Abstract
If early neurological deterioration occurs following anterior cervical discectomy, the patient should be evaluated by urgent MRI scanning. In order to interpret such a scan it is essential to know what the normal post-operative MRI appearance is following an uncomplicated procedure. In the lumbar spine it is well recognized that early post-operative imaging following discectomy is difficult to interpret with a high rate of false positive scans.The normal appearance of MRI in the early post-operative period was evaluated prospectively in 15 patients undergoing anterior cervical discectomy without fusion for either cervical radiculopathy or myelopathy. MRI was performed on the first post-operative day, at 6 weeks and 6 months. The successful outcome of the procedure was validated by uniform improvement of Visual Analogue Scale measurement for neck and arm pain, the Neck Disability Index and European Myelopathy Score as appropriate.In contrast to the established findings following lumbar discectomy, only two cases showed a persistent epidural mass in the first post-operative scan and this had completely resolved at 6 months. All patients had foraminal narrowing and root or cord compression pre-operatively. Sixty six percent of cases showed persistent foraminal narrowing on sequential imaging up to 6 months despite showing good symptomatic improvement. All cases demonstrated high signal in the operated disc space on T2 weighted imaging on the first post-operative day and this finding persisted in 13 of 15 scans performed at 6 weeks. Post contrast imaging demonstrated no enhancement of operated disc space and adjacent vertebral body on the first post-operative day, whereas all scans at 6 weeks showed enhancement and such enhancement persisted at 6 months in 50%. Persistent epidural filling defects are uncommon following successful anterior cervical discectomy but persistence of foraminal narrowing is common despite successful outcome. Enhancement of the disc space is also common and does not in itself imply infection.
Keywords: Cervical spine, Anterior cervical discectomy, Post-operative findings, Magnetic resonance imaging
Introduction
Evaluation of patients who have neurological complications in the early post-operative period after anterior cervical discectomy (ACD) can be a diagnostic challenge. An unexplained neurological deterioration occurs in a small number of patients (<1%) undergoing ACD for the treatment of radiculopathy or myelopathy. Post-operative epidural haematoma or a missed disc fragment must be considered in the evaluation of these patients. Magnetic resonance imaging (MRI) is presently the diagnostic investigation of choice. However, its use in the early post-operative period is limited by insufficient knowledge of the normal post-operative changes in the cervical disc space, vertebral end-plates and epidural region and their clinical correlation, thus making the interpretation of urgent post-operative MRI scanning difficult. The normal healing process during the immediate post-operative period can make identification of pathological conditions, such as haematoma, discitis and residual or migrated disc fragments difficult. There is no published literature, which evaluates MRI of the cervical spine after ACD without fusion. The aim of this study is to determine the normal features of MRI scans in the early post-operative period following uncomplicated surgery to remove cervical disc prolapse.
Materials and methods
Fifteen consecutive patients undergoing ACD without fusion for either radiculopathy or myelopathy due to single level cervical disc protrusion were prospectively entered into the study. Ethical committee permission was obtained for this study and informed consent was taken from all the patients. All the procedures were performed under the supervision of two senior neurosurgical consultants with a special interest in spinal surgery. All patients underwent a standardized surgical procedure comprising a transverse cervical right-sided incision and routine anterior cervical approach to the cervical spine. A surgical microscope was used during discectomy, posterior longitudinal ligament release and proximal root canal decompression. Vertebral distracters and high-speed drills were not used during decompression. All the patients underwent diagnostic MRI study prior to surgery. Post-operative MRI scans, before and after contrast, were performed on the first post-operative day, at 6 weeks, and at 6 months following the procedure. The MRI scans were performed on the GE Signa Horizon LX MRI scanner using a spine coil with an identical protocol consisting of T1 sagittal images (TR 440, TE 13, Field of view 24/24 cm), T2 sagittal images (TR 4000, TE 13, Field of view 24/24 cm), T1 axial images (TR 500, TE 8.1, Field of view 20/20 cm) and T2 axial images (TR 720, TE 15, Field of view 20/20 cm). Slice thickness was 3 mm in all the images. T2 weighted gradient echo sequence was used. Standard T1 spin echo sequence was used after intravenous contrast administration. All patients completed Visual Analogue Scale (VAS) measurement for arm and neck pain, and Neck Disability Index (NDI) [12] pre-operatively and at the time of each post-operative MRI scan to allow assessment of the successful outcome of the surgery. Those patients presenting with myelopathy also completed the European Myelopathy Score (EMS) at the same intervals. Three independent observers, blinded to clinical presentation and outcome, analysed these MRI scans. One was a consultant neurosurgeon and the other two were senior neuroradiologists. None of the observers were involved in the management of these patients. Observers looked for disc protrusion, osteophyte causing foraminal narrowing, cervical cord and nerve root compression, intensity of signal in the disc and epidural space, and posterior compression from ligamentum flavum infolding in all three post-operative MRI scans and then compared with the pre-operative MRI scan. Post contrast T1 weighted images were specifically examined to identify enhancement of the disc space, vertebral end-plates and marrow, and remnants of disc material either in the epidural space or in the nerve root foramina.
Results
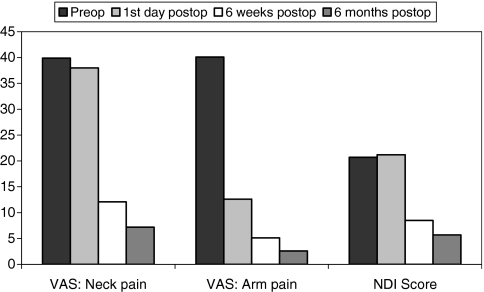
The mean patient age at operation was 46 years (range 24–61 years). Nine were females and six were males. Presenting symptoms were radiculopathy only in ten patients, myelopathy only in four patients and myeloradiculopathy in one patient. The mean duration of radiculopathy was 16 months (range 3–30 months) and myelopathy was 13 months (range 3–26 months). There were no post-operative complications. VAS for neck pain and arm pain and NDI score uniformly improved during the early post-operative period in all of our patients (Fig. 1). The mean EMS of 13 (range 10–14) in the pre-operative period had improved to 16 (range 14–17) at 6 months after surgery in the myelopathy group.
Fig. 1.
showing uniform improvement of Visual Analogue Scale measurement for neck pain and arm pain, and Neck Disability Index score from pre-operative period to first day, 6 weeks and 6 months post-operative period
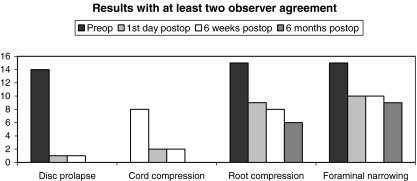
Disc prolapse (both hard and soft disc) was noted in all pre-operative images except one, which showed root compression by osteophyte correlating with radiculopathy presentation. All showed narrowing of the foramina and root compression. Two patients showed persisting cord compression, possibly due to remnants of disc or osteophyte material in the early and 6 weeks post-operative scans. However the degree of compression was much less than the pre-operative scan and these changes resolved at 6 months. Foraminal narrowing persisted in 66% of the first post-operative scans and did not resolve in the follow-up scans up to 6 months (Fig. 2). Interobserver agreement as assessed by the kappa value showed good to moderate agreement in the interpretation of the pre-operative and early serial post-operative scans for cervical cord and root compression (Table 1).
Fig. 2.
MRI findings. Both disc prolapse and cord compression resolved completely by 6 months whereas root compression and foraminal narrowing persisted in up to 66% of cases at 6 months, following surgery
Table 1.
Interobserver agreement and kappa value between the six sets of observations, by observer A, B and C, after grouping them into two categories, cord and root compression
| Observer | Agreement (%) | Kappa value | ||
|---|---|---|---|---|
| Cord Compression | A–B | 90 | 0.67 | Good |
| B–C | 85 | 0.55 | Moderate | |
| C–A | 87 | 0.67 | Good | |
| Root Compression | A–B | 70 | 0.41 | Moderate |
| B–C | 80 | 0.55 | Moderate | |
| C–A | 72 | 0.44 | Moderate |
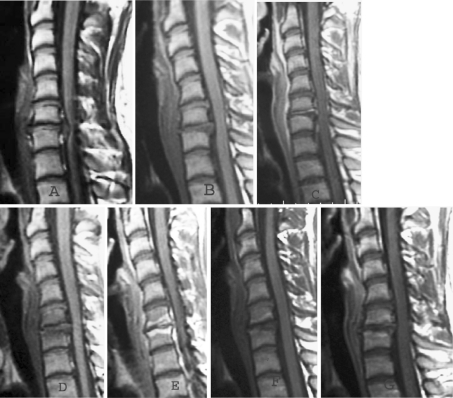
None of the post-operative scans showed haematoma formation in the spinal canal in the early post-operative images. Similarly no patient developed posterior cord compression secondary to ligamentum flavum infolding. There were no metal artefacts in the post-operative images. High signal in T2 weighted images at the operated disc space were seen in all patients on the first post-operative day and in 13 of the 15 cases at 6 weeks post surgery (Fig. 3). Only one patient showed this persisting high signal at the operated level at 6 months post surgery. All five of our patients with myelopathy showed high signal in the cord at operated level in the pre-operative scan. The high signal in the cord persisted in four patients at 6 months post surgery. Post contrast T1 weighted images showed enhancement of the disc space, vertebral end-plates and adjacent vertebral body at the operated level in all patients at 6 weeks, whereas no enhancement was seen in the first day post-operative scans. This enhancement in the disc space and in the vertebral bodies persisted in 8 out of our 15 patients at 6 months (Fig. 4).
Fig. 3.
a, b, c and d Sagittal T2 weighted MRI images of 49-year-old male presented with 12 month history of radiculopathy. a. Pre-operative image showing disc prolapse at C5/6 level. b. First day post-operative image showing high signal at operated disc space with no indentation on to the cord and no haematoma in the spinal canal. c. 6 weeks post-operative image showing high signal both at operated disc space and adjacent vertebral bodies. d. 6 months post-operative image showing low signal at operated level
Fig. 4.
Pre-operative T1 weighted MRI sagittal image (a) of a 23-year-old female patient presented with 3 month history of radiculopathy and myelopathy, showing disc prolapse at C6/7 level. Compared to first post-operative day pre contrast T1 weighted image (b), the post contrast T1 weighted image (c) has shown no enhancement of vertebral end-plates at operated level. At 6 weeks, compared to pre contrast image (d), the post contrast image (e) has shown brilliant enhancement of end-plates and adjacent vertebral marrow. But at 6 months, compared to pre contrast image (f), the post contrast image (g) has shown low grade enhancement in vertebra marrow at operated level
Discussion
A number of studies [1, 3, 4, 5] have documented the normal sequence of MRI changes in the lumbar spine following surgery for disc herniation using both plain and contrast enhanced scans. Findings such as residual disc herniation, annular bulge and displaced nerve root were found to occur commonly on initial follow-up scans in spite of excellent results in terms of pain relief or improved neurology.
Annertz et al. [1] examined 20 patients who had undergone successful surgery for lumbar disc herniation. All patients underwent MRI scanning on the fifth post-operative day and 19 of the 20 were found to have persistent deformation of the thecal sac despite the relief of their symptoms. Boden et al. [3] in a similar study of 15 patients found a persistent mass effect at the site of the original disc herniation in 38% at 3 weeks. Deutsch et al. [4] found persisting mass effects in 13 of 23 successful cases of lumbar disc surgery at 12 months following the operation. Floris et al. [5] performed early post-operative MRI at 3 days and follow-up MRI at 8 weeks following lumbar microdiscectomy. They noted that 24 patients (80%) had apparent disc herniation on the early post-operative MRI scans with this persisting in 12 patients (50%) at 8 weeks.
It is clear that post-operative MRI of patients following successful lumbar disc surgery carries a significant false positive rate. The use of MRI scanning to assess patients who experience complications early after lumbar disc surgery must, therefore, be very carefully interpreted. It is possible that the same situation may occur in patients undergoing cervical disc surgery but the current literature does not provide strong evidence as to whether this is correct. Technically cervical discectomy differs from lumbar disc surgery, as it is normal to excise both the entire disc and posterior longitudinal ligament in the cervical region, whereas in lumbar disc surgery only a small amount of disc material is removed.
Scarabino et al. [10] examined 26 patients with MRI scans following cervical surgery. Sixteen of them had undergone anterior cervical discectomy and fusion (ACDF) whereas seven had posterior decompression and three had vertebral body removal. In the ACDF group they noted massive signal changes in the bone graft and lower vertebral end-plates, which were hypointense on T1 and hyperintense on T2. It was unclear at what stage following the procedure the MRI scans were performed. Schneider et al. [11] performed MRI scanning at seven days and also at 6 months, following ACD and implantation of methacrylate along with fibrin sponge, in 14 patients. They found protrusion of the posterior ligament at seven days in 80% of cases, which mimicked residual disc or osteophytes. This disappeared at 6 months in all patients. In the presence of gelatinous sponge, which they used to protect the dura from the heat of the methacrylate polymerization, it may be difficult to identify the cause for persistent protrusion in early post-operative scans.
MRI signal changes in the vertebral body and adjacent end-plates following ACD depend upon the status of vertebral body marrow, the amount of trauma received during surgery, the degree of revascularization and the extent of post-operative stresses at that level. In a retrospective study Ross et al. [8] noted spectrum of graft and vertebral body signal changes up to 2 years following ACDF. Patients studied more than 2 years following ACDF generally showed solid bony fusion without evidence of the graft or original disc space. Kleft van de et al. [6] performed MRI 6 months after ACD without fusion in 45 patients. They noted low signal intensity in the disc space on T2 weighted images at operated level in all patients.
The metallic artefacts described by other authors [10] in post-operative cervical MRI scans probably arise from the metal suction tip as it is occasionally hit by a high speed drill [7]. Salazar et al. [9] described four cases with artefacts following ACDF, which gave the appearance of persistence of the disc herniation in the early post-operative period. Arunkumar and Rajshekhar [2] presented a further two cases with similar findings.
In our study we found that persistence of an epidural filling defect on the first post-operative day was most uncommon. Such a finding should imply a strong likelihood of the presence of a missed disc fragment. However, foraminal narrowing as judged by MRI was found in two-thirds of cases despite good surgical outcomes implying little significance of this radiological finding. Finally, enhancement of the post-operative disc space is a universal finding at 6 weeks and persists in 50% at 6 months. Such a finding does not necessarily imply post-operative disc space infection.
Conclusions
Our findings following simple anterior cervical discectomy without fusion show that the finding of epidural compression on MRI following uncomplicated surgery is rare. Should a patient suffer neurological deterioration following surgery, then the findings of persisting the epidural compression should alert the surgeon to the likelihood that there is a retained disc fragment. On the other hand, apparent foraminal narrowing as assessed by MRI is common even following successful surgery.
The appearance of persisting enhancement of the disc space and end-plates following gadolinium is common in the early post-operative period following ACD. Enhancement of the structures per se does not imply infection.
References
- 1.Annertz M, Jonsson B, Stromqvist B, et al. Serial MRI in the early postoperative period after lumbar discectomy. Neuroradiology. 1995;37:177–182. doi: 10.1007/BF01578253. [DOI] [PubMed] [Google Scholar]
- 2.Arunkumar MJ, Rajshekhar V. Artifacts in magnetic resonance images following anterior cervical discectomy and fusion: report of 2 cases. Br J Neurosurg. 1998;12(6):553–5. doi: 10.1080/02688699844411. [DOI] [PubMed] [Google Scholar]
- 3.Boden SD, Spallone A, Aref TY, et al. Contrast-enhanced MR imaging performed after successful lumbar disk surgery: prospective study. Radiology. 1992;182(1):59–64. doi: 10.1148/radiology.182.1.1727310. [DOI] [PubMed] [Google Scholar]
- 4.Deutsch Lumbar spine following successful surgical discectomy. Magnetic resonance imaging features and implications. Spine. 1993;18(8):1054–60. doi: 10.1097/00007632-199306150-00016. [DOI] [PubMed] [Google Scholar]
- 5.Floris R, Spallone A, Aref TY, et al. Early postoperative MRI findings following surgery for herniated lumbar disc. Acta Neurochir (Wien) 1997;139(3):169–75. doi: 10.1007/BF01844746. [DOI] [PubMed] [Google Scholar]
- 6.Kleft E, Vyve M, Selosse P. Post surgical follow-up by MRI after anterior cervical discectomy without fusion. Eur J Radiol. 1992;15:196–99. doi: 10.1016/0720-048X(92)90105-I. [DOI] [PubMed] [Google Scholar]
- 7.Peterman SB, Hoffman JC, Malko LA. Magnetic resonance artifact in the postoperative cervical spine. A potential pitfall. Spine. 1991;16(7):721–5. doi: 10.1097/00007632-199107000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Ross JS, Masaryk TJ, Modic MT. Postoperative Cervical Spine: MR Assessment. J Comput Assist Tomogr. 1987;11(6):955–962. doi: 10.1097/00004728-198711000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Salazar JL, Misra M, Bloom D, et al. MRI artifacts following anterior cervical discectomy. Surg Neurol. 1997;48(1):23–9. doi: 10.1016/S0090-3019(96)00418-1. [DOI] [PubMed] [Google Scholar]
- 10.Scarabino T, Perfetto F, Giannatempo GM, et al. Imaging with magnetic resonance imaging of the operated cervical spine. Radiol Med (Torino) 1996;92F(6):671–6. [PubMed] [Google Scholar]
- 11.Schneider T, Brechtelsbauer D, Wildforster U, et al. MRI findings after uncomplicated anterior cervical discectomy. Acta Neurochir (Wien) 2000;142(5):553–6. doi: 10.1007/s007010050468. [DOI] [PubMed] [Google Scholar]
- 12.Vernon H, Minor S. The disability index. A study of reliability and validity. J Manipulative Physiol Ther. 1991;141:409–415. [PubMed] [Google Scholar]