Abstract
Percutaneous endoscopic lumbar discectomy (PELD) for migrated disc herniations is technically demanding due to the absence of the technical guideline. The purposes of this study were to propose a radiologic classification of disc migration and surgical approaches of PELD according to the classification. A prospective study of 116 consecutive patients undergoing single-level PELD was conducted. According to preoperative MRI findings, disc migration was classified into four zones based on the direction and distance from the disc space: zone 1 (far up), zone 2 (near up), zone 3 (near down), zone 4 (far down). Two surgical approaches were used according to this classification. Near-migrated discs were treated with “half-and-half” technique, which involved positioning a beveled working sheath across the disc space to the epidural space. Far-migrated discs were treated with “epiduroscopic” technique, which involved introducing the endoscope into the epidural space completely. The mean follow-up period was 14.5 (range 9–20) months. According to the Macnab criteria, satisfactory results were as follows: 91.6% (98/107) in the down-migrated discs; 88.9% (8/9) in the up-migrated discs; 97.4% (76/78) in the near-migrated discs; and 78.9% (30/38) in the far-migrated discs. The mean VAS score decreased from 7.5 ± 1.7 preoperatively to 2.6 ± 1.8 at the final follow-up (P < 0.0001). There were no recurrence and no approach-related complications during the follow-up period. The proposed classification and approaches will provide appropriate surgical guideline of PELD for migrated disc herniation. Based on our results, open surgery should be considered for far-migrated disc herniations.
Keywords: Percutaneous endoscopic lumbar discectomy, Migrated disc herniation, Radiologic classification
Introduction
Beginning in 1973, Kambin introduced the concept of indirect decompression of the spinal canal via a posterolateral approach using a Craig cannula for evacuation of a protruded disc [5]. Hijikata in 1975 described the first percutaneous discectomy [3]. Since then, many surgeons have developed new techniques for percutaneous endoscopic discectomy [7, 10, 11].
Currently, percutaneous endoscopic lumbar discectomy (PELD) is growing in popularity for the treatment of disc herniation. With advances in instrumentation including endoscopes and side-firing Ho:YAG laser, the range of indications for PELD has expanded. The procedure offers several theoretical advantages over conventional open surgery. Most current percutaneous discectomy techniques are based on the Kambin’s transforaminal approach and offers favorable outcomes for soft disc herniation [1, 2, 4, 6, 13].
Although some authors suggested the anatomic classification of the disc herniation in relation to the lumbar vertebral body, an illustrative technical explanation of the removal of a migrated fragment of soft disc is lacking [9, 12]. The purposes of this study were to propose an anatomic classification of disc migration and surgical approaches of PELD.
Clinical materials and methods
Patient population
The present study was approved by our Institutional Review Board, and all patients provided informed consent. The study population consisted of 116 consecutive patients with radiculopathy due to migrated disc fragments who were treated with PELD by a single surgeon (S. L). The inclusion criteria were as follows: (1) neurological signs including radiculopathy, sensory changes, motor weakness and the presence of abnormal reflex due to migrated disc at a single-level (more than one of the above signs); (2) symptoms corresponding with preoperative magnetic resonance (MR) images and computed tomography (CT) scans; (3) unsuccessful conservative treatment including root blocks and analgesics for at least 4 weeks; (4) no past history of back surgery; (5) an age of 18–65 years. The exclusion criteria were as follows: (1) central stenosis (less than 10 mm) or lateral recess stenosis (less than 3 mm) confirmed by MR imagings and CT scans; (2) a narrowing foramen (less than 7 mm); (3) a combined endplate fracture; (4) sequestered disc below the center of the pedicle of the lower vertebral body; and (5) segmental instability confirmed by dynamic radiographs.
Preoperative and postoperative MR images were obtained in all patients. Postoperative MR images were taken immediately after procedure to ensure adequate removal of the migrated disc. Clinical follow-ups were taken at the end of a month, 3 months, and a year. The clinical outcome was assessed by an independent surgeon (S.H.L) using the Macnab criteria [8]. It was defined that excellent outcome as there is no pain and no limitation of normal life; good outcome as there is occasional pain or paresthesia, but no need medication, and no limitation of normal life; fair outcome as pain is somewhat improved but needs medication, and some limitation of normal life; poor outcome as no improvement or worsening, additional operation is needed due to incomplete decompression, development of instability. Excellent and good outcomes were rated as clinical success.
The intensity of leg pain was measured by a visual analog scale (VAS), ranging from no pain (point 0) to worst pain imaginable (point 10).
Radiologic classification
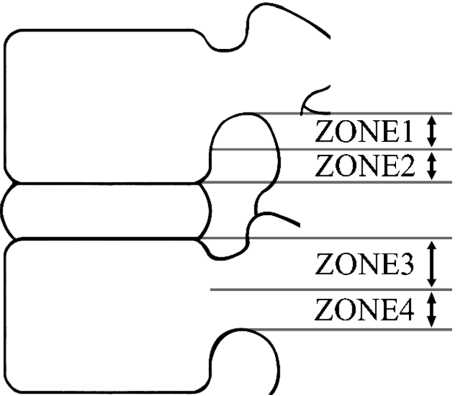
According to preoperative sagittal MR images, disc migration was classified into four zones depending on the direction and distance from the disc space (Table 1; Fig. 1).
Table 1.
Radiologic classification of migrated disc herniations
| Zone | Direction | Range of distance |
|---|---|---|
| Zone 1 | Far-upward | From the inferior margin of upper pedicle to 3 mm below of the inferior margin of upper pedicle |
| Zone 2 | Near-upward | From 3 mm below of the inferior margin of upper pedicle to the inferior margin of upper vertebral body |
| Zone 3 | Near-downward | From the superior margin of lower vertebral body to the center of lower pedicle |
| Zone 4 | Far-downward | From the center to the inferior margin of lower pedicle |
Fig. 1.
Schematic representation of the four anatomic zones and levels of disc herniation
Surgical techniques
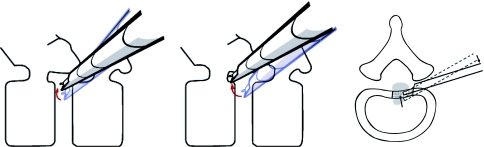
Two surgical approaches are used on the basis of this classification. One is designed for near-migrated discs and is termed as the “half-and-half” technique (Fig. 2, left). In this technique, a beveled working sheath (YESS system; Richard Wolf, Knittlingen, Germany) is positioned across the disc space to the epidural space. The other is the “epiduroscopic” technique used for far-migrated discs, in which we move the working sheath completely into the epidural space from the disc space and no part of the cannula tip is positioned in the disc space (Fig. 2, middle). The major difference between these two approaches is the extent to which the working sheath is introduced into the epidural space, i.e., partially or completely.
Fig. 2.
Illustration of the technique used. Left the “half-and-half” technique involves positioning the window of beveled working sheath across the disc space to the epidural space. It stars from the disc space (blue line). The tip of the working tube is lifted to the direction of the epidural space (black line). Middle the “epiduroscopic” technique involves introducing an endoscope completely into the epidural space. Initial procedure is done from the disc space (blue line). Finally, the working cannula goes over the outer surface of the annulus completely and moves toward the migrated fragment. Therefore, lateral window faces the targeting mass (black line). These two approaches are possible after release of the annulus and removal of inferior part of superior articular process. Right the annulus, which traps the disc fragment, is removed so that the tip of the working sheath is readily advanced over the posterior vertebral body level. The disc material which is located in the epidural space can be removed easily. It is usually performed from inside to outside. The dotted line indicates the original position of the working sheath and the solid line is the migrated position after annular release
Surgical procedures are based on conventional transforaminal endoscopic approach using the YESS endoscope. All the procedures are performed in prone position under local anesthesia. An imaginary line drawn to the annular puncture site through the foramen designates the skin entry point and surgical trajectory. Basically it is parallel to the disc space. According to this guideline, the entry point is 9–13 cm from the mid-line to Korean patients. Under fluoroscopic guidance, an 18-G needle is inserted. The ideal position of the needle tip just prior to puncture of the disc is on the posterior vertebral body line on the lateral C-arm view, and on the medial pedicular line on the anteroposterior (AP) view, especially below the L3/4 level. This should be correspond to the safe triangle in the axillary area between the exiting and traversing nerve root [10]. The location of nerve roots and the safe triangle are confirmed with the use of epidurogram with radio–opaque dye. Then, an obturator is used to introduce the beveled working sheath with lateral window into the disc space. For the removal of extruded disc fragments, the working sheath should have a lateral window. The window opens forward the targeting mass and moves to the target mass. At this point, a small amount of disc is removed using large forceps to create working space. Approximately one third of posterior nucleus pulposus and annulus are removed before the ruptured fragment removal. This provides adequate room for effective handling of the working sheath. All of these procedures start from the disc space. To bring the opening of the working tube to the epidural space, annular release is the key procedure. Then, the tip of the working tube is lifted to the direction of the epidural space (Fig. 2, right). Without annular release it is difficult for surgeon to lever-up the working sheath to the direction of the epidural space. Annular release is usually performed from inside (medial side) to outside (lateral side). For this procedure, additional foraminoplasty is needed in patients with a small foraminal size and/or far-migrated disc herniation (zones 1 and 4) (Fig. 2, left and middle). Epidural bleeding is controlled with the use of a bipolar coagulator (Ellman®; Ellman International LLC, USA) under cold saline irrigation. The side-firing laser is helpful for annular release and foraminoplasty. The well-decompressed nerve roots are confirmed by visualization of the thecal sac and nerve root pulsation following respiration and valsalva.
Near-migrated disc herniation (zones 2 and 3)
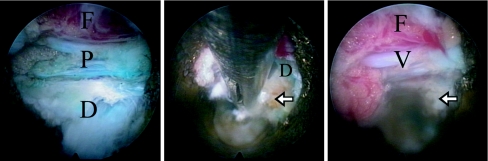
The “half-and-half” technique is sufficient to remove near-migrated disc fragments under the endoscopic view. The working sheath should be moved along the direction of the migrated disc. If the half of the working sheath is placed beyond the posterior vertebral bodyline (properly under the herniated mass), disc fragments will be dropped into the working sheath and can easily be removed using forceps (Fig. 3, left). Therefore the release of the annulus and the posterior longitudinal ligament (PLL) is a key procedure for free movement of the working sheath. Moreover, the annulus usually traps the ruptured nucleus pulposus. Endoscopic views are shown in Fig. 4. The working sheath is positioned across the disc space to the epidural space (Fig. 4, left). After the annular release, the tip of the working sheath is advanced to the epidural space. Then, the extruded disc can be removed using forceps (Fig. 4, middle). Finally, the traversing nerve root and epidural fat remain unimpeded (Fig. 4, right).
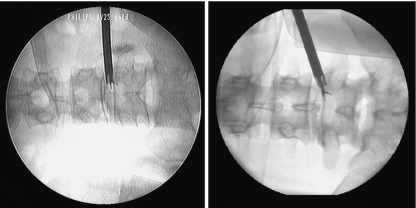
Fig. 3.
Intraoperative C-arm views for down-migrated discs. Left annular release allows the forceps to enter the epidural space. With the “half-and-half” technique, the fragment located at zone 3 can be removed. Right after foraminoplasty, the working sheath can be completely advanced to the epidural space so that the fragment at zone 4 can be removed
Fig. 4.
Intraoperative endoscopic views. Left initial appearance of the “half-and-half” technique: the working sheath is positioned across the disc space to the epidural space. Middle after annular release, the tip of the working sheath is advanced to epidural space. The extruded disc can be removed by forceps. Right final appearance. The arrow indicates the posterior margin of the vertebral body. (D herniated disc stained by indigo carmine, F epidural fat, P posterior longitudinal ligament, V epidural veins)
Far-migrated disc herniation (zones 1 and 4)
The “epiduroscopic” technique is necessary for far-migrated disc. If the disc is not sequestered, it can be grabbed at the proximal end by forceps. However, if the migrated disc is broken into pieces, the “epiduroscopic” technique should be combined with foraminoplasty. Therefore, “epiduroscopic” technique provides sufficient epidural access of endoscope and forceps. The working sheath should be placed in the direction of the migrated disc (Fig. 3, right). Direct approach to the epidural space without violation of disc may be very dangerous. So, all procedures start from the disc space. As it is mentioned earlier, the annular cutting procedure is also essential for achieving proper access to the fragment.
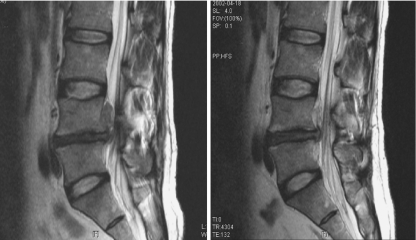
To complete endoscopic approach to the epidural space, the size of the foramen must large enough. Generally, additional foraminoplastic procedures were not need in the upper lumbar level. But lower lumbar usually needed foraminoplasty for this approach. Foraminal ligaments and the foraminal part of the superior facet should be removed using laser and the bone cutter (Shaded area in Fig. 2, middle). A widened foramen allows comfortable access to pathologic lesion. All the steps for foraminoplasty and insertion of the working sheath must be performed under endoscopic view. A clinical case with up-migrated disc is illustrated in Fig. 5. The upward migrated disc was located at zone 1 from the foraminal area to the paramedian area (Fig. 5, left). Annular release was performed from inside to outside and the forceps was gradually approached to the main migrated disc fragment. The far-migrated disc fragment totally disappeared after surgery (Fig. 5, right).
Fig. 5.
Comparison of magnetic resonance images before (Left) and after the procedure (Right). Left the up-migrated disc fragment (zone 1). Right the far-migrated disc fragment totally disappeared
Results
There were 73 males and 43 females, with a mean age of 35.5 (range 18–65) years. The mean follow-up period was 14.5 (range 9–20) months. The L4-5 disc was the most commonly herniated level (65 cases, 56.0%) followed by L5-S1 (47 cases, 40.5%), L3-4 (3 cases, 2.6%), and L2-3 (1 case, 0.9%). Herniations were localized at zones 1–4 in 4 (3.5%), 5 (4.3%), 73 (62.9%), and 34 (29.3%) cases, respectively.
According to the modified Macnab criteria, satisfactory (excellent or good) results were distributed as follows: 91.6% (98/107) in the down-migrated discs; 88.9% (8/9) in the up-migrated discs; 97.4% (76/78) in the near-migrated discs; and 78.9% (30/38) in the far-migrated discs (Table 2). The difference between near-migrated group (97.4%) and far-migrated group (78.9%) was statistically significant (P = 0.002), while the difference between down-migrated group (91.6%) and up-migrated group (88.9%) was not statistically significant (P = 0.569).
Table 2.
Clinical outcome according to the Macnab criteria
| Zones | Number of patient (% in each zone) | ||||
|---|---|---|---|---|---|
| Excellent | Good | Fair | Poor | Total | |
| Zone 1 | 0 (0.0) | 3 (75.0) | 1 (25.0) | 0 (0.0) | 4 |
| Zone 2 | 3 (60.0) | 2 (40.0) | 0 (0.0) | 0 (0.0) | 5 |
| Zone 3 | 39 (53.4) | 32 (43.8) | 1 (1.4) | 1 (1.4) | 73 |
| Zone 4 | 10 (29.4) | 17 (50.0) | 1 (3.0) | 6 (17.6) | 34 |
The preoperative mean VAS of leg pain was 7.5 ± 1.7 (range 5–9), which significantly decreased to 2.6 ± 1.8 (range 0–3) at the final follow-up (P < 0.0001). The average return to work period was 14 days (range 1–48 days). During the follow-up period, there were no recurrent disc herniations and no approach related complications such as dural tearing or infection.
Discussion
Although Kambin et al. reported similar results with transforaminal endoscopic surgery compared to open microdiscectomy for the same indications and good surgical results for lateral recess stenosis and fragmentectomy, they did not employ radiologic classification and provide a detailed technical description for the removal of migrated disc fragments [2, 4, 6]. Additionally, most surgeons thought that migrated disc fragments could not be safely removed using the percutaneous endoscopic method. Several authors reported that they could treat the migrated disc through epidural space (out to in approach, Thessys®) after partial removing the facet joint or through a biportal approach. However, the “out to in” approach has a potential risk of neural injury. In this study, we safely removed the migrated disc from inside of disc to the direction of epidural space. We achieved the favorable results without a biportal approach.
The authors defined the location of the migrated discs in four zones. This classification can be a yardstick for preoperative evaluation and in determining the proper technique. Moreover, a comprehensive account is given on each surgical procedure for each zone.
Both techniques are performed on a basis of a transforaminal inside-out technique, from the disc space to the direction of the epidural space. In case of “half-and-half” technique, the ventral half of the lateral window of the cannula positions inside of the disc space and only the dorsal half of it lies in the epidural space. It seems to be dangerous, but actually it is not just under the neural structures but under disc fragment interposing between thecal sac and disc space. In case of “epiduroscopic” technique, entire portion of the lateral window of the working sheath is located completely in the epidural space. The endoscope and forceps can access closely to the far-migrated fragment by this approach.
Some surgeons use an extreme lateral entry to get a proper angle to approach to epidural space directly, but it may cause serious complications by peritoneal perforation or psoas muscle injury. In contrast, the “half-and-half” and “epiduroscopic” techniques involving the annular release and working sheath levering can minimize this potential risks; it provides a safe and direct access to the fragment, as well. However, the “epiduroscopic” technique presents such problems as epidural bleeding, risk of neural injuries, and intraoperative pain and it requires the removal of the ventral part of the superior articular process. Fortunately there were no neural and vascular complications in our cases.
Even in “epiduroscopic” approach, initial procedure is done from the disc space (blue line in Fig. 2, middle). Finally, the working cannula goes over the outer surface of the annulus completely and moves toward the migrated fragment. Therefore, lateral window faces the targeting mass (black line in Fig. 2, middle). During epidural technique, further annular release at the annular tear site is sometimes essential in those migrated herniations that are still trapped by a part of the annulus fibrosus.
Generally direction of needle insertion is parallel to the disc space. Sometimes skin entry point should be moved to the opposite direction of the target mass in case of caudal or cephalic migration. It is more comfortable in removing the mass.
Usually those severely migrated herniations are multi-fragmented. It is very difficult to detect such fragmentation on preoperative radiologic studies. In addition they are easily snapped off when a surgeon pulls it out. Those fragmented herniations cannot be completely removed just by grasping the proximal part of the herniation. That is the reason why the “epiduroscopic” approach should be used for approaching to the tip of migrated fragment. We, however, believe that they did not affect the results in our study, as the number of severely migrated herniations was very few.
In this study, we evaluated the clinical results after a minimum period of 9 months from the procedure using a modified Macnab criteria [8]. The authors had thought that a simple grading system was easy and fast for clinical evaluation. However, to minimize the bias towards positive results, the clinical outcome was assessed by an independent observer. And since sciatica is the main reason for this procedure, reduction of leg pain was analyzed using a VAS. There was a significant improvement in the VAS and the clinical outcome at the end of postoperative 1 month, and this significant improvement was well maintained throughout follow-up.
According to our results, patients with far-migrated discs had worse outcomes than those with near-migrated discs. It is revealed not only by clinical evaluation, but also by postoperative MRI. A possibility of missing the fragment or disconnecting the stalk is higher in far-migrated discs. Therefore we think that open micro-discectomy will be better in far-migrated disc herniations. One of the contraindications is severe foraminal stenosis, which makes difficult to achieve a proper epidural access.
The most important point for successful endoscopic treatment is the accurate approach to the proper indication. The authors recommend open surgery if there is possibility of incomplete removal of the disc fragment, as in patients with a sequestered disc in zones 1 and 4. In addition, endoscopic surgery requires appreciation of the endoscopic anatomy matching the fluoroscopic view. After mastering surgical anatomy and with strict adherence to technical guidelines, endoscopic surgery does not present difficulties for dealing with migrated discs.
Conclusion
Disc migration can be classified into four zones based on the direction and distance from the disc space. Two techniques of PELD can be used according to this classification: the “half-and-half” technique for near-migrated discs and the epiduroscopic technique for far-migrated discs. Our results suggest that open microdiscectomy may give superior results in far-migrated discs. The results of this study will contribute to the establishment of surgical guidelines for PELD in the treatment of migrated disc herniation. A prolonged follow up is necessary to determine the validity of these initial results.
Acknowledgments
The authors thank Dr. Ki-Bum Park, Hye-Ran Lee, Il Lee, and Ji-Hee Hwang for the help in preparing the manuscript and figures. This work was supported by a grant from the Wooridul Spine Foundation.
References
- 1.Ahn Y, Lee SH, Park WM, et al. Posterolateral percutaneous endoscopic lumbar foraminotomy for L5-S1 foraminal or lateral exit zone stenosis. Technical note. J Neurosurg. 2003;99(3 Suppl):320–323. doi: 10.3171/spi.2003.99.3.0320. [DOI] [PubMed] [Google Scholar]
- 2.Hermantin FU, Peters T, Quartararo L, et al. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am. 1999;81:958–965. doi: 10.2106/00004623-199907000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Hijikata S, Yamagishi M, Nakayama T, et al. Percutaneous nucleotomy: a new treatment method for lumbar disc herniation. J Toden Hosp. 1975;5:5–13. [Google Scholar]
- 4.Kambin P, Casey K, O’Brien E, et al. Transforaminal arthroscopic decompression of lateral recess stenosis. J Neurosurg. 1996;84:462–467. doi: 10.3171/jns.1996.84.3.0462. [DOI] [PubMed] [Google Scholar]
- 5.Kambin P, Gellman H. Percutaneous lateral discectomy of the lumbar spine. A preliminary report. Clin Orthop. 1983;174:127–132. [Google Scholar]
- 6.Kambin P, O’Brien E, Zhou L. Arthroscopic microdiscectomy and selective fragmentectomy. Clin Orthop. 1998;347:150–167. [PubMed] [Google Scholar]
- 7.Knight MTN, Goswami AKD. Endoscopic laser foraminoplasty. In: Savitz MH, Chiu JC, Yeung AT, editors. The practice of minimally invasive spinal technique, first edition. Richmond: AAMISMS Education, LLC; 2000. pp. 337–340. [Google Scholar]
- 8.Macnab I. Negative disc exploration An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am. 1971;53:891–903. [PubMed] [Google Scholar]
- 9.McCulloch JA, Young PH (1988) Musculoskeletal and neuroanatomy of the lumbar spine. In: Essentials of spinal microsurgery. Lippincott-Raven, Philadelphia, 18:249–292
- 10.Onik G, Mooney V, Maroon JC, et al (1990) Automated percutaneous discectomy: a prospective multi-institutional study. Neurosurgery 26:228–232; discussion 232–233 [PubMed]
- 11.Sherk HH, Black JD, Prodoehl JA, et al. Lasers in orthopedic surgery: laser discectomy. Orthopedics. 1993;16:573–576. doi: 10.3928/0147-7447-19930501-10. [DOI] [PubMed] [Google Scholar]
- 12.Wiltse LL, Berger PE, McCulloch JA. A system for reporting the size and location of lesions of the spine. Spine. 1997;22:1534–1537. doi: 10.1097/00007632-199707010-00023. [DOI] [PubMed] [Google Scholar]
- 13.Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine. 2002;27:722–731. doi: 10.1097/00007632-200204010-00009. [DOI] [PubMed] [Google Scholar]