Abstract
Injection drug use is a growing problem on the US–Mexico border, where Tijuana is situated. We studied the context of injection drug use among injection drug users (IDUs) in Tijuana to help guide future research and interventions. Guided in-depth interviews were conducted with 10 male and 10 female current IDUs in Tijuana. Topics included types of drug used, injection settings, access to sterile needles, and environmental influences. Interviews were taped, transcribed verbatim, and translated. Content analysis was conducted to identify themes. Of the 20 IDUs, median age and age at first injection were 30 and 18. Most reported injecting at least daily: heroin (“carga,” “chiva,” “negra”), methamphetamine (“crico,” “cri-cri”), or both drugs combined. In sharp contrast to Western US cities, almost all regularly attended shooting galleries (“yongos” or “picaderos”) because of the difficulties obtaining syringes and police oppression. Almost all shared needles/paraphernalia [“cuete” (syringe), “cacharros” (cookers), cotton from sweaters/socks (filters)]. Some reported obtaining syringes from the United States. Key themes included (1) pharmacies refusing to sell or charging higher prices to IDUs, (2) ample availability of used/rented syringes from “picaderos” (e.g., charging approximately 5 pesos or “10 drops” of drug), and (3) poor HIV/AIDS knowledge, such as beliefs that exposing syringes to air “kills germs.” This qualitative study suggests that IDUs in Tijuana are at high risk of HIV and other blood-borne infections. Interventions are urgently needed to expand access to sterile injection equipment and offset the potential for a widespread HIV epidemic.
Keywords: Border, HIV/AIDS, Injection drug use, Mexico, Needle exchange programs, Pharmacies
INTRODUCTION
Tijuana, Mexico, is home to an estimated population of 1.27 million people and is adjacent to the city of San Diego, California.1 The area of Tijuana covers 1,393 km2 compared with San Diego which is almost eight times larger in size.2 The population of Tijuana is growing at a very fast pace given the large numbers who migrate to this city. In 1990, it was estimated that 56% of the population in Tijuana was born elsewhere in Mexico.3 With more than 40,000 vehicles and 25,000 pedestrians crossing the border each day, the US–Mexico border crossing at San Ysidro—an ambiguous line that separates Tijuana from San Diego, California—is reportedly the busiest port of entry in the world.4 It is estimated that almost one quarter of Tijuana’s population over 5 years old has recently arrived in Tijuana or is in transit on their way to the United States.3 There are tremendous social inequities along the 2,000 mile border between the Unites States and Mexico, which is the most extensive land frontier separating a developed and developing country. The gap in median incomes between inhabitants of Mexico, and the United States is reportedly the largest between any two contiguous countries.5 In 2004, the per capita gross domestic product in the United States was estimated at $37,800, whereas the per capita gross domestic product for Mexico was $9000 in 2003.6 The municipal budgets of San Diego and Tijuana between the years of 1996 and 1998 were $49 million and $3 million, respectively.2
After Colombia, Mexico is the second most important source of heroin entering the United States, accounting for 30% of all heroin sold in the United States and 98% of heroin sold west of the Mississippi river.7 Given its proximity to the United States and the heavy traffic at the border crossing, Tijuana is positioned along a major drug trafficking route whereby heroin, cocaine, and methamphetamine are transported to the United States. It has been demonstrated elsewhere that cities and towns positioned on drug trafficking routes often experience burgeoning injection drug use epidemics among their residents.8–10 However, only recently has the growing number of injection drug users (IDUs) in Tijuana been recognized as a public health problem.11
Tijuana is thought to have one of the fastest growing IDU populations in Mexico.12,13 In 2004, it was estimated that there were approximately 6,000 persons injecting in more than 200 shooting galleries in Tijuana, typically defined as abandoned houses, hidden rooms, or alleyways where people inject in groups. In a study that mapped approximately 600 high and low density neighborhoods (“colonias”) of injection drug use in Tijuana, heavy drug use was observed in the Zona Norte, an area very close to the US–Mexico border.14 In recent years, there has been a dramatic increase in the cultivation of opium poppy in Mexico.11 Increases in heroin trafficking and purity in Mexico coupled with decreasing prices appear to have fueled an injection drug use epidemic that is virtually unstudied.
The joint United Nations Programme on HIV/AIDS considers Mexico a country of low HIV/AIDS prevalence,15 but the distribution of known HIV infections varies by region. HIV prevalence in the adult Mexican population is estimated at 0.28%,16,17 but is nearly double this figure in Baja California, where Tijuana is located. Baja California ranks third in HIV prevalence among Mexico’s 32 states.16 Recent reports suggest that national and state-level HIV/AIDS surveillance data may mask a dynamic HIV subepidemic among drug users in Baja California. In 2003, a study by Viani et al.18 found that in a sample of over 1,000 women in labor at Tijuana General Hospital, HIV prevalence was 1.1% overall, 0% among non-drug-using women, and 6% among those admitting to injecting drugs. Also in 2003, HIV prevalence among street-recruited IDUs and female sex workers in Tijuana was 6% and 10%, respectively (Dr. Carlos Magis, oral communication, August 2004). In a cross-sectional study of risk behaviors and HIV infection among IDUs in Tijuana in 2003, half of the male IDUs in Tijuana reported sex with men; this subgroup had three-fold higher odds of recent needle sharing than other IDUs.19 The availability of access to sterile syringes for IDUs who cannot or will not cease injecting has been associated with low, stable rates of HIV infection among IDUs in many international settings.20–22 Although no needle exchange programs (NEPs) currently operate in Tijuana, there are 1,630 registered pharmacies where IDUs can theoretically purchase syringes legally over the counter. Despite this, access to sterile syringes among IDUs in Tijuana may be limited.11 Studying the context through which micro- and macroconditions create vulnerabilities to the acquisition of blood-borne viruses may help identify avenues for intervention in Tijuana and other Mexican border cities and their US counterparts. Given the paucity of information on injection behaviors in Tijuana, we conducted a qualitative study to describe the context of injection drug use and HIV-related injection risks and resiliencies among IDUs in Tijuana. These data were also used to develop a conceptual framework for understanding the risk environment to aid hypothesis testing in subsequent quantitative studies.
METHODS
In April and May, 2004, a team of four Mexican interviewers conducted guided in-depth interviews with 20 IDUs (10 males, 10 females) residing in Tijuana who injected at least once within the prior month. Qualitative methods allow the researcher to explore life experiences within a social context without preestablished parameters or variables.23 Through the administration of depth interviews, a richer, more holistic insight into injection drug use in Tijuana could be obtained. To understand the variability in drug-use practices, we used targeted sampling methods24 to recruit a balanced number of IDUs who used opiates (i.e., heroin) and stimulants (e.g., cocaine, methamphetamine). Interviewers contacted potential participants and informally screened for eligibility in street locations known for drug use, in shooting galleries and in drug treatment programs. After providing written informed consent, a brief, structured screening form consisting of 20 questions was administered by the interviewer to collect sociodemographic information such as age, employment status, and primary drug used. To optimize rapport, interviewers were matched to respondents based on gender. Interviews were conducted in private locations based on availability and client preference (e.g., drug-treatment programs, outreach offices, and participants’ homes).
The interviewer then engaged the participant in an open-ended interview. A general interview checklist was used to ensure that certain topics were addressed, but the interview was open-ended and conversational. Interview topics included types of drugs used, injection settings and venues, perceived barriers related to acquiring sterile injection equipment, and environmental influences affecting drug use (e.g., police and border security). Each interview lasted approximately an hour and was tape-recorded for subsequent transcription and translation; no identifiers were recorded. Participants in the study received 200 pesos (approximately $20) as compensation for their time.
Interviews were taped, transcribed verbatim, and translated from Spanish into English. A dictionary was developed to catalog various words and phrases used in the local drug culture. Content analysis was conducted to identify primary risk-related themes corresponding to the interview guide and the study’s main objectives. Transcripts were coded by hand for themes, primarily by one investigator (Michelle Firestone). A second investigator (Patricia Case) coded a sample of transcript extractions independently, and the two codings were compared to check for consistency. Where there was inconsistency in coding, the discrepancy was discussed for clarification and the second investigator then coded another sample of transcript extractions. This process was repeated until consistency in coding was attained.
RESULTS
Sociodemographic characteristics of the study sample are summarized in Table 1. Of the 20 respondents, the median age was 30 and the median age of first injection was 18. Almost two thirds were born in Baja California, and one third reported being currently employed. In drug use, over half reported that the main drug they injected in the previous 6 months was heroin; however, one quarter reported primarily injecting heroin and methamphetamine in combination, which was referred to by one participant as a “Mexican speedball” (Table 2).
TABLE 1.
Sociodemographic data among injection drug users (IDUs) in Tijuana, Mexico (N = 20)
| Variable | Median | Minimum | Maximum |
|---|---|---|---|
| Age (years) | 30 | 18 | 47 |
| Age of first injection (years) | 18 | 13 | 34 |
| Time spent on the streets/day (h) | 10.5 | 1 | 24 |
|
| |||
| % | |||
|
| |||
| Male | 50 | ||
| Presently employed | 30 | ||
| Born in Tijuana | 65 | ||
| Civil status | |||
| Single | 25 | ||
| Married | 60 | ||
| Divorced | 0 | ||
| Separated | 10 | ||
| Widowed | 5 | ||
| In last 6 months, lived or slept in any of the following places | |||
| The house/flat of parent/relative/partner or friend | 85 | ||
| Work place/rented room | 45 | ||
| Car, bus, truck, or other vehicle | 45 | ||
| Abandoned building | 45 | ||
| Jail, prison, or detention center | 60 | ||
| Drug treatment center | 45 | ||
| On the streets | 40 | ||
TABLE 2.
Injection and sexual behavior among injection drug users (IDUs) in Tijuana, Mexico (N = 20)
| Behaviors occurring in the prior 6 months | % |
|---|---|
| Injected drugs | |
| Heroin + methamphetamine | 60 |
| Heroin + cocaine | 15 |
| Heroin alone | 85 |
| Methamphetamine alone | 75 |
| Cocaine alone | 20 |
| Tranquilizers | 25 |
| Barbiturates | 5 |
| Other | 10 |
| Most frequently injected drug | |
| Heroin + methamphetamine | 25 |
| Heroin alone | 60 |
| Methamphetamine alone | 15 |
| Frequency of injection | |
| Every day | 90 |
| 4–6 times a week | 5 |
| 2–3 times a week | 5 |
| When was last time injected? (days ago) | |
| 0–today | 70 |
| 1 | 10 |
| 2 | 5 |
| 11 | 10 |
| 21 | 5 |
| Received money/drugs for sex* | 15† |
| Gave drugs for sex* | 5‡ |
| Sex partner is an IDU* | 50 |
N = 16.
All were female and reported receiving money in exchange for sex.
Pertains to one male who gave drugs in exchange for sex with a female.
Context of Syringe Sharing
During the interview, 80% of the participants reported that they share syringes regularly with other IDUs. For some IDUs, this meant sharing only with a spouse, family member, or someone they trusted. For example, when one male IDU was asked if he had ever shared syringes or drugs, he said: “Syringes, yes with my brother. He is the only one that I share with” (male, age 20). A female IDU explained
I almost only share with my husband, very seldom times, when there is no other option, when I don’t have my stuff very rarely when I don’t have my stuff, but I can tell you that there are tecatos [heroin users] that share the same, as I tell you, my husband and I have let others borrow them and everything, but it depends on if it is someone we know and trust, but when we share its because we are going to let them keep it, ahh “keep it, because we don’t need it, take it for you, we can buy another one”, because my husband has to use new ones often, if possible daily but not always, we buy often. (female, age 43)
However, for the majority of respondents, sharing needles was considered a common occurrence:
Mmm, yes, truthfully, it’s rare for someone to just use their own [syringe] for themselves, most of them share, they’re not as selfish as one says that they don’t want to give any to one sometimes, because one has the malilla [heroin withdrawal] and if they have some and one doesn’t, but most everyone, we all share. (male, age 44)
Harm-reduction messages and outreach programs like the prevemovihl, a mobile HIV prevention unit supported by the municipal HIV/AIDS committee in Tijuana have likely influenced syringe disinfection practices among some IDUs. For example, one male IDU reported that although he was aware that bleach should be used to clean a syringe before injecting, this is not what happens when the pressures of withdrawal begin to set in:
When one is done using, you wash it with water and the next guy uses it; when one is beginning, you wash it with bleach, but after a while, when you’re real “malilla” and what you want is the cure [to inject yourself], you just rinse it with water and use it just like that . . . (male, age 38)
Use of other nonsterile-injection equipment that could lead to abscesses, cellulitis, or endocarditis was also commonly cited, such as the sharing of “cacharros” (cookers), filters (which were often cotton pulled from sweaters/socks), and unclean water to wash syringes. As one woman explained: “The cacharro [cooker] was from the trash, the syringe I bought, the water from here [pointing to tap], the cotton from a sweatshirt, from any sweatshirt” (female, age 18).
At shooting galleries (referred to as “yongos” or “picaderos”), syringes were reportedly loaned and borrowed in exchange for several drops (“gotas”) of prepared drug, typically heroin. One woman described her experience:
Well I went to a place and sometimes . . . they don’t have one [syringe], so I went to another place and I asked, “hey loan me this” and you have to give the person some drops, a little and they let you use one, they loan the syringe. (female, age 42)
One man explained that there is a specific name for sharing half of one’s drugs with someone else and using the same syringe “ . . . it’s like a ‘vaquero’ [cow] . . . you say ‘we’re going to do a vaquero’ and we do half and half” (male, age 38).
When participants were asked whether drug users in Tijuana share their blood when they share syringes, 15 of the 20 IDUs reported having either seen or heard of such behavior in Tijuana. The sharing of blood seemed to occur as a consequence of not cleaning syringes properly or not wanting to waste the drug preparation and did not appear to be linked to a desire for a more intense high, as two respondents explained:
[W]ell, yes, it happens to happen, if the syringe isn’t washed for example, when I use the syringe and I loan it to another and the other is the one who rinses it when one cures, the little bleeding that . . . that the needle leaves, the other one washes, and they’re 2 or 3 washes with just water, so there can be some transmission of blood from a tiny drop of blood in the water that we use to wash the syringes. (male, age 25)
I think it’s like a slip-up of the person, right? Of the person who’s asking for the borrowed syringe and well, if there’s a responsible person for the person who’s loaning the syringe with blood because, one is crazy, right? When one feels bad he doesn’t care if you get a dirty syringe or it has blood in it, one doesn’t care . . . (female, age 18)
Another woman felt that rinsing a syringe with blood in it could mean losing a few drops of drug, a loss she was not willing to accept.
There is a certain amount of blood in the syringe, in that cuete [syringe], so now you left me less dose, or I left less dose for you, so if you do it, you lift, even if you don’t lift everything, like more than 7 calos [lines on the syringe], and you leave me my 7 calos there, then I don’t care, I’m not going to care when you inject, I’m not going to care about rinsing the syringe, why? Because in between blood or no blood there’s going to be a few drops [of drug] that are useful to me so I don’t care, even if ah . . . even if it comes back and you do it again and again, right? If you get the dose and it doesn’t mark, you pull it again including the blood, and you try to put it in again and you pull it out again, I don’t care if that’s your blood, understand? I’ll get it like it is and mark myself, I’ll put it in and I won’t care if it comes with blood from you, and you’re not going to care if it comes with my blood because you need the dose now and the addict is like that. I am like that. (female, age 22)
On the other hand, the context of needle sharing may be determined by social norms within specific networks. One male participant insisted that the drug users he associated with did not share blood, whereas a female participant explained that neither blood nor syringes were shared.
No, everyone uses their own syringe, and we call it a “cuete” [rocket], the syringe, everyone uses their own cuete and they rinse it. (female, age 18)
Barriers to Sterile Syringe Access
Although purchasing syringes at a pharmacy without a prescription is legal in Tijuana, in practice, many participants encountered difficulties when trying to buy syringes. Many pharmacists or clerks refused to sell syringes to persons they perceived to be IDUs, whereas others charged them higher prices. Several IDUs described the tactics they developed in an attempt to overcome such obstacles, such as claiming to be a diabetic or purchasing syringes in a veterinary clinic.
I buy them in the pharmacy and they cost 13 [pesos] sometimes, they can cost up to 20 in a pharmacy, I’ve even bought a syringe for 100 pesos [$9 equivalent] . . . almost all pharmacies will refuse to sell them. I’ll give a story about how they’re for insulin, for someone diabetic, they still refuse to sell them. That pharmacy that I know . . . I found it through some friends that use drugs also, and that was how I learned where to buy them, it’s the only pharmacy that sells them right away. (female, age 22)
Syringes, well, I can acquire a syringe in a vet pharmacy. I do that, I do it with lies supposedly, but the truth is that a lot [pharmacy employees] detect me and they won’t sell it to me, but there are places where, there are vet pharmacies where one asks for one [syringe] for a rooster, just like that you go and ask for a rooster, and it’s for putting in some vitamins into the rooster, see. (male, age 30)
One participant explained that nighttime pharmacy employees will charge more for a syringe and will then pocket the extra money.
We were in Plaza Rio and I was really crazy, I don’t remember exactly the location of the pharmacy, but they sold it for 45 pesos, so if the price goes up it depends on the type of person, no? It was at night, and the employee gets that money for himself, it’s not the pharmacy but the person in charge at night . . . (female, age 22)
Two participants reported buying syringes in pharmacies in the United States.
It’s been a long time since I bought syringes, no, because I bought, like, 20 with my sister from the other side, she brought them here from San Diego. (female, age 47) They can be expensive [syringes]. Sometimes I buy just one for 5 pesos, each one, sometimes up to 10, I’ve paid up to 20 pesos on the street . . . but most of the time, my wife brings me boxes of syringes from the other side [USA]. (male, age 44)
Almost all IDUs in Tijuana reported regularly attending shooting galleries, which were typically described as abandoned houses, hidden rooms, and alleyways. Coupled with the challenges of purchasing new syringes and the influence and oppression of the police in Tijuana, IDUs were increasingly forced to rent and borrow used syringes from picaderos. A female IDU described how these environmental factors influenced her injection behavior and the choices she feels forced to make:
It depends on the place where we were and how much money I had and who the person was, or rather how much you were willing to give . . . if the place was “hot”, because of the police and all that, there’s times when you can’t get a syringe in a pharmacy even if you have money. Sometimes a pharmacy is open and you don’t have money, even 13 pesos, then you know that you lift only what you’re going to inject, you don’t care about the syringe (inaudible), and you could rent them. (female, age 22)
Participants commonly reported being charged 5 pesos or “10 drops” of drug to access a syringe and inject themselves at an established shooting gallery. One male participant explained this process:
The oldest one in the place is the one that charges the “sica”, the “sica” is what you call what you have to leave, by law, when you go to a shooting gallery, for instance, I go to a shooting gallery, I put my dose where I’m going to dilute it and before injecting that dose, I have to give ten lines of the insulin syringe to the person in charge of the shooting gallery, because he’s in charge of maintaining the place, understand? (male, age 30)
In some cases, shooting gallery operators exerted some influence on injection behaviors occurring in their establishment. From the perspective of one such shooting gallery operator, he maintained “laws” to protect all his clients from infection:
I destroy the syringes that they use or if I loan them a syringe so that they can use it new I give it to them, take it! When they don’t have one I give them one and I make them take it or I destroy it, most of the time they have their own syringe, they are the syringes that they carry around with them all the time . . . it’s a law that I have, because each shooting gallery has laws, no one is allowed to lay a hand on my table . . . So I try to have some rules in the place so that there won’t be contamination, or we all get infected. (male, age 44)
Although this shooting gallery operator felt strongly that he was preventing infection, he nevertheless described situations where he allowed IDUs to retrieve used syringes from the disposal can, suggesting that lack of access to sterile syringes can still drive risks.
I ask him if he has a syringe, if he doesn’t have one I give it and when he’s done, I give him a can and he throws it there, if they’re going to keep it they take it, if they’re going to leave it they throw it in the can and I destroy the can because of the syringes that are in it . . . there have been persons that come and I don’t have new syringes they get them from the can to use.
In contrast, a few IDUs reported no problems in obtaining syringes. One participant said: “Well in the pharmacies they sell to any person . . . they sell syringes” (male, age 25).
I am one of those who go to the pharmacy or barn to buy my syringe and well, they sell it to me easy. (male, age 39)
Influence of Police
Police presence was cited as a main reason why IDUs sought to inject in shooting galleries
We do it that way [inject] in “yongos”, those are shooting galleries, abandoned lots, abandoned houses . . . we do it this way because we don’t want to be seen by the authorities. (male, age 30)
Both male and female IDUs characterized their experiences with the police in Tijuana as violent, corrupt, and frightening. Most of these interactions resulted in arrest followed by 36 h spent in jail (“pinta”). Visible track marks and possession of used or sterile syringes—even in the absence of drug possession—were common causes for arrest. One male IDU described how the Tijuana police confiscated syringes and drugs:
Even if you don’t have anything! They [police] arrest you and if you have a syringe, they give you the maximum in jail for minor infractions which is 36 hours. Just for having a syringe even if you don’t have any drugs, now if you have drugs, you have a syringe and it’s already made and in the syringe, if a friend of theirs comes around and is an addict and – I say “friend” because they have him as an informant – they take away my dose and give it to him, you understand? And if their friend doesn’t come along, they throw it at me, in my face and if the syringe isn’t made [loaded with drugs] they break it and throw it away and they take the drugs, and they don’t even present it to the judge, you know, they sell it to another addict, when it’s large amounts they take it away, they give it to a certain person that they’ve scared or that they have as an employee selling drugs, that’s the truth. (male, age 30)
A female participant explained that her appearance alone could influence the degree to which the police harass her:
He [policeman] saw that I had an addict face, and he saw me dirty, the jacket that I had was dirty, because when I’m dressed up – I’m not dressed up now, I haven’t showered – but when I’m dressed up they don’t bother me at all, they don’t bother me at all, at all, they don’t even look at me, if they see my face and see that I’m wearing makeup, “that lady is a homemaker.” (woman, age 47)
HIV/AIDS Knowledge
For the most part, participants had relatively good awareness that HIV/AIDS transmission could occur through syringe sharing. A number of participants also linked diseases like tuberculosis and hepatitis to injection drug use. For example, when IDUs were asked about diseases that can be passed by consuming drugs or sharing a needle, one male participant explained:
Tuberculosis, the ones that you mentioned, AIDS, I know that it’s a disease that doesn’t have a cure, right, that can be controlled a little if it’s detected early, right? I know that, it destroys the body’s defenses, right, the hepatitis; I know that there’s type A, B and C. I know that it can be caught also by contact with blood. (male, age 30)
There was, however, a range of understanding, and among some IDUs, a lack of confidence about which diseases were or were not spread through contaminated syringes, as reflected by one participant when asked whether there were diseases that could be spread by injecting drugs:
Well, AIDS, hepatitis, many, the problem is that they pass their blood, if someone is sick in the blood, hepatitis, AIDS, and I only know those two that can pass by the blood, another I don’t know if it passes through the blood, other cases a person has lupus they can’t get, a person to another person can’t get cancer, passing blood from other people, hepatitis yes, and AIDS yes. (female, age 42)
Some participants had had been provided with misinformation, and their understanding of HIV/AIDS transmission was very low, as suggested by one participant’s description of how he cleaned syringes:
No, well, I . . . I rinse it many times with water, because if . . . there’s no bleach . . . with water and . . . I . . . take out the stopper and . . . so that it gets air in it, because someone told me that when the air hits it . . . the bacteria . . . the AIDS bacteria . . . it dies and that’s what I try to do. (male, age 22)
Another participant reported hearing similar misinformation from a doctor:
One doctor told me that if I don’t want to get infected with AIDS and because the virus dies with air, he said to take the thing out so it will get air [in] to . . . the syringe . . . and then I insert it again and I rinse it. (male, age 37)
One participant thought that HIV could be seen with the naked eye:
With the needles, they say there’s no blood in it, but the virus is really small, I’ve seen it with a magnifying glass, a very small animal I saw, tiny, tiny, the AIDS virus I say, and another one [disease] can be . . . from the lungs. (female, age 47)
Another woman appeared to suggest that HIV was a man-made virus when she was asked whether people spoke about AIDS on the street:
Yes, we spend our time talking about that, or rather if we know about how it’s passed and all that . . . they say that it’s a – what do you call it – a disease – that some dudes, I don’t remember where they invented it, to kill us or something, I don’t know what, they got it from monkeys and like that, we start talking about it but, the virus, the virus is already made, it’s just, it has to be developed and we all have it, that’s it. (female, age 18)
Awareness and Acceptability of NEPs
Only three of the twenty participants had heard of an NEP or were aware of its purpose. Although awareness of NEPs was limited, once the idea was explained, the majority of participants expressed an interest in having NEPs implemented in Tijuana. When asked whether people in Tijuana would take advantage of a NEP, IDUs said:
Of course, because it’s to prevent diseases right, so you could have your syringe for yourself right, not be using someone else’s even if it was washed, but germs are still left behind. (male, age 44)
Yes, in reality yes I think so, it’s something very good, there wouldn’t be as many venereal diseases, understand? It would be more controlled and it would be taken advantage of. (male, age 30)
Because to avoid to get a disease, well yeah not to get sick and here well, in the last 2 years, I have heard a lot of people that have been infected with AIDS, because of that, because they were using other people’s syringes, yes I think so, well and me, well yes I think so, I will make good use of it in case they would have a program like that here. (female, age 27)
A few subjects, however, were concerned that police pressure could undermine the feasibility of an NEP in Tijuana. When asked whether people would feel safe attending a NEP, one IDU answered
No well . . . if the police finds the “R” [abbreviation for ‘rocket’, meaning syringe] on you, they take you . . . who knows . . . only because they have a permit and said “no, I got this from the program ‘x’, only that way they would not take you . . . (male, age 20)
In contrast, one female IDU associated the concept of a needle exchange program with increased risk and exposure to diseases: “Being in a needle exchange program you could get a disease or AIDS” (female, age 27).
DISCUSSION
Although previous studies suggest that HIV prevalence among IDUs in Tijuana has thus far remained low, our study of the context of HIV-risk behaviors in this city suggests that this situation could soon change. Our study revealed high-risk injection behaviors amidst social and environmental influences that appeared to exacerbate the risk environment. The main themes emerging from our analysis included barriers to sterile syringe access, ample access to used syringes that are rented or bought, constant police pressure that created a perceived need to inject in shooting galleries, and low HIV/AIDS awareness. Below, we discuss how these factors appeared to influence syringe sharing in Tijuana, in comparison with other international settings.
Most of the IDUs we interviewed reported that syringe sharing was a common occurrence. Not surprisingly, multi-person use of syringes appeared to be primarily driven by the inability to procure a consistent supply of sterile syringes. In contrast to some cities in the United States, Canada, and Pakistan (Kuo I, Ul-Hasan T, Galai N, et al., unpublished data, 2004),25,26 we did not find evidence of practice of “booting” or “jerking,” which is the intentional sharing of blood to intensify the high.
Although there are no laws prohibiting the purchase of syringes at pharmacies without a prescription in Baja California, most IDUs reported that pharmacies refused to sell syringes to persons they perceived to be IDUs. It has been well established in other settings that restrictive prescription and paraphernalia laws are associated with needle sharing and syringe reuse,27–29 but even in the absence of such regulations, the inability of IDUs to purchase syringes has been linked to nonpermissive attitudes of individual pharmacists.30–32 To combat this trend, Tijuana officials held a meeting in 2003 to inform pharmacists that denying IDUs access to sterile syringes can lead to increased needle sharing and increased transmission of HIV and other blood-borne infections.11 Our findings suggest that further educational efforts of this kind are needed, not only with pharmacists, but also with pharmacy clerks who may also refuse to sell syringes or sell to IDUs at higher prices.
The existence of numerous shooting galleries in Tijuana was clearly described as a venue that contributed to multi-person syringe use. IDUs defined a shooting gallery as a place where they were required to pay the shooting gallery operator a “sica” [fee], which was typically a few pesos or “gotas” [drops of liquid drug preparation from their syringe] in exchange for using the premises. Without access to sterile syringes from pharmacies, IDUs felt pressured to make use of used syringes from shooting galleries, which appeared to be normative.
Although shooting galleries are common in many eastern US cities33,34 and Puerto Rico,35 drug users in Western US cities have been found to inject less often in groups compared with those in Eastern US cities.36 Shooting galleries appear to thrive in communities where there is fear of prosecution for possession of drugs and even syringes.34,37 The experiences of the drug users we studied support this interpretation in Tijuana. IDUs uniformly described being harassed, arrested, or jailed for simple possession of a syringe, even if it was unused. Some drug users reported having been arrested for having visible track marks or for “looking like a tecato” [injector].
In various contexts, fear of police detainment or arrest has been shown to discourage IDUs from carrying syringes, leading them to share needles at the point of sale or inject with rented needles in shooting galleries.27,38–41 These practices can promote disassortative mixing, which in turn can increase the risk of blood-borne infections.27 A recent campaign in Tijuana called “Ponle Dedo Al Picadero” [target the shooting galleries] could potentially exacerbate this phenomenon. Although it may seem logical to shut down shooting galleries as a public health measure, such attempts could actually drive drug users further underground to even less safe environments such as vacant lots and alleyways. As an alternative, shooting galleries could serve as venues for harm-reduction interventions, as is being conducted in Miami (Bryan Page, oral communication, August 2004). That the punitive practices of pharmacists, clerks, and police operate in an environment where IDUs’ access to sterile syringes is theoretically legal serves as a paradoxical reminder of how laws “on the books” can differ from laws “on the streets.”42,43
Beyond these environmental influences, we also observed varying levels of HIV/AIDS awareness among IDUs in Tijuana. Although most IDUs appeared knowledgeable that syringe sharing could transmit HIV, there was a general lack of knowledge about the extent to which other infections could be transmitted parenterally. Very few of the IDUs we interviewed appeared knowledgeable about transmission risks from other injection paraphernalia (e.g., cotton, cookers, water). A few IDUs were under the impression that air would inactivate HIV. Such misconceptions could serve to minimize the perceived risks associated with the sharing of syringes and other injection equipment. Although basic HIV/AIDS knowledge is present, there is a clearly defined need for more education among IDUs in Tijuana.
Only three of the twenty IDUs we interviewed had heard of an NEP, even after the concept was explained by the interviewer. To our knowledge, the only NEP operating in Mexico is operated by Programa Compañeros in Ciudad Juarez.11 Interestingly, of the three IDUs who had heard of NEPs and were aware of its purpose, all learned of NEPs through experiences on the “other side” (i.e., travel to the United States), but none reported having used an NEP in any location. Two participants reported that they or someone they injected with purchased syringes in the United States, which suggests that some IDUs do cross the border to purchase or obtain syringes. This suggests that cross-border interventions to increase access to sterile syringes could be effective in slowing the spread of blood-borne infection on both sides of the US–Mexico border.
Congressional restriction of federal funding of NEPs and other syringe access programs has limited the scope of NEPs in California and other border states (e.g., Texas). In spite of this, our findings suggest that the influence of NEPs in the United States may nevertheless be a positive influence on the health of IDUs in Tijuana and assist in future development of NEPs in Mexican–US border cities. Most of the IDUs we interviewed were interested in attending an NEP, if it were available; however, many were wary that NEPs would expose them to arrest, and one thought NEPs could “spread disease,” perhaps drawing a parallel between NEPs and the familiar environment of a shooting gallery. Our findings suggest that there is sufficient interest to further explore the feasibility of implementing NEPs in Tijuana, but that in doing so, outreach and further health education of IDUs and cooperation of police and legislative officials will be critical to ensure their success.
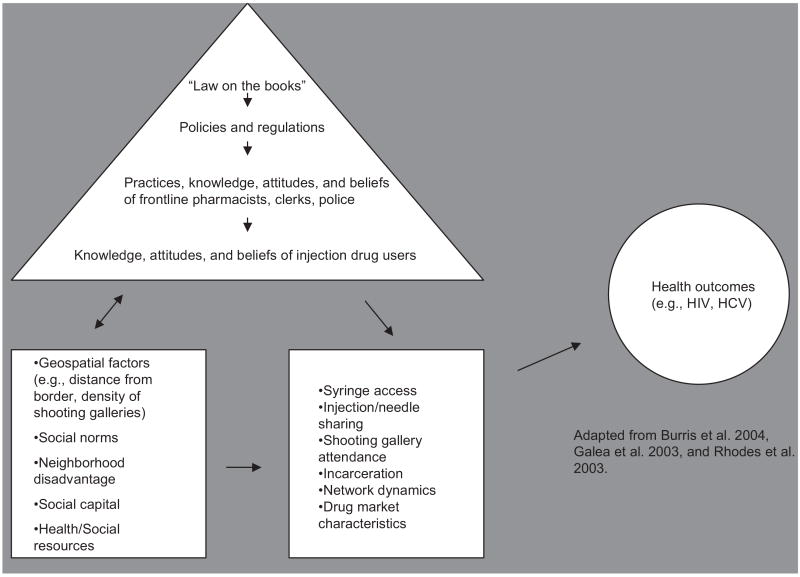
In considering the context of high-risk behaviors and the lack of available interventions in Tijuana, it is useful to consider how this information could inform future studies and new interventions. Recently, Burris and colleagues37 developed a model describing how the “drug policy transformation process” may influence health outcomes among IDUs. We adapted this model to include microlevel factors proposed by Rhodes et al.,27 macroenvironmental factors proposed by Galea et al.,44 and geospatial factors (e.g., density of shooting galleries, pharmacies, distance from the border) which we posit could influence IDUs’ attitudes, behaviors, and subsequent risks of acquiring blood-borne infections in Tijuana (Figure). For example, laws “on the books” are transformed in practice to policies and regulations of individual inter-actors with IDUs, such as police and pharmacy clerks. This in turn may affect the knowledge, behaviors, and attitudes of local IDUs. Macro-level factors which may operate to influence these relationships include social disadvantage, social capital, geospatial factors related to the nearby border crossing, and the lack of key resources (e.g., NEPs, drug-treatment programs). Microlevel factors that relate to both contexts include shooting gallery attendance, incarceration, and drug market characteristics (e.g., drug purity, availability, and price). These interrelationships may serve to heighten vulnerabilities to blood-borne infections among IDUs in Tijuana. If aspects of this model are supported by future studies, the next logical step would be to alter the manner in which drug policies, syringe regulations, and/or policing are operationalized in Tijuana (e.g., by training pharmacists and law enforcement officials) in an effort to reduce the risk of acquiring blood-borne infections.
FIGURE.
Conceptual model depicting relationships between contextual factors and risk of blood-borne infections among injection drug users (IDUs) in Tijuana.
Acknowledgments
The authors gratefully acknowledge support from the National Institute on Drug Abuse (DA09225-S11) and the UCSD Center for AIDS Research which is funded by the National Institute of Health (AI36214-06). Kimberly Brouwer is supported by a Ruth L. Kirschstein National Research Service Award sponsored by the NIH (5 T32 AI07384). We thank the interviewers and transcribers and the study respondents who gave so generously of their time in sharing their experiences.
References
- 1.INEGI (Instituto Nacional de Estadistica, Geografia e Informatica) Preliminary Results for the XII National Population and Housing Census-2000; Resultados Preliminares del XII Censo Nacional de Población y Vivienda 2000; México, Distrito Federal. 2000. [Google Scholar]
- 2.COPLADEM (Comité de Planeación para el Desarrollo del Estado de México) Plan Municipal de Desarrollo 1996–1998, Tijuana. [Accessed April 15, 2005];SDSU Institute for Regional Studies of the Californias. Available at: http://www-rohan.sdsu.edu/~irsc/tjreport/tj9.html.
- 3. [Accessed April 15, 2005];SDSU Institute for Regional Studies of the Californias. Available at: http://www-rohan.sdsu.edu/~irsc/tjreport/tj3.html.
- 4.Lange JE, Lauer EM, Voas RB. A survey of the San Diego-Tijuana cross-border binging. Eval Rev. 1999;23:378–398. doi: 10.1177/0193841X9902300402. [DOI] [PubMed] [Google Scholar]
- 5.Huntington SP. The Hispanic challenge. [Accessed June 30, 2004];Foreign Policy [serial online] Available at: http://www.foreignpolicy.com/story/cms.php?story_id=2495.
- 6.Central Intelligence Agency. [Accessed March 10, 2005];The world factbook. Available at: http://www.cia.gov/cia/publications/factbook/
- 7.Drug Enforcement Administration. Mexico: country profile for 2003. [Accessed July 12, 2004];Drug Intelligence Report DEA-03047. Available at: http://www.usdoj.gov/dea/pubs/intel/03047/03047.pdf.
- 8.Beyrer C, Razak MH, Lisam K, Chen J, Lui W, Yu XF. Overland heroin trafficking routes and HIV-1 spread in south and south-east Asia. AIDS. 2000;14:75–83. doi: 10.1097/00002030-200001070-00009. [DOI] [PubMed] [Google Scholar]
- 9.Adelekan ML, Stimson GV. Problems and prospects of implementing harm reduction for HIV and injecting drug use in high risk sub-Saharan African countries. J Drug Issues. 1997;27:97–116. [Google Scholar]
- 10.Bastos FI, Strathdee SA, Derrico M, Pina MDF. Drug abuse and the spread of HIV/AIDS in South America and the Caribbean. Drugs Educ Prev Policy. 1999;6:29–50. [Google Scholar]
- 11.Bucardo J, Brouwer KC, Magis C, et al. Historical trends in the production and consumption of illicit drugs in Mexico: implications for the prevention of blood borne infections. Drug and Alcohol Dependence. doi: 10.1016/j.drugalcdep.2005.02.003. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Magis-Rodriguez C, Ruiz-Badillo A, Ortiz-Mondragon R, Loya-Sepulveda M, Bravo-Portela MJ, Lozada R. Estudio sobre prácticas de riesgo de infección para VIH/SIDA en inyectores de drogas de la cd. de Tijuana B.C. [Accessed July 25, 2004];Biblioteca Virtual en Salud [serial online] 2002 Available at: http://bvs.insp.mx/componen/svirtual/ppriori/09/0399/arti.htm.
- 13.Secretaria de Salud, Consejo Nacional Contra las Adicciones (SSA-CONADIC) [Accessed February 14, 2004];Encuesta Nacional de Adicciones 1999. Available at: http://www.salud.gob.mx/unidades/conadic/epidem.htm.
- 14.Morales S, Lozada R, Magis C, Saavedra JA, Monitoreo Evaluation of HIV prevention interventions in injectable drug users in Mexico. XV International Conference on AIDS; July 11–17, 2004; Bangkok, Thailand. [Google Scholar]
- 15.UNAIDS. Report on the Global HIV/AIDS Epidemic, 2002. Geneva, Switzerland: Jul, 2002. [Google Scholar]
- 16.CONASIDA. [Accessed October 29, 2002];Panorama Epidemiológico del VIH/SIDA e ITS en México [Epidemiologic overview of HIV/AIDS and STD in México] Available at: http://www.salud.gob.mx/conasida/comite/minutas/cua20020.pdf.
- 17.Magis-Rodríguez C, Bravo-García E, Rivera Reyes P. El sida en México en el año 2000. In: Uribe P, Magis C, editors. La Respuesta Mexicana Al SIDA: Mejores Prácticas. México: Ángulos Del SIDA. Mexico, Distrito Federal: Consejo Nacional para la Prevencion y Control del SIDA; 2000. pp. 13–22. [Google Scholar]
- 18.Viani RM, Hubbard P, Araneta MR, et al. Pregnant women in Baja California, Mexico: evidence of an emerging crisis?. XV International Conference on AIDS; July 11–17, 2004; Bangkok, Thailand. [Google Scholar]
- 19.Magis C, Brouwer KC, Morales S, et al. Correlates of receptive needle sharing among injection drug users (IDUs) in the US-Mexican border city of Tijuana. 3rd International Conference on Urban Health; October 20–22, 2004; Boston, MA. [Google Scholar]
- 20.Normand J, Vlahov D, Moses LE. Preventing HIV Transmission: The Role of Sterile Needles and Bleach. Washington, DC: National Academy Press; 1995. [PubMed] [Google Scholar]
- 21.Bastos FI, Strathdee SA. Evaluating effectiveness of syringe exchange programmes: current issues and future prospects. Soc Sci Med. 2000;51:1771–1782. doi: 10.1016/s0277-9536(00)00109-x. [DOI] [PubMed] [Google Scholar]
- 22.Des J, Hagan H, Friedman SR, et al. Maintaining low HIV seroprevalence in populations of injecting drug users. JAMA. 1995;274:1226–1231. doi: 10.1001/jama.274.15.1226. [DOI] [PubMed] [Google Scholar]
- 23.Emerson R. Producing ethnographies: theory, evidence and representation. In: Emerson R, editor. Contemporary Field Research. Prospect Heights, IL: Waveland Press; 2001. pp. 295–296. [Google Scholar]
- 24.Watters JK, Biernacki P. Targeted sampling. options for the study of hidden populations. Soc Probl. 1989;36:416–430. [Google Scholar]
- 25.Greenfield L, Bigelow GE, Brooner RK. HIV risk behavior in drug users: increased blood “booting” during cocaine injection. AIDS Educ Prev. 1992;4:95–107. [PubMed] [Google Scholar]
- 26.Bruneau J, Lamothe F, Franco E, et al. High rates of HIV infection among injection drug users participating in needle exchange programs in Montreal: results of a cohort study. Am J Epidemiol. 1997;146:994–1002. doi: 10.1093/oxfordjournals.aje.a009240. [DOI] [PubMed] [Google Scholar]
- 27.Rhodes T, Mikhailova LA, Sarang A, et al. Situational factors influencing drug injecting, risk reduction and syringe exchange in Togliatti City, Russian Federation: a qualitative study of micro risk environment. Soc Sci Med. 2003;57:39–54. doi: 10.1016/s0277-9536(02)00521-x. [DOI] [PubMed] [Google Scholar]
- 28.Burris S, Lurie P, Abrahamson D, Rich JD. Physician prescribing of sterile injection equipment to prevent HIV infection: time for action. Ann Intern Med. 2000;133:218–226. doi: 10.7326/0003-4819-133-3-200008010-00015. [DOI] [PubMed] [Google Scholar]
- 29.Case PL, Meehan T, Jones TS. Arrests and incarceration of injection drug users for syringe possesion in Massachusetts: implications for HIV prevention. J Acquir Immune Defic Syndr. 1998;18:S71–S75. doi: 10.1097/00042560-199802001-00013. [DOI] [PubMed] [Google Scholar]
- 30.Case PL, Beckett GA, Jones TS. Access to sterile syringes in Maine: pharmacy practice after the 1993 repeal of the syringe prescription law. J Acquir Immune Defic Syndr. 1998;18:S94–S101. doi: 10.1097/00042560-199802001-00017. [DOI] [PubMed] [Google Scholar]
- 31.Taussig JA, Weinstein B, Burris S, Jones TS. Syringe laws and pharmacy regulations are structural constraints on HIV prevention in the US. AIDS. 2000;14:S47–S51. doi: 10.1097/00002030-200006001-00007. [DOI] [PubMed] [Google Scholar]
- 32.Reich W, Compton WM, Horton JC, et al. Pharmacist ambivalence about sale of syringes to injection drug users. J Am Pharm Assoc (Wash) 2002;42:S52–S57. doi: 10.1331/1086-5802.42.0.s52.reich. [DOI] [PubMed] [Google Scholar]
- 33.Celentano D, Vlahov D, Cohn S, Anthony JC, Solomon L, Nelson KE. Risk factors for shooting gallery use and cessation among intravenous drug users. Am J Public Health. 1991;81:1291–1295. doi: 10.2105/ajph.81.10.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Page JB, Smith PC, Kane N. Shooting galleries, their proprietors, and implications for prevention of AIDS. Drugs Soc. 1990;5:69–85. [Google Scholar]
- 35.Robles RR, Marrero CA, Reyes JC, et al. Risk behaviors, HIV seropositivity, and tuberculosis infection in injecting drug users who operate shooting galleries in Puerto Rico. J Acquir Immune Defic Syndr. 1998;17:477–483. doi: 10.1097/00042560-199804150-00014. [DOI] [PubMed] [Google Scholar]
- 36.Garfein RS, Monterroso E, Tong TC, et al. Comparison of HIV infection risk behaviors among injection drug users from east and west coast US cities. J Urban Health. 2004;81:260–267. doi: 10.1093/jurban/jth112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burris S, Blankenship KM, Donoghoe M, et al. Addressing the “risk environment” for injection drug users: the mysterious case of the missing cop. Milbank Q. 2004;82:125–156. doi: 10.1111/j.0887-378X.2004.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Koester S. Copping, running and paraphernalia laws: contextual and needle risk behaviors among drug users in Denver. Human Organ. 1994;53:287–295. [Google Scholar]
- 39.Strathdee SA, Zafar T, Brahmbhatt H, Baksh A, ul Hassan S. Rise in needle sharing among injection drug users in Pakistan during the Afghanistan war. Drug Alcohol Depend. 2003;71:17–24. doi: 10.1016/s0376-8716(03)00072-3. [DOI] [PubMed] [Google Scholar]
- 40.Harvey E, Strathdee SA, Patrick DM, et al. A qualitative investigation into an HIV outbreak among injection drug users in Vancouver, British Columbia. AIDS Care. 1998;10:313–321. doi: 10.1080/713612412. [DOI] [PubMed] [Google Scholar]
- 41.Rhodes T, Lowndes C, Judd A, et al. Explosive spread and high prevalence of HIV infection among injecting drug users in Togliatti city, Russia. AIDS. 2002;16:25–31. doi: 10.1097/00002030-200209060-00002. [DOI] [PubMed] [Google Scholar]
- 42.Bardach E. The Implementation Game: What Happens After a Bill Becomes Law. Cambridge, MA: MIT Press; 1997. [Google Scholar]
- 43.Percy SL. Disability, Civil Rights, and Public Policy: The Politics of Implementation. Tuscaloosa, AL: University of Alabama Press; 1989. [Google Scholar]
- 44.Galea S, Ahern J, Vlahov D. Contextual determinants of drug use risk behavior: a theoretic framework. J Urban Health. 2003;80:50–58. doi: 10.1093/jurban/jtg082. [DOI] [PMC free article] [PubMed] [Google Scholar]