Abstract
Cyclophilins have been suggested to act as leukocyte chemotactic factors produced in the course of inflammation. Therefore we looked for the presence of cyclophilins in the synovial fluids (SF) from patients with rheumatoid arthritis (RA). Peptidyl prolyl cis–trans isomerase activity (PPIase) was measured in SF from knee punctures of 26 patients with RA and five patients with knee osteoarthritis (OA). PPIase was detected in SF from RA patients, but not in samples from OA patients. Enzyme activity was sensitive to inhibition by cyclosporin A (IC50 = 28–50 nM). Estimated concentrations of the SF-derived cyclophilin based on the enzyme activity were in the range of 11 to 705 nM. The presence of cyclophilin in the SF showed disease correlation; its concentration correlated with the number of cells in the SF (r = 0.91, P <0.0001) and with the percentage of neutrophils in the cellular infiltrate and was higher in more acute cases of joint swelling. In immunoblots of partially purified preparations of SF from RA patients, an ∼18-kD protein band reacted with polyclonal antibodies that recognize cyclophilin A and B, but not with antibodies specific for cyclophilin B. Sequencing of this protein revealed identity of the NH2-terminal amino acids with those of human cyclophilin A. The finding is unexpected since cyclophilin B rather than A is generally regarded as the secreted isoform, the presence of cyclophilin A being confined to the cytoplasm. Our data support the hypothesis that cyclophilins may contribute to the pathogenesis of inflammatory diseases, possibly by acting as cytokines. This may offer a possible explanation of the effectiveness of cyclosporin A in RA, in addition to the known immunosuppressive effects of the drug.
Inflammation is accompanied by a characteristic accumulation of polymorphonuclear leukocytes (PMN) in the tissue, which is observed in a variety of pathological conditions. In the case of rheumatoid arthritis (RA), the synovial fluid in affected joints of patients contains large numbers of different exudate cells; as the disease progresses, the PMNs become the predominant cell type. These cells may contribute to the eventual tissue destruction observed in RA and other arthritic conditions, since they are a major source of enzymes including those which degrade cartilage. Therefore, identification of factors responsible for the recruitment of PMNs is crucial for the understanding of the pathogenesis of synovial inflammation.
We have demonstrated that the chemokine IL-8 (also designated human neutrophil activating peptide, NAP-1) is present in synovial fluids (SF) in a high proportion of RA cases (1). The major activities of this peptide include neutrophil activation and induction of neutrophil and lymphocyte chemotaxis (2, 3). The observed correlation between concentration of IL-8 in SF and cellular influx into the joint was strongly suggestive of a pathogenic role for IL-8 in RA.
During our search for additional factors that are responsible for the attraction of PMNs, we asked whether cyclophilin(s) might be involved in synovial inflammation. Cyclophilins are a family of proteins characterized by their prolyl cis-trans isomerase activity and the ability to bind cyclosporin A (4, 5). More recently, secreted cyclophilins have been described (6–9), and human, rodent and bovine cyclophilins have been shown to be chemotactic to polymorphonuclear leukocytes and monocytes (9, 10). In this paper, we demonstrate the presence of cyclophilin A in synovial fluids of patients with RA.
Materials and Methods
Patients and Synovial Fluids.
Knee punctures were taken from 26 RA patients and five osteoarthritis (OA) patients. RA patients (6 male, 20 female) had a mean age of 52 yr (range 36–66); their mean disease duration was 6 yr (0.5–16). OA patients (1 male, 2 female) had a mean age of 68 (62–78); mean disease duration was 8 yr (6–12). Knee punctures were performed under sterile conditions. The volume of synovial fluid (SF) removed was between 4 and 30 ml; SF was collected in sterile EDTA tubes. The SF was centrifuged immediately at 1,000 g for 15 min; the cell-free supernatant was transferred into plastic tubes and stored at 4°C until analysis. Cell number and differential cell counts were determined in a Coulter counter. Synovial cells were analyzed for morphological criteria and cell lysis in a FACS®. Synovial IgM rheumatoid factor (IgMRF) determination was done by a standard nephelometric method (11). All RA patients were treated with different disease modifying antirheumatic drugs, e.g., antimalarials, methotrexate, azathioprine, or oral gold derivatives; 12 of the patients were additionally treated with oral steroids. All OA patients were treated with non-steroidal antirheumatic drugs.
Proteins and Antibodies.
Recombinant human cyclophilins A and B were provided by M. Zurini and Sandoz Basle; the cyclophilin B corresponds to the mature form of the protein lacking the NH2-terminal leader sequence (6). Polyclonal antibodies against purified recombinant human cyclophilin A were raised in rabbits and purified via DEAE Sephadex and protein A–Sepharose (Pharmacia, Uppsala, Sweden) chromatography; these antibodies show strong cross-reaction with cyclophilin B. Polyclonal antibodies against recombinant cyclophilin B or against the COOH-terminal peptide of cyclophilin B (12), both raised in rabbits, were kindly provided by Prof. G. Spik (University of Lille, France); these antibodies do not react with cyclophilin A in Western blots. Recombinant human NAP-1/IL-8 was produced and purified as previously described (2). Goat polyclonal antibodies and mouse monoclonal antibodies against IL-8 have been described before (13).
Enzyme Assay.
Peptidyl prolyl cis-trans isomerase activity in the cell-free supernatants of synovial fluids was measured using the assay essentially as described by Kofron et al. (14). In brief, samples (50 μl) or purified cyclophilin B as control were diluted with 50 mM Hepes, 100 mM NaCl, pH 8.0 (875 μl), in a photometer cuvette and cooled to 10°C. Then, 50 μl of α-chymotrypsin (Serva, Heidelberg, Germany) (10 mg/ml in 1 mM HCl) were added, and the reaction was started by addition of 25 μl 4 mM N-succinyl-Ala-Ala-Pro-Phe p-nitroanilide (Bachem, Bubendorf, Switzerland) in trifluoroethanol/470 mM lithium chloride. The increase in absorbance at 390 nm was recorded with a Cary 1E spectrophotometer. Data points were obtained every 0.5 s and fitted to a first-order rate law to obtain the reaction rate in units of absorbance (ABS) per min. In the case of inhibition experiments compounds were added from stock solutions in ethanol before addition of the chymotrypsin; solvent concentration did not exceed 2%. Isomerization rates observed in presence of different concentrations of inhibitor were used to calculate IC50 values.
Protein Purification and Identification.
For partial purification of the cyclophilin, samples of cell-free supernatants of synovial fluids were subjected to fractionated ammonium sulfate precipitation (30– 60% wt/vol). The precipitate was redissolved in against 10 mM Hepes, pH 8.0, 1 mM DTE, 0.1 mM EDTA and dialyzed against the same buffer. This solution was then passed through a Superose 12 column (2.6 × 60 cm; Pharmacia) at flow of 2 ml/min of the same buffer; 4-ml fractions were collected. Protein was detected by measuring absorbance at 280 nm, and enzyme activity by the isomerase assay as above.
SDS–polyacrylamide gel electrophoresis was performed on gels containing 20% acrylamide using the Pharmacia PhastSystem device. Gels were either stained with Coomassie Brillant Blue or blotted to nitrocellulose membranes. For Immunodetection, blots were incubated with primary antibodies, and reactive bands were visualized with biotinylated second antibody followed by the ECL detection system (Amersham, Braunschweig, Germany) and exposure to x-ray film.
Automated sequence analysis of protein samples electroblotted to Glassybond (Biometra, Göttingen, Germany) (15) was performed on a model 470A amino acid sequencer coupled to an on-line PTH-amino acid analyzer, model 120A (Applied Biosystems, Foster City, CA) with reverse-phase PTH C-18 micro-bore column (2.1 × 220 mm) using a standard gradient system (16).
Results
To investigate the presence of cyclophilins in synovial fluids, we chose to measure the peptidyl prolyl cis–trans isomerase activity associated with the proteins in a spectrophotometric assay using a synthetic peptide substrate (14). SF from knee punctures of patients with RA or OA were tested. Isomerase activity was detected in 26 out of 27 samples from RA patients. The only RA synovial fluid that did not show activity was derived from a patient (PF) that had been treated with a human IL-1 receptor antagonist, a treatment that reduces monocytotrophic synovial activity (17). In the five samples of OA patients no enzyme activity was present.
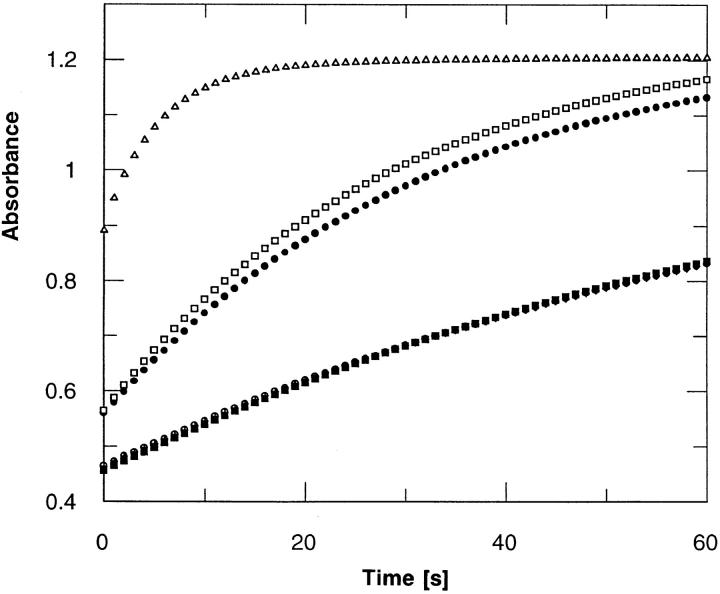
Since cyclophilins but also FK 506 binding proteins (FKBP) are able to isomerize the substrate used here, we performed experiments with specific inhibitors of the enzymes. The isomerase activity in the synovial fluids of the RA patients could be inhibited with cyclosporin A, an inhibitor of cyclophilins, but not with the macrophilin FK 506 (Fig. 1). This indicates that isomerization activity is due to a cyclophilin rather than to a FKBP. In five different SF, 50% inhibition of the activity was observed with cyclosporin A at concentrations of 28 to 50 nM.
Figure 1.
Time course of the peptidyl prolyl cis-trans isomerase activity. (Triangles) Cyclophilin B added (25 nM final concentration); (filled circles) 50 μl synovial fluid from a patient with RA (patient WA, left knee); (open squares) same as filled circles, but 20 μM FK 506 included; (open circles) Same as filled circles, but 20 μM cyclosporin A included; (filled squares) 50 μl synovial from a patient with OA (patient HU) added; (+) no synovial fluid added, i.e., substrate cleavage proceeding in the absence of isomerase (control). Note that the last three curves coincide.
To quantify the cyclophilin-like activity in the synovial fluids, a calibration curve (concentration versus reaction rate) with purified recombinant cyclophilin A was prepared, which was linear in the range of 2 to 30 nM (regression curve: μM cyclophilin A = 5.07 × rate [ABS/min] + 0.927, r = 0.997, n = 13). Using this calibration and assuming that the isomerase activity in the SF is due to an enzyme with specific activity similar to cyclophilin A, an estimate of the cyclophilin concentration was obtained (Table 1). Cyclophilin concentrations in the range of 11 to 705 nM were found.
Table 1.
Concentration of Cyclophilin-like Activity in Synovial Fluids (Knee Punctures) and Disease Parameters
| Disease | Patient initials | Cyclophilin concentration* | Synovial fluid cell count | Neutrophils | IgMRF | Duration of joint swelling | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| nM | cc 103/ml | % | wk | |||||||||
| RA | BE | 159 | 22,700 | 92 | + | <1 | ||||||
| RA | PF‡ | <2 | 1,200 | 68 | + | 4 | ||||||
| RA | HS | 100 | 25,600 | 94 | − | <1 | ||||||
| RA | MK | 87 | 20,500 | 89 | + | <1 | ||||||
| RA | MA | 237 | 32,400 | 96 | − | <1 | ||||||
| RA | FB | 48 | 16,300 | 85 | + | 2 | ||||||
| RA | GL | 242 | 53,500 | 96 | − | <1 | ||||||
| RA | BR | 11 | 10,600 | 80 | + | 4 | ||||||
| RA | HR | 33 | 14,800 | 84 | + | 3 | ||||||
| RA | SD | 89 | 22,600 | 90 | + | 1 | ||||||
| RA | PA | 24 | 13,000 | 79 | + | 3 | ||||||
| RA | WA, left§ | 117 | 31,700 | 96 | + | <1 | ||||||
| RA | WA, right§ | 49 | 24,600 | 88 | + | <1 | ||||||
| RA | HG | 13 | 9,700 | 78 | + | >4 | ||||||
| RA | FH | 30 | 13,200 | 82 | − | 4 | ||||||
| RA | LR | 70 | 20,200 | 87 | + | 2 | ||||||
| RA | KM | 89 | 23,400 | 90 | − | 1 | ||||||
| RA | HN | 29 | 16,400 | 83 | + | 4 | ||||||
| RA | LA | 28 | 15,100 | 80 | − | >4 | ||||||
| RA | HH | 24 | 11,600 | 78 | − | >4 | ||||||
| RA | KK | 92 | 23,400 | 90 | + | <1 | ||||||
| RA | KL | 573 | 68,200 | 92 | + | <1 | ||||||
| RA | NN | 105 | 27,300 | 90 | + | <1 | ||||||
| RA | KP | 17 | 11,000 | 88 | + | 2 | ||||||
| RA | PM | 147 | 32,600 | 94 | + | <1 | ||||||
| RA | AA | 705 | 82,900 | 96 | − | <1 | ||||||
| RA | EM | 110 | 30,800 | 91 | + | <1 | ||||||
| OA | HU | <2 | <100 | NA‖ | − | >4 | ||||||
| OA | SN | <2 | <100 | NA | − | >4 | ||||||
| OA | SL | <2 | 120 | NA | − | >4 | ||||||
| OA | PE | <2 | <100 | NA | − | 4 | ||||||
| OA | KR | <2 | <100 | NA | − | >4 |
Concentrations were obtained from a calibration curve with cyclophilin B (see text), and are thus based on the assumption that the PPlase activity is due to an enzyme with specific activity similar to cyclophilin B.
Treatment with recombinant human IL1 receptor antagonist.
SF from patient WA was first taken from the left knee and subsequently intraarticular cortisone instillation was given into that knee. 24 h later, SF from the right knee was taken.
NA, not applicable.
One may ask whether the cyclophilin activity in the fluids arises by active secretion of protein from synovial cells or merely as a consequence of cellular destruction. We, therefore, analyzed the synovial cells by FACS® for morphological criteria in a forward side scatter mode; there was no evidence of significant cell lysis (less than 1% in samples of all patients).
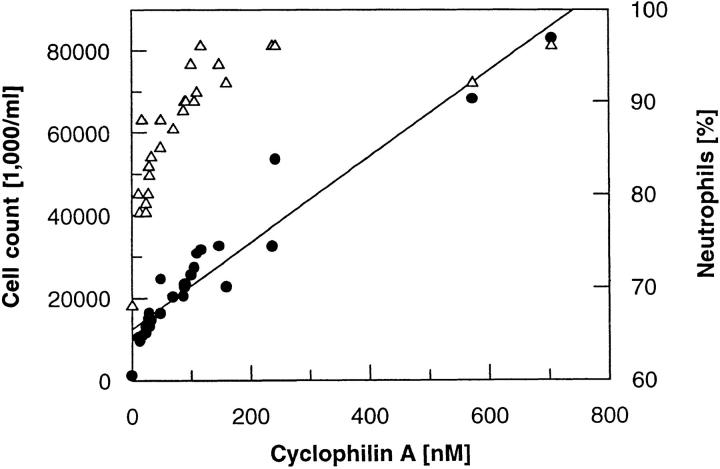
We also determined the cell counts in the synovial fluids; a linear correlation was observed between the cell count and the cyclophilin concentration (Fig. 2 A; correlation coefficient r = 0.91, P <0.0001). Furthermore, SF with higher enzyme concentration contained the higher percentage of neutrophils in the cellular infiltrate (Fig. 2 B). In addition, we noted that the highest cyclophilin concentrations were all observed in patients with a short anamnestic duration of joint swelling (⩽1 wk) (Table 1). No correlation was seen between the titer of synovial IgM RF and cyclophilin concentration (Table 1).
Figure 2.
Correlation of cyclophilin-like protein concentration with total cell counts in synovial fluids of RA patients (filled circles) and with percentage of neutrophils (open triangles).
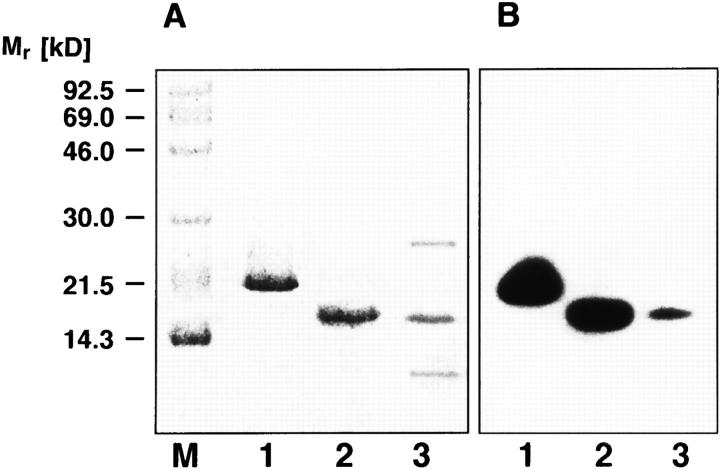
To identify the protein responsible for the cyclophilinlike activity, we performed a fractionation of synovial fluids. Two separate experiments were performed with SF pools of patients KK, NN, and PH and patients KL and AA. First, fractionated ammonium sulfate precipitation was performed; the enzymatic activity precipitated between 20 and 60% saturation. This was followed by gel filtration chromatography on Superose 12; this step separated the bulk of protein contained in the SF from the enzymatic activity. In the pooled fractions containing the isomerase activity, SDS gel electrophoresis followed by Coomassie staining revealed the presence of a protein band that comigrates with cyclophilin A besides some other contaminating bands (Fig. 3 A). Using a polyclonal antiserum raised against cyclophilin A which cross-reacts with cyclophilin B, an immunoreactive band migrating to the same position as cyclophilin A was detected (Fig. 3 B). This protein did not react with antibodies specifically recognizing cyclophilin B (not shown). To further substantiate the assumption that the SF contain cyclophilin A, we performed NH2-terminal sequencing of the 18-kD protein partially purified from pooled SF of patients KL and AA after blotting from SDS gels. The sequence of the first 20 NH2-terminal amino acids was determined to Val-Asn-Pro-Thr-Val-Phe-Phe-Asp-Ile-Ala-ValAsp-Gly-Glu-Pro-Leu-Gly-Arg-Val-Ser. This is identical to the known sequence of human cyclophilin A (18).
Figure 3.
SDS–polyacrylamide gel electrophoresis of partially purified cyclophilin A from synovial fluids of patients (KL and AA) with RA. Lane 1, recombinant cyclophilin B; lane 2, recombinant cyclophilin A; lane 3, pooled fractions of gel filtration chromatography containing the synovial cyclophilin activity. A Gel (20%) stained with Coomassie brillant blue. (B) Immunoblot developed with antibodies which recognize cyclophilins A and B. Positions of marker proteins (M) are indicated.
It has been reported that recombinant cyclophilin A is recognized on Western blots by antibodies directed against IL-8 (19). Using a polyclonal antiserum as well as a monoclonal antibody against IL-8 (13) we observed cross-reaction with the authentic cyclophilin from synovial fluids, too (immunoblot not shown).
Discussion
Cyclophilins are a family of highly conserved and ubiquitous proteins that possess peptidyl cis-trans isomerase activity (4, 5). This activity is thought to be important for protein folding in vivo (20). The most abundant isoform, cyclophilin A, has been described as a cytosolic protein while the more recently discovered cyclophilin B is located in the endoplasmatic reticulum (21, 22). Cyclophilin B is known to be retained in reticulum vesicles by its COOHterminal extension (23), but its appearance in human milk (6) and in the extracellular compartment of embryonic chick tissues (7) indicated that it is also a secreted protein. Furthermore, it has recently been shown that cyclophilin B is released by human leukocytes into the blood (12). Besides their enzymatic activity, a possible function of cyclophilins as cytokines has been suggested; a secreted cyclophilin was identified as a proinflammatory product of lipopolysaccharide-activated murine macrophages (9), bovine and human cyclophilin A were shown to be chemotactic for eosinophils and neutrophils (10), and embryonic chick cyclophilin B was found to possess growth factor activity (7). Moreover, cyclophilin B binds specifically to the surface of T cells (24, 25).
Here we demonstrated that cyclophilin A is present in the synovial fluids of patients with RA, as evidenced by (a) its enzymatic activity and (b) the occurrence of an immunoreactive protein of the same molecular weight and with the same NH2-terminal sequence known for this protein. The natural human protein shows similar sensitivity to inhibition of its PPIase activity by cyclosporin A (IC50 between 28 and 50 nM) as recombinant cyclophilin A (IC50 = 27 nM under similar conditions).
So far only human cyclophilin B has been regarded to be a secreted isoform, while the presence of cyclophilin A was thought to be confined to the cytoplasm (26). To our knowledge, this is the first time that cyclophilin A has been detected in an extracellular fluid or inflammatory exudate in man. However, a proinflammatory cyclophilin secreted by lipopolysaccharide-activated murine macrophages has been shown by partial sequencing to be identical to the intracellular murine cyclophilin A (9). It appears that the cyclophilin in the synovial fluids is secreted by the cells at the site, rather than being released as a consequence of cell destruction. Whereas we cannot completely exclude that cytoplasmic cyclophilin A and the protein contained in the SF have minor variations of sequence or posttranslational modifications, their immune reactivity and enzymatic properties do not suggest major differences.
The appearance of the cyclophilin A in SF shows correlation with disease parameters; its concentration correlates with the amount of cells in the fluid, with the percentage of neutrophils in the cellular infiltrate and is higher in more acute cases of joint swelling. Further studies will have to clarify whether the cyclophilin A purified from SF has chemotactic activity, as has been reported for the recombinant protein (10). If in fact cyclophilin A from the natural source can be shown to be chemotactic, it will be interesting to study to which extent it may contribute to the neutrophil activating activity in synovial fluids of RA patients, in view of the presence of IL-8 and other cytokines in the exudate. Seitz et al. (27) reported that 90% of the neutrophil-activating activity of synovial fluids from RA patients could be neutralized by a polyclonal anti–IL-8 antiserum; as a caveat, the cross-reactivity of antibodies against IL-8 and cyclophilin (see our findings and the results of Bang et al. [19]) may have led to an overestimation of the role of IL-8. In fact, more recently Strieter et al. (28) reported an only 27 to 57% reduction in neutrophil chemotactic activity with their IL-8 neutralizing antibodies, which indicates a substantial role for other chemotactic proteins.
Cyclosporin A is an immunosuppressive drug used for prevention of organ rejection, but is also useful in inflammatory diseases like psoriasis. It is also effective in RA (for review see reference 29). The mode of action of the immunosuppressive activity of cyclosporin A is understood in considerable detail (20): the compound does not exert its effect by inhibiting the isomerase activity of cyclophilin, but its binding enables cyclophilin to form a tertiary complex with the protein phosphatase calcineurin; this interaction leads to modulation of the response of T cells to immune stimuli on the transcriptional level. However, based on the chemotactic properties of cyclophilins it has been proposed that a second, complementary mechanism of action may exist (9, 24, 30), namely direct interaction of the drug with secreted cyclophilin isoforms. In view of this still open debate, our finding that cyclophilin A in fact is present in biological fluids of patients with an inflammatory disease that is responsive to therapy with cyclosporin A should stimulate further investigation of the role of cyclosporin A as an antiinflammatory compound and of the cytokine-like effects of cyclophilins.
Footnotes
We are indebted to Dr. Mauro Zurini and Sandoz Basle, for providing us with recombinant proteins, and to Prof. G. Spik (Université de Lille, France), for the anti-cyclophilin B antibodies. We are grateful to Dr. Brigitte Rosenwirth for helpful discussions during the initial phase of this work. We thank Dr. Fritz Schmook for help with the statistical evaluation.
References
- 1.Peichl P, Ceska M, Effenberger F, Haberhauer G, Broell H, Lindley IJD. Presence of NAP-1/IL-8 in synovial fluids indicates a possible pathogenic role in rheumatoid arthritis. Scand J Immunol. 1991;34:333–339. doi: 10.1111/j.1365-3083.1991.tb01554.x. [DOI] [PubMed] [Google Scholar]
- 2.Lindley I, Aschauer H, Seifert JM, Lam C, Brunowsky W, Kownatzki E, Thelen M, Peveri P, Dewald B, von Tscharner V, et al. Synthesis and expression in E. coliof the gene encoding monocyte-derived neutrophilactivating factor: biological equivalence between natural and recombinant neutrophil-activating factor. Proc Natl Acad Sci USA. 1988;85:9199–9203. doi: 10.1073/pnas.85.23.9199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larsen CG, Anderson AO, Appela E, Oppenheim JJ, Matsushima K. The neutrophil-activating protein (NAP-1) is also chemotactic for T-lymphocytes. Science (Wash DC) 1989;243:1464–1466. doi: 10.1126/science.2648569. [DOI] [PubMed] [Google Scholar]
- 4.Fischer G, Wittmann-Liebold B, Kiefhaber T, Schmid FX. Cyclophilin and peptidyl-prolyl cis-transisomerase are probably identical proteins. Nature (Lond) 1989;337:476–478. doi: 10.1038/337476a0. [DOI] [PubMed] [Google Scholar]
- 5.Takahashi N, Hayano T, Suzuki M. Peptidylprolyl cis-transisomerase is the cyclosporin A-binding protein cyclophilin. Nature (Lond) 1989;337:473–475. doi: 10.1038/337473a0. [DOI] [PubMed] [Google Scholar]
- 6.Spik G, Haendler B, Delmast O, Mariller C, Chamoux M, Maes P, Tartar A, Montreuil J, Stedman K, Kocher HP, et al. A novel secreted cyclophilin-like protein (SCYLP) J Biol Chem. 1991;266:10735–10738. [PubMed] [Google Scholar]
- 7.Caroni P, Rothenfluh A, McGlynn E, Schneider C. S-cyclophilin. J Biol Chem. 1991;266:10739–10742. [PubMed] [Google Scholar]
- 8.Price ER, Zydowsky LD, Jin M, Baker CH, McKeon FD, Walsh CT. Human cyclophilin B: a second cyclophilin gene encodes a peptidyl-prolyl isomerase with a signal sequence. Proc Natl Acad Sci USA. 1991;88:1903–1907. doi: 10.1073/pnas.88.5.1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sherry B, Yarlett N, Strupp A, Cerami A. Identification of cyclophilin as a proinflammatory secretory product of liposaccharide-activated macrophages. Proc Natl Acad Sci USA. 1992;89:3511–3515. doi: 10.1073/pnas.89.8.3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu Q, Leieva MC, Fischkoff SA, Handschumacher RE, Lyttle CR. Leukocyte chemotactic activity of cyclophilin. J Biol Chem. 1992;267:11968–11971. [PubMed] [Google Scholar]
- 11.Egeland T, Munthe E. Rheumatoid factors. Clin Rheum Dis. 1983;9:135–160. [PubMed] [Google Scholar]
- 12.Allain F, Boutillon C, Mariller C, Spik G. Selective assay for CyPA and CyPB in human blood using highly specific anti-peptide antibodies. J Immunol Methods. 1995;178:113–120. doi: 10.1016/0022-1759(94)00249-v. [DOI] [PubMed] [Google Scholar]
- 13.Peichl P, Ceska M, Broell H, Effenberger F, Lindley IJD. NAP-1/IL-8 acts as an autoantigen in rheumatoid arthritis. Ann Rheum Dis. 1992;51:19–22. doi: 10.1136/ard.51.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kofron JL, Kuzmic P, Kishore V, Colon-Bonilla E, Rich DH. Determination of kinetic constants for peptidyl prolyl cis-trans isomerases by an improved spectrophotometric assay. Biochemistry. 1992;30:6127–6134. doi: 10.1021/bi00239a007. [DOI] [PubMed] [Google Scholar]
- 15.Eckerskorn C, Mewes W, Goretzki H, Lottspeich F. A new siliconized-glass fiber as support for proteinchemical analysis of electroblotted proteins. Eur J Biochem. 1988;176:509–519. doi: 10.1111/j.1432-1033.1988.tb14308.x. [DOI] [PubMed] [Google Scholar]
- 16.Hunkapiller RM, Hood LE. Protein sequence analysis: automated microsequencing. Science (Wash DC) 1983;219:650–659. doi: 10.1126/science.6687410. [DOI] [PubMed] [Google Scholar]
- 17.Paulus HE, Egger MJ, Ward JR, Williams HJ the Cooperative Systematic Studies of Rheumatic Diseases Group. Analysis of improvement in individual rheumatoid arthritis patients treated with disease-modifying antirheumatic drugs, based on the findings in patients treated with placebo. Arthritis Rheum. 1990;33:477–484. doi: 10.1002/art.1780330403. [DOI] [PubMed] [Google Scholar]
- 18.Haendler B, Hofer-Warbinek R, Hofer E. Complementary DNA for human T-cell cyclophilin. EMBO (Eur Mol Biol Organ) J. 1987;6:947–950. doi: 10.1002/j.1460-2075.1987.tb04843.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bang H, Brune K, Nager C, Feige U. Interleukin-8 is a cyclosporin A binding protein. Experientia. 1993;49:533–538. doi: 10.1007/BF01955157. [DOI] [PubMed] [Google Scholar]
- 20.Walsh CT, Zydowsky ID, McKeon FD. Cyclosporin A, the cyclophilin class of peptidylprolyl isomerases, and blockade of T cell signal transduction. J Biol Chem. 1992;267:13115–13118. [PubMed] [Google Scholar]
- 21.Hasel KW, Glass JR, Godbout M, Sutcliffe JG. An endoplasmic reticulum-specific cyclophilin. Mol Cell Biol. 1991;11:3484–3491. doi: 10.1128/mcb.11.7.3484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bergsma DJ, Eder C, Gross M, Kersten H, Sylvester D, Appelbaum E, Cusimano D, Livi GP, McLaughin MM, Kasoyan K, et al. The cyclophilin multigene family of peptidyl prolyl isomerase. J Biol Chem. 1991;266:23204–23214. [PubMed] [Google Scholar]
- 23.Arber S, Krause KH, Caroni P. S-Cyclophilin is retained intracellularly via a unique COOH-terminal sequence and colocalizes with the calcium storage protein calreticulin. J Cell Biol. 1992;116:113–125. doi: 10.1083/jcb.116.1.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Allain F, Denys A, Spik G. Characterization of surface binding sites for cyclophilin B on a human tumor T-cell line. J Biol Chem. 1994;269:16537–16540. [PubMed] [Google Scholar]
- 25.Mariller C, Haendler B, Allain F, Denys A, Spik G. Involvement of the N-terminal part of cyclophilin B in the interaction with specific Jurkat T-cell binding sites. Biochem J. 1996;317:571–576. doi: 10.1042/bj3170571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stamnes MA, Rutherford SL, Zuker CS. Cyclophilins: a new family of proteins involved in intracellular folding. Trends Cell Biol. 1992;2:272–276. doi: 10.1016/0962-8924(92)90200-7. [DOI] [PubMed] [Google Scholar]
- 27.Seitz M, Dewald B, Gerber N, Baggiolini M. Enhanced production of neutrophil-activating peptide 1/interleukin-8 in rheumatoid arthritis. J Clin Invest. 1991;87:463–469. doi: 10.1172/JCI115018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Strieter RM, Koch AE, Antony VB, Fick RB, Standiford TJ, Kunkel SL. The immunopathology of chemotactic cytokines: the role of interleukin-8 and monocyte chemattractant protein-1. J Lab Clin Med. 1994;123:183–197. [PubMed] [Google Scholar]
- 29.Dougados, M. 1995. Cyclosporin in rheumatoid arthritis. Clin. Exp. Rheumatol. 12(Suppl. 11):S575–578. [PubMed]
- 30.Erlanger BF. Why cyclosporin is an effective drug. Immunol Today. 1993;14:369. doi: 10.1016/0167-5699(93)90238-G. [DOI] [PubMed] [Google Scholar]