Abstract
Idiopathic pulmonary alveolar proteinosis (I-PAP) is a rare disease of unknown etiology in which the alveoli fill with lipoproteinaceous material. We report here that I-PAP is an autoimmune disease with neutralizing antibody of immunoglobulin G isotype against granulocyte/macrophage colony-stimulating factor (GM-CSF). The antibody was found to be present in all specimens of bronchoalveolar lavage fluid obtained from 11 I-PAP patients but not in samples from 2 secondary PAP patients, 53 normal subjects, and 14 patients with other lung diseases. It specifically bound GM-CSF and neutralized bioactivity of the cytokine in vitro. The antibody was also found in sera from all I-PAP patients examined but not in sera from a secondary PAP patient or normal subjects, indicating that it exists systemically in I-PAP patients. As lack of GM-CSF signaling causes PAP in congenital cases and PAP-like disease in murine models, our findings strongly suggest that neutralization of GM-CSF bioactivity by the antibody causes dysfunction of alveolar macrophages, which results in reduced surfactant clearance.
Keywords: autoantibody, granulocyte/macrophage colony-stimulating factor, pulmonary alveolar proteinosis, alveolar macrophage, surfactant protein
Pulmonary alveolar proteinosis (PAP) is a heterogeneous group of congenital and acquired diseases characterized by accumulation of excessive surfactant composed of phospholipids and surfactant proteins designated as surfactant protein (SP)-A, -B, -C, and -D in the alveoli and terminal bronchioli 1 2.
Most PAPs are acquired cases that predominantly affect adults, including idiopathic (I)-PAP and secondary (S)-PAP cases. S-PAP was reported in several clinical settings, such as pulmonary infection, hematologic malignancies, and inhalation of chemicals and minerals 3. The most common form is I-PAP, but its etiology is still not known. Standard therapy of the disease is whole lung lavage, which usually provides temporal symptomatic relief 4. The accumulation of surfactant protein is due to reduced surfactant clearance rather than excessive secretion, and SP-A specifically increases in the lungs of PAP patients as compared with other surfactant proteins 5 6. Because alveolar macrophages (AMs) catabolize SP-A 7, it was suggested that defective SP-A clearance in AMs caused PAP.
One kind of congenital form is associated with defective expression of the β chain of the GM-CSF receptor in hematopoietic cells 8. In mice, a defect in the gene for GM-CSF or the β chain of the GM-CSF receptor results in PAP-like disease with alveolar accumulation of surfactant 9 10. Thus, lack of GM-CSF signaling seems to cause AM dysfunction that leads to PAP.
Recently, we found a factor in the bronchoalveolar lavage fluid (BALF) from I-PAP patients that neutralized the bioactivity of GM-CSF 11. The factor directly bound GM-CSF and blocked its binding to GM-CSF receptors on the cells. Here we show that the factor is a neutralizing autoantibody directed against GM-CSF and present in the BALF and sera of patients with I-PAP. We propose that the autoantibody against GM-CSF is a causative agent for I-PAP.
Materials and Methods
Subjects.
We obtained BALF from 11 patients with I-PAP, 2 patients with S-PAP, 14 patients with other lung diseases (3 cases each of sarcoidosis and collagen vascular lung disease; 2 cases each of interstitial pneumonitis, hypersensitive pneumonitis, and eosinophilic pneumonia; and 1 case each of bronchiolitis obliterans organizing pneumonia and lung cancer), and 53 normal subjects. Diagnosis of PAP was based on biochemical analysis of BALF and histopathological findings of lung biopsy. The I-PAP patients had no history of hematological disorders, infectious diseases, or toxic inhalation. Two S-PAP patients were in the blast phase of chronic myelogenous leukemia. 5 of 11 I-PAP patients, 1 of 2 S-PAP patients, and 30 normal subjects underwent venipuncture to obtain sera at various periods after bronchoalveolar lavage. Written informed consent to participate in this study was obtained from all subjects.
Cytokines, Antibodies, and a Cell Line.
Recombinant human (rh)GM-CSF was provided by Kirin Brewery Co., Ltd. (Takasaki, Japan), and 125I–Bolton Hunter–labeled rhGM-CSF was purchased from NEN Life Science Products. rhIL-3 was purchased from R & D Systems, Inc. Biotinylated or nonlabeled rat anti–human GM-CSF mAb (BVD2-21C11 and BVD2-23B6, respectively) was purchased from PharMingen. Peroxidase-labeled rabbit anti–human IgA, -D, -E, -G, and -M polyclonal antibodies were purchased from DAKO Corp. A GM-CSF– or IL-3–dependent cell line, TF-1 12, was provided by Dr. Kitamura (The Institute of Medical Science, The University of Tokyo, Tokyo, Japan).
Blot Assay with 125I–GM-CSF.
Proteins in BALF or sera were subjected to SDS-PAGE using gradient gel (2–15%) under nonreducing conditions at 30 mA constant current for 150 min. Separated proteins were transferred electrophoretically to a polyvinylidene fluoride (PVDF) membrane at 12 V constant voltage for 75 min. The membrane was fixed with 10% (vol/vol) acetic acid and 50% (vol/vol) methanol, stained with Coomassie brilliant blue solution, washed with methanol, and treated with a blocking reagent (PBS supplemented with 1% [wt/vol] BSA and 0.1% [vol/vol] Tween 20) overnight at 4°C. The membrane was then incubated with 0.16 nM 125I–GM-CSF for 1 h at room temperature. After washing, the membrane was exposed to x-ray film for 4 d.
Competition Assay of GM-CSF Binding to the mAb in ELISA.
The method of this assay was described previously 11. In brief, after coating a micro-ELISA plate with anti–human GM-CSF mAb (BVD2-23B6), rhGM-CSF and BALF were incubated in the wells. rhGM-CSF bound to BVD2-23B6 antibody was detected using biotinylated anti–human GM-CSF mAb (BVD2-21C11) and streptavidin conjugated to horseradish peroxidase. Color was developed using tetramethylbenzidine, and the absorbance was measured at 450 nm using a microplate spectrometer (model 3550; Bio-Rad Labs.). Binding activity was calculated with the following equation: binding activity = 1 − detected GM-CSF (ng/ml)/applied GM-CSF (ng/ml).
Purification of the GM-CSF Binding Protein.
BALF was centrifuged at 1,000 g for 5 min. To remove lipoid materials, the supernatant was mixed vigorously with an equal volume of 1-butanol, and the mixture was centrifuged at 1,000 g for 5 min. After removing the butanol layer, the procedure was repeated. The aqueous layer was dialyzed against 10 mM ammonium acetate, pH 7.0, and lyophilized. Delipidated BALF was purified by using HiTrap SP column, a cation exchange column (equilibrated with 20 mM ammonium acetate, pH 6.0, and eluted with a linear sodium chloride gradient); HiTrap Q column, an anion exchange column (equilibrated with 20 mM Tris-HCl, pH 9.0, and eluted with a linear sodium chloride gradient); Superose 12 column, a gel filtration column (equilibrated with PBS containing 0.1% [vol/vol] NP-40 and eluted with the same buffer); RESOURCE Q column, an anion exchange column (equilibrated with 20 mM Tris-HCl, pH 9.0, and eluted with a linear sodium chloride gradient); and RESOURCE S column, a cation exchange column (equilibrated with 20 mM ammonium acetate, pH 6.0, and eluted with a linear sodium chloride gradient). All of these columns were from Pharmacia Biotech.
Purification of Igs.
Delipidated BALF was applied on recombinant protein A affinity column (Pharmacia Biotech) equilibrated with 20 mM sodium phosphate, pH 7.0. Ig bound to the column was eluted by pH gradient (pH 3.0–7.0).
NH2-terminal Sequencing of Protein.
NH2-terminal sequencing of protein was performed by the phenyl isothiocyanate method using the HP G1005A NH2-terminal protein sequencing system (Hewlett-Packard Bioscience Products).
Antigen Capture Assay to Determine the Isotype of the Antibody.
Various concentrations of Ig purified from BALF of an I-PAP patient (39–5,000 ng/ml) were transferred to micro-ELISA plates coated with 1 μg/ml rhGM-CSF, and the plate was kept at room temperature for 1 h. After washing, 0.3 μg/ml of peroxidase-labeled anti–human IgA, -D, -E, -G, or -M polyclonal antibody was added to each well and incubated at room temperature for 1 h. Color was developed using tetramethylbenzidine, and the absorbance was measured at 450 nm.
3-[4,5-Dimethylthiazol-2yl]-2,5-Diphenyltetrazolium Bromide Assay.
The method of this assay was described previously 13. In brief, TF-1 cells (2 × 104 cells/well) were incubated for 3 d with 1 ng/ml of rhGM-CSF or rhIL-3 and 1 μg/ml of Igs purified from BALF of an I-PAP patient. To the culture, 5 μg/ml of 3-[4,5-dimethylthiazol-2yl]-2,5-diphenyltetrazolium bromide (MTT; Sigma Chemical Co.) was added and incubated. After formation of formazan crystals, isopropanol/HCl was added to dissolve the crystal, and the absorbance was measured at 595 nm.
Results
Occurrence of GM-CSF Binding Factor in BALF.
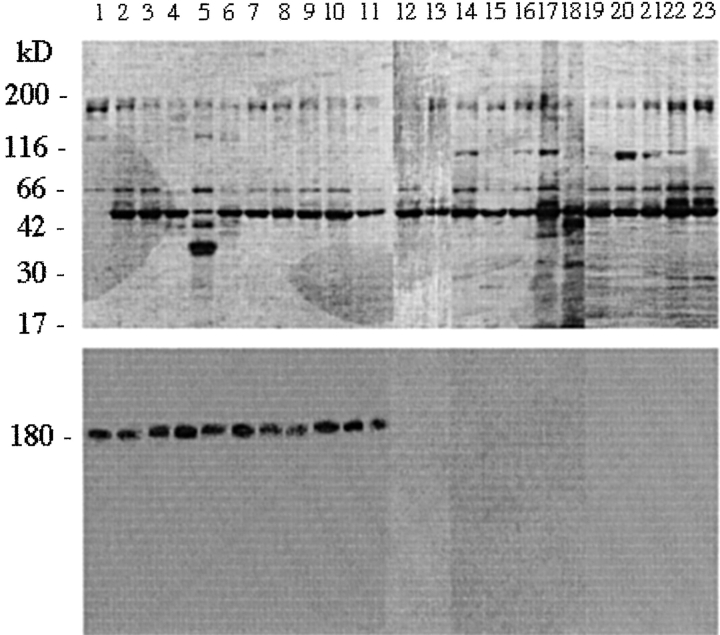
Occurrence of the GM-CSF binding factor in BALF supernatant was studied from 80 donors, including 11 I-PAP patients. As shown in Fig. 1, blot assay with 125I–GM-CSF gave a single band with a molecular mass of 180 kD in all I-PAP cases examined. In contrast, no band was detected in S-PAP patients, normal subjects, or patients with other lung diseases such as sarcoidosis, collagen vascular lung disease, interstitial pneumonitis, hypersensitive pneumonitis, and eosinophilic pneumonia.
Figure 1.
Occurrence of GM-CSF binding factor in BALF from I-PAP patients. Proteins in BALF from I-PAP patients (lanes 1–11), S-PAP patients (lanes 12–13), normal subjects (lanes 14–18), and patients with other lung diseases (namely sarcoidosis, lane 19; collagen vascular lung disease, lane 20; interstitial pneumonitis, lane 21; hypersensitive pneumonitis, lane 22; and eosinophilic pneumonia, lane 23) were subjected to SDS-PAGE under nonreducing conditions, stained with Coomassie blue (top panel), and assayed with 125I–GM-CSF (bottom panel). Molecular mass markers are shown at left (kD). Radioactive 180-kD bands are seen in all I-PAP samples but not in samples from S-PAP patients, normal subjects, or patients with other lung diseases. No such band was detected in BALF from an additional 48 normal subjects or 9 patients with other lung diseases.
Purification and Characterization of the GM-CSF Binding Factor.
The binding factor in BALF was purified by cation- and anion-exchange chromatography and gel filtration chromatography (Fig. 2 A). For evaluation of binding activity, a competition assay of GM-CSF binding to the mAb (BVD2-23B6) in ELISA was used. The purified protein showed a single band of 180 kD on SDS-PAGE under nonreducing conditions and two bands of 28 and 57 kD under reducing conditions (Fig. 2 B). 125I–GM-CSF binding to the purified 180-kD protein was confirmed by blot assay (Fig. 2 C), and bound 125I–GM-CSF was released when treated with citrate buffer, pH 2.0 (data not shown).
Figure 2.



Characterization of GM-CSF binding factor in BALF from I-PAP patients. Molecular mass markers are shown at left in A–E (kD). (A) Protein profiles of SDS-PAGE at each purification step (stained by silver stain). Delipidated BALF (lane 1) was purified using HiTrap SP (lane 2), HiTrap Q (lane 3), Superose 12 (lane 4), RESOURCE Q (lane 5), and RESOURCE S columns (lane 6). (B) SDS-PAGE of the purified protein under nonreducing (lane 1) and reducing conditions (lane 2). Stained by silver stain. (C) Coomassie blue staining (lanes 1 and 2) and GM-CSF binding activity (lanes 3 and 4) of crude (lanes 1 and 3) and purified factor (lanes 2 and 4). (D) GM-CSF binding activity of Ig isolated using recombinant protein A column. Protein profile stained with Coomassie blue (top panel) and results of 125I–GM-CSF binding (bottom panel) are shown. Lane 0, delipidated BALF; lanes 1–9, pass-through fractions; lanes 10–14, proteins eluted from column by changing pH gradient. (E) Competition of 125I–GM-CSF binding with nonradioactive GM-CSF. Lane 1, without nonradioactive GM-CSF; lanes 2 and 3, with 50- and 500-fold concentrations of nonradioactive GM-CSF, respectively.
The GM-CSF Binding Factor Is an Antibody against the Cytokine.
The 57-kD band was electroblotted onto a PVDF membrane and sequenced directly. The NH2-terminal sequence of the 57-kD protein was EVQLVESGGGLVQPGGSLRL, identical to the NH2-terminal sequence of human Ig H chain. The data suggest that the GM-CSF binding protein in the BALF is an antibody. To show that the binding factor is actually an antibody, Ig in BALF from an I-PAP patient was isolated using a recombinant protein A column. Ig eluted from the column by changing pH gradient showed 125I–GM-CSF binding activity (Fig. 2 D). Specificity of binding to GM-CSF was demonstrated by effective competition of 125I–GM-CSF binding with nonradioactive GM-CSF (Fig. 2 E). 125I–GM-CSF binding activity was not affected by the presence of nonspecific human Ig (data not shown).
Bioactivity of the Isolated Ig.
To confirm the bioactivity of isolated Ig, its inhibitory effect on growth of the TF-1 cell line was examined using the MTT assay. Growth of TF-1 cells is dependent on either GM-CSF or IL-3. The Ig purified from BALF inhibited GM-CSF–dependent growth of TF-1 cells but not IL-3–dependent growth (Fig. 3). The results indicate that the antibody inhibits growth of this cell line by neutralizing the bioactivity of GM-CSF.
Figure 3.

Inhibition of TF-1 cell growth by isolated Ig. Concentrations used: 1 ng/ml GM-CSF, 100 μg/ml delipidated BALF, 1 μg/ml isolated Ig, and 1 ng/ml IL-3.
The Isotype of the Autoantibody.
The isotype of the antibody was determined by antigen capture assay. The Ig captured by GM-CSF reacted with only anti–human IgG, whereas no other antiisotype antibody reacted, indicating that the isotype of the antibody is IgG (data not shown).
Presence of the Autoantibody in the Serum.
To know whether the I-PAP patients have circulating antibody against GM-CSF, we performed a blot assay with 125I–GM-CSF of sera from 36 donors, including 5 I-PAP patients, 1 S-PAP patient, and 30 normal subjects who underwent bronchoalveolar lavage during this study. Serum samples from all I-PAP patients showed a single 180-kD band, whereas no such band was detected in samples from the S-PAP patient and normal subjects (Fig. 4). Interestingly, the band was observed even in those from three patients who had entered remission and whose chest x-rays showed no opacity at the time of study. The isotype of the antibody in sera was also IgG (data not shown). These results indicate that the antibody is not limited to the lung but exists systemically in I-PAP patients.
Figure 4.

Occurrence of antibody against GM-CSF in sera from I-PAP patients. Proteins in sera from I-PAP patients (lanes 1–5), an S-PAP patient (lane 6), and normal subjects (lanes 7–11) were subjected to SDS-PAGE under nonreducing conditions, stained with Coomassie blue (top panel), and assayed for 125I–GM-CSF binding (bottom panel). Molecular mass markers are shown at left (kD). Radioactive 180-kD bands are seen in all I-PAP samples but not in samples from the S-PAP patient and normal subjects. No such band was detected in sera from 25 additional normal subjects.
Discussion
We have shown in this paper that autoantibody against GM-CSF is present in the lungs and sera of I-PAP patients but not in those of S-PAP patients, normal subjects, or patients with other lung diseases. Because GM-CSF is a key factor for maintaining the differentiation and proliferation of macrophages, dysfunction of AMs due to the neutralization of GM-CSF bioactivity by an autoantibody is a plausible explanation for the pathogenesis of human I-PAP. In fact, AMs from patients with active acquired PAP are known to be functionally impaired 14 15. Furthermore, one type of congenital PAP was known to be associated with a defect of the GM-CSF receptor, and in murine models, knockout of the gene for GM-CSF or its receptor induced PAP-like disease. The disease in these murine models was corrected by transgenic expression of GM-CSF in the pulmonary epithelia or bone marrow transplantation from wild-type mice 16 17.
It is increasingly understood that sera in some healthy and diseased individuals contain autoantibodies against cytokines. Natural antibodies have been reported against rh IL-1β, IL-2, IL-8, and TNF-α 18 19 20 21. Most of these autoantibodies were neutralizing antibodies and interfered with the binding of cytokines to receptors by simple competition 19 20 21. Recently, it was reported that anti–GM-CSF autoantibody was frequently detected in pharmaceutically prepared human IgG 22 and that 0.3–2% of sera had a low titer of anti–GM-CSF antibody 22 23. However, it was not reported that autoantibody against GM-CSF is associated with any disease or symptoms. Our results strongly suggest that I-PAP is an autoimmune disease with neutralizing autoantibody against the cytokine. As mentioned above, previous work in the patient case report and in mice has established that impaired production or action of GM-CSF can cause PAP. It is, therefore, reasonable to ascribe causality to the presence of autoantibody in the cases presented here, frequently and solely in the patients with I-PAP. This is, therefore, the first disease for which it can be argued that the cause is an autoantibody to a cytokine.
It is not clear at the time of this writing why autoantibody is generated in I-PAP patients. One possibility is that the autoantibody was provoked by a cross-reactive antigen, possibly from infectious pathogen(s). Alternatively, the autoantibody was generated to endogenously regulate GM-CSF bioactivity.
Although the functional consequences are predominantly manifest within the lung, our data suggest that the pathophysiologic disorder of I-PAP may originate from the systemic generation of autoantibody against GM-CSF. In this regard, recent clinical trials of GM-CSF administration to acquired PAP are intriguing 24. The hematopoietic response to GM-CSF in the patients was attenuated. The impaired response was not due to altered expression of GM-CSF receptor on PBMCs. It is possible that the administrated GM-CSF was neutralized by anti–GM-CSF antibody before it reached the target organs.
Finally, our observations have therapeutic implications. Whole lung lavage provides temporary remission in most cases, but additional lavage is required in more than 50% of patients 25. Measurement of the autoantibody in the lung after whole lung lavage may identify patients who require further therapy or who have risk for recurrence.
Acknowledgments
The authors thank T. Tomita, T. Nukiwa, A. Kurashima, T. Sakai, T. Abe, Y. Abe, T. Sugie, M. Niijima, K. Watari, M. Fujisawa, S. Kudoh, and A. Azuma for providing patient samples and clinical information. We are very grateful to W. Rom and M. Weiden for critical review of the manuscript and K. Arai, K. Akagawa, and S. Mori for valuable discussions.
References
- van Golde L.M.G., Batenburg J.J., Robertson B. The pulmonary surfactant systembiochemical aspect and functional significance. Physiol. Rev. 1988;68:374–455. doi: 10.1152/physrev.1988.68.2.374. [DOI] [PubMed] [Google Scholar]
- Kuroki Y., Voelker D.R. Pulmonary surfactant protein. J. Biol. Chem. 1994;269:25943–25946. [PubMed] [Google Scholar]
- Prakash U.B., Barham S.S., Carpenter H.A., Dines D.E., Marsh H.M. Pulmonary alveolar phospholipoproteinosisexperience with 34 cases and a review. Mayo Clin. Proc. 1987;62:499–518. doi: 10.1016/s0025-6196(12)65477-9. [DOI] [PubMed] [Google Scholar]
- Ramirez R.J. Alveolar proteinosisimportance of pulmonary lavage. Am. Rev. Respir. Dis. 1971;103:666–678. doi: 10.1164/arrd.1971.103.5.666. [DOI] [PubMed] [Google Scholar]
- Alberti A., Luisetti M., Braschi A., Rodi G., Iotti G., Sella D., Poletti V., Benori V., Baritussio A. Bronchoalveolar lavage fluids composition in alveolar proteinosis. Early changes after therapeutic lavage. Am. J. Respir. Crit. Care Med. 1996;154:817–820. doi: 10.1164/ajrccm.154.3.8810625. [DOI] [PubMed] [Google Scholar]
- Honda Y., Takahashi H., Shijubo N., Kuroki Y., Akino T. Surfactant protein-A concentration in bronchoalveolar lavage fluids of patients with pulmonary alveolar proteinosis. Chest. 1993;103:496–499. doi: 10.1378/chest.103.2.496. [DOI] [PubMed] [Google Scholar]
- Bates S.R., Fosfer A.B. Surfactant protein A is degraded by alveolar macrophages. Am. J. Physiol. 1996;271:L258–266. doi: 10.1152/ajplung.1996.271.2.L258. [DOI] [PubMed] [Google Scholar]
- Dirksen U., Nishinakamura R., Groneck P., Hattenhorst U., Nogee L., Murray R., Burdach S. Human pulmonary alveolar proteinosis associated with a defect in GM-CSF/IL-3/IL-5 receptor common β chain expression. J. Clin. Invest. 1997;100:2211–2217. doi: 10.1172/JCI119758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dranoff G., Crawford A.D., Sadelain M., Ream B., Rashid A., Bronson R.T., Dickersin G.R., Bachurski C.J., Mark E.L., Whitsett J.A. Involvement of granulocyte-macrophage colony stimulating factor in pulmonary homeostasis. Science. 1994;264:713–716. doi: 10.1126/science.8171324. [DOI] [PubMed] [Google Scholar]
- Nishinakamura R., Nakayama N., Hirabayashi Y., Inoue T., Aud D., McNeil T., Azuma S., Yoshida S., Toyoda Y., Arai K. Mice deficient for the IL-3/GM-CSF/IL-5 beta c receptor exhibit lung pathology and impaired immune response, while beta IL-3 receptor-deficient mice are normal. Immunity. 1995;2:211–222. doi: 10.1016/1074-7613(95)90046-2. [DOI] [PubMed] [Google Scholar]
- Tanaka N., Watanabe J., Kitamura T., Yamada Y., Kanegasaki S., Nakata K. Lungs of patients with idiopathic pulmonary alveolar proteinosis express a factor which neutralizes granulocyte-macrophage colony stimulating factor. FEBS Lett. 1999;442:246–250. doi: 10.1016/s0014-5793(98)01668-8. [DOI] [PubMed] [Google Scholar]
- Kitamura T., Tange T., Terasawa T., Chiba S., Kuwaki T., Miyagawa K., Piao Y.F., Miyazono K., Urabe A., Takaku F. Establishment and characterization of a unique human cell line that proliferates dependently on GM-CSF, IL-3, or erythropoietin. J. Cell. Physiol. 1989;140:323–334. doi: 10.1002/jcp.1041400219. [DOI] [PubMed] [Google Scholar]
- Mosmann T. Rapid colorimetric assay for cellular growth and survivalapplication to proliferation and cytotoxicity assays. J. Immunol. Methods. 1983;65:55–57. doi: 10.1016/0022-1759(83)90303-4. [DOI] [PubMed] [Google Scholar]
- Golde D.W., Territo M., Finley T.N., Cline M.J. Defective lung macrophages in pulmonary alveolar proteinosis. Ann. Intern. Med. 1976;85:304–309. doi: 10.7326/0003-4819-85-3-304. [DOI] [PubMed] [Google Scholar]
- Nugent K.M., Pesanti E.L. Macrophage function in pulmonary alveolar proteinosis. Am. Rev. Respir. Dis. 1983;127:780–781. doi: 10.1164/arrd.1983.127.6.780. [DOI] [PubMed] [Google Scholar]
- Nishinakamura R., Wiler R., Dirksen U., Morikawa Y., Arai K., Miyajima A., Burdach S., Murray R. The pulmonary alveolar proteinosis in granulocyte macrophage colony-stimulating factor/interleukins 3/5 βc receptor–deficient mice is reversed by bone marrow transplantation. J. Exp. Med. 1996;183:2657–2662. doi: 10.1084/jem.183.6.2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman J.A., Hull W.M., Dranoff G., Mulligan R.C., Whitsett J.A. Pulmonary epithelial cell expression of GM-CSF corrects the alveolar proteinosis in GM-CSF–deficient mice. J. Clin. Invest. 1996;97:649–655. doi: 10.1172/JCI118461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallay P., Mach J.-P., Carrel S. Characterization and detection of naturally occurring antibodies against IL-1α and IL-1β in normal human plasma. Eur. Cytokine Netw. 1991;2:329–338. [PubMed] [Google Scholar]
- Tiberio L., Caruso A., Pozzi A., Rivoltini L., Morelli D., Monti E., Balsari A. The detection and biological activity of human antibodies to IL-2 in normal donors. Scand. J. Immunol. 1993;38:472–476. doi: 10.1111/j.1365-3083.1993.tb02590.x. [DOI] [PubMed] [Google Scholar]
- Amiral J., Marfaing-Koka A., Wolf M., Alessi M.C., Tardy B., Boyer-Neumann C., Vissac A.M., Fressinaud E., Poncz M., Meyer D. Presence of autoantibodies to interleukin-8 or neutrophil-activating peptide-2 in patients with heparin-associated thrombocytopenia. Blood. 1996;88:410–416. [PubMed] [Google Scholar]
- Sioud M., Dybwad A., Jespersen L., Suleyman S., Natvig J.B., Forre O. Characterization of naturally occurring autoantibodies against tumor necrosis factor-alpha (TNF-α)in vitro function and precise epitope mapping by phage epitope library. Clin. Exp. Immunol. 1994;98:520–525. doi: 10.1111/j.1365-2249.1994.tb05522.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svenson M., Hansen M.B., Ross C., Diamant M., Rieneck K., Nielsen H., Bendtzen K. Antibody to granulocyte-macrophage colony-stimulating factor is a dominant anti-cytokine activity in human IgG preparations. Blood. 1998;91:2054–2061. [PubMed] [Google Scholar]
- Ragnhammar P., Friesen H.J., Frodin J.E., Lefvert A.K., Hassan M., Osterborg A., Mellstedt H. Induction of anti-recombinant human granulocyte-macrophage colony-stimulating factor (Escherichia coli-derived) antibodies and clinical effects in nonimmunocompromised patients. Blood. 1994;84:4078–4087. [PubMed] [Google Scholar]
- Seymour J.F., Begley C.G., Dirksen U., Presneil J.J., Nicola N.A., Moore P.E., Schoch O.D., van Asperen P., Roth B., Burdach S. Attenuated hematopoietic response to granulocyte-macrophage colony stimulating factor in patients with acquired pulmonary alveolar proteinosis. Blood. 1998;92:2657–2667. [PubMed] [Google Scholar]
- Goldstein L.S., Kavuru M.S., Curtis-McCarthy P., Christie H.A., Farver C., Stoller J.K. Pulmonary alveolar proteinosisclinical features and outcomes. Chest. 1998;114:1357–1362. doi: 10.1378/chest.114.5.1357. [DOI] [PubMed] [Google Scholar]