The job of the immune system is to respond to signals released by tissues that are being destroyed by foreign invaders, such as viruses and bacteria, and to destroy the invaders. These signals have been termed “danger” signals (1). Destruction of tissues by uncontrolled cell growth characteristic of cancer is expected to also generate danger signals, albeit possibly qualitatively different due to the absence of infectious agents. Evidence that the immune system not only detects the presence of cancer but also destroys it and remembers it through the recognition of tumor-specific antigens was provided in the late 1950's (2) and has been confirmed many times in increasingly more sophisticated animal models and in cancer patients. What has not been fully accepted, however, in part because supporting data are only now emerging, is that the immune system can recognize precursors of cancer and in most instances destroy them before they become clinically apparent. This concept termed “immune surveillance” has had as many proponents as opponents, the debate being fueled by reasoned arguments rather than experimental data. In recent years, this has begun to change. Studies in animal models and in certain human diseases are providing evidence that the immune system monitors and modulates tumor growth (3, 4). As the report by Dhodapkar et al. (5) in this issue illustrates, one way to document cancer surveillance by the human immune system could be to analyze immune responses against a premalignant disease, precursor to cancer.
A Fresh Look at Cancer Immunosurveillance.
If the immune system is involved in protection from tumor growth, then immunodeficient animals should develop tumors more frequently. Schreiber and colleagues tested this hypothesis and found that, indeed, mice lacking lymphocytes or deficient in IFN signaling (RAG2−/− mice and STAT1−/− mice, respectively) develop spontaneous tumors and are more susceptible to carcinogen-induced tumors than WT mice (3). Furthermore, they have shown that tumors grown in immunocompetent mice are much less aggressive and often express different antigens to those from immunodeficient mice. This influence of the immune system on the nature of the tumor has been termed “cancer immunoediting.”
Support for cancer immunoediting in humans comes from highly reproducible findings of tumor-specific cellular and humoral immune responses in patients with cancer, concomitant with loss of either the antigens or the presenting HLA molecules on the tumor cells (6). However, proof that these immune responses actually alter the course of disease in people is more difficult to find. Evidence has been sought in patients with paraneoplastic neurologic degeneration (7). These patients present initially with neurologic problems, but after a more thorough examination they are found to harbor small adenocarcinomas. These tumors, which are most frequently breast, ovarian, or lung cancers, express defined neuronal antigens, and the patients produce high titer antibodies and a high frequency of cytotoxic T cells against these antigens. This immunity, which is destructive to neuronal tissue, appears to have been generated in response to the tumor and to be suppressing the growth of the tumor (8). In general, tumors in these patients are very small, not metastatic, and often extensively infiltrated with lymphocytes. They have also been known to spontaneously regress. These rare windows of opportunity to witness effective antitumor immunity in humans suggest that it should be possible to use cancer vaccines to generate protective tumor-specific immunity (9, 10).
Moving Toward Premalignancy Vaccines.
Despite our extensive knowledge of antitumor immune effector mechanisms and the long list of well-defined tumor antigens (11), attempts to elicit or boost effective immune responses in patients who have clinically evident cancer (therapeutic vaccines) have had very limited success (9). Although it is almost certain that the vaccines tested could be improved further, the greatest barriers to success have been the immunosuppressed status of cancer patients and the many immune evasion mechanisms acquired by tumors as they progress from an early preneoplastic lesion to a fully malignant cancer (6). Even if we can elicit more robust immune responses in cancer patients, the immune evasion mechanisms will be hard to overcome.
To take advantage of the strengths of the immune response (its specificity, multiple effector functions, and memory) while recognizing its weaknesses (that it is slow to develop and ineffective against established tumors), we must change the target of antitumor vaccines. Until now, tumor immunologists have focused on antigens expressed on tumor cells. However, cancer geneticists, molecular biologists, and pathologists have provided a better understanding of the process of tumorigenesis, and for several human cancers the premalignant states have been defined (12–16). It appears that these early steps in the process do not escape the attention of the immune system.
Immune Response Against Premalignancy.
In this issue, Dhodapkar et al. (5) focus on patients with preneoplastic gammopathy (MGUS), a clonal expansion of transformed plasma cells that is a direct precursor of multiple myelomas (17). Many of these patients do not progress to myelomas. The authors postulated that the lack of progression might be due in part to immune surveillance. They found that MGUS patients had effector CD8+ T cells that responded in vitro to DCs that had taken up and processed the preneoplastic plasma cells. In contrast, in myeloma patients T cells must be expanded for 1–2 wk in culture before tumor-specific T cell responses can be detected (18). MGUS-specific T cells reside in the BM, also the residence of the preneoplastic plasma cells. The exact mechanism of control of tumor progression by MGUS-specific T cells is not known. The T cells produce IFN-γ, and thus, in addition to directly eliminating the preneoplastic cells they can potentially modulate the IFN-γ responsive STAT-3 and IL-6 signaling important for myeloma growth (19, 20). IFN-γ can also inhibit angiogenesis and osteoclastogenesis, which are features of multiple myelomas but not of MGUS (21).
The target antigens recognized by MGUS-specific T cells were not expressed on one multiple myeloma cell line that was tested. If this holds true for other myeloma cell lines, it would imply that full transformation to myeloma might be a result of mutations that allow escape from T cell immunity. Alternatively, the inability of the immune response to fully eliminate the preneoplastic clone may in some cases lead to exhaustion or deletion of MGUS-specific T cells and allow development of myelomas. Although the frequency of MGUS-specific T cells was more than 50 times higher than myeloma-specific T cells, this frequency (55/105) may still be too low to completely eliminate the preneoplastic clone. One is tempted to postulate that boosting the frequency 10-fold or more by vaccination could result in a complete elimination of preneoplastic cells.
Identification of immunogenic antigens on preneoplastic cells provides an unprecedented opportunity to prepare the immune system through vaccination for the elimination of transformed cells at their earliest manifestation. Thus, future efforts should be focused on identifying antigens that are differentially expressed between normal cells and preneoplastic cells. Several mouse models of human cancer exist in which tumors develop early in life and undergo step-wise progression similar to the human cancer (10, 22). Others are in the process of being created either using transgenic or gene knockout approaches. These models will be useful in documenting the effectiveness of the immune system to control tumor formation and progression and its specificity in eliminating abnormal cells while sparing normal tissue. Several tumor antigens that have been well characterized for their tumor-specific expression and immunogenicity are already known to be expressed in preneoplastic precursor lesions. They are ready to be tested in vitro and in animal models for their ability to protect against incipient tumors.
MUC1.
Epithelial mucin MUC1 was the first human tumor antigen to be reported as a target for human cytotoxic T cells (23). Moreover, it was the first example of a tumor antigen recognized by T cells that is shared by different tumors, such as breast, colon, pancreas, ovary, lung, and multiple myelomas. Expression of MUC1 on normal tissues is usually at a much lower level and characterized by a different repertoire of immune epitopes. Some of the epitopes are exquisitely tumor specific, owing in part to differential glycosylation in normal and tumor cells (24). Tumor forms of MUC1 and other mucins are also expressed in many preneoplastic lesions, such as pancreatic intraepithelial neoplasia, which are precursors of pancreatic cancer (12), and adenomatous polyps, which are precursors of colon cancer (25). Considering that MUC1 is also expressed on multiple myeloma, the report by Dhodapkar et al. (5) begs the question whether MUC1-specific T cells can be detected in MGUS patients. We have shown recently that some patients who have had adenomatous polyps removed have high levels of antibody against MUC1 (26). Importantly, this antibody is of the IgG isotype, suggesting the involvement of helper T cells. In contrast, patients with colon cancer have low levels of anti-MUC1 antibodies of the IgM isotype, indicating the lack of T cell help (27).
Vaccination against tumor-specific epitopes on MUC1 protects mice from a MUC1+ tumor challenge (28). A good mouse model of spontaneous pancreatic cancer has been developed in which the potential of MUC1-specific immunity to eliminate preneoplastic lesions and prevent tumor progression can be studied (22). Early in life, these mice exhibit dysplasia in the pancreas that progress to microadenomas and then to fully transformed MUC1+ pancreatic adenocarcinomas. This process is accompanied by appearance at ∼15 wk of age of low frequency MUC1-specific CD8+ T cells that disappear as the tumor progresses (29). However, when expanded in vitro and adoptively transferred in large numbers, these T cells can prevent growth of a transplanted tumor (30). These results suggest that inducing a robust anti-MUC1 response before tumor occurrence could serve to prevent development and progression of pancreatic cancer.
Cyclin B1.
Another shared tumor antigen shown recently to be recognized by both human antibodies and T cells is cyclin B1 (31). Tumors of various types, leukemias, lymphomas, and epithelial adenocarcinomas were found to overexpress cyclin B1 protein in the cytoplasm, and cyclin B1–derived peptides were presented in the context of HLA–class I and class II molecules. Patients with cyclin B1–overexpressing tumors have circulating cyclin B1–specific CD8+ T cells and several different isotypes of anti–cyclin B1 antibody. As in the case of anti-MUC1 responses, the T cell frequency is low, as is the antibody titer. Cyclin B1 overexpression is a result of inactivation of p53 function (32). Thus, all tumors that have either mutated or deleted p53 can be targets of anti–cyclin B1 immunity. P53 mutations are early events in the carcinogenesis of many tumors and are found with high frequency in premalignant lesions (33, 34). This makes early lesions especially good targets for cyclin B1–specific immune responses. For example, many lung cancers overexpress cyclin B1 and those that do have a much more aggressive phenotype (35). Robust cyclin B1–specific immunity would be desirable to change the course of these cancers, but generating robust immunity in lung cancer patients, as in all other cancer patients, is likely to be very difficult. Premalignant lesions in the lung are characterized by p53 mutations (36), which would be expected to lead to cyclin B1 overexpression. There is currently no treatment for individuals with preneoplastic lung disease. These individuals would be ideal candidates for prophylactic vaccines, and cyclin B1 is one potential candidate antigen.
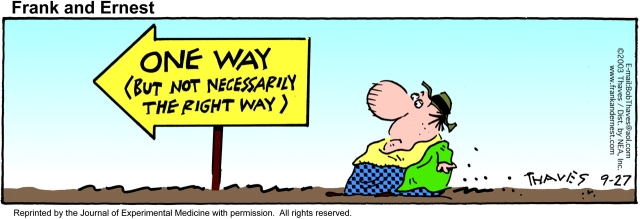
Change in Direction.
In addition to MUC1 and cyclin B1, there are many other tumor antigens that are being tested as components of therapeutic cancer vaccines, which may also be expressed in premalignancy and could be potentially much more effective in the prophylactic setting. In parallel with screening of the known tumor antigens for their expression in premalignant disease, effort and resources need to be invested in the search for new antigens that characterize preneoplastic disease and in the development of animal models in which their potential to prevent cancer can be tested. The tremendous effort that has gone into tumor antigen discovery in the last 15 yr has yielded many candidate antigens that can be used in prophylactic vaccines. More importantly, it has established numerous experimental methods that can now be applied to antigen discovery in premalignant disease.
Figure .
References
- 1.Matzinger, P. 2002. The danger model: a renewed sense of self. Science. 296:301–305. [DOI] [PubMed] [Google Scholar]
- 2.Prehn, R.T., and J.M. Main. 1957. Immunity to methylcholantrene-induced sarcomas. J. Natl. Cancer Inst. 18:769–778. [PubMed] [Google Scholar]
- 3.Dunn, G.P., A.T. Bruce, H. Ikeda, L.J. Old, and R.D. Schreiber. 2002. Cancer immunoediting: from immunosurveillance to tumor escape. Nat. Immunol. 3:991–998. [DOI] [PubMed] [Google Scholar]
- 4.Darnell, R.B., and J.B. Posner. 2003. Observing the invisible: successful tumor immunity in humans. Nat. Immunol. 4:201. [DOI] [PubMed] [Google Scholar]
- 5.Dhodapkar, M.V., J. Krasovsky, K. Osman, and M.D. Geller. 2003. Vigorous premalignancy-specific effector T cell response in the bone marrow of patients with monoclonal gammopathy. J. Exp. Med. 198:1753–1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marincola, F.M., E.M. Jaffee, D.J. Hicklin, and S. Ferrone. 2000. Escape of human solid tumors from T-cell recognition: molecular mechanisms and functional significance. Adv. Immunol. 74:181–273. [DOI] [PubMed] [Google Scholar]
- 7.Musunuru, K., and R.B. Darnell. 2001. Paraneoplastic neurologic disease antigens: RNA-binding proteins and signaling proteins in neuronal degeneration. Annu. Rev. Neurosci. 24:239–262. [DOI] [PubMed] [Google Scholar]
- 8.Albert, M.L., J.C. Darnell, A. Bender, L.M. Francisco, N. Bhardwaj, and R.B. Darnell. 1998. Tumor-specific killer cells in paraneoplastic cerebellar degeneration. Nat. Med. 4:1321–1324. [DOI] [PubMed] [Google Scholar]
- 9.Finn, O.J. 2003. Cancer vaccines: between the idea and the reality. Nat. Rev. Immunol. 3:630–641. [DOI] [PubMed] [Google Scholar]
- 10.Finn, O.J., and G. Forni. 2002. Prophylactic cancer vaccines. Curr. Opin. Immunol. 14:172–177. [DOI] [PubMed] [Google Scholar]
- 11.Van Der Bruggen, P., Y. Zhang, P. Chaux, V. Stroobant, C. Panichelli, E.S. Schultz, J. Chapiro, B.J. Van Den Eynde, F. Brasseur, and T. Boon. 2002. Tumor-specific shared antigenic peptides recognized by human T cells. Immunol. Rev. 188:51–64. [DOI] [PubMed] [Google Scholar]
- 12.Hruban, R.H., N.V. Adsay, J. Albores-Saavedra, C. Compton, E.S. Garrett, S.N. Goodman, S.E. Kern, D.S. Klimstra, G. Kloppel, D.S. Longnecker, et al. 2001. Pancreatic intraepithelial neoplasia: a new nomenclature and classification system for pancreatic duct lesions. Am. J. Surg. Pathol. 25:579–586. [DOI] [PubMed] [Google Scholar]
- 13.Tsutsumi, M., and Y. Konishi. 2000. Precancerous conditions for pancreatic cancer. J. Hepatobiliary Pancreat. Surg. 7:575–579. [DOI] [PubMed] [Google Scholar]
- 14.Kirkali, Z., and K. Yorukoglu. 2001. Premalignant lesions in the kidney. Scientific World Journal. 1:855–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Petty, T.L. 2003. Sputum cytology for the detection of early lung cancer. Curr. Opin. Pulm. Med. 9:309–312. [DOI] [PubMed] [Google Scholar]
- 16.Schnitt, S.J. 2003. The diagnosis and management of pre-invasive breast disease: flat epithelial atypia-classification, pathologic features and clinical significance. Breast Cancer Res. 5:263–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kyle, R.A., T.M. Therneau, S.V. Rajkumar, J.R. Offord, D.R. Larson, M.F. Plevak, and L.J. Melton, III. 2002. A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N. Engl. J. Med. 346:564–569. [DOI] [PubMed] [Google Scholar]
- 18.Dhodapkar, M.V., J. Krasovsky, and K. Olson. 2002. T cells from the tumor microenvironment of patients with progressive myeloma can generate strong, tumor-specific cytolytic responses to autologous, tumor-loaded dendritic cells. Proc. Natl. Acad. Sci. USA. 99:13009–13013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Catlett-Falcone, R., W.S. Dalton, and R. Jove. 1999. STAT proteins as novel targets for cancer therapy. Signal transducer an activator of transcription. Curr. Opin. Oncol. 11:490–496. [DOI] [PubMed] [Google Scholar]
- 20.Portier, M., X.G. Zhang, E. Caron, Z.Y. Lu, R. Bataille, and B. Klein. 1993. gamma-Interferon in multiple myeloma: inhibition of interleukin-6 (IL-6)-dependent myeloma cell growth and downregulation of IL-6-receptor expression in vitro. Blood. 81:3076–3082. [PubMed] [Google Scholar]
- 21.Takayanagi, H., K. Ogasawara, S. Hida, T. Chiba, S. Murata, K. Sato, A. Takaoka, T. Yokochi, H. Oda, K. Tanaka, et al. 2000. T-cell-mediated regulation of osteoclastogenesis by signalling cross-talk between RANKL and IFN-gamma. Nature. 408:600–605. [DOI] [PubMed] [Google Scholar]
- 22.Gendler, S.J., and P. Mukherjee. 2001. Spontaneous adenocarcinoma mouse models for immunotherapy. Trends Mol. Med. 7:471–475. [DOI] [PubMed] [Google Scholar]
- 23.Barnd, D.L., M.S. Lan, R.S. Metzgar, and O.J. Finn. 1989. Specific, major histocompatibility complex-unrestricted recognition of tumor-associated mucins by human cytotoxic T cells. Proc. Natl. Acad. Sci. USA. 86:7159–7163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vlad, A.M., S. Muller, M. Cudic, H. Paulsen, L. Otvos, Jr., F.G. Hanisch, and O.J. Finn. 2002. Complex carbohydrates are not removed during processing of glycoproteins by dendritic cells: processing of tumor antigen MUC1 glycopeptides for presentation to major histocompatibility complex class II–restricted T cells. J. Exp. Med. 196:1435–1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scheiden, R., J. Sand, M. Pandin, Y. Wagener, and C. Capesius. 2000. Colorectal high-grade adenomas: incidence, localization and adenoma-adenocarcinoma ratio in a retrospective and comparative population-based study of 225 consecutive cases between 1988 and 1996. Int. J. Colorectal Dis. 15:29–34. [DOI] [PubMed] [Google Scholar]
- 26.Turner, M.S., J.R. McKolanis, R.K. Ramanathan, D.C. Whitcomb, and O.J. Finn. 2003. Mucins in gastrointestinal cancers. Cancer Chemotherapy and Biological Response Modifiers, Annual 21. R.S.G. Giaccone, and P. Sondel, editors. Elsevier Science Publishing Co. Inc., New York. In press. [DOI] [PubMed]
- 27.Kotera, Y., J.D. Fontenot, G. Pecher, R.S. Metzgar, and O.J. Finn. 1994. Humoral immunity against a tandem repeat epitope of human mucin MUC-1 in sera from breast, pancreatic, and colon cancer patients. Cancer Res. 54:2856–2860. [PubMed] [Google Scholar]
- 28.Soares, M.M., V. Mehta, and O.J. Finn. 2001. Three different vaccines based on the 140-amino acid MUC1 peptide with seven tandemly repeated tumor-specific epitopes elicit distinct immune effector mechanisms in wild-type versus MUC1-transgenic mice with different potential for tumor rejection. J. Immunol. 166:6555–6563. [DOI] [PubMed] [Google Scholar]
- 29.Mukherjee, P., A.R. Ginardi, C.S. Madsen, T.L. Tinder, F. Jacobs, J. Parker, B. Agrawal, B.M. Longenecker, and S.J. Gendler. 2001. MUC1-specific CTLs are non-functional within a pancreatic tumor microenvironment. Glycoconj. J. 18:931–942. [DOI] [PubMed] [Google Scholar]
- 30.Mukherjee, P., A.R. Ginardi, T.L. Tinder, C.J. Sterner, and S.J. Gendler. 2001. MUC1-specific cytotoxic T lymphocytes eradicate tumors when adoptively transferred in vivo. Clin. Cancer Res. 7:848s–855s. [PubMed] [Google Scholar]
- 31.Kao, H., J.A. Marto, T.K. Hoffmann, J. Shabanowitz, S.D. Finkelstein, T.L. Whiteside, D.F. Hunt, and O.J. Finn. 2001. Identification of cyclin B1 as a shared human epithelial tumor-associated antigen recognized by T cells. J. Exp. Med. 194:1313–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yu, M., Q. Zhan, and O.J. Finn. 2002. Immune recognition of cyclin B1 as a tumor antigen is a result of its overexpression in human tumors that is caused by non-functional p53. Mol. Immunol. 38:981–987. [DOI] [PubMed] [Google Scholar]
- 33.Hollstein, M., D. Sidransky, B. Vogelstein, and C.C. Harris. 1991. p53 mutations in human cancers. Science. 253:49–53. [DOI] [PubMed] [Google Scholar]
- 34.Fedorov, L.M., T. Papadopoulos, O.Y. Tyrsin, T. Twardzik, R. Gotz, and U.R. Rapp. 2003. Loss of p53 in craf-induced transgenic lung adenoma leads to tumor acceleration and phenotypic switch. Cancer Res. 63:2268–2277. [PubMed] [Google Scholar]
- 35.Soria, J.C., S.J. Jang, F.R. Khuri, K. Hassan, D. Liu, W.K. Hong, and L. Mao. 2000. Overexpression of cyclin B1 in early-stage non-small cell lung cancer and its clinical implication. Cancer Res. 60:4000–4004. [PubMed] [Google Scholar]
- 36.Kalomenidis, I., D. Orphanidou, G. Papamichalis, T. Vassilakopoulos, A. Scorilas, A. Rasidakis, H. Papastamatiou, J. Jordanoglou, C. Roussos, and A. Skorilas. 2001. Combined expression of p53, Bcl-2, and p21WAF-1 proteins in lung cancer and premalignant lesions: association with clinical characteristics. Lung. 179:265–278. [DOI] [PubMed] [Google Scholar]