Abstract
Surgical instrumentation for the correction of adolescent idiopathic scoliosis (AIS) is a complex procedure involving many difficult decisions (i.e. spinal segment to instrument, type/location/number of hooks or screws, rod diameter/length/shape, implant attachment order, amount of rod rotation, etc.). Recent advances in instrumentation technology have brought a large increase in the number of options. Despite numerous clinical publications, there is still no consensus on the optimal surgical plan for each curve type. The objective of this study was to document and analyse instrumentation configuration and strategy variability. Five females (12–19 years) with AIS and an indication for posterior surgical instrumentation and fusion were selected. Curve patterns were as follows: two right thoracic (Cobb: 34°, 52°), two right thoracic and left lumbar (Cobb T/L: 57°/45°, 72°/70°) and 1 left thoraco-lumbar (Cobb: 64°). The pre-operative standing postero-anterior and lateral radiographs, supine side bending radiographs, a three-dimensional (3D) reconstruction of the spine, pertinent 3D measurements as well as clinical information such as age and gender of each patient were submitted to six experienced independent spinal deformity surgeons, who were asked to provide their preferred surgical planning using a posterior spinal approach. The following data were recorded using the graphical user interface of a spine surgery simulator (6×5 cases): implant types, vertebral level, position and 3D orientation of implants, anterior release levels, rod diameter and shape, attachment sequence, rod rotation (angle, direction), adjustments (screw rotation, contraction/distraction), etc. Overall, the number of implants used ranged from 11 to 26 per patient (average 16; SD ±4). Of these, 45% were mono-axial screws, 31% multi-axial screws and 24% hooks. At one extremity of the spectrum, one surgeon used only mono-axial screws, while at the other, another surgeon used 81% hooks. The selected superior- and inferior-instrumented vertebrae varied up to six and five levels, respectively (STD 1.2 and 1.5). A top-to-bottom attachment sequence was selected in 61% of the cases, a bottom-up in 29% and an alternate order in 11%. The rod rotation maneuver of the first rod varied from 0° (no rotation) to 140°, with a median at 90°. In conclusion, a large variability of instrumentation strategy in AIS was documented within a small experienced group of spinal deformity surgeons. The exact cause of this large variability is unclear but warrants further investigation with multicenter outcome studies as well as experimental and computer simulation studies. We hypothesize that this variability may be attributed to different objectives for correction, to surgeon’s personal preferences based on their previous experience, to the known inter-observer variability of current classification systems and to the current lack of clearly defined strategies or rational rules based on the validated biomechanical studies with modern multi-segmental instrumentation systems.
Keywords: Scoliosis, Surgical instrumentation, Pre-operative planning, Spine
Introduction
Spinal instrumentation and fusion is the recommended treatment for severe or progressive scoliotic deformities. The treatment of adolescent idiopathic scoliosis (AIS) with instrumentation became popular in the early 1960’s with the introduction of the Harrington instrumentation [15]. With this system, hooks attached to posterior elements of the upper and lower end vertebrae apply distraction forces to the concave side of the spinal curve using a ratchet mechanism. Rules for the selection of instrumentation and fusion levels were proposed and agreed upon by a majority of surgeons. Newer generations of spinal instrumentation systems consist of multiple types of hooks and/or screws attached to bilateral rods. They allow selective and three-dimensional (3D) correction of spinal deformities and strong fixation. Conversely they have brought a large increase in the number of possible options for the correction offered to the surgeon. Preoperative planning is now a complex procedure involving many difficult decisions. The goal of surgery is to obtain a stable, well-balanced spine and is achieved by reducing the magnitude of the deformity and obtaining fusion in order to prevent curve progression. During surgical planning, each surgeon has many factors to take into consideration: patient characteristics (spinal curve shape, balance, spine flexibility, neurologic status, rib deformities, skeletal maturity and remaining growth potential, etc.), instrumentation parameters (type, location and number of hooks and/or screws, spinal segments to instrument, diameter, length and shape of the rods, implant attachment order, peri-operative instrumentation maneuvers, etc.) and other surgery-related needs (transfusion, bone grafting, spinal cord monitoring and postoperative pain management) [17].
Despite numerous clinical publications [4, 5, 18, 19, 23, 30, 31, 33, 37, 43], there is no clear consensus on the preferred instrumentation system to use and even less consensus on the optimal operative plan for each curve type with modern multi-segmental instrumentation systems. Selection of the appropriate fusion levels remains one of the most challenging decisions in scoliosis surgery, and many guidelines have been proposed. A traditional teaching principle dating from the Harrington instrumentation era has been the fusion from T4 to L4 for combined thoracic and lumbar curves. Ferguson [10] suggested that the ideal fusion should extend to the vertebrae that have their distant surfaces parallel to each other. Moe [28] and Goldstein [11, 12] suggested fusing from the neutrally rotated vertebra above to the neutrally rotated vertebra below, the neutral vertebra being determined by the criteria established by Nash and Moe [29]. Harrington [16] proposed that the lower end of the fusion should lie in the “stable zone”, determined by two vertical lines drawn through the lumbosacral facets. He also recommended fusing one level above and two levels below the Cobb-measured curve. King et al. [18] The classic work of differentiated various curve patterns and recommended fusion to the “stable vertebra”, which is the inferior vertebra in the thoracic curve that is most closely bisected by the center sacral line. More recently Lenke et al. [24] proposed a comprehensive classification that takes into account regional curve deformations in the coronal and sagittal planes and the structural criteria to guide the extent of spinal arthrodesis and surgical choices.
The choice of the best rod-to-spine fixation devices is still a debated topic. Several studies have demonstrated better curve correction and shorter fusion length using pedicle screws rather than hooks in lumbar curves [3, 13, 14, 25] and more recently in thoracic curves [25, 41, 40, 39], while other studies question the benefits of pedicle screw fixation in thoracic curves [27, 32]. Chen and Yen [7] documented a correction rate of 67% and a loss at final follow-up of 7.8% after surgery using only hooks in 80 AIS patients who had King II and III curve patterns. A correction rate of 56% with 6.6% loss for thoracic curves, and 66.7% with 6.7% loss for lumbar curve has been reported with an hybrid technique, that uses both hooks and screws for fixation, in 61 AIS patients with King II and III curve patterns. A correction rate of 77% was achieved with an all-screw method [6].
All these studies, however, are based on cases series which are difficult to compare. For obvious reasons it is not possible to compare the result of different instrumentation configurations on the same individual patient, so the results of these studies are influenced by the variability of patients’ characteristics within each cohort as well as by the strategy adopted by the participating surgeons. To our knowledge, the variability of instrumentation strategy within a group of surgeons for the same subjects with AIS, has not been documented and remains unknown. It is assumed that faced with the same subject and using the same clinical and radiological information as well as the same instrumentation system, experienced spine surgeons should in general agree on the optimal surgical plan. The purpose of this study was specifically to document and analyze instrumentation configuration and strategy variability that exist between surgeons for the same subjects, in order to answer the following question: when confronted to the same patient, do spinal deformity surgeons have the same strategy and plan?
Material and methods
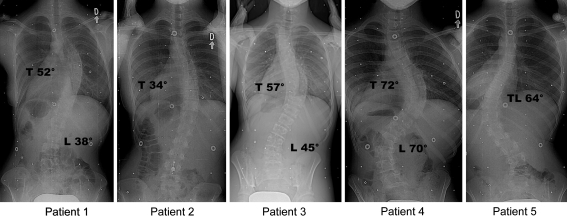
Five females (12–19 years) with AIS and an indication for posterior surgical instrumentation and fusion were selected. Curve patterns were as follows: two right thoracic (Cobb: 34°, 52°), two right thoracic and left lumbar (Cobb thoracic/lumbar: 57°/45°, 72°/70°) and one left thoraco-lumbar (Cobb: 64°). These cases were selected in order to represent common deformities seen in AIS, as can be seen on their coronal radiographs shown in Fig. 1.
Fig. 1.
Preoperative standing postero-anterior radiographs of the five patients
Six spinal deformity surgeons of the Scoliosis Research Society with a well established experience in spinal surgery agreed to participate in the study. They were coming from different hospitals in North America and at different stages of career. They were provided with the following information on each of the five patients: age, gender, preoperative standing postero-anterior and lateral radiographs, supine side bending radiographs and Cobb angles measurements of each curve (Fig. 1 and Table 1).
Table 1.
Patients’ characteristics
| Patient | Age (years) | Cobb thoracic (°) | Cobb thoraco-lumbar (°) | Cobb lumbar (°) | Cobb right Bending (°) | Cobb left bending (°) |
|---|---|---|---|---|---|---|
| 1 | 19 | 52 (right) | 36 | |||
| 2 | 18 | 34 (right) | 7 | |||
| 3 | 14 | 57 (right) | 45 (left) | 25 | 11 | |
| 4 | 15 | 72 (right) | 70 (left) | 36 | 40 | |
| 5 | 13 | 64 (left) | 23 |
For each case, a 3D reconstruction of the spine shape was also provided. It was obtained from a multiplanar radiographic technique, which has been detailed in previous publications [1, 9]. For the current study, all 3D reconstructions were performed with calibrated postero-anterior and lateral radiographs. A detailed geometric model [1, 9] of vertebrae was added to the reconstructions to allow easier visual interpretation. The spine could be visualized in any desired projection on a micro-computer. From the 3D reconstructed spine the following additional indices were computed and provided to the surgeons: Cobb angle in the plane of maximum curvature and the orientation of this plane, and axial orientation of the apical vertebra measured by the Stokes method [38].
Each surgeon was asked to detail his preferred surgical planning for each case using a posterior instrumentation system familiar to all these surgeons (CD Horizon, Medtronic Sofamor-Danek, Memphis, TN, USA). The following data was recorded using the graphical user interface of a dedicated in-house software (six surgeons × five cases):
Implant types: hooks (pedicular, laminar, transverse process), mono- and/or multi-axial screws
Vertebral level, position and 3D orientation of all implants
Number of rods, diameter and shape of each rod
Attachment sequence of each rod to the selected implants
Rod rotation (angle, direction)
Adjustments (screw rotation, compression/distraction)
They were also allowed to give any other comments or additional maneuvre (i.e. anterior release levels, etc.), which were saved by the software.
The variability of the parameters of surgical planning mentioned above, among the observations within the sample of 6×5 cases was analyzed first with standard descriptive statistics average, range and standard deviation (SD). Differences in the number of implants used for the left and right or concave and convex sides of the spine as well as the implant type (hooks, hybrid, all-screw groups) were assessed with two-sided Student t-tests for independent samples. The level of significance was set at 0.05.
Results
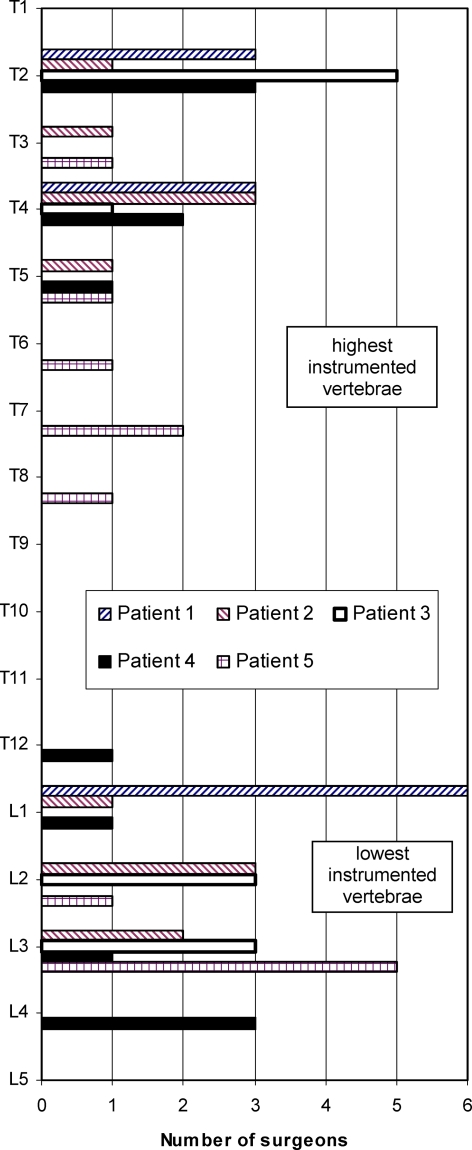
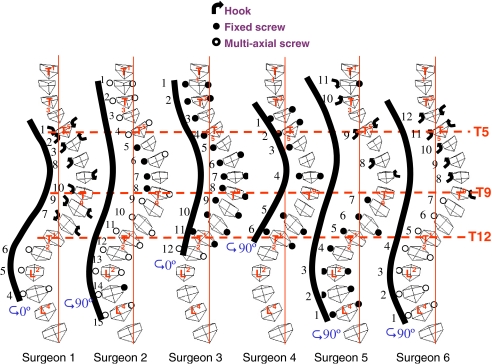
The pertinent results are summarized in Figs. 2, 3 and 4. Overall, the number of instrumented spinal segments varied significantly from 7 to 15 vertebrae, with an average and a standard deviation of 11.5±2.0 vertebrae. On a patient basis, no individual case was planned to be instrumented at the same levels by all surgeons, and in only one case (patient #1) there was complete agreement between surgeons for the selection of the lowest vertebra to instrument. The range of variation of the selected highest and lowest instrumented vertebrae was respectively six and five levels (SD: 1.2 and 1.5 level) (Fig. 2). The highest instrumented vertebra was selected at the same level only in 4% of all cases (superior limit of the main thoracic curve). It was one, two, three and four levels above respectively in 25%, 25%, 25% and 21% of the cases. The lowest instrumented vertebra was determined at the same level in 21% of all cases (inferior limit of the main thoracic curve). It was one and two levels above respectively in 14% and 4% of the cases and one, two, three and four levels below respectively in 14%, 32%, 4% and 11% of the cases. For example, for case #4 one surgeon proposed to instrument only the main thoracic curve, while one surgeon included the proximal thoracic curve, two surgeons included the lumbar curve while the remaining two surgeons chose to instrument all three curves (Fig. 3).
Fig. 2.
The variation in the choice of the highest and lowest instrumented vertebrae
Fig. 3.
The selection of fusion levels and the instrumentation configurations proposed by the six surgeons for patient #4
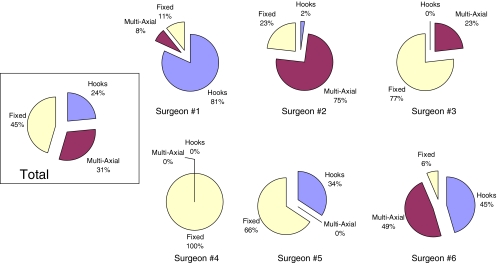
Fig. 4.
Types of implants selected by the six surgeons
The number and type of implants selected also varied significantly among surgeons and ranged from 11 to 26 per case with an average of 16 and a SD of four implants. On a specific patient basis, for the main scoliotic curve the number of implants installed on the convex side was significantly smaller (P = 0.0094) than on the concave side. The apical vertebra of the main scoliotic curve was instrumented on both sides in 43% of the cases, while it was instrumented on one side in 42% of the cases (equal number on either side).
Forty five percent of selected implants were mono-axial screws, 31% multi-axial screws, and 24% hooks (Fig. 4). At one end of the spectrum, one surgeon (#4) used only mono-axial screws, while at the other end another surgeon (#1) used mostly hooks, the remaining surgeons using a mix of screws and hooks (Fig. 4). At the apical vertebra a pedicle hook was used in 18% and 13% of the cases respectively on its convex and concave sides; a mono-axial screw in 37% and 43% of the cases respectively on its convex and concave sides; and a multi-axial screw in 10% and 7% of the cases respectively on its convex and concave sides.
A strategy using only hooks for correction was selected by one surgeon for two of the cases submitted (7%), while a hybrid or only-screw strategy were each used in 46% of the cases. There was no statistical difference between the two latter groups concerning the number of instrumented vertebrae (P=0.8502) or the number of implants used (P=0.0835).
The attachment order of the implants to the first rod also differed significantly. The top-to-bottom attachment was selected in 61% of the cases, the bottom-up attachment in 29% of the cases, while an alternate order was chosen for the remaining 11% of cases. The rotation maneuver of first rod also varied significantly (according to a non-Gaussian distribution) from 0° (no rotation) to 140° with a median at 90°. All instrumentation was made using two rods.
Discussion and conclusion
To our knowledge, this is the first attempt to document and compare pre-operative planning for the same subjects within a group of surgeons. This study has documented a large variability between experienced spinal deformity surgeons in their pre-operative planning and instrumentation strategies for common cases of AIS requiring instrumentation and fusion using a posterior approach. The lack of agreement appears particularly important for the selection of the proper vertebral levels to instrument and fuse. A careful analysis of Fig. 2 and of the wide range of levels selected strongly suggests that this variability can be attributed to disagreement as to which spinal curve, i.e. high thoracic, main thoracic or lumbar, needs to be instrumented and included in the fusion. In other words, surgeons do not agree on which curves are structural and therefore need to be included in the fusion. This is reflected by current controversies in the literature regarding the definition of a structural upper thoracic [20, 21, 42, 44] or lumbar curve [19, 21, 34, 36]. We suspect that part of the disagreement can also be explained by the well documented inter-observer variability of current surgical classification systems [8, 22, 24, 35]. However, as the surgeons were not asked to report which curve classification they were using and to classify each case with either using the King [18] or Lenke [24] system, it is not possible to confirm the effect of curve classification in the current study.
The number and type of implants selected were also found to be highly inconsistent between surgeons. We believe this finding also reflects current controversies in the literature concerning the optimal choice of implants for correction of AIS, and the evolving role of the use and indications of pedicle screws in this disorder. For many years, hook insertion technique was considered as the standard procedure for treating AIS. Nowadays pedicle screws have gained in popularity, initially for the lumbar segment but now more and more frequently in the thoracic region [41]. Various surgical methods for the correction of scoliotic spines are now available. When planning the surgical treatment for the different types of curves met in AIS, the familiarity of a surgeon with one or more of these instrumentation systems is important.
Between the surgeons that participated in this study there is a large variability regarding the type of implants used. We could identify one surgeon using hooks for the thoracic spine and screws for the lumbar spine and another two surgeons using hooks for the upper part of the curve, including the apex, and screws for the spine below the thoracic apex. As mentioned in the results section, one surgeon used only mono-axial screws and another one used mono-axial screws for the thoracic spine and multi-axial screws for the lumbar spine. The last surgeon used mono-axial screws in the apex region and multi-axial screws or hooks at both extremities of the curve. The surgeon’s selection of instrumentation also rely on personal experience, in a way that the surgeon recalls cases of patients seen in his practice and presenting similar characteristics with the present patient and he selects the method that gave good results in the past patients.
Several limitations of this study must be considered. First, the surgeons were in front of a computer, an artificial condition that does not totally correspond to the reality of the operating room, where the surgeon can change his preoperative planning approach because of different patient’s characteristics discovered only in the operating theater. Second, the small number of cases and relatively small number of surgeons made the ANOVA difficult and thus the possible detection of multiple factors and their interactions that influence the treatment choice.
However, the most important issue is the correction effect on scoliosis of different surgery strategies proposed. Using computer simulations, like a spine surgery simulator [2], is the only possibility to find out the surgical outcome of different instrumentation techniques, given the impossibility of practicing the surgery on the same patient for more than one time. In this way, the best spinal instrumentation configuration for a given patient can be chosen and a personalized biomechanical model of the patient’s spine could help to minimize the risk of complications.
In conclusion, a large variability of instrumentation strategy in AIS was documented within a small experienced group of spine surgeons, and therefore they do not have the same strategy and plan, when confronted to the same patient. The exact cause of this large variability is unclear, but warrants further investigation with multicentre outcome studies as well as with experimental and computer simulation studies [2]. We hypothesize that the current lack of agreement detected in this study may be explained by different objectives for correction, by personal surgeon’s preferences based on their previous experience, by the known inter-observer variability of current classification systems and/or by the current lack of clearly defined strategies or rational rules based of validated biomechanical studies with modern multi-segmental instrumentation systems.
Acknowledgements
This project was funded by the Natural Sciences and Engineering Research Council of Canada, the Canada Research Chair Program, and by an unrestricted educational grant of Medtronic Sofamor Danek. Special thanks to Drs L. Lenke MD, T. Lowe MD, J. Emans MD, D. Sucato MD, T. Kuklo MD, and Mr. M. Robitaille.
References
- 1.Aubin CE, Descrimes JL, Dansereau J, Skalli W, Lavaste F, Labelle H. Geometrical modeling of the spine and the thorax for the biomechanical analysis of scoliotic deformities using the finite element method (in French) Ann Chir. 1995;49(8):749–761. [PubMed] [Google Scholar]
- 2.Aubin CE, Petit Y, Stokes IA, Poulin F, Gardner-Morse M, Labelle H. Biomechanical modeling of posterior instrumentation of the scoliotic spine. Comput Methods Biomech Biomed Eng. 2003;6:27–32. doi: 10.1080/1025584031000072237. [DOI] [PubMed] [Google Scholar]
- 3.Barr SJ, Schuette AM, Emans JB. Lumbar pedicle screws versus hooks. Results in double major curves in adolescent idiopathic scoliosis. Spine. 1997;22:1369–1379. doi: 10.1097/00007632-199706150-00016. [DOI] [PubMed] [Google Scholar]
- 4.Bridwell KH. Surgical treatment of adolescent idiopathic scoliosis: the basics and the controversies. Spine. 1994;19:1095–1100. doi: 10.1097/00007632-199405000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Burton DC, Asher MA, Lai SM. The selection of fusion levels using torsional correction techniques in the surgical treatment of idiopathic scoliosis. Spine. 1999;24:1728–1739. doi: 10.1097/00007632-199908150-00015. [DOI] [PubMed] [Google Scholar]
- 6.Chen PQ. Management of scoliosis. J Formos Med Assoc. 2003;102:751–761. [PubMed] [Google Scholar]
- 7.Chen PQ, Yen LJ (2001) A 8 to 13–year follow-up of Cotrel-Dubousset instrumentation for the correction of King II and III adolescent idiopathic scoliosis. In: 21st annual combined meeting of the ASEAN and IOA, 2001, Bali
- 8.Cummings RJ, Loveless EA, Campbell J, Samelson S, Mazur JM. Interobserver reliability and intraobserver reproducibility of the system of King et al. for the classification of adolescent idiopathic scoliosis. J Bone Joint Surg Am. 1998;80:1107–1111. doi: 10.2106/00004623-199808000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Delorme S, Petit Y, Guise JA, Labelle H, Aubin CE, Dansereau J. Assessment of the 3-D reconstruction and high-resolution geometrical modeling of the human skeletal trunk from 2-D radiographic images. IEEE Trans Biomed Eng. 2003;50:989–998. doi: 10.1109/TBME.2003.814525. [DOI] [PubMed] [Google Scholar]
- 10.Ferguson AB. The study and treatment of scoliosis. South Med J. 1930;23:116–120. [Google Scholar]
- 11.Goldstein LA. The surgical management of scoliosis. Clin Orthop. 1964;35:95–115. [PubMed] [Google Scholar]
- 12.Goldstein LA. The surgical management of scoliosis. Clin Orthop. 1971;77:32–56. [PubMed] [Google Scholar]
- 13.Halm H, Niemeyer T, Link T. Liljenqvist. Eur Spine J. 2000;9:191–197. doi: 10.1007/s005860000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamill CL, Lenke LG, Bridwell KH, Chapman MP, Blanke K, Baldus C. The use of pedicle screw fixation to improve correction in the lumbar spine of patients with idiopathic scoliosis. Is it warranted? Spine. 1996;21:1241–1249. doi: 10.1097/00007632-199605150-00020. [DOI] [PubMed] [Google Scholar]
- 15.Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. Am J Orthop. 1962;44-A:591–610. [PubMed] [Google Scholar]
- 16.Harrington PR. Technical details in relation to the successful use of instrumentation in scoliosis. Orthop Clin North Am. 1972;3:49–67. [PubMed] [Google Scholar]
- 17.Herring JA. Tachdjian’s pediatric orthopedics. Philadelphia: Saunders; 2002. pp. 234–241. [Google Scholar]
- 18.King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:1302–1313. [PubMed] [Google Scholar]
- 19.Knapp DR, Jr, Price CT, Jones ET, Coonrad RW, Flynn JC. Choosing fusion levels in progressive thoracic idiopathic scoliosis. Spine. 1992;17:1159–1165. doi: 10.1097/00007632-199210000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Lee CK, Denis F, Winter RB, Lonstein JE. Analysis of the upper thoracic curve in surgically treated idiopathic scoliosis. A new concept of the double thoracic curve pattern. Spine. 1993;18:1599–1608. doi: 10.1097/00007632-199309000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Lenke LG, Betz RR, Bridwell KH, Clements DH, Harms J, Lowe TG, Shufflebarger HL. Intraobserver and interobserver reliability of the classification of thoracic adolescent idiopathic scoliosis. J Bone Joint Surg Am. 1998;80:1097–1106. doi: 10.2106/00004623-199808000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Lenke LG, Betz RR, Haher TR, Lapp MA, Merola AA, Harms J, Shufflebarger HL. Multisurgeon assessment of surgical decision-making in adolescent idiopathic scoliosis: curve classification, operative approach, and fusion levels. Spine. 2001;26:2347–2353. doi: 10.1097/00007632-200111010-00011. [DOI] [PubMed] [Google Scholar]
- 23.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83-A:1169–1181. [PubMed] [Google Scholar]
- 24.Lenke LG, Bridwell KH, Baldus C, Blanke K. Preventing decompensation in King type II curves treated with Cotrel-Dubousset instrumentation. Strict guidelines for selective thoracic fusion. Spine. 1992;17:S274–281. doi: 10.1097/00007632-199208001-00011. [DOI] [PubMed] [Google Scholar]
- 25.Liljenqvist U, Lepsien U, Hackenberg L, Niemeyer T, Halm H. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J. 2002;11:336–343. doi: 10.1007/s00586-002-0415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liljenqvist UR, Allkemper T, Hackenberg L, Link TM, Steinbeck J, Halm HF. Analysis of vertebral morphology in idiopathic scoliosis with use of magnetic resonance imaging and multiplanar reconstruction. J Bone Joint Surg Am. 2002;84-A:359–368. doi: 10.2106/00004623-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 28.Moe JH. Methods of correction and surgical techniques in scoliosis. Orthop Clin North Am. 1972;3:17–48. [PubMed] [Google Scholar]
- 29.Nash CL, Jr, Moe JH. A study of vertebral rotation. J Bone Joint Surg Am. 1969;51:223–229. [PubMed] [Google Scholar]
- 30.Nowakowski A, Labaziewicz L, Skrzypek H, Tobjasz F. [Classification of the adolescent idiopathic scoliosis and preoperative strategy] Chir Narzadow Ruchu Ortop Pol. 1999;64:319–325. [PubMed] [Google Scholar]
- 31.Osebold WR, Yamamoto SK, Hurley JH. The variability of response of scoliotic spines to segmental spinal instrumentation. Spine. 1992;17:1174–1179. doi: 10.1097/00007632-199210000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Papin P, Arlet V, Marchesi D, Rosenblatt B, Aebi M (1999) Unusual presentation of spinal cord compression related to misplaced pedicle screws in thoracic scoliosis. Eur Spine J 8:156–9; discussion 160 [DOI] [PMC free article] [PubMed]
- 33.Puno An RM KC, Puno RL, Jacob A, Chung SS. Treatment recommendations for idiopathic scoliosis: an assessment of the Lenke classification. Spine. 2003;28:2102–2115. doi: 10.1097/01.BRS.0000088480.08179.35. [DOI] [PubMed] [Google Scholar]
- 34.Richards BS, Birch JG, Herring JA, Johnston CE, Roach JW. Frontal plane and sagittal plane balance following Cotrel-Dubousset instrumentation for idiopathic scoliosis. Spine. 1989;14:733–737. doi: 10.1097/00007632-198907000-00015. [DOI] [PubMed] [Google Scholar]
- 35.Richards BS, Sucato DJ, Konigsberg DE, Ouellet JA. Comparison of reliability between the Lenke and King classification systems for adolescent idiopathic scoliosis using radiographs that were not premeasured. Spine. 2003;28:1148–1156. doi: 10.1097/00007632-200306010-00012. [DOI] [PubMed] [Google Scholar]
- 36.Roye DP, Jr, Farcy JP, Rickert JB, Godfried D. Results of spinal instrumentation of adolescent idiopathic scoliosis by King type. Spine. 1992;17:S270–273. doi: 10.1097/00007632-199208001-00010. [DOI] [PubMed] [Google Scholar]
- 37.Shufflebarger HL, Clark CE. Fusion levels and hook patterns in thoracic scoliosis with Cotrel-Dubousset instrumentation. Spine. 1990;15:916–920. doi: 10.1097/00007632-199009000-00015. [DOI] [PubMed] [Google Scholar]
- 38.Stokes IA, Bigalow LC, Moreland MS (1986) Measurement of axial rotation of vertebrae in scoliosis [published erratum appears in Spine 1991 May;16(5):599–600] [see comments]. Spine 11(3), 213–8. 1986 [DOI] [PubMed]
- 39.Suk SI, Kim WJ, Kim JH, Lee SM. Restoration of thoracic kyphosis in the hypokyphotic spine: a comparison between multiple-hook and segmental pedicle screw fixation in adolescent idiopathic scoliosis. J Spinal Disord. 1999;12:489–495. doi: 10.1097/00002517-199912000-00008. [DOI] [PubMed] [Google Scholar]
- 40.Suk SI, Kim WJ, Lee CS, Lee SM, Kim JH, Chung ER, Lee JH. Indications of proximal thoracic curve fusion in thoracic adolescent idiopathic scoliosis: recognition and treatment of double thoracic curve pattern in adolescent idiopathic scoliosis treated with segmental instrumentation. Spine. 2000;25:2342–2349. doi: 10.1097/00007632-200009150-00012. [DOI] [PubMed] [Google Scholar]
- 41.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. doi: 10.1097/00007632-199506000-00012. [DOI] [PubMed] [Google Scholar]
- 42.Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994;18:341–346. doi: 10.1007/BF00187077. [DOI] [PubMed] [Google Scholar]
- 43.Wimmer C, Gluch H, Nogler M, Walochnik N. Treatment of idiopathic scoliosis with CD-instrumentation: lumbar pedicle screws versus laminar hooks in 66 patients. Acta Orthop Scand. 2001;72:615–620. doi: 10.1080/000164701317269049. [DOI] [PubMed] [Google Scholar]
- 44.Winter RB. The idiopathic double thoracic curve pattern. Its recognition and surgical management. Spine. 1989;14:1287–1292. doi: 10.1097/00007632-198912000-00003. [DOI] [PubMed] [Google Scholar]