Abstract
Interleukin-12 (IL-12), a heterodimeric cytokine produced by activated monocytes and dendritic cells, plays a crucial role in regulating interferon (IFN)-γ production and in the generation of IFN–γ–producing T helper 1 (Th1) cells. Here we show that the IL-12 receptor (IL12R) β2 subunit, a recently cloned binding and signal transducing component of the IL-12R, is expressed on human Th1 but not Th2 clones and is induced during differentiation of human naive cells along the Th1 but not the Th2 pathway. IL-12 and type I but not type II interferons induce expression of the IL-12R β2 chain during in vitro T cell differentiation after antigen receptor triggering. The selective expression and regulation of the IL-12R β2 subunit may help to understand the basis of Th1/Th2 differentiation and may provide therapeutic options for altering the Th1/Th2 balance in several immuno-pathological conditions such as autoimmune diseases and allergies.
CD4+ T helper cells can be divided into three major subsets termed Th1, Th2, and Th0, based on the pattern of lymphokines they produce. Th1 cells produce IFN-γ and predominantly promote cell-mediated immune responses, whereas Th2 cells, which produce IL-4, IL-5, and IL-13, provide help for some B cell responses. IL-4 in particular is the major inducer of B cell switching to IgE production (1), and therefore plays a crucial role in allergic reactions involving IgE and mast cells. Th cells producing cytokines typical of both Th1 and Th2 clones have also been described in both the murine and human system, and they have been named Th0 (2). The differential development of these subsets is a major determinant of the outcome of physiological, as well as pathological, immune responses including autoimmune, allergic, and infectious diseases (3, 4). Thus, understanding the mechanisms underlying Th cell differentiation is essential for therapeutic manipulation of the cytokine phenotype in disease conditions. Differentiation towards the Th1 or Th2 phenotype has been shown to be directed by exogenous cytokines present at the time of antigen exposure. IL-4 promotes Th2 development (5, 6), whereas IL-12 produced by APCs is a potent inducer of Th1 cells (7–9). Consistent with the necessity of IL-12 for induction of Th1 cell differentiation is the finding that IL-12 p40−/− mice are defective in IFN-γ production and almost completely lack the ability to generate a Th1 response (10). Conversely, knockout of the IL-4 gene resulted in deficient Th2 responses (11, 12). Furthermore, the crucial role of IL-12 and IL-4 signaling in the differentiation of Th subsets has been analyzed more recently in mice deficient in the signal transducers and activators of transcription 6 and 4 (Stat6 and Stat4)1. These proteins are thought to mediate functional responses to IL-4 and IL-12, respectively. Stat6-deficient T lymphocytes fail to differentiate into Th2 cells in response to IL-4 (13–15), and the analysis of Stat4−/− T cells revealed an impaired production of IFN-γ upon antigen triggering, indicative of a defect in Th1 differentiation (16, 17).
In the present paper, we have studied IL-12 signaling and IL-12 receptor expression and regulation during differentiation of human naive T cells into the Th1 and the Th2 subsets. As previously reported in the murine system, IL-12 induces tyrosine phosphorylation of the transcription factor Stat4 in human Th1, but not Th2 cells. IL-12–dependent signaling in human Th1 cells correlates with the selective expression of the transcripts encoding the signaling component of the IL-12 receptor (IL-12R) β2 and with the presence of high affinity IL-12 binding sites selectively on Th1 cells. IL-12R β2 transcripts, which were absent in naive T cells, were found as early as 24 h after mitogen stimulation. IL-12 and type I but not type II IFNs induce expression of IL-12R β2 mRNAs, whereas IL-12R β2 transcripts could not be detected in cells stimulated in the presence of IL-4. The selective expression and regulation of the IL-12 receptor β2 subunit may help understand the molecular events controlling Th cell development.
Materials and Methods
Generation of Th1 and Th2 Lines from Cord Blood Leukocytes.
Human neonatal leukocytes were isolated from freshly collected, heparinized, neonatal blood by Ficoll-Paque (Pharmacia Biotech AB, Uppsala, Sweden) density gradient centrifugation (18). Neonatal T cell preparations were >70% CD45RA+ and 50–60% CD4+. Th1 and Th2 cell lines were generated by stimulating cord blood leukocytes with 2 μg/ml PHA (Wellcome, Beckenham, UK) in the presence of 2 ng/ml IL-12 (Hoffmann-La Roche Inc., Nutley, NJ) and 200 ng/ml neutralizing anti–IL-4 antibodies (No. 18500D; PharMingen, San Diego, CA) for Th1 cultures, or 200 U/ml IL-4 (PharMingen) and 2 μg/ml neutralizing anti–IL-12 antibodies 17F7 and 20C2 (provided by M. Gately, Hoffmann-La Roche Inc.) for Th2 cultures, respectively. The cord blood–derived T cell lines were 60–90% CD4+. The remaining cells were CD8+ T cells. Cells were washed on day 3 and expanded in RPMI 1640 medium supplemented with 5% FCS, 2 mM l-glutamine, 1 mM sodium pyruvate, 100 U/ml penicillin-streptomycin, and containing 100 U/ml IL-2 (HoffmannLa Roche Inc.). Cells were washed again on day 10 and 105 cells were restimulated in 96-well round-bottom plates for 24 h with plate-bound anti-CD3 antibodies (clone TR66; reference 19) to measure IFN-γ and IL-4 in culture supernatants by ELISA assays (provided by H. Gallati, F. Hoffmann-La Roche AG, Basel, Switzerland; reference 20). To test the effects of type I and type II interferons on T helper cell differentiation, T cell lines were generated by stimulating cord blood leukocytes with PHA in the presence of the indicated cytokines or anti-cytokine antibodies as above. IFN-α or IFN-γ (1,000 U/ml; F. Hoffmann-La Roche AG) were added at the time of priming to the cultures. Cytokine production was determined on day 10 as above.
Purification and Stimulation of CD45RA+ T Cells.
PBMCs were isolated from human blood buffy coats from healthy donors by Ficoll-Paque (Pharmacia Biotech AB) density gradient centrifugation. Monocytes were depleted by two rounds of plastic adherence and B cells were depleted by adherence to nylon wool as described (18). CD45RA+ T cells were isolated by two rounds of immunomagnetic negative selection with a mixture of the following monoclonal antibodies: anti-CD16 (B73.1; reference 21), anti-CD45RO (UCHL-1; reference 22) and anti–HLA-DR (1-1C4; reference 23). The suspension was incubated with goat anti–mouse IgG-coated Dynabeads (Dynal, Inc., Geat Neck, NY) and exposed to a magnetic field using a magnetic particle concentrator (Dynal, Inc.) according to the manufacturer's instructions. The purity of the CD3/CD45RA+ T cells using this procedure was typically >98% as determined by flow cytometry. Purified CD45RA+ T cells were stimulated with plate-bound anti-CD3 mAbs (TR66; reference 19) without the addition of cytokines or in the presence of IL-12 (2 ng/ml) or IL-4 (200 U/ml).
T Cell Clones.
Th1 and Th2 cells generated from cord blood lymphocytes were cloned by limiting dilution as described (24). In brief, 0.3 cells/well were plated in 96-well plates in the presence of irradiated (5,000 rads) allogeneic PBMCs, PHA (2 μg/ml), and IL-2 (100 U/ml). Positive wells were restimulated and expanded and cytokine production of individual clones was measured as above. Three T cell clones that produced IFN-γ but not IL-4 were categorized as Th1, and five T cell clones able to produce IL-4 but not IFN-γ were categorized as Th2 clones (data not shown).
Cell Extracts, Immunoprecipitations, and Western Blot Analysis.
Th1 and Th2 lines generated from cord blood lymphocytes were harvested on day 10 after priming. Th1 (CB13) and Th2 (CB21) clones were harvested on day 13 after restimulation. 5 × 106 cells were washed and incubated for 15 min at 37°C in 1 ml RPMI with 5% FCS with or without 2 ng/ml IL-12. Cells were washed once in PBS before lysing the cell pellet in 250 μl IP buffer (10 mM Tris/HCl, pH 7.4, 150 mM NaCl, 1 mM EDTA, pH 8.0, 1 mM EGTA, pH 8.0, 1% NP-40, 0.25% sodium deoxycholate, 10 μg/ml aprotinin, leupeptin, and NaF, 1 mM AEBSF and sodium orthovanadate). The lysate was incubated 30 min on a shaker at 4°C and insoluble debris was removed by centrifugation (13,000 rpm, 4°C, 30 min). Stat4 was immunoprecipitated with rabbit polyclonal anti-Stat4 antisera (Santa Cruz Biotechnology, Inc., Santa Cruz, CA) and resolved by SDS-PAGE. After transfer to nitrocellulose, blots were probed with anti-phosphotyrosine antibody 4G10 (Upstate Biotechnology Inc., Lake Placid, NY), and immunoreactive bands were visualized using the enhanced chemiluminescence Western blotting system (Amersham, Milan, Italy), according to the company's protocols. To control for equal protein loading, blots were stripped and reprobed with anti-Stat4 antisera.
Ribonuclease Protection Assays.
A 327-bp DNA fragment encompassing the cytoplasmic region of the human IL-12R β2 subunit (25) and a 553-bp EcoRI/BamHI fragment derived from the IL-12R β1 cDNA (26) were subcloned into pGEM 3Z. The constructs were linearized with EcoRI and radiolabeled antisense transcripts were synthesized with SP6 polymerase and a commercial kit according to the manufacturer's protocol (Promega Corp., Madison, WI). RNA was extracted from Th1 and Th2 lines or clones using Ultraspec total RNA extraction reagent (Biotecx Laboratories Inc., Houston, TX) as described (27). The antisense RNA probes were hybridized to 10 μg total RNA and ribonuclease protection assays were performed with a commercial kit (Ambion Inc., Austin, TX) according to the company's protocol. Products were resolved on 6% denaturing polyacrylamide gels and the protected fragments were visualized by autoradiography. The radioactivity present in the protected fragments was also quantitated using a MolecularImager (Bio-Rad Labs., Richmond, CA). An 18S RNA probe was used as a control for equal RNA loading.
Scatchard Analysis of [125I]IL-12 Binding to Human Th1 and Th2 Cell Lines.
Th1 and Th2 lines were generated as described above. [125I]IL-12 binding to human Th1 and Th2 cell lines was determined as described previously (28). Specific binding was analyzed using the LIGAND program (29) and plotted by the Scatchard method.
Results and Discussion
IL-12 Induces Stat4 Phosphorylation in Human Th1 but Not Th2 Cells.
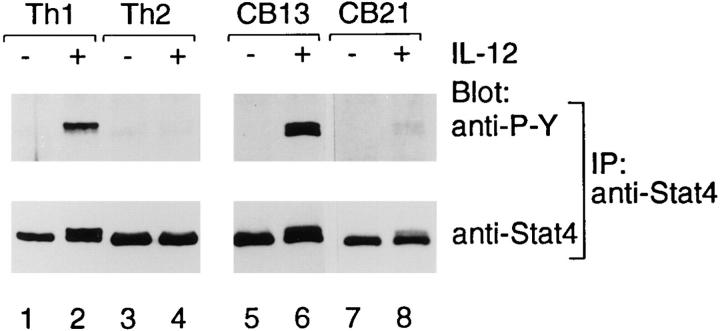
To characterize the role of IL-12 and other cytokines in the differentiation of T helper cell subsets, we have generated Th1 and Th2 lines by stimulating human cord blood leukocytes with mitogen in the presence of IL-12, and neutralizing anti–IL-4 mAb or IL-4, and neutralizing anti–IL-12 mAb, respectively. This protocol allows the establishment of human T cell lines with strongly polarized cytokine production. Neonatal T cells primed under the Th1 conditions produced up to 2 ng/ml of IFN-γ and <0.2 ng/ml IL-4 upon restimulation with plate-bound anti-CD3 mAb, whereas neonatal T cells primed in the presence of IL-4 and anti–IL-12 mAb produced 1.2 ng/ml of IL-4 and <0.02 ng/ml IFN-γ (Fig. 1 A). Subsequent cloning of the Th1 and the Th2 lines resulted in a series of T cell clones with either a Th1 or a Th2 polarized cytokine profile, respectively (Fig. 1 B). Using a murine TCR transgenic system, Szabo et al. observed that IL-12 selectively activated the Janus kinase Jak2, and the signal transducers and activators of transcription Stat3 and Stat4 in Th1, but not in differentiated Th2 cells (30). To ascertain whether human Th1 and Th2 subsets also differ in IL-12 signaling, we examined Stat4 expression and tyrosine phosphorylation in response to IL-12 in Th1 and Th2 lines and clones. As shown in Fig. 2, IL-12 treatment induced tyrosine phosphorylation of Stat4 selectively in Th1 but not in Th2 cells, although both cell types expressed comparable amounts of the Stat4 protein (Fig. 2, bottom) required for IL-12 signaling (31, 32). Similarly, after IL-12 stimulation, Jak2 (33), which was also expressed at comparable levels in Th1 and Th2 cells, was phosphorylated only in Th1 cells (data not shown).
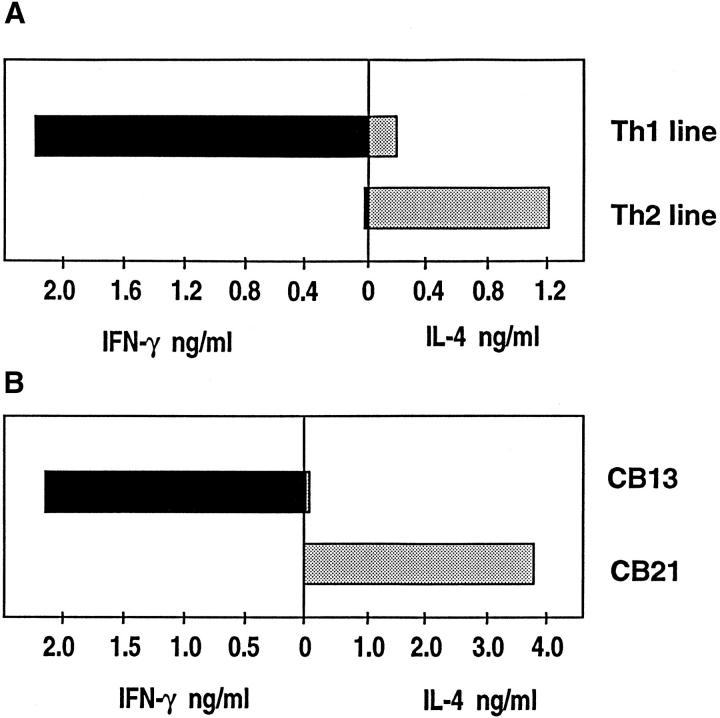
Figure 1.
Cytokine profiles of cord blood derived Th1 and Th2 lines and of established human T cell clones. (A) IFN-γ and IL-4 production by Th1 and Th2 lines generated from cord blood lymphocytes. Cells were washed on day 10 after priming, 105 cells were restimulated in 96well round-bottom plates for 24 h with plate-bound anti-CD3 antibodies (clone TR66; reference 19), to determine IFN-γ and IL-4 in culture supernatants by ELISA assays. The results shown are representative of five independent experiments. (B) IFN-γ and IL-4 production by established Th1 (CB13) and Th2 (CB21) clones.
Figure 2.
IL-12–dependent signaling in human Th1 and Th2 cell lines and clones. IL-12 induces Stat4 phosphorylation in human Th1 but not Th2 cells. Th1 and Th2 lines generated from cord blood lymphocytes as in Fig. 1 A were harvested on day 10 after priming. Th1 (CB13) and Th2 (CB21) clones were harvested on day 13 after restimulation. 5 × 106 cells were washed and incubated 15 min at 37°C in medium with or without 2 ng/ml IL-12 followed by the preparation of whole cell extracts and immunoprecipitation with anti-Stat4 antiserum. Precipitated proteins were separated by SDS-PAGE (8%), transferred to nitrocellulose, and probed with anti-phosphotyrosine antibody 4G10 (anti-P-Y, top). As a control for Stat4 expression, blots were stripped and reprobed with anti-Stat4 antibodies (bottom).
Selective Expression of the IL-12R β2 Chain in Th1 Cells.
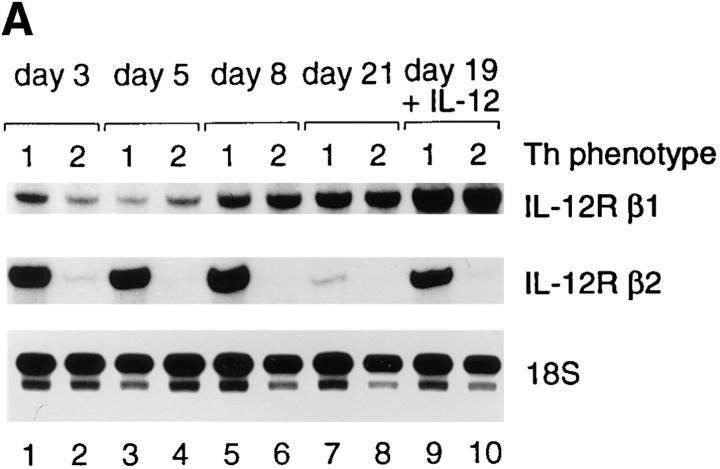
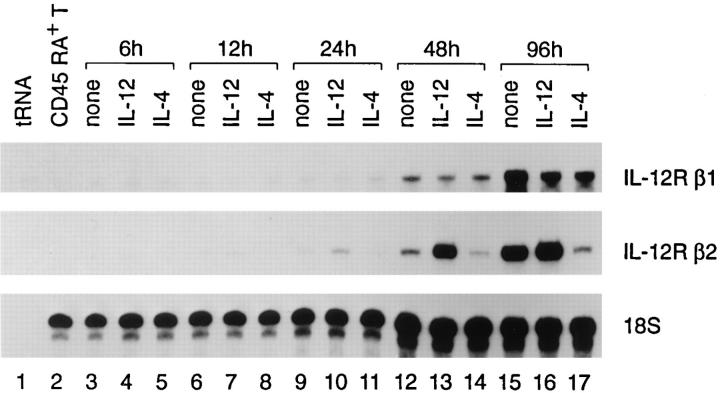
We next examined whether the defect in IL-12 signaling observed in Th2 cells is due to a differential expression of IL-12 receptors in the two cell types. To date, two IL-12R subunits, termed β1 and β2, have been identified. IL-12R β1 or β2, independently expressed in COS cells, bind human IL-12 with low affinity (K D = 3–5 nM), whereas coexpression of IL-12R β1 and β2 in COS cells gives rise to high affinity binding sites (K D = 50 pm) (25, 26). These studies have also shown that the IL-12R β2 is the signaling component of the IL-12R, in agreement with the fact that the IL-12R β2, in contrast to the IL-12R β1, contains tyrosine residues in its cytoplasmic domain (25). We analyzed the mRNA expression levels for the IL-12R β1 and β2 subunits by ribonuclease protection assays in both Th1 and Th2 lines at different time points after priming and in Th1 and Th2 clones at day 13 after restimulation. Whereas IL-12R β1 transcripts were expressed in similar amounts in both Th1 and Th2 cells (Fig. 3, A and B), the transcripts coding for the IL-12R β2 subunit were selectively expressed in established Th1, but not Th2 lines (Fig. 3 A) and clones (Fig. 3 B). Maximum expression in Th1 cells was seen between day 3 and day 8, and declined thereafter. Th2 cells, in contrast, expressed little IL-12R β2 transcripts on day 3, and none were detected after day 8 (Fig. 3 A). A key question is whether cytokine signaling is required for IL-12R induction or whether stimulation via the TCR/CD3 complex is sufficient to induce IL-12R in naive T cells. IL-12R transcripts were therefore analyzed in purified CD45RA+ T cells before and after stimulation with plate-bound anti-CD3 mAb. IL-12R transcripts were not found in naive T cells (Fig. 4, lane 2), but could be detected as early as 24 h after T cell activation (Fig. 4, lane 9). Priming of naive T cells in the presence of IL-12 resulted in enhanced expression of IL-12R β2 transcripts in this population (Fig. 4, lane 13); priming of cells in the presence of IL-4, in contrast, resulted in very low levels of IL-12R β2 transcripts (Fig. 4, lane 14). Thus, antigen receptor triggering is sufficient to make naive T cells susceptible to IL-12 signaling.
Figure 3.
Transcripts encoding IL-12 receptor subunits in human Th1 and Th2 cells. (A) IL-12R β2 transcripts are selectively expressed in human Th1 cells. Th1 and Th2 lines generated from cord blood lymphocytes were harvested on the indicated time after priming. In lanes 9 and 10, cells were washed on day 19 and incubated for 48 h in medium containing 2 ng/ml IL-12 before RNA extraction on day 21. Transcripts encoding the IL-12R β1 subunit (top), the IL-12R β2 subunit (middle) and an 18S RNA gene fragment as loading control (bottom) were quantitated with ribonuclease protection assays as described in Materials and Methods. (B) Expression of IL-12R β1 and β2 mRNAs in human Th1 (CB13) and Th2 (CB21) T cell clones. Th1 and Th2 cells were incubated on day 11 after restimulation for 48 h with or without 2 ng/ml IL-12, followed by RNA extraction on day 13. Quantitation of the IL-12R β1 and β2 transcripts in IL-12 treated and untreated Th1 and Th2 cells was performed by RNase protection assays.
Figure 4.
Antigen receptor triggering induces expression of IL-12R β1 and β2 mRNAs in purified CD45RA+ T cells. CD45RA+ T cells were purified by negative selection from buffy coats as described in Materials and Methods. Purified CD45RA+ T cells (5 × 106) were stimulated with platebound anti-CD3 mAb with or without the addition of IL-12 (2 ng/ml) or IL-4 (200 U/ml). RNA was extracted from unstimulated CD45RA+ T cells (lane 2) or at the indicated time after CD3 stimulation. Transcripts encoding IL-12R subunits were quantitated in RNase protection assays.
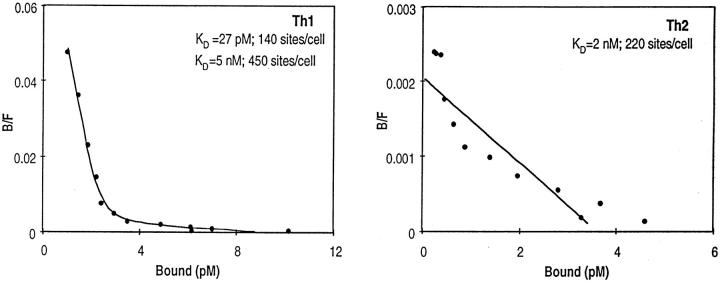
We next analyzed IL-12R expression by radioligand binding assays. Scatchard analysis of specific [125I]IL-12 binding to human cord blood derived Th1 and Th2 cell lines is shown in Fig. 5. In Th1 cell lines, both high (KD of 27 pM, 140 sites/cell) and low affinity (KD of 5 nM, 450 sites/cell) [125I]IL-12 binding sites were measured. In contrast, Th2 cells lines exhibited only low affinity [125I]IL-12 binding sites (KD of 2 nM 220 sites/cell). The absence of measurable high affinity [125I]IL-12 binding to the human Th2 cell lines is in agreement with the observed lack of IL-12R β2 expression in these cells. On the contrary, similar levels of high and low affinity IL-12 binding were measured in mouse Th1 and Th2 cell lines (30 and data not shown). This difference in IL-12 binding behavior in the mouse and human systems may reflect the dominant role mouse IL-12R β1 plays in binding IL-12 (34), whereas in humans, both IL-12R β1 and β2 appear to contribute equally to IL-12 binding (25). These results demonstrate that the IL-12R β2 subunit is selectively expressed in Th1 cells where it is induced upon T cell activation. Moreover, our data suggest that the lack of IL-12R β2 chain expression could be the reason underlying the inability of IL-12 to activate the Jak2-Stat4 pathway in Th2 cells.
Figure 5.
Scatchard analysis of [125I]IL-12 binding to human Th1 and Th2 cell lines. Th1 and Th2 lines were generated as described above. Scatchard analysis was performed using [125I]labeled human IL-12 binding on human Th1 and Th2 cell lines on day 9 after priming as described in Materials and Methods. Comparable [125I]IL- 12 binding data were obtained in three independently derived Th1 and Th2 cell lines.
Regulation of IL-12R β2 mRNA Expression during T Helper Cell Differentiation.
To determine whether IL-12 directly influences expression of the IL-12R β2 transcripts, we added IL-12 to both Th1 and Th2 lines at day 19 after priming. Culturing the cells in the presence of IL-12 for 48 h resulted in a sevenfold increase in IL-12R β2 transcripts in Th1 lines and a twofold increase in Th2 lines (Fig. 3 A, lanes 9 and 10). These results were confirmed and extended using established Th1 and Th2 clones. IL-12 induced IL-12R β2 mRNA upregulation (threefold) in both cell types (Fig. 3 B). Time course experiments revealed that the IL-12 induced upregulation of the IL-12R β2 mRNA in primed T cells was transient; maximal induction was seen 24–48 h after the addition of IL-12, but returned to the level of the control cultures after 96 h (data not shown). The IL-12–induced transient upregulation of the IL-12R β2 transcripts in Th2 clones may account for the transient period of IFN-γ production in cells with an established Th2 phenotype (35, 36).
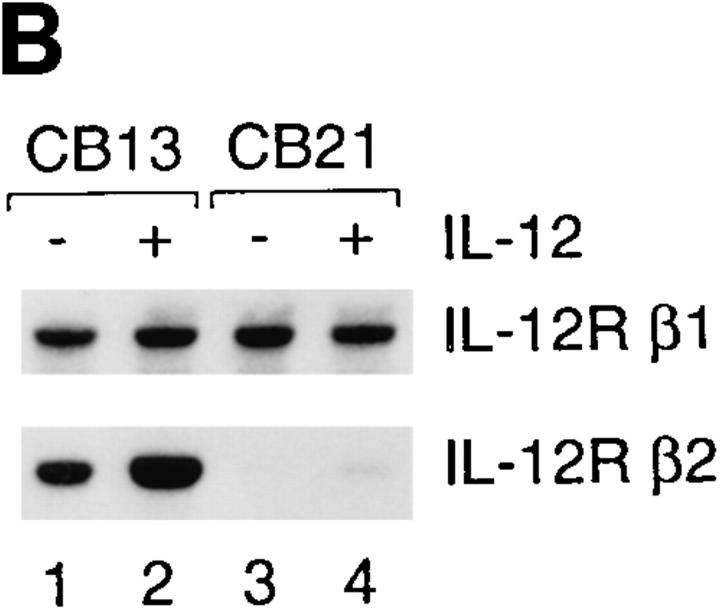
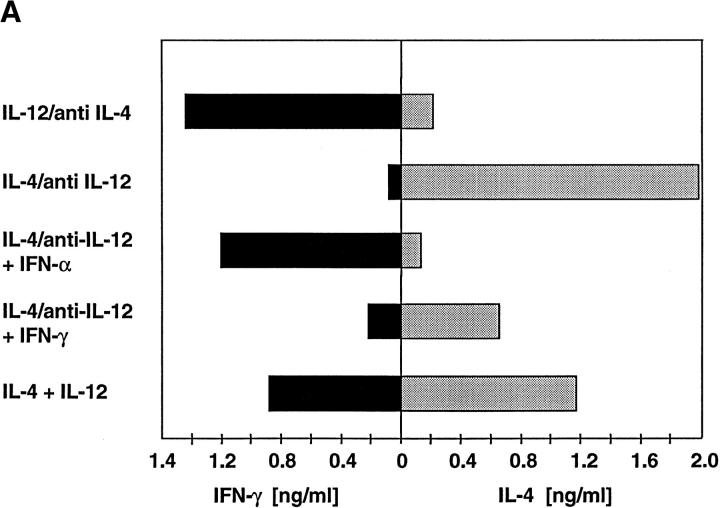
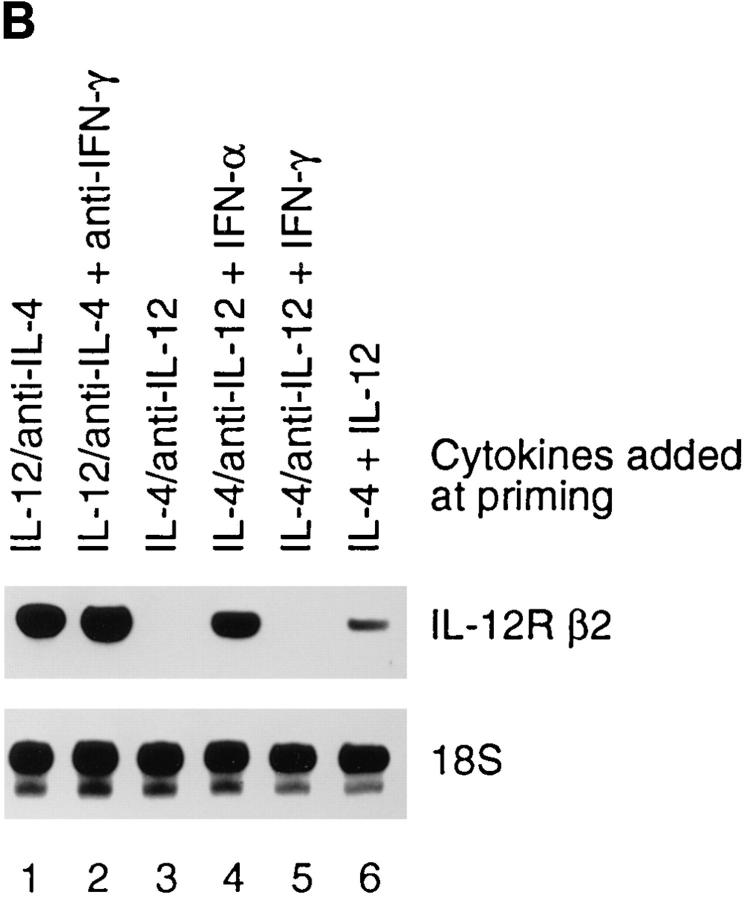
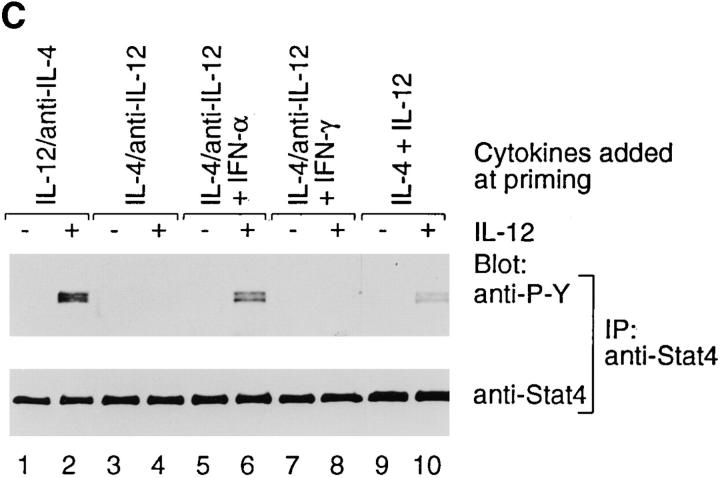
In the mouse, IL-4 has been shown to block the development of naive CD4+ T cells into Th1 effectors. The block is complete if IL-12 is not present in the priming culture, but incomplete if IL-12 is present (9). Consistent with this observation, we found that cord blood lymphocytes primed in the presence of IL-4 and IL-12 together developed into cells secreting both IL-4 (1.1 ng/ml) and IFN-γ (0.9 ng/ml) (Fig. 6 A). These cells phosphorylate Stat4 in response to IL-12 and accordingly express the IL-12R β2 mRNA, although to a lower level, as compared to Th1 cells (Fig. 6, B and C). In contrast, neonatal cells primed in the presence of IL-4 and neutralizing anti–IL-12 mAb completely lost IL-12R β2 expression (Figs. 3 A and 6 B) and consequently, IL-12–mediated signaling (Figs. 2 and 6 C). Although the mechanism by which IL-4 induces the generation of IL-12 nonresponsive Th2 cells remains to be clarified, our results are consistent with a model in which IL-12 prevents the gradual extinction of the IL-12R β2 subunit that appears to follow exposure to IL-4. Alternatively, the presence of IL-12 or IL-4 could result in the preferential expansion of IL-12 responsive Th1 cells or IL-12 nonresponsive Th2 cells, respectively.
Figure 6.
Function of type I and II IFNs in the development of T helper cell subsets and on the expression of the IL-12R β2 subunit. (A) IFN-α induces Th1 development. T cell lines were generated by stimulating cord blood lymphocytes with PHA in the presence of the indicated cytokines or anti-cytokine antibodies. IFN-α or IFN-γ (1,000 U/ml) were added at the time of priming to the cultures as indicated. Cytokine production was determined on day 10. IFN-α, but not IFN-γ, induces a Th1 phenotype even in the presence of IL-4 and neutralizing anti–IL-12 antibodies. (B) IFN-α induced Th1 cells express IL-12R β2 transcripts. RNA was extracted from T cell lines 10 d after priming in the presence of the indicated cytokines or neutralizing anti-cytokine antibodies. RNase protection assays were performed as described above. (C) IFN-α induced Th1 cells are IL-12 responsive. T cell lines (Fig. 6 A) were harvested on day 10 after priming. 8 × 106 cells were washed and incubated 15 min at 37°C in medium with or without 2 ng/ml IL-12 in 1 ml RPMI-FCS. IL-12 induced Stat4 phosphorylation was determined as described above.
IFN-α Induces IL-12R β2 mRNA Expression and IL-12 Responsiveness in Human T Cells.
In addition to IL-12, IFN-α and IFN-γ have also been shown to influence Th1 cell development (37, 38). We therefore examined the effect of these cytokines on the regulation of the IL-12R β2 expression. The addition of IFN-α (Fig. 6 A) as well as IFN-β (data not shown) to human cord blood leukocytes stimulated under Th2-inducing conditions (IL-4 and anti– IL-12 mAb) resulted in cells producing IFN-γ (>1 ng/ml) upon restimulation with anti-CD3 mAb (Fig. 6 A). IL-12R β2 mRNA was expressed in the IFN-α–treated T cell lines (Fig. 6 B) and IL-12 induced Stat4 phosphorylation in these cells (Fig. 6 C). In contrast, addition of IFN-γ to cultures containing IL-4 and anti–IL-12 (Th2-inducing conditions) or addition of neutralizing anti–IFN-γ mAb at the time of Th1 priming had no significant effect on the pattern of Th cell development (Fig. 6 A and data not shown) or IL-12R β2 expression (Fig. 6 B). IFN-α or IFN-γ had no significant effect on the expression of the IL-12R β1 transcripts (data not shown). Our findings differ from previous reports showing that in the mouse IFN-γ but not IFN-α influences Th1 cell development (38). Our data, together with the evidence that IFN-α in vitro favors the development of human allergen-specific T cells into a Th1 phenotype (37), suggest that type I and type II IFNs could have different functional effects on human as compared to mouse T cells. Indeed, preliminary results indicate that in human Th2 cells, both IFN-α and IFN-β are able to induce a much stronger (10-fold higher) phosphorylation of Stat1 as compared to IFN-γ (data not shown), suggesting a quantitative rather than a qualitatitive difference in IFNinduced signaling in human and mouse cells.
Our data indicate the presence of two major signaling pathways influencing IL-12R β2 expression. Triggering of the antigen receptor on naive T cells is sufficient for the initial expression of functional IL-12 receptors on activated T cells. Depending on the cytokines present during the differentiation, T cells will then develop into IL-12–responsive Th1 cells or IL-12–nonresponsive Th2 cells. Analysis of the IL-12R β2 promoter should provide insights into the molecular mechanisms by which TCR triggering and signals mediated by IL-12, IFN-α, IL-4, and other cytokines are integrated to regulate IL-12R β2 chain expression.
The IL-12R β2 chain appears to be the first Th1 subset– specific noncytokine gene to be identified to date. Here we provide evidence that IFN-α, but not IFN-γ, can induce Th1 development in neonatal T cells even in the presence of the Th2-inducing cytokine IL-4. We also demonstrate that IL-12 and IFN-α, by inducing the upregulation of the β2 component of the IL-12R after antigen receptor triggering, play an important role in both the functional activity and development of Th1 cells. The understanding of the molecular events controlling T cell development may allow the selective manipulation of Th subsets in vivo. The possibility of forcing expression in vivo of the IL-12R β2 by IFN-α or IL-12 treatment, for example, could have important therapeutic implications in Th2-mediated pathological conditions, such as allergies.
Acknowledgments
We would like to thank M. Gately for the IL-12 and anti–IL-12 antibodies, H. Gallati and R. Lang for the IL-4 and IFN-γ ELISA assays, P. Vigano for the cord blood samples, R. Pardi for the mAbs, R. Germain and E. Bianchi for critically reading the manuscript, and K. Murphy for communicating results before publication.
Footnotes
1 Abbreviations used in this paper: IL-12R, IL-12 receptor; Stat, signal transducers and activators of transcription.
References
- 1.Coffman RL, Lebman DA, Rothman P. The mechanism and regulation of immunoglobulin isotype switching. Adv Immunol. 1993;54:228–269. doi: 10.1016/s0065-2776(08)60536-2. [DOI] [PubMed] [Google Scholar]
- 2.Seder RA, Paul WE. Acquisition of lymphokine-producing phenotype by CD4+T cells. Annu Rev Immunol. 1994;12:635–673. doi: 10.1146/annurev.iy.12.040194.003223. [DOI] [PubMed] [Google Scholar]
- 3.Romagnani S. Lymphokine production by human T cells in disease states. Annu Rev Immunol. 1994;12:227–257. doi: 10.1146/annurev.iy.12.040194.001303. [DOI] [PubMed] [Google Scholar]
- 4.Abbas AK, Murphy KM, Sher A. Functional diversity of helper T lymphocytes. Nature (Lond) 1996;383:787–793. doi: 10.1038/383787a0. [DOI] [PubMed] [Google Scholar]
- 5.Seder RA, Paul WE, Davis MM, de St BF, Groth The presence of interleukin-4 during in vitro priming determines the lymphokine-producing potential of CD4+T cells from T cell receptor transgenic mice. J Exp Med. 1992;176:1091–1098. doi: 10.1084/jem.176.4.1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hsieh CS, Heimberger AB, Gold JS, O'Garra A, Murphy KM. Differential regulation of T helper phenotype development by interleukins 4 and 10 in an alpha beta T cell–receptor transgenic system. Proc Natl Acad Sci USA. 1992;89:6065–6069. doi: 10.1073/pnas.89.13.6065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hsieh C-S, Macatonia SE, Tripp CS, Wolf SF, O'Garra A, Murphy KM. Development of TH1 CD4+ T cells through IL-12 produced by Listeria-induced macrophages. Science (Wash DC) 1993;260:547–549. doi: 10.1126/science.8097338. [DOI] [PubMed] [Google Scholar]
- 8.Manetti R, Parronchi P, Giudizi MG, Piccinni M-P, Maggi E, Trinchieri G, Romagnani S. Natural killer cell stimulatory factor (interleukin 12 [IL-12]) induces T helper 1 type (Th1)-specific immune responses and inhibits the development of IL-4-producing Th cells. J Exp Med. 1993;177:1199–1204. doi: 10.1084/jem.177.4.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seder RA, Gazzinelli R, Sher A, Paul WE. IL-12 acts directly on CD4+T cells to enhance priming for interferon γ production and diminishes interleukin 4 inhibition of such priming. Proc Natl Acad Sci USA. 1993;90:10188–10192. doi: 10.1073/pnas.90.21.10188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Magram J, Connaughton SE, Warrier RR, Carvajal DM, Wu C-Y, Ferrante J, Stewart C, Sarimiento U, Faherty DA, Gately MK. IL-12 deficient mice are defective in IFNγ production and type I cytokine responses. Immunity. 1996;4:471–481. doi: 10.1016/s1074-7613(00)80413-6. [DOI] [PubMed] [Google Scholar]
- 11.Kühn R, Rajewsky K, Müller W. Generation and analysis of interleukin-4–deficient mice. Science (Wash DC) 1991;254:707–710. doi: 10.1126/science.1948049. [DOI] [PubMed] [Google Scholar]
- 12.Kopf M, Le Gros G, Bachmann M, Lamers MC, Bluethmann H, Köhler G. Disruption of the murine IL-4 gene blocks Th2 cytokine responses. Nature (Lond) 1993;362:245–248. doi: 10.1038/362245a0. [DOI] [PubMed] [Google Scholar]
- 13.Kaplan MH, Schindler U, Smiley ST, Grusby MJ. Stat6 is required for mediating responses to IL-4 and for the development of Th2 cells. Immunity. 1996;4:313–319. doi: 10.1016/s1074-7613(00)80439-2. [DOI] [PubMed] [Google Scholar]
- 14.Takeda K, Tanaka T, Shi W, Matsumoto M, Minami M, Kashiwamura S-I, Nakanishi K, Yoshida N, Kishimoto T, Akira S. Essential role of Stat6 in IL-4 signalling. Nature (Lond) 1996;380:627–630. doi: 10.1038/380627a0. [DOI] [PubMed] [Google Scholar]
- 15.Shimoda K, van Deursen J, Sangster MY, Sarawar SR, Carson RT, Tripp RA, Chu C, Quelle FW, Nosaka T, Vignalli DAA, et al. Lack of IL-4–induced Th2 response and IgE class switching in mice with disrupted Stat6 gene. Nature (Lond) 1996;380:630–633. doi: 10.1038/380630a0. [DOI] [PubMed] [Google Scholar]
- 16.Thierfelder WE, van Deursen JM, Yamamoto K, Tripp RA, Sarawar SR, Carson RT, Sangster MY, Vignali DAA, Doherty PC, Grosveld GC, Ihle JN. Requirement for Stat4 in interleukin-12–mediated responses of natural killer and T cells. Nature (Lond) 1996;382:171–174. doi: 10.1038/382171a0. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan MH, Sun Y-L, Hoey T, Grusby MJ. Impaired IL-12 responses and enhanced development of Th2 cells in Stat4-deficient mice. Nature (Lond) 1996;382:174–177. doi: 10.1038/382174a0. [DOI] [PubMed] [Google Scholar]
- 18.Coligan, J.E., A.M. Kruisbeek, D.H. Margulies, E.M. Shevach, and W. Strober. 1991. Current Protocols in Immunology. 1st ed. Greene & Wiley, New York. 7.1–7.8.
- 19.Lanzavecchia A, Scheidegger D. The use of hybrid hybridomas to target human cytotoxic T lymphocytes. Eur J Immunol. 1987;17:105–111. doi: 10.1002/eji.1830170118. [DOI] [PubMed] [Google Scholar]
- 20.Gallati H, Pracht I, Schmidt J, Häring P, Garotta G. A simple, rapid and large capacity ELISA for biologically active native and recombinant human IFN-γ. J Biol Regul Homeostatic Agents. 1987;1:109–118. [PubMed] [Google Scholar]
- 21.Perussia B, Starr S, Abraham S, Fanning V, Trinchieri G. Human natural killer cells analyzed by B73.1, a monoclonal antibody blocking Fc receptor functions. I. Characterization of the lymphocyte subset reactive with B73.1. J Immunol. 1983;130:2133–2139. [PubMed] [Google Scholar]
- 22.Norton AJ, Ramsay AD, Smith SH, Beverly PCL, Isaacson PG. Monoclonal antibody (UCHL-1) that recognizes normal and neoplastic T cells in fixed tissues. J Clin Pathol (Lond) 1986;39:399–405. doi: 10.1136/jcp.39.4.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cammarota G, Scheirle A, Takacs B, Doran DM, Knorr R, Bannwarth W, Guardiola J, Sinigaglia F. Identification of a CD4 binding site on the β2domain of HLA-DR molecules. Nature (Lond) 1992;356:799–801. doi: 10.1038/356799a0. [DOI] [PubMed] [Google Scholar]
- 24.Sinigaglia F, Romagnoli P, Guttinger M, Takacs B, Pink JRP. Selection of T cell epitopes and vaccine engineering. Methods Enzymol. 1991;203:370–386. doi: 10.1016/0076-6879(91)03021-8. [DOI] [PubMed] [Google Scholar]
- 25.Presky DH, Yang H, Minetti LJ, Chua AO, Nabavi N, Wu C-Y, Gately MK, Gubler U. A functional interleukin-12 receptor complex is composed of two β type cytokine receptor subunits. Proc Natl Acad Sci USA. 1996;93:14002–14007. doi: 10.1073/pnas.93.24.14002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chua AO, Chizzonite R, Desai BB, Truitt TP, Nunes P, Minetti LJ, Warrier RR, Presky DH, Levine JF, Gately MK, Gubler U. Expression cloning of a human IL-12 receptor component: a new member of the cytokine receptor superfamily with strong homology to gp130. J Immunol. 1994;153:128–136. [PubMed] [Google Scholar]
- 27.Passini N, Larigan JD, Genovese S, Appella E, Sinigaglia F, Rogge L. The 37/40-kilodalton autoantigen in insulin-dependent diabetes mellitus is the putative tyrosine phosphatase IA-2. Proc Natl Acad Sci USA. 1995;92:9412–9416. doi: 10.1073/pnas.92.20.9412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chizzonite R, Truitt T, Desai BB, Nunes P, Podlaski FJ, Stern AS, Gately MK. IL-12 receptor. I. Characterization of the receptor on phytohemagglutininactivated human lymphoblasts. J Immunol. 1992;148:3117–3124. [PubMed] [Google Scholar]
- 29.McPherson GA. Analysis of radioligand binding experiments. A collection of computer programs for the IBM PC. J Pharmacol Methods. 1985;14:213–228. doi: 10.1016/0160-5402(85)90034-8. [DOI] [PubMed] [Google Scholar]
- 30.Szabo SJ, Jacobson NG, Dighe AS, Gubler U, Murphy KM. Developmental commitment to the Th2 lineage by extinction of IL-12 signaling. Immunity. 1995;2:665–675. doi: 10.1016/1074-7613(95)90011-x. [DOI] [PubMed] [Google Scholar]
- 31.Bacon CM, Petricoin EF, III, Ortaldo JR, Rees RC, Larner AC, Johnston JA, O'Shea JJ. Interleukin 12 induces tyrosine phosphorylation and activation of STAT4 in human lymphocytes. Proc Natl Acad Sci USA. 1995;92:7307–7311. doi: 10.1073/pnas.92.16.7307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jacobson NG, Szabo SJ, Weber-Nordt RN, Zhong Z, Schreiber RD, Darnell JE, Murphy KM. Interleukin 12 signaling in T helper type 1 (Th1) cells involves tyrosine phosphorylation of signal transducer and activator of transcription (Stat) 3 and 4. J Exp Med. 1995;181:1755–1762. doi: 10.1084/jem.181.5.1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bacon CM, McVicar DW, Ortaldo JR, Rees RC, O'Shea JJ, Johnston JA. Interleukin 12 (IL-12) induces tyrosine phosphorylation of Jak2 and Tyk2: differential use of Janus family tyrosine kinases by IL-2 and IL-12. J Exp Med. 1995;181:399–404. doi: 10.1084/jem.181.1.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chua AO, Wilkinson VL, Presky DH, Gubler U. Cloning and characterization of a mouse IL-12 receptor-beta component. J Immunol. 1995;155:4286–4294. [PubMed] [Google Scholar]
- 35.Manetti R, Gerosa F, Giudizi MG, Biagiotti R, Parronchi P, Piccinni M-P, Sampognaro S, Maggi E, Romagnani S, Trinchieri G. Interleukin 12 induces stable priming for interferon γ (IFN-γ) production during differentiation of human T helper (Th) and transient IFN-γ production in established Th2 cell clones. J Exp Med. 1994;179:1273–1283. doi: 10.1084/jem.179.4.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yssel H, Fasler S, de Vries JE, de Waal R, Malefyt IL-12 transiently induces IFN-γ transcription and protein synthesis in human CD4+allergen-specific Th2 T cell clones. Int Immunol. 1994;6:1091–1096. doi: 10.1093/intimm/6.7.1091. [DOI] [PubMed] [Google Scholar]
- 37.Parronchi P, Mohapatra S, Sampognaro S, Giannarini L, Wahn U, Chong P, Mohapatra S, Maggi E, Renz H, Romagnani S. Effects of interferon-α on cytokine profile, T cell receptor repertoire and peptide reactivity of human allergen-specific T cells. Eur J Immunol. 1996;26:697–703. doi: 10.1002/eji.1830260328. [DOI] [PubMed] [Google Scholar]
- 38.Wenner CA, Güler ML, Macatonia SE, O'Garra A, Murphy KM. Roles of IFN-γ and IFN-α in IL-12 induced T helper cell–1 development. J Immunol. 1996;1156:1442–1447. [PubMed] [Google Scholar]