Abstract
Interleukin (IL)-10 and transforming growth factor (TGF)-β1 are suppressor cytokines that frequently occur together during a regulatory T cell response. Here we used a one gene doxycycline (Dox)-inducible plasmid encoding TGF-β1 to analyze this association and test its utility. In initial studies, we showed that intranasal administration of this plasmid (along with Dox) led to the appearance of TGF-β1–producing cells (in spleen and lamina propria) and the almost concomitant appearance of IL-10–producing cells. Moreover, we showed that these cells exert Dox-regulated suppression of the T helper cell (Th)1-mediated inflammation in trinitrobenzene sulfonic acid colitis. In subsequent in vitro studies using retroviral TGF-β1 expression, we established that IL-10 production by Th1 cells occurs after exposure to TGF-β1 from either an endogenous or exogenous source. In addition, using a self-inactivating retrovirus luciferase reporter construct we showed that TGF-β1 induces Smad4, which then binds to and activates the IL-10 promoter. Furthermore, intranasal TGF-β1 plasmid administration ameliorates bleomycin-induced fibrosis in wild-type but not IL-10–deficient mice, strongly suggesting that the amelioration is IL-10 dependent and that IL-10 protects mice from TGF-β1–mediated fibrosis. Taken together, these findings suggest that the induction of IL-10 by TGF-β1 is not fortuitous, but instead fulfills important requirements of TGF-β1 function after its secretion by regulatory T cells.
Keywords: Th1 cells, trinitrobenzene sulfonic acid, fibrosis, doxycycline, transcription
Introduction
In recent years, evidence has accumulated indicating that naturally occurring regulatory cells producing TGF-β and/or IL-10 can prevent or even reverse Th1 cell–mediated inflammation (1–3). To take advantage of this finding for the treatment of Th1-mediated mucosal inflammation, we previously developed a method of creating “genetically engineered” regulatory cells in vivo by direct introduction of DNA encoding a regulatory cytokine, TGF-β1(4). In this method the TGF-β1–encoding DNA (in the form of a plasmid) is instilled into the nose and is either taken up by migrating cells in the nasal mucosa or by cells at distant sites exposed to plasmid that gains access to the circulation. In either case, cells (both T cells and macrophages) producing TGF-β1 can subsequently be found in the gastrointestinal tract, where they either prevent colitis caused by intrarectal administration of trinitrobenzene sulfonic acid (TNBS), or treat such colitis after it is established (5, 6). One unexpected finding arising from this method of inducing TGF-β1–producing cells is that at sites of inflammation, T cells producing large amounts of IL-10 are also found, and both cytokines participate in the regulatory effect. This observation is consonant with previous findings showing that TGF-β1 and IL-10 secretion tends to occur together at site of inflammation (7–9). In this study, we sought to determine the molecular and cellular basis of this association and to examine its clinical consequences.
For this purpose, we developed a one gene/integrated doxycycline (Dox)-regulatable plasmid (10) that allows for the rapid up-regulation and down-regulation of TGF-β1 by in vivo Dox administration. We observed that cosecretion of IL-10 induced by plasmid is limited to T cells and macrophages and that transduced CD4+ T cells, reminiscent of naturally occurring suppressor T cells, produce large amounts of IL-10 as a result of TGF-β1–induced Smad4-mediated transcriptional activation of the IL-10 promoter. Further, we found that TGF-β1 plasmid administration somewhat paradoxically reverses bleomycin-induced pulmonary fibrosis in wild-type mice and such reversal is IL-10 dependent because it does not occur in IL-10–deficient mice in whom the plasmid does not induce IL-10. This suggests that the association of TGF-β1 and IL-10 secretion has advantages not only in relation to immunologic suppression, but also in relation to the ability of TGF-β1 to mediate fibrosis (11).
Materials and Methods
Mice.
Specific pathogen-free, 5–7-wk-old male SJL/J mice and C57BL/6 mice were obtained from the National Cancer Institute animal facility. IL-10–deficient mice were from Taconic.
Construction of pTet-On-TGF-β1.
Porcine-active TGF-β1 cDNA (12) was subcloned into pSuperlinker 1180 (Amersham Biosciences) and then inserted into pRetro-On (CLONTECH Laboratories, Inc.). rtTA-TGF-β1 cDNA mini–CMV-TRE fragment was then inserted into the XhoI site of pCI (Promega) that had two SV40 poly(A) in opposite directions (see Fig. 1 a).
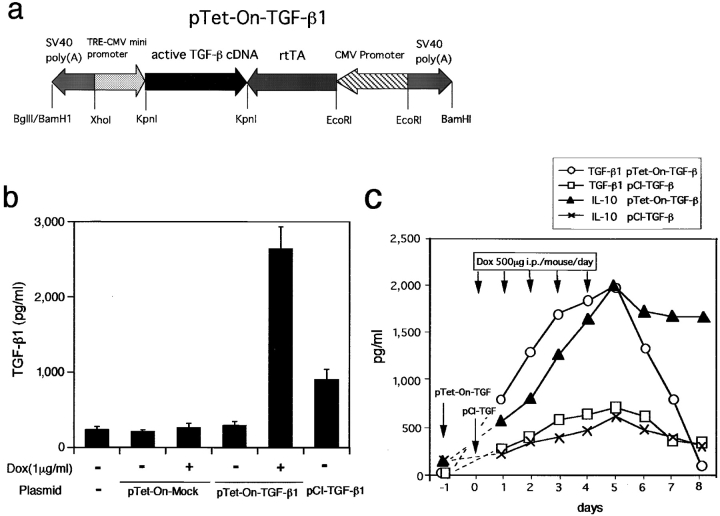
Figure 1.
Active TGF-β expression in vitro and in vivo by pTet-On-TGF-β1. (a) Schematic map of the pTet-On-TGF-β1 construct. TRE, Tet-responsive element; rtTA, reverse tetracycline-controlled transactivator. (b) In vitro production of active TGF-β1 by Cos 7 cells transfected with pTet-On-TGF-β1 exhibited background TGF-β1 production in the absence of Dox and induced much greater amount of TGF-β1 than pCI-TGF-β1. (c) In vivo expression of active TGF-β1 and IL-10 in SJL/J mouse spleen cells after intranasal administration of pTet-On-TGF-β1 plasmid. Spleen cells from mice (n = 3) killed on the indicated days were cultured with anti-CD3/anti-CD28 in the absence of Dox and culture supernatants were assayed for active TGF-β1 and IL-10 by ELISA. Because Dox was not added to the splenocyte cultures, TGF-β1/IL-10 production measured reflect the capacity of cells to produce these cytokines in vivo. TGF-β1 and IL-10 production was rapidly induced by Dox in mice administered pTet-On-TGF-β. In addition, TGF-β1 but not IL-10 production rapidly declined after cessation of Dox.
Intranasal Administration of Plasmid DNA and Induction of TGF-β1.
We administered pTet-On-TGF-β1 intranasally (100 μg plasmid in 20 μl PBS/mouse). Starting the next day, Dox was administered for 5 d (500 μg in PBS, i.p./day/mouse).
Induction of TNBS Colitis and Culture of Lamina Propria (LP) Mononuclear Cells.
We administered 2.5 mg TNBS (Sigma-Aldrich) dissolved in 45–50% ethanol per rectum (4–7). After mice were killed, we isolated LP mononuclear cells from colon (13) and cultured them in 24-well plates (106 cells/ml; Costar) with the stimulation of coated anti-CD3ɛ and soluble anti-CD28 (BD Biosciences) to assess IFN-γ and IL-10, and with the stimulation of IFN-γ and SAC (Calbiochem) to assess IL-12 production. Cytokine productions in the supernatants were determined by ELISA kits (Endogen; references 4 and 7). Culture in serum-free medium supplemented with 1% nutridoma-SP (Roche Molecular Biochemicals) was performed for TGF-β1 ELISA without acid treatment (Max TGF-β1 assay kit; Promega).
Bleomycin Treatment.
C57BL/6J mice were anesthetized by i.p. injection of ketamine-HCl and xylazine-HCl. We induced pulmonary fibrosis by intratracheal instillation of 0.15 U bleomycin hydrochloride (Calbiochem) in 50 μl PBS using a 25-gauge bulb-end needle.
Histological Examination.
The left lung of each mouse was first perfused in situ, inflated, and then fixed with 10% buffered formalin. Paraffin-embedded sections were stained by the Masson's trichrome method.
Collagen Assay.
We harvested right lungs on days 14–21 after bleomycin treatment and homogenized them in 10 mg tissue/10 ml 0.5 M acetic acid containing 1 mg pepsin and incubated them for 24 h at 4°C with stirring. We determined lung collagen content by assaying total soluble collagen using the Sircol Collagen Assay kit (Biocolor; references 14 and 15). Sircol dye reagent is known to bind specifically to hydroxy proline, i.e., [Gly-X-Y]n helical structures of Types I–V collagens. Acid soluble Type I collagen supplied with kit was used to generate a standard curve.
TGF-β1 Retroviral Transfection of Primary T Cells.
We inserted active TGF-β1 cDNA into pBMN-IRES–green fluorescent protein (GFP; provided by G. Nolan, Stanford University, Stanford, CA) and then transfected it into Phoenix-eco (American Type Culture Collection) to collect retroviral supernatants. We stimulated SJL/J spleen CD4+ T cells purified by CD4+ T cell–enriched columns (R&D Systems) with anti-CD3ɛ/anti-CD28 under the Th1 (rIL-12 and anti–IL-4 mAb) or Th2 (rIL-4 and anti–IL-12 mAb) conditions (15), or OVA-specific T cell lines with 100 μg/ml OVA and APC. After 24 h stimulation, we added retroviral supernatant in the presence of polybrene and IL-2, and spun it at 1,000 g for 90 min, followed by overnight incubation at 32°C, and then resumed culture at 37°C (16). Every 12 d, Th1- and Th2-polarizing cells were restimulated. In some experiments, 2 ng/ml rTGF-β1 (R&D Systems) was added every 3 d. We also transfected nonviral TGF-β1 plasmid into various cell lines using LipofectAMINE2000 (Invitrogen) or the electroporation method.
Intracellular Cytokine Staining.
On day 7 after stimulation of αCD3/CD28, CD4+ T cells were stimulated with 50 ng/ml PMA and 0.5 mM ionomycin for 6 h with monensin, and then washed and fixed with 4% formaldehyde, and processed for cytokine staining with PE–anti–IL-10 and/or APC–anti–IFN-γ mAb (BD Biosciences).
Preparation of Nuclear Protein Extracts and Electrophoretic Mobility Shift Assays (EMSAs).
Jurkat cells stimulated with 5 ng/ml TGF-β1 for 1 h were lysed in ice-cold hypotonic buffer (10 mM Hepes, pH 7.9, 1.5 mM MgCl2, 10 mM KCl, 0.1 mM EDTA, pH 8.0, 0.1 mM EGTA, 1 mM DTT, 0.6% Nonidet P-40, proteinase inhibitor cocktail, sodium vanadate, and sodium fluoride). The lysates were centrifuged to obtain nuclei pellets that were then extracted with high salt nuclear extraction buffer (20 mM Hepes-KOH, pH 7.9, 1.2 mM MgCl2, 420 mM NaCl, 25% glycerol, 0.5 mM DTT, proteinase inhibitors, sodium vanadate, and sodium fluoride) as described. Binding reactions containing 10 μg nuclear extracts and 2 ng end-labeled oligonucleotides were performed for 20 min at room temperature in 15 μl binding buffer (20 mM Hepes, pH 7.9, 30 mM KCl, 4 mM MgCl 2, 0.1 mM EDTA, 0.8 mM NaPi, 20% glycerol, 4 mM spermidine, and 3 mg poly dI–dC; references 17 and 18). The probe sequences used for EMSA are: Smad-binding element (SBE) variant in IL-10 promoter, 5′-GGGAAGGTCCAGACATAATC-3′; specific competitor of SBE variant, 5′-CAGGGTGTCCAGACGGCCAC-3′; nonspecific competitor of SBE variant, 5′-GGGAAGTTTTAGACATAATC-3′; wild-type SBE sequence, 5′-CAGGGTGTCTAGACGGCCAC-3′; and specific competitor of wild-type SBE, 5′-AGAATCGTCTAGACATATCT-3′. Antibody supershift assay using anti-Smad4 (Santa Cruz Biotechnology, Inc.) was performed as previously described (18). Protein–DNA complexes were resolved in 4% polyacrylamide gels in 0.5X TBE.
Preparation of Self-inactivated Retrovector for IL-10 Promoter Luciferase Assay in Primary T Cells.
A 1.37 kb murine IL-10 promoter region was prepared by PCR using 5′Xho primer (265–290) 5′-GCAGTTCTCGAGTCAATTCCATTC and NcoI primer (1637–1614, GenBank M84340) 5′-AGCCAGCCATGGTGGAGCTCTCTT and ligated into pGL3-Basic vector (Promega). pBMN-IRES-EGFP was self-inactivated by converting the “TATA box” (AATAAA) in the 3′-LTR to the EcoRI GAATTC sequence (19) using a site-directed mutagenesis kit (Stratagene) with oligo 5′-CCCCGAGCTCGAATTCAGAGCCCAC-3′. IRES-EGFP fragment is replaced with two fragments: IL-10 promoter luciferase-DSE-U′–deleted SV40 polyA, which enables both polyadenylation and read through transcripts, and CMV promoter EGFP. Smad-binding sequence (726–733 in M84340) is mutated with the mutant SBE variant primer 5′-GTCCCTACTGAAGGGAAGTTTTAGACATAATCAAAGGACTACC-3′. Primary CD4 cells under Th1 or Th2 developing conditions were retrovirally infected and harvested on day 6. Cell lysates were analyzed for luciferase assays (Promega). All luciferase activities were normalized by the percentage of GFP expression by the flow cytometric analysis.
Results
Regulation of pTet-On-TGF-β1 In Vitro.
As shown in Fig. 1 a, the regulatable “Tet-on” plasmid (termed pTet-On-TGF-β1) consisted of two expression units: a TGF-β1 cDNA that contains a mutation that results in production of “active” TGF-β1 (TGF-β1 not bound to latency-associated protein) under a mini-CMV promoter (12) and a CMV promoter-driven Tet-On transactivator (rtTA-VP16) that binds a Tet-responsive element after interaction with Dox (20, 21).
In initial studies, we transfected pTet-On-TGF-β1 into Cos 7 cells and showed that there was no expression of TGF-β1 in the absence of Dox. This is probably due to the fact that the two expression units are arrayed in the plasmid in opposite orientation so as to reciprocally block background transcription (22). In addition, as shown in Fig. 1 b, we observed that the transduced cells produce large amounts of TGF-β1 (2,600 pg/ml) in the presence of Dox, whereas cells transduced with a conventional unregulatable TGF-β1 expression plasmid (pCI-TGF-β1) secreted only moderate amounts of TGF-β1 (890 pg/ml).
Regulation of pTet-On-TGF-β1 In Vivo and Its Relation to IL-10 Secretion.
In the next series of studies, we examined the in vivo expression and regulatability of TGF-β1 derived from pTet-On-TGF-β1 and its relation to IL-10 secretion. As shown in Fig. 1 c, we showed that after intranasal pTet-On-TGF-β1 administration accompanied by Dox coadministration, there was the rapid appearance of spleen cells secreting high amounts of TGF-β1 and the rapid disappearance of these cells after cessation of Dox administration. Perhaps more remarkably, we observed that the emergence of these TGF-β1–secreting cells was accompanied by the appearance of IL-10–producing cells, which then persisted after TGF-β1 secretion declined. These results clearly show that TGF-β1 secretion rapidly induces IL-10 secretion in vivo and that once such secretion is turned on it is not rapidly down-regulated as is the TGF-β1 secretion (which is under the control of a doxy-regulated promoter).
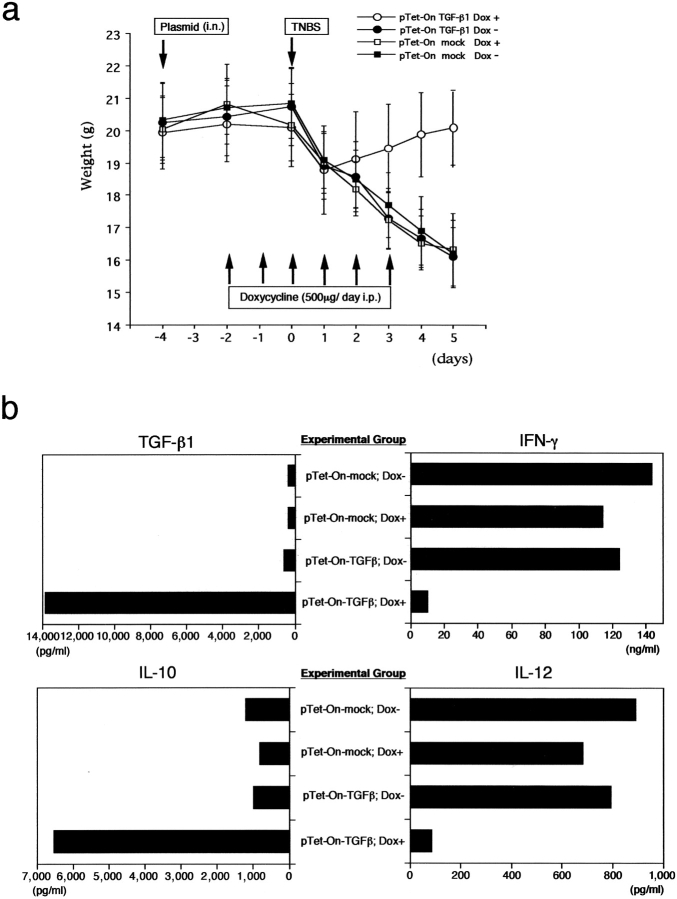
In a further study we investigated the ability of the Tet-On-TGF-β1 plasmid to affect an inflammatory state, exemplified by the Th1-type colitis induced by TNBS (4–7). Four groups of mice were studied: those receiving pTet-On-TGF-β1 with or without Dox and those receiving control plasmid (pTet-On-mock) also with or without Dox. As shown in Fig. 2 a, using body weight as an indicator of colitis, it was clear that the group that received pTet-On-TGF-β1 (i.n.) and Dox (i.p.) was protected from developing colitis, whereas the group receiving the plasmid in the absence of Dox (or those mice receiving pTet-ON-mock again with and without Dox) developed colitis. In addition, although LP cells from all three groups developing colitis produced large amounts of IL-12 and IFN-γ and small amounts of TGF-β1, LP cells from mice prevented from developing colitis produced small amounts of IL-12 and IFN-γ and very large amounts of TGF-β1 (Fig. 2 b). Of interest, the latter was much greater than that produced by cells taken from mice without inflammation, reflecting the activation of the CMV promoter in an inflammatory milieu. In addition, LP cells from this group, but not those from the groups in which the plasmid was not accompanied by Dox administration, produced large amounts of IL-10. Thus, it was obvious that such IL-10 secretion was due to plasmid-induced TGF-β1 and not simply to the presence of a Th1 inflammation. In further studies not shown, we found that intranasal administration of pTet-On-TGF-β1 also reversed TNBS colitis after inflammation was established, but only in the presence of concomitant Dox administration.
Figure 2.
Effect of intranasal pTet-On-TGF-β1 administration on TNBS-induced colitis. (a) Weight changes of mice groups administered intrarectal TNBS and intranasal pTet-On-TGF-β or pTet-On-mock (control plasmid) with or without Dox (i.p.) Each group, n = 10. (b) LP cells from mice 5 d after TNBS colitis induction were stimulated and cultured for ELISA assays of TGF-β1, IFN-γ, IL-10, and IL-12. As shown, LP cells from mice administered Dox plus pTet-On-TGF-β1 produced large amounts of TGF-β1 and IL-10 and exhibited suppressed IL-12 and IFN-γ production. Data shown is representative of three independent experiments.
Cell Types Producing IL-10 in Response to TGF-β1.
Next, we defined the cell types capable of producing IL-10 in response to exposure to TGF-β1. Here we first transfected various murine cell lines with pCI-TGF-β1 under optimal conditions or, in the case of CD4+ T cells that exhibit low transfection efficiency, we infected the cells with a retrovirus encoding TGF-β1 (see below). We then determined IL-10 production in the modified cells. As shown in Table I, a Th1 CD4+ cell line (OVA-3), i.e., a T cell line maintained by repeated OVA plus APC stimulation for >6 wk, and two macrophage cell lines (RAW264 and MH-S) secreted substantial amounts of IL-10 after transfection (or infection). In contrast, a thymus-derived T cell (EL-4) as well as epithelial, squamous, and fibroblast cell lines from lung and other tissues did not produce IL-10 after transfection (although they did produce TGF-β1). These studies indicate that only certain types of hematopoietic cells are capable of IL-10 secretion as a result of exposure to TGF-β1.
Table I.
Induction of IL-10 in T Cells and Macrophages by TGF-β1–expressing Constructs
| TGF-β 1 (pg/ml)b
|
IL-10 (pg/ml)
|
||||
|---|---|---|---|---|---|
| Cell linea | Plasmid/retrovirus | mock | TGF-β | mock | TGF-β |
| T cell | |||||
| OVA-3 T cell clone | regional LN | <30 | 327 | <25 | 1,620 |
| EL-4 (anti-CD3/anti-CD28) | thymus | 184 | 353 | <25 | <25 |
| Macrophage | |||||
| RAW264 (LPS 0.5 μg) | Mθ | 214 | 924 | 181 | 930 |
| MH-S (LPS 0.5 μg) | alveolar Mθ | 119 | 636 | <25 | 161 |
| Epithelial | |||||
| CMT93 | colon epithelial | 440 | 1,270 | <25 | <25 |
| C10 | lung epithelial | <30 | 468 | 44 | <25 |
| E10 | lung epithelial | <30 | 1,028 | <25 | <25 |
| LA-4 | lung epithelial Ca | <30 | 128 | <25 | <25 |
| KLN205 | lung squamous | 88 | 552 | 48 | <25 |
| Fibroblast | |||||
| MLg | lung fibroblast | <30 | 268 | <25 | <25 |
| 3T3 | embryo fibroblast | 128 | 1,430 | <25 | <25 |
The value obtained for each cell line is the mean value from three independent experiments.
Mouse cell lines were transfected with pCI-TGF-β1 plasmid using TransfectAMINE 2000 or by electroporation (EL-4). The OVA-3 T cell clone was infected with a retrovirus of pBMN-TGF-β1-GFP.
TGF-β1 ELISA was performed after acid treatment.
IL-10 Production by Polarized Th1 Cell Populations in Response to Both Endogenous and Exogenous TGF-β1.
Next, we addressed the question of whether the production of IL-10 in a Th1 milieu could arise from the Th1 cells themselves. To this end, we transduced naive CD4+ T cells stimulated with anti-CD3/anti-CD28 with a bicistronic retroviral vector expressing both TGF-β and GFP (termed pBMN-TGF-β1 or retro-TGF-β1) under Th1 priming conditions (IL-12 and anti–IL-4) or Th2 priming conditions (IL-4 and anti–IL-12; reference 16). This allowed us to distinguish infected cells (GFP+, TGF-β1–producing cells) from uninfected cells (GFP−, TGF-β1–nonproducing cells). As shown in Fig. 3 a, although developing CD4+ Th1 cells infected with control retrovirus (pBMN-mock or retro-mock, i.e., retrovirus encoding only GFP) did not produce IL-10, similar cells infected with retro-TGF-β1 (retrovirus encoding both TGF-β1 and GFP) produced IL-10 whether or not they were GFP+. On the other hand, as shown in Fig. 3 b, developing Th2 cells exhibited IL-10 production when infected with either retrovirus regardless of GFP positivity. These studies show quite clearly that Th1 cells produce IL-10 either when they produce TGF-β1 themselves or are exposed to TGF-β1 produced by other cells.
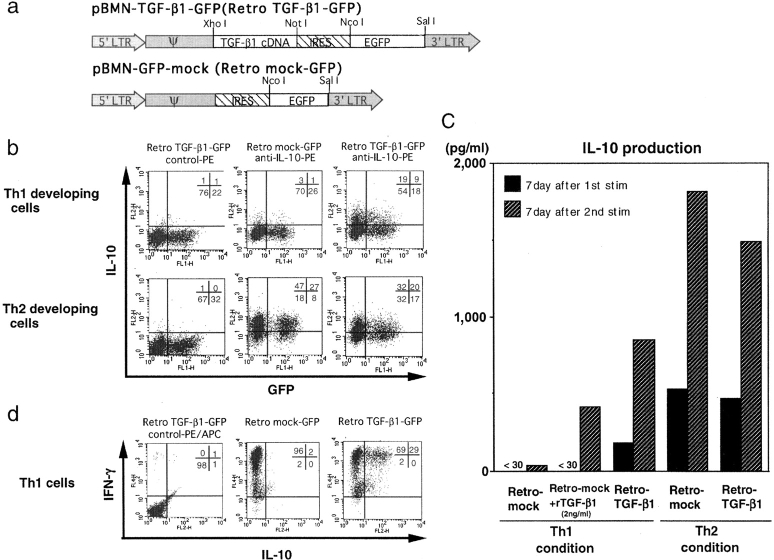
Figure 3.
Production of IL-10 by Th1 cells infected with a TGF-β1–expressing retrovirus. (a) Schematic map of the retroviruses used. (b) Intracellular IL-10 staining of developing Th1 and Th2 cells on day 6 after stimulation with αCD3/CD28 with retroviral infection by retro-TGF-β1-GFP or retro-mock-GFP. IL-10 is produced by both GFP− and GFP+ Th1 developing cells. Th2 cells produce IL-10 in the absence of retro-TGF-β1-GFP infection. (c) Secretion of IL-10 by CD4+ T cells infected with retro-TGF-β1-GFP or retro-mock-GFP under Th1 or Th2 priming conditions. IL-10 production by cells infected with retro-mock-GFP under Th1 condition with the addition of rTGF-β1 was also studied. Retro-TGF-β1–infected Th1 and Th2 cells produced more amounts of IL-10 after the second stimulation, however, although Th2 cells produce IL-10 with the infection of retro-mock, Th1 cells only do so with the addition of rTGF-β1 or infection of retro-TGF-β1. (d) Intracellular staining of IL-10 and IFN-γ of Th1 cells after the third round stimulation with αCD3/CD28.
In complementary studies, we measured the secretion of IL-10 by naive cell populations infected with retro-mock or retro-TGF-β1 and then subjected them to two rounds of stimulation under either Th1 and Th2 conditions. As shown in Fig. 3 c, in this case, cells stimulated under Th1 conditions again required infection with retro-TGF-β1 to produce IL-10 and cells stimulated under Th2 conditions produced (even higher levels of) IL-10 when infected with either retro-TGF-β1 or retro-mock. In addition, IL-10 production was increased in both Th1 and Th2 cells after the second round of stimulation. Finally, we noted that Th1 cells infected with retro-mock could produce IL-10 with repeated addition of rTGF-β1 to the culture, but only after the second round of stimulation. These studies show that repeated stimulation of Th1 cells in the presence of TGF-β1 (from retro-TGF-β1 or soluble rTGF-β1) leads to Th1 cells capable of IL-10 production. In addition, they suggest that exogenous TGF-β1 is a less efficient means of inducing IL-10 than endogenous TGF-β1. Parenthetically, as shown in Fig. 3 d, repeated stimulation of Th1 cells exposed to TGF-β1 become dual producers of IFN-γ and IL-10.
The Molecular Basis of TGF-β1 Induction of IL-10.
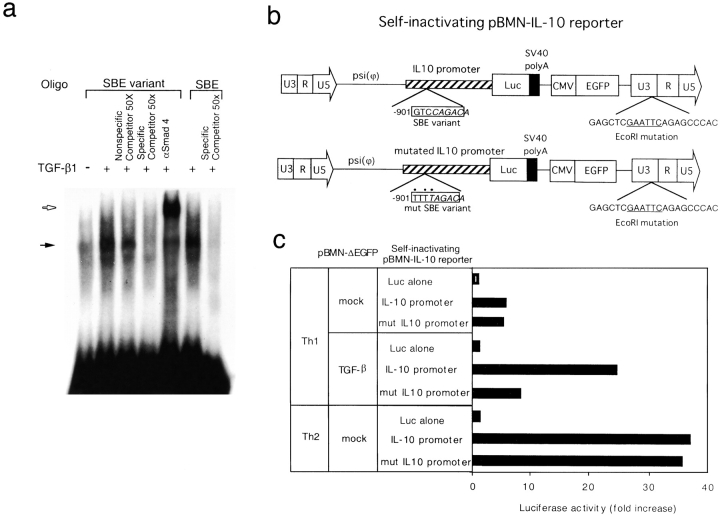
On the assumption that TGF-β1 induction of IL-10 observed above could be related to TGF-β1 signaling via Smad activation of the IL-10 promoter, we searched the murine IL-10 promoter region for an SBE (17, 18, 23, 24). Indeed, we found an “SBE variant” site GTCCAGAC at −901 that closely resembled the consensus SBE, GTCTAGAC, and contained overlapping CAGA sequences (termed a CAGA box; reference 25). In additional studies of whether this sequence actually binds to Smad proteins, we performed an EMSA using nuclear extracts of TGF-β1–stimulated Jurkat T cells and radiolabeled oligo with the SBE variant sequence. As shown in Fig. 4 a, we found that the nuclear extracts contained proteins that bound to the variant sequence and that such binding was blocked by an unlabeled competitor sequence, but not by a mutated variant sequence. Furthermore, we showed that the addition of anti-Smad4 to the mixture containing the extract plus variant sequence causes a supershift. Thus, activated Smad4 does in fact bind to an SBE variant sequence in the IL-10 promoter.
Figure 4.
TGF-β1 activates IL-10 promoter transcription through Smad4 in Th1 cells. (a) EMSA shows that TGF-β1–induced nuclear extracts exhibited binding activity to an SBE variant oligo as well as native SBE oligo. Anti-Smad4 antibody causes supershift of the complex with the SBE variant. (b) Schematic map of self-inactivating pBMN-IL-10 luciferase reporter genes. (c) Luciferase activity of IL-10 promoter was assayed by infection with self-inactivating retroviruses. Retrovirally expressed TGF-β1 induces IL-10 promoter activity in developing Th1 cells signaling through SBE variant sequence, but TGF-β1 is not required for activation of IL-10 promoter in developing Th2 cells.
To assess whether the IL-10 promoter not only binds Smad but also responds to Smad signaling, we constructed self-inactivating retroviral reporter vectors that express luciferase under the control of the IL-10 promoter rather than the retroviral promoter (19, 26). These included a vector containing an IL-10 promoter with a mutated SBE variant. The retroviruses also expressed GFP, which allowed assessment of infection efficiency of the retrovirus and normalization. We then coinfected polarized Th1 and Th2 cells with these retroviruses as well as with retroviruses expressing either pBMN-TGF-β1 or pBMN-mock (in which the GFP cassette has been deleted) and monitored TGF-β1 production by the coinfected cells by ELISA. As shown in Fig. 4 b, in Th1 cells, the wild-type IL-10 promoter gene generated a strong luciferase signal in cells expressing TGF-β1, whereas only a basal luciferase signal was seen in cells with a mutated promoter. In contrast, in Th2 cells both the wild-type and mutated promoters were activated even in the absence of TGF-β1, indicating that IL-10 production is independent of TGF-β1-Smad signaling and the transcriptional activation of IL-10 in Th2 cells does not depend on the SBE variant sequence. These data provide strong support for the view that TGF-β1 induces IL-10 via transcriptional activation of the IL-10 promoter by activated Smad protein(s).
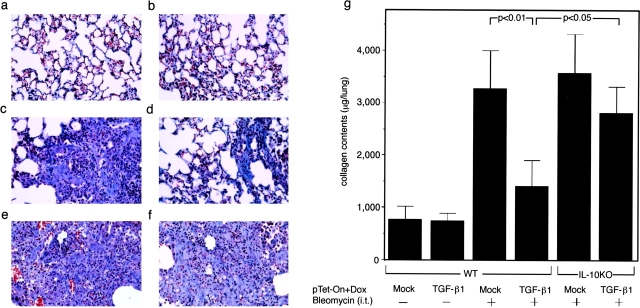
IL-10 Induced by Intranasal pTet-On-TGF-β1 Ameliorates Bleomycin-induced Lung Fibrosis.
The above evidence that TGF-β1 production by T cells is associated with IL-10 induction whereas such production in other non–T cells is not, implied that the IL-10 production has effects on TGF-β function during lymphoid cell interactions. We investigated this possibility in relation to the induction of fibrosis, a notorious side effect of TGF-β1 secretion (27–29). In particular, we examined the effect of intranasal administration of pTet-On-TGF-β1 on bleomycin-induced fibrosis in the lung, as quantified by Masson trichrome staining and by collagen content. In control studies shown in Fig. 5 , a and b, we established that intranasal administration of either pTet-mock or pTet-On-TGF-β1 did not induce fibrotic changes. Then, as shown in Fig. 5, c and d, we established that although bleomycin induced severe fibrosis when accompanied by the administration of pTet-mock, such fibrosis was significantly decreased when accompanied by the administration of pTet-On-TGF-β1 plus Dox. Thus, rather than itself inducing fibrosis, pTet-On-TGF-β1 inhibited fibrosis induced by bleomycin. Finally, as shown in Fig. 5, e and f, the same study performed in IL-10–deficient mice showed that in the absence of IL-10 induction, the protective effect of the pTet-On-TGF-β1 plasmid was lost and in this case bleomycin did induce fibrosis in mice administered pTet-On TGF-β1 plus Dox. As shown in Fig. 5 g, confirmation of this result was obtained by measurement of the collagen content of the lungs studied under the various conditions outlined above. This provides strong evidence that the ability of pTet-On-TGF-β1 to inhibit bleomycin-induced fibrosis is in fact due to its ability to induce IL-10.
Figure 5.
Amelioration of bleomycin-induced lung fibrosis by intranasal administration of pTet-On-TGF-β1. (a–f) Masson's trichrome stain of lung sections from bleomycin-treated and control mice including B6 wild-type (a–d) and IL-10 KO (e and f). pTet-On-mock and Dox-treated mouse lungs (a, c, and e) and pTet-On-TGF-β1 and Dox-treated mouse lungs (b, d, and f) without (a and b) or with bleomycin induction (c–f). Representative pictures are shown. ×400. (g) Collagen content (n = 9 in each group) in the bleomycin-induced fibrotic lungs evaluated by Sircol dye assay. Administration of pTet-On-TGF-β effectively reduces fibrotic changes in both assays.
Discussion
In these studies, using a regulatable TGF-β1–expressing plasmid (termed pTet-On-TGF-β1), we show that in vivo TGF-β1 secretion rapidly induces IL-10 secretion and that such induction occurs in Th1 cells via Smad4 binding to and activation of the IL-10 promoter. The close association of these two major “regulatory” cytokines thus revealed mirrors their association during suppressor function occurring in association with Th1-mediated inflammation (30). Powrie et al. (31) for instance, has shown that in the SCID-transfer model of colitis, the regulatory effect of the subpopulation of cells in the memory CD45RBlow cells is abrogated by administration of anti–TGF-β1 or anti–IL-10R and that such cells either produce or induce TGF-β1 and/or IL-10 (8, 9). In addition, we have shown that the regulation of TNBS colitis by feeding TNP-substituted proteins requires both TGF-β1 and IL-10 (7). Finally, we and others have also shown that both “self–MHC-reactive” and CD4+ CD25+ regulatory T cells produce both TGF-β1 and IL-10 upon appropriate stimulation (32–34).
The fact that TGF-β induces IL-10 as shown here whereas IL-10 does not induce TGF-β1 strongly suggests that IL-10 facilitates TGF-β1 regulatory function and not the other way around (4, 7). One way such facilitation could occur is through IL-10 enhancement of TGF-β1 signaling. This possibility is supported by Cottrez and Groux (35) who showed that IL-10 maintains TGF-β1RII expression on activated cells that would otherwise down-regulate this receptor. In addition, it is known that Th1 cytokines such as IFN-γ and TNF-α up-regulate Smad7, a cytosolic intermediate that inhibits TGF-β1 signaling via other Smads (36, 37) and it is thus possible (but not yet proven) that IL-10 inhibits such Smad7 up-regulation.
Another way that IL-10 could facilitate TGF-β1 regulatory activity is via an ability to sustain TGF-β1 secretion or allow the expansion of TGF-β1–producing cells. Support for this possibility comes from our recent observation that TGF-β1–mediated regulatory function induced by feeding antigen is not only abrogated by anti–TGF-β1 administration, but also by anti–IL-10 administration and that in fact no TGF-β1 production occurs in such fed mice given anti–IL-10 (7). Further work showed that the effect of anti–IL-10 does not occur during the induction of TGF-β1–producing cells (in the absence of Th1 cytokines), but rather during the expansion of these cells (in the presence of Th1 cytokines) when they might be expected to undergo antigen-induced proliferation. These findings suggest that either nascent TGF-β1–producing regulatory cells undergo a turn-off of TGF-β1 production or fail to expand in the face of Th1 cytokine production. Thus, it is reasonable to suggest that IL-10 sustains TGF-β1 secretion directly by counteracting the negative effect of Th1 cytokines on TGF-β1 production or indirectly by down-regulating Th1 cytokine secretion. Both of these possibilities would explain the observation that mice expressing large amount of IL-10 in epithelial cells as a result of an epithelial cell–specific IL-10 transgene exhibit an increase in TGF-β1 expression in the underlying LP (38). In addition, it accords with the observation that T cell TGF-β1 secretion is not seen during the Th1 response observed when TNBS colitis is induced in SJL/J mice but is seen during the Th2 response observed in the oxazolone colitis occurring in the same strain (39). Taken together, these considerations strongly suggest that TGF-β1 induction of IL-10 fulfills an important requirement of regulatory T cell activity.
Although TGF-β1 and IL-10 as discussed above might be interdependent during a regulatory response, it is possible that their cosecretion also occurs because these cytokines regulate different aspects of an inflammatory response and are thus synergistic in their activity. This is supported by the fact that in Th1-driven inflammation, although TGF-β1 regulates Th1 cells via its ability to down-regulate T-bet and the IL-12Rβ2 chain (4, 40), IL-10 regulates via down-regulation of IL-12 and TNF-α secretion (4, 41, 42). Thus, the regulatory activity of TGF-β1 and IL-10 acting together is greater than either of these cytokines acting alone.
An important and interesting aspect of TGF-β1 induction of IL-10 relates to our observation that such induction affects Th1 cells rather than Th2 cells (which exhibit IL-10 secretion in the absence of TGF-β1 and which are not induced to produce additional IL-10 by the presence of TGF-β). In a previous study by Blokzijl et al. (43) using the HT-2 cell line (a cell line that produces IL-10 but not IL-4 or IL-5), it was found that TGF-β1–induced Smad3 interacts directly with GATA-3 and the complex formed acts cooperatively to up-regulate IL-10 expression (by ∼1.8-fold) in a Smad3- and GATA-3–dependent fashion. This result is somewhat at odds with our data showing that IL-10 production by freshly prepared Th2 cells is not enhanced by TGF-β1 and is best explained by differences in the cells being studied. Blokzijl et al. (43) used an established cell line of uncertain lineage, whereas we used a freshly stimulated Th2 cell line. Finally, we observed that CD4+ T cells exposed to TGF-β1 during induction of T cell differentiation produced much lower amounts of IL-10 when stimulated under neutral priming conditions than under Th1 priming conditions (unpublished data). This indicates that activation of the IL-10 promoter is not solely dependent on TGF-β1, but also involves other unknown factors induced during the differentiation of Th1 cells.
In addition to its role as a suppressor of inflammation, TGF-β1 has a known capacity to induce collagen and fibronectin synthesis and thus to promote fibrosis. In contrast, IL-10 has been shown to inhibit collagen synthesis and prevent fibrosis (44, 45), not only that caused by TGF-β1, but also by TNF-α (46, 47) and IL-13 (14). On this basis we explored the possibility that the fibrogenic properties of TGF-β1 can be brought under control by IL-10 cosecretion. In these studies we showed that intranasal administration of pTet-On-TGF-β1 did not induce fibrosis of the lung, the organ most exposed to TGF-β1 as a result of intranasal plasmid administration. In contrast, such administration prevented bleomycin-induced pulmonary fibrosis, a fibrosis that is at least in part mediated by endogenous TGF-β production (27, 48). That this seemingly paradoxical effect was due to the cosecretion of IL-10 was shown by the fact that TGF-β1 plasmid administration did not prevent bleomycin-induced fibrosis in IL-10–deficient mice (in whom IL-10 cosecretion cannot occur). These findings strongly suggest that the IL-10 antifibrotic effect is dominant over the TGF-β1 profibrotic effect, even in the face of endogenous (nonlymphoid origin) TGF-β production and that IL-10 protects the animal from TGF-β1–mediated fibrosis. By extension, they suggest that induction of TGF-β1–secreting cells by administration of a plasmid such as pTet-On-TGF-β1 that leads to superphysiologic IL-10 secretion may have an unexpected antifibrotic effect that bodes well for its use as a therapy for autoimmune diseases.
Acknowledgments
We thank Sara Kaul for preparing this manuscript. We also thank Drs. Zu-Xi, Yu, and Ryuta Nishikomori for valuable advice.
Abbreviations used in this paper: Dox, doxycycline; EMSA, electrophoretic mobility shift assay; GFP, green fluorescent protein; LP, lamina propria; SBE, Smad-binding element; TNBS, trinitrobenzene sulfonic acid.
References
- 1.Chen, Y., V.K. Kuchroo, J. Inobe, D.A. Hafler, and H.L. Weiner. 1994. Regulatory T cell clones induced by oral tolerance: suppression of autoimmune encephalomyelitis. Science. 265:1237–1240. [DOI] [PubMed] [Google Scholar]
- 2.Groux, H., A. O'Garra, M. Bigler, M. Rouleau, S. Antonenko, J.E. de Vries, and M.G. Roncarolo. 1997. A CD4+ T-cell subset inhibits antigen-specific T-cell responses and prevents colitis. Nature. 389:737–742. [DOI] [PubMed] [Google Scholar]
- 3.Zuany-Amorim, C., E. Sawicka, C. Manlius, A. Le Moine, L.R. Brunet, D.M. Kemeny, G. Bowen, G. Rook, and C. Walker. 2002. Suppression of airway eosinophilia by killed Mycobacterium vaccae-induced allergen-specific regulatory T-cells. Nat. Med. 8:625–629. [DOI] [PubMed] [Google Scholar]
- 4.Kitani, A., I. Fuss, K. Nakamura, O.M. Schwartz, T. Usui, and W. Strober. 2000. Treatment of experimental (trinitrobenzene sulfonic acid) colitis by intranasal administration of transforming growth factor (TGF)β1 plasmid: TGF-β1–mediated suppression of T helper cell type 1 response occurs by interleukin (IL)-10 induction and IL-12 receptor β2 chain downregulation. J. Exp. Med. 192:41–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neurath, M.F., I. Fuss, B.L. Kelsall, D.H. Presky, W. Waegell, and W. Strober. 1996. Experimental granulomatous colitis in mice is abrogated by induction of TGF-beta–mediated oral tolerance. J. Exp. Med. 183:2605–2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neurath, M.F., S. Pettersson, K.H. Meyer zum Buschenfelde, and W. Strober. 1996. Local administration of antisense phosphorothioate oligonucleotides to the p65 subunit of NF-kappa B abrogates established experimental colitis in mice. Nat. Med. 2:998–1004. [DOI] [PubMed] [Google Scholar]
- 7.Fuss, I.J., M. Boirivant, B. Lacy, and W. Strober. 2002. The interrelated roles of TGF-beta and IL-10 in the regulation of experimental colitis. J. Immunol. 168:900–908. [DOI] [PubMed] [Google Scholar]
- 8.Asseman, C., S. Mauze, M.W. Leach, R.L. Coffman, and F. Powrie. 1999. An essential role for interleukin 10 in the function of regulatory T cells that inhibit intestinal inflammation. J. Exp. Med. 190:995–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maloy, K.J., L. Salaun, R. Cahill, G. Dougan, N.J. Saunders, and F. Powrie. 2003. CD4+ CD25+ T(R) cells suppress innate immune pathology through cytokine-dependent mechanisms. J. Exp. Med. 197:111–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gould, D.J., M. Berenstein, H. Dreja, F. Ledda, O.L. Podhajcer, and Y. Chernajovsky. 2000. A novel doxycycline inducible autoregulatory plasmid which displays “on”/“off” regulation suited to gene therapy applications. Gene Ther. 7:2061–2070. [DOI] [PubMed] [Google Scholar]
- 11.Letterio, J.J., and A.B. Roberts. Regulation of immune responses by TGF-beta. 1998. Annu Rev. Immunol. 16:137–161. [DOI] [PubMed] [Google Scholar]
- 12.Samuel, S.K., R.A. Hurta, P. Kondaiah, N. Khalil, E.A. Turley, J.A. Wright, and A.H. Greenberg. 1992. Autocrine induction of tumor protease production and invasion by a metallothionein-regulated TGF-β1 (Ser223, 225). EMBO J. 11:1599–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van der Heijden, P.J., and W. Stok. 1987. Improved procedure for the isolation of functionally active lymphoid cells from the murine intestine. J. Immunol. Methods. 103:161–167. [DOI] [PubMed] [Google Scholar]
- 14.Lee, C.G., R.J. Homer, Z. Zhu, S. Lanone, X. Wang, V. Koteliansky, J.M. Shipley, P. Gotwals, P. Noble, Q. Chen, et al. 2001. Interleukin-13 induces tissue fibrosis by selectively stimulating and activating transforming growth factor β1. J. Exp. Med. 194:809–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tokuda, A., M. Itakura, N. Onai, H. Kimura, T. Kuriyama, and K. Matsushima. 2000. Pivotal role of CCR1-positive leukocytes in bleomycin-induced lung fibrosis in mice. J. Immunol. 164:2745–2751. [DOI] [PubMed] [Google Scholar]
- 16.Usui, T., R. Nishikomori, A. Kitani, and W. Strober. 2003. GATA-3 suppresses Th1 development by down-regulation of STAT-4, not through effects on IL-12Rβ2 chain or T bet. Immunity. 18:415–428. [DOI] [PubMed] [Google Scholar]
- 17.von Gersdorff, G., K. Susztak, F. Rezvani, M. Bitzer, D. Liang, and E.P. Bottinger. 2000. Smad3 and Smad4 mediate transcriptional activation of the human Smad7 promoter by transforming growth factor β. J. Biol. Chem. 275:11320–11326. [DOI] [PubMed] [Google Scholar]
- 18.Denissova, N.G., C. Pouponnot, J. Long, D. He, and F. Liu. 2000. Transforming growth factor β-inducible independent binding of SMAD to the Smad7 promoter. Proc. Natl. Acad. Sci. USA. 97:6397–6402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nakajima, K., K. Ikenaka, K. Nakahira, N. Morita, and K. Mikoshiba. 1993. An improved retroviral vector for assaying promoter activity. Analysis of promoter interference in pIP211 vector. FEBS Lett. 315:129–133. [DOI] [PubMed] [Google Scholar]
- 20.Gossen, M., and H. Bujard. 1992. Tight control of gene expression in mammalian cells by tetracycline-responsive promoters. Proc. Natl. Acad. Sci. USA. 89:5547–5551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gossen, M., S. Freundlieb, G. Bender, G. Muller, W. Hillen, and H. Bujard. 1995. Transcriptional activation by tetracyclines in mammalian cells. Science. 268:1766–1769. [DOI] [PubMed] [Google Scholar]
- 22.Paulus, W., I. Baur, F.M. Boyce, X.O. Breakefield, and S.A. Reeves. 1996. Self-contained, tetracycline-regulated retroviral vector system for gene delivery to mammalian cells. J. Virol. 70:62–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zawel, L. J.L. Dai, P. Buckhaults, S. Zhou, K.W. Kinzler, B. Vogelstein, and S.E. Kern. 1998. Human Smad3 and Smad4 are sequence-specific transcription activators. Mol. Cell 1:611–617. [DOI] [PubMed] [Google Scholar]
- 24.Kim, J.M., C.I. Brannan, N.G. Copeland, N.A. Jenkins, T.A. Khan, and K.W. Moore. 1992. Structure of the mouse IL-10 gene and chromosomal localization of the mouse and human genes. J. Immunol. 148:3618–3623. [PubMed] [Google Scholar]
- 25.Dennler, S., S. Itoh, D. Vivien, P. ten Dijke, S. Huet, and J.M. Gauthier. 1998. Direct binding of Smad3 and Smad4 to critical TGFβ-inducible elements in the promoter of human plasminogen activator inhibitor-type 1 gene. EMBO J. 17:3091–3100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu, S.F., T. von Ruden, P.W. Kantoff, C. Garber, M. Seiberg, U. Ruther, W.F. Anderson, E.F. Wagner, and E. Gilboa. 1986. Self-inactivating retroviral vectors designed for transfer of whole genes into mammalian cells. Proc. Natl. Acad. Sci. USA. 83:3194–3198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coker, R.K., G.J. Laurent, S. Shahzeidi, P.A. Lympany, R.M. du Bois, P.K. Jeffery, and R.J. McAnulty. 1997. Transforming growth factors-beta 1, -beta 2, and -beta 3 stimulate fibroblast procollagen production in vitro but are differentially expressed during bleomycin-induced lung fibrosis. Am. J. Pathol. 150:981–991. [PMC free article] [PubMed] [Google Scholar]
- 28.Sime, P.J., Z. Xing, F.L. Graham, K.G. Csaky, and J. Gauldie. 1997. Adenovector-mediated gene transfer of active transforming growth factor-β induces prolonged severe fibrosis in rat lung. J. Clin. Invest. 100:768–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Tol, E.A., L. Holt, F.L. Li, F.M. Kong, R. Rippe, M. Yamauchi, J. Pucilowska, P.K. Lund, and R.B. Sartor. 1999. Bacterial cell wall polymers promote intestinal fibrosis by direct stimulation of myofibroblasts. Am. J. Physiol. 277:245–255. [DOI] [PubMed] [Google Scholar]
- 30.Levings, M.K., R. Bacchetta, U. Schulz, and M.G. Roncarolo. 2002. The role of IL-10 and TGF-beta in the differentiation and effector function of T regulatory cells. Int. Arch. Allergy Immunol. 129:263–276. [DOI] [PubMed] [Google Scholar]
- 31.Powrie, F., J. Carlino, M.W. Leach, S. Mauze, and R.L. Coffman. 1996. A critical role for transforming growth factor-beta but not interleukin 4 in the suppression of T helper type 1–mediated colitis by CD45RB(low) CD4+ T cells. J. Exp. Med. 183:2669–2674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kitani, A., K. Chua, K. Nakamura, and W. Strober. 2000. Activated self-MHC-reactive T cells have the cytokine phenotype of Th3/T regulatory cell 1 T cells. J. Immunol. 165:691–702. [DOI] [PubMed] [Google Scholar]
- 33.Nakamura, K., A. Kitani, and W. Strober. 2001. Cell contact–dependent immunosuppression by CD4+ CD25+ regulatory T cells is mediated by cell surface–bound transforming growth factor beta. J. Exp. Med. 194:629–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang, X., L. Izikson, L. Liu, and H.L. Weiner. 2001. Activation of CD25(+)CD4(+) regulatory T cells by oral antigen administration. J. Immunol. 167:4245–4253. [DOI] [PubMed] [Google Scholar]
- 35.Cottrez, F., and H. Groux. 2001. Regulation of TGF-beta response during T cell activation is modulated by IL-10. J. Immunol. 167:773–778. [DOI] [PubMed] [Google Scholar]
- 36.Ulloa, L., J. Doody, and J. Massague. 1999. Inhibition of transforming growth factor-beta/SMAD signalling by the interferon-gamma/STAT pathway. Nature. 397:710–713. [DOI] [PubMed] [Google Scholar]
- 37.Bitzer, M., G. von Gersdorff, D. Liang, A. Dominguez-Rosales, A.A. Beg, M. Rojkind, and E.P. Bottinger. 2000. A mechanism of suppression of TGF-beta/SMAD signaling by NF-kappa B/RelA. Genes Dev. 14:187–197. [PMC free article] [PubMed] [Google Scholar]
- 38.Heller, F., I.J. Fuss, E.E. Nieuwenhuis, R.S. Blumberg, and W. Strober. 2002. Oxazolone colitis, a Th2 colitis model resembling ulcerative colitis, is mediated by IL-13-producing NK-T cells. Immunity. 17:629–638. [DOI] [PubMed] [Google Scholar]
- 39.De Winter, H., D. Elewaut, O. Turovskaya, M. Huflejt, C. Shimeld, A. Hagenbaugh, S. Binder, I. Takahashi, M. Kronenberg, and H. Cheroutre. 2002. Regulation of mucosal immune responses by recombinant interleukin 10 produced by intestinal epithelial cells in mice. Gastroenterology. 122:1829–1841. [DOI] [PubMed] [Google Scholar]
- 40.Gorelik, L., S. Constant, and R.A. Flavell. 2002. Mechanism of transforming growth factor beta–induced inhibition of T helper type 1 differentiation. J. Exp. Med. 195:1499–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Segal, B.M., B.K. Dwyer, and E.M. Shevach. 1998. An interleukin (IL)-10/IL-12 immunoregulatory circuit controls susceptibility to autoimmune disease. J. Exp. Med. 187:537–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fiorentino, D.F., A. Zlotnik, T.R. Mosmann, M. Howard, and A. O'Garra. 1991. IL-10 inhibits cytokine production by activated macrophages. J. Immunol. 147:3815–3822. [PubMed] [Google Scholar]
- 43.Blokzijl, A., P. ten Dijke, and C.F. Ibánez. 2002. Physical and functional interaction between GATA-3 and Smad3 allows TGF-β regulation of GATA target genes. Curr. Biol. 12:35–45. [DOI] [PubMed] [Google Scholar]
- 44.Yamamoto, T., B. Eckes, and T. Krieg. 2001. Effect of interleukin-10 on the gene expression of type I collagen, fibronectin, and decorin in human skin fibroblasts: differential regulation by transforming growth factor-beta and monocyte chemoattractant protein-1. Biochem. Biophys. Res. Commun. 281:200–205. [DOI] [PubMed] [Google Scholar]
- 45.Arai, T., K. Abe, H. Matsuoka, M. Yoshida, M. Mori, S. Goya, H. Kida, K. Nishino, T. Osaki, I. Tachibana, et al. 2000. Introduction of the interleukin-10 gene into mice inhibited bleomycin-induced lung injury in vivo. Am. J. Physiol. Lung. Cell. Mol. Physiol. 278: L914–L922. [DOI] [PubMed] [Google Scholar]
- 46.Piguet, P.F., M.A. Collart, G.E. Grau, Y. Kapanci, and P. Vassalli. 1989. Tumor necrosis factor/cachectin plays a key role in bleomycin-induced pneumopathy and fibrosis. J. Exp. Med. 170:655–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ortiz, L.A., J. Lasky, R.F. Hamilton, Jr., A. Holian, G.W. Hoyle, W. Banks, J.J. Peschon, A.R. Brody, G. Lungarella, and M. Friedman. 1998. Expression of TNF and the necessity of TNF receptors in bleomycin-induced lung injury in mice. Exp. Lung Res. 24:721–743. [DOI] [PubMed] [Google Scholar]
- 48.Zhang, K., K.C. Flanders, and S.H. Phan. 1995. Cellular localization of transforming growth factor-beta expression in bleomycin-induced pulmonary fibrosis. Am. J. Pathol. 147:352–361. [PMC free article] [PubMed] [Google Scholar]