Abstract
Low back pain (LBP) has been identified as one of the most costly disorders among the worldwide working population. Sitting has been associated with risk of developing LBP. The purpose of this literature review is to assemble and describe evidence of research on the association between sitting and the presence of LBP. The systematic literature review was restricted to those occupations that require sitting for more than half of working time and where workers have physical co-exposure factors such as whole body vibration (WBV) and/or awkward postures. Twenty-five studies were carefully selected and critically reviewed, and a model was developed to describe the relationships between these factors. Sitting alone was not associated with the risk of developing LBP. However, when the co-exposure factors of WBV and awkward postures were added to the analysis, the risk of LBP increased fourfold. The occupational group that showed the strongest association with LBP was Helicopter Pilots (OR=9.0, 90% CI 4.9–16.4). For all studied occupations, the odds ratio (OR) increased when WBV and/or awkward postures were analyzed as co-exposure factors. WBV while sitting was also independently associated with non-specific LBP and sciatica. Vibration dose, as well as vibration magnitude and duration of exposure, were associated with LBP in all occupations. Exposure duration was associated with LBP to a greater extent than vibration magnitude. However, for the presence of sciatica, this difference was not found. Awkward posture was also independently associated with the presence of LBP and/or sciatica. The risk effect of prolonged sitting increased significantly when the factors of WBV and awkward postures were combined. Sitting by itself does not increase the risk of LBP. However, sitting for more than half a workday, in combination with WBV and/or awkward postures, does increase the likelihood of having LBP and/or sciatica, and it is the combination of those risk factors, which leads to the greatest increase in LBP.
Keywords: Sitting, LBP, Sciatica, Epidemiology, Review
Introduction
Low back pain (LBP) is an important public health problem in all industrialized countries. It remains the leading cause of disability in persons younger than 45 years old and comprises approximately 40% of all compensation claims in the United States [17, 19, 42, 46, 78]. More than one-quarter of the working population is affected by LBP each year [35], with a lifetime prevalence of 60–80% [21, 35] and a large percentage of LBP claims for long durations (more than 90 workdays lost) [55].
Approximately one-third of American workers are in jobs that contribute to an increased risk of developing back disorders, although the causes of lumbar disorders are complex and difficult to identify [57]. This situation is similar in Great Britain, where the average estimated year-prevalence derived from British population surveys is 38% [61, 77].
Because of the potential economic and social benefits to be gained from reducing the magnitude of LBP in industry, many investigations have focused their attention on the factors that lead to injury, particularly on those activities and events associated with the onset of symptoms [67]. The major thrust of research about LBP has been to identify occupational risk factors associated with its presence and occurrence [58].
With the rapid development of modern technology, sitting has now become the most common posture in today’s workplace [38]. Reinecke et al. [66] reports that three-quarters of all workers in industrialized countries have sedentary jobs that require sitting for long periods. For many activities, however, sitting can be a less straining posture than standing [32]. Both postures are commonly used, and have advantages and disadvantages depending on the task to be performed. In this review, “sitting” is discussed in the context of Western standards. Sitting is described as an erect posture in which the head and trunk are vertical, the lower legs are bent at about 90° at the hips and knees, and the feet are firmly placed on the floor [16]. The concept of sitting is very different in non-Western societies. In India and Southeast Asia, for example, it is still common to see workers sitting cross-legged on the ground, squatting (knees bent severely, the thighs close to the trunk, and weight concentrated on the heels), or kneeling [32]. Although common, these variations of sitting are not discussed in this review.
The existence of the relationship between workplace factors and the occurrence of LBP has long been recognized [1, 3, 13, 29]. Among the occupational exposures identified, sitting is commonly cited as a risk factor in the literature, in addition to heavy physical work, heavy or frequent lifting, non-neutral postures (i.e., trunk rotation, forward bending), pushing and pulling, and exposure to whole body vibration (WBV) (i.e., motor vehicle driving) [12, 20, 25, 31, 35, 37, 39, 47, 51, 53, 76, 79].
Laboratory studies have focused on biomechanical hypotheses to explain the association between sitting and LBP [45, 47, 56, 74, 80]. The literature on this subject is extensive, but the evidence is somewhat contradictory. It has been shown that intradiscal pressure is increased in the sitting posture [56]. In a more recent investigation, Wilke et al. [80] reevaluated the intradiscal pressure in sitting and found that, in fact, it can be lower in sitting than in erect standing. Another hypothesis is that prolonged static sitting postures may have a negative effect on the nutrition of the intervertebral disc [47]. Thus, a constantly changing position may promote the flow of fluid (nutrition) to the disc [75].
The purpose of this paper is to review the more recent literature that examines the association between sitting and the report of LBP among working populations. This review also intends to identify if there is an interaction between occupational LBP/sciatica and sitting in combination with WBV and/or awkward postures. The importance of this association cannot be underestimated. Understanding the risk factors for LBP and sciatica can lead to prevention programs that have the potential to mitigate the high prevalence rates of occupational LBP. Although other factors (i.e., physiological and psychosocial) may also be important, they are not the focus of this paper.
For this review, sitting is defined as a sustained upright trunk posture with limited possibilities to change posture or position [16, 30]. LBP is represented here by reported or examined ache, pain, stiffness, or discomfort in the lumbar spine [9]. Sciatic pain is considered a reported or examined radiating pain extending below the knee in one or both legs [9]. Workers in occupations who performed tasks while sitting may also be exposed to WBV and/or awkward posture, and these exposures are independently analyzed in the literature. Awkward posture represents a non-neutral trunk posture (i.e., bending forward and/or twisting of the trunk) [10, 12, 25, 30, 51]. “Postural load” [7] and “unfavorable posture” [49] are terms used in the literature that refer to awkward posture. WBV is present when the body receives continuous vibration transmitted from the seat over a period of time [7, 9].
This systematic review seeks to examine the association between the presence and/or occurrence of LBP and sciatica among occupational groups in which the seated posture is the major physical requirement for the work. The following questions were considered: (1) Is there evidence in the recent epidemiological literature for an association between occupational groups exposed to sitting and reported LBP?, (2) Is there evidence in the recent epidemiological literature of an association between exposure to WBV while sitting and reported LBP?, (3) Is there evidence in the recent epidemiological literature for an association between awkward posture while sitting and reported LBP?, and (4) Is there evidence in the recent epidemiological literature for an association between the combined effect (both WBV and awkward posture) while sitting and reported LBP?
Methodology
Using MEDLINE (US National Library of Medicine), HEALTHSTAR, and CINAHL as the principal databases, studies published between 1990 and May of 2004 were retrieved. The primary keywords used were LBP and sitting. The secondary keywords used were WBV, static posture, occupational back pain, awkward posture, sedentary occupation, trunk twisting, and sciatica. Several specific occupations such as different forms of professional driving that require a combination of sitting and WBV or awkward postures were also reviewed. Reference lists of studies retrieved were carefully screened in order to locate additional papers. Articles written only in English were included, and a total of 155 studies were identified.
Those studies that described the presence and/or occurrence of reported or examined LBP in occupational groups in which the major physical requirement is sitting (calculated as sitting for more than half of work-time) were included. Job titles were also used as the selection criteria to identify those occupations in which the worker is required to sit for a major part of the day. If there was doubt about the amount of sitting required for a specific occupation, ONET, the US Department of Labor’s Occupational Information Network, was consulted [59]. Forty-one publications met this criterion and were reviewed using a Critical Appraisal form [65].
Quality criteria were established for inclusion and carefully analyzed by the authors. The criteria were: a clear definition of LBP and/or sciatica; a control group (if applicable) that is well described and relevant (consisting of similar or internal groups subjected to less exposure to sitting); a response rate reported if a questionnaire was used to gather data; exposure described or at least graded; and a statistical measure of association (OR or Risk Ratio).
After applying the evaluation criteria, 17 articles were excluded from the final review. Of the 17 articles, 5 articles were experimental studies [27, 36, 38, 50, 66] and 12 articles were observational studies [11, 12, 26, 28, 33–35, 47, 52, 63, 70, 73]. The main exclusion criteria pertained to the lack of a statistical measure of association. Ten of the 12 observational studies were excluded for this reason [11, 26, 28, 33–35, 47, 52, 63, 70]. Two epidemiological studies were excluded, one because of small sample size [12] and one because the focus was placed on psychosocial factors rather than on physical work-related factors while sitting [73].
The remaining 24 publications were critically reviewed to measure the possible associations between sitting at work and reported LBP or sciatica [4–7, 9, 10, 14, 15, 20, 22, 24, 31, 37–39, 41, 43, 44, 48, 49, 53, 62, 69, 76].
Results
LBP
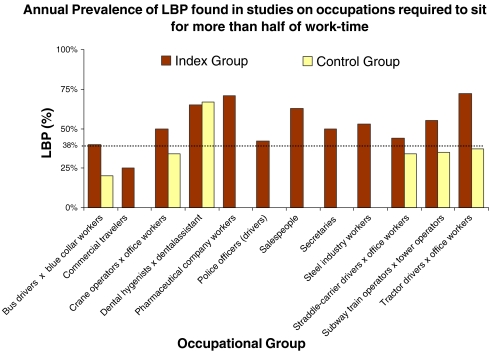
Figure 1 depicts the results of studies undertaken between 1990 and 2004 that measured the annual prevalence rates of LBP among occupational groups that are required to sit for more than half of their work-time. The estimated annual prevalence rate of LBP in the general population of Europe was used for comparison [61, 77]. European population data was chosen as a comparison group because 72% of the studies reviewed were conducted in Europe. The average age of the populations listed in Fig. 1 was 30–50 years old and most of the workers were male. In general, the figure shows a higher annual prevalence rate for those occupational groups that spend more than half their working day in a sitting position. Commercial travelers [62] and office workers (in control groups) [7, 14] showed a lower prevalence rate (25%) than the average of annual prevalence rate (38%) found in the compared European general population [61, 77]. Tractor drivers reported the highest annual prevalence rate, with almost two times the annual prevalence rate (72%) of the general population [14].
Fig. 1.
Annual prevalence of LBP found in studies of occupations where sitting is required for more than half of work-time
Twenty-four publications were selected according to specific criteria for a more detailed review of the association between presence and/or occurrence of LBP and occupational groups in which sitting is the major physical requirement. Seventeen of these studies were conducted in Europe, [4–7, 9, 10, 14, 20, 22, 43, 44, 48, 49, 54, 62, 72, 76], one was conducted in Asia [15], one was conducted in Israel, [69] three were conducted in Canada, [31, 39, 41] and two were conducted in the US [24, 37]. The studies yielded different types of prevalence estimates (i.e., point, period, lifetime); however, in the majority of studies, the OR for annual prevalence was provided. For the papers that reported a significant association but did not report an OR, if enough information was available, an OR was calculated so that all papers could be compared using the same measure of association. In general, the definition for LBP was consistent with the definition for sciatica. Most authors described how data had been collected and attempted to categorize participants as exposed/non-exposed, or even to quantify their exposure. It should be noted that for all the studies analyzed, the parameter that indicates the greatest exposure (magnitude or duration) was selected by the authors for each of the factors described. For instance, Bovenzi and Betta [7] provided the OR for three parameters of the exposure ‘vibration duration’ such as 5–15, 16–25, and greater than 25 years. The later parameter (>25 years) was selected for this review. LBP was self-reported in all the publications reviewed, with the exception of two that used a medical examination [22, 69].
Table 1 shows the OR for LBP in the occupational groups in which sitting is the major physical requirement (accounts for more than half of work-time). The occupational group that demonstrated the strongest association between sitting and reported LBP was helicopter pilots [4] (OR=9.0, 90% CI 4.9–16.4), compared with a control group of non-flying officers. Crane operators also presented a high OR [14]; they had 3.29 times (95% CI 1.52–7.12) the risk of reporting LBP than office workers. Bus drivers were the subject of two separate studies. Although the OR in both studies was not equal, both studies showed a positive association between sitting and reported LBP (≥1.5) [9, 44]. In fact, Bovenzi and Zadini [9] reported an OR of 2.57 (95% CI 1.52–4.35) while Magnusson et al. [44] reported an OR of 1.79 (95% CI 1.16–2.75).
Table 1.
Association between the presence of LBP and occupations requiring sitting for >1/2 of working time
| Study | Study design | Study population | Outcome | Exposure | Risk indicator OR (95% CI or P value) | Adjusted for |
|---|---|---|---|---|---|---|
| Bongers et al. [4] | Cross-sectional cohort | Helicopter pilots (n=133) × Non-flying officers (n=228) | LBP | Pilot a helicopter | OR=9.0 (4.9–16.4)a | Age, height, weight, climate, bending forward, twisted posture and mental stress |
| Boshuizen et al. [6] | Cross-sectional cohort | Truck and tractor drivers (n=196) × Blue-collar workers (n=107) | LBP | Drive a tractor or a truck | OR=1.39 (0.71–2.7)a | Age |
| Bovenzi and Betta [7] | Cross-sectional cohort | Tractor drivers (n=1,155) × Office workers (n=220) | LBP (previous 12 months) | Drive a tractor | OR=2.39 (1.57–3.66) | Age, BMI, education, sport activity, car driving, marital status, mental stress, climate, history of trauma and postural load |
| Bovenzi and Zadini [9] | Cross-sectional cohort | Bus drivers (n=234) × Maintenance workers (n=125) | LBP (previous 12 months) | Drive a bus | OR=2.57 (1.52–4.35) | Age, awkward posture, BMI, mental load, education, smoking, sport activity and previous jobs at risk for LBP |
| Burdorf et al. [14] | Cross-sectional | Crane operators (n=94) and Straddle-carrier drivers (n=95) × office workers (n=86) | LBP (previous 12 months) | Crane operator | OR=3.29 (1.52–7.12) | Age, individual characteristics, work-related risk factors in previous jobs and work-related risk factors pertaining to the current job |
| Straddle-carrier driver | OR=2.51 (1.17–5.38) | |||||
| Heliövaara et al. [22] | Cross-sectional cohort | Professional drivers (n=310) × Non-professional drivers (n=5,363) | Unspecified LB syndromeb | Occupational vehicle driving | OR=1.83 (1.12–3.0)a | Sex, age, body height, BMI, previous trauma, physical and mental stress, smoking, alcohol consumption, no. of births (women) |
| Liss et al. [41] | Cross-sectional | Dental hygienists n=950) × Dental assistants (n=108) | LBP (previous 12 months) | Work as a dental hygienist | OR=0.9 (0.6–1.4) | Age |
| MacFarlane et al. [43] | Longitudinal cohort (population-based) | Workforce population of Northwest England (n=1,412) | Occurrence of LBP (1 year follow-up) | Drive a car (> 4 h/day) | OR=1.1 (0.5–2.7) | Age |
| Magnusson et al. [44] | Cross-sectional cohort | Bus drivers (n=111) Truck drivers (n=117) × Sedentary workers (n=137) | LBP (previous 12 months) | Drive a bus or truck | OR=1.79 (1.16–2.75) | None |
| Masset and Malchaire [49] | Cross- sectional | Steel industry workers (n=618) | LBP (previous 12 months) | Work in a seated position | OR=1.46 (P=0.09) | Vehicle driving, efforts with the shoulders |
| Moen and Bjorvatn [54] | Cross-sectional | Dentists (n=96) × Dental auxiliaries (n=83) and Office workers (n=25) | LBP (employment period) | Being a dentist | OR=1.0 (0.5–1.9) | None |
| Rotgoltz et al. [69] | Cross-sectional | Pharmaceutical factory workers (n=208) | LBP (previous 12 months) | Work in sitting position (packing, laboratories and offices) | OR=1.97 (1.37–2.81) | Age and sex |
| Pietri et al. [62] | Longitudinal cohort | Commercial travelers (n=1,719) | LBP (previous 12 months) | Drive a car (<5 h/day) | OR=2.1 (1.3–3.4) | None |
| 1st episode of LBP (in 1 year follow-up) | Drive a car (>5 h/day) | OR=3.7 (0.9–14.0) | None | |||
| Hartvigsen et al. [20] | Twin-control | Danish Twin Registry | LBP | Sitting only | 0.95 (0.8–1.14) | None |
| Vingard et al. [76] | Case-control | Those living in the municipality of Norrtalje, Sweden and who sought care treatment for LBP | LBP | Sitting > 5 h/day | RR men: 1.1 (0.7–1.7); women: 0.7 (0.4–1.1) | Age, gender |
| Kopec et al. [31] | Cohort | Canadian National Population Health Survey | LBP | Sitting only | 1 (referent) | Adjusted sample to match the Canadian population |
| Miyamoto et al. [53] | Cross-sectional | Truck Drivers from a large chemical industry company in Toyko | LBP | Sitting only | 1.3 (0.6–2.7) | Age, height, weight, BMI, working period |
| Levangie [37] | Case-control | Patients referred to physical therapists for treatment of LBP (n=150) × patients being treated by phys therapists for an unrelated problem (n=138) | LBP | Sitting | <4 h-referent | Geographic distribution, socioeconomic group, health care access, willingness to seek medical attention |
| 4–6 h: 1.54 (0.81–2.91) | ||||||
| 6–8 h: 0.71 (0.37–1.35) | ||||||
| >9 h: 1.42 (0.73–2.78) | ||||||
| Liira et al. [39] | Cross-sectional | All residents outside institutions and Indian reservations in Ontario, Canada with White Collar Occupations | LBP | Sitting | 1.08 (0.71–1.63) | Sex, age, smoking |
a90% Confidence interval
b“Unspecified low back syndrome” was defined by the authors as low back diagnoses other than sciatica (i.e., spondylolisthesis, spondyloarthosis, chronic muscular pain and others)
However, results for the association between sitting and LBP in professional drivers (automobile, bus, tractor or truck drivers) are somewhat controversial. Four out of six studies showed a moderate positive association (average OR=2.1) between sitting and LBP [7, 9, 22, 44]. The remaining two studies found an almost null association between professional driving and LBP [6, 53].
Nine studies showed a non-significant association (OR=≤ 1.4 and CI including 1) between sitting and LBP [20, 31, 37–39, 41, 43, 53, 76]. For instance, when dental hygienists were compared with a control group of dental assistants, a small protective effect was evident (OR=0.9, 95% CI 0.6–1.4) [41], and when dentists were compared with office workers, no association was found (OR=1, 95% CI 0.5–1.9) [38].
Two studies [43, 62] evaluated the effect of extended daily periods of driving (>4 h/day and >5 h/day). Each study found OR > 1 (0.5–2.7) and OR=3.7 (0.9–14), respectively; however, the P value was not significant in any of the studies (P>0.05). Working in a seated position among steel industry workers produced a slight increase in the OR of LBP (OR=1.46, P=0.09); however, the OR was not significant [49]. In the Danish Twin Registry, sitting has a slight protective effect (OR=0.95, 95% CI 0.8–1.14). In fact, previous studies conducted on populations in Sweden and Canada also found that sitting did not increase the odds of LBP [31, 39, 76].
Overall, the average OR for LBP in the occupations presented in Table 1 was 1.99. However, almost half the OR’s factored in were not significant, weakening the supposed effect of sitting [6, 20, 36, 37, 39, 41, 43, 53, 62, 76].
Currently, the evidence is controversial in finding an association between sitting and occupational LBP. In fact, the more recent studies (1995–2004) almost unanimously found no association between sitting alone and LBP [20, 31, 37–39, 41, 43, 53, 76].
Table 2 summarizes the studies that examine the association between the presence and/or occurrence of LBP and exposure to WBV among occupations that require sitting for more than half of working time. All studies used vibration dose as the exposure measured; however, some studies also provided the OR for vibration magnitude [5, 7, 9] and/or duration [4, 5, 7, 9]. To calculate vibration dose, the studies used the formula Σ a2i. tI, where ai is the estimated vector sum of accelerations measured on the vehicle and tI is the time in years (or hours in the case of helicopter pilots). In all studies, vibration measurements on the vehicles were performed according to the recommendations of the international standard ISO 2631-1 [23]. Seven of the nine studies included in Table 2 showed a positive association between LBP and exposure to WBV [4–7, 9, 15, 39]. The occupational group that shows the strongest association between LBP and vibration dose is helicopter pilots, with OR=6.6 (90% CI 2.9–15.1). It is noteworthy that this was the only occupational group that used total hours as a measurement for duration of exposure because pilots systematically document their flight hours in a flight log. Both the magnitude and the duration were positively associated with LBP. However, duration had a stronger impact on increasing the risk of LBP in each of the studies (OR>2.5) [5, 7, 9]. One study, conducted by Liira [39], showed a small association between the presence of LBP and the duration of the WBV (OR=1.71). In Chen’s study, when the analysis of the dose–response of WBV was conducted, the results showed an increase in the risk of LBP of 3.7 as the daily vibration dose was increased [15].
Table 2.
Association between the presence of LBP and exposure to whole body vibration among occupations that require sitting for >1/2 of working time
| Study | Study design | Study group | Control group | Outcome | Vibration dose, magnitude and/or duration | Risk indicator OR (95% CI) | Confounders adjusted for |
|---|---|---|---|---|---|---|---|
| Bongers et al. [4] | Cross-sectional cohort | Helicopter pilots (n=133) | Non-flying air force officers (n=228) | LBP | Duration: Total flight time/>4,000 h | OR=13.4 (5.7–32.0)a | Age, height, weight, climate, bending forward, twisted posture and mental stress |
| Dose: >800–1,200 m2 h/s4 | OR=6.6 (2.9–15.1)a | ||||||
| Boshuizen et al. [5] | Longitudinal cohort | Tractor drivers (n=450) | Agricultural workers (n=110) | LBP | Magnitude: >0.7 m/s2 | OR=2.10 (1.07–4.1)a | Duration of exposure, age, height, weight, smoking, twisting, lifting, mental stress, employing company |
| Duration:>10 years | OR=3.6 (1.21–11)a | ||||||
| Dose: >5 year m2/s4 | OR=2.8 (1.64–5.0)a | ||||||
| Boshuizen et al. [6] | Cross-sectional cohort | Truck and tractor drivers (n=196) | Blue-collar workers (n=107) | LBP | Dose: 15 year m2/s4 | OR=1.96 (1.03–3.7)a | Age, mental stress, no. of years lifting + twisting, no. of times/day lifting + twisting, body height, smoking, prolonged sitting and time spent looking backward |
| Bovenzi and Zadini [9] | Cross-sectional cohort | Bus drivers (n=234) | Maintenance workers (n=125) | LBP (previous 12 months) | Magnitude: >0.60 m/s2 | OR=1.76 (0.86–3.58) | Age, awkward posture, BMI, mental load, education, smoking, sport activity and previous jobs at risk for LBP |
| Duration: >15 years | OR=2.90 (1.54–5.46) | ||||||
| Dose: >4.5 years m2/s4 | OR=2.63 (1.35–5.12) | ||||||
| Bovenzi and Betta [7] | Cross-sectional cohort | Tractor drivers (n=1,155) | Office workers (n=220) | LBP (previous 12 months) | Magnitude: >1.25 m/s2 | OR=2.29 (1.43–3.68) | Age, BMI, education, sport activity, car driving, marital status, mental stress, climate, history of trauma and postural load |
| Duration: >25 years | OR=2.74 (1.69–4.45) | ||||||
| Dose: >30 years m2/s4 | OR=2.36 (1.48–3.74) | ||||||
| Magnusson et al. [44] | Cross-sectional cohort | Bus drivers (n=111) | Sedentary workers (n=137) | LBP (previous 12 months) | Bus drivers: Dose: 48.18 years m2/s4 |
OR=2.0 (0.98–4.1) | None |
| Truck drivers (n=117) | |||||||
| Truck drivers: Dose: 79.97 years m2/s4 | |||||||
| Chen et al. [15] | Cross-sectional | Taxi drivers | N/A-general population | LBP | Increment of daily vibration exposure by each m2/s4 h | 3.7 (1.1–12.2) | Age, body mass index, professional seniority, registration type, seat inclination, vehicle engine size, use of lumbar support |
| Liira et al. [39] | Cross-sectional | All Residents outside institutions and Indian reservations in Ontario, Canada with White Collar Occupations that were exposed to WBV | Those from the same population who were not exposed to WBV | LBP | Duration: always or often (at least several hours per day) | 1.71 (1.09–2.67) | Sex, age, smoking |
a90% Confidence interval
Table 3 summarizes the studies that examine the association between the presence and/or occurrence of LBP and exposure to awkward posture among occupations that require sitting for more than half of work-time. Four studies [7, 9, 10, 48] were included in Table 3. Bovenzi and Zadini [9] showed that the reporting of LBP increased when exposure to awkward postures increased (OR=2.29, 95% CI 1.22–4.29) for bus drivers when compared with maintenance workers. With exposure to frequent awkward postures, Bovenzi and Betta [7] found that tractor drivers are almost five times more likely to report LBP than office workers. Bridger [10] showed that “sitting forward” (as opposed to sitting up straight) resulted in a large increase in LBP (OR=6.02), and that further increments resulted in smaller increases in the OR (3.15) of LBP. Massaccesi [48] showed that exposure to awkward posture (trunk flexed, bent, and twisted) in drivers of Road Washing Vehicles increased the OR of LBP to 10.59.
Table 3.
Association between the presence of LBP and awkward posture among occupations that require sitting for >1/2 of working time
| Study | Study design | Study population | Outcome | Exposure | Risk indicator OR (95%CI) | Adjusted for |
|---|---|---|---|---|---|---|
| Bovenzi and Zadini [9] | Cross-sectional cohort | Bus drivers (n=234) × Maintenance workers (n=125) | LBP (previous 12 months) | Awkward postures | OR=2.29 (1.22–4.29) | None |
| Bovenzi and Betta [7] | Cross-sectional cohort | Tractor drivers (n=1,155) × Office workers (n=220) | LBP (12 month prevalence) | Awkward posture | OR=4.56 (2.59–8.03) | Age, BMI, education, sport activity, car driving, marital status, mental stress, climatic conditions, back trauma and total vibration dose |
| Bridger et al. [10] | Cross-sectional | Navy helicopter pilots | LBP | For VFF, slightly forward posture vs. sitting up straight | 6.02 (P<0.01)a | None (but there were no significant differences based on other variables) |
| For IF, sitting noticeably forward vs. sitting slightly forward | 3.15 (P<0.05)a | |||||
| Massaccesi et al. [48] | Cross-sectional | Drivers of road washing vehicles (sitting in an awkward posture) (n=38) × Drivers of rubbish collection vehicles (sitting in a standard posture) (n=39) | LBP | Awkward posture | 10.59a | None |
aOR was not reported in the paper, but enough information was given to calculate the OR
As indicated in Table 4, only one study measured associations for reported LBP and for the combined effects of exposure to WBV and awkward postures. This study was done by Bovenzi and Betta, [7] who also looked at agricultural tractor drivers exposed to WBV and the association of postural stress with the occurrence of chronic LBP. The tractor drivers were 4.56 times (95% CI 2.59–8.03) more likely to report LBP compared with the control group. Bovenzi and Betta [7] categorized postural stress by rating the workers’ perception of the frequency and duration of each posture. They calculated the frequency using a five-item index scale assigning a value from 0 (never) to 4 (very often). Following this step, a mean value was used to determine the duration by calculating the postural indices during a typical workday. Finally, they categorized the average postural load into one of the four grades described on the table (mild = 0–0.99, moderate = 1–1.99, hard = 2–2.99, and very hard = 3–4). The results of this study show that after combining the exposure factors, the risk of the occurrence of chronic LBP increases as vibration dose and postural load increase. In fact, the risk for chronic back pain increases more than threefold compared with the unexposed group (office workers).
Table 4.
Association between the combined effects of vibration dose (years m2/s4)/postural load and the occurrence of chronic LBP
| Total vibration dose (years m2/s4) | Postural load (grades)a | |||
|---|---|---|---|---|
| 1 (Mild) | 2 (Moderate) | 3 (Hard) | 4 (Very hard) | |
| 5 | OR=1.29 | OR=1.79 | OR=2.50 | OR=3.48 |
| 10 | OR=1.41 | OR=1.96 | OR=2.73 | OR=3.79 |
| 20 | OR=1.55 | OR=2.15 | OR=2.99 | OR=4.16 |
| 30 | OR=1.63 | OR=2.27 | OR=3.16 | OR=4.39 |
| 40 | OR=1.70 | OR=2.36 | OR=3.29 | OR=4.58 |
Modified from Bovenzi and Betta [7]. Low-back disorders in agricultural tractor drivers exposed to whole-body vibration and postural stress
aOR adjusted for age, BMI, education, sport activity, car driving, marital status, mental stress, climatic conditions and back trauma
Sciatica
A parallel literature review was conducted to find the association between sitting for more than half of the work-time and the presence of sciatica. Using the inclusion criteria mentioned earlier, five studies were included [4, 6, 7, 9, 24]. These studies collected information about the prevalence of sciatica using questionnaires that asked about the presence of back pain with radiation to a leg [24]. Table 5 describes the prevalence of sciatica in occupations where sitting is the major physical requirement with co-exposure factors such as WBV and awkward postures. The prevalence rates for reported sciatica in all the occupations analyzed were two to three times (OR ranging from 1.16 to 3.9, 95% CI 0.62–8.71) higher than their correspondent control groups. However, the prevalence of LBP as mentioned above was much higher for all occupations compared with the prevalence of sciatica pain, except for crane operators [4] (50% prevalence of LBP versus a 61% prevalence of sciatica pain).
Table 5.
Sciatica prevalence in occupations that require sitting for >1/2 of working time
Table 6 shows the association between the presence of sciatica pain and sitting for more than half of working time. The occupational groups that presented the strongest association of sitting and reported LBP were subway train operators [24] and tractor drivers [7], with an OR of 3.9 (95% CI 1.7–8.6) and an OR of 3.9 (95% CI 1.75–8.71), respectively. Taking into account that the occupational groups presented in Table 6 were exposed to other factors such as WBV and awkward postures, these groups will be analyzed independently below.
Table 6.
Association between the presence of sciatica pain and occupations that require sitting for >1/2 of working time
| Study | Study design | Study population | Outcome | Exposure | Risk indicator (95% CI) | Adjusted for |
|---|---|---|---|---|---|---|
| Bongers et al. [4] | Cross-sectional cohort | Helicopters pilots (n=133) × Non-flying officers (n=228) | Sciatica | Pilot a helicopter | OR=3.3 (4.9–16.4)a | Age, height, weight, climate, bending forward, twisted posture and mental stress |
| Boshuizen et al. [6] | Cross-sectional cohort | Truck and tractor drivers (n=196) × Blue-collar workers (n=107) | Sciatica | Drive a tractor or a truck | OR=1.16 (0.62–2.2)a | Age |
| Bovenzi et al. [7] | Cross-sectional cohort | Tractor drivers (n=1,155) × Office workers (n=220) | Sciatica | Drive a tractor | OR=3.9 (1.75–8.71) | Age, BMI, education, sport activity, car driving, marital status, mental stress, climate, history of trauma and postural load |
| Bovenzi and Zadini [9] | Cross-sectional cohort | Bus drivers (n=234) × Maintenance workers (n=125) | Sciatica (previous 12 months) | Drive a bus | OR=2.57 (1.52–4.35) | Age, awkward posture, BMI, mental load, education, smoking, sport activity and previous jobs at risk for LBP |
| Johanning [24] | Cross-sectional | Subway train operators (n=492) × Tower operators (n=92) | Sciatica (previous 12 months) | Operate a subway train | OR=3.9 (1.7–8.6) | Age, gender, job title and employment duration |
a90% Confidence interval
Table 7 shows the association between vibration magnitude, duration of vibration exposure, and total vibration dose while sitting with sciatica pain. An overall positive association was found between sciatica pain and WBV when the OR was greater than or equal to 1.5 (OR≥1.5). There was a significant trend of increased reported presence of sciatica with increased vibration dose expressed as a variable derived from the duration of exposure and the magnitude of the exposure.
Table 7.
Association between the presence of sciatica pain and exposure to whole body vibration among occupations that require sitting for >1/2 of working time
| Study | Study design | Study group | Control group | Outcome | Vibration dose, magnitude and/or duration | Risk indicator OR (95% CI) | Confounders adjusted for |
|---|---|---|---|---|---|---|---|
| Bongers et al. [4] | Cross-sectional cohort | Helicopter pilots (n=133) | Non-flying air force officers (n=228) | Sciatica | Duration: Total flight time/> 4,000 h | OR=3.3 (1.0–10.4)a | Age, height, weight, climate, bending forward, twisted posture and mental stress |
| Dose: >1,200 m2 h/s4 | OR=5.6 (1.5–21.2)a | ||||||
| Boshuizen et al. [5] | Longitudinal cohort | Tractor drivers (n=450) | Agricultural workers (n=110) | Sciatica | Magnitude: >0.7 m/s2 | OR=1.60 (0.71–3.6)a | Duration of exposure, age, height, weight, smoking, twisting, lifting, mental stress, employing company |
| Duration: > 10 years | OR=1.42 (0.40–5.1)a | ||||||
| Dose: > 5 year m2/s4 | OR=1.59 (0.84–3.0)a | ||||||
| Bovenzi and Zadini [9] | Cross-sectional cohort | Bus drivers (n=234) | Maintenance workers (n=125) | Sciatica (previous 12 months) | Magnitude: >0.60 m/s2 | OR=2.26 (1.4–4.49) | Age, awkward posture, BMI, mental load, education, smoking, sport activity and previous jobs at risk for LBP |
| Duration: >15 years | OR=2.06 (0.93–4.53) | ||||||
| Dose: >4.5 years m2/s4 | OR=2.28 (1.19–4.35) | ||||||
| Bovenzi and Betta [7] | Cross-sectional cohort | Tractor drivers (n=1155) | Office workers (n=220) | LBP (previous 12 months) | Magnitude >1.25 m/s2 | OR=3.65 (1.56–8.53) | Age, BMI, education, sport activity, car driving, marital status, mental stress, climate, history of trauma and postural load |
| Duration >25 years | OR=4.46 (1.86–10.7) | ||||||
| Dose >30 years m2/s4 | OR=4.14 (1.18–9.61) |
a90% Confidence interval
Helicopter pilots with a vibration dose greater than 1,200 m2 h/s4 were 5.6 times more likely to have sciatica pain [4]. At the same time, tractor drivers with a vibration dose greater than 30 years m2/s4 were 4.14 times more likely to develop sciatica pain compared with office workers [7]. In contrast with LBP without sciatica, the magnitude of vibration presents a greater risk for having sciatica pain when compared with exposure to long-term vibration [5, 7, 9]. For instance, Bovenzi and Zadini [9] found a greater association between exposure to a vibration magnitude of 0.60 m/s2 and sciatica (OR=2.26, 95% CI 1.4–4.49), than compared with exposure to a vibration duration of more than 15 years (OR=2.06, 95% CI 0.93–4.53).
Only two studies investigated the independent association of awkward postures while sitting with the presence of sciatica (Table 8). Although the OR was higher than 2 in each study, Bovenzi and Betta [7] found that the association was not significant (95% CI 0.68–7.61). In Bovenzi and Zandini [9], the confidence interval was not provided, so it is not included in the calculation. However, it seems that awkward posture at work was associated with the presence of back pain with radiation to a leg to a lesser extent than WBV.
Table 8.
Association between the presence of sciatica pain and exposure to awkward postures among occupations that require sitting for >1/2 of working time
| Study | Study design | Study population | Outcome | Exposure | Risk indicator OR (95%CI) | Adjusted for |
|---|---|---|---|---|---|---|
| Bovenzi and Zadini [9] | Cross-sectional cohort | Bus drivers (n=234) × Maintenance workers (n=125) | Sciatica (previous 12 months) | Awkward postures | OR=2.44 | None |
| Bovenzi and Betta [7] | Cross-sectional cohort | Tractor drivers (n=1,155) × Office workers (n=220) | Sciatica (12 month prevalence) | Awkward postures | OR=2.27 (0.68–7.61) | Age, BMI, education, sport activity, car driving, marital status, mental stress, climatic conditions, back trauma, and total vibration dose |
Discussion
The prevalence rates of LBP have been affecting the economy of industrialized countries in many ways [17, 19]. As was described in Fig. 1, the prevalence rate of reported LBP in those occupations that require the worker to sit for the majority of a working day is significantly higher than the prevalence rate of the general population [61, 77]. Physical factors, psychosocial factors, and individual characteristics contributed to these findings [12, 25, 47, 67, 79], but only the physical factors will be discussed here.
Sitting
Sitting has been a complex topic for researchers of LBP. For many years, the sitting position has been identified as one of the major risk factors for developing LBP [29, 45]. Nachemson and Elfström found that body position affects the magnitude of the loads on the lumbar spine, and that the magnitude of the loads increases markedly when sitting is compared with upright standing and well-supported reclining [39]. This finding created much controversy, and while some subsequent lab studies supported this finding [2, 36], others have found different results [47, 80]. For instance, the conclusions of Wilke et al. reevaluate the assumption that there is an increased presence of higher intradiscal pressure while sitting as opposed to erect standing [80]. In fact, Rohlmann et al. reports that intradiscal pressure is up to 10% less when standing [68]. Some studies have reported OR’s as low as 0.7 for occupations in which the major physical requirement is sitting, indicating that people in these occupations may actually have a lower risk of LBP than in other occupations [37, 76]. However, although the rate of LBP among occupations requiring extended periods of sitting may not be as high as the rate of LBP among more strenuous occupations, Lee et al. reported that this group had the highest hospitalization rate for LBP, indicating that when low back injuries occur among persons in these occupations, these injuries tend to be more severe [35]. Hence, the risk of prolonged sitting in the workplace should not be overlooked. A definitive experimental conclusion about the effect of sitting on LBP has yet to be confirmed. However, the majority of the literature reviewed for this paper has shown that sitting by itself does not imply a markedly increased association with the presence and/or occurrence of reported or examined LBP. In fact, a considerably stronger association was found only when the occupational groups studied were exposed to WBV and/or awkward postures while sitting [4–7, 9, 10, 15, 39, 48]. It is still unknown if other confounders as psychosocial factors may affect the strength of the association between sitting alone and LBP.
Sitting and exposure to WBV
One of the major co-exposure factors for all the occupations analyzed was WBV. There is a clear indication of an increased risk of reported LBP and/or sciatica in occupations with exposure to WBV while sitting, mostly in professional driving occupations [4, 6–9, 12, 15, 22]. Many authors have carefully reviewed the risk effect expressed as increased associations from exposure to WBV and LBP, and have concluded that there is indeed an association between WBV and LBP [8, 18, 40, 60]. However, there is limited evidence regarding a dose–response relationship. There are many confounding factors that interfere with the relationship between LBP and WBV exposure. A worker’s age, duration of exposure, history of LBP, previous exposure, and even posture while being exposed to WBV seems to affect that relationship [4, 6, 9, 60, 71]. Chen et al. [15] found that daily increments of the vibration dose by each m2/s4-hour resulted in an increase in the OR of LBP by 3.7 even after controlling for age and professional seniority, which is almost analogous to duration of exposure [15].
Even though the number of studies that use control and exposure groups to analyze the association between LBP and WBV is limited, there is strong evidence of a major association between WBV while sitting and LBP/sciatica [4–7, 9]. For instance, occupational groups such as helicopter pilots have shown a very high OR (OR=6.6, 90% CI 2.9–15.1) for a vibration-dose exposure greater than 800 m2 h/s4 after adjusting for awkward postures [4]. Only one study [12] did not find an association between sitting plus WBV and LBP; however, the low response rate in that study compromised its quality. Therefore, this does not affect the conclusion that there is a strong relationship between sitting plus WBV and LBP.
In addition to dose, the magnitude and duration of exposure have also been found to be important exposure factors for the presence of occupational LBP and sciatica. The articles reviewed showed that the duration of the exposure had a slightly stronger association with the presence of LBP than did magnitude of vibration [5, 7, 9]. This finding suggests a cumulative effect. As the duration of exposure increases, the risk of LBP increases. Bovenzi and Betta [7] found that prolonged tractor driving and exposure to WBV were the factors most associated with chronic LBP and sick leave. They suggested an excessive accumulated vibration dose effect as the main reason, which is in agreement with the Boshuizen findings [6]. However, in the case of sciatica the pattern is not the same. The duration of the exposure was constantly related to sciatica to a lesser extent than vibration magnitude for all the occupations [5, 9]. The reasons for such results are not clear. Moreover, it is important to understand that in both cases either duration or magnitude were positively associated with the presence of reported LBP or sciatica symptoms. It is also important to take into account that the recommended ISO standards did not reveal any preventive health effect. Even with following ISO recommendations, the levels of vibration magnitude to which most drivers are exposed seems to be higher than the recommended maximum level of exposure, especially when exposed for long periods of time. Many authors argue that these recommendations should be reviewed [4, 6, 7].
Sitting and awkward posture
It has been postulated that sustained awkward seating posture (lordosed or kyphosed, overly arched, or slouched) can result in higher intradiscal pressure and may be injurious to spinal postural health [64]. Therefore, awkward postures while sitting have been described as possible risk factors for the presence of LBP [12, 25, 30, 71, 80]. Many experimental studies [2, 30] have demonstrated that postural changes affect spinal loads. Keyserling et al. [30] used a computer-aided system to investigate trunk posture during work by measuring the time spent in neutral and non-neutral postures. Their results suggested that by controlling non-neutral trunk posture, the risk of developing back pain on industrial jobs can be reduced. Non-industrial occupations such as professional drivers, dentists, and helicopter pilots are also potentially exposed to awkward postures. However, only four epidemiological studies showed the associated risk of being exposed to awkward postures and having LBP and/or sciatica [7, 9, 10, 48]. The results of these studies confirms that in the case of bus drivers [9], tractor drivers [7], road washing vehicle [48] drivers, and helicopter pilots [10], the risk of having LBP increases due to awkward posture while driving. The Road Washing Vehicle drivers have the highest OR of all the occupations (OR=10.59) [48]. It may be important to note that these drivers are exposed to trunk flexion, bending, and twisting, whereas the other occupational groups are exposed to only one of these factors. Hence, flexion, bending, and twisting may be more detrimental than only flexion. The question to be asked in this case is if the observed adverse effects of driving in these studies should be attributed to the exposure to awkward posture alone or to a combination of prolonged sitting, twisting, and bending postures, once sitting per se was not investigated.
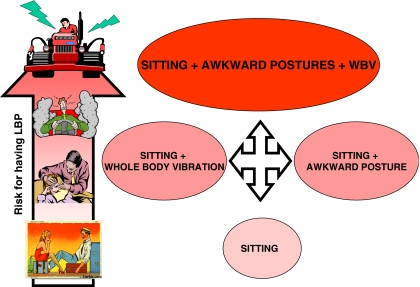
A proposed model
The literature reviewed has indicated an increased risk of LBP and sciatica for individuals in those occupations that require prolonged sitting (defined as sitting for more than half of a working day). However, the risk increases after combining factors such as WBV and awkward postures. In fact, for all the occupations studied, these co-exposure factors were the variables that led to a significantly increased risk. The fact of being seated for an extended period does not significantly demonstrate an impressive risk of having LBP and/or sciatica. Bovenzi and Betta [7] compared a group of agricultural tractor drivers with a group of office workers. Both groups were exposed to static load due to prolonged sitting. However, only the tractor drivers group was exposed to the combined factors of WBV and awkward posture. They found that tractor drivers were 2.39 times more likely to report LBP than office workers (OR=2.39, 95% CI 1.57–3.66). The association was similar (OR=2.36, 95% CI 1.48–3.74) when they looked at WBV while sitting (adjusted for awkward posture). The association increased when postural load was analyzed adjusting for vibration dose (OR=4.56, 95% CI 2.59–8.03).
A model was constructed based on WBV and awkward postures (Fig. 2). The model aims to describe how the risk effect of prolonged sitting increases significantly as other co-exposure factors (in this case WBV and awkward postures) play a role. As such, just the fact of sitting probably does not present a risk until the worker is exposed to a certain level of WBV and/or an awkward posture. When these co-exposure factors are combined, the risk for reporting LBP and/or sciatica increases (Fig. 2). Bovenzi and Betta [7] tried to demonstrate this finding after analyzing the combined effect of postural load and total vibration dose. They found, as mentioned above (Table 4), that the combination of vibration dose and postural load increases the risk of reporting LBP. In fact, there was a linear trend of increasing prevalence of LBP as the combined effect increases, perhaps demonstrating a dose–response relationship.
Fig. 2.
The risk for having low back pain while sitting increases significantly as the combination of physical factors such as exposure to whole body vibration and awkward posture plays an additive effect
It could be argued that this model has many limitations due to the fact that LBP is multi-factorial in its origin. Through this literature review, some physical (mechanical) factors (WBV, awkward posture, and a combination of both) were identified that are associated with the occupations performed while sitting. However studies have shown that there are other risk factors for LBP to which workers are exposed during the time period when they are sitting or not sitting, such as manual material handling or lifting activities, or psychosocial factors.
Summary
No previous research has been reported that investigated the sitting posture with respect to LBP and sciatica in a manner similar to this literature review, so no direct comparisons can be made. However, it could be argued that the conclusions of this paper, as well as of this model, have some limitations due to the fact that LBP is multi-factorial in its origin. Through this literature review, an association was made between some work-related factors while sitting (WBV, awkward posture, and the combination of both) and reported LBP and sciatica. A quantitative determination of how much exposure to these risk factors (WBV and awkward posture) would alter the risk of occupational-related LBP was not conducted (dose–response relationship). Just being seated on the job is not a risk factor; sitting becomes risky when combined with other risk factors. There is a lack of research on how much the risk increases for all populations. Other individual or psychosocial risk factors that have been found to be predictive of LBP were not studied in this literature review. Thus, no conclusions can be made about the interactions between these factors while sitting and the presence of LBP/sciatica.
Conclusion and implications
More epidemiological studies are needed to provide clear evidence of the association between sitting and occupational LBP. However, our review suggests the following conclusions:
Sitting by itself does not show an increased association with the presence of reported LBP.
Sitting in combination with other co-exposures such as WBV and awkward posture does increase the association with the presence of LBP.
Sitting in combination with WBV and awkward posture seems to have the strongest association with the presence of LBP. However, this conclusion is based on only one study whose results have not since been replicated. Hence more studies are needed to confirm this hypothesis.
Occupational groups exposed to WBV while sitting are at an increased risk of having LBP. Also, the influence of the duration of the exposure seems more important than the magnitude of the exposure, suggesting a cumulative effect.
Although awkward posture while sitting has not been as well investigated as WBV, the results of the preliminary research reveal a strong association with the presence of LBP. Thus, occupational groups exposed to awkward postures while sitting have an increased risk of having LBP. However, further research is needed on this topic due to the lack of valid and reliable instruments for its measurement.
The interaction of factors such as sitting, WBV, and awkward posture should also be carefully analyzed in terms not only of their association with LBP, but also of their dose–response.
Awkward posture and WBV have been previously associated with LBP, even without sitting. Further research should be conducted to probe if sitting adds to the risk of LBP.
References
- 1.Andersson GBJ. Epidemiologic aspects of low-back pain in industry. Spine. 1981;6(1):53–60. doi: 10.1097/00007632-198101000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Andersson GBJ, Örtengren R. Myoelectric back muscle activity during sitting. Scand J Rehabil Med. 1974;3:73–90. [PubMed] [Google Scholar]
- 3.Black K, Lis A, Nordin M (2001) Association between sitting and occupational low back pain. In: Grammer symposium, Ulm, Germany. Ergomechanics, Chap. 1, pp 11–35
- 4.Bongers PM, Hulshof CTJ, Dijkstra L, Boshuizen HC. Back pain and exposure to whole body vibration in helicopter pilots. Ergonomics. 1990;33(8):1007–1026. doi: 10.1080/00140139008925309. [DOI] [PubMed] [Google Scholar]
- 5.Boshuizen HC, Bongers PM, Hulshof CTJ. Self-reported back pain in tractor drivers exposed to whole body vibration. Int Arch Occup Environ Health. 1990;62:109–115. doi: 10.1007/BF00383586. [DOI] [PubMed] [Google Scholar]
- 6.Boshuizen HC, Bongers PM, Hulshof CTJ. Self-reported back pain in fork-lift truck and freight-container tractor drivers exposed to whole body vibration. Spine. 1992;17(1):59–65. doi: 10.1097/00007632-199201000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Bovenzi M, Betta A. Low-back disorders in agricultural tractor drivers exposed to whole body vibration and postural stress. Appl Ergon. 1994;25(4):231–241. doi: 10.1016/0003-6870(94)90004-3. [DOI] [PubMed] [Google Scholar]
- 8.Bovenzi M, Hulshof CTJ. An update review of epidemiologic studies on the relationship between exposure to whole body vibration and low back pain (1986–1997) Int Arch Occup Environ Health. 1999;72:351–365. doi: 10.1007/s004200050387. [DOI] [PubMed] [Google Scholar]
- 9.Bovenzi M, Zadini A. Self-reported low back symptoms in urban bus drivers exposed to whole body vibration. Spine. 1992;17(9):1048–1059. doi: 10.1097/00007632-199209000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Bridger RS, Groom MR, Jones H, Pethybridge RJ, Pullinger N. Task and postural factors are related to back pain in helicopter pilots. Aviat Space Environ Med. 2002;73:805–811. [PubMed] [Google Scholar]
- 11.Brown JJ, Wells GA, Trottier AJ, et al. Back pain in a large Canadian police force. Spine. 1998;23(7):821–827. doi: 10.1097/00007632-199804010-00017. [DOI] [PubMed] [Google Scholar]
- 12.Burdorf A, Zondervan H. An epidemiological study of low-back in crane operators. Ergonomics. 1990;33(8):981–987. doi: 10.1080/00140139008925307. [DOI] [PubMed] [Google Scholar]
- 13.Burdorf A. Exposure assessment of risk factors for disorders of the back on occupational epidemiology. Scand J Work Environ Health. 1992;18:1–9. doi: 10.5271/sjweh.1615. [DOI] [PubMed] [Google Scholar]
- 14.Burdorf A, Naaktgeboren B, deGroot HCWM. Occupational risk factors for low back pain among sedentary workers. J Occup Med. 1993;35(12):1213–1220. [PubMed] [Google Scholar]
- 15.Chen JC, Chang WR, Shih TS, Chen CJ, Chang WP, Dennerlein JT, Ryan LM, Christiani DC. Using ‘exposure prediction rules’ for exposure assessment: an example on whole-body vibration in taxi drivers. Epidemiol. 2004;15(3):293–299. doi: 10.1097/01.ede.0000121378.62340.a7. [DOI] [PubMed] [Google Scholar]
- 16.Dainoff MJ (1999) Ergonomics of seating and chairs. In: Salvendy C (ed) Handbook of human factors and ergonomics, chap. 97. CRC Press, Boca Raton
- 17.Frymoyer JW, Cats-Baril WL. An overview of the incidences and costs of low back pain. Orthop Clin North Am. 1991;22(2):263–271. [PubMed] [Google Scholar]
- 18.Griffin MJ. The evaluation of vehicle vibration and seats. Appl Ergon. 1978;9(1):15–21. doi: 10.1016/0003-6870(78)90214-4. [DOI] [PubMed] [Google Scholar]
- 19.Guo HR, Tanaka S, Cameron LL, et al. Back pain among workers in United States: National estimates and workers at high risk. Am J Ind Med. 1995;28:591–602. doi: 10.1002/ajim.4700280504. [DOI] [PubMed] [Google Scholar]
- 20.Hartvigsen JK, Kyvik KOP, Leboeuf YC, Lings S, Bakketeig L. Ambiguous relation between physical workload and low back pain: a twin contol study. Occup Environ Med. 2003;60:109–114. doi: 10.1136/oem.60.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hartvigsen J, Leboeuf YC, Lings S, Corder EH. Is sitting-while-at-work associated with low back pain? A systematic critical literature review. Scand J Public Health. 2000;28(3):230–239. [PubMed] [Google Scholar]
- 22.Heliövaara M, Mäkelä M, Knekt P, et al. Determinants of sciatica and low back pain. Spine. 1991;16(6):608–614. doi: 10.1097/00007632-199106000-00002. [DOI] [PubMed] [Google Scholar]
- 23.International Organization for Standardization (1985) Guide for the evaluation of human exposure to whole body vibration. Part 1: General requirements, 1st edn. ISO, Geneva. 1985:ISO 2631–1
- 24.Johanning E. Back disorders and health problems among subway train operators exposed to whole body vibration. Scand J Work Environ Health. 1991;17:414–419. doi: 10.5271/sjweh.1681. [DOI] [PubMed] [Google Scholar]
- 25.Johanning E. Evaluation and management of occupational low back disorders. Am J Ind Med. 2000;37:94–111. doi: 10.1002/(SICI)1097-0274(200001)37:1<94::AID-AJIM8>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 26.Johanning E, Bruder R (1998) Low back disorders and dentistry—stress factors and ergonomic intervention. In: Murphy DC (ed) Ergonomics and the dental care worker. Washington DC, pp 355–373
- 27.Johanning E, Wilder DG, Landrigan PJ, Pope MH. Whole body vibration exposure in subway cars and review of adverse health effects. J Occup Med. 1991;33(5):605–612. [PubMed] [Google Scholar]
- 28.Kamwendo K, Linton SJ, Moritz U. Neck and shoulder disorders in medical secretaries. Scand J Rehabil Med. 1991;23:127–133. [PubMed] [Google Scholar]
- 29.Kelsey JL. An epidemiological study of the relationship between occupations and acute herniated lumbar intervertebral discs. Int J Epidemiol. 1975;4(3):197–205. doi: 10.1093/ije/4.3.197. [DOI] [PubMed] [Google Scholar]
- 30.Keyserling WM, Punnet L, Fine LJ. Trunk posture and back pain: identification and control of occupational risk factors. Appl Ind Hyg. 1988;3(3):87–92. [Google Scholar]
- 31.Kopec JA, Sayre EC, Esdaile JM. Predictors of back pain in a general population cohort. Spine. 2004;29(1):70–78. doi: 10.1097/01.BRS.0000103942.81227.7F. [DOI] [PubMed] [Google Scholar]
- 32.Kroemer KHE, Kroemer HB, Kroemer-Ebert KE (1994) Ergonomics: how to design for ease and efficiency, Chap. 8. Prentice-Hall, Englewood Cliffs
- 33.Kumar A, Varghese M, Mohan D, et al. Effect of whole body vibration on the low back. Spine. 1999;24(23):2506–2515. doi: 10.1097/00007632-199912010-00013. [DOI] [PubMed] [Google Scholar]
- 34.Leclerc A, Tubach F, Landre MF, Ozguler A. Personal and occupational predictors of sciatica in the GAZEL cohort. Occup Med. 2003;53:384–391. doi: 10.1093/occmed/kqg072. [DOI] [PubMed] [Google Scholar]
- 35.Lee P, Helewa A, Goldsmith CH, Smythe HA, Stitt LW. Low back pain: prevalence and risk factors in an industrial setting. J Rheumatol. 2001;28(2):346–351. [PubMed] [Google Scholar]
- 36.Lehman KR, Psihogios JP, Meulenbroek GJ. Effects of sitting versus standing and scanner type on cashiers. Ergonomics. 2001;44(7):719–738. doi: 10.1080/00140130110046180. [DOI] [PubMed] [Google Scholar]
- 37.Levangie PK. Association of low back pain with self-reported risk factors among patients seeking physical therapy services. Phys Ther. 1999;79(8):757–766. [PubMed] [Google Scholar]
- 38.Li G, Haslegrave CM. Seated postures for manual, visual and combined tasks. Ergonomics. 1999;42(8):1060–1086. doi: 10.1080/001401399185144. [DOI] [PubMed] [Google Scholar]
- 39.Liira JP, Shannon HS, Chambers LW, Haines TA. Long-term back problems and physical work exposures in the 1990 Ontario Health Survey. Am J Public Health. 1996;86(3):382–387. doi: 10.2105/ajph.86.3.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lings S, Leboeuf-Yde C. Whole body vibration and low back pain: a systematic, critical review of the epidemiological literature 1992–1999. Int Arch Occup Environ Health. 2000;73:290–297. doi: 10.1007/s004200000118. [DOI] [PubMed] [Google Scholar]
- 41.Liss G, Jesin E, Kusiak A, White P. Musculoskeletal problems among Ontario dental hygienists. Am J Ind Med. 1995;28:521–540. doi: 10.1002/ajim.4700280408. [DOI] [PubMed] [Google Scholar]
- 42.Lu JLP. Risk factors for low back pain among Filipino manufacturing workers and their anthropometric measurements. Appl Occup Environ Hyg. 2003;18(3):170–176. doi: 10.1080/10473220301349. [DOI] [PubMed] [Google Scholar]
- 43.Macfarlane G, Thomas E, Papageorgiou AC, et al. Employment and physical work activities as predictors of future low back pain. Spine. 1997;22(10):1143–1149. doi: 10.1097/00007632-199705150-00015. [DOI] [PubMed] [Google Scholar]
- 44.Magnusson ML, Pope MH, Wilder DG, Areskoug B. Are occupational drivers at an increased risk for developing musculoskeletal disorders? Spine. 1996;21(6):710–717. doi: 10.1097/00007632-199603150-00010. [DOI] [PubMed] [Google Scholar]
- 45.Magora A. Investigation of the relation between low back pain and occupation. 3. Physical requirements: sitting, standing and weightlifting. Scand J Rehabil Med. 1972;41:5–9. [PubMed] [Google Scholar]
- 46.Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain. 2000;84:95–103. doi: 10.1016/S0304-3959(99)00187-6. [DOI] [PubMed] [Google Scholar]
- 47.Marras WS, Lavender SA, Leurgans SE, et al. Biomechanical risk factors for occupationally related low back disorders. Ergonomics. 1995;38(2):377–410. doi: 10.1080/00140139508925111. [DOI] [PubMed] [Google Scholar]
- 48.Massaccesi M, Pagnottaa A, Soccettia A, Masalib M, Masieroc C, Grecoa F. Investigation of work-related disorders in truck drivers using RULA method. Appl Ergon. 2003;34(4):303–307. doi: 10.1016/S0003-6870(03)00052-8. [DOI] [PubMed] [Google Scholar]
- 49.Masset D, Malchaire J. Epidemiologic aspects and work-related factors in the steel industry. Spine. 1994;19(2):143–146. [PubMed] [Google Scholar]
- 50.Masset D, Malchaire J, Lemoine M. Static and dynamic characteristics of the trunk and history of low back pain. Int J Ind Ergon. 1993;11:279–290. doi: 10.1016/0169-8141(93)90078-R. [DOI] [Google Scholar]
- 51.Merlino LA, Rosecrance JC, Anton D, Cook TM. Symptoms of musculoskeletal disorders among apprentice contruction workers. Appl Occup Environ Hyg. 2003;18(1):57–64. doi: 10.1080/10473220301391. [DOI] [PubMed] [Google Scholar]
- 52.Miranda H, Viikari-Juntura E, Martikainen R, Takala EP, Riihimaki H. Individual factors, occupational loading, and physical exercise as predictors of sciatic pain. Spine. 2002;27(10):1102–1108. doi: 10.1097/00007632-200205150-00017. [DOI] [PubMed] [Google Scholar]
- 53.Miyamoto M, Shirai Y, Nakayama Y, Gembun Y, Kaneda K. An epidemiologic study of occupational low back pain in truck drivers. J Nippon Med Sch = Nihon Ika Daigahu Zasshi. 2000;67(3):186–190. doi: 10.1272/jnms.67.186. [DOI] [PubMed] [Google Scholar]
- 54.Moen BE, Bjorvatn K. Musculoskeletal symptoms among dentists in a dental school. Occup Med. 1996;46:65–68. doi: 10.1093/occmed/46.1.65. [DOI] [PubMed] [Google Scholar]
- 55.Murphy PL, Volinn E. Is occupational low back pain on the rise? Spine. 1999;24(7):691–697. doi: 10.1097/00007632-199904010-00015. [DOI] [PubMed] [Google Scholar]
- 56.Nachemson A, Elfström G. Intravital dynamic pressure measurements in lumbar discs. Scand J Rehabil Med. 1970;1(Suppl):1–40. [PubMed] [Google Scholar]
- 57.NIOSH (1989) Proposed National strategy for the prevention of musculoskeletal injuries. US Department of Health and Human Services, NIOSH 89–129
- 58.NIOSH (1997) Musculoskeletal disorders and workplace factors: a critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back. Pub 97–141. Department of Health and Human Services, DHHS
- 59.O*NET 5.1 [database online]. US Department of Labor: National O*NET Consortium; 2004. Available at http://www.onetcenter.org/database.html. Accessed April 11, 2004
- 60.Özkaya N, Willems B, Goldsheyder D, Nordin M. Whole body vibration exposure experienced by subway train operators. J Low Freq Noise Vib. 1994;13(1):13–18. [Google Scholar]
- 61.Papageorgiou AC, Croft PR, Ferry S, et al. Estimating the prevalence of low back pain in the general population: evidence from the South Manchester Back Pain Survey. Spine. 1995;20(17):1889–1894. doi: 10.1097/00007632-199509000-00009. [DOI] [PubMed] [Google Scholar]
- 62.Pietri F, Leclerc A, Boitel L, et al. Low-back pain in commercial travelers. Scand Work Environ Health. 1992;18:52–58. doi: 10.5271/sjweh.1614. [DOI] [PubMed] [Google Scholar]
- 63.Porter JM, Gyi DE. The prevalence of musculoskeletal troubles among car drivers. Occup Med. 2002;52(1):4–12. doi: 10.1093/occmed/52.1.4. [DOI] [PubMed] [Google Scholar]
- 64.Pynt J, Higgs J, Mackey M. Milestones in the evolution of lumbar spinal postural health in seating. Spine. 2002;27(19):2180–2189. doi: 10.1097/00007632-200210010-00020. [DOI] [PubMed] [Google Scholar]
- 65.Quebec Task Force on Whiplash-Associated Disorders Critical appraisal form. Spine. 1995;20:1S–73S. doi: 10.1097/00007632-199501000-00001. [DOI] [PubMed] [Google Scholar]
- 66.Reinecke SM, Hazard RG, Coleman K, Pope MH. A continuous passive lumbar motion device to relieve back pain in prolonged sitting. In: Kumar S, editor. Advances in industrial ergonomics and safety IV. London: Taylor and Francis; 2002. pp. 971–976. [Google Scholar]
- 67.Riihimäki H. Low-back pain, its origin and risk indicators. Scand J Work Environ Health. 2002;17:81–90. [PubMed] [Google Scholar]
- 68.Rohlmann A, Claes LE, Bergmann G, Graichen F, Neef P, Wilke HJ. Comparison of intradiscal pressures and spinal fixator loads for different body positions and exercises. Ergonomics. 2001;44(8):781–794. doi: 10.1080/00140130110047657. [DOI] [PubMed] [Google Scholar]
- 69.Rotgoltz J, Derazne E, Froom P, et al. Prevalence of low back pain in employees of a pharmaceutical company. Isr J Med Sci. 1992;28:615–618. [PubMed] [Google Scholar]
- 70.Rundcrantz BL, Johnsson B, Moritz U. Pain and discomfort in the musculoskeletal system among dentists. Swed Dent J. 1991;15:219–228. [PubMed] [Google Scholar]
- 71.Seidel H, Heide R. Long-term effects of whole body vibration: a critical survey of the literature. Int Arch Occup Environ Health. 1986;58:1–26. doi: 10.1007/BF00378536. [DOI] [PubMed] [Google Scholar]
- 72.Shinozaki T, Yano E, Murata K. Intervention for prevention of low back pain in Japanese forklift workers. Am J Ind Med. 2001;40(2):141–144. doi: 10.1002/ajim.1081. [DOI] [PubMed] [Google Scholar]
- 73.Skov T, Borg V, Orhede E. Psychosocial and physical risk factors for musculoskeletal disorders of the neck, shoulders, and lower back in salespeople. Occup Environ Med. 1996;53(5):351–356. doi: 10.1136/oem.53.5.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Toren A. Muscle activity and range of motion during active trunk rotation in a sitting posture. Appl Ergon. 2001;32:583–591. doi: 10.1016/S0003-6870(01)00040-0. [DOI] [PubMed] [Google Scholar]
- 75.Van Deursen LL, Patijn J, Brouwer R, et al. Sitting and low back pain: the positive effect of rotatory dynamic stimuli during prolonged sitting. Eur Spine J. 1999;8:187–193. doi: 10.1007/s005860050155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vingard E, Alfredsson L, Hagberg M, Kilbom A, Theorell T, Waldenstrom M, Hjelm EW, Wiktorin C, Hogstedt C. To what extent do current and past physical and psychosocial occupational factors explain care-seeking for low back pain in a working population? Results from the Musculoskeletal Intervention Center-Norrtalje Study. Spine. 2000;25(4):493–500. doi: 10.1097/00007632-200002150-00017. [DOI] [PubMed] [Google Scholar]
- 77.Walsh K, Cruddas M, Coggon D. Low back pain in eight areas of Britain. J Epidemiol Commun Health. 1992;46:227–230. doi: 10.1136/jech.46.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Webster BS, Snook S. The cost of compensable low back pain. J Occup Med. 1990;32:13–16. doi: 10.1097/00043764-199001000-00007. [DOI] [PubMed] [Google Scholar]
- 79.Wells R, Moore A, Potvin J, Norman R. Assessment of risk factors for development of work-related musculoskeletal disorders. Appl Ergon. 1994;25(3):157–164. doi: 10.1016/0003-6870(94)90013-2. [DOI] [PubMed] [Google Scholar]
- 80.Wilke HJ, Neef P, Caimi M, et al. New in vivo measurements of pressures in the intervertebral disc in daily life. Spine. 1999;24(8):755–762. doi: 10.1097/00007632-199904150-00005. [DOI] [PubMed] [Google Scholar]