Abstract
This morphometric and experimental study was designed to assess the dimensions and axes of the subaxial cervical pedicles and to compare the accuracy of two different techniques for subaxial cervical pedicle screw (CPS) placement using newly designed aiming devices. Transpedicular fixation is increasingly used for stabilizing the subaxial cervical spine. Development of the demanding technique is based on morphometric studies of the pedicle anatomy. Several surgical techniques have been developed and evaluated with respect to their feasibility and accuracy. The study was carried out on six conserved human cadavers (average age 85 years). Axes and dimensions of the pedicles C3–C7 (60 pedicles) were measured using multislice computed tomography (CT) images prior to surgery. Two groups consisting of 3 specimens and 30 pedicles each were established according to the screw placement technique. For surgical technique 1 (ST1) a para-articular mini-laminotomy was performed. Guidance of the drill through the pedicle with a handheld aiming device attached onto the medial aspect of the pedicle inside the spinal canal. Screw hole preparation monitored by lateral fluoroscopy. In surgical technique 2 (ST2) a more complex aiming device was used for screw holes drilling. It consists of a frame with a fully adjustable radiolucent arm for carrying the instruments necessary for placing the screws. The arm was angled according to the cervical pedicle axis as determined by the preoperative CT scans. Drilling was monitored by lateral fluoroscopy. In either technique 3.5 mm screws made of carbon fiber polyetheretherketone (CF-PEEK) were inserted. The use of the CF-PEEK screws allowed for precise postoperative CT-assessment since this material does not cause artifacts. Screw placement was qualified from ideal to unacceptable into four grades: I = screw centered in pedicle; IIa = perforation of pedicle wall less than one-fourth of the screw diameter; IIb = perforation more than one-fourth of the screw diameter without contact to neurovascular structures; III = screw more than one-fourth outside the pedicle with contact to neurovascular structures. Fifty-six pedicle screws could be evaluated according to the same CT protocol that was used preoperatively. Accuracy of pedicle screw placement did not reveal significant differences between techniques 1 and 2. A tendency towards less severe misplacements (grade III) was seen in ST2 (15% in ST2 vs. 23% in ST1) as well as a higher rate of screw positions graded IIa (62% in ST2 vs. 43% in ST1). C4 and C5 were identified to be the most critical vertebral levels with three malpositioned screws each. Because of the variability of cervical pedicles preoperative CT evaluation with multiplanar reconstructions of the pedicle anatomy is essential for transpedicular screw placement in the cervical spine. Cadaver studies remain mandatory to develop safer and technically less demanding procedures. A similar study is projected to further develop the technique of CPS fixation with regard to safety and clinical practicability.
Keywords: Cervical spine, Cervical pedicle, Anatomical study, Fixation technique
Introduction
There are some situations, primarily pathomorphological as well as postoperative, in which standard posterior stabilization techniques may be insufficient [12, 15, 17, 18]. In certain cases, the possibility of achieving a fixation shorter than feasible with other techniques may be the deciding factor for choosing a pedicle fixation. In consideration of the fact that anterior stabilization may also not be adequate in some situations, concern focused on cervical pedicle for anchoring posterior implants.
Transpedicular stabilization of the subaxial cervical spine is highly efficient but is still a delicate procedure. Thorough understanding of the pedicle anatomy is mandatory to avoid injury to the vertebral artery, spinal cord or a nerve root. Consequently the morphometric parameters of the cervical pedicles were repeatedly investigated [13, 31, 38, 46, 52]. Several biomechanical [7, 41] as well as clinical reports on transpedicular screw fixation techniques [1, 2, 4, 19, 36] have been published. Cervical pedicle screw (CPS) fixation can provide a significantly higher stability compared to other posterior fixation techniques [20, 26, 29, 30].
Following the first description of CPS fixation by Abumi et al. [2], different surgical techniques have been developed and evaluated:
Techniques relying on anatomical landmarks for CPS insertion [8, 13, 19, 23, 38],
Techniques with direct exposure [1, 2] of the pedicle, either by lamino-/foramionotomy or [16, 33, 34] or by the so called “funnel technique” [24],
Computerized image-guided navigation systems [7, 21, 33, 36, 40, 41].
Despite appealing clinical results achieved with practically all techniques [3, 5, 10, 19, 27], several cadaver studies, even utilizing computerized image-guided systems [30, 32, 33, 35], still showed high perforation rates from 18 up to 87.5%.
The purpose of this study was to evaluate the accuracy and practical feasibility of two different CPS placement techniques with newly designed aiming devices both relying on preoperative computed tomography (CT) and intraoperative fluoroscopy.
Materials and methods
Ten randomly chosen and conserved human cadavers were obtained from the Department of Human Anatomy. Their cervical spines were examined with conventional radiographs in two planes (a.p. and lateral) to exclude anomalies, tumors or severe multisegmental changes other than osteoporosis and moderate spondylosis. Four specimens had to be excluded based on these criteria. The remaining six specimens (male-to-female ratio 2:4) were divided into two groups with three specimens each. All six cervical spines had varied degrees of non-quantified osteoporosis and degenerative changes as expected for an average age of 85 years (range 80–90 years).
Pedicle morphometry (Fig. 1)
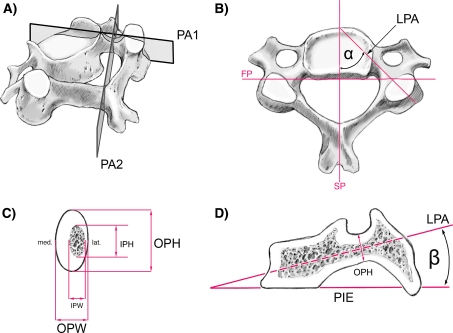
Fig. 1.
Mid-cervical vertebra showing cuts and lines used for the CT measurements: aPA 1 vertical cut through the longitudinal pedicle axis (LPA), PA 2 vertical cut through the isthmus of the pedicle, perpendicular to PA 1. b Superior view: sagittal plane (SP), frontal plane (FP), longitudinal pedicle axis (LPA), pedicle transverse angle α (PTA) between PA 1 and SP. c Cut PA 2 through the pedicle isthmus: outer pedicle height (OPH), outer pedicle width (OPW), inner pedicle height (IPH), inner pedicle width (IPW). Note that the lateral wall is always thinner than the medial one. d Cut PA 1: plane of the inferior vertebral endplate (PIE), pedicle sagittal angle β (PSA) between the plane of the inferior endplate (PIE) and longitudinal pedicle axis (LPA)
Computed tomography scans were preoperatively obtained from C3 to C7 in every case. High longitudinal resolution and proper slice thickness are important for the performance of high quality 2D and 3D reconstructions [25]. Therefore primary images were acquired using a standard algorithm with 1.25 mm slice thickness and 0.6 mm reconstruction interval. Reconstructions were performed with advantage windows 4.2 (GE LightSpeed QX/I, General Electric, Milwaukee, USA).
Sixty pedicles were evaluated with multiplanar reconstructions as illustrated. Using the cursor, direct digital CT measurement (0.6 mm increments) of 4 linear parameters (1–4) was carried out for every pedicle. The pedicle axis was assessed for its sagittal and transverse angle of projection [angular measurements (5–6)]. All measurements were independently performed by two of the authors (MRe, MRi; Fig. 1b, c).
List of measured dimensions and angles
Outer pedicle width (OPW; mm): outer mediolateral diameter of the isthmus of the pedicle.
Outer pedicle height (OPH; mm): outer superoinferior diameter of the isthmus of the pedicle.
Inner pedicle width (IPW; mm): inner mediolateral diameter of the isthmus of the pedicle or width of cancellous core.
Inner pedicle height (IPH; mm): inner superoinferior diameter of the pedicle or the height of the cancellous core of the isthmus of the pedicle.
Pedicle transverse angle α (PTA): angle between the sagittal plane and the longitudinal pedicle axis (LPA).
Pedicle sagittal angle β (PSA): angle between the inferior vertebral endplate (PIE) and LPA.
Multislice CT with identical parameters was applied after bilateral transpedicular screw insertion for each pedicle screw. The accuracy of the screw position was independently evaluated by two authors (MRe, MRi) using postoperative CT cuts and multiplanar reconstructions according to the extent of pedicle wall violation.
Grading of the pedicle screw position
Grade I Screw centered in the pedicle causing only minor plastic deformation of the pedicle cortex at most.
Grade IIa Screw threads or less than one-fourth of the screw cross section penetrating the cortex; no contact of the screw with the spinal cord, nerve root or vertebral artery.
Grade IIb More than one-fourth of the screw cross section penetrating the cortex but no contact with neurovascular structures.
Grade III Screw position according to grade II, however, in contact with neurovascular structures.
Averages and standard deviations were calculated for all linear and angular pedicle measurements. To compare the CT measurements between the right and left pedicles an independent samples t test procedure with the significance set at 95% confidence level was performed. The resultant P > 0.05 showed that all linear and angular measurements could be combined for both the right and left sides. The software SPSS 11.0 for Windows (© SPSS Inc.) was used for statistical analysis.
Implants
Carbon fiber polyetheretherketone (CF-PEEK) screws1 (core diameter 2.8 mm, outer diameter 3.5 mm) containing 0.5 vol% Ta-fibers (Ø50 μm) were used for all pedicles. CF-PEEK was chosen because this material does not create significant artifacts and thus allows for precise postoperative determination of the screw position. The Ta-fibers render the screws fluoroscopically visible without creating significant artifacts in the CT.
Surgical technique
Surgery was performed by two surgeons (FM and MRe). The specimens were randomly divided into two groups with three specimens each (30 pedicles each) for either of the techniques.
The following procedures were identical in both techniques: prone position. Fixation of the head with a halo ring attached to a fully adjustable head fixation device [9] in a slightly flexed position (10–20°) so that the cervical spine is parallel to the floor. The latter was confirmed by lateral fluoroscopy. Straight posterior midline skin incision from the external occipital protuberance to the cervicothoracic junction and exposure of the posterior vertebral elements as far as to the lateral margin of the facet joints. If present, abnormal axial rotation of the cervical spine was corrected by rotating the head in either technique prior to defining the PTA at the exposed spine. Since the PTA refers to the horizontal plane abnormal rotation would lead to a wrong angle of insertion.
ST1: Handheld aiming device (Fig. 2)
Fig. 2.
a Drill and small handheld aiming device assembled. b Curved endplate at the tip of the instrument for positioning onto the medial pedicle in surgical technique 1 (ST1)
This technique is based on direct visualization of the pedicle and an aiming device with a drill sleeve that prevents perforation of the medial pedicle wall.
A para-articular mini-laminotomy at the caudal part of the lamina, close to the facet joint, was performed. The exiting spinal nerve was identified and the medial aspect of the pedicle subperiosteally exposed. An overhanging dorsomedial corner of the upper facet had to be removed in some instances to sufficiently visualize the pedicle. The curved endplate of the aiming device was placed onto the medial pedicle wall strictly avoiding contact with the spinal nerve. Care was taken to maintain contact between the blade of the aiming device and medial pedicle wall throughout the drilling of the screw hole. The visualized pedicle can already give an idea about the direction of the screw. In addition, the orientation of the aiming device in the horizontal plane was determined with a goniometer according to the PTA. Inclination of the 2.7 mm drill bit in the sagittal plane (PSA) was monitored by lateral fluoroscopy.
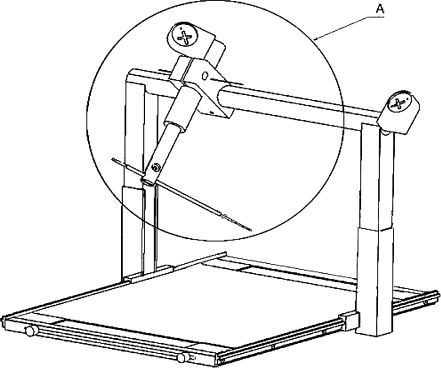
ST2: aiming frame (Fig. 3)
Fig. 3.
Aiming frame with radiolucent and adjustable arm (A) for carrying the instruments necessary for CPS insertion in surgical technique 2 (ST2)
The device consists of an aiming frame mounted onto a radiolucent plate. It has a fully adjustable radiolucent arm for the instruments necessary for the implantation procedure. The frame is placed over the cervicothoracic region. The drill guide jacket is rigidly locked in the radiolucent arm, adjusted according to the PTA and PSA, and placed onto the predetermined entrance point of the screw. Inclination of the drill guide jacket in the sagittal plane was checked by lateral fluoroscopy.
Distinct and consistent posterior anatomic landmarks were localized at every vertebral level for entrance point definition: (a) the lateral vertebral notch level and (b) inferior articular process as proposed by Karaikovic et al. [23]. The entry point of CPS on the posterior surface of the lateral mass was defined by the intersection of two lines, the vertical line crossing the intermediate/lateral third of the inferior articular process (depending on preoperative CT measurements) and the horizontal line passing the lateral vertebral notch2.
Aiming frame adjustment
Adjustment of the drill sleeve according to individual PTA in the horizontal plane.
Insertion of a K-wire into the drill sleeve. Alignment of the K-wire in the sagittal plane according to PSA3. Confirmation of PSA in relation to the plane of the lower vertebral endplate (PIE) (Fig. 1b) with lateral fluoroscopy (Fig. 1).
Centering of K-wire on the predetermined entrance point. Locking of the components of the aiming frame. Replacement of the K-wire by the 2.7 mm drill bit. Drilling of the screw hole monitored by lateral fluoroscopy.
Results
Pedicle measurements
Preoperative CT measurements of 60 pedicles were divided into two groups: (a) 5 linear and (b) two angular parameters by vertebral level (C3–C7) and are provided in Tables 1 and 2. All paired structures of the vertebrae were measured individually for the left and right side. No significant side differences (P > 0.05; independent samples t test) were found for any of the measured dimensions. For this reason, the values are presented without referring to their sides. Summary measures such as the mean and standard deviation were calculated at each level.
Table 1.
Linear parameters measured at the isthmus of the pedicle
| Pedicle | OPW (mm) | OPH (mm) | IPW (mm) | IPH (mm) |
|---|---|---|---|---|
| C3 | ||||
| Mean | 5.7 | 7.5 | 2.2 | 2.9 |
| SD | 0.4 | 0.7 | 0.3 | 0.5 |
| Range | 5.0–6.5 | 7.0–8.8 | 1.8–2.6 | 2.6–3.9 |
| C4 | ||||
| Mean | 5.6 | 7.1 | 2.4 | 2.7 |
| SD | 0.6 | 0.7 | 0.6 | 0.6 |
| Range | 5.0–6.8 | 6.2–8.0 | 1.8–3.4 | 1.8–3.4 |
| C5 | ||||
| Mean | 6.2 | 6.8 | 2.5 | 2.6 |
| SD | 0.6 | 0.5 | 0.4 | 0.5 |
| Range | 5.5–7.0 | 6.4–7.7 | 2.1–3.1 | 2.1–3.2 |
| C6 | ||||
| Mean | 6.7 | 6.7 | 2.7 | 2.6 |
| SD | 0.6 | 1.2 | 0.5 | 0.6 |
| Range | 6.1–7.7 | 5.7–8.3 | 2.3–3.8 | 2.2–3.8 |
| C7 | ||||
| Mean | 7.9 | 7.2 | 3.9 | 3.4 |
| SD | 1.1 | 0.7 | 1.2 | 0.4 |
| Range | 6.6–9.3 | 6.1–8.1 | 2.2–5.8 | 2.9–3.8 |
OPW outer pedicle width, OPH outer pedicle height, IPW inner pedicle width, IPH inner pedicle height (cp. Fig. 1)
Table 2.
Angular CT measurements for pedicle axis characterization
| Pedicle | PTA (°) | PSA (°) |
|---|---|---|
| C3 | ||
| Mean | 47.6 | 19.4 |
| SD | 5.6 | 2.9 |
| Range | 37.7–54.4 | 16.7–24.3 |
| C4 | ||
| Mean | 50.3 | 12.1 |
| SD | 8.3 | 2.7 |
| Range | 41.1–61.6 | 7.6–14.7 |
| C5 | ||
| Mean | 49.3 | 1 |
| SD | 7.2 | 5.1 |
| Range | 37.8–59.3 | −4 to 8.5 |
| C6 | ||
| Mean | 44 | −2.2 |
| SD | 7 | 4.1 |
| Range | 34.2–52.2 | −8.6 to 2.4 |
| C7 | ||
| Mean | 39.1 | −5.3 |
| SD | 6 | 5.5 |
| Range | 30.3–44.3 | −13.7 to 1 |
PTA pedicle transverse angle, PSA pedicle sagittal angle (cp. Fig. 1)
The OPW and IPW showed a slight increase from cranial to caudal ranging from Ø5.7 to 7.9 mm (OPW) and from Ø2.2 to 3.9 mm (IPW), respectively. Pedicle heights were found to be similar in all subaxial vertebrae from C3 to C7 (range OPH Ø6.7–7.5 mm; IPH Ø2.6–3.4 mm) (Table 1).
A total of 8 (13%) pedicles had inner pedicle diameters (IPW) greater than 3.5 mm, 9 (15%) had IPW values of 3.1–3.5 mm, 11 (18%) of 2.6–3 mm and 32 (53%) less or equal of 2.5 mm.
The average IPW was the smallest at C3 (2.2 mm) and largest at C7 (3.9 mm). Significant correlations (P < 0.01; Kendall’s τ-b) existed between the vertebral level and IPW, as well as OPW. The average IPH was smallest at C5 (2.6 mm) and largest at C7 (3.4 mm). No significant interlevel differences were detected.
Angular measurements are shown in Table 2. The average overall PTA was 46° varying from 30° to 62°. The smallest angle was at C7, the largest in C4. The pedicle axis also exhibits varying angles in the sagittal plane (PSA). From C3 to C7 PSA changed from about 19° to −5°. Pedicles are directed slightly caudal (−5° to −2° mean PSA) in the C7 and C6 level, parallel or neutral to the lower endplate in C5, and cranial in C4 and C3 levels (12–19° mean PSA). Significant correlations (P < 0.01; Kendall’s τ-b) existed between the vertebral level and both angular measurements (PTA, PSA).
Techniques I and II
A total of 56 pedicles was instrumented. Measured dimensions (Tables 1, 2) of the instrumented pedicles in both groups (ST1 vs. ST2) did not show significant differences (P > 0.05; independent samples t test).
Table 3 displays the numbers and the incidence of perforated screws depending on the vertebral level (C3–C7) and surgical technique (ST1 vs. T2).
Table 3.
Accuracy of CPS positioning and incidence of screw perforation in relation to vertebral level and surgical technique
| Vertebral level | Technique | No. of inserted screws | Violation of pedicle cortex | |||
|---|---|---|---|---|---|---|
| n (Grade I) | n (Grade IIa) | n (Grade IIb) | n (Grade III) | |||
| C3 | ST1 | 6 | 3 | 2 | 1 | |
| ST2 | 5 | 4 | 1 | |||
| C4 | ST1 | 6 | 3 | 1 | 2 | |
| ST2 | 6 | 1 | 3 | 1 | 1 | |
| C5 | ST1 | 6 | 1 | 2 | 1 | 2 |
| ST2 | 5 | 1 | 2 | 1 | 1 | |
| C6 | ST1 | 6 | 1 | 3 | 1 | 1 |
| ST2 | 5 | 4 | 1 | |||
| C7 | ST1 | 6 | 2 | 2 | 1 | 1 |
| ST2 | 5 | 3 | 1 | 1 | ||
| ST1 (total) | 30 | 4 (13%) | 13 (43%) | 6 (20%) | 7 (23%) | |
| ST2 (total) | 26 | 2 (8%) | 16 (62%) | 4 (15%) | 4 (15%) | |
| 100% | 11% | 52% | 18% | 20% | ||
Four pedicles could not be instrumented due to the following reasons: lateral mass fracture at the removal of an osteophyte; anomalous vertebral artery with aberrant foramen transversarium (1x C6, 1x C7); large bone cyst in the articular mass.
Cortical perforations were compared with regards to the right (27 screws) and left (29 screws) side and were not found to be significantly one-sided (P = 0.476; Mann–Whitney test).
Postoperative CT analysis showed an ideal location of 6 pedicle screws (grade I; Fig. 2). 29 screws had tolerable perforations with screw threads or minor parts of the screw shank penetrating the cortex (grade IIa; Fig. 2). 10 pedicle perforations were graded IIb and 11 graded III.
In 55% of the cases (n = 33) the screws violated the lateral wall of the pedicle towards the foramen transversarium.
Both techniques did not reveal statistically significant differences in pedicle wall violation (P = 0.568; Mann–Whitney test). There was only a trend for safer screw positing with technique 2 in terms of a higher rate of non-critical pedicle wall violations (grade IIa) with ST2 [(62% (ST2) vs. 43% (ST1)] and lower rate of malpositioned screws (grade III) [15% (ST2) vs. 23% (ST1)] (Table 3).
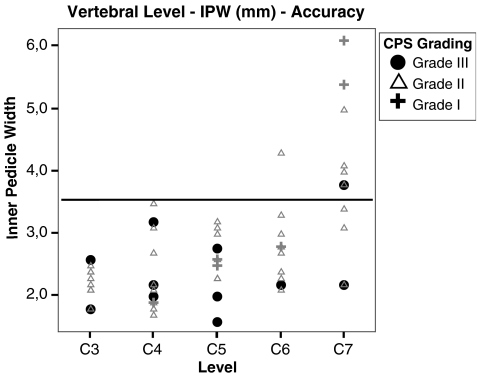
C4 and C5 were the most critical vertebral levels with three malpositioned screws each. The lowest rate of grade III screws was observed at C6 (n = 1). However, nominal directional measures (λ, P = 0.654) did not indicate a significance of the relationship between vertebral level and CPS accuracy/grading. Nevertheless, most severely malpositioned screws were located in the upper cervical levels with smaller IPW (cp. Fig. 4).
Fig. 4.
Relationship of vertebral level, IPW (mm) and grading of pedicle screw position. Malpositioned screws (grade III, solid black dots) were mostly located at the levels C3–C5 and at pedicles of smaller inner diameter (IPW <3 mm). Horizontal bar representing the outer diameter of implants (3.5 mm)
Discussion
Transpedicular screw fixation is advantageous for certain pathologies of the cervical spine. Previous biomechanical data showed superior stabilization capabilities of transpedicular screw fixation for patients with poor bone quality, severe spinal injuries or multilevel instability [20, 26, 29, 48]. Nevertheless, justification from the biomechanical standpoint has to be weighted against the potential risk of injury to neurovascular structures [10, 14, 43, 44]. While clinical studies report a relatively low risk of significant complications [5], anatomic studies did not reveal the same success [32–34, 42, 49, 52].
The goal of this study was to evaluate the feasibility and accuracy of two new transpedicular subaxial screw placement techniques based on pre- and postoperative morphometric studies.
CT pedicle measurements
Cervical pedicle screw fixation requires profound knowledge of the cervical spine anatomy. Therefore morphometric CT measurements were carried out prior to surgery to determine the dimensions and axes of the subaxial pedicles. This allowed for the individual assessment of each segment and determination of intra- and interindividual variations of pedicle anatomy. Multiplanar CT measurements allow for precise determination of the outer as well as the inner pedicle diameters [35]. In general, measurements and values of pedicle dimensions presented in this study are consistent with those published earlier [11, 13, 22, 38, 39, 45, 47, 49]. In concordance with these studies, we found no significant differences between the measurements of the right and left side. The transverse pedicle angle (PTA) decreased from cranial (C3/C4) to caudal (C7) (Table 2). The pedicle axis (PSA) was found to be directed superiorly in the upper spine and inferiorly in the lower cervical spine, both with large individual variations. We noticed a minimal increase of pedicle height, but a more pronounced increase of pedicle width from cranial to caudal. An increase in pedicle height and width was matched by a commensurate increase in cancellous core height and width.
Internal dimensions of the cancellous core were evaluated as well, since the stability of CPS can largely depend on the internal characteristics of the pedicle, and not so much on its external dimensions [20, 39, 50]. However, others have stressed the importance of the CPS purchase within the vertebral body [35].
A distinct characteristic of human cervical pedicles is that the lateral pedicle wall adjacent to the vertebral artery is always thinner than the medial wall [19, 22, 39].
Surgical techniques: CPS placement
Several modifications of the first description for cervical transpedicular screw fixation as developed by Abumi et al. [2] have been published. Abumi et al. opened the articular mass down to the introitus of the pedicle and probed the pedicle prior to CPS insertion [2]. Karaikovic et al. [24] used a modified funnel technique for CPS placement without intraoperative radiographic control. The thicker medial cortex of the pedicle served as a guide for entering the vertebral body. Miller et al. [34] used a partial laminectomy. The angulation for the CPS was determined by placing a dental probe through the laminar window onto the superior, medial and inferior borders of the pedicle. Different open techniques have already proven to reduce the incidence and severity of pedicle violations [6, 8, 16, 19, 24, 33, 34].
So far, surgery with computer-assisted image guidance systems (CAS) seems to have the lowest pedicle violation rate [21, 27, 33, 37, 41]. But even when utilizing CAS, some screws still caused pedicle wall perforation [21]. Ludwig et al. [33] presented a comparative analysis of three different CPS placement techniques: (1) surface landmarks; (2) open technique (lamino–foraminotomy); (3) computer-assisted surgical system. They found statistically significant differences of accurately placed screws between the three groups (12.5 vs. 45 vs. 76%).
Roh et al. [42] described a technique called “perfect pedicle technique” with a setup of two crossed C-bows. This technique may work well under laboratory conditions. Our attempt to apply the “perfect pedicle view” technique for the determination of the CPS entry points in cadavers failed. The shoulders, table or the head holder prevented proper positioning of the C-bow.
We have examined two techniques of pedicle screw insertion in three randomly selected cadavers each. Both techniques rely on preoperative CT measurements as well as on intraoperative fluoroscopy to monitor the drill direction.
In technique 1 (ST1) drilling of the screw hole was performed through the drill sleeve of a small handheld aiming device. The endplate of the device was applied onto the medial border of the pedicle through a para-articular mini-laminotomy. In technique 2 (ST2) a more complex and fully adjustable aiming device was used. It consists of a frame, mounted on a radiolucent base plate, and a radiolucent arm for carrying the instruments necessary for placing the screws.
The screws consisted of carbon fibers and PEEK (CF-PEEK) with a small amount of Ta-fibers. The latter renders the screws fluoroscopically visible without creating significant artifacts in the CT. In their first description of the CPS placement technique Abumi et al. [2] already pointed out that the CT-assessment of the screw position is difficult because of the artifacts when metal screws are used. Raters tend to “overcall” pedicle wall violation, presumably due to a boundary artifact, despite optimal bone windows and even with titanium screws [25].
ST1 can be considered an “open” technique with direct visualization of the medial pedicle wall. In contrast, ST2 may be called a “closed” technique because only the outer surfaces of the posterior vertebral elements are exposed. The aiming device is set in accordance with CT measurements and anatomic landmarks for CPS entrance point localization. Once the entrance point and correct drill direction is set, the new aiming device assists in maintaining the proper drill direction. Safe CPS placement using technique 2 strongly depends not only on the proper screw orientation but also on the identification of the entry points for the screws. A variety of techniques have been developed to identify the entrance point for the CPS at the posterior cortex of the articular mass [2, 13, 19, 21, 51]. We have adopted the technique proposed by Karaikovic et al. [23].
Results
Pertinent literature describes different ways to evaluate the postoperative screw position. We determined the postoperative screw position by applying the same CT protocol as used preoperatively and subsequently graded the screw position into four categories, from ideal to unacceptable.
Fifty-six pedicle screws could be evaluated (cp. Table 3). Accuracy of pedicle screw placement did not significantly differ between techniques 1 and 2, and was not dependent upon the level or pedicle diameters. However, some trends regarding the screw position could be observed. A tendency to less severe misplacements in ST2 (15% in ST2 vs. 23% in ST1) as well as a higher rate of acceptable screw positions (62% in ST2 vs. 43% in ST1) were observed. This may be attributed to the more rigid guiding of the instruments by the aiming frame.
The tendency for a lateral pedicle wall perforation was obviously higher than medial wall perforation. This is consistent with the results published by Jones et al. [20]. One reason may be the fact that the lateral pedicle wall is thinner and therefore less resistant [22, 39]. Another reason may be a too steep angle of CPS insertion which is likely to occur when CPS is inserted through a standard posterior approach to the cervical spine. The counter pressure of the nuchal muscles may deviate the instruments towards the sagittal plane or even cause their bending. With regard to the clinical relevance of lateral misplacement Abumi et al. [5] opine that the likelihood of injury to the vertebral artery might not be high because the vertebral artery does not occupy the whole cross sectional diameter of the transverse foramen.
Similar to observations described by Ludwig et al. [33], Miller et al. [34] and Jones et al. [20], we did not detect any cranial or caudal violations of the pedicle. This can be explained by the fact that cervical pedicles have an oval shape with a significantly greater height than width at all levels [38].
Screw dimension still remains an important issue for CPS fixation. We acknowledge the fact that in a clinical setting differences of pedicle dimensions have to be carefully addressed. Cervical segments with very small inner diameters of the pedicle or without medullary canal should be excluded from the procedure [41]. In this study the diameter of the screw was 3.5 mm consistently and thus was not matched to the individual pedicle dimensions. Retrospectively, we do believe that most minor pedicle wall violations (grade IIa) may be attributed to the disproportion between screw diameter and the IPW. A total of 50 (83.3%) pedicles of this series had an IPW of 3.5 mm or less.
We found that large insertion angles are applicable under experimental conditions, but may exclude the CPS insertion through a standard posterior approach since this would require an unacceptable wide retraction of the nuchal muscles.
This problem can be overcome by inserting CPS transcutaneously through stab incisions as proposed by Jeanneret et al. [19].
Conclusion
Cadaver studies and careful preoperative CT evaluation with multiplanar reconstructions of pedicle dimensions are essential and contribute to the safety of cervical transpedicular screw placement. In comparison with published literature, the incidence of pedicle wall violation could not be significantly lowered by either one of the two techniques described in this study. Results of in-vitro studies relying on CAS seem to outmatch those achieved with other surgical techniques. Therefore further investigation using screw sizes matched to the pedicles and modified aiming frame (ST2: transcutaneous screw placement) will be performed and compared with computer-assisted guidance as control to further increase accuracy of a less expensive and technically less demanding surgical technique (ST2) for CPS placement.
Acknowledgments
Specimens for this study were provided by Prof. H. Maurer, Department of Human Anatomy and Embryology, Medical University Innsbruck, Austria. Implants were provided by Icotec AG, Altstaetten, Switzerland.
Footnotes
ICOTEC AG, Altstaetten, Switzerland
Definition “lateral vertebral notch”: most medial part of the ridge of the pars interarticularis located on the lateral mass [23]
Due to the fact that the PSA as measured in the CT reconstructions refers to the lower endplate of the individual vertebral body at every level, the direction of the respective lower endplate had to be determined by lateral fluoroscopy at first.
References
- 1.Abumi K, Kaneda K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine. 1997;22(16):1853–1863. doi: 10.1097/00007632-199708150-00010. [DOI] [PubMed] [Google Scholar]
- 2.Abumi K, Ito M, Taneichi H, Kaneda K. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord. 1994;7:19–28. doi: 10.1097/00002517-199407010-00003. [DOI] [PubMed] [Google Scholar]
- 3.Abumi K, Kaneda K, Shono Y, Fujiya M. One-stage posterior decompression and reconstruction of the cervical spine by using pedicle screw fixation systems. J Neurosurg. 1999;90(1 Suppl):19–26. doi: 10.3171/spi.1999.90.1.0019. [DOI] [PubMed] [Google Scholar]
- 4.Abumi K, Takada T, Shono Y, Kaneda K, Fujiya M. Posterior occipitocervical reconstruction using cervical pedicle screws and plate-rod systems. Spine. 1999;24(14):1425–1434. doi: 10.1097/00007632-199907150-00007. [DOI] [PubMed] [Google Scholar]
- 5.Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine. 2000;25(8):962–969. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 6.Albert TJ, Klein GR, Joffe D, Vaccaros AR. Use of cervicothoracic junction pedicle screws for reconstruction of complex cervical spine pathology. Spine. 1998;23:1596–1599. doi: 10.1097/00007632-199807150-00017. [DOI] [PubMed] [Google Scholar]
- 7.Albert TJ, Klein GR, Vaccaro AR. Image-guided anterior cervical corpectomy. A feasibility study. Spine. 1999;24(8):826–830. doi: 10.1097/00007632-199904150-00017. [DOI] [PubMed] [Google Scholar]
- 8.Barrey C, Cotton F, Jund J, Mertens P, Perrin G. Transpedicular screwing of the seventh cervical vertebra: anatomical considerations and surgical technique. Surg Radiol Anat. 2003;25(5–6):354–360. doi: 10.1007/s00276-003-0163-5. [DOI] [PubMed] [Google Scholar]
- 9.Blauth M, Duschek R, Schmidt U. Gerät zur Reposition und intraoperativen Lagerung instabiler Verletzungen der Halswirbelsäule. Operat Orthop Traumatol. 1994;6(4):285–289. doi: 10.1007/BF02511336. [DOI] [Google Scholar]
- 10.Borne GM, Bedou GL, Pinaudeau M. Treatment of pedicular fractures of the axis. A clinical study and screw fixation technique. J Neurosurg. 1984;60(1):88–93. doi: 10.3171/jns.1984.60.1.0088. [DOI] [PubMed] [Google Scholar]
- 11.Bozbuga M, Ozturk A, Ari Z, Sahinoglu K, Bayraktar B, Cecen A. Morphometric evaluation of subaxial cervical vertebrae for surgical application of transpedicular screw fixation. Spine. 2004;29(17):1876–1880. doi: 10.1097/01.brs.0000137065.62516.01. [DOI] [PubMed] [Google Scholar]
- 12.Choueka J, Spivak JM, Kummer FJ, Steger T. Flexion failure of posterior cervical lateral mass screws. Influence of insertion technique and position. Spine. 1996;21(4):462–468. doi: 10.1097/00007632-199602150-00010. [DOI] [PubMed] [Google Scholar]
- 13.Ebraheim NA, Xu R, Knight T, Yeasting RA. Morphometric evaluation of lower cervical pedicle and its projection. Spine. 1997;22(1):1–6. doi: 10.1097/00007632-199701010-00001. [DOI] [PubMed] [Google Scholar]
- 14.Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine. 1993;18(15):2231–2238. doi: 10.1097/00007632-199311000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Fehlings MG, Cooper PR, Errico TJ. Posterior plates in the management of cervical instability: long-term results in 44 patients. J Neurosurg. 1994;81(3):341–349. doi: 10.3171/jns.1994.81.3.0341. [DOI] [PubMed] [Google Scholar]
- 16.Hardy RW., Jr The posterior surgical approach to the cervical spine. Neuroimaging Clin N Am. 1995;5(3):481–490. [PubMed] [Google Scholar]
- 17.Heller JG, Carlson GD, Abitbol JJ, Garfin SR. Anatomic comparison of the Roy-Camille and Magerl techniques for screw placement in the lower cervical spine. Spine. 1991;16(10 Suppl):S552–S557. doi: 10.1097/00007632-199110001-00020. [DOI] [PubMed] [Google Scholar]
- 18.Heller JG, Silcox DH, III, Sutterlin CE., III Complications of posterior cervical plating. Spine. 1995;20(22):2442–2448. doi: 10.1097/00007632-199511001-00013. [DOI] [PubMed] [Google Scholar]
- 19.Jeanneret B, Gebhard JS, Magerl F. Transpedicular screw fixation of articular mass fracture-separation: results of an anatomical study and operative technique. J Spinal Disord. 1994;7(3):222–229. doi: 10.1097/00002517-199407030-00004. [DOI] [PubMed] [Google Scholar]
- 20.Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine. 1997;22(9):977–982. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 21.Kamimura M, Ebara S, Itoh H, Tateiwa Y, Kinoshita T, Takaoka K. Cervical pedicle screw insertion: assessment of safety and accuracy with computer-assisted image guidance. J Spinal Disord. 2000;13(3):218–224. doi: 10.1097/00002517-200006000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Karaikovic EE, Daubs MD, Madsen RW, Gaines RW., Jr Morphologic characteristics of human cervical pedicles. Spine. 1997;22(5):493–500. doi: 10.1097/00007632-199703010-00005. [DOI] [PubMed] [Google Scholar]
- 23.Karaikovic EE, Kunakornsawat S, Daubs MD, Madsen TW, Gaines RW., Jr Surgical anatomy of the cervical pedicles: landmarks for posterior cervical pedicle entrance localization. J Spinal Disord. 2000;13(1):63–72. doi: 10.1097/00002517-200002000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Karaikovic EE, Yingsakmongkol W, Gaines RW., Jr Accuracy of cervical pedicle screw placement using the funnel technique. Spine. 2001;26(22):2456–2462. doi: 10.1097/00007632-200111150-00012. [DOI] [PubMed] [Google Scholar]
- 25.Kim HS, Heller JG, Hudgins PA, Fountain JA. The accuracy of computed tomography in assessing cervical pedicle screw placement. Spine. 2003;28(21):2441–2446. doi: 10.1097/01.BRS.0000090830.94641.AE. [DOI] [PubMed] [Google Scholar]
- 26.Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems. An assessment of transpedicular screw fixation in the cervical spine. Spine. 1994;19(22):2529–2539. doi: 10.1097/00007632-199411001-00007. [DOI] [PubMed] [Google Scholar]
- 27.Kotani Y, Abumi K, Ito M, Minami A. Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg. 2003;99(3 Suppl):257–263. doi: 10.3171/spi.2003.99.3.0257. [DOI] [PubMed] [Google Scholar]
- 28.Kothe R, O’Holleran JD, Liu W, Panjabi MM. Internal architecture of the thoracic pedicle. An anatomic study. Spine. 1996;21(3):264–270. doi: 10.1097/00007632-199602010-00002. [DOI] [PubMed] [Google Scholar]
- 29.Kothe R, Ruther W, Schneider E, Linke B. Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine. 2004;29(17):1869–1875. doi: 10.1097/01.brs.0000137287.67388.0b. [DOI] [PubMed] [Google Scholar]
- 30.Kowalski JM, Ludwig SC, Hutton WC, Heller JG. Cervical spine pedicle screws: a biomechanical comparison of two insertion techniques. Spine. 2000;25(22):2865–2867. doi: 10.1097/00007632-200011150-00005. [DOI] [PubMed] [Google Scholar]
- 31.Ludwig SC, Kramer DL, Vaccaro AR, Albert TJ. Transpedicle screw fixation of the cervical spine. Clin Orthop. 1999;359:77–88. doi: 10.1097/00003086-199902000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Ludwig SC, Kowalski JM, Edwards CC, Heller JG. Cervical pedicle screws: comparative accuracy of two insertion techniques. Spine. 2000;25(20):2675–2681. doi: 10.1097/00007632-200010150-00022. [DOI] [PubMed] [Google Scholar]
- 33.Ludwig SC, Kramer DL, Balderston RA, Vaccaro AR, Foley KF, Albert TJ. Placement of pedicle screws in the human cadaveric cervical spine: comparative accuracy of three techniques. Spine. 2000;25(13):1655–1667. doi: 10.1097/00007632-200007010-00009. [DOI] [PubMed] [Google Scholar]
- 34.Miller RM, Ebraheim NA, Xu R, Yeasting RA. Anatomic consideration of transpedicular screw placement in the cervical spine. An analysis of two approaches. Spine. 1996;21(20):2317–2322. doi: 10.1097/00007632-199610150-00003. [DOI] [PubMed] [Google Scholar]
- 35.Misenhimer GR, Peek RD, Wiltse LL, Rothman SL, Widell EH., Jr Anatomic analysis of pedicle cortical and cancellous diameter as related to screw size. Spine. 1989;14(4):367–372. doi: 10.1097/00007632-198904000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Nolte LP, Zamorano L, Visarius H, Berlemann U, et al. Clinical evaluation of a system for precision enhancement in spine surgery. Clin Biomech (Bristol, Avon) 1995;10(6):293–303. doi: 10.1016/0268-0033(95)00004-5. [DOI] [PubMed] [Google Scholar]
- 37.Nolte LP, Zamorano LJ, Jiang Z, Wang Q, Langlotz F, Berlemann U. Image-guided insertion of transpedicular screws. A laboratory set-up. Spine. 1995;20(4):497–500. doi: 10.1097/00007632-199502001-00016. [DOI] [PubMed] [Google Scholar]
- 38.Panjabi MM, Duranceau J, Goel V, Oxland T, Takata K. Cervical human vertebrae. Quantitative three-dimensional anatomy of the middle and lower regions. Spine. 1991;16(8):861–869. doi: 10.1097/00007632-199108000-00001. [DOI] [PubMed] [Google Scholar]
- 39.Panjabi MM, Shin EK, Chen NC, Wang JL. Internal morphology of human cervical pedicles. Spine. 2000;25(10):1197–1205. doi: 10.1097/00007632-200005150-00002. [DOI] [PubMed] [Google Scholar]
- 40.Reichle E, Sellenschloh K, Morlock M, Eggers C. Placement of pedicle screws using different navigation systems. A laboratory trial with 12 spinal preparations. Orthopade. 2002;31(4):368–371. doi: 10.1007/s00132-001-0277-6. [DOI] [PubMed] [Google Scholar]
- 41.Richter M, Mattes T, Cakir B. Computer-assisted posterior instrumentation of the cervical and cervico-thoracic spine. Eur Spine J. 2004;13(1):50–59. doi: 10.1007/s00586-003-0604-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roh JS, Teng AL, Rice JA et al (2004) In: 32nd annual meeting, C_Ped III. Cervical Spine Research Society (ed) Paper #16: Accurate pedicle screw placement using laser-guided fluoroscopy: the “Perfect Pedicle” technique, vol 16. Cervical Spine Research Society, Boston, p 69
- 43.Roy-Camille R, Salient G, Mazel C (1989) Internal fixation of the unstable cervical spine by a posterior osteosynthesis with plates and screws. In: The Cervical Spine Research Society (Hrsg.) The cervical spine, 2nd edn. Aufl. JB Lippincott, Philadelphia, pp 390–403
- 44.Roy-Camille R, Mazel C, Saillant G, Benazet JP. Rationale and techniques of internal fixation in trauma of the cervical spine. In: Errico T, Bauer RD, Waugh T, editors. Spinal trauma. Philadelphia: JB Lippincott; 1991. pp. 163–191. [Google Scholar]
- 45.Sakamoto T, Neo M, Nakamura T. Transpedicular screw placement evaluated by axial computed tomography of the cervical pedicle. Spine. 2004;29(22):2510–2514. doi: 10.1097/01.brs.0000144404.68486.85. [DOI] [PubMed] [Google Scholar]
- 46.Shin EK, Panjabi MM, Chen NC, Wang JL. The anatomic variability of human cervical pedicles: considerations for transpedicular screw fixation in the middle and lower cervical spine. Eur Spine J. 2000;9(1):61–66. doi: 10.1007/s005860050011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stanescu S, Ebraheim NA, Yeasting R, Bailey AS, Jackson WT. Morphometric evaluation of the cervico-thoracic junction. Practical considerations for posterior fixation of the spine. Spine. 1994;19(18):2082–2088. doi: 10.1097/00007632-199409150-00014. [DOI] [PubMed] [Google Scholar]
- 48.Sutterlin CE, III, McAfee PC, Warden KE, Rey RM, Jr, Farey ID. A biomechanical evaluation of cervical spinal stabilization methods in a bovine model. Static and cyclical loading. Spine. 1988;13(7):795–802. doi: 10.1097/00007632-198807000-00015. [DOI] [PubMed] [Google Scholar]
- 49.Ugur HC, Attar A, Uz A, Tekdemir I, et al. Surgical anatomic evaluation of the cervical pedicle and adjacent neural structures. Neurosurgery. 2000;47(5):1162–1168. doi: 10.1097/00006123-200011000-00029. [DOI] [PubMed] [Google Scholar]
- 50.Weinstein JN, Rydevik BL, Rauschning W. Anatomic and technical considerations of pedicle screw fixation. Clin Orthop. 1992;284:34–46. [PubMed] [Google Scholar]
- 51.Xu Morphology of the second cervical vertebra and the posterior projection of the C2 pedicle axis. Spine. 1995;20(3):259–263. doi: 10.1097/00007632-199502000-00001. [DOI] [PubMed] [Google Scholar]
- 52.Xu R, Kang A, Ebraheim NA, Yeasting RA. Anatomic relation between the cervical pedicle and the adjacent neural structures. Spine. 1999;24(5):451–454. doi: 10.1097/00007632-199903010-00008. [DOI] [PubMed] [Google Scholar]