Abstract
Post-operative management after lumbar surgery is inconsistent leading to uncertainty amongst surgeons and patients about post-operative restrictions, reactivation, and return to work. This study aimed to review the evidence on post-operative management, with a view to developing evidence-based messages for a patient booklet on post-operative management after lumbar discectomy or un-instrumented decompression. A systematic literature search produced a best-evidence synthesis of information and advice on post-operative restrictions, activation, rehabilitation, and expectations about outcomes. Evidence statements were extracted and developed into patient-centred messages for an educational booklet. The draft text was evaluated by peer and patient review. The literature review found little evidence for post-operative activity restrictions, and a strong case for an early active approach to post-operative management. The booklet was built around key messages derived from the literature review and aimed to reduce uncertainty, promote positive beliefs, encourage early reactivation, and provide practical advice on self-management. Feedback from the evaluations were favourable from both review groups, suggesting that this evidence-based approach to management is acceptable and it has clinical potential.
Keywords: Advice, Booklet, Patient education, Post-operative management, Rehabilitation, Review, Spinal surgery
Introduction
Lumbar surgery for disc prolapse and spinal stenosis is well-established and common, but the results remain variable [24, 25, 62]. A significant proportion of patients have persistent or recurrent back pain or nerve root pain. Partly related to residual symptoms, but also depending on other biopsychosocial factors [63, 66], many patients fail to rehabilitate fully and have persistent disability. For example, Yorimitisu et al. [68] found that only 40% of patients returned to their pre-sciatica activity levels after discectomy, while McGregor and Hughes [50] reported minimal or limited improvement in function after decompression. Occupational outcomes vary in different series but, overall, approximately 20% of patients go on to long-term incapacity [58, 60].
Optimum surgical outcomes depend on (a) the technical outcome of surgery, and (b) post-operative recovery and rehabilitation. Most of the surgical literature has focused on the former and, until recently, less attention has been given to improving post-operative management. However, recovery cannot just be assumed if surgery is ‘successful.’ Structural changes in the spine and spinal muscles are inevitable and may be exacerbated by surgery [59, 69]. By the time patients come to surgery, they are likely to have some degree of deconditioning syndrome [31, 47]. The more severe and chronic the condition, the greater the need for post-operative rehabilitation. A Cochrane review confirmed that intensive post-operative exercise leads to improved functional outcomes [52]. Yet many patients (at least in the UK) receive little or no formal rehabilitation after surgery (A.H. McGregor et al., submitted for publication).
The Cochrane review also concluded that activity after surgery is not harmful [52]. Yet a recent UK survey (A.H. McGregor et al., submitted for publication) showed wide variation and inconsistencies in the advice surgeons give about post-operative activity and restrictions, e.g. for sitting, driving, or sedentary work. Magnusson et al. [42] found similar inconsistency and lack of scientific rationale in advice about lifting, with recommendations about work demonstrating even greater variability [33, 40]. Lack of advice, or inconsistent and contradictory advice, makes patients uncertain what they should or should not do post-operatively, which is likely to increase anxiety and inhibit their rehabilitation. Indeed a recent study has suggested that return to work may be delayed by these post-operative restrictions [26].
Modern patients are active partners in their own health care, for which they need and want accurate, practical information and advice [20]. Considerable material is now available through the internet and Consumer Health services, but the quality is very variable, often reflecting the views of individuals or interest groups rather than current evidence or best practice [11, 12]. This may add to rather than reduce patients’ confusion [38].
The aim of this project was therefore to review the evidence on post-operative management of spinal surgery patients from the scientific literature and to synthesize this information into key messages and advice. The secondary aim of this project was to incorporate the messages and advice gained from the literature review into an informational booklet that would be acceptable to patients and spinal surgeons. It was impractical to cover every kind of spinal surgery in a single booklet, so we focused on the common procedures for lumbar disc prolapse and spinal stenosis (surgery involving instrumentation was not included). Although these are different patient populations and surgical procedures, there are sufficient shared issues in post-operative management to make this feasible.
Methods
Literature review
A systematic search was made for published evidence on the post-operative management of patients undergoing lumbar discectomy or decompression. Inclusion criteria were elastic to include any relevant material about post-operative recovery, rehabilitation, and outcomes, but there was also a specific focus on information, advice, and prescriptions about exercise, activities, and restrictions. The main limitation was to publications in English. Purely technical data about surgical or post-surgical procedures were also excluded.
Medline was searched from 1984 through March 2005 using a combination of appropriate keywords including spinal surgery, decompression, stenosis, discectomy, recommendations, restrictions, rehabilitation, physiotherapy, and exercise. The electronic search was supplemented by citation tracking, Internet searches, and personal databases. Titles were identified of possible interest and abstracts screened by one of the authors for their general content. Full papers were obtained of clinical studies or reviews that appeared relevant and those meeting the inclusion criteria were reviewed by two of the authors.
A full systematic review methodology would be impracticable and inappropriate for the present purpose, so an alternative strategy had to be adopted. This was based on a qualitative evaluation of the scientific evidence to judge its relevance and appropriateness for identifying patient needs, informing key themes and developing patient information and advice, an approach used in previous studies [48]. Included articles were scrutinized and the pertinent information extracted and tabulated under the general themes of post-operative restrictions and post-operative activity/exercise/physiotherapy (though inevitably, there was some reciprocity between these headings). Evidence statements were synthesized by extensive discussion, reiterative drafting, and consensus between the reviewers, while recognizing the limitations of that evidence in many areas. Qualitative evaluation of the quantity, quality, and consistency of the evidence currently available was built into each statement, in a similar manner to that described previously for this type of review [48]. Thus, the literature review may best be summarized as systematic searching of the published scientific literature with a qualitative evaluation of the strength of that evidence as the basis for patient information and advice.
Development of the booklet
Building on the themes and evidence statements from the review, appropriate patient-centred messages were developed, and a booklet text was written with a view to patients receiving the booklet prior to surgery. This followed the general philosophy and style of The Back Book [56], which has been shown to be highly acceptable to health professionals and patients, and effective in changing patient beliefs and improving functional outcomes [4, 10]. The main aim of the present booklet was to improve understanding, reduce uncertainty and anxiety, promote positive expectations and beliefs, and build confidence during post-operative recovery. Practical advice on self-management and staged activation was also given. The outline structure of the booklet comprised of an introduction outlining the aims of the booklet, educational material on sciatica including what causes it, details of the operative procedure and the associated care pathway, advice on what to do postoperatively, along with practical tips on pain control, how to get going, etc., and a section on how to ‘get on with your life’ following surgery. Reiterative drafts of the text over a period of several months refined its content, clarity, and readability (4,760 words, Flesch Reading Ease 70%, Flesch-Kincaid Grade Level 6.5).
The professional evaluation included all relevant health professions: seven spinal surgeons, three general practitioners, six physiotherapists and complementary practitioners, one pain specialist, one rheumatologist, and one clinical psychologist. Lay professional comment was sought from a medical journalist and the UK back pain charity BackCare. On reviewing the draft content of the booklet, each reviewer was asked to give detailed narrative comment on the accuracy of its content, the messages, and the tone.
The second evaluation was in patients who were either waiting for, or who had recently had, surgery for disc prolapse or spinal stenosis, although the booklet was designed to be given to patients prior to surgery, it was felt that people who had recently had surgery would be able to offer important comments and/or criticisms. Patients at the Hammersmith Hospitals NHS Trusts, Queen’s Medical Centre Nottingham NHS Trust and the University of Leicester Hospitals NHS Trust were approached, and written informed consent obtained. Each patient was given a copy of the draft text to read at their leisure, and asked to complete and return an evaluative questionnaire. The questionnaire had two parts: (1) 11 forced-choice questions on readability, style, information level, believability, length, content, and helpfulness (for example, in information level—I learned some new, helpful things, I knew most of it anyway, I didn’t really find it helpful); (2) open questions about the most important messages they took from the booklet, anything they did not like or understand, if they had any concerns that were not covered, if they thought the booklet would change what they did after surgery, and their overall rating of the booklet on a scale from 1 to 10. A copy of the questionnaire is available on request from the corresponding author.
Results
Literature review
One hundred and nineteen papers were considered, of which 32 provided pertinent evidence. Tables 1 and 2 list the evidence statements, and links to the supportive literature.
Table 1.
Evidence statements derived with respect to imposition of restrictions following spinal surgery
| Evidence statement | Direct evidencea | Indirect evidenceb |
|---|---|---|
| The balance of the available evidence does not support the imposition of post-operative restrictions for discectomy or decompression surgery; what little support is offered comes from theoretical considerations rather than empirical evidence | [6, 18, 35, 36] | [1, 13] |
| There is limited evidence that activity specific restriction in respect of lifting, pushing, pulling is unnecessary | [42] | [68] |
| There is a lack of consensus among surgeons in respect of the need for, and the nature and timing of post-operative restrictions | [14, 42; A.H. McGregor et al., submitted for publication] | |
| The available evidence suggests that patients are uncertain about what activities they can or should undertake post-operatively | [7] | [2, 18, 45, 50, 51, 55] |
| The imposition of post-operative restrictions seems to relate to clinician/patient anxiety/uncertainty | [18] | |
| There is strong evidence that most post-operative restrictions are not necessary | [35–37] | |
| There is strong evidence that most post-operative restrictions delay recovery and return to work | [6, 35, 36] | [13] |
aStudy (or review) specifically addressing the topic
bStudy (or review) having incidental findings impacting on the topic
Table 2.
Evidence statements derived with respect to activity, work, and rehabilitation following spinal surgery
| Evidence statement | Direct evidencea | Indirect evidenceb |
|---|---|---|
| There is strong evidence that encouragement of mobility and return to full activities as soon as possible after surgery produces better relief of pain, and an earlier return to work | [6, 18, 32, 67] | [32, 61] |
| There is strong evidence that early post-operative rehabilitation programmes improve activities of daily living. Rehabilitation programmes vary considerably, and it is not possible categorically to state which components in what intensity are the most effective | [13, 16, 21, 34–37, 45, 67] | [2, 28, 32, 44, 53, 61] |
| There is strong evidence that early post-operative rehabilitation programmes improve return to work rates/times. Rehabilitation programmes vary considerably, and it is not possible categorically to state which components in what intensity are the most effective, though a focus on information about the course of disability and activity has been shown to be effective | [13, 18, 34–37, 45] | [2, 32, 44, 53] |
| There is strong evidence that early post-operative return to work is generally advantageous, and some studies suggest it can be as early as 1 week (but that will depend on the nature of the work and the surgical procedure). A progressive return to previous duty is desirable. The same evidence indicates that early post-operative return to work is not detrimental (but that may depend on the nature of the work) | [5, 6, 18, 35, 36] | [13, 29, 57] |
| There is some direct evidence and considerable indirect evidence suggesting that early post-operative return to work specifically results in faster recovery and better clinical outcomes | [16] | [2, 13, 29, 32, 35, 36, 44, 53, 61, 67] |
| Work/exercise is good for physical and mental health | [16, 35–37, 44, 45] | |
| Cohort studies show that return to work rates vary from less than 40% to more than 90%, with sickness absence times varying from as little as a day to over 12 months; the determinants include the type of procedure and the timing and nature of rehabilitation | [5, 6, 17, 18] | |
| The rate of recovery (both for clinical and vocational outcomes) is greatest in the first 3 months, with further improvement occurring more slowly | [18, 65] | [27, 50] |
| There is moderate evidence that patients’ expectations and satisfaction are important factors—recovery is facilitated by knowing what to expect | [18, 51] | |
| The concept of ‘let pain be your guide’ to guide reactivation is counterproductive | [18, 43] | [17] |
aStudy (or review) specifically addressing the topic
bStudy (or review) having incidental findings impacting on the topic
There is widespread agreement throughout this literature that patients do not know what they should or should not do during recovery from surgery [7, 18] that they need better information [18], and that surgeons should give clearer, more consistent, evidence-based advice [42; A.H. McGregor et al., submitted for publication].
There is little evidence for any post-operative restrictions (Table 1). There is strong evidence that activity is not harmful, together with theoretical arguments and considerable circumstantial evidence that progressive activity is beneficial (Table 2). For post-operative rehabilitation, there is strong evidence that intensive exercise therapies 4–6 weeks post-operatively produce faster recovery, with limited evidence for earlier intervention [54], though there is conflicting evidence on whether that produces any long-term benefit at 1 year [46]. There is no clear evidence on any specific type of exercise or physiotherapy, for supervised training versus home exercises, or for multidisciplinary rehabilitation. The timing of return to work has also generated much speculation, with Carragee et al. [6] advocating work as early as 1–2 weeks after discectomy (with some patients managing to return the following day), while others are more cautious [17, 29]: there is no clear evidence on what is optimum.
It is apparent that current practice does not reflect that evidence: many surgeons impose restrictions with little justification, while exercise and rehabilitation are not generally used (A.H. McGregor et al., submitted for publication). This may partly reflect the limited evidence, but surgeons may also be unaware of or lack confidence in the evidence, relying instead on what they were taught during training, personal experience, and clinical impression. The concern is that ill-founded advice and restrictions may unwittingly reinforce illness behaviour and delay recovery.
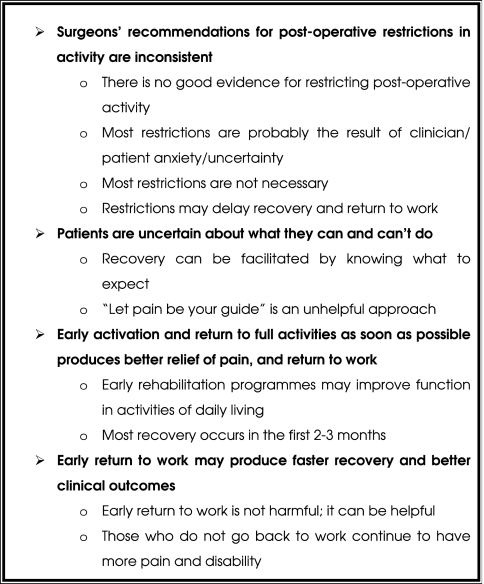
Despite the limitations of the evidence, it was sufficient to develop key themes and messages (Fig. 1). These were incorporated into the booklet, and supplemented by factual descriptions of the anatomy and pathology, surgical techniques, wound care, and warning signs of possible complications. Practical advice was provided on progressive reactivation, starting immediately post-operatively, with the issue of persisting back pain being dealt with in a realistic yet optimistic manner.
Fig. 1.
Key themes derived from the literature review
Booklet evaluations
All the professional reviewers stated they strongly supported the themes and messages of the booklet and recognized the need for such material. There were few and minor criticisms of the accuracy of the information provided, although some reviewers expressed views on the relative balance of the information and wording of technical matters. These comments and suggestions were discussed among the authors and changes made to the text as appropriate. Importantly, all the surgeons welcomed the booklet and considered it would be useful in their practices.
Booklets were sent to 20 patients for evaluation and 14 were returned (70%). The non-responders were not followed-up and reasons for non-response is not known. Of the responders, all 14 patients reported that they found the booklet easy to read, clear, and interesting. All stated that they felt the contents were helpful, and would recommend the booklet to other patients. Thirteen felt it was the right length, while one felt it was too long. Ten said they had learned new information, though that number may be depressed because two of the patients were health professionals. All the patients said they appreciated the information about the surgical procedure; half indicated they would like more rather than less. A few offered practical tips from their own experience. The narrative questions showed that patients appreciated information about the strength of the spine, the surgical procedure, post-operative practical tips, and setting realistic expectations. They took the messages that early activation was an important part of recovery, that they had a large role to play in the rehabilitation process, and that it was important to get on with their lives; one respondent felt that too much responsibility was placed on the patient. The patients’ average overall rating of the booklet was 9/10. The patients’ responses were again discussed by the authors, and appropriate changes made to the text.
Discussion
Modern patients want and have the right to expect the best possible information and advice, and the quality of that information, and the manner in which it is imparted is than important. The current situation in lumbar surgery is clearly unsatisfactory, with patients often receiving limited, inaccurate or inconsistent verbal information only.
Booklets are a simple, cheap, and popular method of providing health-related information to patients [30], and have been shown to be feasible and effective in low back pain [4, 10]. More generally, studies have suggested that such material can improve compliance [15], alleviate anxiety and promote psychological well being [23], and reduce medical negligence claims [39]. Although other media including video and internet have been explored [9, 19, 41], written material is by far the simplest, cheapest and therefore potentially the most cost-effective method [38]. However, developing acceptable and effective informational material is not easy, even for the apparently simple medium of booklets or leaflets [3, 12, 20].
Existing material for these patients retrieved during the present research was not evidence-based, lacked quality assurance, and was inconsistent in both form and content. The present study showed that it is possible to redress this situation. The present booklet [64] was developed according to established principles: an extensive review of the evidence base, careful synthesis into patient-centred messages, intensive work on appropriately targeted text [22], and evaluation by peers and end-users [8, 49]. To foster realistic expectations and recognizing that addressing potential adverse effects can reduce anxiety [3, 9], the possibility of residual back pain and other problems was discussed openly and frankly. This did not produce any negative response from the evaluators. The format, presentation, and illustrations of the booklet were developed in close collaboration with a publisher, and Your Back Operation has now been published [64].
This booklet is intended to be given by surgeons to patients, and it can be seen as a clinical tool to supplement and reinforce verbal communication. It can also serve as a guide and aide memoire to the surgeon for that verbal advice. Its use should help to overcome the current inconsistency. Pilot studies show that it is welcomed by surgeons and patients alike, and that it is likely to improve patient satisfaction. It will be interesting to see if there is any associated improvement in functional outcomes; this is currently being tested in an RCT of rehabilitation strategies for post-operative management after lumbar surgery.
Acknowledgements
This study was conducted in line with the UK requirements on such studies and ethical approval was obtained for the patient evaluation of the booklets.
References
- 1.Alaranta H, Hurme M, Einola S, Kallio V, Knuts L, Torma T. Rehabilitation after surgery for lumbar disc herniation: results of a randomised clinical trial. Int J Rehabil Res. 1986;9:247–257. doi: 10.1097/00004356-198609000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Brennan G, Shultz BB, Hood RS, Zahniser JC, Johnson SC, Gerber AH. The effects of aerobic exercise after lumbar microdiscectomy. Spine. 1994;19:735–739. doi: 10.1097/00007632-199404000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Burton AK, Waddell G (2002) Educational and informational approaches. In: Linton SJ (ed) New avenues for the prevention and management of chronic musculoskeletal pain and disability. Pain research and clinical management, vol. 12. Elsevier Science, Amsterdam, pp 245–258
- 4.Burton AK, Waddell G, Tillotson M, Summerton N. Information and advice to patients with back pain can have a positive effect. Spine. 1999;24:2484–2491. doi: 10.1097/00007632-199912010-00010. [DOI] [PubMed] [Google Scholar]
- 5.Carragee EJ, Helms E, O’Sullivan GS. Are postoperative activity restrictions necessary after posterior lumbar discectomy? A prospective study of outcomes in 50 consecutive cases. Spine. 1996;21:1893–1897. doi: 10.1097/00007632-199608150-00013. [DOI] [PubMed] [Google Scholar]
- 6.Carragee EJ, Han MY, Yang B, Kim DH, Kraemer H, Billys J. Activity restrictions after posterior lumbar discectomy. A prospective study of outcomes in 152 cases with no postoperative restrictions. Spine. 1999;24:2346–2351. doi: 10.1097/00007632-199911150-00010. [DOI] [PubMed] [Google Scholar]
- 7.Christensen FB, Laurberg I, Bunger CE. Importance of the Back-café concept to rehabilitation after lumbar spinal fusion: a randomised clinical study with a 2 year follow up. Spine. 2003;28:2561–2569. doi: 10.1097/01.BRS.0000097890.96524.A1. [DOI] [PubMed] [Google Scholar]
- 8.Chumbley GM, Hall GM, Salmon P. Patient controlled analgesia: what information does the patient want? J Adv Nurs. 2002;39:459–471. doi: 10.1046/j.1365-2648.2002.02311.x. [DOI] [PubMed] [Google Scholar]
- 9.Coudeyre E, Poiraudeau S, Revel M, Kahan A, Drape JL, Ravaud P. Beneficial effects of information leaflets before spinal steroid injection. Joint Bone Spine. 2002;69:597–603. doi: 10.1016/S1297-319X(02)00457-8. [DOI] [PubMed] [Google Scholar]
- 10.Coudeyre E, Rannou F, Coriat F, Brin S, Revel M, Poiraudeau S (2005) Impact of the back book on acute low back pain outcome. In: Presented to the international society for the study of the lumbar spine, New York
- 11.Coulter A. Evidence based patient information. BMJ. 1998;317:225–226. doi: 10.1136/bmj.317.7153.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coulter A, Entwistle V, Gilbert D. Informing patients. London: King’s Fund Publishing; 1998. [Google Scholar]
- 13.Danielsen JM, Johnsen R, Kibsgaard SK, Hellevik E. Early aggressive exercise for postoperative rehabilitation after discectomy. Spine. 2000;25:1015–1020. doi: 10.1097/00007632-200004150-00017. [DOI] [PubMed] [Google Scholar]
- 14.Dicken BJ, McGregor AH, Jamrozik KD. Trends in the management of postoperative low back pain. J Bone Joint Surg. 2005;87-B(Suppl. I):38. [Google Scholar]
- 15.Dickinson D, Raynor DK, Duman M. Patient information leaflets for medicines: using consumer testing to determine the most effective design. Patient Educ Couns. 2001;43:147–159. doi: 10.1016/S0738-3991(00)00156-7. [DOI] [PubMed] [Google Scholar]
- 16.Dolan P, Greenfield K, Nelson RJ, Nelson IW. Can exercise therapy improve the outcome of microdiscectomy? Spine. 2000;15(25):1523–1532. doi: 10.1097/00007632-200006150-00011. [DOI] [PubMed] [Google Scholar]
- 17.Donceel P, Du Bois M. Fitness for work after surgery for lumbar disc herniation: a retrospective study. Eur Spine J. 1998;7:29–35. doi: 10.1007/s005860050023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donceel P, Du Bois M, Lahaye D. Return to work after surgery for lumbar disc herniation: a rehabilitation oriented approach in insurance medicine. Spine. 1999;24:872–876. doi: 10.1097/00007632-199905010-00007. [DOI] [PubMed] [Google Scholar]
- 19.Eaden J, Abrams K, Shears J, Mayberry J. Randomised controlled trial comparing the efficacy of a video and information leaflet versus information leaflet alone on patient knowledge about surveillance and cancer risk in ulcerative colitis. Inflamm Bowel Dis. 2002;8:407–412. doi: 10.1097/00054725-200211000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Entwistle VA, Watt IS. Disseminating information about healthcare effectiveness: a survey of consumer health information services. Qual Health Care. 1998;7:124–129. doi: 10.1136/qshc.7.3.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Filiz M, Cakmak A, Ozcan E. The effectiveness of exercise programmes after lumbar disc surgery: a randomised controlled study. Clin Rehabil. 2005;19:4–11. doi: 10.1191/0269215505cr836oa. [DOI] [PubMed] [Google Scholar]
- 22.Garrud P, Wood M, Stainsby L. Impact of risk information in a patient education leaflet. Patient Educ Couns. 2001;43:301–304. doi: 10.1016/S0738-3991(00)00168-3. [DOI] [PubMed] [Google Scholar]
- 23.George CF, Walters WE, Nicholas JA. Prescription information leaflets: a pilot study in general practice. Br Med J. 1983;287:1193–1196. doi: 10.1136/bmj.287.6400.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gibson JN, Waddell G. Surgery for degenerative lumbar spondylosis. Cochrane Database Syst Rev. 2005;18(2):CD001352. doi: 10.1002/14651858.CD001352.pub2. [DOI] [PubMed] [Google Scholar]
- 25.Gibson JN, Grant IC, Waddell G. The Cochrane review of surgery for lumbar disc prolapse and degenerative lumbar spondylosis. Spine. 1999;24:1820–1832. doi: 10.1097/00007632-199909010-00012. [DOI] [PubMed] [Google Scholar]
- 26.Greenfield K, O’Neill C, Findlay G, Nelson RJ (2005) Health economic evaluation of a randomised clinical trial comparing lumbar microdiscectomy with conservative management. In: Proceedings of International Society for the Study of the Lumbar Spine, New York
- 27.Häkkinen A, Ylinen J, Kautiainen H, Airaksinen O, Herno A, Tarvainen U, Kiviranta I. Pain, trunk muscle strength, spinal mobility and disability following lumbar disc surgery. J Rehabil Med. 2003;35:236–240. doi: 10.1080/16501970306096. [DOI] [PubMed] [Google Scholar]
- 28.Häkkinen A, Ylinen J, Kautiainen H, Tarvainen U, Kirviranta I. Effects of home strength training and stretching versus stretching alone after lumbar disc surgery: a randomised study with a 1 year follow-up. Arch Phys Med Rehabil. 2005;86:865–870. doi: 10.1016/j.apmr.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 29.Hall H, McIntosh G, Melles T, Holowachuk B, Wai E. Effect of discharge recommendations on outcome. Spine. 1994;19:2033–2037. doi: 10.1097/00007632-199409150-00002. [DOI] [PubMed] [Google Scholar]
- 30.Hawkey GM, Hawkey CJ. Effect of information leaflets on knowledge in patients with gastrointestinal diseases. Gut. 1989;30:1641–1646. doi: 10.1136/gut.30.11.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hides JA, Richardson CA, Jull GA. Multidius muscle recovery is not automatic after resolution of acute first episode low back pain. Spine. 1996;21:2763–2769. doi: 10.1097/00007632-199612010-00011. [DOI] [PubMed] [Google Scholar]
- 32.Johannsen F, Remvig L, Kryger P, Beck P, Lybeck K, Larsen LH, Warming S, Dreyer V. Supervised endurance exercise training compared to home training after first lumbar discectomy: a clinical trial. Clin Exp Rheumatol. 1994;12:609–614. [PubMed] [Google Scholar]
- 33.Kahanovitz N, Viola K, Muculloch J. Limited surgical discectomy and microdiscectomy. A clinical comparison. Spine. 1989;14:79–81. doi: 10.1097/00007632-198901000-00016. [DOI] [PubMed] [Google Scholar]
- 34.Kara B, Tulum Z, Acar U. Functional results and the risk factors of reoperations after lumbar disc surgery. Eur Spine J. 2005;14:43–48. doi: 10.1007/s00586-004-0695-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kjellby-Wendt G, Styf J. Early active training after lumbar discectomy. Spine. 1998;23:2345–2351. doi: 10.1097/00007632-199811010-00019. [DOI] [PubMed] [Google Scholar]
- 36.Kjellby-Wendt G, Styf J, Carlsson SG. Early active rehabilitation after surgery for lumbar disc herniation: a prospective, randomised study of psychometric assessment in 50 patients. Acta Orthop Scand. 2001;72:518–524. doi: 10.1080/000164701753532871. [DOI] [PubMed] [Google Scholar]
- 37.Kjellby-Wendt G, Carlsson S, Styf J. Results of early active rehabilitation 5–7 years after surgical treatment for lumbar disc herniation. J Spinal Disord Tech. 2002;15:404–409. doi: 10.1097/00024720-200210000-00010. [DOI] [PubMed] [Google Scholar]
- 38.Little P, Roberts L, Blowers H, Garwood J, Cantrell T, Langridge J, Chapman J. Should we give detailed advice and information to patients with back pain: a randomised controlled factorial trial of a self-management booklet and doctor advice to take exercise for back pain. Spine. 2001;26:2065–2072. doi: 10.1097/00007632-200110010-00003. [DOI] [PubMed] [Google Scholar]
- 39.Livesley PJ, Rider MA. Joint replacement and patient education. Int Orthop. 1993;17(1):34–36. doi: 10.1007/BF00195221. [DOI] [PubMed] [Google Scholar]
- 40.Long DM. Decision making in lumbar disc disease. Clin Neurosurg. 1992;39:36–51. [PubMed] [Google Scholar]
- 41.Lorig KR, Laurent DD, Deyo RA, Marnell ME, Minor MA, Ritter PL. Can a back pain email discussion group improve health status and lower health care costs? Arch Intern Med. 2003;162:792–796. doi: 10.1001/archinte.162.7.792. [DOI] [PubMed] [Google Scholar]
- 42.Magnusson ML, Pope MH, Wilder DG, Szpalski M, Spratt K. Is there a rational basis for post-surgical lifting restrictions? 1. Current understanding. Eur Spine J. 1999;8:170–178. doi: 10.1007/s005860050153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Manniche C. Assessment and exercise in low back pain: with special reference to the management of pain and disability following first-time lumbar disc surgery. Dan Med Bull. 1995;42:301–313. [PubMed] [Google Scholar]
- 44.Manniche C, Asmussen K, Lauristen B, Vinterberg H, Karbo H, Abildstrup S, Fischer-Nielsen K, Krebs R, Ibsen K. Intensive dynamic back exercises with or without hyperextension in chronic back pain after surgery for lumbar disc protrusion: a clinical trial. Spine. 1993;18:560–567. doi: 10.1097/00007632-199304000-00007. [DOI] [PubMed] [Google Scholar]
- 45.Manniche C, Skall HF, Braendholt L, Christensen B, Christopherson L, Ellegaard B, Heilbuth A, Ingerslev M, Jorgensen OE, Larsen E, Lorentzen L, Nielsen CJ, Nielsen H, Windelin M. Clinical trial of postoperative dynamic back exercises after first lumbar discectomy. Spine. 1993;18:92–97. doi: 10.1097/00007632-199301000-00014. [DOI] [PubMed] [Google Scholar]
- 46.Mannion AF, Dvorak J, Muntener M, Grob D (2003) A randomised trial of post-operative rehabilitation after surgical decompression of the lumbar spine: initial readings. In: Proceedings of International Society for the Study of the Lumbar Spine, New York [DOI] [PMC free article] [PubMed]
- 47.Mayer TG, Vanharanta H, Gatchel RJ, Mooney V, Barnes D, Judge L, Smith S, Terry A. Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine. 1989;14:33–36. doi: 10.1097/00007632-198901000-00006. [DOI] [PubMed] [Google Scholar]
- 48.McClune T, Burton AK, Waddell G. Whiplash associated disorders: a review of the literature to guide patient information and advice. Emerg Med J. 2002;19:499–506. doi: 10.1136/emj.19.6.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McIntosh A, Shaw CF. Barriers to patient information provision in primary care: patients’ and general practitioners’ experiences and expectations of information for low back pain. Health Expect. 2003;6:19–29. doi: 10.1046/j.1369-6513.2003.00197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McGregor AH, Hughes SPF. The evaluation of the surgical management of nerve root compression in low back pain patients: part 1—the assessment of outcome. Spine. 2002;27:1465–1470. doi: 10.1097/00007632-200207010-00018. [DOI] [PubMed] [Google Scholar]
- 51.McGregor AH, Hughes SPF. The evaluation of the surgical management of nerve root compression in low back pain patients: part 2—patient expectations and satisfaction. Spine. 2002;27:1471–1476. doi: 10.1097/00007632-200207010-00019. [DOI] [PubMed] [Google Scholar]
- 52.Ostelo RWJG, de Vet HCW, Waddell G, Kerckhoffs MR, Leffers P, van Tulder MW (2000) Rehabilitation after lumbar disc surgery. The Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD003007. DOI 10.1002/14651858.CD003007 [DOI] [PubMed]
- 53.Ostelo RWJG, Vet HCW, Vlaeyen JWS, Kerckhoffs MR, Berfelo WM, Wolters PMJC, Brandt PA. Behavioural graded activity following first time lumbar disc surgery. Spine. 2003;28:1757–1765. doi: 10.1097/01.BRS.0000083317.62258.E6. [DOI] [PubMed] [Google Scholar]
- 54.Ostelo RWJG, Vet HCW, Waddell G, Kerckhoffs MR, Leffers P, Tulder M. Rehabilitation following first-time lumbar disc surgery. Spine. 2003;28:209–218. doi: 10.1097/00007632-200302010-00003. [DOI] [PubMed] [Google Scholar]
- 55.Ostelo RWJG, Goossens MEJB, Vet HCW, Brandt PA. Economic evaluation of a behavioural graded activity program compared to physical therapy for patient following lumbar disc surgery. Spine. 2004;29:615–622. doi: 10.1097/01.BRS.0000115130.42394.0B. [DOI] [PubMed] [Google Scholar]
- 56.Roland M, Waddell G, Klaber Moffett J, Burton K, Main C, Cantrell T. The back book. London: The Stationery Office; 1996. [Google Scholar]
- 57.Rompe JD, Eysel P, Zöllner J, Heine J. Prognostic criteria for work resumption after standard lumbar discectomy. Eur Spine J. 1999;8:132–137. doi: 10.1007/s005860050143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Scheer SJ, Radack KL, O’Brien DR., Jr Randomized controlled trials in industrial low back pain relating to return to work. Part 2. Discogenic low back pain. Arch Phys Med Rehabil. 1996;77:1189–1197. doi: 10.1016/S0003-9993(96)90147-1. [DOI] [PubMed] [Google Scholar]
- 59.Taylor MW. Return to work following back surgery: a review. Am J Ind Med. 1989;16:79–88. doi: 10.1002/ajim.4700160109. [DOI] [PubMed] [Google Scholar]
- 60.Taylor H, McGregor AH, Mehdi-Zadeh S, Richards S, Khan N, Alaghband-Zadeh J, Hughes SPF. The impact of self-retaining retractors on the paraspinal muscles during posterior spinal surgery. Spine. 2002;27:2758–2762. doi: 10.1097/00007632-200212150-00004. [DOI] [PubMed] [Google Scholar]
- 61.Timm KE. A randomized control study of active and passive treatments for chronic low back pain following L5 laminectomy. J Orthop Sports Phys Ther. 1994;20:276–286. doi: 10.2519/jospt.1994.20.6.276. [DOI] [PubMed] [Google Scholar]
- 62.Turner JA, Erek M, Herron L, Deyo R. Surgery for lumbar spinal stenosis: attempted meta-analysis of the literature. Spine. 1992;17:1–8. doi: 10.1097/00007632-199201000-00001. [DOI] [PubMed] [Google Scholar]
- 63.Waddell G, Burton AK. Concepts of rehabilitation for the management of common health problems. London: The Stationery Office; 2004. [Google Scholar]
- 64.Waddell G, Sell P, McGregor A, Burton K (2005) Your back operation. The Stationery Office, London, www.tso.co.uk/bookshop
- 65.Watkins RG, IV, Williams LA, Watkins RG., III Microscopic lumbar discectomy results for 60 cases in professional and Olympic athletes. Spine J. 2003;3:100–105. doi: 10.1016/S1529-9430(02)00569-7. [DOI] [PubMed] [Google Scholar]
- 66.WHO (2001) International classification of functioning, disability and health. World Health Organisation, Geneva
- 67.Yilmaz F, Yilmaz A, Merdol F, Parlar D, Sahin F, Kuran B. Efficacy of dynamic lumbar stabilization exercise in lumbar microdiscectomy. J Rehabil Med. 2003;35:163–167. doi: 10.1080/16501970306125. [DOI] [PubMed] [Google Scholar]
- 68.Yorimitisu E, Chiba K, Toyama Y, Hirabayashi K. Long-term outcomes of standard discectomy for lumbar disc herniation. Spine. 2001;26:652–657. doi: 10.1097/00007632-200103150-00019. [DOI] [PubMed] [Google Scholar]
- 69.Zhu X, Parnianpour M, Nordin M, Kahanovitz N. Histochemistry and morphology of erector spinae muscle in lumbar disc herniation. Spine. 1989;14:391–397. doi: 10.1097/00007632-198904000-00008. [DOI] [PubMed] [Google Scholar]