Abstract
The cellular basis of immunological memory remains a controversial area with respect to the identity of memory T cells and the role of persisting antigen. CD4 T cells are phenotypically divided by the expression of high and low molecular weight isoforms of CD45, surface markers that are frequently used to identify “naive” (CD45Rhigh) and “memory” (CD45Rlow) subsets. The latter subset responds rapidly in antigen recall assays but paradoxically has a short life span, a property that is difficult to reconcile with long-term memory. The present study examines these issues using a DTH (delayed-type hypersensitivity) model in which contact sensitivity to dinitrochlorobenzene (DNCB) was transferred to athymic nude rats by recirculating CD4 T cell subsets defined in the rat by the anti-CD45RC mAb OX22. As expected, CD45RC+ (but not RC−) CD4 T cells from normal unprimed rats transferred a DNCB-specific DTH response, whereas, 4 d after sensitization the CD45RC− (memory) subset alone contained the DNCB reactivity. However, when donor cells were collected from thymectomized rats sensitized two mo earlier, DNCB-specific responses were transferred by both CD45RC− and RC+ subsets suggesting that many of the latter had developed from cells with a memory phenotype. This was confirmed when CD45RC− CD4 T cells from 4-d primed rats were parked in intermediate nude recipients and recovered 2 mo later. DNCB-specific activity was now found wholly within the CD45RC+ “revertant” subset; the CD45RC− CD4 T cell population was devoid of activity. Importantly, we found that the total switch-back from CD45RC− to RC+ could be prevented, apparently by persisting antigen. The results indicate that there are two functionally distinct categories of memory T cells: one, a short-lived CD45Rlow type which orchestrates the rapid kinetics, the other, a longer-lived CD45Rhigh revertant which ensures that immunological memory endures.
Ahallmark of the immune response is memory, the ability to recall an earlier encounter with specific antigen, often years later, by producing a faster and larger response. A definitive investigation by Gowans and Uhr (1) using adoptive transfer, squarely laid the basis of immunological memory with recirculating lymphocytes recovered from the thoracic duct. At the time, it was generally accepted that immunological memory was vested in lymphocytes, which, after an initial antigen encounter, were imbued with the quality of long life (2). This view was challenged by the experiments of Gray and colleagues (3, 4) that suggested that the survival of both B and T memory cells depended critically on the persistence of antigen. The role that persisting antigen plays in maintaining memory has been reexamined recently for CD8 T cells specific for viruses (5–9). The balance of evidence suggests that in the absence of antigen, specific CD8 T cells may survive, although some argue that protective immunity by CD8 T cells ultimately depends on the persistence of antigen (8, 9). To what extent CD4 T cell memory is governed by residual antigen has not been resolved.
T cells stimulated by antigen undergo a number of welldescribed changes. The question is which of these, if any, are retained and can be used to identify memory T cells. The increased expression of CD44 after antigen stimulation has been used to identify CD8 and CD4 memory T cells in mice (10). In some mouse strains, but not others (11), CD44 remains high on CD8 T cells for many months (9, 11, 12), but the high density is not maintained on CD4 T cells (12). The idea that memory T cells exclusively recirculate to lymph nodes via afferent lymphatics (13, 14) is not supported by later studies that show that cells with a memory phenotype readily cross high endothelial venules within lymph nodes (15, 16). The downregulation of L-selectin (CD62L) (9, 17–19) and the increased expression of the α4 integrin subunit (CD49d) (9, 19) that alters migration have also been used as markers of memory T cells, but modulation of these adhesion molecules is reversible and closely linked with the activation state of the cell (9, 12, 18). The high and low molecular weight isoforms of CD45R are consistently used to identify naive and memory CD4 (but not CD8 [18]) T cells (20–22). CD45Rlow CD4 T cells have rapid in vitro antigen recall responses (23, 24) and are able to help primed B cells produce antibody (21, 22), functions which suggest memory T cells. Equating the CD45Rlow phenotype with memory, however, poses a dilemma. Whereas CD45Rhigh (naive) T cells are nondividing long-lived cells, the CD45Rlow subset tends to be a rapidly dividing, shortlived population (12, 27–29). Furthermore, CD45Rlow CD4 T cells upregulate Fas (CD95) and downregulate bcl-2 (30, 31), a phenotype associated with impending apoptosis. It is difficult to reconcile a short-lived cell with the fact that immunological memory endures.
The antigen-driven switch from CD45Rhigh to CD45Rlow (32, 33) was initially considered to be one-way (20, 23, 24). In vivo studies in rats (34) and subsequently in humans (27) indicated that CD45Rlow isoform expression was reversible. Although the time-frame for humans may be longer (29), the speed with which rat CD4 T cells could revert in vivo from CD45Rlow to CD45Rhigh was striking (28); a majority of CD4 T cells had switched back to the CD45Rhigh phenotype within a week. This implied that T cells that have previously encountered antigen, i.e., memory T cells, should be found in both CD45Rlow and CD45Rhigh subsets. Direct evidence for this supposition is lacking. It has also been suggested that persisting antigen could control CD45R isoform expression (35), but this issue has not yet been addressed for CD4 T cells.
In the present investigation, we used a delayed-type hypersensitivity (DTH)1 model in which a specific response to the contact sensitizing agent 2,4-dinitrochlorobenzene (DNCB) could be adoptively transferred to athymic nude rats by recirculating CD4 T cells. By using allotype-marked donor cells we were able to follow changes in CD45R isoform expression after transfer. The results demonstrated that antigen-experienced CD4 memory T cells revert en masse (default) from CD45Rlow to CD45Rhigh. Importantly though, residual antigen could prevent the total switchback from occurring.
Materials and Methods
Rats.
Congenic allotype-marked PVG-RT1u-RT7b and athymic PVG-RT1u-rnu/rnu(RT7a) nude rats were bred and maintained under conventional conditions in the Animal Unit, University of Manchester Medical School, and used at 2–3 mo of age. In some experiments PVG-RT1u -RT7b rats were thymectomized at 4–6 wk of age and rested for 1 mo before use.
Induction and Measurement of Contact Sensitivity.
Rats were sensitized by applying 200 μl of a 5% solution of DNCB (BDH Chemicals Ltd., Poole, UK) in ethanol on the shaven abdomen. On day 4 after sensitization rats were challenged by applying to both sides of the ear a total of 40 μl of a 1% solution of DNCB (400 μg) in ethanol to the left ear and 40 μl of ethanol only to the right ear. Ear thickness was measured 24 h after challenge (time of maximum response) using a spring-loaded engineer's micrometer (“ODITEST” ODI OOT; Kröplin GMBH, Hessen, Germany) by full release of the spring. The response was recorded as the difference in ear thickness between the left and right ears and expressed as μm ± SD. Differences between groups were compared using Student's t test.
Antibodies.
The following mAbs were used for cell separation and phenotyping: OX6 (anti-class II MHC), OX7 (anti-Thy-1), OX8 (anti-CD8), OX12 (anti-Igk chain), OX22 (anti-CD45RC), OX40 (against a molecule with some homology to CD40 and nerve growth factor receptor; present on activated CD4 T cells [36]), W3/25 (anti-CD4), R73 (anti-αβ TcR) and 8G6.1 (rat anti-RT7b; a gift from Dr. Simon Hunt, Oxford). Mouse mAbs were detected with FITC-conjugated F(ab′)2 rabbit anti–mouse Ig (Dako Ltd., High Wycombe, UK) absorbed extensively against rat Ig. Biotinylated mAbs were detected with phycoerythrinstreptavidin (Sera-lab, Cowley, UK). Mouse mAbs were purchased from Serotec (Bicester, Oxon, UK) or produced as ascites in the laboratory by injecting the relevant hybridoma into pristaneprimed Balb/c mice. The R73 clone (37) was a gift from Prof. T. Hünig (Würzburg, Germany). Other hybridoma cell lines were provided by ECAAC (Porton Down, UK). The dual fluorescence staining technique used to phenotype allotype-marked (RT7b) donor cells after transfer to wild-type (RT7a) recipients was described elsewhere (28).
Cell Separation.
Lymphocytes from lymph nodes (LN) or the thoracic duct (TDL) were incubated for 30 min at 4°C with saturating concentrations of OX6, OX8, OX12, and OX7 (to remove B cells, CD8 T cells and CD45RC− Thy-1+ recent thymic emigrants [38]), washed in Dulbecco's phosphate buffered saline supplemented with mineral salts A and B (Oxoid Ltd., Basingstoke, UK) plus 2% fetal calf serum and mixed on a roller/rocker for 30 min at 4°C with goat anti–mouse IgG–coated Biomag™ particles (Metachem Diagnostics Ltd., Piddington, UK). The resulting rosettes were removed from suspension by a magnet (Dynal Ltd., New Ferry, UK) applied to the wall of the container. The remaining CD4 T cells (>98% CD4+; FITC-conjugated W3/25) were incubated with saturating concentrations of mAb OX22 (anti-CD45RC), positively selected onto goat anti-mouse– coated Biomag™ particles, the cell/particle rosettes washed free of unbound CD45RC− cells, resuspended at appropriate concentrations and the CD45RC+ CD4 T cells injected intravenously with particles attached. The unbound nonrosetting cells were restained with OX22, mixed with Biomag™ particles and depleted of mAb-stained cells as above by 2 or 3 rounds of magnetic adhesion. The CD45RC− CD4 T cells (>98% pure) were injected intravenously.
Adoptive Transfer of DNCB Response.
Purified CD4 T cells or CD45RC+ and RC− subsets were collected from allotypemarked (RT7b) PVG-RT1u-RT7b euthymic donors and a standard dose of 10 × 106 T cells transferred intravenously to PVGRT1u (RT7a) athymic nude rats. Recipients were skin-sensitized 3 wk after transfer, unless otherwise indicated, ear-challenged 4 d later and ear thickness always measured after 24 h.
Results
Kinetics of Response in Euthymic Rats.
The DNCB-induced DTH response, recorded as the difference between left (DNCB in ethanol) and right ears (ethanol only control), was always recorded 24 h after ear-painting, i.e., challenge. To determine the kinetics of the response, rats were sensitized, i.e., DNCB applied to the abdomen, and ear-challenged on days 1–18. The maximum response to challenge (410 μm ± 82) was induced 4 d after primary sensitization and declined if challenge was delayed further. The response to DNCB subsided rapidly to a plateau of around 120 μm by day 8, a typical response pattern reported by others (39).
Adoptive Transfer to Nude Recipients.
A series of experiments showed that the DNCB response could be adoptively transferred to athymic PVG-RT1u nude rats by whole LN cells or by CD4 T cells purified from TDL of unprimed PVG-RT1u rats. To standardize the procedure, we opted to transfer 10 × 106 T cells 3 wk before sensitization, an interval designed to allow donor T cells to spontaneously proliferate in nude recipients (40). Ears were always challenged 4 d after sensitization and ear thickness measured 24 h later. The assay was designed to identify the presence or absence of DNCB-specific T cells in the cell inoculum and, within limits, the size of the response was cell dose dependent (data not shown).
In the rat CD4 T cells are divided into two functionally distinct subsets by the anti-CD45RC mAb OX22 (25, 26) that detects an epitope on the C exon product of CD45R (41). Exon C is one of three (A, B, or C) that can be variably spliced out of the CD45R molecule by posttranslational mRNA transcription (42, 43) and is expressed (CD45RC+) by three-quarters of the rat CD4 T cell population (25, 34). T cells emerge from the thymus (recent thymic emigrants, RTE) with the phenotype CD45RC− Thy-1+ and develop within a week into mature CD45RC+ Thy-1− T cells (38, 44). Thus, CD45RC− CD4 T cells in the periphery are a mixture of immature Thy-1+ RTE (40%) and mature Thy-1− antigen-experienced T cells (60%) (45) derived from the CD45RC+ subset (32, 38). To avoid ambiguity, RTE were always removed from the CD45RC− subset during purification.
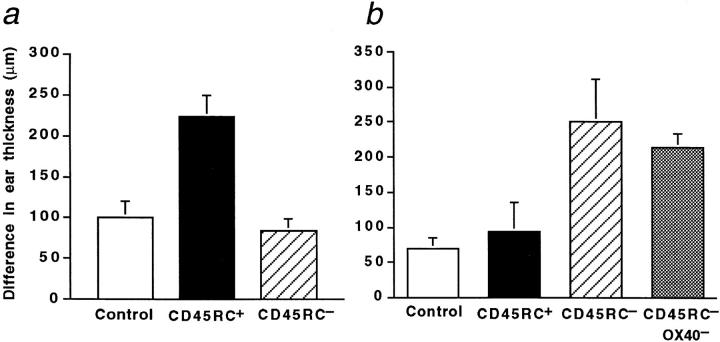
Using T cell subsets purified from TDL of unprimed rats, the DNCB response was transferred to nude recipients by the CD45RC+ subset alone, as expected; the CD45RC− subset from unprimed rats lacked T cells specific for DNCB (Fig. 1 a). To show that specific antigen altered isoform expression, CD45RC+ and RC− subsets were purified from TDL of DNCB-primed rats 4 d after sensitization, a time at which ear-challenge would normally induce immediate ear swelling. Fig. 1 b shows that the DNCB response was now transferred with the CD45RC− subset alone. Note, however, that in contrast with the experiment in Fig. 1 a, nude recipients in Fig. 1 b were ear-challenged immediately (instead of at 3 wk) after cell transfer, a protocol that also demonstrated that the CD45RC− subset was responsible for the effector stage of the response. Although recently stimulated, the DNCB-responding T cells were not in a state of hyperacute activation. For example, the purified CD45RC− subset displayed size and granularity characteristics that were indistinguishable from small lymphocytes (15). Furthermore, depleting the CD45RC− subset of OX40+ cells, a marker of activated T cells in the rat (36), did not significantly reduce the adoptively transferred DTH response (Fig. 1 b). This evidence is compatible with the notion that the low molecular weight isoform of CD45R marks memory T cells (20–24, 32, 33).
Figure 1.
DNCB-specific CD4 T cells are found exclusively in the CD45RC+ subset of unprimed rats but after sensitization reside in the CD45RC− subset. The latter transfers the effector stage of the DTH response. (a) PVG-RT1u athymic nude rats received no cells (control) or were injected intravenously with 10 × 106 CD45RC+ or 10 × 106 CD45RC− CD4 T cells, purified from TDL of unprimed PVG-RT1uRT7b rats. Nude rats were sensitized after 3 wk, ear-challenged 4 d later, and ear thickness measured after 24 h. Histograms represent means ± SD 4, 6, or 4 rats per group (left to right). Test of significance: control vs CD45RC+, P <0.001. (b) PVG-RT1u nude rats received no cells (control) or were injected with 110 × 106 CD45RC+, 50 × 106 CD45RC− or 50 × 106 CD45RC−/OX40− CD4 T cells purified from LN or TDL of 4-d sensitized PVG-RT1u-RT7b rats. LN and TDL results were pooled as no difference was found between them. Rats were ear-challenged immediately after cell transfer and ear thickness measured 24 h later. Histograms are means ± SD of 4, 9, 7 or 4 rats per group (left to right). Test of significance: control vs CD45RC+, NS (not significant P >0.05); vs CD45RC− or CD45RC−/OX40−, P <0.001; CD45RC− vs CD45RC−/OX40−, NS.
Antigen-specific CD45RC− CD4 T Cells Revert to CD45RC+.
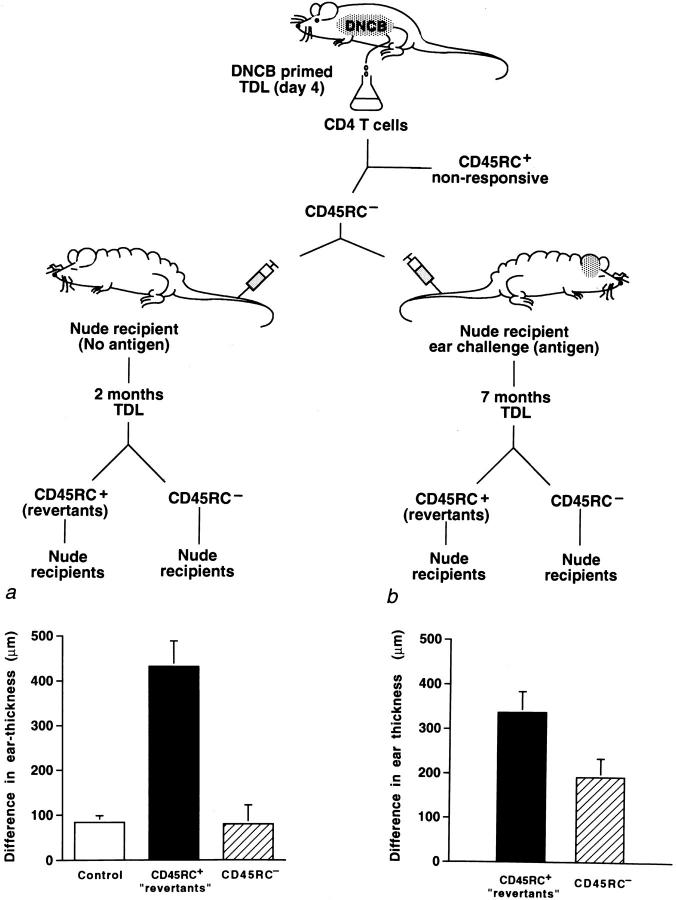
Investigations based on whole cell populations, but with no regard for antigen specificity, have indicated that CD45RC− T cells (and comparable CD45RA− RO+ T cells in humans) will reexpress with time the high molecular weight isoform (CD45RC+ in rats; CD45RA+ in humans) both in vitro (46–49) and in vivo (27–29, 34, 45). However, there is no clear demonstration that such a reversion (from a memory to a naive phenotype) will occur within an antigen-specific population in vivo. Therefore, we determined whether DNCB-specific memory T cells remained CD45RC− or could revert to CD45RC+ with time. To exclude a contribution of newly generated naive CD45RC+ CD4 T cells from the thymus, animals were thymectomized. 2 mo after sensitization, CD45RC+ and RC− subsets were obtained from TDL and adoptively transferred to nude recipients (Fig. 2 a). Over half the DNCB-specific activity was now found within the CD45RC+ subset (Fig. 2 b), suggesting that antigen-specific T cells had switched back from a CD45RC− state. It was also clear that at 2 mo, the CD45RC− subset still retained a large population of DNCB-specific T cells.
Figure 2.
Evidence that antigen-experienced DNCB-specific CD45RC− CD4 T cells revert to a CD45RC+ phenotype in DNCB-sensitized rats. Donor rats (thymectomized) were sensitized with DNCB, TDL collected 2 mo (a, b) or 4 d (c, d) later, separated into CD45RC+ and CD45RC− subsets and 10 × 106 (or 50 × 106 as indicated) T cells transferred to athymic nude rats. Recipients were reconstituted for 3 wk (b) or for 2 mo (d), sensitized, earchallenged 4 d later and ear thickness measured after 24 h. Histograms represent means ± SD of 3 or 4 rats in each group. Test of significance: (b) CD45RC+ vs CD45RC−, P <0.02.
This experiment does not exclude the possibility that the response generated by the CD45RC+ subset at 2 mo could have originated from residual naive T cells not stimulated during the primary sensitization. We asked, therefore, how efficient was the sensitization in converting naive T cells to a CD45RC− phenotype. At day 4 after sensitization CD4 T cells were separated into CD45RC+ and RC− subsets and transferred to nude recipients (Fig. 2 c), but not immediately challenged (unlike the experiment in Fig. 1 b). 2 mo later the reconstituted nude recipients were sensitized and ear-challenged. The results demonstrated that virtually all the DNCB-specific activity at day 4 after priming was confined within the CD45RC− subpopulation (Fig. 2 d); five times as many CD45RC+ CD4 T cells failed to transfer a significant DTH response. Thus, by day 4, the CD45RC+ subset was essentially devoid (clonally depleted) of DNCBspecific T cells. Hence, the reappearance of DNCB activity within the CD45RC+ subset at 2 mo strongly suggested that specific T cells reverted from the CD45RC− subset.
To investigate more conclusively whether antigen-experienced memory T cells can revert from CD45RC− to RC+, highly purified CD45RC− CD4 T cells (>98.0% pure) from 4-d sensitized rats were “parked” in athymic nude recipients until retransfer (Fig. 3, left protocol). Approximately 60% of the donor-derived population (carrying the RT7b allotype marker) subsequently re-expressed the high molecular weight isoform (CD45RC+) (e.g., 34, 35). Donor-derived CD45RC+ revertants and CD45RC− CD4 T cells were recovered from TDL of the intermediate nude rats after 2 mo, purified and re-transferred to secondary nude recipients. Surprisingly, the DNCB-specific response was contained entirely within the CD45RC+ subset (Fig. 3 a). No specific DTH activity remained within the CD45RC− subset; an equal number of retransferred CD45RC− CD4 T cells gave a response that was indistinguishable from the negative control. Clearly antigen-specific memory T cells survived in the complete absence of antigen, but all expressed the CD45RC+ phenotype.
Figure 3.
Antigen-experienced CD45RC− CD4 T cells that transfer a DNCB-specific DTH response revert completely to CD45RC+ in nude recipients, a change that was inhibited by residual antigen. CD45RC− CD4 T cells were purified from TDL of rats sensitized 4 d before with DNCB and adoptively transferred into intermediate nude recipients. TDL were recovered (a) 2 mo later (left protocol) or (b) 7 mo later from DNCB ear-challenged intermediate nude rats (right protocol), separated into CD45RC+ revertants and CD45RC− CD4 T cells and transferred (10 × 106 cells/recipient) into secondary nude rats. These were sensitized with DNCB after 3 wk and ear-challenged 4 d later. Ear thickness was measured after 24 h. Histograms are means ± SD of 4, 4, 2, 4, and 4 (left to right) rats per group. Test of significance: (a) control vs CD45RC+, P <0.001; CD45RC+ vs CD45RC−, P <0.01; (b) CD45RC+ vs CD45RC−, P <0.01.
Because the switch-back was so decisive, we asked whether the DNCB-specific activity remaining in the CD45RC− subset of the previous experiment (Fig. 2 a) could have been caused by persisting antigen. To test this idea, CD45RC− CD4 T cells (>98.5% pure) were transferred into intermediate nude recipients as before, except that the animals were ear challenged on the day of transfer. The T cell–injected nude rats were those from the experiment in Fig. 1 b; they received no other source of antigen. 7 mo later donor-derived CD4 T cells were recovered from TDL, purified into CD45RC+ and RC− subsets, and transferred into secondary nude recipients. After 3 wk, these animals were sensitized and ear challenged in the standard way (Fig. 3, right protocol). Again, a majority of antigen-experienced memory T cells reverted to a CD45RC+ phenotype. However, a significant number of DNCB-specific T cells were still found within the CD45RC− subset. This suggests that residual antigen was preventing antigen-experienced CD45RC− T cells from defaulting to a CD45RC+ state. Furthermore, the results indicate that there are two distinct categories of memory CD4 T cells, one CD45RC− the other CD45RC+.
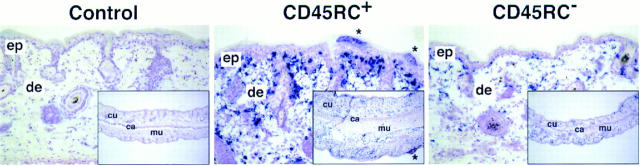
CD4 T Cell Infiltration.
The ears of DNCB challenged nude recipients were examined immunohistochemically for the presence of donor-derived CD4 T cells, i.e., those staining positive for the RT7b allotype marker. Representative samples from the experiment in Fig. 3 a are illustrated in Fig 4. The ears of uninjected nude controls, which showed no net increase in ear thickness, were devoid of allotypemarked cells. In contrast, recipients' ears of CD45RC+ revertants were heavily infiltrated; donor T cells were abundant in the greatly thickened dermis and epidermis. Curiously, all samples in this group had numerous consolidated foci on the outer surface of the epidermis containing dense collections of polymorphonuclear leukocytes. The increased ear thickness, induced by the CD45RC+ revertants and measured in situ, was clearly visible in cross section (Fig. 4, insets). The ears of nude rats injected with nonresponsive CD45RC− CD4 T cells, lacking DNCB-specific T cells, were also infiltrated with donor-derived CD4 T cells, but to a lesser extent. Clearly, both DNCB-specific and nonspecific CD4 T cells had ready access to the ear, but only the former induced changes (presumably by cytokine release) that caused a local increase in ear thickness.
Figure 4.
Donor-derived CD4 T cells infiltrate the ears of DNCB-challenged, T cell reconstituted nude rats. Ears from uninjected nude rats (Control) or from nude rats injected with CD45RC+ revertants or with unresponsive CD45RC− T cells (all taken from rats of experiment Fig. 3 a at 48 h) were snap frozen, sectioned, and stained for the presence of RT7b allotype-marked donor cells as described elsewhere (50). There was a heavy infiltrate of donorderived CD4 T cells in the dermis (de) and epidermis (ep) of recipients reconstituted with CD45RC+ revertant T cells and the surface of the epidermis showed necrotic foci (*) containing numerous polymorphonuclear leukocytes. In cross section, the ears were swollen, more cellular, and increased in thickness compared with ears from control and CD45RC− T cell–injected nude rats (insets). The ears of the latter recipients showed a modest infiltrate of donor-derived cells but were not swollen. Original magnification ×80; inset ×10. cu, cutis; ca, cartilage; mu, muscle. The immunostaining and photographs were kindly provided by K. Bankes-John and Jürgen Westermann, Hannover, Germany.
Response of CD45RC+ CD4 T Cell Revertants.
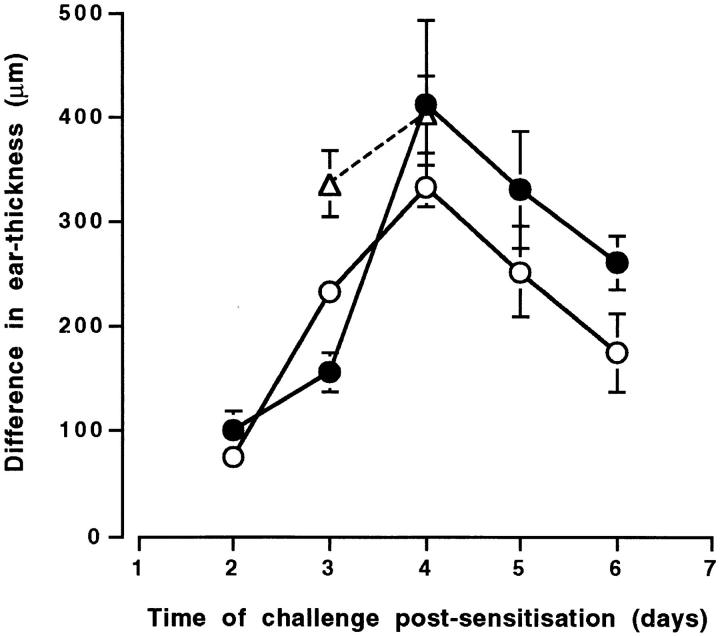
An important question arises as to whether CD45RC+ revertants display characteristics similar to or different from truly naive antigen-inexperienced CD45RC+ T cells. Available evidence suggests that CD45RC+ “revertants” behaved like unprimed T cells. For example, when revertants were collected from 2-mo primed thymectomized rats, transferred to nude recipients and challenged immediately (a measure of effector cell potential), they were unable to evoke a DTH response (CD45RC+: 74 μm ± 17; control: 62 μm ± 15). In addition, the kinetics of the DTH response in sensitized rats was comparable with that of rats resensitized 6.5 or 8 wk after primary sensitization. Once- or twice-primed rats were ear challenged on various days after sensitization. When compared with the once-primed animals, the kinetics of the DNCB responses in twice-primed rats were remarkably similar (Fig. 5). The peak responses occurred at day 4 in both once- and twice-primed rats suggesting, but not proving, that CD45RC+ revertants responded with primary kinetics. There was, however, a significant increase in the response at day 3 after secondary sensitization (P <0.001). Although not proven, this early increase could be due to DNCB-specific CD45RC− CD4 T cells in sensitized rats being retained in an upregulated state by persisting antigen.
Figure 5.
The kinetics of the DNCB response in once- or twiceprimed rats is similar. Rats were sensitized with DNCB on day 0 and earchallenged at various times after sensitization (closed circles) or were sensitized with DNCB a second time at 6.5 wk (open triangles) or 8 wk (open circles) and ear-challenged at the times indicated. Each point is the mean ± SD of 3–5 rats. The twice-primed rats were thymectomized before sensitization.
Discussion
The main conclusions of the present investigation were (a) that antigen-specific CD4 T cells, which expressed a low molecular weight isoform (CD45RC−) after antigen encounter, reexpressed the high molecular weight isoform (CD45RC+) in large numbers, (b) that, in the absence of antigen, the switch back was total and (c) that persisting antigen could prevent reversion. Since both CD45RC+ and RC− subsets represent functionally distinct populations, the results indicate that there are two major types of antigenexperienced CD4 memory T cells.
CD4 T cells are pivotal in the immune response in that they control the development and activation of B cells, CD8 T cells, macrophages and other inflammatory cells. Assessing the response of memory CD4 T cells in vivo is consequently indirect (antibody production, cytotoxicity, intracellular killing, inflammation, infiltration, swelling). Although primary sensitization occurs centrally within draining LNs (51, 52), we presume that the ear swelling measured here is the culmination of factors released by antigen-specific CD4 T cells exposed locally to DNCB. A number of studies in mice have shown that contact sensitivity is mediated by CD4 T cells (39, 53), although recent investigations have linked the effector stages with CD8 T cells (54). In our experiments the effector stage of the response was transferred to nude rats by antigen-experienced CD45RC− CD4 T cells and donor-derived CD4 T cells were identified in large numbers within the inflamed ears (Fig. 4). We have not rigorously excluded a role for CD8+ T cells, but, if involved, they must be of extrathymic origin (55) and subservient to CD4 T cells.
In unprimed naive rats, DNCB-specific CD4 T cells were found only within the CD45RC+ subset; the CD45RC− compartment was devoid of reactivity. In contrast, after acute sensitization, DNCB-primed T cells were concentrated in the CD45RC− population. Neither of these observations was unexpected and confirm what others have shown (9, 18, 32, 33). What has not been highlighted before was the completeness of the isoform switch. It was known from earlier work that antigen rapidly recruited specific lymphocytes into secondary lymphoid tissues, effectively removing them for a period of time from the recirculating pool (56– 58). Our evidence suggested that recruitment was highly efficient and that the entire DNCB-specific population switched from CD45RC+ to RC− by day 4 after sensitization. Consequently, the CD45RC+ subset became negatively selected, devoid of DNCB-specific T cells. Nude recipients injected with this depleted CD45RC+ subset never developed a DNCB response, even many months after reconstitution.
One of the primary aims of the investigation was to determine whether antigen-specific T cells, once induced to express the low molecular weight isoform, returned to a CD45RC+ naive phenotype. That DNCB-specific CD45RC− CD4 T cells did revert was shown in two different systems: thymectomized rats and subset-reconstituted nude recipients.
The total switch from CD45RC+ to RC− 4 d after sensitization, followed by a return of the majority of DNCBspecific T cells to the CD45RC+ state 2 mo later (Fig. 2 a), clearly argues for a switch-back. Although unlikely, it was difficult to exclude the possibility, first, that a few CD45RC+ DNCB-specific T cells escaped priming and formed the basis of the revertant population. Second it was suggested from DNA (Brdu) labeling studies that CD45RBhigh T cells (the mouse equivalent of rat CD45RC+ T cells) might divide without changing phenotype (12). Third, it was not possible to exclude the effect of persisting antigen. Therefore, the switch-back was tested in more decisive experiments. Highly purified 4 d primed CD45RC− CD4 T cells were parked in intermediate nude rats in which the influence of persisting antigen could be eliminated. The unambiguous and complete reversion of DNCB-specific T cells in the absence of antigen exceeded our most optimistic expectations. Using intermediate nude recipients, we also found that ovalbumin-primed CD45RC− CD4 T cells which helped primed B cells produce specific antibody, reverted to a CD45RC+ state (Bell, E.B., S. Hayes, and C. Bunce, unpublished observation). More importantly, though, the DNCB studies showed for the first time that residual antigen could prevent CD45RC− to RC+ reversion.
It was remarkable that a nonreplicating antigen continued to exert an influence on the DNCB-specific CD4 T cell population even 7 mo after application. This observation could explain the difficulty, e.g., in a human context, of demonstrating that antigen-experienced CD45RO T cells revert to a CD45RA state. In practice the organism may never rid itself of residual antigen. Others have hypothesized that once primed, T cells may be readily activated and could be maintained in a CD45Rlow memory state by restimulation with low affinity cross-reacting antigens (59). The fact that the DNCB-specific population reverted in its entirety to a naive phenotype indicates that, at least for this antigen, putative cross-reacting antigens played no demonstrable role. Given that specific antigen was found to exert a long-term effect, it is not necessary to hypothesize a role for cross-reacting antigen.
Earlier evidence from whole populations indicated that isoform exchange was cyclic (28). Thus, a switch between CD45RC+ and RC− could occur more than once, perhaps governed by chance encounter with retained antigen. This proposed pattern of events coincides with the known turnover of the two subsets (12, 28). The CD45RBhigh subset in mice was shown to be comprised largely of long-lived cells in interphase, whereas a majority of the CD45RBlow fraction was rapidly dividing and incorporated Brdu (12). A small but significant fraction of resting CD45RBhigh cells was also labeled with Brdu (12, 60). The present results would indicate that the labeled CD45RBhigh cells were likely to be revertants, rather than “T cells which divided without losing their naive phenotype” (12). Life span studies in humans based on cells bearing radiation-induced dicentric chromosomes (27, 29) and in rats after the loss of transferred allotype-marked CD4 T cells (28) both reached the same conclusion: CD45RA+ (human) or CD45RC+ (rat) T cells were long-lived; CD45RA− (CD45RO+) or CD45RC− T cells were short-lived. It is important to note that turnover of human lymphocytes was measured in months, not days as in rodents, reflecting the considerable difference in life span between these species.
If CD45Rlow T cells were to be the sole purveyors of memory, it becomes difficult to reconcile the long duration of functional memory in vivo with the known characteristics of the CD4 CD45Rlow subset. We think the present observations resolve this paradox. There are two types of CD4 memory T cells: (a) memory T cells (CD45Rlow) that respond quickly (24), upregulate adhesion molecules, migrate differently (13–15, 21) but survive less well (12, 27– 31) and (b) the antigen-experienced revertants that regain a full resting state and migrate conventionally but endure. The former contributes the qualitative attribute (speed) of the classical memory response, the latter only the quantitative element. This idea (35) has also been supported by others (61).
What, therefore, is the nature of the CD45RC+ revertants? Have they been changed by their previous encounter with antigen? We have been unable to find any phenotypic or functional characteristics that distinguish the revertants from CD45RC+ CD4 T cells that have never seen antigen. For example CD45RC+ revertants regain their ability to induce graft-versus-host responses (34, 46). CD44 and L-selectin (CD62L), markers associated with activated CD8 memory T cells (6, 9, 10, 18, 19), were not decisive in the rat. CD44 expression in the rat was not significantly upregulated in the CD45RC− CD4 T cell subset and was similar in this regard with certain mouse strains (11). With respect to L-selectin, essentially all CD45RC+ CD4 T cells, which would include revertants, and two thirds of the CD45RC− subset were L-selectinhigh (mAb HRL-1 and HRL-2 [62]). The populations of CD45RC− T cells defined by high and low expression of L-selectin are under investigation. A detailed assessment of mRNA encoding splice variants of CD45R (using reverse transcription and the polymerase chain reaction) showed that revertants were identical with truly naive CD4 T cells, generated from recent thymic emigrants (Hargreaves, M., and E.B. Bell, manuscript submitted for publication). When DNCB-primed rats were resensitized, the kinetics of the new response were the same as those in once-primed animals (Fig. 5). However, we do not know whether the revertant T cells remained committed to the cytokine profile (Th1 or Th2) induced by DNCB. Others reported that the cytokine patterns of resting memory CD4 T cells were permanently polarized (22). However, the antigen-primed transgeneic T cells used in that study remained CD45RBlow and never returned to the CD45RBhigh phenotype described in the present investigation.
There is no theoretical constraint that would conflict with the contention that revertant memory T cells adopt their former naive characteristics. Revertants would qualify as memory cells by virtue of the fact that they have seen antigen and clonally expanded. Recent experiments (Bunce, C., and E.B. Bell, unpublished) showed that DNCB-specific CD4 T cells increased three- to fivefold among the CD45RC+ revertant population. An increase in frequency of antigen-specific T cells after antigen stimulation was clearly documented for CD8 T cells (63–65) and many of these down-regulated activation molecules with time (9, 18, 19).
The present results afford a new perspective on the role of persisting antigen in the maintenance of immunological memory. Persisting antigen ensures an accelerated response by CD45Rlow T cells and the ability of these to migrate into non-lymphoid sites, qualities important for functional protection against, e.g., viruses (9, 65). Should antigen disappear entirely, memory T cells simply revert to a quiescent state and decay more slowly; for some infections, quantity may be more important than speed. Immunity is not, of course, always permanent and failure to protect could be a consequence of T cells merely downregulating their activation state or be due to the eventual loss of the CD45Rhigh resting population itself. We suggest, therefore, that the amount of persisting antigen could apportion the distribution of specific T cells between the two subsets and determine the precise character of the secondary response, balancing the desirability of rapid onset against the need to retain a high frequency of specific cells with which to combat an infrequent antigenic insult.
Acknowledgments
We would like to thank Ian Townsend and Neil Yates for maintaining the nude rat colony, Professor Jürgen Westermann for valuable discussions, Mr. K. Bankes-John (Hannover, Germany) for providing the immunohistology and Sheila Sparshott for reviewing the manuscript.
Footnotes
The work was supported by grants (to E.B. Bell) from the UK Medical Research Council and The Arthritis & Rheumatism Council.
1 Abbreviations used in this paper: DNCB, 2,4-dinitrochlorobenzene; DTH, delayed-type hypersensitivity; TDL, thoracic duct lymphocytes.
References
- 1.Gowans JL, Uhr JM. The carriage of immunological memory by small lymphocytes in the rat. J Exp Med. 1966;124:1017–1030. doi: 10.1084/jem.124.5.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sprent J, Miller JFAP. Fate of H2-activated T lymphocytes in syngeneic hosts. III. Differentiation into longlived recirculating memory cells. Cell Immunol. 1976;21:314–326. doi: 10.1016/0008-8749(76)90059-9. [DOI] [PubMed] [Google Scholar]
- 3.Gray D, Skarvall H. B-cell memory is short-lived in the absence of antigen. Nature (Lond) 1988;336:70–73. doi: 10.1038/336070a0. [DOI] [PubMed] [Google Scholar]
- 4.Gray D, Matzinger P. T cell memory is shortlived in the absence of antigen. J Exp Med. 1991;174:969–974. doi: 10.1084/jem.174.5.969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Müllbacher A. The long-term maintenance of cytotoxic T cell memory does not require persistence of antigen. J Exp Med. 1994;179:317–321. doi: 10.1084/jem.179.1.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lau LL, Jamieson BD, Somasundaram T, Ahmed R. Cytotoxic T-cell memory without antigen. Nature (Lond) 1994;369:648–652. doi: 10.1038/369648a0. [DOI] [PubMed] [Google Scholar]
- 7.Hou S, Hyland L, Ryan KW, Portner A, Doherty PC. Virus-specific CD8+T-cell memory determined by clonal burst size. Nature (Lond) 1994;369:652–654. doi: 10.1038/369652a0. [DOI] [PubMed] [Google Scholar]
- 8.Oehen S, Waldner H, Kündig TM, Hengartner H, Zinkernagel RM. Antivirally protective cytotoxic T cell memory to lymphocytic choriomeningitis virus is governed by persisting antigen. J Exp Med. 1992;176:1273–1281. doi: 10.1084/jem.176.5.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zimmermann C, Brduscha-Riem K, Blaser C, Zinkernagel RM, Pircher H. Visualization, characterization, and turnover of CD8+memory T cells in virus-infected hosts. J Exp Med. 1996;183:1367–1375. doi: 10.1084/jem.183.4.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tabi Z, Lynch F, Ceredig R, Allan JE, Doherty PC. Virus-specific memory T cells are Pgp-1+and can be selectively activated with phorbol ester and calcium ionophore. Cell Immunol. 1988;113:268–277. doi: 10.1016/0008-8749(88)90026-3. [DOI] [PubMed] [Google Scholar]
- 11.Lynch F, Ceredig R. Mouse strain variation in Ly-24 (Pgp-1) expression by peripheral T cells and thymocytes: implications for T cell differentiation. Eur J Immunol. 1989;19:223–229. doi: 10.1002/eji.1830190202. [DOI] [PubMed] [Google Scholar]
- 12.Tough DF, Sprent J. Turnover of naive- and memory-phenotype T cells. J Exp Med. 1994;179:1127–1135. doi: 10.1084/jem.179.4.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Picker LJ. Control of lymphocyte homing. Curr . Opin Immunol. 1994;6:394–406. doi: 10.1016/0952-7915(94)90118-x. [DOI] [PubMed] [Google Scholar]
- 14.Mackay CR, Marston WL, Dudler L, Spertini O, Tedder TF, Hein WR. Tissue-specific migration pathways by phenotypically distinct subpopulations of memory T cells. Eur J Immunol. 1992;22:887–895. doi: 10.1002/eji.1830220402. [DOI] [PubMed] [Google Scholar]
- 15.Bell EB, Sparshott SM, Ager A. Migration pathways of CD4 T cell subsets in vivo: the CD45RC− subset enters the thymus via α4integrin—VCAM-1 interaction. Int Immunol. 1995;11:1861–1871. doi: 10.1093/intimm/7.11.1861. [DOI] [PubMed] [Google Scholar]
- 16.Westermann J, Pabst R. How organ-specific is the migration of ‘naive' and ‘memory' T lymphocytes? . Immunol Today. 1996;17:278–282. doi: 10.1016/0167-5699(96)80545-7. [DOI] [PubMed] [Google Scholar]
- 17.Bradley LM, Atkins GG, Swain SL. Long-term CD4+memory T cells from the spleen lack MEL-14, the lymph node homing receptor. J Immunol. 1992;148:324–331. [PubMed] [Google Scholar]
- 18.Hou S, Doherty PC. Partitioning of responder CD8+T cells in lymph node and lung of mice with Sendai virus pneumonia by LECAM-1 and CD45RB. J Immunol. 1993;150:5494–5500. [PubMed] [Google Scholar]
- 19.Tripp RA, Hou S, Doherty PC. Temporal loss of the activated L-selectin-low phenotype for virus-specific CD8+memory T cells. J Immunol. 1995;154:5870–5875. [PubMed] [Google Scholar]
- 20.Sanders ME, Makgoba MW, Shaw S. Human naive and memory T cells. Immunol Today. 1988;9:195–199. doi: 10.1016/0167-5699(88)91212-1. [DOI] [PubMed] [Google Scholar]
- 21.Mackay C. T-cell memory: the connection between function, phenotype and migration pathways. Immunol Today. 1991;12:184–192. doi: 10.1016/0167-5699(91)90051-T. [DOI] [PubMed] [Google Scholar]
- 22.Swain SL, Croft M, Dubey C, Haynes L, Rogers P, Zhang X, Bradley LM. From naive to memory T cells. Immunol Rev. 1996;150:142–167. doi: 10.1111/j.1600-065x.1996.tb00700.x. [DOI] [PubMed] [Google Scholar]
- 23.Morimoto C, Letvin NL, Distaso JA, Aldrich WR, Schlossman SF. The isolation and characterization of the human suppressor inducer T cell subset. J Immunol. 1985;134:1508–1515. [PubMed] [Google Scholar]
- 24.Merkenschlager M, Terry L, Edwards R, Beverley PCL. Limiting dilution analysis of proliferative responses in human lymphocyte populations defined by the monoclonal antibody UCHL1: implications for differential CD45 expression in T cell memory formation. Eur J Immunol. 1988;18:1653–1661. doi: 10.1002/eji.1830181102. [DOI] [PubMed] [Google Scholar]
- 25.Spickett GP, Brandon MR, Mason DW, Williams AF, Woollett GR. MRC OX-22, a monoclonal antibody that labels a new subset of T lymphocytes and reacts with the high molecular weight form of the leukocyte-common antigen. J Exp Med. 1983;158:795–810. doi: 10.1084/jem.158.3.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arthur RP, Mason D. T cells that help B cell responses to soluble antigen are distinguishable from those producing interleukin 2 on mitogenic or allogeneic stimulation. J Exp Med. 1986;163:774–786. doi: 10.1084/jem.163.4.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Michie CA, McLean A, Alcock C, Beverley PCL. Lifespan of human lymphocyte subsets defined by CD45 isoforms. Nature (Lond) 1992;360:264–265. doi: 10.1038/360264a0. [DOI] [PubMed] [Google Scholar]
- 28.Sparshott SM, Bell EB. Membrane CD45R isoform exchange on CD4 T cells is rapid, frequent and dynamic in vivo . Eur J Immunol. 1994;24:2573–2578. doi: 10.1002/eji.1830241102. [DOI] [PubMed] [Google Scholar]
- 29.McLean AR, Michie CA. In vivoestimates of division and death rates of human T lymphocytes. Proc Nat Acad Sci USA. 1995;92:3707–3711. doi: 10.1073/pnas.92.9.3707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Akbar AN, Borthwick N, Salmon M, Gombert W, Bofill M, Shamsadeen N, Pilling D, Pett S, Grundy JE, Janossy G. The significance of low bcl-2 expression by CD45RO T cells in normal individuals and patients with acute viral infections. The role of apoptosis in T cell memory. J Exp Med. 1993;178:427–438. doi: 10.1084/jem.178.2.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Salmon M, Pilling D, Borthwick NJ, Viner N, Janossy G, Bacon PA, Akbar AN. The progressive differentiation of primed T cells is associated with an increasing susceptibility to apoptosis. Eur J Immunol. 1994;24:892–899. doi: 10.1002/eji.1830240417. [DOI] [PubMed] [Google Scholar]
- 32.Powrie F, Mason D. The MRC OX-22− CD4+ T cells that help B cells in secondary immune responses derive from naive precursors with the MRC OX-22+ CD4+phenotype. J Exp Med. 1989;169:653–662. doi: 10.1084/jem.169.3.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee WT, Yin X-m, Vitetta ES. Functional and ontogenetic analysis of murine CD45Rhi and CD45Rlo CD4+T cells. J Immunol. 1990;144:3288–3295. [PubMed] [Google Scholar]
- 34.Bell EB, Sparshott SM. Interconversion of CD45R subsets of CD4 T cells in vivo . Nature (Lond) 1990;348:163–166. doi: 10.1038/348163a0. [DOI] [PubMed] [Google Scholar]
- 35.Bell EB. Function of CD4 T cell subsets in vivo: expression of CD45R isoforms. Semin Immunol. 1992;4:43–50. [PubMed] [Google Scholar]
- 36.Paterson DJ, Jefferies WA, Green JR, Brandon MR, Corthesy P, Puklavec M, Williams AF. Antigens of activated rat T lymphocytes including a molecule of 50,000 Mrdetected only on CD4 positive T blasts. Mol Immunol. 1987;24:1281–1290. doi: 10.1016/0161-5890(87)90122-2. [DOI] [PubMed] [Google Scholar]
- 37.Hünig T, Wallny H-J, Hartley JK, Lawetzky A, Tiefenthaler G. A monoclonal antibody to a constant determinant of the rat T cell antigen receptor that induces T cell activation. Differential reactivity with subsets of immature and mature T lymphocytes. J Exp Med. 1989;169:73–86. doi: 10.1084/jem.169.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang C-p, Bell EB. Functional maturation of recent thymic emigrants in the periphery: development of alloreactivity correlates with the cyclic expression of CD45RC isoforms. Eur J Immunol. 1992;22:2261–2269. doi: 10.1002/eji.1830220913. [DOI] [PubMed] [Google Scholar]
- 39.Gautam SC, Matriano JA, Chikkala NF, Edinger MG, Tubbs RR. L3T4 (CD4+) cells that mediate contact sensitivity to trinitrochlorobenzene express I-A determinants. Cell Immunol. 1991;135:27–41. doi: 10.1016/0008-8749(91)90251-6. [DOI] [PubMed] [Google Scholar]
- 40.Bell EB, Sparshott SM, Drayson MT, Ford WL. The stable and permanent expansion of functional T lymphocytes in athymic nude rats after a single injection of mature T cells. J Immunol. 1987;139:1379–1384. [PubMed] [Google Scholar]
- 41.McCall MN, Shotton DM, Barclay AN. Expression of soluble isoforms of rat CD45. Analysis by electron microscopy and use in epitope mapping of anti-CD45R monoclonal antibodies. Immunology. 1992;76:310–317. [PMC free article] [PubMed] [Google Scholar]
- 42.Woollett GR, Barclay AN, Puklavec M, Williams AF. Molecular and antigenic heterogeneity of the rat leukocyte-common antigen from thymocytes and T and B lymphocytes. Eur J Immunol. 1985;15:168–173. doi: 10.1002/eji.1830150211. [DOI] [PubMed] [Google Scholar]
- 43.Trowbridge IS, Thomas ML. CD45: an emerging role as a protein tyrosine phosphatase required for lymphocyte activation and development. Annu Rev Immunol. 1994;12:85–116. doi: 10.1146/annurev.iy.12.040194.000505. [DOI] [PubMed] [Google Scholar]
- 44.Hosseinzadeh H, Goldschneider I. Recent thymic emigrants in the rat express a unique antigenic phenotype and undergo post-thymic maturation in peripheral lymphoid tissues. J Immunol. 1993;150:1670–1679. [PubMed] [Google Scholar]
- 45.Sparshott SM, Bell EB, Sarawar SR. CD45R CD4 T cell subset-reconstituted nude rats: subset-dependent survival of recipients and bi-directional isoform switching. Eur J Immunol. 1991;21:993–1000. doi: 10.1002/eji.1830210420. [DOI] [PubMed] [Google Scholar]
- 46.Sarawar SR, Sparshott SM, Sutton P, Yang C-p, Hutchinson IV, Bell EB. Rapid re-expression of CD45RC on rat CD4 T cells in vitrocorrelates with a change in function. Eur J Immunol. 1993;23:103–107. doi: 10.1002/eji.1830230117. [DOI] [PubMed] [Google Scholar]
- 47.Brod SA, Rudd CE, Purvee M, Hafler DA. Lymphokine regulation of CD45R expression on human T cell clones. J Exp Med. 1989;170:2147–2152. doi: 10.1084/jem.170.6.2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rothstein DM, Yamada A, Schlossman SF, Morimoto C. Cyclic regulation of CD45 isoform expression in a long-term human CD4+ CD45RA+T cell line. J Immunol. 1991;146:1175–1183. [PubMed] [Google Scholar]
- 49.Warren HS, Skipsey LJ. Loss of activation-induced CD45RO with maintenance of CD45RA expression during prolonged culture of T cells and NK cells. Immunology. 1991;74:78–85. [PMC free article] [PubMed] [Google Scholar]
- 50.Westermann J, Smith T, Peters U, Tschernig T, Pabst R, Steinhoff G, Sparshott SM, Bell EB. Both activated and nonactivated leukocytes from the periphery continuously enter the thymic medulla of adult rats: phenotypes, sources and magnitude of traffic. Eur J Immunol. 1996;26:1866–1874. doi: 10.1002/eji.1830260830. [DOI] [PubMed] [Google Scholar]
- 51.Macatonia SE, Edwards AJ, Knight SC. Dendritic cells and the initiation of contact sensitivity to fluorescein isothiocyanate. Immunology. 1986;59:509–514. [PMC free article] [PubMed] [Google Scholar]
- 52.Kripke ML, Munn CG, Jeevan A, Tang J-M, Bucana C. Evidence that cutaneous antigen-presenting cells migrate to regional lymph nodes during contact sensitization. J Immunol. 1990;145:2833–2838. [PubMed] [Google Scholar]
- 53.Miller SD, Jenkins MK. In vivoeffects of GK1.5 (anti-L3T4) monoclonal antibody on induction and expression of delayed-type hypersensitivity. Cell Immunol. 1985;92:414–426. doi: 10.1016/0008-8749(85)90022-x. [DOI] [PubMed] [Google Scholar]
- 54.Xu H, DiIulio NA, Fairchild RL. T cell populations primed by hapten sensitization in contact sensitivity are distinguished by polarized patterns of cytokine production: interferon γ-producing (Tc1) effector CD8+ T cells and interleukin (Il) 4/IL-10-producing (Th2) negative regulatory CD4+T cells. J Exp Med. 1996;183:1001–1012. doi: 10.1084/jem.183.3.1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gracie JA, Sarawar SR, Bolton EM, Bradley JA, Tanaka T, Bell EB. Renal allograft rejection in CD4+ T cell-reconstituted athymic nude rats. The origin of CD4+ and CD8+graft-infiltrating cells. Transplantation. 1990;50:996–1000. doi: 10.1097/00007890-199012000-00020. [DOI] [PubMed] [Google Scholar]
- 56.Rowley DA, Gowans JL, Atkins RC, Ford WL, Smith ME. The specific selection of recirculating lymphocytes by antigen in normal and preimmunized rats. J Exp Med. 1972;136:499–513. doi: 10.1084/jem.136.3.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sprent J, Miller JFAP, Mitchell GF. Antigeninduced selective recruitment of circulating lymphocytes. Cell Immunol. 1971;2:171–181. doi: 10.1016/0008-8749(71)90036-0. [DOI] [PubMed] [Google Scholar]
- 58.Ford WL. The recruitment of recirculating lymphocytes in the antigenically stimulated spleen. Clin Exp Immunol. 1972;12:243–254. [PMC free article] [PubMed] [Google Scholar]
- 59.Beverley PCL. Is T-cell memory maintained by crossreactive stimulation? . Immunol Today. 1990;11:203–205. doi: 10.1016/0167-5699(90)90083-l. [DOI] [PubMed] [Google Scholar]
- 60.Hayden KA, Tough DF, Webb SR. In vivo response of mature T cells to Mlsaantigens. J Immunol. 1996;156:48–55. [PubMed] [Google Scholar]
- 61.Mitchison NA. Specialisation, tolerance, memory, competition, latency and strife among T cells. Annu Rev Immunol. 1992;10:1–12. doi: 10.1146/annurev.iy.10.040192.000245. [DOI] [PubMed] [Google Scholar]
- 62.Tamatani T, Kitamura F, Kuida K, Shirao M, Mochizuki M, Suematsu M, Schmid-Schönbein GW, Watanabe K, Tsurufuji S, Miyasaka M. Characterization of rat LECAM-1 (L-selectin) by the use of monoclonal antibodies and evidence for the presence of soluble LECAM-1 in rat sera. Eur J Immunol. 1993;23:2181–2188. doi: 10.1002/eji.1830230920. [DOI] [PubMed] [Google Scholar]
- 63.McHeyzer-Williams MG, Davis MM. Antigenspecific development of primary and memory T cells in vivo. . Science (Wash DC) 1995;268:106–111. doi: 10.1126/science.7535476. [DOI] [PubMed] [Google Scholar]
- 64.Doherty PC, Topham DJ, Tripp RA. Establishment and persistence of virus-specific CD4+ and CD8+T cell memory. Immunol Rev. 1996;150:23–44. doi: 10.1111/j.1600-065x.1996.tb00694.x. [DOI] [PubMed] [Google Scholar]
- 65.Kündig TM, Bachmann MF, Ohashi PS, Pircher H, Hengartner H, Zinkernagel RM. On T cell memory: arguments for antigen dependence. Immunol Rev. 1996;150:63–90. doi: 10.1111/j.1600-065x.1996.tb00696.x. [DOI] [PubMed] [Google Scholar]