Abstract
AUTONOMIC DYSREFLEXIA IS AN ACUTE SYNDROME OF EXCESSIVE, UNCONTROLLED SYMPATHETIC OUTPUT that can occur in patients who have had an injury to the spinal cord (generally at or above the sixth thoracic neurologic level). It is caused by spinal reflex mechanisms that remain intact despite the patient's injury, leading to hypertension. This review describes the clinical features of autonomic dysreflexia, its common causes (most frequently stimulation of the lower urinary tract) and a recommended approach to treatment. The condition can nearly always be managed successfully, but prompt recognition is essential — without treatment there may be dire consequences, including death.
The case
Mr. H is a 27-year-old man whose spinal cord was injured just over 2 years ago in a motor vehicle crash, which resulted in complete tetraplegia from the level of the fifth cervical neurologic level, with no movement or feeling below the level of the biceps muscle. He is otherwise fairly healthy. He uses an indwelling catheter for bladder management and evacuates his bowels every 2 days. His only regular medications are a stool softener and baclofen.
Mr. H is brought by his caregiver to the emergency department of his local hospital with severe headache, sweating and nasal congestion. The nurse taking his vital signs reports to the attending physician that his blood pressure is 135/95 mm Hg. The patient relates that it is usually about 90/60 mm Hg. He is feeling progressively worse.
Autonomic dysreflexia is an acute syndrome of excessive, uncontrolled sympathetic output with potentially serious consequences that can occur in patients who have had an injury to the spinal cord. Recognition of the clinical features (described later) is extremely important because, although the condition can nearly always be managed successfully, failure to do so can have dire consequences, including death.
The reported frequency of autonomic dysreflexia varies widely, but the condition appears to be relatively common, especially in patients with spinal cord lesions at or above the sixth thoracic neurologic level (T6). Estimates of lifetime frequency have ranged from 19% to 70%,1,2 the true value probably lying somewhere in between. On rare occasions, the condition is also seen in paraplegic patients with lesions below T6, but in this situation the reaction is usually somewhat milder.3 Autonomic dysreflexia is more common in patients with complete lesions than in those with incomplete lesions, and the reaction seems to be less severe in the latter group.4 Incomplete injuries involve sparing of the most distal sacral segments of the spinal cord (i.e., preservation of perianal sensation or voluntary contraction of the external anal sphincter).5
Pathophysiology
Autonomic dysreflexia is caused by spinal reflex mechanisms that remain intact despite the patient's injury. A noxious stimulus (i.e., one that might be expected to cause pain or discomfort in a person without spinal cord injury) below the level of the lesion produces an afferent impulse that generates a generalized sympathetic response, which in turn results in vasoconstriction below the neurologic lesion.6 With lesions at or above the T6 level, the splanchnic vascular bed becomes involved, which provides the critical mass of blood vessels required to cause elevation of the blood pressure.
In a person without spinal cord injury, descending central (brain stem) inhibitory pathways would respond to the rise in blood pressure and would modulate the sympathetic response. However, the injury to the spinal cord prevents such signals from descending to the sympathetic chain7 (Fig. 1). The end result is peripheral and splanchnic vasoconstriction followed by development of hypertension. The excessive parasympathetic output (and lack of sympathetic tone) above the level of the lesion results in peripheral vasodilation and is thought to be responsible for the headache, flushing and sweating in the head and neck region and the nasal congestion that characterize this condition.
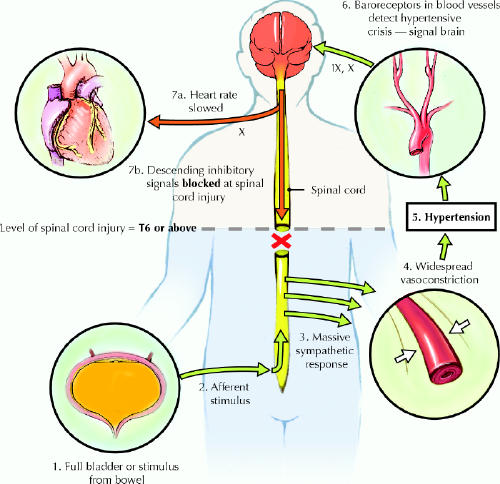
Fig 1: Diagram illustrating how autonomic dysreflexia occurs in a person with spinal cord injury. The afferent stimulus, in this case a distended bladder, triggers a peripheral sympathetic response, which results in vasoconstriction and hypertension. Descending inhibitory signals, which would normally counteract the rise in blood pressure, are blocked at the level of the spinal cord injury. The roman numerals (IX, X) refer to cranial nerves. Photo: Chesley Sheppard
Clinical features
The presenting symptoms of autonomic dysreflexia generally include a bilateral, pounding headache along with sweating above the level of the injury, nasal congestion, malaise and nausea. Blurring of vision is also reported by some patients.
Signs include flushed, sweaty skin above the level of the lesion and cool, pale skin below this level. The main physical finding is elevation of the blood pressure. It is important to remember that resting blood pressure declines after a spinal cord injury, often to the range of 90/60 mm Hg. This means that even readings of 120/80 mm Hg might be considered elevated. Systolic blood pressure as high as 250–300 mm Hg and diastolic pressure as high as 200–220 mm Hg have been reported during an episode of autonomic dysreflexia.8 Reflex bradycardia secondary to vagal stimulation is often seen, but tachycardia is also common.
The differential diagnosis includes migraine and cluster headaches, essential hypertension, posterior fossa tumours, pheochromocytoma and toxemia of pregnancy.9
Precipitants
Any noxious stimulus occurring below the level of the injury to the spinal cord (Table 1) can trigger an episode of autonomic dysreflexia. Stimulation of the lower urinary tract accounts for most episodes of autonomic dysreflexia, and bladder distension appears to be the precipitant in 75% to 85% of cases.10 The distension can result from a blocked or kinked catheter or insufficient frequency of intermittent catheterization. Other urinary tract triggers include infection, urethral distension, instrumentation, stones and testicular torsion.
Table 1
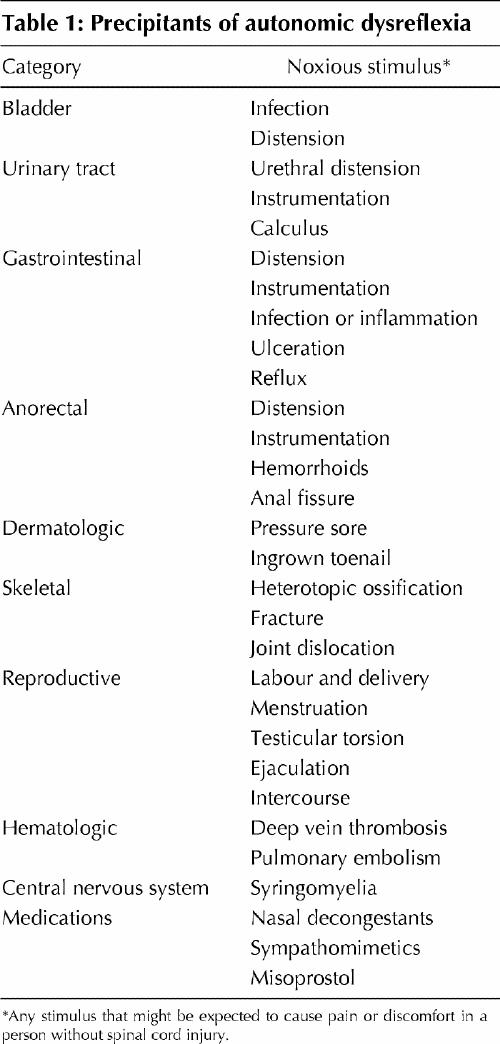
The second most common precipitant of autonomic dysreflexia is bowel distension due to fecal impaction, which accounts for 13% to 19% of cases.10 Other potential noxious stimuli in this area include anorectal distension triggered by manual evacuation of stool, instrumentation, hemorrhoids and anal fissures. Other gastrointestinal precipitants include appendicitis, cholecystitis, esophageal reflux, and ulcer erosion or perforation.
In addition to urinary and gastrointestinal triggers, a long list of other potential precipitative factors has been reported. Among the more common of these are cutaneous triggers such as pressure sores and ingrown toenails. Also important to consider in this population are conditions such as heterotopic ossification, fractures of the long bone of the lower extremity and hip dislocation. Menstruation and labour and delivery may be precipitating factors in women. Less common triggers include deep vein thrombosis, pulmonary embolism, syringomyelia and sexual activity, including ejaculation. Medications may also induce autonomic dysreflexia, especially nasal decongestants and potentially misoprostol.10,11
Treatment
Early recognition of the condition is essential so that treatment (Table 2) can be initiated immediately. Failure to properly manage autonomic dysreflexia can result in severe hypertension leading to cerebral or subarachnoid hemorrhage, seizures, atrial fibrillation, neurogenic pulmonary edema, retinal hemorrhage, coma or death.9 Proper management significantly decreases the likelihood of these complications.
Table 2
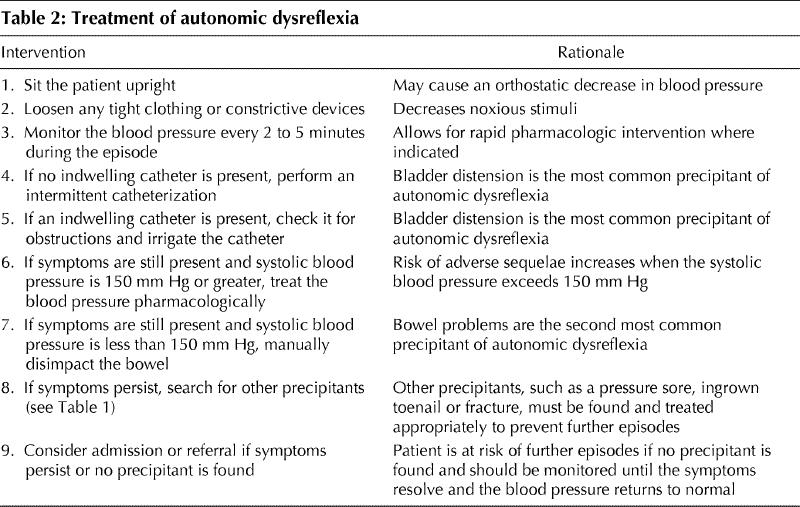
Once elevation of blood pressure, along with the typical signs and symptoms of autonomic dysreflexia, has been confirmed, the first step in management is to sit the patient upright.12 This provokes an orthostatic drop in blood pressure. At the same time, any tight or restrictive clothing or devices should be removed. During treatment, blood pressure should be carefully monitored every 2 to 5 minutes.12 Unlike the management of most hypertensive crises, treatment in this situation is based on the blood pressure itself, and not on its effects on the end organs.
The next step is to look for a precipitant and eliminate it, if possible. If the patient has an indwelling Foley catheter, the catheter should be checked for kinks or obstructions and flushed if necessary. If the patient uses intermittent catheterization, a catheter should be inserted (with the application of lidocaine jelly) to drain the bladder.
In many cases, draining the bladder alleviates the symptoms as well as the hypertension. However, if such improvements do not occur, other triggers must be sought. If, after performing the steps outlined above, the systolic blood pressure is 150 mm Hg or greater, pharmacologic therapy should be undertaken.12 The goal of such intervention is to alleviate symptoms and avoid the complications associated with uncontrolled hypertension.
In general, the best antihypertensive medications to use in this situation have a rapid onset and short duration of action.12 Nitrates and, especially, nifedipine (immediate- release form) appear to be the most commonly used medications,1,8,9,12,13,14 although no randomized controlled trials have been undertaken and much of the evidence available comes from case reports or small series of patients.
Nifedipine is generally given using the “bite and swallow” method, rather than sublingually, in a dose of 10 mg. There have been no reported adverse events from the use of nifedipine in the treatment of autonomic dysreflexia.12 The application of 2.5 cm (1 inch) of 2% nitropaste above the level of the lesion12 is useful, as the paste can be readily removed when the hypertension subsides and there may be less chance of subsequent hypotension. If neither of these agents is successful and the pressure remains elevated, an intravenous drip of sodium nitroprusside for rapid titration of blood pressure may be required.12 More men with spinal cord injuries are now using sildenafil for the treatment of erectile dysfunction, so it should be noted that, because of the risk of sudden and profound hypotension, the use of nitrates is contraindicated in patients taking this medication.8 Therefore, if the patient is to receive nitropaste, he should be questioned about use of sildenafil; if the latter drug has been used in the previous 24 hours, the nitropaste should not be applied. Similarly, if a patient is given nitropaste, he should be cautioned not to use sildenafil for at least the next 24 hours.
Other antihypertensive agents reported to be effective in this setting include hydralazine, mecamylamine, diazoxide, prazosin and clonidine.1,2,8,9
If the bladder is empty and symptoms continue, but the systolic blood pressure is less than 150 mm Hg, the bowel should be manually disimpacted with a gloved finger coated with 2% lidocaine jelly.12 If neither the bladder nor the bowel is the precipitant of the episode, then more in-depth investigations will be required. Hospital admission for observation and investigation may be needed in some cases.
During labour and delivery, the risk of autonomic dysreflexia in patients with lesions at or above T6 is 85% to 90%.15 The syndrome must be differentiated from pre-eclampsia. In autonomic dysreflexia, unlike pre-eclampsia, the elevation of blood pressure and other symptoms usually occur during contraction of the uterus and then subside with relaxation.15 The use of epidural or spinal anesthesia can prevent autonomic dysreflexia and should be used routinely in at-risk patients16 (any woman with an injury at or above T6, especially where the injury is complete; those who have had previous episodes of autonomic dysreflexia are considered at highest risk).
Some patients have difficulty with recurrent episodes of autonomic dysreflexia because of noxious stimuli that may take time to resolve, such as a severe pressure sore. In this situation, prophylactic treatment may be needed, for which the most common agents are α-blocking agents such as terazosin.17 This medication can be discontinued when the underlying problem has resolved.
Prevention of autonomic dysreflexia is the best approach. Therefore, patients with spinal cord injury should receive counselling about proper bowel, bladder and skin management techniques. They may need to carry with them (e.g., on a wallet-sized card) information about the clinical findings and treatment for this condition, for the benefit of health care providers who may not be familiar with it.
When in doubt about the cause or management of the dysreflexic episode, or if dysreflexic episodes are recurrent or unexplained, the physician should consult a specialist in physical medicine and rehabilitation. Any patient who presents to a physician with acute autonomic dysreflexia and elevated blood pressure should be referred to the nearest emergency department for management. Admission of the patient should be considered when the blood pressure cannot be controlled through the usual treatment regimen, when an in-depth assessment is needed to determine the cause of the autonomic dysreflexia or when there is evidence of complications, such as pulmonary edema or intracerebral hemorrhage. The patient can be discharged when the blood pressure has been brought under control and the trigger identified. When the inciting event is not apparent, more severe precipitants of dysreflexia (e.g., pulmonary embolism) must be considered and ruled out. If the blood pressure is well controlled and serious causes are ruled out, other investigations can be done on an outpatient basis. Follow-up should continue until a precipitating cause is found or the dysreflexic episodes cease.
A summary of the clinical practice guidelines12 for managing autonomic dysreflexia can be obtained through the Paralyzed Veterans of America (www.pva.org).
The case revisited
Mr. H's physician recognizes the presentation as classic autonomic dysreflexia. She sits him upright and instructs the nurse to monitor the blood pressure every 2–3 minutes. She notes that Mr. H's urine bag has only about 50 mL of urine in it, although he claims to have last emptied it several hours ago.
No obvious blockages or kinks are noted along the length of the catheter. However, when the nurse irrigates it with saline, a large amount of cloudy, foul-smelling urine is returned, which is sent for analysis. The patient's symptoms quickly subside and his blood pressure drops to 100/70 mm Hg over the next few minutes. No pharmacologic intervention is required. Mr. H is counselled regarding dysreflexia, and his caregiver is shown how to irrigate the catheter should it become blocked again in the future.
β See related article page 928
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
Correspondence to: Dr. Jeff Blackmer, The Rehabilitation Centre, 505 Smyth Rd., Ottawa ON K1H 8M2; fax 613 737-9638; jblackmer@ottawahospital.on.ca
References
- 1.Braddom RL, Rocco JF. Autonomic dysreflexia. A survey of current treatment. Am J Phys Med Rehabil 1991;70:234-41. [PubMed]
- 2.Snow JC, Sideropoulos HP, Kripke BJ, Freed MM, Shah NK, Schlesinger RM. Autonomic hyperreflexia during cystoscopy in patients with high spinal cord injuries. Paraplegia 1978;15:327-32. [DOI] [PubMed]
- 3.Moeller BA, Scheinberg D. Autonomic dysreflexia in injuries below the sixth thoracic segment [letter]. JAMA 1973;224:1295. [PubMed]
- 4.Kewalramani LS. Autonomic dysreflexia in traumatic myelopathy. Am J Phys Med 1980;59:1-21. [PubMed]
- 5.American Spinal Injury Association. International standards for neurological classification of spinal cord injury. 5th ed. Chicago: The Association; 2000.
- 6.Karlsson AK, Friberg P, Lonnroth P, Sullivan L, Elam M. Regional sympathetic function in high spinal cord injury during mental stress and autonomic dysreflexia. Brain 1998;121:1711-9. [DOI] [PubMed]
- 7.Erickson RP. Autonomic hyperreflexia: pathophysiology and medical management. Arch Phys Med Rehabil 1980;61:431-40. [PubMed]
- 8.Karlsson AK. Autonomic dysreflexia. Spinal Cord 1999;37:383-91. [DOI] [PubMed]
- 9.Lee BY, Karmakar MG, Herz BL, Sturgill RA. Autonomic dysreflexia revisited. J Spinal Cord Med 1994;18:75-87. [DOI] [PubMed]
- 10.Lindan R, Joiner E, Freehafer A, Hazel C. Incidence and clinical features of autonomic dysreflexia in patients with spinal cord injury. Paraplegia 1980; 18: 285-92. [DOI] [PubMed]
- 11.Vaidyanathan S, Krishnan KR. Misoprostol associated autonomic dysreflexia in a traumatic tetraplegic patient [letter]. Paraplegia 1996;34:121-2. [DOI] [PubMed]
- 12.Consortium for Spinal Cord Medicine. Acute management of autonomic dysreflexia: individuals with spinal cord injury presenting to health care facilities [clinical practice guideline]. 2nd ed. Washington: The Consortium, Paralyzed Veterans of America; 2001.
- 13.Dykstra DD, Sidi AA, Anderson LC. The effect of nifedipine on cystoscopy-induced autonomic hyperreflexia in patients with high spinal cord injuries. J Urol 1987;138:1155-7. [DOI] [PubMed]
- 14.Thyberg M, Ertzgaard P, Gylling M. Effect of nifedipine on cystometry-induced elevation of blood pressure in patients with a reflex urinary bladder after a high level spinal cord injury. Paraplegia 1994;32:308-13. [DOI] [PubMed]
- 15.Burns AS, Jackson AB. Gynecologic and reproductive issues in women with spinal cord injury. Phys Med Rehabil Clin North Am 2001;12:183-99. [PubMed]
- 16.American College of Obstetrics and Gynecology Committee Opinion: management of labor and delivery for patients with spinal cord injury. Int J Gynecol Obstet 1991;68:523-6.
- 17.Frost FS. Spinal cord injury medicine. In: Braddom RL editor. Physical medicine and rehabilitation. 2nd ed. Philadelphia: WB Saunders; 2000. p. 1230-82.


