Abstract
Repeated attempts to show that costimulation for negative selection is controlled by a single cell surface molecule have been unsuccessful. Thus, negative selection may involve multiple cell surface molecules acting in consort. In support of this idea, we show here that at least three cell surface molecules, namely CD28, CD5, and CD43, contribute to Fas-independent negative selection of the tolerance-susceptible population of heat-stable antigen (HSA)hiCD4+8− cells found in the medulla. The costimulatory function of these three molecules can be blocked by certain cytokines, IL-4 and IL-7, and coinjecting these cytokines with antigen in vivo abolishes negative selection; Fas-dependent negative selection, however, is maintained. The results suggest that efficient negative selection requires the combined functions of at least four cell surface molecules: CD28, CD5, CD43, and Fas.
Keywords: thymus, tolerance, costimulatory signals, lymphokines, medulla
Negative selection of thymocytes destroys autoreactive T cells in situ and is crucial for self-tolerance induction 1 2 3 4. Negative selection is directed to agonist self-peptides bound to MHC molecules and causes immature thymocytes with specificity for these ligands to die via apoptosis 3 4.
As TCR ligation alone is insufficient to kill thymocytes 5 6 7 8 9, the onset of apoptosis during negative selection is presumed to be under the control of costimulatory molecules 5 6 7 9. However, despite concerted efforts, the issue of which particular cell surface molecules provide costimulatory function for negative selection has yet to be resolved. Based on studies with gene knockout and mutant mice, several molecules, including CD30 10, TNFR 11, CD28−/− 12, and Fas 13 14 appear to influence the destruction of cortical thymocytes seen after injecting normal or TCR-transgenic mice with anti-TCR/CD3 mAbs or specific peptides. Whether these data are relevant to physiological negative selection, however, is questionable, because destruction of cortical thymocytes can be a reflection of stress induced by mAb- or peptide-induced activation of mature T cells in the peripheral lymphoid tissues 15 16 17. This problem does not pertain to negative selection directed to endogenous self-antigens. For these antigens, mice lacking CD30 molecules display impaired negative selection of TCR-transgenic cortical thymocytes specific for the male (HY) antigen 10. However, CD30−/− mice show no defect in negative selection to endogenous superantigens (Sags).1 For these antigens, negative selection occurs late in thymocyte differentiation and is most prominent in the medulla 18 19. The observation that CD30 controls negative selection in the cortex but not the medulla is surprising, because expression of CD30 and CD30L is largely confined to the medulla 20 21 22.
For the late onset form of negative selection directed to endogenous Sags, little or no defect in negative selection is seen in TNFR−/− 11, CD28−/− 23, or Fas-deficient lpr/lpr 24 mice. CD40L−/− mice do show impaired negative selection to Sags, implying that CD40L may act as an important costimulatory molecule for negative selection 25. However, the alternative possibility is that CD40L promotes negative selection by increasing the expression of other costimulatory molecules on thymic APCs 11. With regard to other molecules, Fas has been found to influence negative selection of a population of semimature heat-stable antigen (HSA)hiCD4+8− cells found in the medulla 26 27. In neonatal mice, Vβ-specific deletion of these cells after injection of soluble Sags is prominent in normal mice but defective in lpr/lpr mice, though only when high doses of antigen are injected.
As a whole, the approach of using gene knockout mice to define the molecules that provide costimulation for negative selection has been unsuccessful. It is conceivable that further studies will reveal that negative selection is mediated via a single, as yet undiscovered costimulatory molecule. However, the alternative possibility is that negative selection is controlled by several different molecules acting in consort. According to this redundancy model, deletion of individual costimulatory molecules would have little or no effect on negative selection because of compensatory function by the other molecules.
A prediction of the above model is that a number of different cell surface molecules on thymocytes can provide costimulation for apoptosis after TCR ligation. To address this issue, we have assessed the requirements for inducing TCR-dependent apoptosis of typical immature cortical CD4+8+ thymocytes and also the population of semimature HSAhiCD4+8− thymocytes found in the medulla. For HSAhiCD4+8− thymocytes, the results show that at least three different cell surface molecules, CD28, CD5, and CD43, can provide costimulation for TCR-mediated apoptosis. Two cytokines, IL-4 and IL-7, impair the function of these molecules and can abolish negative selection both in vitro and in vivo.
Materials and Methods
Mice.
Adult C57BL/6 (B6), B6lpr/lpr, BALB/cByJ, B6 CD28−/− 28, B6 CD43−/− 29, and C3H/HeJ mice aged 6–10 wk were obtained from The Jackson Laboratory. For in vivo studies, CD28−/−, CD43−/−, CD28−/− lpr/lpr, and CD43−/− lpr/lpr mice were backcrossed to BALB/c (H-2d) for four to five generations; newborn (2-d-old mice) were used.
Antibodies.
Antibodies specific for the following markers were previously described 26 30: CD3 (C363.29B, rat IgG), CD4 (RL172, rat IgM), CD8 (3.168.8, rat IgM), CD25 (7D4, rat IgM), CD45 (104.2.1, mouse IgG2), and HSA (J11D, rat IgM). The following mAbs were purchased from PharMingen: anti–TCR-β (H57-597, hamster IgG), anti-CD2 (RM2-5, rat IgG), anti-CD5 (53-7.3, rat IgG), anti–LFA-1 (CD11) (M17/4, rat IgG), anti-CD27 (LG.3A10, hamster IgG), anti-CD28 (37.51, hamster IgG), anti-CD40L (CD154, MR1, hamster IgG), anti-CD43 (S7, rat IgG), anti-CD48 (HM48-1, hamster IgG), anti-CD49d (very late antigen [VLA]-4; R1-2, rat IgG), anti-CD81 (2F7, hamster IgG), anti–thymic shared antigen (TSA)-1 (MTS35, rat IgG), anti–CTL-associated antigen (CTLA)-4 (CD152; UC10-4F10-11, hamster IgG), anti-CD95 (Fas; Jo2, hamster IgG), and Cy-Chrome–conjugated anti-CD4 (H129.19, rat IgG). PE-conjugated anti-CD8 (53.6.7, rat IgG) was purchased from GIBCO BRL. Anti-CD30 (2SH12-5F-2D, hamster IgG) mAb 31 was provided by Dr. Eckhard R. Podack (University of Miami School of Medicine, Miami, FL).
Cell Purification.
TCRloCD4+8+ and HSAhiCD4+8− thymocytes were purified as previously described 8 9 26. In brief, TCRloCD4+8+ cells were prepared by treating thymocytes with mAbs specific for CD3 (C363.29B) and CD25 (7D4) plus guinea pig complement (C) for 45 min at 37°C and then positively panning the surviving cells on plastic plates coated with anti-CD8 (3.168.8) mAb. HSAhiCD4+8− cells were prepared by treating thymocytes with mAbs specific for CD8 (3.168.8) and CD25 (7D4) plus guinea pig C at 37°C, followed by sequential positive panning with anti-CD4 (RL1720 and anti-HSA [J11D]) mAbs, respectively.
Culture Conditions.
Purified thymocytes (3 × 105) were cultured in 0.2 ml of RPMI supplemented with 5 × 10−5 M 2-ME, l-glutamine, and 10% FCS in 96-well tissue culture plates coated with anti-TCR (H57-597)+/− anti-CD28 (37.51) mAbs or medium alone 26. Where indicated, recombinant IL-2, IL-4, IL-7, and IFN-γ 32 33 were added to the cultures at 100 U/ml.
In Vivo Treatment for the Deletion of Immature Thymocytes.
As described elsewhere 27, newborn (1–6-d-old) mice were injected intraperitoneally with staphylococcal enterotoxin B (SEB; Sigma Chemical Co.) at the dose specified. 44 h after injection (on day 2), the mice were killed and cell surface markers of thymocytes were analyzed.
Flow Cytometric Analysis.
For the in vivo studies, thymocytes were incubated with FITC-conjugated anti-HSA (M1/69), PE-conjugated anti-CD8 (53-6.7), Cy5-conjugated anti-CD4 (GK1.5), and biotinylated anti-Vβ8 (F23.1), anti-Vβ6 (RR4-7), or anticlonotype DO11 (KJ1.25) mAbs, followed by TRI-COLOR–conjugated streptavidin (Caltag Labs.). For in vitro studies, thymocytes were stained with PE-conjugated anti-CD8, Cy-Chrome–conjugated anti-CD4 (H129.19), and Cy5-conjugated anti-HSA (J11D) mAbs, and then TUNEL (TdT-mediated dUTP-biotin nick-end labeling)-stained after cell fixation. TUNEL staining was described previously 8 9. In many of the figures, the data are expressed as difference in (Δ) apoptosis, i.e. percent apoptosis induced by mAb ligation minus the background percent apoptosis for cells cultured in medium alone.
Results
Experimental System.
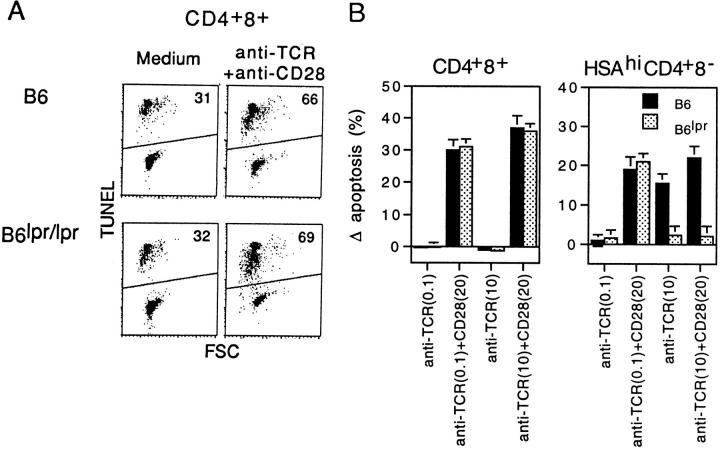
To examine which particular molecules on thymocytes provide costimulation for negative selection, we employed the system of Punt et al. 6, in which purified subsets of thymocytes are cultured overnight in wells coated with anti-TCR mAb plus/minus other mAbs. Using TUNEL staining to detect apoptotic cells, we previously showed 26 that exposure to a mixture of cross-linked anti-TCR and anti-CD28 mAbs induces significant apoptosis of immature TCRloCD4+8+ and semimature TCRhiHSAhiCD4+8− thymocytes; with either mAb alone, levels of apoptosis are not above the background found for cells cultured in medium alone. Representative TUNEL staining and differences in apoptosis levels are shown in Fig. 1.
Figure 1.
Features of TCR-dependent apoptosis of CD4+8+ and HSAhiCD4+8− thymocyte subsets in vitro. Purified TCRloCD4+8+ or HSAhiCD4+8− thymocytes from B6 or B6lpr/lpr mice were cultured for 20 h in vitro in 200-μl wells coated with anti-TCR (H57-597) mAb at 0.1 or 10 μg/ml plus/minus anti-CD28 (37.51) mAb at 20 μg/ml; as controls, cells were cultured in medium alone or in wells coated with anti-CD28 mAb alone. Apoptosis was detected by TUNEL staining and FACS™ analysis. (A) Representative TUNEL staining versus forward scatter (FSC) for CD4+8+ cells cultured in medium alone or in wells coated with a mixture of anti-TCR (0.1 μg/ml) and anti-CD28 mAbs; the numbers in the panels show the proportion of TUNEL+ cells. (B) Difference in (Δ) apoptosis levels (%) for CD4+8+ and HSAhiCD4+8− cells cultured with anti-TCR mAb (0.1 or 10 μg/ml) alone or with anti-TCR plus anti-CD28 mAbs. The data show mean percent differences in apoptosis for triplicate cultures.
For the experiments considered below, it is important to emphasize that TCR-mediated apoptosis of HSAhiCD4+8− thymocytes can be either Fas dependent or Fas independent, depending upon the conditions used (Fig. 1). In our studies, Fas plays no role in apoptosis when the “strength” of TCR ligation is kept at a low to moderate level, e.g., when (a) thymocytes are cultured with a low concentration of cross-linked anti-TCR mAb (plus a high concentration of anti-CD28 mAb) in vitro or (b) mice are injected with low doses of a soluble Sag 27. In these situations, TCR-dependent apoptosis of HSAhiCD4+8− thymocytes is prominent with both normal and lpr/lpr mice. Fas only plays a role in apoptosis when TCR ligation is intense, e.g., when thymocytes are subjected to strong TCR/CD28 ligation in vitro or mice are injected with high doses of Sags. Here, apoptosis is clearly apparent in normal mice but minimal in lpr/lpr mice. The implication, therefore, is that the Fas-independent pathway(s) of negative selection fails when the strength of TCR-dependent signaling exceeds a certain threshold; in this situation, Fas-mediated apoptosis becomes important as a “back-up” mechanism for negative selection. It should be noted that, in our results, Fas does not play a discernible role in TCR-dependent apoptosis of cortical CD4+8+ cells (Fig. 1).
Cell Surface Molecules Provide Costimulation for TCR-dependent Apoptosis of Thymocytes In Vitro.
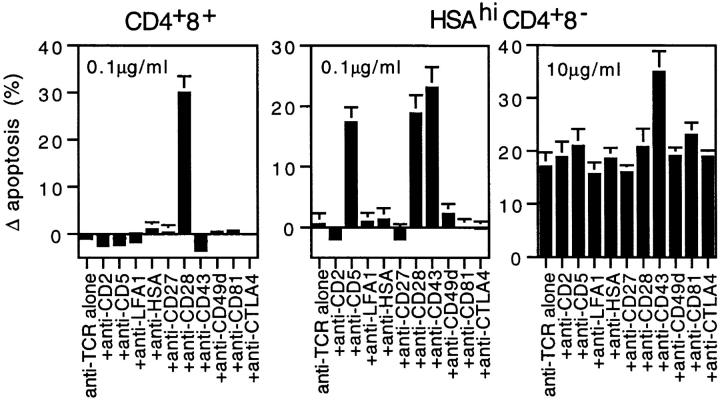
In the experiments shown in Fig. 2, we examined the effects of culturing purified TCRloCD4+8+ and HSAhiCD4+8− thymocytes with low (0.1 μg/ml) versus high (10 μg/ml) concentrations of anti-TCR mAb plus/minus a high concentration (20 μg/ml) of mAbs specific for various cell surface molecules on thymocytes; all mAbs were presented in cross-linked form, i.e., in wells precoated with mAbs. The data are shown as difference in apoptosis.
Figure 2.
Capacity of various cell surface molecules on thymocytes to provide costimulation for TCR-dependent apoptosis of CD4+8+ and HSAhiCD4+8− thymocytes in vitro. Purified subsets of thymocytes from normal B6 mice were cultured overnight with anti-TCR mAb at 0.1 or 10 μg/ml plus/minus the mAbs shown (all at 20 μg/ml). The data represent mean percent differences in (Δ) apoptosis for triplicate cultures. The concentrations of anti-TCR mAbs used are shown in the panels.
For CD4+8+ cells, out of a total of 15 mAbs tested, only one mAb, anti-CD28, provided costimulation for TCR-dependent apoptosis. Data for anti-CD28 and nine other mAbs are shown in Fig. 2, left; negative results were observed with mAbs specific for five further molecules, i.e., CD30, CD40L, CD45, CD48, and TSA. Except for a slight increase by anti-CD45 mAb, none of the mAbs tested affected apoptosis when CD4+8+ cells were cultured without anti-TCR mAb (data not shown). The sole capacity of anti-CD28 mAb to provide costimulation for death of CD4+8+ cells was previously reported by Punt et al. 34 and applied to both low (Fig. 2, left) and high (data not shown) concentrations of anti-TCR mAb.
Different results were observed with HSAhiCD4+8− cells (Fig. 2, center). For these cells, mAbs specific for three cell surface molecules, CD28, CD5, and CD43, provided costimulation for TCR-dependent apoptosis; with the other 12 mAbs, differences in apoptosis levels were very low or undetectable (Fig. 2, center and data not shown). As with CD4+8+ cells, none of the mAbs tested altered apoptosis of cells cultured without anti-TCR mAb.
The capacity of mAbs specific for CD28, CD5, or CD43 to provide costimulation for death of HSAhiCD4+8− thymocytes applied to Fas-independent apoptosis, i.e., to apoptosis induced by a low concentration of anti-TCR mAb (Fig. 2, center). With a high concentration of anti-TCR mAb, the Fas-dependent apoptosis induced by TCR ligation alone was augmented by only one mAb, anti-CD43 (Fig. 2, right); none of the other mAbs tested had more than marginal effects on Fas-dependent apoptosis.
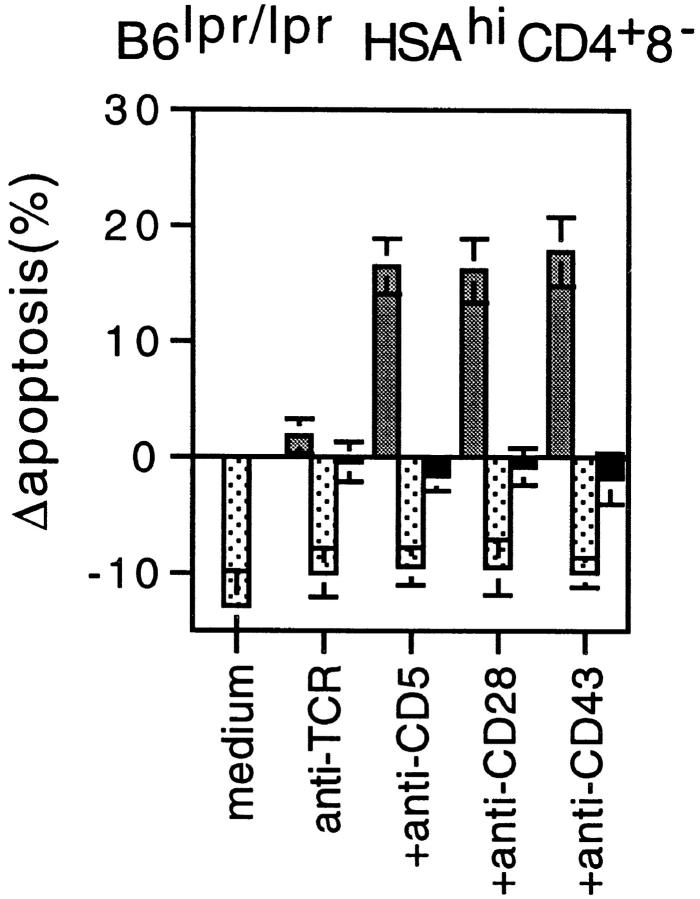
It was mentioned earlier that Fas-independent apoptosis of HSAhiCD4+8− cells induced by combined TCR/CD28 ligation fails with strong TCR ligation, i.e., with a high concentration of anti-TCR mAb. Similar findings applied with costimulation via CD5 or CD43. Thus, with HSAhiCD4+8− cells from Fas-deficient B6lpr/lpr mice, TCR-dependent apoptosis induced by coligation of CD28, CD5, or CD43 declined to near background levels when the concentration of anti-TCR mAb was increased to a high level, 10 μg/ml (Fig. 3).
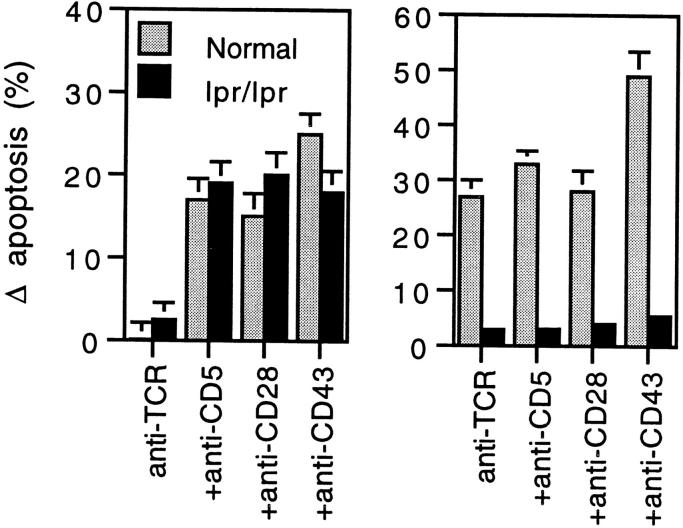
Figure 3.
For CD28, CD5, and CD43, costimulation for Fas-independent apoptosis of HSAhiCD4+8− cells in vitro fails with strong TCR ligation. HSAhiCD4+8− cells from normal B6 or B6lpr/lpr mice were cultured overnight with either a low (0.1 μg/ml; left) or high (10 μg/ml; right) concentration of anti-TCR mAb plus/minus anti-CD5, anti-CD28, or anti-CD43 mAbs (20 μg/ml). The data show mean percent differences in (Δ) apoptosis for triplicate cultures.
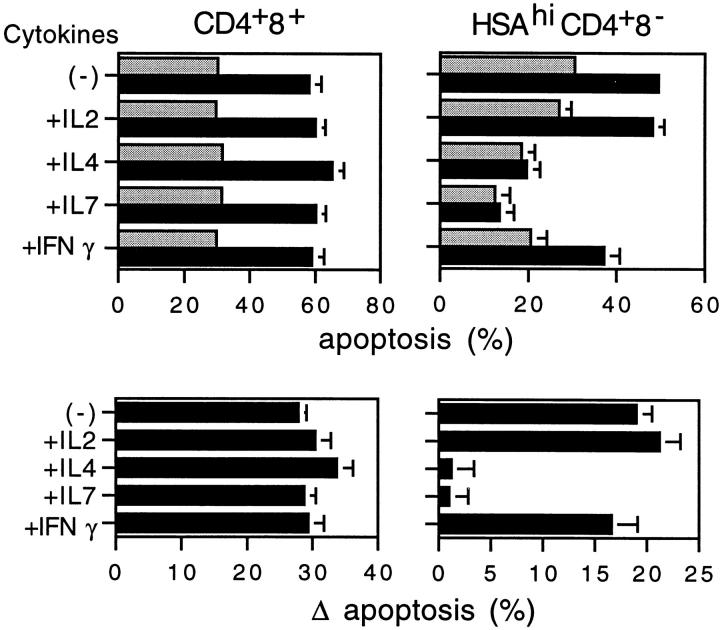
Capacity of Cytokines to Inhibit Fas-independent Apoptosis of HSAhiCD4+8− Thymocytes.
We tested four cytokines, IL-2, IL-4, IL-7, and IFN-γ, for their capacity to influence Fas-independent apoptosis. For CD4+8+ cells, none of these cytokines affected either spontaneous (background) apoptosis (Fig. 4, top left) or change in apoptosis induced by TCR/CD28 ligation (Fig. 4, bottom left). For HSAhiCD4+8− cells, however, two of the cytokines, IL-4 and IL-7, considerably reduced spontaneous apoptosis (Fig. 4, top right) and abolished TCR/CD28-mediated apoptosis (Fig. 4, bottom right).
Figure 4.
Capacity of cytokines to inhibit Fas-independent apoptosis of thymocyte subsets in vitro. Purified CD4+8+ or HSAhiCD4+8− thymocytes from normal B6 mice were cultured overnight either in medium alone (gray bars) or with a mixture of anti-TCR (0.1 μg/ml) and anti-CD28 mAbs (black bars); where indicated, the recombinant cytokines shown were added to the cultures at 100 U/ml. The data show mean percent apoptosis (top panels) and percent difference in (Δ) apoptosis (bottom panels).
Significantly, the capacity of these two cytokines to protect against TCR/CD28-mediated apoptosis also applied to apoptosis mediated by TCR/CD5 and TCR/CD43 ligation. Data for the effects of IL-7 on B6lpr/lpr HSAhiCD4+8− cells are shown in Fig. 5. It can be seen that, with low-level TCR ligation (anti-TCR mAb at 0.1 μg/ml), apoptosis induced by coligation of CD28, CD5, or CD43 was abolished by addition of IL-7; confirming the data in Fig. 3, costimulation-dependent apoptosis was not seen with strong TCR ligation (anti-TCR mAb at 10 μg/ml).
Figure 5.
Costimulation-dependent apoptosis induced by TCR/CD28, TCR/CD5, or TCR/CD43 ligation in vitro is abolished by IL-7. Purified HSAhiCD4+8− thymocytes from B6lpr/lpr mice were cultured with either a low or high concentration of anti-TCR mAb plus/minus mAbs specific for CD28, CD5, or CD43; where indicated, IL-7 was added to the cultures at 100 U/ml. The data show mean levels of difference in (Δ) apoptosis for triplicate cultures. Gray bar, anti-TCR (0.1 μg/ml); dotted bar, anti-TCR (0.1 μg/ml) plus IL-7; black bar, anti-TCR (10 μg/ml).
In contrast to Fas-independent apoptosis, Fas-dependent apoptosis of HSAhiCD4+8− cells induced by strong TCR ligation (anti-TCR mAb at 10 μg/ml) was not inhibited by IL-4 or IL-7 (or by IL-2 or IFN-γ) (data not shown).
Effects of Cytokines on Negative Selection In Vivo.
The above findings indicated that IL-4 and IL-7 selectively blocked Fas-independent apoptosis but did not affect Fas-dependent apoptosis. These observations raised the question of whether cytokines would be able to inhibit physiological negative selection in vivo. For Fas-independent apoptosis, it is notable that the inhibitory effects of IL-4 and IL-7 applied to all three of the molecules that provided costimulation for death of HSAhiCD4+8− cells, i.e., CD28, CD5, and CD43. Thus, even though physiological negative selection may involve other as yet untested cell surface molecules, inhibition via IL-4 or IL-7 could apply to all forms of costimulation leading to Fas-independent apoptosis. If so, these cytokines would be expected to block negative selection in vivo, but only Fas-independent and not Fas-dependent negative selection.
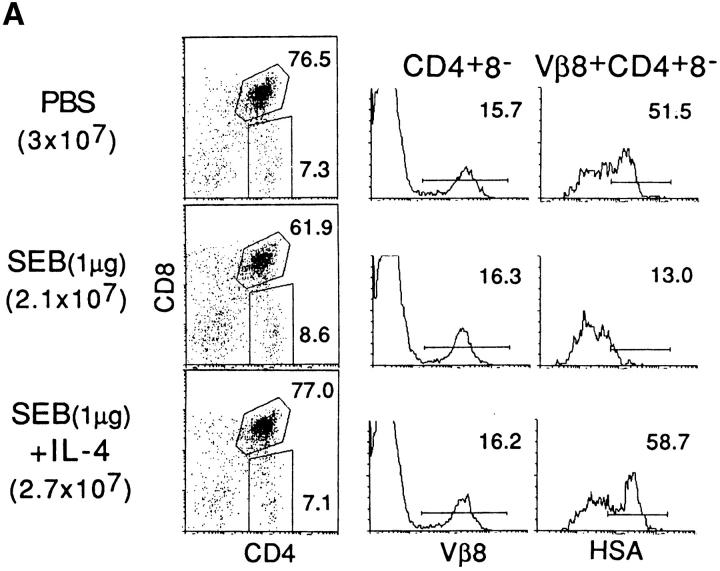
To test this prediction, we examined negative selection in neonatal mice injected with high versus low doses of a soluble Sag, SEB. With this model, previous studies showed that injecting neonatal mice with SEB had little effect on CD4+8+ cells but caused selective deletion of SEB-reactive Vβ8+ cells at the level of HSAhiCD4+8− thymocytes 27; deletion of these semimature T cells was accompanied by expansion of fully mature Vβ8+HSAloCD4+8− cells. Testing normal versus lpr/lpr mice showed that negative selection of HSAhiCD4+8− cells was Fas independent when the dose of SEB was kept at a low to moderate level (<1 μg/mouse) but was Fas dependent when high doses of SEB (50–100 μg) were injected 27.
The effects of injecting SEB plus/minus 40,000 U of IL-4 into neonatal normal C3H/HeJ mice are shown in Fig. 6; C3H/HeJ (IAkIEk) rather than B6 (IAbIE−) mice were used because SEB is presented by IE much more effectively than by IA molecules. Confirming previous findings 27, injection of a moderate dose of 1 μg SEB without IL-4, i.e., a dose of SEB that induces Fas-independent negative selection, caused selective removal of Vβ8+HSAhiCD4+8− cells when measured on day 2 after injection (Fig. 6 A); data on total numbers of Vβ8+ cells per thymus (and Vβ6+ cells as a control) are shown in Fig. 6 B. Note that, because of expansion of fully mature HSAloCD4+8− cells, negative selection is not apparent at the level of CD4+8− thymocytes unless these cells are typed for HSA expression; the elimination of HSAhi cells reflects deletion rather than maturation into HSAlo cells 27.
Figure 6.
Capacity of IL-4 to abolish Fas-independent but not Fas-dependent negative selection to SEB in vivo. Neonatal (2-d-old) C3H/HeJ mice were injected intraperitoneally with PBS or the indicated amount of SEB plus/minus 40,000 U of IL-4; thymi were removed on day 2. Thymocyte suspensions were counted and four-color stained for CD4, CD8, HSA, and Vβ8 or Vβ6 expression and FACS™ analyzed (see Materials and Methods). (A) Representative data showing CD4/CD8 expression on whole thymocytes, Vβ8 expression on gated CD4+8− cells, and HSA expression on gated Vβ8+CD4+8− cells; percentages positive cells are shown. Data in parentheses refer to mean total numbers of viable thymocytes per mouse (three mice per group). (B) Data show total numbers of Vβ8+ and Vβ6+ cells per mouse at the level of semimature HSAhiCD4+8− cells and fully mature HSAloCD4+8− cells.
The key finding was that coinjection of IL-4 with SEB completely inhibited the elimination of Vβ8+HSAhiCD4+8− thymocytes (Fig. 6a and Fig. b). With a high dose of SEB, however, the results were quite different. In this situation, i.e., where negative selection is Fas dependent, coinjection of IL-4 had no effect on SEB-induced deletion of Vβ8+HSAhi CD4+8− thymocytes (Fig. 6 B). Thus, IL-4 selectively blocked Fas-independent negative selection in vivo and did not influence Fas-dependent negative selection.
Negative Selection in Mice Lacking CD28 or CD43 Molecules.
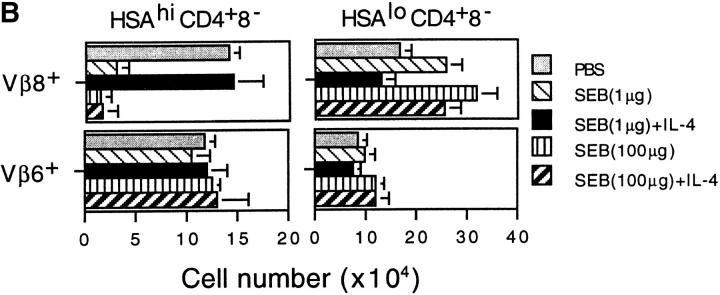
The notion that a number of different cell surface molecules on thymocytes provide costimulation for negative selection raises the question of whether individual molecules are totally redundant in this process or only partly so. Total redundancy would seem likely because CD28−/− mice show no obvious defects in negative selection to endogenous antigens 14 23; there are currently no reports on negative selection in CD43−/− 35 36 and CD5−/− 37 mice. However, it is conceivable that individual costimulatory molecules do play a discernible role in negative selection at limited concentrations of antigen.
To assess this possibility, we examined negative selection in normal, neonatal, CD28−/− and CD43−/− mice given graded doses of SEB (Fig. 7); for these studies, mice on an IE+BALB/c (H-2d) background were used. With injection of high doses of SEB (50 μg/mouse), elimination of Vβ8+ HSAhiCD4+8− thymocytes was as extensive in CD28−/− and CD43−/− mice as in normal mice (Fig. 7 A, left). With this high dose of antigen, negative selection was largely Fas dependent because minimal deletion occurred in Fas-deficient CD28−/− lpr/lpr and CD43−/− lpr/lpr mice (Fig. 7 B, left). However, for Fas-independent negative selection induced by a low dose of SEB, e.g., 1 μg, negative selection was clearly less marked in CD28−/− and CD43−/− mice than in normal mice (Fig. 7 A, left). These data refer to SEB-reactive Vβ8+ cells; numbers of Vβ6+ cells were largely unaffected by SEB injection (Fig. 7A and Fig. B, right panels).
Figure 7.
Fas-independent negative selection induced by low doses of SEB in vivo is defective in CD28−/ − and CD43−/ − mice. Mice on a BALB/c (H-2d) background were injected with graded doses of SEB; on day 2, thymocytes were stained and analyzed as in Fig. 6. The data show total numbers of Vβ8+ and Vβ6+ cells/mouse (three to five mice per group) at the level of HSAhiCD4+8− cells. The data refer to (A) cells from normal CD28+/+43+/+ (□), CD28−/ −43+/+ (○), and CD28+/+43−/ − (▵) mice and to (B) CD28+/+43+/+ lpr/lpr (▪), CD28−/ −43+/+ lpr/lpr (•), and CD28+/+43−/ − lpr/lpr (▴) mice.
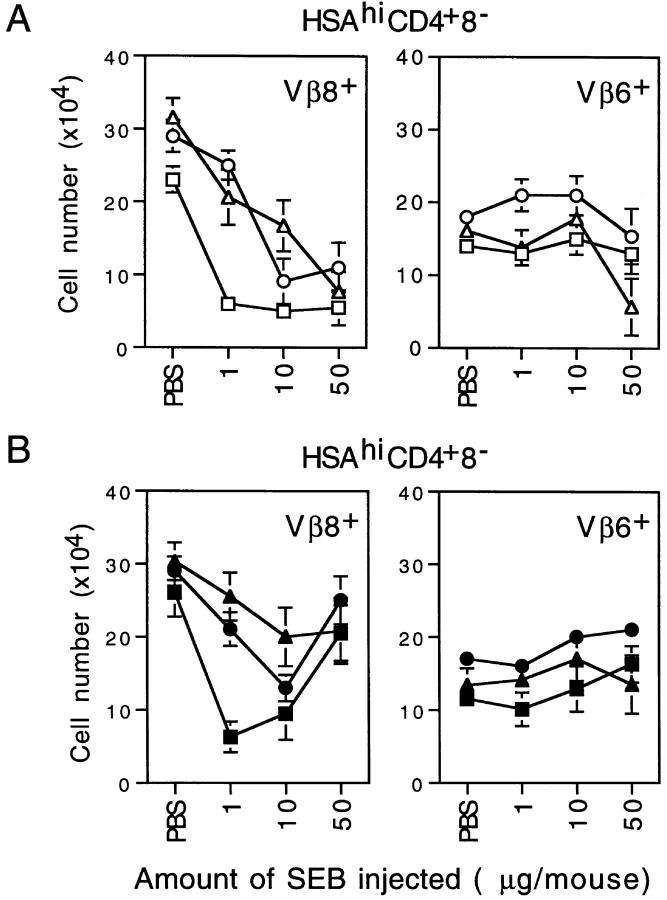
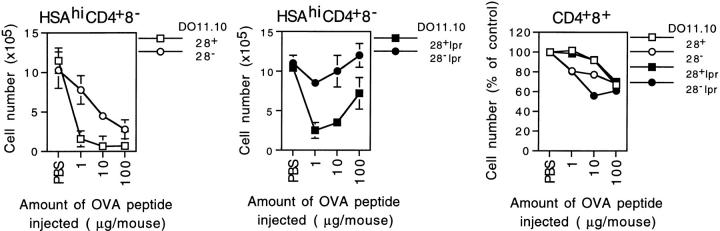
For CD28, comparable findings applied when neonatal D011.10 TCR-transgenic mice were injected with specific peptide, ova 323–339 (Fig. 8). Thus, with injection of limiting doses of peptide, e.g., 1 μg, deletion of TCR clonotype–positive HSAhiCD4+8− cells was substantial in normal D011 mice but minimal in CD28−/− D011 mice (Fig. 8, left). With a high dose of peptide (100 μg), negative selection was near complete in both normal and CD28−/− D011 mice; negative selection in this situation was Fas dependent because negative selection induced by a high dose of peptide was minimal in both CD28+lpr/lpr and CD28−/− lpr/lpr D011 mice (Fig. 8, center). These data refer to HSAhiCD4+8− cells. Elimination of CD4+8+ cells after peptide injection was minimal and was not decreased by CD28 or Fas expression (Fig. 8, right).
Figure 8.
Fas-independent and Fas-dependent negative selection in D011.10 TCR-transgenic mice injected with specific peptide. Neonatal normal, CD28−/ −, and CD28−/ − lpr/lpr D011.10 mice on a BALB/c (H-2d) background were injected with graded doses of ova 323–339 peptide or PBS; after 2 d, thymocytes were stained for CD4, CD8, HSA, and TCR clonotype (KJ25) expression. The data show total numbers of TCR clonotype–positive cells at the level of HSAhiCD4+8− cells (left and center) and CD4+8+ cells (right) (three mice per group).
Discussion
As mentioned earlier, it is generally agreed that induction of negative selection in the thymus requires some form of costimulation 5 6 7 8 9 34. As activation of mature T cells appears to be largely under the control of a single costimulatory molecule, CD28 29 38 39, it was initially presumed that CD28 must also play a crucial role in negative selection. The fact that most groups have found little or no impairment of negative selection in CD28−/− mice thus seems puzzling. In light of this finding, the tacit assumption has been that negative selection is controlled by some other, as yet unknown costimulatory molecule. However, in view of the largely negative data derived from studies on many different gene knockout mice (see Introduction), the notion that negative selection is under the control of a single costimulatory molecule is becoming increasingly unlikely.
Although future studies on gene knockout mice may bring surprises, serious consideration has to be given to the idea that negative selection is not controlled by a single costimulatory molecule but rather by multiple molecules acting in consort 11 26 27. Why has this notion generated little enthusiasm? Perhaps the major concern is that attributing negative selection to the action of multiple costimulatory molecules is a marked departure from the idea that only a single molecule, CD28, provides costimulation for mature T cells. However, here the precise definition of costimulation becomes important. If costimulation is defined in terms of cytokine production and survival of the responding T cells, CD28 is clearly a dominant costimulatory molecule for mature T cells 29 38. This point is illustrated by a recent study in which naive T cells were subjected to TCR ligation in the presence of cross-linked mAbs specific for a variety of cell surface molecules 40. The clear-cut finding was that, of the molecules tested, only CD28 provided costimulation for cytokine (IL-2) production and protection of T cells from apoptosis. For induction of T proliferative responses, however, CD28 ligation was no more effective than ligation of a number of other cell surface molecules. Thus, although CD28 is crucial for inducing a “productive” immune response (IL-2 production and extended T cell survival), CD28 is merely one of several molecules that can provide costimulation for the initial activation of T cells.
This point is important because the unique capacity of CD28 to costimulate productive responses of mature T cells may be largely irrelevant to the induction of apoptosis during negative selection (which presumably does not depend on cytokine production). Thus, inducing negative selection may not require classic costimulation but simply augmentation of TCR-dependent signaling; many cell surface molecules may have this property, i.e., as for eliciting initial proliferation of mature T cells.
As argued above, it would seem plausible that a number of different cell surface molecules are capable of inducing or promoting the signaling events that cause T cells to die during negative selection. In line with this view, we show here that, based on studies with cross-linked mAbs, at least three different molecules on thymocytes, CD28, CD5, and CD43, provided effective costimulation for TCR-mediated apoptosis of HSAhiCD4+8− thymocytes in vitro. As many other molecules on thymocytes have yet to be tested, negative selection could well involve a multiplicity of different costimulatory molecules. If so, demonstrating conspicuous defects in negative selection would be expected to require combined deletion of several of these molecules. On this point, it is surprising that induction of negative selection in vivo was clearly less efficient in mice deficient in only a single costimulatory molecule, i.e., in CD28−/− and CD43−/− mice (Fig. 7). It should be emphasized, however, that defective negative selection in these mice was only apparent when limiting doses of antigen were injected. Our expectation is that the defects in negative selection in CD28−/− and CD43−/− mice will be more pronounced in combined CD28−/−CD43−/− mice; we are in the process of testing this prediction.
The signaling events that lead to negative selection are still largely obscure, although the MKK6-p38 MAP (mitogen-activated protein) kinase pathway 41 and certain transcription factors, notably Nur77 42 43 44, appear to play an important role. As mentioned above, negative selection could be independent of classic costimulation and merely depend on potentiation of TCR-dependent signaling. If so, one would expect that the range of cell surface molecules able to induce negative selection of thymocytes and initial activation (proliferation) of mature T cells would be quite similar. In agreement with this notion, the three molecules shown here to induce TCR-mediated apoptosis of thy-mocytes, CD28, CD5, and CD43, are all reported to be capable of providing costimulation for proliferation of naive T cells 40 45. However, at least two other molecules able to costimulate mature T cells, CD2 and LFA-1 40, showed no detectable capacity to potentiate negative selection in our hands (Fig. 2). Thus, costimulation for negative selection is presumably more complex than simply augmenting TCR signaling.
Although the signaling pathways leading to negative selection via CD28, CD5, and CD43 could be fundamentally different, it is notable that for Fas-independent negative selection, the costimulatory function of these three molecules was completely inhibited by IL-4 or IL-7. Significantly, the inhibitory effect of these cytokines also applied to negative selection in vivo. Thus, when mice were injected with a low dose of SEB (thereby excluding Fas-dependent apoptosis), coinjection of a single dose of IL-4 totally abolished the elimination of SEB-reactive Vβ8+ cells at the level of HSAhiCD4+8− cells (Fig. 6). This finding could explain why the neonatal thymus, which is enriched in IL-4–producing T cells 46, shows less efficient negative selection to endogenous Sags than the adult thymus 47 48. Similarly, the impaired negative selection seen in graft-versus-host disease 49 50 could reflect migration of IL-4–producing, host-reactive T cells to the thymus.
How IL-4 and IL-7 block Fas-independent negative selection is unknown. However, preliminary work has shown that adding IL-4 or IL-7 during exposure of HSAhiCD4+8− thymocytes to weak TCR/CD28 ligation in vitro causes strong activation of NKκB (our unpublished data). As NFκB activation can protect cells from apoptosis 51, the inhibitory effects of IL-4 on negative selection may thus reflect induction of antiapoptotic molecules in the responding T cells. This idea could also explain the paradox that Fas-independent negative selection only operates with relatively low doses of antigen in vivo or with weak TCR/CD28 (CD5, CD43) ligation. Under these conditions, NFκB activation is low, thus favoring apoptosis induction. However, with strong TCR/CD28 ligation, NFκB activation is pronounced and apoptosis is minimal (our unpublished data). A priori, NFκB activation could be a direct consequence of strong TCR/CD28 ligation per se. Alternatively, strong TCR/CD28 ligation may induce the T cells to produce IL-4 or IL-7, which in turn could stimulate NFκB activation. This second possibility is under investigation.
In view of the above findings, the failure of Fas-independent negative selection after strong TCR (TCR/CD28) ligation (or weak TCR ligation in the presence of IL-4 or IL-7) may reflect protection against apoptosis via induction of antiapoptotic molecules. Thus, to guard against this problem, a quite separate pathway of apoptosis induction could be crucial as a backup for negative selection. Fas could play this role. In our hands, Fas only contributes to negative selection when the dose of antigen (or the strength of TCR ligation) is high, i.e., under conditions where the Fas-independent pathway is inoperative. Here it is of interest that, unlike Fas-independent apoptosis, the Fas-dependent pathway of apoptosis appears to be resistant to the protective effects of cytokines. Thus, the capacity of IL-4 to block negative selection after SEB injection applied only with a low dose and not a high dose of SEB (Fig. 6); as discussed previously 27 and confirmed here, studies with normal versus lpr/lpr mice indicate that negative selection induced by a high dose of SEB is strongly Fas dependent.
As the Fas-independent and -dependent pathways of negative selection seem to be distinctly different, demonstrating significant deficits in negative selection in normal mice in response to a broad range of antigen concentrations would presumably require the inactivation of both pathways. Although our data on this point are still limited, it is notable that double-deficient CD28−/ − lpr/lpr and CD43−/ − lpr/lpr mice showed a conspicuous defect in negative selection after SEB injection (Fig. 7); especially for CD43−/ − lpr/lpr mice, this finding applied irrespective of the dose of SEB injected. A similar marked defect in negative selection was seen in CD28−/ − lpr/lpr D011 mice after injection of specific peptide (Fig. 8). Thus, although multiple cell surface molecules may be involved in negative selection, some of these molecules (CD28, CD43, and Fas) may be more important than others.
The data in this paper refer only to negative selection affecting medullary HSAhiCD4+8− cells. The costimulation requirements for deletion of CD4+8+ cells could be quite different. On this point it is worth noting that, confirming the findings of others 34, the only molecule on CD4+8+ cells found capable of costimulating TCR-dependent apoptosis was CD28; ligation of other molecules, including CD30 (see Introduction), CD5, and CD43 was totally ineffective. These data on cortical CD4+8+ cells are not easily interpreted, especially in light of the finding that antigens expressed selectively in the cortex are unable to induce negative selection 52. Why CD4+8+ cells are resistant to TCR-dependent death via CD5 or CD43 ligation is unclear. The simplest possibility is that, in contrast to CD28, signaling via CD5 or CD43 is inoperative in thymocytes until after the transition of CD4+8+ cells to HSAhiCD4+8− cells. This idea is being investigated.
Acknowledgments
We thank Ms. Barbara Marchand for typing the manuscript.
This work was supported by grants CA38355, CA25803, AI21487, AI32068, and AG01743 from the United States Public Health Service. H. Kishimoto is the recipient of a fellowship from the Cancer Research Institute. This is publication no. 12288-IMM from the Scripps Research Institute.
Footnotes
1used in this paper: HSA, heat-stable antigen; Sags, superantigens; SEB, staphylococcal enterotoxin; TUNEL, Tdt-mediated dUTP-biotin nick-end labeling
References
- Fowlkes B.J., Ramsdell F. T-cell tolerance. Curr. Opin. Immunol. 1993;5:873–879. doi: 10.1016/0952-7915(93)90099-e. [DOI] [PubMed] [Google Scholar]
- Nossal G.J.V. Negative selection of lymphocytes. Cell. 1994;76:229–239. doi: 10.1016/0092-8674(94)90331-x. [DOI] [PubMed] [Google Scholar]
- Sprent J. Central tolerance of T cells. Int. Rev. Immunol. 1995;13:95–105. doi: 10.3109/08830189509061740. [DOI] [PubMed] [Google Scholar]
- Jameson S.C., Bevan M.J. T-cell selection. Curr. Opin. Immunol. 1998;10:214–219. doi: 10.1016/s0952-7915(98)80251-3. [DOI] [PubMed] [Google Scholar]
- Page D.M., Kane L.P., Allison J.P., Hedrick S.M. Two signals are required for negative selection of CD4+8+ thymocytes. J. Immunol. 1993;151:1868–1880. [PubMed] [Google Scholar]
- Punt J.A., Osborne B.A., Takahama Y., Sharrow S.O., Singer A. Negative selection of CD4+CD8+ thymocytes by T cell receptor–induced apoptosis requires a costimulatory signal that can be provided by CD28. J. Exp. Med. 1994;179:709–713. doi: 10.1084/jem.179.2.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiba Y., Mazda O., Davis M.M., Muramatsu S., Katsura Y. Requirements of a second signal from antigen-presenting cells in the clonal deletion of immature T cells. Int. Immunol. 1994;6:1475–1483. doi: 10.1093/intimm/6.10.1475. [DOI] [PubMed] [Google Scholar]
- Kishimoto H., Surh C.D., Sprent J. Upregulation of surface markers on dying thymocytes. J. Exp. Med. 1995;181:649–655. doi: 10.1084/jem.181.2.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishimoto H., Cai Z., Brunmark A., Jackson M.R., Peterson P.A., Sprent J. Differing roles for B7 and intercellular adhesion molecule-1 in the negative selection of thymocytes. J. Exp. Med. 1996;184:531–537. doi: 10.1084/jem.184.2.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amakawa R., Hakem A., Kundig T.M., Matsuyama T., Simard J.J.L., Timms E., Wakeham A., Mittruecker H.-W., Greisser H., Takimoto H. Impaired negative selection of T cells in Hodgkin's disease antigen CD30-deficient mice. Cell. 1996;84:551–562. doi: 10.1016/s0092-8674(00)81031-4. [DOI] [PubMed] [Google Scholar]
- Page D.M., Roberts E.M., Peschon J.J., Hedrick S.M. TNF receptor-deficient mice reveal striking differences between several models of thymocyte negative selection. J. Immunol. 1998;160:120–133. [PubMed] [Google Scholar]
- Noel P.J., Alegre M.L., Reiner S.L., Thompson C.B. Impaired negative selection in CD28-deficient mice. Cell. Immunol. 1998;187:131–138. doi: 10.1006/cimm.1998.1332. [DOI] [PubMed] [Google Scholar]
- Castro J.E., Listman J.A., Jacobson B.A., Wang Y., Lopez P.A., Ju S., Finn P.W., Perkins D.L. Fas modulation of apoptosis during negative selection of thymocytes. Immunity. 1996;5:617–627. doi: 10.1016/s1074-7613(00)80275-7. [DOI] [PubMed] [Google Scholar]
- Dautigny N., Campion A., Lucas B. Timing and casting for actors of thymic negative selection. J. Immunol. 1999;162:1294–1302. [PubMed] [Google Scholar]
- Jondal M., Okret S., McConkey D. Killing of immature CD4+8+ thymocytes in vivo by anti-CD3 or 5′-(N-ethyl)-carboxamide adenosine is blocked by glucocorticoid receptor antagonism RU-486. Eur. J. Immunol. 1993;23:1246–1250. doi: 10.1002/eji.1830230608. [DOI] [PubMed] [Google Scholar]
- Xue Y., Murdjeva M., Okret S., McConkey D., Kiuossis D., Jondal M. Inhibition of I-Ad-, but not Db-restricted peptide-induced thymic apoptosis by glucocorticoid receptor antagonist RU486 in T cell receptor transgenic mice. Eur. J. Immunol. 1996;26:428–434. doi: 10.1002/eji.1830260224. [DOI] [PubMed] [Google Scholar]
- Martin S., Bevan M.J. Antigen-specific and nonspecific deletion of immature cortical thymocytes caused by antigen injection. Eur. J. Immunol. 1997;27:2726–2736. doi: 10.1002/eji.1830271037. [DOI] [PubMed] [Google Scholar]
- Marrack P., Kappler J.W. The staphylococcal enterotoxins and their relatives. Science. 1990;248:705–711. doi: 10.1126/science.2185544. [DOI] [PubMed] [Google Scholar]
- Surh C.D., Sprent J. T-cell apoptosis detected in situ during positive and negative selection in the thymus. Nature. 1994;372:100–103. doi: 10.1038/372100a0. [DOI] [PubMed] [Google Scholar]
- Romagnani P., Annunziato F., Manetti R., Mavilla C., Lasagni L., Manuelli C., Vannelli G.B., Vanini V., Maggi E., Pupilli C. High CD30 ligand expression by epithelial cells and Hassal's corpuscles in the medulla of human thymus. Blood. 1998;91:3323–3332. [PubMed] [Google Scholar]
- Romagnani P., Annunziato F., Romagnani S. Pleiotropic biologic functions of CD30/CD30L. The Immunologist. 1998;6:137–141. [Google Scholar]
- Horie R., Watanabe T. CD30expression and function in health and disease. Semin. Immunol. 1998;10:457–470. doi: 10.1006/smim.1998.0156. [DOI] [PubMed] [Google Scholar]
- Walunas T.L., Sperling A.I., Khattri R., Thompson C.B., Bluestone J.A. CD28 expression is not essential for positive and negative selection of thymocytes or peripheral T cell tolerance. J. Immunol. 1996;156:1006–1013. [PubMed] [Google Scholar]
- Theofilopoulos A.N. The basis of autoimmunityPart I. Mechanisms of aberrant self-recognition. Immunol. Today. 1995;16:90–98. doi: 10.1016/0167-5699(95)80095-6. [DOI] [PubMed] [Google Scholar]
- Foy T.M., Page D.M., Waldscmid T.J., Schoneveld A., Lamen J.D., Masters S.R., Tygrett L., Ledbetter J.A., Aruffo A., Claassen E. An essential role for gp39, the ligand for CD40, in thymic selection. J. Exp. Med. 1995;182:1377–1388. doi: 10.1084/jem.182.5.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishimoto H., Sprent J. Negative selection in the thymus includes semimature T cells. J. Exp. Med. 1997;185:263–271. doi: 10.1084/jem.185.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishimoto H., Surh C.D., Sprent J. A role for Fas in negative selection of thymocytes in vivo. J. Exp. Med. 1998;187:1427–1438. doi: 10.1084/jem.187.9.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahinian A., Pfeffer K., Lee K.P., Kundig T.M., Kishihara K., Wakeham A., Kawai K., Ohashi P.S., Thompson C.B., Mak T.W. Differential T cell costimulatory requirements in CD28-deficient mice. Science. 1993;261:609–612. doi: 10.1126/science.7688139. [DOI] [PubMed] [Google Scholar]
- Schwartz R.H. Costimulation of T lymphocytes; the role of CD28, CTLA-4, and B7/BB1 in interleukin-2 production and immunotherapy. Cell. 1992;71:1065–1068. doi: 10.1016/s0092-8674(05)80055-8. [DOI] [PubMed] [Google Scholar]
- Kosaka H., Surh C.D., Sprent J. Stimulation of mature unprimed CD8+ T cells by semiprofessional antigen-presenting cells in vivo. J. Exp. Med. 1992;176:1291–1302. doi: 10.1084/jem.176.5.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen M.A., Lee R.K., Miragliotta G., Nam S.Y., Podack E.R. Structure and expression of murine CD30 and its role in cytokine production. J. Immunol. 1996;156:442–449. [PubMed] [Google Scholar]
- Karasuyama H., Melchers F. Establishment of mouse cell lines which constitutively secrete large quantities of interleukin-2, 3, 4, or 5, using modified cDNA expression vectors. Eur. J. Immunol. 1988;18:97–104. doi: 10.1002/eji.1830180115. [DOI] [PubMed] [Google Scholar]
- Rolink A., Kudo A., Karasuyama H., Kikuchi Y., Melchers F. Long-term proliferating early pre B cell lines and clones with the potential to develop to surface Ig-positive, mitogen reactive B cells in vitro and in vivo. EMBO (Eur. Mol. Biol. Organ.) J. 1991;10:327–336. doi: 10.1002/j.1460-2075.1991.tb07953.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punt J.A., Havran W., Abe R., Sarin A., Singer A. T cell receptor (TCR)-induced death of immature CD4+8+ thymocytes by two distinct mechanisms differing in their requirement for CD28 costimulationimplications for negative selection in the thymus. J. Exp. Med. 1997;186:1911–1922. doi: 10.1084/jem.186.11.1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstein Y., Park J.K., Hahn W.C., Rosen F.S., Bierer B.E., Burakoff S.J. CD43, a molecule defective in Wiskott-Aldrich syndrome, binds ICAM-1. Nature. 1991;354:233–235. doi: 10.1038/354233a0. [DOI] [PubMed] [Google Scholar]
- Ostberg J.R., Barth R.K., Frelinger J.G. The Roman god Janusa paradigm for the function of CD43. Immunol. Today. 1998;19:546–550. doi: 10.1016/s0167-5699(98)01343-7. [DOI] [PubMed] [Google Scholar]
- Tarakhovsky A., Kanner S., Hombach J., Ledbetter J., Muller W., Killen N., Rajewsky K. A role for CD5 in TCR-mediated signal transduction and thymocyte selection. Science. 1995;269:535–537. doi: 10.1126/science.7542801. [DOI] [PubMed] [Google Scholar]
- June C.H., Bluestone J.A., Nadler L.M., Thompson C.B. The B7 and CD28 receptor families. Immunol. Today. 1994;15:321–331. doi: 10.1016/0167-5699(94)90080-9. [DOI] [PubMed] [Google Scholar]
- Janeway C.A., Bottomly K. Signals and signs for lymphocytes responses. Cell. 1994;76:275–285. doi: 10.1016/0092-8674(94)90335-2. [DOI] [PubMed] [Google Scholar]
- Yashiro Y., Tai X.G., Toyo-oka K., Park C.S., Abe R., Hamaoka T., Kobayashi M., Neben S., Fujiwara H. A fundamental difference in the capacity to induce proliferation of naive T cells between CD28 and other co-stimulatory molecules. Eur. J. Immunol. 1998;28:926–935. doi: 10.1002/(SICI)1521-4141(199803)28:03<926::AID-IMMU926>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- Sugawara T., Moriguchi T., Nishida E., Takahama Y. Differential roles of ERK and p38 MAP kinase pathways in positive and negative selection of T lymphocytes. Immunity. 1998;9:565–574. doi: 10.1016/s1074-7613(00)80639-1. [DOI] [PubMed] [Google Scholar]
- Woronicz J.D., Calnan B., Ngo V., Winoto A. Requirement for the orphan steroid receptor Nur77 in apoptosis of T-cell hybridomas. Nature. 1994;367:277–281. doi: 10.1038/367277a0. [DOI] [PubMed] [Google Scholar]
- Liu Z.G., Smith S.W., McLaughlin K.A., Schwartz L.M., Osborne B.A. Apoptotic signals delivered through the T-cell receptor of a T-cell hybrid require the immediate-early gene nur77. Nature. 1994;367:281–284. doi: 10.1038/367281a0. [DOI] [PubMed] [Google Scholar]
- Zhou T., Cheng J., Yang P., Liu C., Su X., Bluethmann H., Mountz J.D. Inhibition of Nur77/Nurr1 leads to inefficient clonal deletion of self-reactive T cells. J. Exp. Med. 1996;183:1879–1892. doi: 10.1084/jem.183.4.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperling A.I., Green J.M., Lee Mosley R., Smith P.L., DiPaolo R.J., Klein J.R., Bluestone J.A., Thompson C.B. CD43 is a murine T cell costimulatory receptor that functions independently of CD28. J. Exp. Med. 1995;182:139–146. doi: 10.1084/jem.182.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendelac A., Schwartz R.H. CD4+ and CD8+ T cells acquire specific lymphokine selection potentials during thymic maturation. Nature. 1991;353:68–71. doi: 10.1038/353068a0. [DOI] [PubMed] [Google Scholar]
- Schneider R., Lees R., Pedrazzini T., Odermatt B., Speiser D.E., Zinkernagel R.M., Hengartner H., MacDonald H.R. Fate of potentially self-reactive T cells in neonatal miceanalysis of Vβ 6+ T cells in Mlsa mice. Thymus. 1989;13:35–43. [PubMed] [Google Scholar]
- Signorelli K., Benoist C., Mathis D. Why is clonal deletion of neonatal thymocytes defective? Eur. J. Immunol. 1992;22:2487–2493. doi: 10.1002/eji.1830221004. [DOI] [PubMed] [Google Scholar]
- Fukushi N., Arase H., Wang B., Ogasawara K., Gotohda T., Good R.A., Onoe K. Thymusa direct target tissue in graft-versus-host reaction after allogeneic bone marrow transplantation that results in abrogation of induction of self-tolerance. Proc. Natl. Acad. Sci. USA. 1990;87:6301–6305. doi: 10.1073/pnas.87.16.6301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander G.A., Widmer B., Burakoff S.J. Loss of normal thymic repertoire selection and persistence of autoreactive T cells in graft vs. host disease. J. Immunol. 1994;152:1609–1617. [PubMed] [Google Scholar]
- Van Antwerp D.J., Martin S.J., Kafri T., Green D.R., Verma I.M. Suppression of TNF-α-induced apoptosis by NF-κB. Science. 1996;274:787–789. doi: 10.1126/science.274.5288.787. [DOI] [PubMed] [Google Scholar]
- Lo D., Reilly C.R., Burkly L.C., Dekoning J., Laufer T.M., Glimcher L.H. Thymic stromal cell specialization and the T-cell repertoire. Immunol. Res. 1997;16:3–14. doi: 10.1007/BF02786320. [DOI] [PubMed] [Google Scholar]