Abstract
A retrospective case control review was conducted to determine if the MW construct offers a superior means of correction of Cobb angles and pelvic obliquity in neuromuscular scoliosis. Posterior spinal fusion (PSF) in patients with neuromuscular scoliosis presents a surgical challenge. Particularly difficult is the correction of pelvic obliquity. Numerous instrumentation techniques have sought to address these difficulties. Most recently Arlet et al have introduced the MW construct. (in Eur Spine 8(3):229–231, 1999). They theorize that this construct may allow for superior spinopelvic fixation. Six patients with neuromuscular scoliosis who underwent PSF with the MW construct were compared with six subjects undergoing PSF utilizing the Galveston technique. Subjects were matched on the basis of preoperative Cobb angles and similar amounts of preoperative pelvic obliquity. Individuals who underwent PSF utilizing the MW construct obtained nearly 30% better correction of pelvic obliquity than did those who received a Galveston construct. A trend toward superior correction of Cobb angles with the MW construct was also observed. The MW construct may be a superior construct for curve correction in PSF for neuromuscular scoliosis, particularly those cases with excessive pelvic obliquity.
Keywords: Posterior spinal fusion, MW construct, Galveston, Pelvic obliquity, Neuromuscular scoliosis
Key points
Correction of pelvic obliquity in neuromuscular scoliosis is a surgical challenge.
There are numerous instrumentation techniques to achieve spinopelvic fixation in these patients.
The MW construct may be a superior instrumentation technique for the correction of pelvic obliquity and Cobb angles in neuromuscular scoliosis.
Mini Abstract
The MW construct is a newly described means of achieving spinopelvic fixation in neuromuscular scoliosis. It has been theorized that this construct may provide for superior correction of pelvic obliquity in neuromuscular patients. Our study retrospectively examines this theory by comparing the results of posterior spinal fusion using the new MW technique to matched controls undergoing surgery utilizing the Galveston construct.
Introduction
Posterior spinal fusion in patients with neuromuscular scoliosis presents a surgical challenge. Fixation of the lumbosacral spine poses numerous technical and biomechanical difficulties. Particularly difficult is adequate correction of the pelvic obliquity, which often accompanies long C-shaped neuromuscular curves. Several constructs have sought to address these difficulties.
Allen and Ferguson [1] are credited with first describing the well-recognized Galveston technique. This construct entails the use of rods inserted into the iliac wings, just above the sciatic notch, as a means of pelvic fixation. In 1996 Doubousset [2] described the use of 7 mm iliosacral screws, inserted from the iliac wing into the S1 pedicle, to correct pelvic obliquity. Other surgeons have supplanted the rods of the originally described Galveston technique with 7 mm screws [3]. The two aforementioned constructs have demonstrated the strongest lumbosacral fixation in biomechanical studies [4].
More recently Arlet et al. [5] have combined these two constructs into a single means of spinopelvic fixation. They utilized iliac screws (7 mm) inserted in a Galveston manner, and iliosacral screws (7 mm) to maximize construct strength and coined the technique the “MW Construct” based on its radiographic appearance (Fig. 1). The authors theorize that increased biomechanical purchase into the pelvis allows for superior correction.
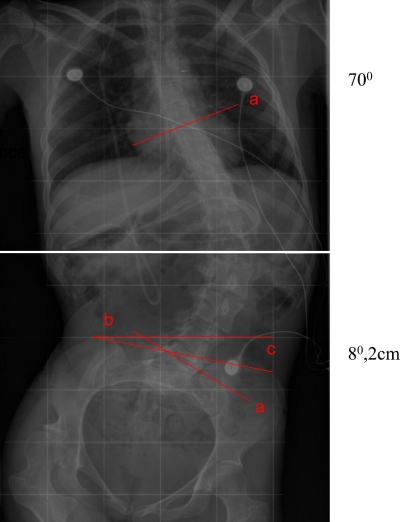
Fig. 1.
One preoperative and two postoperative images demonstrating the radiographic appearance of the MW construct on AP and lateral views
In our study, we sought to examine this idea. We compared the amount of Cobb angle correction and the relative amount of pelvic obliquity correction achieved with the MW construct versus the traditional Galveston type fixation in a small group of neuromuscular curves treated with posterior spinal fusion.
Materials and methods
Arlet et al has described well the technical aspects of the MW construct. [5]. In summary, the instrumentation of the scoliotic curve is completed with hooks, pedicle screws, or sublaminar wires. In the current study, the thoracic portion of the spine was instrumented utilizing Luque wire fixation, while the lumbar spinal curves were instrumented by a combination of Luque wires and pedicle screws.
The pelvis was then instrumented first with 7 mm iliosacral screws placed in a manner originally described by Cotrel and Dubousset [2]. Arlet and colleagues recommend performing a small hemilaminotomy to allow for direct visualization of the nerve root and to facilitate direct visualization during screw placement. Finally, 6 or 7 mm screws were inserted into the iliac wing parallel to the sciatic notch emerging approximately 2 cm above it. The starting point for these screws is approximately 1.5 cm below the iliosacral screw. These four points of pelvic fixation are then connected to the remainder of the spinal hardware and correction of the curve and pelvic obliquity are sequentially addressed [5].
We retrospectively reviewed our first six cases of neuromuscular scoliosis in which the MW construct was used to achieve correction of pelvic obliquity. The underlying diagnosis included three patients with spastic quadriparesis cerebral palsy, two with quadriparesis from traumatic events and one patient with myelodysplasia.
Despite the admitted limitations of matching on limited criteria, we chose six controls, patients with neuromuscular scoliosis matched solely upon their preoperative Cobb angle and preoperative pelvic obliquity. All had undergone posterior spinal fusion utilizing the traditional Galveston technique. All six were chosen from our prospective longitudinal cerebral palsy database and had spastic quadriparesis. All surgeries were performed within a 4-year period at the same academic medical center.
Medical records of those in the Galveston and MW study groups were obtained. The same individual reviewed immediate preoperative and 3 months postoperative films. It was assured that all radiographic studies were obtained in a similar manner for matched groups. For example, Galveston pre-and postoperative films obtained while sitting were matched with MW studies obtained in a similar fashion.
Though no gold standard has been established in the literature for measuring pelvic obliquity, we chose to measure obliquity as outlined in Fig. 2. We acknowledge that this method of measurement may be wrought with intraobserver and interobserver reliability. Nonetheless, the Cobb angles and the amount of pelvic obliquity were recorded for each patient. Mean preoperative and postoperative Cobb angle and pelvic obliquity were calculated. The pelvic obliquity was measured in degrees by intersecting lines, one drawn from the top of the iliac wing and the second line along the horizontal axis of the patient. The pelvic obliquity was also measured in the vertical height difference from the previously mentioned horizontal axis of the patient. The average amount of curve correction and correction of pelvic obliquity were noted for each group.
Fig. 2.
Anteroposterior image of a neuromuscular scoliosis patient which demonstrates the technique employed by the authors to measure Cobb angles and pelvic obliquity, in both a degree and distance measurement
Results
There were four males and two females in the MW group. The mean age was 15 years with the oldest and youngest patients being 24 and 11, respectively. Data for the MW group is summarized in Table 1. The mean preoperative and postoperative Cobb angles were 59.9° and 6.8°, and amount of pelvic obliquity 10.0° and 3.9°, respectively. The average pelvic obliquity was 2.7 cm preoperatively, and 1.12 cm postoperatively.
Table 1.
Summary of preoperative, postoperative, and relative correction measurements of Cobb angles and pelvic obliquity measurements in the MW group
| MW construct | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Preop | Postop | Correction | |||||||
| Cobb angle | Pelvic obliquity | Cobb angle | Pelvic obliquity | Cobb angle | Pelvic obliquity | ||||
| 1 | 54° | 8.6° | 2 cm | 5° | 2.7° | 0.5 cm | 49° | 5.9° | 1.5cm |
| 2 | 59.1° | 9° | 2.3 cm | 20° | 4.8° | 1.4 cm | 39.1° | 4.2° | 0.9 cm |
| 3 | 68° | 10° | 3.4 cm | 7° | 4° | 1.3 cm | 61° | 6° | 2.1 cm |
| 4 | 57.8° | 14.6° | 4 cm | 1.5° | 9.3° | 2.7 cm | 56.3° | 5.3° | 1.3 cm |
| 5 | 55.8° | 7.1° | 1.5 cm | 21° | 1° | 0.1 cm | 34.8° | 6.1° | 1.4 cm |
| 6 | 65.2° | 10.8° | 3.3 cm | 9.0° | 2.0° | 0.75 cm | 63.2° | 8.8° | 2.55 cm |
| Avg | 59.9° | 10.0° | 2.75 | 6.8° | 3.96° | 1.12 cm | 50.5° | 6.05° | 1.62 cm |
There were four females and two males in the Galveston group. The mean age was 17, with the oldest and youngest patients being 25 and 11, respectively. Data for the Galveston group is summarized in Table 2. The mean preoperative and postoperative Cobb angles were 53.8° and 21°, respectively. The mean preoperative and postoperative pelvic obliquity as measured by an angle measurement was 12.3° and 8.2°, respectively. The average amount of pelvic obliquity was 3.6 cm preoperatively, and 2.4 cm postoperatively.
Table 2.
Summary of preoperative, postoperative, and relative correction measurements of Cobb angles and pevic obliquity measurements in the Galveston group
| Galveston construct | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Preop | Postop | Correction | |||||||
| Cobb Angle | Pelvic obliquity | Cobb angle | Pelvic obliquity | Cobb angle | Pelvic obliquity | ||||
| 1 | 59° | 8.2° | 2.2 cm | 28° | 6.7° | 1.8 cm | 31° | 1.5° | 0.4 cm |
| 2 | 65° | 9.0° | 2.5 cm | 35° | 2.5° | 1.0 cm | 30° | 6.5° | 1.5 cm |
| 3 | 74° | 23° | 8 cm | 32° | 15.4° | 4 cm | 42° | 7.6° | 4 cm |
| 4 | 35° | 12° | 4.0 cm | 10° | 8.8° | 3 cm | 25° | 3.2° | 1 cm |
| 5 | 45° | 11° | 1.5 cm | 10° | 3° | 0.5 cm | 35° | 8° | 1.0 cm |
| 6 | 45° | 11° | 3.4 cm | 16° | 12.8° | 4.2 cm | 29° | 0° | 0 cm |
| Avg | 53.8° | 12.3° | 3.6 cm | 21° | 8.2° | 2.4 cm | 32° | 4.5° | 1.3 cm |
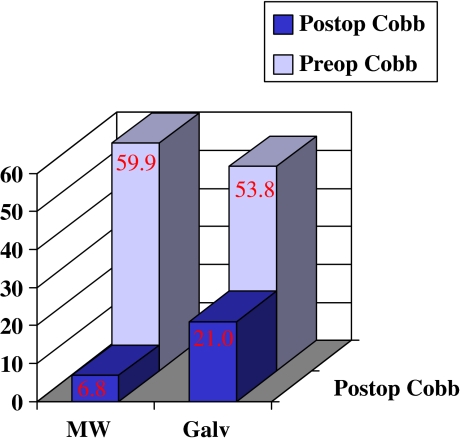
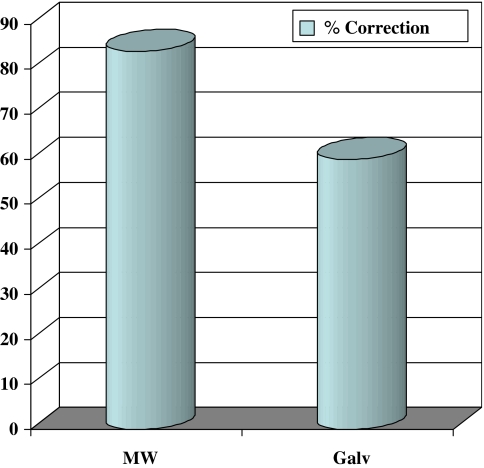
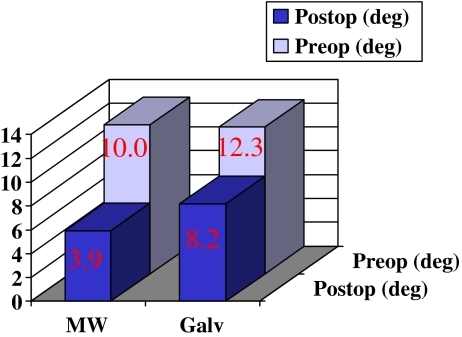
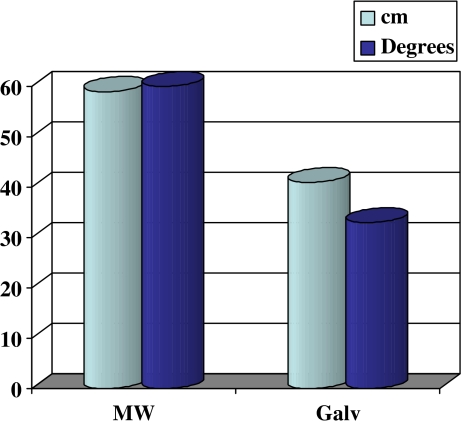
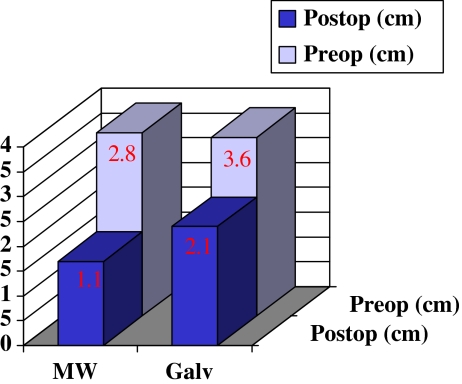
The average amount of curve correction was 50.5° in the MW group and 32ο in the Galveston group (see Figs. 3, 4). The average amount of pelvic obliquity correction in a degree measurement was 6.05 in the MW group and 4.5° in the Galveston group (see Figs. 5, 7). The average improvement in pelvic obliquity in a distance measurement (cm) was 1.62 cm in the MW group, as compared to 1.3 cm in the Galveston group (see Figs. 6, 7).
Fig.3 .
Graphical representation of the mean preoperative and postoperative Cobb angles for patients in both the MW and Galveston group
Fig. 4.
Graphical representation of the percent correction of the Cobb angle in each study group. Note the improved correction in Cobb angles in those undergoing fusion with the MW construct
Fig. 5.
Graphical representation of the average amount of preoperative and postoperative pelvic obliquity (in a degree measurement) for the MW and Galveston groups
Fig. 7.
Graphical demonstration of the superior correction of pelvic obliquity in those undergoing fusion with the MW construct as demonstrated by percent correction in each respective study group
Fig. 6.
Similar representation to that presented in Fig. 5, however, with pelvic obliquity as measured in distance (cm)
The mean blood loss was not significantly different between the two groups. The average operative time was 72 min longer in the MW group. The increased operative time reflected our learning curve, as each subsequent patient undergoing MW fixation required a decreasing amount of operative time. We had no significant complications in the MW fusion group or the Galveston controls.
The comparison radiographs and correction values were obtained at 3 months postoperatively. The results appear to be stable in the MW group as we currently have an average follow up of 18 months, with less than 1° loss of correction. The observed trend towards superior correction of both Cobb angle and pelvic obliquity appears well maintained.
Discussion
As previously outlined fixation to the lumbosacral pelvis in neuromuscular scoliosis poses many challenges. An ideal construct offers rigid biomechanical purchase thereby allowing for superior correction of pelvic obliquity. The combination of the two strongest individual constructs, 7 mm screws inserted in a Galveston fashion and 7 mm iliosacral screws, seems to attain increased purchase into the sacropelvis and thereby afford greater correction potential. In the current study, the MW group showed a trend toward superior correction of both Cobb angles and pelvic obliquity.
Individuals undergoing lumbosacral fusion utilizing the MW construct achieved nearly 30% more correction of pelvic obliquity as compared to those receiving the standard Galveston technique. Moreover, curve correction in the remainder of the thoracolumbar spine was on average 18° greater in the MW group.
There are several limitations to our study including small sample size and short follow-up. Additionally, the retrospective nature of the study and lack of randomization introduces the possibility of selection bias.
Moreover, it is difficult to currently surmise the clinical relevance of the improved correction in Cobb angles and pelvic obliquity. In follow-up of our patients there was a subjective improvement in the sitting and truncal balance of those patients stabilized with MW fixation. We have no objective data at this time to confirm this observation, but have an ongoing study examining wheelchair pressure maps to confirm this clinical suspicion.
Nonetheless, our study reveals superior correction of coronal deformity and pelvic obliquity using the MW construct in a limited number of patients with neuromuscular scoliosis. The improved pelvic fixation obtained using this technique allows more aggressive attempts at correction of pelvic obliquity and curve magnitude, which is evident during the learning curve. These findings warrant a larger, prospective, multicenter trial to determine if these early conclusions are valid in a larger population of patients.
References
- 1.Allen BL, Jr, Ferguson RL. The Galveston technique of pelvic fixation with L-rod instrumentation of the spine. Spine. 1984;9:388–394. doi: 10.1097/00007632-198405000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Dubousset J. Pelvic obliquity correction. In: Margulies JY, Floman Y, Farcy JP, Neuwirth MG, editors. Lumbosacral and spinopelvic fixation. Philadelphia: Lippincott-Raven; 1996. [Google Scholar]
- 3.Asher MA. Lumbopelvic fixation with the Isola system. In: Margulies JY, Floman Y, Farcy JP, Neuwirth MG, editors. Lumbosacral and spinopelvic fixation. Philadelphia: Lippincott-Raven; 1996. [Google Scholar]
- 4.McCord DH, Cunningham BW, Shono Y, Myers JJ, McAfee PC. Biomechanical analysis of lumbosacral fixation. Spine. 1992;17:S235–S243. doi: 10.1097/00007632-199208001-00004. [DOI] [PubMed] [Google Scholar]
- 5.Arlet V, Aebi M, Marchesi D, Papin P. The ‘MW’ sacropelvic construct: an enhanced fixation of the lumbosacral junction in neuromuscular pelvic obliquity. Eur Spine. 1999;J.8(3):229–231. doi: 10.1007/s005860050163. [DOI] [PMC free article] [PubMed] [Google Scholar]