Abstract
The aim of the study was to compare the results of brace treatment of adolescent idiopathic scoliosis (AIS) in male patients with matched female patients and to assess the effectiveness of bracing of boys in AIS and to discuss the results with published data. Between 1987 and 1995, 51 consecutive male patients with AIS were treated with the Boston brace. The patients were advised to wear the brace 23 h/day. The medical records of all patients were reviewed. Cobb angles and Risser signs were measured before bracing, in brace, at brace discontinuation and at final follow-up. Everyone of 51 male patients was compared with a female patient who was treated by the same method and matched by Risser sign, curve pattern, curve magnitude and duration of treatment and follow-up time. Compliance with brace was noted at every visit. Fourteen boys had worn the brace only during nighttime or occasionally and were considered non-compliant. Only compliant patients with treatment period > 1 year and follow-up > 1 year after treatment were accepted for the analyses of effectiveness of brace treatment and its prognostic factors. Thirty-three boys met these inclusion criteria. Bracing was considered to have a failure if > 5° progression occurred or if surgery was performed. At the final follow-up study progression > 5° was found in 16/51 (31.4%) of male patients. Corresponding figures of female patients were 11/51 (21.6%), respectively. In compliant boys progression > 5° occurred in 6/33 boys compared with 9/33 girls. The association between risk of progression and correction% in brace was statistically significant. The overall results of brace treatment of idiopathic scoliosis in male patients were inferior compared with matched females. One reason for inferior overall results in boys was poor compliance with brace wear. However, brace treatment in AIS may be recommended with the same principles in both genders.
Keywords: Adolescent idiopathic scoliosis, Male patients, Brace treatment, Comparative study
Introduction
Some studies suggest that effect of bracing in idiopathic scoliosis is unresolved [4, 5, 16]. Efficacy of bracing has not been proved definitely in prospective randomised clinical studies but the literature almost universally supports that bracing of growing children with idiopathic scoliosis improves natural history of the disease [15, 19, 21]. These studies reflect series, which consist of mainly adolescent girls. The results of bracing of male patients have been suggested to be inferior but the data available is incomplete.
Karol et al. [9] concluded that risk of progression of curves is increased among boys. It has also been reported that results of operative treatment of scoliosis among boys may be less successful [6, 22]. These studies suggest that results worsen because of relative stiffness of the spine in male patients. Because of this assumed stiffness and more usual lack of compliance, bracing of boys with adolescent idiopathic scoliosis (AIS) has been concluded questionable [8]. The aim of this study was to compare the results of male patients with the matched female patients and to assess the effectiveness of bracing in males.
Patients and methods
From 1987 to 1995, 51 consecutive male patients with AIS were treated at our institution with the Boston brace. All patients presenting at age > 10 years were included. Curves > 25° were braced immediately and curves between 20 and 25° were braced if progression of > 5° was found during observation. The thoracic Boston brace was used when the apex of the major curve was T 10 or more cranial. In the rest of cases the lumbar Boston brace was used. The patients were advised to wear the brace 23 h/day. The brace was adjusted at the hospital and checked at the outpatient clinic at 6 months intervals. The weaning was started when the growth had ceased and the iliac apophyses were ossified to Risser 4. All patients had completed treatment.
Each boy was compared retrospectively with a female patient who had been treated in the same way at the same hospital with the similar brace and matched precisely by Risser sign, the curve pattern and apex of the major curve. Magnitude of the curve, duration of treatment and follow-up time were matched as well as possible. The control female patients were gathered from the database of the hospital without knowing the results of their treatment in advance.
The medical records of all patients were reviewed. Information at presentation, at the time of brace discontinuation and final visit was gathered. At every visit patients and parents were asked success or lacks in scheduled wear of the brace. Non-compliance with bracing was roughly estimated by reviewing the orthopaedic clinic notes and the orthotic department records as described by Karol [8]. Those patients who wore the brace only during nighttime or occasionally were considered non-compliant. Because of the retrospective nature of the study, more accurate data of compliance were not available and no questionnaire to assess compliance was administered.
At the first visit postero-anterior (p-a) and sagittal radiographs of the entire spine were taken. At each later visit standing (p-a) radiographs of the spine were controlled. Radiographs using the Cobb technique were measured by radiologist (M.Y.) who was not involved in the treatment. Curve patterns were recorded: thoracic, thoracolumbar, lumbar and double major. The Risser sign was noted on radiographs at presentation and during follow-up. The initial correction of the curves achieved in the brace was recorded.
Bracing was considered to have failed if > 5° of progression occurred or if surgery was performed. Successes and failures were analysed for patient’s age, curve size, curve pattern and Risser sign.
The overall results of treatment of males and females were recorded. When assessing factors for prognosis of treatment in males, clearly non-compliant patients were excluded and the rest of the patients with a minimum period of bracing > 1 year and a minimum follow-up of > 1 year after cessation of bracing were analysed separately and compared with matched females.
The results were analysed by using Student’s t test with a P < 0.05 representing statistical significance.
Results
Overall results
At brace prescription an average age of 51 male patients was 14.8 years and of 51 female patients 13.1 years. Before brace treatment the average major curve magnitude on standing radiograph was 33.1° in boys and 32.4° in girls. The average bracing period was 2.1 years and follow-up after treatment was 2.4 years. At the weaning of the brace the mean curve magnitude was 31.4° in males and 27.0° in females. At the latest follow-up visit the mean magnitude of the major curve of male patients was 34.8° and in female patients 32.0°. Progression of major curve > 5° had occurred in 16/51 (31.4%) of boys and 11/51 (21.6%) girls. The difference between male and female patients was statistically significant (P < 0.05). Three of the boys but none of the girls had been operated.
Effectiveness of bracing
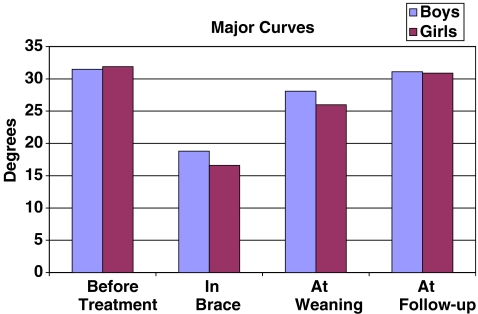
According to medical records 14/51 boys (27.5%) had worn the brace only during nighttime or occasionally and were considered non-compliant. In additional four boys the bracing period was < 1 year. The data of the remaining 33 compliant males were analysed separately for prognostic factors of treatment and compared with the matched females. The average age of these boys at brace prescription was 14.9 (SD 1.2, range 11–17) years and in girls 13.0 (SD 1.5, range 9–16). The major curve was thoracic in 24 patients and thoracolumbar or lumbar in nine patients in both genders. Risser sign was 0–1 in 18 and 2–3 in 15 patients in both males and females. The average Cobb angle of the major curve before treatment was 31.5° (SD 6.9, range 22–47) in boys and 31.9° (SD 6.0, range 22–47) in girls. In brace radiographs the mean curve size of male patients was 18.8° with 41% correction. The corresponding numbers in females were 16.8° and 49%. The average bracing period was 2.1 (1–7.1) years in both genders. At cessation of treatment the average magnitude of the major curve was 28.1° (SD 7.3, range 15–44) in boys and 26.0° (SD 9.2, range 9–48) in girls. The follow-up time after treatment was 2.4 (SD 1.1, range 1–4) years in boys and 2.6 (SD 0.9, range 1–5) years in girls. At the latest follow-up visit the mean magnitude of the major curve of male patients was 31.1° (SD 7.6, range 15–47) and in female patients 30.9° (SD 10.0, range 9–53). Progression > 5° had occurred in 6/33 males and in 9/33 females. (Fig. 1; Tables 1, 2).
Fig. 1.
Cobb angles of major curves in 33 compliant boys and matched 33 girls
Table 1.
Data of 33 compliant boys and matched girls
| n | Age (years) | Before treatment (°) | In brace (°) | Correction in brace (%) | At weaning (°) | At follow-up (°) | |
|---|---|---|---|---|---|---|---|
| Boys | |||||||
| Risser 0–1 | 18 | 14.6 | 30.6 | 16.3 | 47.0 | 26.3 | 28.7 |
| Risser 2–3 | 15 | 15.2 | 32.5 | 15.2 | 34.0 | 30.2 | 34.0 |
| Thoracic | 24 | 15.0 | 32.5 | 15.0 | 41.0 | 28.7 | 32.7 |
| Thracolumbar + lumbar | 9 | 14.7 | 28.7 | 18.3 | 39.0 | 26.3 | 26.9 |
| Girls | |||||||
| Risser 0–1 | 18 | 12.0 | 29.9 | 12.7 | 58.0 | 23.3 | 28.1 |
| Risser 2–3 | 15 | 14.0 | 34.3 | 21.2 | 39.0 | 29.3 | 34.3 |
| Thoracic | 24 | 13.0 | 32.1 | 16.6 | 49.0 | 25.7 | 30.5 |
| Thracolumbar + lumbar | 9 | 13.0 | 31.6 | 16.4 | 50.0 | 26.9 | 31.8 |
Table 2.
Data of averages in 33 compliant boys and matched girls and curve progression > 5
| n | Age (years) | Before treatment (°) | In brace (°) | Correction in brace (%) | At weaning (°) | At follow-up (°) | Progression > 5 (n) | |
|---|---|---|---|---|---|---|---|---|
| Boys | 33 | 14.9 | 31.5 | 18.8 | 41.0 | 28.1 | 31.1 | 6 |
| Girls | 33 | 13.0 | 31.9 | 16.8 | 48.0 | 26.0 | 30.9 | 9 |
In the analysis of the data of the compliant boys, the age of the patient, the curve pattern or the curve magnitude did not have statistical influence on the risk of progression (P > 0.05). The importance of Risser sign remained obscure but the association between the risk of progression > 5° and correction% in brace was statistically significant (P < 0.05).
Discussion
Natural history of AIS is not totally known. It is usually referred to the studies of Prevalence and Natural History committee of Scoliosis Research Society [14] and Lonstein and Carlson [11]. These studies report that risk of progression in curves between 20 and 29° is > 60% and increases with the curve magnitude. There are no studies comparing natural history of AIS between boys and girls. Thus we do not know, whether there is any difference between genders. However, the general impression is that the results of treatment are inferior among boys.
Effectiveness of bracing in different studies is often compared to the data of the brace study
Of the Scoliosis Research Society [19] and studies by Lonstein and Winter [12]. These studies, which include mainly female patients, demonstrate less curve progression in patients with orthotic treatment compared with untreated controls.
It is generally accepted that treatment may be considered as a failure if there is progression of the curve > 5° in Cobb angle or if surgery is needed. Most of the brace studies with female patients report that up to 20–35% of the curves progress > 5° for different reasons [3, 15].
There are only few studies, which analyse braced male patients with scoliosis. Katz et al. [10] had 25 male patients included in large series with the Boston brace and the Charleston bending brace. They found that 80% curves with the Boston brace progressed > 5° compared with 36% in girls. Karol [8] was the first to report the brace study of only males. She had 112 male patients with the Milwaukee brace, Boston brace and Charleston bending brace. The progression of > 5° occurred in 74% of the patients and there was no statistical difference between brace designs. In this study progression > 5° were found in 31.4% of all boys. This risk of progression was statistically significantly increased compared with 21.6% of matched females. These numbers indicate that bracing of boys with idiopathic scoliosis improves natural history and that the results of treatment may be significantly better than previously reported.
Goldberg et al. [5] reported an untreated series of 153 children and found that 28% had undergone surgery. Lonstein and Winter [12] reviewed 1,020 patients and concluded that 22% of patients needed surgery after treatment with the Milwaukee brace. In Karol’s study [8] of male patients 46% of curves progressed to 50° or spinal arthrodesis surgery. Curves measuring > 30° progressed to surgical magnitudes in > 50% of patients.
In the present study only 3 of 51 boys (6%) were qualified for operation. All of these three cases had curve size at presentation > 30°.
Acceptance for bracing is a principal prerequisite for a good result of treatment and the compliance always remains a serious problem because it is impossible to detect it accurately. It is evident that true brace compliance is less than estimated clinically and by the patient questionnaire [7] and full compliance is seldom achieved with a 23-h per day schedule. Studies of compliance monitoring by a data logger and a temperature sensor have shown the same in part-time wear, too [23].
Karol [8] reported that only 38% of the boys were according to medical records compliant throughout the entire course of the brace wear but included all patients in the analysis of effectiveness of bracing. However, if the compliance is very low, it is difficult to draw profound conclusions of the effectiveness of the treatment method itself. In this study we used Karol’s method to roughly clarify compliance with brace wearing but excluded 14/51 clearly non-compliant cases from the analysis of the effectiveness of brace treatment. Nevertheless, confounding factors remain because with this method it is not possible to better quantify compliance with brace wear.
Curve magnitude and the influence of maturity determined by Risser sign and age of the patients are usually analysed as parameters for the risk of progression. The importance of age of the patient has remained obscure but Risser sign has found to be significant in most studies. Final results have been reported to worsen if initial curve is > 30–35° [8, 18]. In this study we did not find statistical association between risk of progression > 5° and age of the patient, curve pattern or curve magnitude. Influence of Risser sign remained a little obscure. One reason for better results in this study might be that we had larger amount (45%) of Risser 2–3 (in Karol’s study 29% [8]). However, this may explain only partially big differences between the results.
Curves with good in brace correction have been shown to have a favourable final result [2, 3, 18]. Noonan et al. [16] concluded that maximum in brace correction is prognostic for curve progression. It has been suggested that effectiveness of bracing increases significantly if in brace correction is > 50% in full-time braces in standing p-a radiographs. This is often achieved in girls [17]. In Karol’s study of male patients [8] in brace correction in Boston brace group was 36% and no statistical association between correction% in brace and risk of progression was found. In this study the average correction in brace in the compliant male patients were 41% and the risk of progression correlated significantly with correction in brace.
The achieved correction of curves tends to decrease during the first years after brace treatment [1, 3]. It has been suggested that in boys the risk of progression may persist after Risser grade 4 is achieved [9], when weaning is usually recommended. This may worsen final results. In the present study the average increase in curve magnitude after treatment was in male patients 3.0° and in female patients 4.9° during the follow-up period of 2.4 years after brace treatment.
These figures do not support the concept of significant differences between genders in the risk of curve progression after brace treatment. However, this needs further data.
One reason of inferior results in male patients has been thought to be differences in curve stiffness. Mellin et al. [13] reported that structurally normal girls have decreased spinal mobility compared with boys and Poussa et al. [20] concluded that there was no change of general flexibility in 29 scoliotic girls compared with normal controls. Differences in curve stiffness between genders in scoliotic patients have not been definitely proved but it is usually related with correction% in brace, which has been inferior among boys in many studies. In this study average in brace correction in boys was 41% and in the control group of girls 49%. This result supports the concept that scoliotic curves in boys are stiffer or that girls tolerate better the correction of the spinal curve.
In conclusion, this study supports the concept that bracing improves natural history also in boys with adolescent idiopathic scoliosis. There was a clear correlation between the amount of correction in brace and a successful outcome.
The overall results of treatment of boys were statistically inferior compared with matched girls. One reason for inferior overall results in boys was poor compliance with brace wear.
Progression of curves > 5° occurred in 31.4% of male patients, which, however, corresponds with many published results of female patients.
The results of this study suggest that bracing of boys may be recommended with the same principles as girls in adolescent idiopathic scoliosis.
References
- 1.Bassett GS, Bunnell WP, MacEwen GD. Treatment of idiopathic scoliosis with the Wilmington brace. Results in patients with a twenty- to thirty-nine-degree curve. J Bone Joint Surg. 1986;68A:602–605. [PubMed] [Google Scholar]
- 2.Carr WA, Moe JH, Winter RB, Lonstein JE. Treatment of idiopathic scoliosis in the Milwaukee brace. J Bone Joint Surg Am. 1980;62:599–612. [PubMed] [Google Scholar]
- 3.Emans JB, Kaelin A, Bancel P, Hall Miller JE; ME. The Boston bracing system for idiopathic scoliosis. Follow-up results in 295 patients. Spine. 1986;11:792–801. doi: 10.1097/00007632-198610000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Focarile FA, Bonaldi A, Giarolo M-A, Ferrari U, Zilioli E, Ottaviani C. Effectiveness of nonsurgical treatment for idiopathic scoliosis. Overview of available evidence. Spine. 1991;16:395–401. doi: 10.1097/00007632-199104000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Goldberg CJ, Moore DP, Fogarty EE, Dowling FE. Adolescent idiopathic scoliosis: the effect of brace treatment and the incidence of surgery. Spine. 2001;26:42–47. doi: 10.1097/00007632-200101010-00009. [DOI] [PubMed] [Google Scholar]
- 6.Helenius I, Remes V, Yrjönen T, Ylikoski M, Schlenzka D, Helenius M, Poussa M. Does gender affect outcome of surgery in adolescent idiopathic scoliosis. Spine. 2005;30:462–467. doi: 10.1097/01.brs.0000153347.11559.de. [DOI] [PubMed] [Google Scholar]
- 7.Houghton GR, McInerney A, Tew A. Brace compliance in adolescent idiopathic scoliosis. J Bone Joint Surg Br. 1997;69:852. [Google Scholar]
- 8.Karol LA. Effectiveness of bracing in male patients with idiopathic scoliosis. Spine. 2001;26:2001–2005. doi: 10.1097/00007632-200109150-00013. [DOI] [PubMed] [Google Scholar]
- 9.Karol LA, Johnston CE, Brownw RH, et al. Progression of the curve in boys who have idiopathic scoliosis. J Bone Joint Surg Am. 1993;75:1804–1810. doi: 10.2106/00004623-199312000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Katz DE, Richards BS, Browne RH, et al. A comparison between the Boston brace and the Charleston bending brace in adolescent idiopathic scoliosis. Spine. 1997;22:1302–1312. doi: 10.1097/00007632-199706150-00005. [DOI] [PubMed] [Google Scholar]
- 11.Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg. 1984;66A:1061–1071. [PubMed] [Google Scholar]
- 12.Lonstein JE, Winter RB. The Milwaukee brace for the treatment of adolescent idiopathic scoliosis: a review of one thousand and twenty patients. J Bone Joint Surg Am. 1994;76:1207–1221. doi: 10.2106/00004623-199408000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Mellin G, Harkonen H, Poussa M. Spinal mobility and posture and their correlations with growth velocity in structurally normal boys and girls aged 13 to 14. Spine. 1988;13(2):152–154. doi: 10.1097/00007632-198802000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Nachemson A, Lonstein JE, Weinstein ST (1982) Prevalence and natural history commitee report. Read at the Annual Meeting of the Scoliosis Research Society, Denver, Colorado, Sept 25
- 15.Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis: a prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am. 1995;77:815–821. doi: 10.2106/00004623-199506000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Noonan KJ, Weinstein SL, Jacobson WC, et al. Use of the Milwaukee brace for progressive idiopathic scoliosis. J Bone Joint Surg Am. 1996;78:557–567. doi: 10.2106/00004623-199604000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Olafsson Y, Saraste H, Söderlund V, Hoffsten M. Boston brace in the treatment of idiopathic scoliosis. J Pediatr Orthop. 1995;15:524–527. doi: 10.1097/01241398-199507000-00023. [DOI] [PubMed] [Google Scholar]
- 18.Peltonen J, Poussa M, Ylikoski M. Three-year results of bracing in scoliosis. Acta Orthop Scand. 1988;59:487–490. doi: 10.3109/17453678809148769. [DOI] [PubMed] [Google Scholar]
- 19.Peterson LE, Nachemson AL. Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity; logistic regression analysis based on the data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am. 1995;77:823–827. doi: 10.2106/00004623-199506000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Poussa M, Harkonen H, Mellin G. Spinal mobility in adolescent girls with idiopathic scoliosis and structurally normal controls. Spine. 1989;14(2):217–219. doi: 10.1097/00007632-198902000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Rowe DE, Bernstein SM, Riddick MF, et al. A meta-analysis of the efficacy of non-operative treatment for idiopathic scoliosis: J Bone Joint Surg Am. 1997;79:664–674. doi: 10.2106/00004623-199705000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Sucato DJ, Hedequist D, Karol LA. Operative correction of adolescent idiopathic scoliosis in male patients. J Bone Joint Surg Am. 2004;86:2005–2014. doi: 10.2106/00004623-200409000-00020. [DOI] [PubMed] [Google Scholar]
- 23.Takemitsu M, Bowen R, Rahman T, Glutting J, Scott C. Compliance monitoring of brace treatment for patients with idiopathic scoliosis. Spine. 2004;29:2070–2074. doi: 10.1097/01.brs.0000138280.43663.7b. [DOI] [PubMed] [Google Scholar]