ml) in the presence of polymyxin B (10 μg/ml), and the supernatant was assayed for TNF by ELISA 4 h after stimulation. Data represent mean ± SEM of two separate experiments (in triplicate). (B) HMG-1 induces increased expression of TNF mRNA in human PBMCs. Human PBMCs were cultured in OPTI-MEM I medium with rHMG-1 (1 μg/ml) and polymyxin B (10 μg/ml). Cells were harvested at the indicated time points and assayed for TNF mRNA and GAPDH mRNA levels in controls by RNase Protection assay. Data are representative of two independent experiments. (C) Phenotypic characterization of TNF-producing PBMCs stimulated with HMG-1. Typical localization of intracellular TNF accumulation demonstrated by indirect immunofluorescence (A, Oregon Green) 8 h after HMG-1 stimulation. The same cells were stained with rhodamine for a monocytic marker (B, calprotectin 1). (D) Intracellular TNF expression after HMG-1 stimulation of PBMCs. Human PBMCs were cultured alone or with HMG-1 (1 μg/ml) in the presence of polymyxin B or LPS (100 ng/ml). The cells were harvested at the indicated time points, fixed, and stained for TNF using indirect immunofluorescence. Only monocytes contributed to the TNF formation as judged by morphology and two-color staining. The results are expressed as frequency of TNF-producing cells in the monocyte population. Data represent mean ± SEM of three separate experiments (in duplicate). *P < 0.05 vs. LPS stimulation.
Table 1.
HMG-1 Activates Cytokine Synthesis in C3H/HeJ Macrophages
| [HMG-1] | TNF-producing cells |
|---|---|
| μg/ml | % |
| 0 | 0.5 |
| 1 | 5.8 |
| 10 | 19.2 |
| 100 | 4.8 |
Resident peritoneal macrophages were obtained by peritoneal lavage from C3H/HeJ mice, and cultured for 2 h with rHMG-1 or vehicle in the doses shown. Cells were harvested, fixed on adhesive glass slides, and stained for intracellular TNF using indirect immunofluorescence. Results are based on means of 2,000 counted macrophages on each microscopy slide (in duplicate).
HMG-1 Stimulates Increased Expression of TNF mRNA in Human PBMCs.
To address the molecular basis of HMG-1–induced monocyte activation, we measured TNF mRNA levels in HMG-1–stimulated human PBMCs. Results obtained by an RNase Protection assay demonstrated that stimulation with rHMG-1 significantly induced TNF mRNA production in a time-dependent manner (Fig. 1 B). Upregulation was observed within 4 h after rHMG-1 addition, but peak TNF mRNA levels were not reached until 10 h and remained elevated for at least 22 h. This TNF mRNA kinetic profile differs significantly from that observed after LPS stimulation, in which peak TNF mRNA levels occurred within 1 or 2 h.
HMG-1 Stimulation of Intracellular TNF Synthesis in Human PBMCs Is Delayed and Biphasic Compared with LPS.
To characterize the cell type responding to HMG-1, and the kinetics of newly synthesized TNF in individual cells, we performed two-color immunofluorescent staining of PBMCs using TNF-specific and monocyte-specific (anti–calprotectin-1) antibodies (Fig. 1 C). As shown previously, addition of LPS alone to the PBMC cultures activated TNF synthesis in nearly 40% of monocytes within 1 h as judged by morphology and two-color staining (Fig. 1 D). Stimulation of PBMCs by HMG-1 also caused a significant increase in cell-associated TNF synthesis that was restricted to monocytes; TNF synthesis was not increased in lymphocytes after exposure to HMG-1. The kinetic pattern of HMG-1–induced TNF synthesis differed significantly compared with LPS-induced cells (Fig. 1 D, and Fig. 2). HMG-1–activated TNF synthesis occurred in a biphasic pattern, with an early peak at 3 h after addition of HMG-1, followed by another peak after 8–10 h. The percentage of TNF-producing cells during the early peak after HMG-1 stimulation was significantly smaller compared with LPS stimulation. HMG-1 stimulation activated a significantly higher number of TNF-producing monocytes during the later peak (Fig. 1 D), which was surprising because the release of HMG-1 itself is delayed after endotoxin administration 11. Thus, this late mediator of endotoxin lethality is also a monocyte-activating cytokine that stimulates a delayed release of TNF.
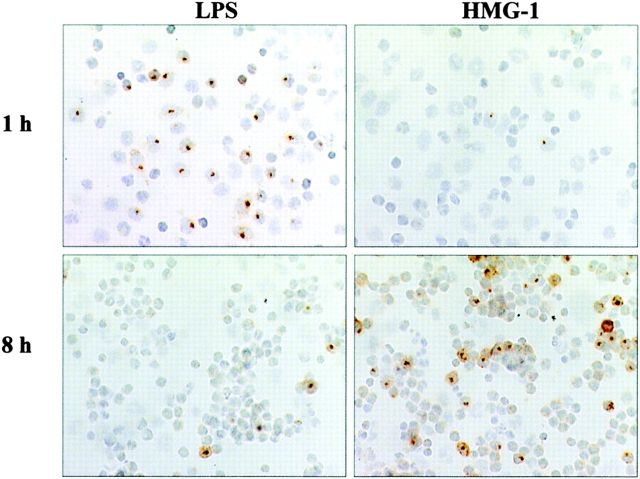
Figure 2.
TNF expression in HMG-1–stimulated human PBMCs. Human PBMCs were cultured alone or with either rHMG-1 (1 μg/ml) or LPS (100 ng/ml) (1 or 8 h), then stained for intracellular TNF. TNF-producing monocytes are revealed with an intracellular, round brown dot, representing an accumulation of TNF in the Golgi organelle of producer cells. The number of TNF-expressing monocytes in the LPS-stimulated cultures was increased significantly within 1 h compared with HMG-1–stimulated or unstimulated cultures. In contrast, HMG-1 stimulation significantly increased TNF expression at 8 h. No TNF was detected in unstimulated cells. Note pronounced monocyte aggregation after 8 h of culture.
In separate dose–response studies, we observed that HMG-1 concentrations that significantly increased TNF release by PBMCs (Fig. 1 A) also significantly upregulated the number of TNF-producing monocytes. Computer-assisted image analysis of these cultures revealed that after 8 h of stimulation with HMG-1 the intensity of individual cells staining positive for TNF compared favorably with the peak staining intensity induced by LPS stimulation for 1 h (not shown).
Administration of HMG-1 to Mice Stimulates Increased Serum TNF.
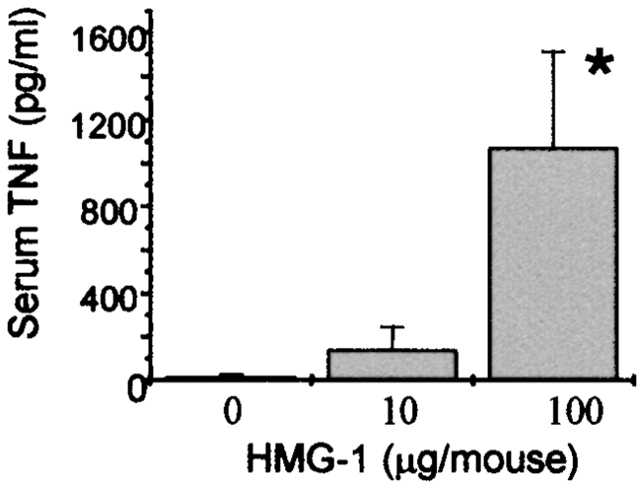
These results strongly implicated HMG-1 as a stimulus for TNF synthesis and release. Our earlier work indicated that high levels of HMG-1 are found in the serum of endotoxemic mice and septic humans 11. To determine whether HMG-1 can also stimulate TNF synthesis in vivo, we administered purified rHMG-1 to Balb/c mice and measured serum TNF by ELISA. Administration of sublethal doses of HMG-1 (10 or 100 μg) to mice significantly stimulated the appearance of TNF in the serum within 6 h (Fig. 3), indicating that systemic exposure to sublethal doses of HMG-1 activates systemic TNF release in vivo.
Figure 3.
Administration of HMG-1 in vivo stimulates increased serum TNF in mice. Balb/c mice received an intraperitoneal injection of rHMG-1 in the doses indicated; blood was obtained after 6 h and serum was analyzed for TNF by ELISA (means ± SEM, n = 3).
HMG-1 Stimulates the Synthesis of Proinflammatory Cytokines and Chemokines in Human PBMCs.
To determine whether the induction of monocyte-derived cytokines by HMG-1 is specific to TNF, we measured the production of IL-1α, IL-1β, IL-1RA, IL-6, IL-8, IL-10, MIP-1α, and MIP-1β in HMG-1–stimulated PBMCs (Fig. 4). Interestingly, the inducible cytokine response to HMG-1 was totally confined to the monocyte population as revealed by immunohistochemistry. HMG-1 significantly activated the synthesis of all cytokines assayed, with the exception of the antiinflammatory cytokine IL-10 (Fig. 4) and the proinflammatory cytokine IL-12 (not shown). The frequency of proinflammatory cytokine– or chemokine-producing monocytes was remarkably similar after HMG-1 or LPS stimulation, except that the induction of cytokine synthesis was delayed by 1–4 h in the HMG-1–treated cultures compared with LPS. However, there was no delay in the upregulation of the antiinflammatory cytokines IL-1RA and IL-10 (Fig. 4). HMG-1 stimulation of both IL-6 and TNF was biphasic.
Figure 4.

HMG-1 stimulates the expression of cytokines and chemokines in human PBMCs. Human PBMCs were cultured with either rHMG-1 (1 μg/ml) plus polymyxin B (10 μg/ml) or LPS alone (100 ng/ml). Cells were harvested in longitudinal studies, fixed, and stained using indirect immunofluorescence. Monocytes were the only cells contributing to the synthesis of the studied mediators, confirmed by two-color staining. *P < 0.05 vs. LPS.
Discussion
These results demonstrate for the first time that HMG-1 acts as a cytokine that specifically stimulates cytokine synthesis in human monocytes. Macrophages and monocytes occupy a central role in coordinating the immune response to injury and infection. The observation that HMG-1, a mediator of late endotoxin lethality, can activate additional downstream cytokine cascades has widespread implications, especially because HMG-1 is nearly as potent as LPS in stimulating monocyte cytokine synthesis.
Our findings also indicate that monocytes, but not lymphocytes, are cellular targets for the cytokine-inducing activity of HMG-1. We have previously reported that LPS, TNF, or IL-1 can stimulate the production of HMG-1 by monocytes 11. The present study extends these findings, and importantly reveals a reciprocal functional relationship between the activities of the early (TNF and IL-1) and late (HMG-1) cytokines. It is now apparent that HMG-1 can participate in “cross-talk” for the propagation and amplification of downstream proinflammatory responses. Here we used three independent cytokine detection assays to confirm the production of TNF after HMG-1 exposure in vitro (Fig. 1 and Fig. 2) or in vivo (Fig. 3). TNF synthesis was readily demonstrated at the mRNA level (Fig. 1 B) and at the protein level both intracellularly (Fig. 1c and Fig. d, and Fig. 2) and extracellularly (Fig. 1 A and Fig. 3). The computer-assisted image analysis to detect intracellular TNF offered a significant advantage over flow cytometry analysis. The latter method would have grossly underestimated the magnitude of TNF produced, which mainly occurred in aggregates of activated monocytes (Fig. 2), routinely gated out by the flow cytometer.
HMG-1 was previously implicated as a ligand for the monocyte receptors for advanced glycated proteins (RAGE) 23 24. RAGE receptor–ligand interaction with glycated proteins can indeed activate macrophages 25, and radiolabeled HMG-1 binds specifically to human monocytes (Yang, H., and K.J. Tracey, unpublished observations), but it is presently unknown whether HMG-1 bound to RAGE mediates cytokine synthesis. It remains theoretically possible that HMG-1 activation of monocytes may also occur via receptor-independent pathways. For instance, HMG-1 significantly increases cellular uptake of DNA 26, and bacterial DNA containing CpG motifs that activate monocyte cytokine synthesis are ubiquitous during infection 27. Our observations that HMG-1 stimulates monocytes but not lymphocytes to produce cytokines indicate that the proinflammatory role of HMG-1 is cell type specific.
Cytokines are defined as proteins released from activated immunocytes that influence diverse metabolic or immunological response in other cells 28. It is now clear that as a cytokine, extracellular HMG-1 occupies a unique position in the proinflammatory mediator cascade. Clinical reports indicated that increased levels of antibodies against HMG-1 can be found in patients with autoimmune diseases 29 30, and that HMG-1 levels are increased in patients with sepsis or hemorrhagic shock 11 12. HMG-1 has been termed a late mediator of endotoxin lethality, because its release is delayed by several hours compared with other proinflammatory cytokines that mediate shock and tissue injury 11. Once released, however, HMG-1 is a potent activator of monocyte cytokine synthesis that mediates a delayed and prolonged phase of monocyte activation.
Acknowledgments
This work was supported by grants to U. Andersson from the Swedish Medical Research Council, the Swedish National Cancer Foundation, the Swedish Association against Rheumatism, B. von Kantzow's Foundation, and King Gustaf V's Foundation; and by a grant to K.J. Tracey from the National Institutes of Health.
References
- Canaple L., Decoville M., Leng M., Locker D. The Drosophila DSP1 gene encoding an HMG 1-like proteingenomic organization, evolutionary conservation and expression. Gene. 1997;184:285–290. doi: 10.1016/s0378-1119(96)00616-6. [DOI] [PubMed] [Google Scholar]
- Goodwin G.H., Johns E.W. The isolation and purification of the high mobility group (HMG) nonhistone chromosomal proteins. Methods Cell Biol. 1977;16:257–267. doi: 10.1016/s0091-679x(08)60104-1. [DOI] [PubMed] [Google Scholar]
- Bustin M., Reeves R. High-mobility-group chromosomal proteinsarchitectural components that facilitate chromatin function. Prog. Nucleic Acid Res. Mol. Biol. 1996;54:35–100. doi: 10.1016/s0079-6603(08)60360-8. [DOI] [PubMed] [Google Scholar]
- Ferrari S., Ronfani L., Calogero S., Bianchi M.E. The mouse gene coding for high mobility group 1 protein (HMG1) J. Biol. Chem. 1994;269:28803–28808. [PubMed] [Google Scholar]
- Landsman D., Bustin M. A signature for the HMG-1 box DNA-binding proteins. Bioessays. 1993;15:539–546. doi: 10.1002/bies.950150807. [DOI] [PubMed] [Google Scholar]
- Einck L., Bustin M. The intracellular distribution and function of the high mobility group chromosomal proteins. Exp. Cell. Res. 1985;156:295–310. doi: 10.1016/0014-4827(85)90539-7. [DOI] [PubMed] [Google Scholar]
- Bianchi M.E., Beltrame M., Paonessa G. Specific recognition of cruciform DNA by nuclear protein HMG1. Science. 1989;243:1056–1059. doi: 10.1126/science.2922595. [DOI] [PubMed] [Google Scholar]
- Bianchi M.E., Beltrame M. Flexing DNAHMG-box proteins and their partners. Am. J. Hum. Genet. 1998;63:1573–1577. doi: 10.1086/302170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giese K., Cox J., Grosschedl R. The HMG domain of lymphoid enhancer factor 1 bends DNA and facilitates assembly of functional nucleoprotein structures. Cell. 1992;69:185–195. doi: 10.1016/0092-8674(92)90129-z. [DOI] [PubMed] [Google Scholar]
- Bianchi M.E., Falciola L., Ferrari S., Lilley D.M. The DNA binding site of HMG1 protein is composed of two similar segments (HMG boxes), both of which have counterparts in other eukaryotic regulatory proteins. EMBO (Eur. Mol. Biol. Organ.) J. 1992;11:1055–1063. doi: 10.1002/j.1460-2075.1992.tb05144.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Bloom O., Zhang M., Vishnubhakat J.M., Ombrellino M., Che J., Frazier A., Yang H., Ivanova S., Borovikova L. HMG-1 as a late mediator of endotoxin lethality in mice. Science. 1999;285:248–251. doi: 10.1126/science.285.5425.248. [DOI] [PubMed] [Google Scholar]
- Ombrellino M., Wang H., Ajemian M.S., Talhouk A., Scher L.A., Friedman S.G., Tracey K.J. Increased serum concentrations of high-mobility-group protein 1 in haemorrhagic shock. Lancet. 1999;354:1446–1447. doi: 10.1016/S0140-6736(99)02658-6. [DOI] [PubMed] [Google Scholar]
- Fong Y., Tracey K.J., Moldawer L.L., Hesse D.G., Manogue K.R., Kenney J.S., Lee A.T., Kuo G.C., Allison A.C., Lowry S.F., Cerami A. Antibodies to cachectin/TNF reduce interleukin-1β and interleukin-6 appearance during lethal bacteremia. J. Exp. Med. 1989;170:1627–1633. doi: 10.1084/jem.170.5.1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracey K.J., Fong Y., Hesse D.G., Manogue K.R., Lee A.T., Kuo G.C., Lowry S.F., Cerami A. Anti-cachectin/TNF monoclonal antibodies prevent septic shock during lethal bacteraemia. Nature. 1987;330:662–664. doi: 10.1038/330662a0. [DOI] [PubMed] [Google Scholar]
- Dinarello C.A. Biologic basis for interleukin-1 in disease. Blood. 1996;87:2095–2147. [PubMed] [Google Scholar]
- Okusawa S., Yancey K.B., van der Meer J.W.M., Endres S., Lonnemann G., Hefter K., Frank M.M., Burke J.F., Dinarello C.A., Gelfand J.A. C5a stimulates secretion of tumor necrosis factor from human mononuclear cells in vitro. J. Exp. Med. 1988;168:443–448. doi: 10.1084/jem.168.1.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinarello C.A., Cannon J.G., Wolff S.M., Bernheim H.A., Beutler B., Cerami A., Figari I.S., Palladino M.A.J., O'Connor J.V. Tumor necrosis factor (cachectin) is an endogenous pyrogen and induces production of interleukin 1. J. Exp. Med. 1986;163:1433–1450. doi: 10.1084/jem.163.6.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henter J.I., Soder O., Andersson U. Identification of individual tumor necrosis factor/cachectin-producing cells after lipopolysaccharide induction. Eur. J. Immunol. 1988;18:983–988. doi: 10.1002/eji.1830180703. [DOI] [PubMed] [Google Scholar]
- Sander B., Andersson J., Andersson U. Assessment of cytokines by immunofluorescence and the paraformaldehyde-saponin procedure. Immunol. Rev. 1991;119:65–93. doi: 10.1111/j.1600-065x.1991.tb00578.x. [DOI] [PubMed] [Google Scholar]
- Bjork L., Fehniger T.E., Andersson U., Andersson J. Computerized assessment of production of multiple human cytokines at the single-cell level using image analysis. J. Leukoc. Biol. 1996;59:287–295. doi: 10.1002/jlb.59.2.287. [DOI] [PubMed] [Google Scholar]
- Tracey K.J., Beutler B., Lowry S.F., Merryweather J., Wolpe S., Milsark I.W., Hariri R.J., Fahey T.F., III, Zentella A., Albert J.D. Shock and tissue injury induced by recombinant human cachectin. Science. 1986;234:470–474. doi: 10.1126/science.3764421. [DOI] [PubMed] [Google Scholar]
- Poltorak A., He X., Smirnova I., Liu M.Y., Huffel C.V., Du X., Birdwell D., Alejos E., Silva M., Galanos C. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr micemutations in Tlr4 gene. Science. 1998;282:2085–2088. doi: 10.1126/science.282.5396.2085. [DOI] [PubMed] [Google Scholar]
- Hofmann M.A., Drury S., Fu C., Qu W., Taguchi A., Lu Y., Avila C., Kambham N., Bierhaus A., Nawroth P. RAGE mediates a novel proinflammatory axisa central cell surface receptor for S100/calgranulin polypeptides. Cell. 1999;97:889–901. doi: 10.1016/s0092-8674(00)80801-6. [DOI] [PubMed] [Google Scholar]
- Li J., Qu X., Schmidt A.M. Sp1-binding elements in the promoter of RAGE are essential for amphoterin-mediated gene expression in cultured neuroblastoma cells. J. Biol. Chem. 1998;273:30870–30878. doi: 10.1074/jbc.273.47.30870. [DOI] [PubMed] [Google Scholar]
- Ichikawa K., Yoshinari M., Iwase M., Wakisaka M., Doi Y., Iino K., Yamamoto M., Fujishima M. Advanced glycosylation end products induced tissue factor expression in human monocyte-like U937 cells and increased tissue factor expression in monocytes from diabetic patients. Atherosclerosis. 1998;136:281–287. doi: 10.1016/s0021-9150(97)00221-9. [DOI] [PubMed] [Google Scholar]
- Namiki Y., Takahashi T., Ohno T. Gene transduction for disseminated intraperitoneal tumor using cationic liposomes containing non-histone chromatin proteinscationic liposomal gene therapy of carcinomatosa. Gene Ther. 1998;5:240–246. doi: 10.1038/sj.gt.3300577. [DOI] [PubMed] [Google Scholar]
- Hacker H. Signal transduction pathways activated by CpG-DNA. Curr. Top. Microbiol. Immunol. 2000;247:77–92. doi: 10.1007/978-3-642-59672-8_5. [DOI] [PubMed] [Google Scholar]
- Nathan C.F. Secretory products of macrophages. J. Clin. Invest. 1987;79:319–326. doi: 10.1172/JCI112815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung F., Neuer G., Bautz F.A. Antibodies against a peptide sequence located in the linker region of the HMG-1/2 box domains in sera from patients with juvenile rheumatoid arthritis. Arthritis Rheum. 1997;40:1803–1809. doi: 10.1002/art.1780401012. [DOI] [PubMed] [Google Scholar]
- Ayer L.M., Senecal J.L., Martin L., Dixon G.H., Fritzler M.J. Antibodies to high mobility group proteins in systemic sclerosis. J. Rheumatol. 1994;21:2071–2075. [PubMed] [Google Scholar]