Abstract
Last two decades witnessed great advances in the surgical treatment of idiopathic scoliosis. However, the number of studies evaluating the long-term results of these treatment methods is relatively low. During recent years, besides radiological and clinical studies, questionnaires like SRS-22 assessing subjective functional and mental status and life-quality of patients have gained importance for the evaluation of these results. In this study, surgical outcome and Turkish SRS-22 questionnaire results of 109 late-onset adolescent idiopathic scoliosis patients surgically treated with third-generation instrumentation [Texas Scottish Rite Hospital (TSRH) System] and followed for a minimum of 10 years were evaluated. The balance was analyzed clinically and radiologically by the measurement of the lateral trunk shift (LT), shift of head (SH), and shift of stable vertebra (SS). Mean age of the patients was 14.4±1.9 and mean follow-up period was 136.9±12.7 months. When all the patients were included, the preoperative mean Cobb angle of major curves in the frontal plane was 60.8°±17.5°. Major curves that were corrected by 38.7±22.1% in the bending radiograms, postoperatively achieved a correction of 64.0±15.8%. At the last follow-up visit, 10.3°±10.8° of correction loss was recorded in major curves in the frontal plane with 50.5±23.1% final correction rate. Also, the mean postoperative and final kyphosis angles and lumbar lordosis angles were 37.7°±7.4°, 37.0°±8.4°, 37.5°±8.7°, and 36.3°±8.5°, respectively. A statistically significant correction was obtained at the sagittal plane; mean postoperative changes compared to preoperative values were 7.9° and 12.9° for thoracic and lumbar regions, respectively. On the other hand, normal physiological thoracic and lumbar sagittal contours were achieved in 83.5% and 67.9% of the patients, respectively. Postoperatively, a statistically significant correction was obtained in LT, SH, and SS values (P<0.05). Although, none of the patients had completely balanced curves preoperatively, in 95.4% of the patients the curves were found to be completely balanced or clinically well balanced postoperatively. This rate was maintained at the last follow-up visit. Overall, four patients (3.7%) had implant failure. Early superficial infection was observed in three (2.8%) patients. Radiologically presence of significant consolidation, absence of implant failure, and correction loss, and clinical relief of pain were considered as the proof of a posterior solid fusion mass. About ten (9.2%) patients were considered to have pseudoarthrosis: four patients with implant failure and six patients with correction loss over 15° at the frontal plane. About four (3.7%) patients among the first 20 patients had neurological deficit only wake-up test was used for neurological monitoring of these patients. No neurological deficit was observed in the 89 patients for whom intraoperative neurological monitoring with SSEP and TkMMEP was performed. Overall, average scores of SRS-22 questionnaire for general self-image, function, mental status, pain, and satisfaction from treatment were 3.8±0.7, 3.6±0.7, 4.0±0.8, 3.6±0.8, and 4.6±0.3, respectively at the last follow-up visit. Results of about 10 years of follow-up these patients treated with TSRH instrumentation suggest that the method is efficient for the correction of frontal and sagittal plane deformities and trunk balance. In addition, it results in a better life-quality.
Keywords: Idiopathic scoliosis, Surgical treatment, Instrumentation, Long-term follow-up, SRS-22 questionnaire
Introduction
In the last decade, the three-plane deformity concept of idiopathic scoliosis has led to the evolution of spinal instrumentations correcting the deformity in all three planes. Multiple-level fixation with wires or hooks at strategic vertebrae, double rods, and transverse connecting devices have become the state-of-the-art technology in addressing this complex problem [2, 3, 11–13, 15, 16, 18, 20]. Multiple-hook applications to the strategic vertebrae, “claw” applications to the proximal and distal part of the curve, new locking mechanisms, and improved transverse connectors made these systems biomechanically safer and led higher correction rates to be achieved [11, 14, 18, 20, 36, 37, 39, 40]. One of these third-generation systems is Texas Scottish Rite Hospital (TSRH) system [3].
Although, high correction rates with CD instrumentation are reported in scoliosis patients, studies showing de-compensation and imbalance problems have raised concerns about the value of this system, because de-rotational effect also affects neutral vertebrae [30, 36, 37, 42–44, 48]. Technically, the same disadvantages are also relevant for TSRH instrumentation, because selection of strategic vertebrae and corrective maneuvers are similar; however, only a few studies have been reported about this system.
In the present study, the surgical results of 109 idiopathic scoliosis patients treated with TSRH instrumentation are evaluated. Patients were followed-up for a minimum of 10 years. The preoperative, postoperative, and the last follow-up visit values for the frontal plane deformity and sagittal contours, the correctional rates, and the loss of correction are reviewed. In addition, it is investigated whether the abovementioned balance problems had occurred prior to the operation or not, and any change occurred in terms of trunk balance after a minimum 10 years of follow-up was looked for.
Most of the studies with long-term results are referred to the adolescent idiopathic scoliosis patients instrumented with Harrington rod system. These studies also report that Harrington rod system has comparable clinical and radiological results with the modern instrumentation systems, however, the final deformity-correction rates are very small and the overall life-quality at the last follow-up visit is almost unchanged when compared with the third-generation instrumentation systems [17, 21, 23, 24, 26, 31, 32, 47]. Long-term results with the modern systems are limited [5, 21, 23, 26, 29, 33]. It is reported that there is a 7°–17° correction loss in 5–15 years follow-up, but the vertebral stability is maintained and almost no correction loss is observed after two postoperative years [23, 29, 33, 34].
Asher et al. reported minimal correctional loss with the Isola instrumentation system at the long-term follow-up [7, 9]. There is no study in the literature, giving long-term results with the TSRH system.
The public surveys on preoperative and postoperative self-image, pain, function, and the mental status of the patients with idiopathic scoliosis point out the subjective satisfaction of them and their families. These studies also help us to find out the effect of the treatment on the overall life-quality of the patient. The questionnaires like SRS-22, SRS-24, and Short Form-36 are mostly used ones in recent years [4–8, 22, 31, 33, 34, 38, 45, 46]. In the present study, in addition to other outcome measures, the SRS-22 questionnaire adapted to Turkish by Alanay et al. [1] is used to determine the effect of the treatment on the overall quality of life after a long-term follow-up.
Patients and methods
The first TSRH instrumentation in our clinic was performed in September 1991. From September 1991 to November 1994, 109 patients were operated for the treatment of idiopathic scoliosis using TSRH instrumentation. Mean follow-up period was 136.9±12.7 months (120–159 months). About 45 (41.3%) of the patients were male and 64 (58.7%) were female. Mean age of patients at the time of operation was 14.4±1.9 years.
Preoperatively, patients were evaluated in detail by clinical, radiological, and laboratory examinations. Preoperatively, the angles of the major curves were measured by Cobb method by using bending and standing radiograms. On lateral radiograms, sagittal contours between T2–T12 and L1–L5 vertebra were measured, again by Cobb method. Normal thoracic physiological kyphosis and physiological lumbar lordosis were regarded as 25°–40° and 40°–65°, respectively [25]. The curves were grouped according to King classification [27]. Appropriate planning for the use of the third-generation system was done in accordance with the conclusions of the studies reported by Herring and Johnson [3, 37]. Anterior discectomy and release was performed in patients with rigid major curves above 70° with a correction less than 50% in the bending radiograms, and in patients, who had severe vertical structural changes. Disc space at the planned number (minimum three, maximum six) was excised and anterior release was performed. If the rib deformity was significant (>4 cm), thoracoplasty was added to the levels by resecting 2–3 cm of the costa on which discectomy was performed and one- or two-staged posterior instrumentation and fusion was performed. If the curve was flexible of type III or type II and less than 40°, selective thoracic fusion was performed. Selective thoracolumbar and lumbar fusions were done for flexible type-IV and type-I curves, and both curves were included into the fusion and instrumentation area for the real double major type I and type-II curves. The first 38 patients had only hooks and the following 71 patients had both hooks at the thoracic region and transpedicular screws at the thoracolumbar and lumbar region. The upper vertebra where transpedicular screws were placed was T11. All patients underwent a posterior fusion with a mixture of their local and iliac autologous grafts and allogenic bone grafts.
Autologous blood transfusion was done in all patients using the “cell-saver” (electromedics) system. Intraoperatively, the autotransfusion unit saved an average of 820±135 cc of blood, and an average of 1.7±0.8 units of saved blood was transfused. None of these patients needed homologous blood transfusion. The hematocrite value was reduced by 0.7±0.6 mg/dl on average, which was found to be statistically significant (P<0.05). The mean operation time was 1.8±0.9 h. Wake-up test was performed in the first 20 patients. SSEP and “transcranial cortical magnetic stimulation-motor evoked potentials” (TkMMEP) were combined for neuralgic intraoperative monitoring (using the Caldwell-Quantum 80 system) for the last 89 patients of the present study, after it had become available.
Antibiotic prophylaxis was administered in all patients preoperatively with 2 g first-generation cephalosporine or 1 g sulbactam ampicillin and maintained during three postoperative days, dose being reduced to 0.5 g per day. The patients were turned to their sides at the first postoperative day and were seated on the second day. On the third day, they were encouraged to walk. No postoperative cast or brace was utilized.
Balance analysis of patients was done clinically and radiologically. Shoulder asymmetry and distance from the center of gravity measured by a plumb line swinging from C7 and intergluteal crease was determined. In addition, the subjective complaints of the patients were recorded. Three radiological parameters were analyzed on the radiographs taken preoperatively, soon after surgery and at the last follow-up for the analysis of trunk balance: Lateral Trunk shift (LT), Shift of Head (SH), and Shift of Stable vertebra (SS). The LT was measured as the distance from the midpoint of apical vertebra of major curve to the mid-sacral line (MSL). The SH was measured as the distance between the MSL and midpoint of the seventh cervical vertebra. The SS was measured as the distance between midpoint of stable vertebra and the MSL. If SH and SS were close to 0 cm, i.e., if the vertebra is in the middle line, that curve is considered a “completely balanced” one. If the SH and SS are higher than 0 cm but lower than 1 cm, as a clinically recognizable imbalance was not noticed, it was regarded as clinically “balanced.”
The Cobb angles of secondary curves below and above the curves were measured to determine de-compensation. In addition, the effect of surgical treatment on these curves was also investigated.
Last evaluations were done in November 2004 and the patients with a minimum follow-up of 10 years were included in this study. At the last visit, the patients were evaluated clinically, radiologically, and frontal and sagittal plane Cobb angles and correction loss of balance values were noted. Additionally, the subjective complaints of the patients related to balance, implant failure, and other complications were recorded.
At the last follow-up visit, the Turkish SRS-22 questionnaire about self-imaging, pain, function, mental status, and the treatment satisfaction was administered to the patients. There were five questions each for the first four domains and two questions for the treatment satisfaction. All answers were scored from zero to five and the points were added together and later divided to five in order to grade the results over five. It was examined whether the results differ with the curve types. The correlation of the questionnaire scores with the preoperative curve magnitude, postoperative correction rates and the loss of correction at the last follow-up visit were evaluated. Additionally, the patients’ educational (whether continuing or not), occupational, and marital status, and the number of their children (if married) were recorded.
The statistical evaluation was made using the “difference between means for paired observations” test and the “chi-square” test. In addition, correlation-regression test was used for the evaluation of questionnaire results.
Results
Frontal and sagittal plane
When the patients were classified according to King–Moe classification, there were 11 patients with type I, 35 patients with type II, 50 patients with type III, and 13 patients with type IV. Overall, the mean Cobb angle of the major curves at the frontal plane was 60.8°±7.5°. While there was 38.7±22.1% correction in the bending radiograms, the postoperative correction rate (64.0±15.8%) was higher than that was in the bending radiograms with a statistically significant difference (t: 21.3, P<0.01).
The mean postoperative Cobb angle of the major curves improved to 23.2°±13.0° and this was found to be statistically significant (t: 39.5, P<0.01). At the last follow-up visit (mean 136.9±12.7 months), the final rate of correction regressed to 50.5±23.1%, but the difference between the mean final Cobb angle with preoperative value was statistically significant (t: 17.3, P<0.01) (Table 1). The highest correction rate was obtained in type-III curves (68.8±14.7%), followed by type-IV curves (64.5±15.8%) (Figs. 1, 2). When the mean postoperative and final Cobb values are compared with the preoperative ones, there is a statistically significant improvement in all curve types (P<0.01). Overall, the mean-correction loss was 5.3°±5.8°. There was also statistically significant improvement in postoperative and final sagittal contours in all curve types (Table 2). Although, the correction obtained was statistically significant, it was not numerically too high, particularly at thoracic region (for thoracic region: mean 7.9°±18.5°, for lumbar region: mean 12.9°±12.2°). However, when reference range values are considered (for thoracic region: 25°–40°, for lumbar region: 40°–65°), preoperatively 38.5% (42 patients) of the patients had thoracic, 22.9% (25 patients) had lumbar physiological sagittal contours, but postoperatively normal physiological sagittal contours were obtained in 91 of the patients (83.5%) at the thoracic region and in 74 of the patients (67.9%) at the lumbar region. At the last control visit, these rates were maintained.
Table 1.
Frontal plane analysis of the patients with AIS (n: number of the patients)
| Curve type | Preoperative Cobb | Postoperative Cobb | t | P | Postoperative CR (%) | Final Cobb | t | P | Final CR (%) | LC |
|---|---|---|---|---|---|---|---|---|---|---|
| Type I (n: 11) | 60.5°±9.5° | 25.3°±14.8° | 11.8 | <0.01 | 59.8±18.0 | 30.0°±14.8° | 8.61 | <0.01 | 51.5±19.4 | 4.7°±5.6° |
| Type II (n: 35) | 78.9°±17.9° | 35.1°±17.6° | 19.2 | <0.01 | 56.8±16.3 | 42.5°±20.7° | 14.9 | <0.01 | 47.5±18.8 | 7.4°±6.0° |
| Type III (n: 50) | 51.9°±9.9° | 16.8°±9.8° | 33.8 | <0.01 | 68.8±14.7 | 19.9°±9.1° | 28.6 | <0.01 | 62.3±14.3 | 3.1°±4.4° |
| Type IV (n: 13) | 55.4°±14.9° | 20.6°±10.1° | 17.4 | <0.01 | 64.5±10.5 | 27.6°±12.8° | 14.6 | <0.01 | 51.9±12.5 | 7.0°±3.6° |
| Total (n: 109) | 60.8°±17.5° | 23.2°±13.6° | 38.4 | <0.01 | 64.0±15.8 | 28.2°±16.9° | 32.6 | <0.01 | 50.5±23.1 | 10.3°±10.8° |
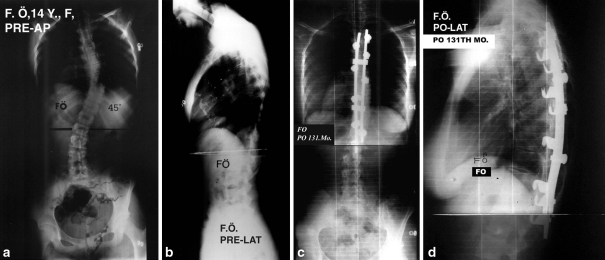
Fig. 1.
The patient (FO) was a 16-year-old girl, with type-III curve. Her preoperative (a, b), and postoperative 131st month follow-up (c, d) PA and lateral radiographies
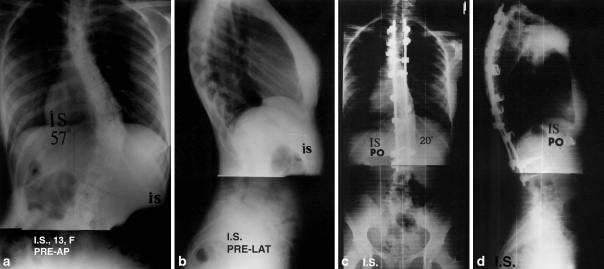
Fig. 2.
The patient (IS) had type-IV curve. Her preoperative (a, b), and postoperative 135th month follow-up (c, d) PA and lateral radiographies
Table 2.
Sagittal plane analysis of the patients
| Type | Preoperative Thoracic Kyphosis | Postoperative Thoracic Kyphosis | Final Kyphosis | Preoperative Lumbar Lordosis | Postoperative Lumbar Lordosis | Final Lumbar Lordosis |
|---|---|---|---|---|---|---|
| Type I (n: 11) | 20.3°±13.6° | 35.4°±5.5° | 35.0°±6.7° | −21.8°±15.4° | −35.2°±11.8° | −35.0°±8.5° |
| Type II (n: 35) | 31.4°±24.4° | 36.9°±6.7° | 36.6°±8.2° | −26.8°±15.4° | −39.6°±8.0° | −38.4°±8.5° |
| Type III (n: 50) | 22.3°±20.6° | 32.0°±10.9° | 31.9°±10.6° | −24.5°±16.2° | −38.0°±8.4° | −36.6°±8.1° |
| Type IV (n: 13) | 31.3°±24.2° | 33.0°±13.9° | 33.7°±14.6° | −21.0°±13.0° | −20.6°±10.9° | −26.0°±10.6° |
| Total (n: 109) | 26.5°±21.0° | 34.4°±9.8° | 33.6°±7.4° | −23.9°±17.3° | −36.9°±10.7° | −35.3°±8.3° |
Balance analysis
The distance between the plumb line and the intergluteal crease was brought to 0.9±0.6 cm postoperatively, while it was 3.7±1.9 cm preoperatively (P<0.01).
Overall, preoperative LT, SS, and SH values of all patients were 37.3±12.7, 18.8±9.5, and 19.8±10.5 mm and postoperative and final correction rates were statistically significant (P<0.01) with minimal loss of correction (Table 3). The correction rates were also statistically significant for all types of curves (P<0.01). Correction rates obtained in LT values correlated the correction rates of Cobb values for the curves in frontal plane.
Table 3.
Trunk balance analysis of the patients
| Types | Preoperative Cobb (secondary curve) | Postoperative Cobb (secondary curve) | t | P | Final Cobb (secondary curve) | t | P |
|---|---|---|---|---|---|---|---|
| Type I | 42.3°±16.5° | 20.9°±11.7° | 6.18 | <0.01 | 25.5°±10.7° | 4.16 | <0.01 |
| Type II | 45.0°±18.2° | 25.6°±13.8° | 10.6 | <0.01 | 28.1°±12.8° | 8.9 | <0.01 |
| Type III | 26.3°±9.5° | 7.6°±9.2° | 15.2 | <0.01 | 8.9°±10.1° | 12.6 | <0.01 |
| Type IV | 28.8°±16.5° | 10.6°±14.3° | 4.9 | <0.01 | 13.0°±14.6° | 3.9 | <0.01 |
| Total | 33.1°±15.9° | 13.1°±13.8° | 20.9 | <0.01 | 16.2°±14.4° | 15.1 | <0.01 |
| Preoperative LT (mm) | Postoperative LT (mm) | t | P | Final LT (mm) | t | P | |
|---|---|---|---|---|---|---|---|
| Type I | 39.3±12.9 | 20.4±9.8 | 5.7 | <0.01 | 23.2±11.1 | 5.4 | <0.01 |
| Type II | 78.4±19.3 | 25.2±13.3 | 14.2 | <0.01 | 27.2±13.5 | 12.4 | <0.01 |
| Type III | 34.5±12.1 | 12.3±8.8 | 23.4 | <0.01 | 14.0±9.5 | 21.3 | <0.01 |
| Type IV | 58.1±30.4 | 23.4±18.4 | 4.5 | <0.01 | 29.4±19.8 | 3.6 | <0.01 |
| Total | 37.3±12.7 | 10.7±7.1 | 18.4 | <0.01 | 12.7±8.3 | 17.5 | <0.01 |
| Preoperative SS (mm) | Postoperative SS (mm) | t | P | Final SS (mm) | t | P | |
|---|---|---|---|---|---|---|---|
| Type I | 26.6±12.7 | 10.2±11.1 | 6.2 | <0.01 | 12.1±10.8 | 5.3 | <0.01 |
| Type II | 25.8±10.6 | 6.8±5.2 | 11.8 | <0.01 | 8.7±5.7 | 10.4 | <0.01 |
| Type III | 12.9±10.3 | 3.5±6.0 | 6.8 | <0.01 | 4.5±6.4 | 6.2 | <0.01 |
| Type IV | 18.8±18.4 | 4.3±6.7 | 3.7 | <0.01 | 7.1±9.2 | 3.5 | <0.01 |
| Total | 18.8±9.5 | 4.2±5.1 | 18.3 | <0.01 | 5.6±5.9 | 17.5 | <0.01 |
| Preoperative SH (mm) | Postoperative SH (mm) | t | P | Final SH (mm) | t | P | |
|---|---|---|---|---|---|---|---|
| Type I | 31.2±25.3 | 10.8±10.5 | 3.7 | <0.01 | 14.2±12.9 | 3.2 | <0.01 |
| Type II | 21.4±10.3 | 3.0±6.8 | 10.8 | <0.01 | 7.6±7.6 | 9.1 | <0.01 |
| Type III | 18.5±9.3 | 2.8±4.0 | 16.5 | <0.01 | 4.3±5.0 | 15.5 | <0.01 |
| Type IV | 30.1±13.8 | 5.7±8.1 | 5.2 | <0.01 | 8.9±7.4 | 4.7 | <0.01 |
| Total | 19.8±10.5 | 3.9±5.4 | 19.5 | <0.01 | 5.6±6.5 | 17.4 | <0.01 |
None of the patients were completely balanced preoperatively. Totally, 22 patients (20.2%) had clinically balanced curves, while 87 patients (79.8%) had abnormal balance patterns. Overall, 43 patients (39.5%) were found to be balanced, while 61 patients (55.9%) had a complete balance in which SS and SH values were brought to zero. The best results were obtained with type-III curves. Totally, 104 of all patients in our series (95.4%) had either a “completely balance” or a “balanced curve.”
Although, the instrumentation had an affirmative effect on the balance values of the curves, imbalance continued in five patients (4.6%) postoperatively. Among these, one of the patients with type-I curves, one of the patients with type-II curves, and one of the patients with type-IV curves had a decrease in SH and SS values, although the imbalance continued. When bending radiograms were re-evaluated, remaining two of the patients with type-III curves that had an increase in SH and SS values were actually found to be type-V curves, because the cervicothoracic major curves were missed. Finally, due to inappropriate planning and application, two (1.8%) patients developed the “imbalance” problems.
As a result, 104 (95.4%) patients were either balanced or completely balanced postoperatively; at the last follow-up visit 99 (90.8%) patients were in this condition. Overall, there were five (4.6%) imbalanced patients postoperatively and this was raised to ten (9.2%) at the final follow-up visit. Five of these five imbalanced patients remained imbalanced. Five of the postoperatively balanced patients had an increase in SS and SH values (>1 cm) and became imbalanced.
Complications
Pseudoarthrosis and implant failure
About two lumbar screws were broken in one patient (0.9%) with type-I curve. As 5° of correction loss and a solid fusion mass was observed in this patient, after 53 months of follow-up, the implants were not removed but revised. Implant failure was noted in three (one rod breakage, one with proximal, and one with distal convex hook dislodgement).
Radiologically, the presence of significant consolidation, absence of implant failure and correction loss, and clinical relief of pain were considered as the proof of a posterior solid fusion mass. About ten (9.2%) patients were considered to have pseudoarthrosis: four patients with implant failure and six patients with correction loss over 15° at the frontal plane. These patients were re-operated and re-fusion was performed. For ten patients with correction loss between 10° and 14°, re-operation was not considered and they were only followed until consolidation was observed radiologically.
Infection
Early superficial infection was observed in three (2.8%) patients. Slight wound opening and serohemorrhagic leakage was seen in these patients and was eradicated with medical treatment and dressing. Deep late-wound infection was seen in one (0.9%) patient and Staphylococcus Aureus was isolated. Sulbactam Ampicillin 0.5 g twice daily was initiated, implants were removed and debridement was performed. After 6 weeks of chemotherapy, infection was totally eradicated and as solid fusion occurred in these patients, revision was not indicated.
Neurological deficit
About Four (3.7%) patients among the first 20 patients had neurological deficit. Only a wake-up test was used for neurological monitoring of these patients. In one patient with type-II curve, late distal paraplegia developed on the second postoperative day, which was attributed to hypovolemia and hypoxia. Implants were removed in the same day and 4×4 g/day dexamethasone was initiated. With active rehabilitation, this patient is now mobilized with walking orthosis. At the last follow-up visit, this patient had 51° correction loss. Implants of the other three patients with neurological deficit were not removed. Two of them totally recovered at the second postoperative week with steroid therapy. In the remaining one patient all neurological deficits were recovered except slight dorsiflexion loss. Later on, tendon transfer to the dorsum of the foot minimized the dorsiflexion loss. No neurological deficit was observed in the 89 patients for whom intraoperative neurological monitoring with SSEP and TkMMEP was performed.
The results of SRS-22 questionnaire
Overall, the average scores of questionnaire for pain, general self-image, function, mental status, and satisfaction from treatment were 3.8±0.7, 3.6±0.7, 4.0±0.8, and 4.6±0.3, respectively, at the last follow-up visit (Table 4). There was no difference between the groups for any of the domains (z: 0.16, P<0.5). Relatively, patients with type-III curves had the best scores. The 89 patients having less than 10° of correction loss had scores of 4 or 5 or over 5 for self-image and mental status irrespective of the curve type, while 20 patients having more than 10° of correction loss had scores 3 or less. In patients with type- III and -IV curves and patients having flexible lumbar curves, self-image and mental status were positively effected and these domains were correlated with the postoperative correction rates (z: 0.422, P<0.001).
Table 4.
The result of SRS-22 questionnaire of the patients
| Type | Self imaging | Mental status | Function | Pain | Satisfaction |
|---|---|---|---|---|---|
| I | 3.8±0.6 | 3.5±0.7 | 3.8±0.8 | 3.5±0.6 | 4.5±0.3 |
| II | 3.6±0.8 | 3.4±0.6 | 3.8±0.8 | 3.4±0.7 | 4.4±0.5 |
| III | 3.9±0.5 | 3.8±0.9 | 4.2±0.5 | 3.8±0.5 | 4.7±0.3 |
| IV | 3.8±0.6 | 3.5±0.6 | 3.9±0.7 | 3.5±0.9 | 4.5±0.4 |
| Total | 3.8±0.7 | 3.6±0.7 | 4.0±0.8 | 3.6±0.8 | 4.6±0.3 |
The pain scores were not correlated with the curve types, final Cobb angle or the amount of correction loss (P>0.01). There were degenerative changes at the uninstrumented sites in the 14 (12.8%) of the patients, who had at least pain complaint for 6 months, but there was no explanation for pain in the remaining 24 (22%) patients. Functional loss was small in patients with neurological deficit and others did not have a clear loss, and the score was three or over in almost all (106) patients. The treatment-satisfaction score was less than 3 in patients, whose implants were removed because of infection and who had 30° of correction loss at the last follow-up due to implant failure, in patients who had 51° correction loss, and in patients had neurological deficit.
All the patients continued their education. About 64 patients (58.4%) living in urban areas found a job and 40 patients living in urban area worked by raising livestock or as a farmhand, but the remaining five were unemployed. About 64 (31.9%) of the patients were married and 12 girls delivered babies by spontaneous vaginal delivery after a normal pregnancy period, three gave birth by cesarean section.
Discussion
The current study is the first in literature with long-term results of the TSRH instrumented idiopathic scoliosis patients. Most of the long-term results in the literature are with the Harrington rod system [23, 24, 32, 47]. Williers et al. reported 40% final correction rate in a 10.8 years follow-up study [47]. Helenius et al. reported relatively lower correction rates with Harrington rod system when compared with the C-D instrumentation [24]. Lespien stated that in 2 years following the operation. the fusion status is completed and vertebral stability is established, meaning no further loss of correction is expected [29].
Many studies with Cotrel–Dubousset system and similarly with TSRH system have reported significant correction of scoliotic curves at all three planes [2, 3, 11–13, 15–17, 19–21, 28]. Also, in our study, when the postoperative values are considered with all patients included, a statistically significant correction was obtained in both frontal (64%) and sagittal planes (P<0.01). Delorme et al. reported the effect of preoperative and intraoperative sagittal contours on postoperative sagittal-plane correction [19]. Benli et al. found no substantial change in the sagittal contours of thoracic region for normokyphotic patients, however they reported a remarkable change in hypokyphotic patients [13]. Rhee et al. suggested that actually correction of the sagittal contours was numerically small [35]. When all the patients are taken into account in our study, the difference between preoperative and postoperative contours was not numerically very high, however the correction was statistically significant. Postoperatively 83.5% had excellent thoracic balance and corresponding figure was 67.9% for lumbar region.
In the present study, the mean final Cobb values were significantly improved during a minimum 10 years follow-up period and the mean final correction rate for the major curves were found to be 56.7±17.7%. The mean loss of correction was 9.1°±11.9°. The loss of correction is higher in patients, whose implants had to be removed before 2 years postoperatively due to infection or neurological deficit. There was no significant difference in terms of sagittal contours; and the postoperative normal physiological sagittal contours were maintained at the final follow-up visit.
By Cotrel–Dubousset system, de-rotation maneuver was introduced to spinal surgery, but during the following years de-compensation and imbalance problems due to the redirection of rotational effect to the stable vertebral levels were reported regarding this maneuver [30, 42–44, 48]. According to Bridwell, de-compensation is mainly the result of inability to detect, or inappropriately select the fusion levels of the double major curves and due to the progression of the structural lumbar and upper thoracic curves [16]. Benli et al. reported that over-correction and neglected structural upper thoracic curves resulted in imbalance and de-compensation problems particularly in King type-III curves [13].
There are limited number of studies with third-generation systems investigating whether imbalance problems continue or not during long-term follow-up. This study has also examined the long-term results for trunk balance. At the last follow-up visit, the ratio of “completely balanced” patients reduced to 48.6% but the ratio of “balanced” patients improved to 42.2%, thus an overall 9.2% of patients being “unbalanced.” Totally, 90.8% of patients were “completely balanced” or “balanced” at the last control visit, similar to postoperative values. The imbalance problems occurred due to the loss of correction. As a result, the postoperative correction rates in the sagittal and frontal planes with the TSRH instrumentation are almost maintained in the long term with a minimum loss of correction; and although the balance values decreased a little, the number of patients with postoperative trunk balance remained the same.
Recently, a subjective questionnaire is also being used in addition to the clinical and radiological assessment when evaluating scoliosis patients. This questionnaire also puts forth the change in patient’s life-quality into consideration [4–8, 31, 38]. Long-term results of treatment with Harrington rods give no significant change in patients’ life-qualities [21, 32]. When the questionnaire is applied both preoperatively and postoperatively, the changes in domains like self-image, pain, function, and mental status can also be evaluated. Merola et al. in a multicenter study of seven different institutions reported an average score of 3.68/5.00 at 24 months and the improvements in the scores were statistically significant [31]. There are also studies on different scoring types and the unique questionnaires developed for each country and languages [5–7, 10]. In the current study, the SRS-22 questionnaires adapted to Turkish by Alanay et al. (also co-author of this study) was used [1]. In our study, overall mean values for pain, general self-image, function, mental status, and satisfaction were 3.8±0.7, 3.6±0.7, 4.0±0.8, and 4.6±0.3, respectively, at the last control visit.
Asher et al. stated in their studies that in idiopathic scoliosis patients treated with Isola instrumentation, the self-imaging scores raised at 3rd and 24th months while the function scores lowered at the 3rd month, returned to the baseline at the 6th month and raised again at the 24th month. They also stated a reverse correlation between postoperative curve magnitude and the scores [6, 7]. In our study, no significant difference was found among different curve types for any domain (P>0.05). In curve type III: single thoracic, with more flexible and less preoperative Cobb angles relatively the best scores were obtained; and this seemed to support the correlation between the preoperative curve magnitude and the scores. Haher et al. reported in their meta analysis of 11,000 patients followed for 35 years that patient satisfaction rate increases with increased surgical correction rate [22]. In our study, we found that in curves as types III, IV and lumbar flexible types self-imaging, and mental status scores were positively affected and these domains correlated with the postoperative correction rates. Additionally, when the correctional loss was less than 10°, the self-imaging and mental status scores were better than the patients with a correctional loss more than 10°. This was thought to be a reverse correlation of these domains with the correctional losses.
White et al. reported the effect of fusion rates on pain scores, and Peres Gruesco et al. stated in their CD instrumented 10 year follow-up study that the changes causing pain was not different than the normal population [33, 45, 46]. Takahashi et al. reported 23% degenerative changes at the uninstrumented lumbar site in 5–9 years follow-up [41].
In the present study, it is also found that the pain score is not correlated with the final Cobb angle and the loss of correction (P>0.01). When the patients with pain were evaluated, it was found that in 14 of the patients having at least 6 months of pain, degenerative changes at the uninstrumented site was responsible for the pain. In the remaining 24 patients no cause for the pain was identified, so mechanical problems, like perivertebral muscle pain, were thought to be the reason.
White et al. reported that surgery improved functional scores [45]. The functional limitations were small in the patients with neurological deficit; the others did not have a significant limitation and in most of the patients the functional scores were four over five.
Rinella et al. stated that as the follow-up period got longer and the patients’ ages got older the satisfaction from the treatment increased, but the final curve status did not correlate with the satisfaction level [38]. Asher et al. reported that the trunk deformity at the last control visit did not correlate with the treatment-satisfaction level [4]. Haher et al. also reported that the radiological status did not correlate with the satisfaction level [22]. In our study, similar to these studies, the treatment-satisfaction scores did not correlate with the curve types and the loss of correction, and almost all patients (106 patients) had scores three or over. The patients with implant removal because of infection, having 30° of correction loss at the last follow-up visit because of implant failure, having implant removal because of neurological deficit, and having 51° of correction loss had treatment-satisfaction scores less than 3. The patients had high treatment-satisfaction scores irrespective of their final curve patterns, and all but one with neurological deficit said “yes” when asked if they would have accepted the same course of treatment.
In our study, patients could successfully continue their education, occupational life, and marriage.
Conclusion
With TSRH instrumentation, postoperatively significantly high correction rates were obtained at the frontal plane and physiological contours were achieved for all curve types. In all curve types, lateral shift of apical, stable vertebrae, and head had a statistically significant correction. Postoperatively, great majority of the patients (95.4%) were either “balanced” or “completely balanced.” At long-term follow-up, the frontal and sagittal plane correctional rates were maintained with minimal loss of correction. The postoperative trunk balance was also maintained after a minimum of 10 years follow-up. The results of the SRS-22 questionnaire results showed that TSRH instrumentation was successful in deformity correction, as well as its positive effects on the self-imaging, mental status, function, and pain domains of the patients. Additionally, the questionnaire scores for self-imaging, mental status, and function domains had a reverse correlation with the preoperative curve magnitude and loss of correction, while they were correlated with the postoperative correction rates. Most of the patients were satisfied with the treatment, and the satisfaction level did no correlate with the curve status at the last control visit. The treatment improved the patients’ life-quality and did not have a negative effect on their education, occupation, and marriage.
Acknowledgments
The authors thank John A. Herring M.D. for helpful review and Joanna Husouski and Nur Sozudogru for professional editing of our manuscript.
References
- 1.Alanay A, Cil A, Berk H, Acaroğlu RA, Yazıcı M, Akcalı O, Kosay C, Genc Y, Surat A (2005) Reliability and validity of adapted Turkish version of Scoliosis Research Society-22 (SRS-22) questionnaire. Spine 30 (in press) [DOI] [PubMed]
- 2.Antuno SA, Mendez JG, Lopez-Fanjul JC, Paz-Jimenez J. Cotrel-dubousset instrumentation in idiopathic scoliosis at 5-year follow-up. Acta Orthop Belg. 1997;63:74–81. [PubMed] [Google Scholar]
- 3.Ashman RB, Herring JA, Johnston CE. Texas Scottish Rite Hospital (TSRH) instrumentation system. In: Bridwell KH, DeWald R, editors. The textbook of spinal surgery. Philadelphia: JB Lippincott Co; 1992. pp. 219–248. [Google Scholar]
- 4.Asher M, Min Lai S, Burton D, Manna B. Spine deformity corraletes beter than trunk deformity with idiopathic scoliosis patients’ quality of life questionnaire responses. Stud Health Technol Inform. 2002;91:462–464. [PubMed] [Google Scholar]
- 5.Asher M, Min Lai S, Burton D, Manna B. The reliability and concurrent of the scoliosis research society—22 patient questionnaires for idiopathic scoliosis. Spine. 2003;28(1):36–69. doi: 10.1097/00007632-200308011-00007. [DOI] [PubMed] [Google Scholar]
- 6.Asher M, Min Lai S, Burton D, Manna B. Scoliosis research society—22 patient questionnaire: responsiveness to change associated with surgical treatment. Spine. 2003;28(1):70–73. doi: 10.1097/00007632-200301010-00016. [DOI] [PubMed] [Google Scholar]
- 7.Asher M, Min Lai S, Burton D, Manna B. Discrimination validity of the scoliosis research society—22 patient questionnaire: relationship to idiopathic scoliosis curve pattern and curve size. Spine. 2003;28(1):74–78. doi: 10.1097/00007632-200301010-00017. [DOI] [PubMed] [Google Scholar]
- 8.Asher M, Min Lai S, Burton D, Manna B. The influence of spine and trunk deformity on preoperative idiopathic scoliosis patients’ health-related quality of life questionnaire responses. Spine. 2004;29(8):861–868. doi: 10.1097/00007632-200404150-00008. [DOI] [PubMed] [Google Scholar]
- 9.Asher M, Lai SM, Burton D, Manna B, Cooper A. Safety and efficacy of Isola instrumentation and arthrodesis for adolescent idiopathic scoliosis: two- to 12-year follow-up. Spine. 2004;29(18):2013–2023. doi: 10.1097/01.brs.0000138275.49220.81. [DOI] [PubMed] [Google Scholar]
- 10.Bago J, Climent JM, Ey A, Perez-Grueso FJ, Izquierdo E. The spanish version of the SRS-22 patient questionnaire for idiopatic scoliosis: transcultural adaptation and reliability analysis. Spine. 2004;29(15):1676–1680. doi: 10.1097/01.BRS.0000132306.53942.10. [DOI] [PubMed] [Google Scholar]
- 11.Benli IT, Akalin S, Tuzuner MM, Tandogan NR, Citak M, Mumcu EF (1994) Three-dimensional analysis treated with Cotrel-Dubousset Instrumentation. GICD’93, Sauramps Medical, Montpellier, pp 26–35
- 12.Benli IT, Tuzuner M, Akalin S, Kis M, Aydin E, Tandogan R. Spinal imbalance and decompensation problems in patients treated with Cotrel-Dubousset instrumentation. Eur Spine J. 1996;5:380–386. doi: 10.1007/BF00301965. [DOI] [PubMed] [Google Scholar]
- 13.Benli IT, Akalın S, Kıs M, Cıtak M, Aydın E, Duman E. Frontal and sagittal balance analysis of late onset idiopathic scoliosis treated with third generation instrumentation. Kobe J Med Sci. 2001;47:231–253. [PubMed] [Google Scholar]
- 14.Bridwell KH, Betz R, Capelli AM, Hum G, Harvey C (1989) Sagittal plane analysis in idiopathic scoliosis patients treated with Cotrel-Dubousset instrumentation. In: Sixth International Congress on CDI, Sauramps Medical, Montpellier, pp 65–71
- 15.Bridwell KH. Spine update. Surgical treatment of adolescent idiopathic scoliosis: the basics and the controversies. Spine. 1994;19:1095–1100. doi: 10.1097/00007632-199405000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Bridwell KH. Spinal instrumentation in management of adolescent idiopathic scoliosis. Clin Orthop Rel Res. 1997;335:64–72. [PubMed] [Google Scholar]
- 17.Bridwell KH, Hanson DS, Rhee JM, Lenke LG, Baldus C, Blanke K. Correction of thoracic adolescent idiopathic scoliosis with segmental hooks, rods, and Wisconsin wires posteriorly: it’s bad and obsolete, correct? Spine. 2002;27(18):2059–2066. doi: 10.1097/00007632-200209150-00018. [DOI] [PubMed] [Google Scholar]
- 18.Chopin D, Morin C. Cotrel-Dubousset instrumentation (CDI) for adolescent and pediatric scoliosis. In: Bridwell KH, DeWald RL, editors. The textbook of spinal surgery. Philadelphia: JB Lippincott Company; 1992. pp. 183–217. [Google Scholar]
- 19.Delorme S, Labelle H, Poitras B, Rivard CH, Coillard C, Dansereau J. Pre-, intra-, and postoperative three-dimensional evaluation of adolescent idiopathic scoliosis. J Spinal Disord. 2000;13(2):93–101. doi: 10.1097/00002517-200004000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Dubousset J, Cotrel Y. Application technique of Cotrel-Dubousset instrumentation for scoliosis deformities. Clin Orthop Rel Res. 1991;264:103–110. [PubMed] [Google Scholar]
- 21.Gotze C, Liljenqvist UR, Slomka A, Gotze HG, Steinbeck J. Quality of life and back pain: outcome 16.7 years after Harrington instrumentation. Spine. 2002;27(13):1456–1463. doi: 10.1097/00007632-200207010-00016. [DOI] [PubMed] [Google Scholar]
- 22.Haher TR, Merola A, Zipnick RI, Gorup J, Mannor D, Orchowski J. Meta-analysis of surgical outcome in adolescent idiopathic scoliosis. A 35-year English literature review of 11,000 patients. Spine. 1995;20(14):1575–1584. doi: 10.1097/00007632-199507150-00005. [DOI] [PubMed] [Google Scholar]
- 23.Haher TR, Gourup JM, Shin TM, Homel P, Merola AA, Grogan DP, Pugh L, Lowe TG, Murray M. Results of the scoliosis research society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis. A multicenter study of 244 patients. Spine. 1999;24(14):1435–1440. doi: 10.1097/00007632-199907150-00008. [DOI] [PubMed] [Google Scholar]
- 24.Helenius I, Remes V, Yrjonen T, Ylikoski M, Schlenka D, Helenius M, Poussa M. Comparison of long-term functional and radiologic outcomes after Harrington instrumentation and spondylodesis in adolescent idiopathic scoliosis: a review of 78 patients. Spine. 2002;27(2):176–180. doi: 10.1097/00007632-200201150-00010. [DOI] [PubMed] [Google Scholar]
- 25.Herring JA. Tachdjian’s pediatric orthopaedics. 3rd. Philadelphia: WB Saunders Company; 2002. p. 326. [Google Scholar]
- 26.Jeng CL, Sponseller PD, Tolo VT. Outcomes of wisconsin instrumentation in idiopathic scoliosis. Minimum 5-year follow-up. Spine. 1993;18(12):1584–1590. doi: 10.1097/00007632-199309000-00003. [DOI] [PubMed] [Google Scholar]
- 27.King HA. Selection of fusion levels for posterior instrumentation and fusion in idiopathic scoliosis. Orthop Clin North Am. 1988;19:247–55. [PubMed] [Google Scholar]
- 28.Labelle H, Dansereau J, Bellefleur C, Poitras B, Rivard CH, Stokes IA, DeGuise J. Comparison between preoperative and postoperative three –dimensional reconstructions of iddiopathic scoliosis with the Cotrel-Dubousset procedure. Spine. 1995;20(23):2487–2492. doi: 10.1097/00007632-199512000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Lepsien U, Bullmann V, Hackenberg L, Liljenqvist U (2002) Long-term results of posterior correction and fusion of scoliosis using the Cotrel-Dubousset instrumentation. Z Orthop Ihre Grenzgeb 140(1):77–82 (abstract) [DOI] [PubMed]
- 30.Mason DE, Carango P. Spinal decompensation in Cotrel-Dubousset instrumentation. Spine. 1991;16:S394–S403. doi: 10.1097/00007632-199108001-00018. [DOI] [PubMed] [Google Scholar]
- 31.Merola AA, Haher TR, Brkariç M, Panagopoulos G, Mothur S, Kohani U, Lowe TG, Lenke LG, Wenger DR, Newton PO, Clements DH, Betz RR. A multicenter study of the outcomes of the surgical treatment of adolescent idiopathic scoliosis using the scoliosis research society (SRS) outcome instrument. Spine. 2002;27(18):2046–2051. doi: 10.1097/00007632-200209150-00015. [DOI] [PubMed] [Google Scholar]
- 32.Padua R, Padua S, Aulisa S, Ceccarelli E, Padua L, Romanini E, Zanoli G, Campi A. Patient outcomes after Harrington instrumentation for idiopathic scoliosis: a 15- to 28- year evaluation. Spine. 2001;26(11):1268–1273. doi: 10.1097/00007632-200106010-00019. [DOI] [PubMed] [Google Scholar]
- 33.Perez-Grueso FS, Fernandez-Baillo N, Arauz Robles S, Garcia Fernandez A. The low lumbar spine below Cotrel-Dubousset instrumentation: long term findings. Spine. 2000;25(18):2333–2341. doi: 10.1097/00007632-200009150-00011. [DOI] [PubMed] [Google Scholar]
- 34.Remes V, Helenius I, Schlenzka D, Yrjonen T, Ylikoski M, Poussa M. Cotrel–Dubousset (CD) or universal spine system (USS) instrumentation in adolescent idiopathic scoliosis (AIS): comparison of midterm clinical, functional, and radiologic outcomes. Spine. 2004;29(18):2024–2030. doi: 10.1097/01.brs.0000138408.64907.dc. [DOI] [PubMed] [Google Scholar]
- 35.Rhee JM, Bridwell KH, Won DS, Lenke LG, Chotigavanichaya C, Hanson DS. Sagittal plane analysis of adolescent scoliosis: the effect of anterior versus posterior instrumentation. Spine. 2002;27(21):2350–2356. doi: 10.1097/00007632-200211010-00008. [DOI] [PubMed] [Google Scholar]
- 36.Richards BS, Birch JG, Herring JA, Johnston CE, Roach JW. Frontal plane and sagittal plane balance following Cotrel-Dubousset instrumentation for idiopathic scoliosis. Spine. 1989;14:733–737. doi: 10.1097/00007632-198907000-00015. [DOI] [PubMed] [Google Scholar]
- 37.Richards BS, Herring JA, Johnston CE, et al. Treatment of adolescent idiopathic scoliosis using Texas Scottish rite hospital instrumentation. Spine. 1994;19:1598–1605. doi: 10.1097/00007632-199407001-00008. [DOI] [PubMed] [Google Scholar]
- 38.Rinella A, Lenke L, Peelle M, Edwards C, Bridwell KH, Sides B. Comparison of SRS questionnaire results submitted by both parents and patients in the operative treatment of idiopathic scoliosis. Spine. 2004;29(3):303–310. doi: 10.1097/01.BRS.0000106489.03355.C5. [DOI] [PubMed] [Google Scholar]
- 39.Sawatzky BJ, Tredwell SJ, Jang SB, Black AH. Effect of three-dimensional assessment on surgical correction and hook strategies in multi-hook instrumentation for adolescent idiopathic scoliosis. Spine. 1998;23:201–205. doi: 10.1097/00007632-199801150-00010. [DOI] [PubMed] [Google Scholar]
- 40.Shufflebarger JL, Crawford AH. Is Cotrel-Dubousset instrumentation the treatment of choice for idiopathic scoliosis in the adolescent who has an operative thoracic curve? Orthopaedics. 1988;11:1579–1588. doi: 10.3928/0147-7447-19881101-12. [DOI] [PubMed] [Google Scholar]
- 41.Takahashi S, Delecrin J, Passuti N. Changes in the unfused lumbar spine in patients with idiopathic scoliosis. A 5- to 9-year assessment after Cotrel-Dubousset instrumentation. Spine. 1997;22(5):517–523. doi: 10.1097/00007632-199703010-00009. [DOI] [PubMed] [Google Scholar]
- 42.Thompson GH, Willbur RE, Shaffer JW, et al. Segmental spinal instrumentation in idiopathic scoliosis: a preliminary report. Spine. 1985;10:623–630. doi: 10.1097/00007632-198509000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Thompson JP, Transfeldt EE, Bradford DS, Ogilvie JW, Boachie-Adjei O. Decompensation after Cotrel-Dubousset instrumentation of idiopathic scoliosis. Spine. 1990;15:927–931. doi: 10.1097/00007632-199009000-00017. [DOI] [PubMed] [Google Scholar]
- 44.Transfeldt E, Thompson J, Bradford D (1989) Three dimensional changes in the spine following CDI for adolescent idiopathic scoliosis. In: Proceedings of the 6th international congress on Cotrel-Dubousset instrumentation, Sauramps Medical, Montpellier, pp 73–80
- 45.White SF, Asher MA, Lai SM, Burton DC. Patients’ perceptions of overall function, pain, and appearanca after primary posterior instrumentation and fusion for idiopathic scoliosis. Spine. 1999;24(16):1693–1699. doi: 10.1097/00007632-199908150-00011. [DOI] [PubMed] [Google Scholar]
- 46.White SF, Asher MA, Lai SM, Burton DC. Patients’ perception of overall function, pain, and appearance after primary posterior instrumentation and fusion for idiopathic scoliosis. Discussion. Spine. 1999;24(16):1699–1700. doi: 10.1097/00007632-199908150-00011. [DOI] [PubMed] [Google Scholar]
- 47.Willers U, Hedlund R, Aaro S, Normelli H, Westman L. Long-term results of Harrington instrumentation in idiopathic scoliosis. Spine. 1993;18(6):713–717. doi: 10.1097/00007632-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 48.Wood KB, Obewski JM, Schendel MS, Boachie-Adjei O, Gupta M. Rotational changes of the vertebral pelvis axis after sublaminar instrumentation in adolescent idiopathic scoliosis. Spine. 1997;22:51–57. doi: 10.1097/00007632-199701010-00009. [DOI] [PubMed] [Google Scholar]