Abstract
To study the characteristics and changes in the total Oswestry Disability Index (ODI) and in its ten component items in female and male patients pre- and post-surgery for lumbar disc herniation. Ninety-eight patients [mean (SD) age 43 (13), 61% males] undergoing lumbar disc herniation surgery were selected for this clinical 12-month follow-up. Subjective disability and back and leg pain were assessed by ODI version 1.0 and the visual analog scale. Pre-operatively females had a significantly higher mean (SD) total ODI [59(3)] than males [51(2)] (P = 0.030). Females were more disabled in the walking, sex life, social life and travelling items of the ODI compared to males. The total Oswestry decreased by 38 (95% CI − 44 to − 31) in females and by 34 (− 39 to − 30) in males at the 1-year follow-up. Most of the improvement (88% in females and 80% in males) occurred during the first 6 weeks; thereafter the changes were minor. In males the changes were greatest in pain, social life and travelling and in females in walking, social life and travelling. Internal consistency value of ODI was 0.88 (95% CI 0.82–0.91). Item analysis of the ODI showed that all the items except pain had high corrected item correlation. As recovery following lumbar disc surgery occurred to a great extent during the first 6 weeks, the early post-operative outcome appears to be quite a reliable indicator of the overall post-operative outcome over the 1-year follow-up. The ODI proved to capture a wide range of disability in these lumbar disc surgery patients, thereby supporting the future use of the index. The “pain intensity” component, which collects data on the use of painkillers in version 1.0 of the ODI did not support the item structure of the index in this study. The use of ODI version 2.0 might remove this problem.
Keywords: Disability, Lumbar disc herniation, Surgery, Pain
Introduction
Surgery for herniation of a lumbar disc is the most common spinal operation. In the early post-operative stages (up to 12 months) success rates over 90% have been reported [11, 14]. When the follow-up time has been longer, from 7 to 11 years, 76–93% of patients have shown good results [9, 16, 18, 23, 26].
Assessment of the results of lumbar disc herniation surgery is complicated by the nature of the disorder and the goals of the surgery. Pain and disability may persist despite the fact that radiology and neuroimaging indicate that the operation has been successful [3]. Therefore, assessment of the outcome has undergone a shift from the earlier predominant reliance on radiological or biochemical measures, or from ratings performed by the treating physician to the patient’s own perception [2]. A variety of instruments have been applied to measure the patient’s view of his/her health and or ability to perform activities of daily living (ADL) [1]. Usually these include ratings for pain, disability in everyday activities, work-capacity and quality of life [6]. Such measures are indispensable, as they assess the factors that will, ultimately, determine whether the patient is able to resume a normal working and social life, or will, instead, continue to make use of the healthcare resources available [17]. Another important question is whether the improvement in a patient observed by repeated measures is clinically relevant.
The disease-specific questionnaires in back surgery are the Oswestry Disability Index (ODI) [8] and the Roland–Morris disability Questionnaire (RDQ) [21]. Both are short, concise questionnaires, easy to use in clinical practice, and patients need approximately 5 min to complete the survey. Of the two, ODI is the most often used. It has also been shown to be valid and responsive to changes in clinical status [20]. In all the earlier studies, associations between various clinical variables with patient self-reports have usually been reported as associations with the total ODI, and therefore little is known about the status of and changes in individual dimensions of the disability index. Therefore, the main purpose of this prospective study was to evaluate changes in the total ODI and also in its ten dimensions in male and female patients pre- and post-lumbar disc herniation surgery on a 1-year period. In addition, the properties of the ODI were studied.
Methods
Subjects
One hundred and forty-five patients received surgery for lumbar disc herniation in Jyväskylä Central Hospital in 2003 according to the method described by Wood and Hanley in 1991 [25]. Twenty-six were excluded due to previous back surgery and 21 patients failed to fill in either the pre-operative or post-operative questionnaire. The final homogeneous study group consisted of 98 (82%) virgin lumbar disc herniation patients. The patients varied in age from 17 to 81 years.
Before surgery, in the department of orthopaedics, the subjects were asked to complete a questionnaire that contained items on both demographic characteristics and on the duration and intensity of back and leg pain. The post-operative outcome was assessed at 6 weeks and at 12 months. Back and leg pain was assessed with the visual analogue scale (VAS, 0–100 mm) [7].
The degree of disability during the past week was assessed with the Oswestry Low Back Pain Disability Questionnaire (ODI), version 1.0, which is divided into ten items designed to assess multiple aspects of disability with respect to pain: pain, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, travelling [8]. Each ODI item is scored on a 0–5 scale, with 5 representing the greatest level of disability. The scores for all items are then summed to give a score out of 50. The total score is then doubled and expressed as a percentage. If a patient marks two statements to a single item, the higher of the two is recorded. If a section is not completed because it is inapplicable, the final score is adjusted to obtain a correct percentage. Disability in this study is defined as an umbrella term for impairments, activity limitations and participation restrictions according to the WHO’s International Classification of Functioning, Disability and Health (ICF) [24].
Statistical analysis
The results are presented as means with standard deviations, standard errors or 95% confidence intervals. The multiple imputation (Markov chain Monte Carlo) method was used to fill in missing values for individual items of the ODI. Statistical comparisons between the sexes were made by using the t test or permutation test. Internal consistency was estimated by calculating Cronbach’s alpha with 95% confidence interval obtained by bias corrected bootstrapping (1,000 replications). The corrected item correlation for the individual items of the ODI was calculated by using a polyserial correlation coefficient.
Results
Pre-operative demographic and clinical characteristics were similar between the sexes except for higher back pain in females (Table 1). The decreases in back and leg pain were more prominent from the pre-operative level to 6 weeks post-operatively in females compared to males (P = 0.016 and P = 0.003). At the 1-year follow-up the changes from 6 weeks were minor, and the gender differences had disappeared.
Table 1.
Demographics and clinical data before surgery for lumbar disc herniation
| Male (N = 60) | Female (N = 38) | Difference between the gender, P value | |
|---|---|---|---|
| Age (years), mean (SD) | 45 (12) | 43 (14) | 0.55 |
| Body mass index, mean (SD) | 26 (4) | 26 (4) | 0.63 |
| Back pain | |||
| Duration, mean (SD) | 16 (24) | 15 (24) | 0.76 |
| Intensity; VAS, mean (SD) | |||
| Pre-operatively | 55 (31) | 73 (23) | 0.003 |
| 6 week post-operatively | 18 (25) | 13 (17) | 0.24 |
| 1 year post-operatively | 31 (32) | 21 (23) | 0.11 |
| Leg pain | |||
| Duration, mean (SD) | 10 (14) | 9 (11) | 0.53 |
| Intensity, VAS, mean (SD) | |||
| Pre-operatively | 72 (23) | 77 (19) | 0.23 |
| 6 wk post-operatively | 24 (28) | 21 (26) | 0.67 |
| 1 year post-operatively | 30 (35) | 19 (22) | 0.78 |
| Level of the operation | |||
| L3–4 | 2 | 4 | |
| L4–5 | 32 | 22 | |
| L5–S1 | 25 | 12 | |
| L4–L5 and L5–S1 | 1 | – | |
| Site of the operation | |||
| Right | 25 | 14 | |
| Left | 31 | 20 | |
| Central | 4 | 4 | |
Pre-operatively females had a significantly higher mean (SD) total ODI [59(3)] than males [51(2)] (P = 0.030). Females were more disabled in walking, sex life, social life and travelling items of the ODI compared to males (Table 2). In both sexes disability was lowest in sleeping and personal care. In males disability was highest in pain and lifting, and in females in pain, lifting, standing, social life and travelling. According to the WHO’s ICF classification the ODI captured all three components of disability: two items in impairments (B), five items in activity limitations (A) and three in participation restrictions (P) (Table 2).
Table 2.
Individual items of the Oswestry index and their coding according to the WHO’s International Classification of Functioning, Disability and Health (ICF)
| Pre-operative value | Coding of items (ICF classification) | |||
|---|---|---|---|---|
| Male (N = 60), mean (SE) | Female (N = 38), mean (SE) | Difference between the gender, P value | ||
| 1. Pain intensity | 3.2 (0.2) | 3.4 (0.2) | 0.44 | B280 |
| 2. Personal care | 1.7 (0.1) | 2.0 (0.3) | 0.26 | A510, A540 |
| 3. Lifting | 3.1 (0.1) | 3.4 (0.2) | 0.16 | A430 |
| 4. Walking | 2.0 (0.2) | 2.7 (0.2) | 0.033 | A450 |
| 5. Sitting | 2.9 (0.2) | 3.1 (0.2) | 0.52 | A415 |
| 6. Standing | 2.9 (0.2) | 3.4 (0.2) | 0.098 | A415 |
| 7. Sleeping | 1.8 (0.2) | 1.8 (0.2) | 0.87 | B134 |
| 8. Sex life | 2.2 (0.2) | 3.1 (0.3) | 0.0074 | P770 |
| 9. Social life | 3.0 (0.2) | 3.4 (0.2) | 0.034 | P990 |
| 10. Travelling | 2.6 (0.2) | 3.4 (0.2) | 0.015 | P460 |
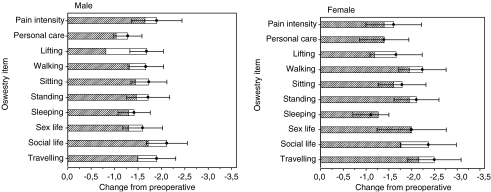
The total ODI decreased by 38 (95% CI − 44 to − 31) in females and by 34 (− 39 to − 30) in males (P < 0.001). Most of the improvement (88% in females and 80% in males) occurred during the first 6 weeks. In females the changes in all items were minor and in males only the change in lifting item from 6 weeks to 1 year was statistically significant (P = 0.002) (Fig. 1). At the 1-year follow-up the mean (SD) ODI of females [22(3)] did not differ from that of males [16(2)]. In males the changes were greatest in pain, social life and travelling and in females in walking, social life and travelling. The change in the total ODI was associated with the change in back pain (r = 0.55; 95% CI 0.39 to 0.68) and in leg pain (r = 0.69; 95% CI 0.58 to 0.78).
Fig. 1.
The mean change in individual items of Oswestry disability index in males and females from baseline to 6 weeks (hatched bars) and to 1 year post-operatively (open bars). Dots show means and whiskers show 95% confidence interval at 12-month follow-up
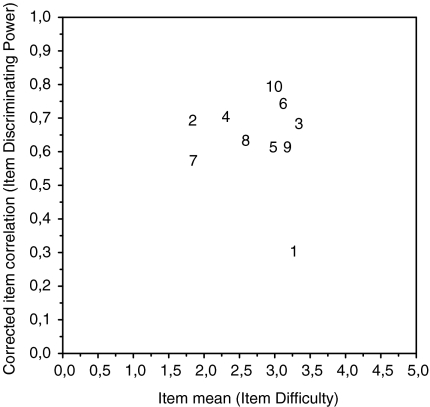
Internal consistency value of ODI was 0.88 (95% CI 0.82 to 0.91). Item analysis of the ODI showed that all the items had a high corrected item correlation except pain, which had a low correlation (Fig. 2).
Fig. 2.
Item analysis of Oswestry disability index (ODI). The number 1 that relates to pain intensity in the ODI had the weakest item discriminating power (the numbers indicate corresponding items)
Discussion
Disability as defined in this study comprises three components, impairments, activity limitations and participation restrictions. Measurements are often disease specific and focus on impairment and activity limitations rather than on aspects of participation or life involvement according to the WHO’s International Classification of Functioning, Disability and Health (ICF) [22, 24]. Further, the interpretation of these measures is generally based on overall scales rather than individual items. The impact of lumbar disc herniation on the individual is commonly assessed using the ODI. At the item level the ODI captures all three components of disability, which supports its future use as an outcome measure.
In our study the internal consistency of ODI was good. However, the corrected item correlation for “pain intensity” was clearly lower than that for the other items indicating that this particular item was less strongly related to the other component items of the ODI. The “pain intensity” question, which collects data on the use of painkillers in version 1.0 of the ODI, is clinically very important. However, as all the other items concern pain-related disability, the item on painkillers clearly does not measure the pain in the same way as the other items. The use of ODI version 2.0 might remove this problem [20] since in that version this particular question has been modified to measure pain intensity, not the use of painkillers.
The relative importance of the different items for any given patient is difficult to estimate and most likely is dependent upon the patient’s sociodemographic characteristics (e.g. age, family and work status, habitual activity), main symptoms (pain, functional disability) as well as the treatments administered [4]. It is also difficult to answer the question of what constitutes an important change. Ostelo and de Vet [19] reported recently that to be clinically important the change in pain in cases of chronic or subacute low back pain should be at least 20 mm and in acute low back pain 35 mm. No data exists on patients who have had with lumbar disc herniation surgery yet both the operation itself and the pain radiating down to leg differentiate these patients from those with other types of back pain and treatments. However, in the present sample, 17% of the patients had no back pain and 23% no leg pain at the 1-year follow-up. Further, the decreases from the pre-operative level to the 1-year follow-up of 48 mm in leg pain and 33 mm in back pain were statistically significant. In our previous survey the mean pain level in the general population aged > 30 years was 20 (95% CI 19 to 21) mm and about 24% (n = 1,038) of the respondents reported no pain (pain score = 0) [15]. Thus, it should be remembered that reports of pain may not wholly be due to the disease in question. The participants may have other co-morbidities, and age as such also increases the prevalence of back pain [13].
Musculoskeletal pain inhibits the motor system and thus may decrease the intensity of muscle contraction during peak pain, and even after the disappearance of the pain sensation [10]. In lumbar disc herniation pain interferes with such ADLs as mobility, dressing, sitting and standing. In our study the changes in back and leg pain correlated highly with changes in the total ODI. Females were more disabled and had higher back pain than males pre-operatively but post-surgery gender differences were not found. Dedering et al. [5] reported a significantly higher pre-operative total ODI in females [50(14)] than in males [36(15)]. In that study the values of different items were not shown, but 4 weeks post-operatively men improved significantly in eight and females in six of the ODI items. The exceptions were lifting and sitting for men and lifting, sitting, sex life and traveling for women. In our study the pain and lifting items accounted for a high proportion of the total ODI pre-operatively in both sexes. These items among all others improved significantly during the follow-up, but their relative proportion of the total ODI remained high. Our patients were instructed to perform their daily activities as normally as possible despite pain. They were informed about the ergonomics of the back when standing, sitting or lifting, and about pain coping. They were instructed to start active straight leg raising, gluteus stretching and rhythmic muscle contractions of the transversus abdominis muscle 1 week after the surgery. In addition they were instructed to gradually increase their walking distance. Unfortunately, compliance with these instructions was not monitored and their importance for action and perceived disability remains open.
Before the surgery the disability was severe in 81% (ODI < 40%) and minimal (ODI > 20%) in 4% of the patients according to the grading of ODI by Fairbank et al. [8]. Eighty-three percent of the improvement in ODI occurred during the first 6 weeks post-operatively indicating that the surgery had good early success. The early post-operative outcome appeared to be a reliable indicator of the post-operative outcome at the 1-year follow-up as the changes recorded from 6 weeks to 1 year post-operatively were minor. However, 13% of the patients reported severe disability at the 1-year follow-up; hence for a substantial number of patients the operation had limited success.
Conclusion
As recovery, measured by the ODI, following lumbar disc surgery occurred to a great extent during the first 6 weeks the early post-operative outcome appeared to be a reliable indicator of the post-operative outcome at the 1-year follow-up. The ODI proved to capture a wide scale of disability in lumbar disc surgery patients, thereby supporting the future use of the index. The “pain intensity” question about the use of painkillers in version 1.0 of ODI did not support the item structure of the index in the present study. The use of ODI version 2.0 might remove this problem.
References
- 1.Angevine PD, McCormick PC. Outcomes research and lumbar discectomy. Neurosurg Focus. 2002;13:1–4. doi: 10.3171/foc.2002.13.2.9. [DOI] [PubMed] [Google Scholar]
- 2.Asch HL, Lewis PJ, Moreland DB, Egnatchik JG, Yu YJ, Clabeaux DE, Hyland AH. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? J Neurosurg. 2002;96(1 Suppl):34–44. doi: 10.3171/spi.2002.96.1.0034. [DOI] [PubMed] [Google Scholar]
- 3.Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the maine lumbar spine study. Spine. 2005;30:927–935. doi: 10.1097/01.brs.0000158954.68522.2a. [DOI] [PubMed] [Google Scholar]
- 4.Bombardier C, Hayden J, Beaton DE. Minimal clinically important difference. Low back pain: outcome measures. J Rheumatol. 2001;28:431–438. [PubMed] [Google Scholar]
- 5.Dedering A, Harms-Ringdahl K, Nemeth G (2005) Back extensor muscle fatigue in patients with lumbar disc herniation pre-operative and post-operative analysis of electromyography, endurance time and subjective factors. Eur Spine J:Jun 7; [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 6.Deyo RA, Andersson G, Bombardier C, Cherkin DC, Keller RB, Lee CK, Liang MH, Lipscomb B, Shekelle P, Spratt KF, Weinstein JN. Outcome measures for studying patients with low back pain. Spine. 1994;19:2032S–2036S. doi: 10.1097/00007632-199409151-00003. [DOI] [PubMed] [Google Scholar]
- 7.Dixon S, Bird H. Reproducibility along a 10 cm visual analogue scale. Ann Rheum Dis. 1981;40:87–89. doi: 10.1136/ard.40.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fairbank JCT, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 9.Findlay GF, Hall BI, Musa BS, Oliveira MD, Fear SC. A 10-year follow-up of the outcome of lumbar microdiscectomy. Spine. 1998;15:1168–1171. doi: 10.1097/00007632-199805150-00019. [DOI] [PubMed] [Google Scholar]
- 10.Graven-Nielsen T, Lund H, Arendt-Nielsen L, Danneskiold-Samsoe B, Bliddal H. Inhibition of maximal voluntary contraction force by experimental muscle pain: a centrally mediated mechanism. Muscle Nerve. 2002;26:708–712. doi: 10.1002/mus.10225. [DOI] [PubMed] [Google Scholar]
- 11.Graver V, Haaland AK, Magnaes B, Loeb M. Seven-year clinical follow-up after lumbar disc surgery: results and predictors of outcome. Br J Neurosurg. 1999;13:178–184. doi: 10.1080/02688699943952. [DOI] [PubMed] [Google Scholar]
- 12.Hagg O, Fritzell P, Nordwall A. Swedish Lumbar Spine Study Group. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12:12–20. doi: 10.1007/s00586-002-0464-0. [DOI] [PubMed] [Google Scholar]
- 13.Hartvigsen J, Christensen K, Frederiksen H. Back and neck pain exhibit many common features in old age: a population-based study of 4,486 Danish twins 70–102 years of age. Spine. 2004;29:576–580. doi: 10.1097/01.BRS.0000099394.18994.2F. [DOI] [PubMed] [Google Scholar]
- 14.Hurme M, Alaranta H. Factors predicting the results of surgery for lumbar intervertebral disc herniation. Spine. 1987;12:933–938. doi: 10.1097/00007632-198711000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Krishnan E, Sokka T, Häkkinen A, Hannonen P. Impact of age and comorbidities on the criteria for remission and response in rheumatoid arthritis. Ann Rheum Dis. 2005;64:1350–1352. doi: 10.1136/ard.2005.037903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Loupasis GA, Stamos K, Katonis PG, Sapkas G, Korres DS, Hartofilakidis G. Seven- to 20-year outcome of lumbar discectomy. Spine. 1999;24:2313–2317. doi: 10.1097/00007632-199911150-00005. [DOI] [PubMed] [Google Scholar]
- 17.Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Semmer NK, Jacobshagen N, Dvorak J, Boos N. Outcome assessment in low back pain: how low can you go? Eur Spine J. 2005;14:1014–1026. doi: 10.1007/s00586-005-0911-9. [DOI] [PubMed] [Google Scholar]
- 18.Moore AJ, Chilton JD, Uttley D. Long-term results of microlumbar discectomy. Br J Neurosurg. 1994;8:319–326. doi: 10.3109/02688699409029620. [DOI] [PubMed] [Google Scholar]
- 19.Ostelo R, Vet HC. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol. 2005;19:593–607. doi: 10.1016/j.berh.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 20.Roland M, Fairbank J. The Roland–Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25:3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 21.Roland M, Morris R. A study of the natural history of back pain. Part 1: Development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Stucki G, Sigl M. Assessment of the impact of disease on the individual. Best Pract Res Clin Rheumatol. 2003;17:451–473. doi: 10.1016/S1521-6942(03)00025-1. [DOI] [PubMed] [Google Scholar]
- 23.Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine. 1983;8:131–140. doi: 10.1097/00007632-198303000-00003. [DOI] [PubMed] [Google Scholar]
- 24.WHO (2001) International Classification of Functioning, Disability and Health: ICF, 1st edn. WHO, Geneva
- 25.Wood EG, Hanley EN. Lumbar disc herniation and open limited discectomy: indications, techniques, and results. Oper Tech Orthop. 1991;1:23–28. doi: 10.1016/S1048-6666(05)80003-5. [DOI] [Google Scholar]
- 26.Yorimitsu E, Chiba K, Toyama Y, Hirabayashi K. Long-term outcomes of standard discectomy for lumbar disc herniation: a follow-up study of more than 10 years. Spine. 2001;26:652–657. doi: 10.1097/00007632-200103150-00019. [DOI] [PubMed] [Google Scholar]