Abstract
To find out whether segmental magnetic resonance imaging (MRI) findings such as intervertebral disc degeneration (DD) and facet joint osteoarthritis (FJO) are associated with motion deficiencies as seen in common mobility tests and observed range of motion (ROM). A total of 112 female subjects, nurses and office workers, with and without low back pain, were examined by clinical experts, and lumbar mobility was measured including modified Schober, fingertip-to-floor distance (FTFD) and ZEBRIS motion analysis. An MRI of the lumbar spine was made. Mobility findings were correlated with segmental morphologic changes as seen on MRI at the levels of L1-2 through L5-S1. Only a few statistically significant correlations between MRI findings and the results of the mobility tests could be found. Lateral bending was weakly and negatively correlated to DD and FJO but only on the level of L5-S1. The FTFD showed a weak positive correlation to endplate changes on the level of L4-5. When ROM is observed by clinical experts, there are several significant relationships between MRI findings and the observed motion. There is a highly significant segmental correlation between DD and disc form alteration as seen on MRI on the level of single motion segments. Pain history and current pain level did not moderate any association between MRI and mobility. There is no clear relationship between the structural changes represented by MRI and the measured mobility tests used in this study. Our findings suggest that close observation of spinal motion may provide at least equal information about the influence of spinal structures on motion than the commonly used measured mobility tests do.
Keywords: Spine, Spine abnormalities, Spine mobility, Intervertebral disk, Facet joints, Spine range of motion
Introduction
Mobility tests are widely used when examining patients with low back disorders. The literature describes different methods on how to measure the lumbar range of motion (ROM). Techniques reach from an easy-to-do fingertip-to-floor distance (FTFD) test to various inclinometer methods and highly invasive measurements with pedicle screws [23, 25, 26]. The more practical, non-invasive and low cost tests, such as the modified Schober, are widely used in medical examinations and have received a large amount of scientific attention. Studies with more sophisticated (due to technical equipment) expensive or invasive measuring devices have provided detailed information about the lumbar ROM in chronic low back pain patients [9, 26], but have few participants and are hardly applicable to everyday clinical practice.
With the development of magnetic resonance imaging (MRI), non-invasive imaging methods became available and are intensively used in various medical specialities. The MRI scan is often part of examination procedures in the field of the low back pain, especially if neural compromise is present. Many findings from MRI are common in both the low back pain patient and the asymptomatic patient [22]. Of these common findings, some may have an influence on the motion characteristics, as has been found in cadaver studies.
These investigations have demonstrated reduced intervertebral motions in degenerated lumbar spines [17, 32, 45]. They found that with moderate disc degeneration (DD) and facet joint osteoarthritis (FJO) the ROM is increased, whereas with severe degenerative structures the ROM is decreased. If degenerative structural changes can influence motion characteristics in cadavers, they may have an influence on the mobility tests. Nevertheless, these findings cannot be transferred directly into the clinical situation.
Therefore, it was the purpose of this study to explore the effect of common lumbar MRI findings on commonly used mobility tests.
Material and methods
The study was performed within the European Project Neuromuscular Assessment in the Elderly Worker (NEW).
Subject selection
The study population was selected with respect to different occupational exposures, i.e. physically monotonous work for office workers and physically heavy work for nurses. Inclusion criteria were a workload of a minimum of 20 h per week, having similar working tasks for the past 5 years and age between 45 and 65 years.
Within the NEW project, participants were divided into a case and a control group. The cases had reported pain in the low back for more than 7 days during the last year and had trouble from no more than two other body regions.
Controls were defined as subjects who did not report aches or discomfort in the low back for more than 7 days during the last year and had no trouble in more than two other body regions.
Exclusion criteria were neurological deficits, spinal cord compression, severe structural deformity, osteoporosis, instability, acute fractures or infections, severe cardiovascular, respiratory, autoimmune or metabolic disease, cancer or previous spinal surgery.
A total of 114 female subjects met the inclusion criteria for either the case or the control group and were given a detailed questionnaire about working posture characteristics and musculoskeletal disorders. Two subjects were excluded at a later stage of the study as they refused to have an MRI scan. Finally, a total of 112 subjects gave an informed consent and participated in the study: 59 nurses and 53 office workers. The case group consisted of 26 nurses and 18 office workers. These groups had very similar anthropometric data. The mean age was 53 years, the average height was 164.7 cm, the average weight was 66.4 kg and the mean BMI was 24.5 kg/m2.
Testing procedure
The participants underwent three mobility tests: the modified Schober test, the FTFD in the sagittal plane, the lateral bending and the ZEBRIS motion analysis. These were conducted and measured by a trained physiotherapist. A physical examination was executed by one of the two experienced rheumatologists involved in the study at the Institute of Physical Medicine at the University Hospital. Each subject received an MRI scan of the lumbar spine at the Orthopaedic University Hospital that was read by an experienced radiologist. The physiotherapist and the rheumatologists were naive with respect to the results of pain reporting, profession and MRI findings; the radiologist was blinded to all other results.
Modified Schober test, fingertip-to-floor distance, lateral bending manoeuvre (LB)
The modified Schober and the FTFD were described previously [4, 15, 19, 27, 31, 39]. For the LB, the participants were told to slowly bend from the upright position to the side with their hand running down a vertical ruler. Attention was paid that this motion was done without rotating the trunk or moving the pelvis. The distance from the fingertip to the floor was measured in standing and in full lateral bending (see Fig. 1). The latter measurement was subtracted from the first and noted. Each side was measured twice and the mean was calculated.
Fig. 1.
Measuring the fingertip-to-floor distance in flexion and lateral bending
ZEBRIS
The ZEBRIS motion analysis (CMS20S, zebris® Medizintechnik, Tübingen, Germany) is a recording unit with ultrasound transmitters and receivers. The transmitters are taped to the skin and send sound pulses at 20 Hz. Three receivers, placed about 1 m behind the participant, pick up the pulses and transmit the information to a computer. There, the three-dimensional movement of each transmitter is calculated and plotted. Eight transmitters were placed on the subjects’ back (see Fig. 2).
Fig. 2.
ZEBRIS transmitter placement on the low back
The subjects were asked to do five warm-up side bending, flexion and extension movements. Then the subjects were instructed to bend to the side in a continuous motion as far as possible, with their hands running down the lateral aspect of their thigh. The subjects were instructed to bend forward as far as possible with the knees completely extended for the flexion-extension movements, then return to the neutral position and continue into extension as far as possible before returning to the neutral position again. After a set containing three of these motion sequences, the patient was allowed to rest for 30 s. A total of three sets were analysed. The entire sequence was measured by the ZEBRIS unit and recorded in the WinData program (zebris® Medizintechnik, Tübingen, Germany). The collected data included change of angles, distances and velocity of the markers during the performance of motion.
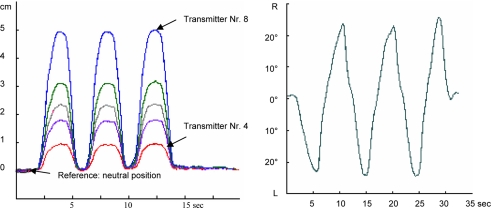
Hereinafter, the data were cleaned from abnormal recordings, and missing values on the curve were interpolated. Figure 3 shows the resulting curves.
Fig. 3.
ZEBRIS motion analysis (changes of distances and angles) plotted for flexion/extension (left change of distances) and lateral bending range (right change of angles). Transmitter 3 was used as reference for the measurements
For the purpose of this study only the distance from marker 3 to 8 was measured in the erect position and in the fully flexed position. Because there is no objective definition of the upright position during lateral bending motion, the total range, and not the individual side, was measured in degrees.
To accommodate a few missing measurements due to technical reasons, the mean of all correct measurements was calculated and used for the analysis.
Expert observation of posture and ROM
Expert observation was performed by two clinicians specialized in musculoskeletal disorders, with more than 10 years of experience. They reached consent about the classification of findings (“normal” and “out of normal” respectively “restricted” and “not restricted”) and underwent a short training at the beginning and at the mid of the inclusion period. Flexion and extension, as well as lateral flexion left and right, were observed closely. Restrictions were noted when the lumbar spine motion was limited or when compensatory mechanisms (i.e., hip flexion, torso rotation) influenced the pure motion. The cutoff ranges for restriction were set at 60° for flexion, 25° for extension and 30° for lateral flexion.
Furthermore, the occurrence of a hyperlordosis, a reduced lordosis, or a decompensated scoliosis (plumb line from C7 > 0.5 cm off the rima ani) was noted on the inspection of the participants back in the standing position.
Magnetic resonance imaging
Each subject received a T1- and T2-weighted MRI scan of the lumbar spine. MRIs of the lumbar spine were acquired on either a 1.0 T Siemens Expert or a 1.5 T Siemens Symphony magnet (Siemens Medical Solutions, Erlangen, Germany). Sagittal T1- and T2-weighted and an axial T2-weighted image was obtained. For the T1-weighted spin-echo sequence, the parameters were as follows: repetition time 500–600 ms, echo time 15 ms. The corresponding parameters for the T2-weighted turbo spin-echo sequence were 4000/96 (Expert) and 5000/122 (Symphony). A staff radiologist with a 17-year experience in MRI of the spine evaluated the MRIs . He was blinded to the results of the physical examination. Each spinal motion segment was evaluated according to Weishaupt [47] with regard to DD, abnormal disk form, nerve root compromise, high intensity zones (HIZ) within the dorsal annulus fibrosus, endplate changes and FJO. The interobserver reliability (kappa value) for grading DD is 0.84, for the disc form 0.79, for the nerve root compromise 0.58, for the FJO 0.50 and for the high intensity zone 0.91.
Similar to the standard protocol used at one of our institutions, the axial images were obtained at the L3-4, L4-5 and L5-S1 levels. If the technician detected abnormalities at the L1/2 or L2/3 levels on the sagittal T2-weighted images, axial images were obtained at the abnormal levels as well. At L1-2 there were only images of four participants available and at L2-3 only 23 images were available. Therefore, a representative evaluation at these levels for nerve root compromise was not possible. If the degree of FJO on the right and left sides at the one level was identical, that score was included in the overview. If the degree differed from left to right, the larger of the two scores was included. The evaluation of the HIZ identified very few abnormal segments. For the purpose of statistical analysis, these numbers were too small to form meaningful groups and were therefore omitted. Of the 1,120 endplates evaluated, there were only 52 superior (4.6%) and 41 (3.7%) inferior endplates found to be changed according to Modic [34]. If at a single disc level, more than one Modic type was found, the most extensive abnormality was reported.
Personal characteristics and pain
The questionnaire was filled out by each participant and included questions about height and weight, as well as a visual analogue scale (VAS), in which participants filled in their subjective pain sensation of the low back.
Statistical analysis
The Spearman correlation coefficient was used for comparing MRI findings and the mobility test, whereas Fisher’s exact test was used for comparing MRI findings with observed motion. The Spearman correlation coefficient was used to compare the different MRI findings amongst each other at each level. In order to elucidate possible effects of pain and the clinical assessors on the results of the mobility tests, the general linear model (GLM) procedure was performed.
Results
Mobility test
The results from the mobility tests for the case and the control groups are shown in Table 1. Student’s t test revealed no statistically significant differences between performances of the two groups.
Table 1.
Results of the mobility tests for case and control groups
| Mobility test | Case | Control | P value (t test) |
|---|---|---|---|
| Modified Schober, N = 110 | 21.5 ± 1.2 (18–24) | 21.6 ± 1.1 (18.5–24.5) | 0.89 (−0.14) |
| Fingertip-to-floor distance, N = 112 | 2.2 ± 7.7 (−9.8–24) | 0.1 ± 8.8 (−18.3–28) | 0.21 (1.27) |
| Lateral bending left, N = 112 | 16.3 ± 2.7 (11.6–22.9) | 16.9 ± 3.0 (11–24.4) | 0.28 (−1.09) |
| Lateral bending right, N = 111 | 15.7 ± 3.0 (10.3–21.9) | 15.9 ± 3.4 (8–24.8) | 0.73 (−0.35) |
| ZEBRIS flexion distance, N = 109 | 5.4 ± 1.1 (2.8–7.9) | 5.5 ± 1.2 (2.4–8.0) | 0.56 (−0.58) |
| ZEBRIS lateral flexion range, N = 96 | 17.1 ± 4.7 (8.0–26.1) | 19.6 ± 8.8 (5.5–50) | 0.11 (−1.59) |
Mean +/− SD (min–max) in cm; N is the number of observations
Expert observation of posture and ROM
Sixteen participants were found to have a hyperlordosis in the physical examination, 67 had a reduced lordosis and 18 had a decompensated scoliosis. Table 2 shows the results of the observed ROM.
Table 2.
Observed range of motion N = 112
| Restrictiona | No restriction | |
|---|---|---|
| Flexion | 19 | 93 |
| Extension | 18 | 94 |
| Right lateral flexion | 24 | 88 |
| Left lateral flexion | 19 | 93 |
aObserved restricted flexion is <60°, restricted extension is <25°, and restricted lateral flexion is <30°
Magnetic resonance imaging
The MRIs of the lumbar motion segments were evaluated for DD, disc form, nerve root compromise, FJO, HIZ and endplate changes. The results are shown in Table 3.
Table 3.
Summary of the MRI readout for each motion segment
| L1-2 | L2-3 | L3-4 | L4-5 | L5-S1 | |
|---|---|---|---|---|---|
| Disc degenerationa | |||||
| Grade 1 | 0 | 0 | 0 | 1 | 0 |
| Grade 2 | 84 | 64 | 54 | 28 | 47 |
| Grade 3 | 21 | 37 | 44 | 51 | 31 |
| Grade 4 | 6 | 7 | 9 | 25 | 17 |
| Grade 5 | 1 | 4 | 5 | 7 | 17 |
| Disc formb | |||||
| Normal | 83 | 66 | 49 | 15 | 40 |
| Bulging | 19 | 28 | 44 | 72 | 33 |
| Protrusion | 7 | 13 | 12 | 14 | 22 |
| Extrusion (sequestration) | 1 (2) | 4 | 7 | 11 | 17 |
| Nerve root compromise (max score from left and right) | |||||
| Normal | – | 5 | 37 | 18 | 55 |
| Contact | 4 | 15 | 60 | 59 | 38 |
| Deviation | – | 3 | 7 | 26 | 16 |
| Compression | – | – | 4 | 9 | 3 |
| Facet joint osteoarthritis (max score from left and right) | |||||
| Normal | 104 | 89 | 34 | 19 | 25 |
| Mild | 8 | 22 | 67 | 59 | 63 |
| Moderate | 0 | 0 | 9 | 28 | 19 |
| Severe | 0 | 1 | 2 | 6 | 5 |
| High intensity zone | 6 | 7 | 13 | 21 | 14 |
| Endplate | |||||
| Normal | 107 | 101 | 93 | 86 | 80 |
| Changed | 5 | 11 | 19 | 26 | 32 |
| Total changes | 160 | 198 | 356 | 443 | 374 |
aDefinition according to Weishaupt et al. [47]
bDisc form: one missing value at L2-3
The two groups did not show any statistical differences with respect to MRI findings. Details were reported elsewhere [42].
Due to the missing differences between cases and controls with respect to mobility tests, clinical observation and MRI findings, we abandoned this division into two groups based on the conditions of the NEW study, and conducted an exploratory analysis in our cohort of working women over 45 years as a whole.
Comparing different segmental MRI criteria
As demonstrated in Table 4, we found highly significant correlations between DD and disc form at all levels. The correlation of DD and FJO was also significant at L1-2, at L2-3 and L4-5. Disc form and FJO correlated significantly at L1-2 and L4-5, and to a lesser extent also at L2-3.
Table 4.
Spearman correlations of disk degeneration, disk form and facet joint osteoarthritis (FJO)
| Disc degeneration disc form | Disc degeneration FJOa | Disc form FJOa | |
|---|---|---|---|
| L1-2 | 0.63** | 0.29** | 0.40** |
| L2-3 | 0.66** | 0.40** | 0.36** |
| L3-4 | 0.58** | 0.27* | 0.23 |
| L4-5 | 0.43** | 0.36** | 0.33** |
| L5-S1 | 0.48** | 0.03 | 0.22 |
*P < 0.01; **P < 0.001
aFacet joint osteoarthritis
Comparing MRI findings and mobility test
The upper lumbar levels, L1-2 to L3-4 had similar findings in the MRIs as did the lower levels with L4-5 having the most degenerative findings overall. As can be expected from an explorative analysis of multiple tests, there will be significant findings by pure chance. To minimize the effect of incidental findings, significance was considered as P ≤ 0.01. Table 5 demonstrates the relationship between the MRI findings at the lumbar levels from L1 to S1 and the mobility tests.
Table 5.
Spearman correlation of MRI findings with mobility tests at different levels (statistically significant correlations only; rho P)
| Level | Mobility test | Influencing pathology | Rho P |
|---|---|---|---|
| L1-2 | |||
| L2-3 | |||
| L3-4 | ZEBRIS flexion distance | Disc form | 0.25** |
| L4-5 | Modified Schober | Disc degeneration | −0.20* |
| Fingertip-to-floor distance | Endplate changes** | 0.36** | |
| L5-S1 | Modified Schober | Endplate changes* | −0.21* |
| Fingertip-to-floor distance | Endplate changes* | 0.20* | |
| Lateral bending right | Disc degeneration** | −0.23* | |
| Nerve root compromise* | −0.23* | ||
| Facet joint osteoarthritis** | −0.25** | ||
| Endplate changes* | −0.23* | ||
| Lateral bending left | Facet joint osteoarthritis* | −0.20* |
*P < 0.05; **P < 0.01
Only occasional statistically significant correlations between MRI findings and the results of the mobility tests could be found. Lateral bending was weakly and negatively correlated to DD and FJO but only on the level of L5-S1. The FTFD showed a weak positive correlation to endplate changes on the level of L4-5. The flexion measured by ZEBRIS showed an isolated statistically significant result with the disc form at L3-4.
Expert observation of posture and ROM
The comparison between the MRI findings and the expert observation revealed several statistically significant relationships.
Observed restriction in flexion was seen with DD at L3-4 (P = 0.008)
An abnormal disk form at L1-2 and L2-3 showed a significant relationship with observed reduced lateral flexion to the right (P = 0.002 and 0.003, respectively), however not to the left. At the level L2-3, a reduction of observed flexion was seen in FJO (P = 0.002) and a reduction of observed extension was seen with endplate changes (P = 0.002). There was a statistically significant relationship between DD of L5-S1 and decompensated scoliosis (P = 0.007). And the observation of a decompensated scoliosis and FJO of L2-3 nearly showed statistically significant correlation (P = 0.017).
Personal characteristics, pain and assessor
We found no correlation between age, height and weight of the subjects with the MRI findings, the mobility tests or the observed ROM in our cohort.
Neither pain history (case and controls, Table 1) nor the actual pain reporting (VAS reported during the mobility tests) correlated with the results of the mobility tests.
The GLM procedure neither showed any statistically significant association between actual pain nor the assessor and the results of the mobility tests. The F values noted between 0.01 (interaction between pain, assessor and lateral bending) and 1.36 (interaction between assessor and Schober). This makes an influence of pain and assessor on the results of the mobility tests unlikely.
Discussion
It was the main purpose of this study to determine the relationship between spinal structures as seen on MRI and mobility tests.
There are several factors that influence spinal ROM. Some studies found gender, age, height, obesity and sitting-to-standing ratio to affect ROM [1, 3, 10, 14, 29, 35], while others could not find any correlation between these factors [11, 24, 29, 30]. ROM is not only affected by anthropometric data but also affected by factors such as pain [11, 29, 30], motivation [7], time of day [11] and sport [5]. Furthermore, from cadaver studies we have learned that motion of the spine is increased to a certain degree of degeneration and decreased beyond that [17, 33, 36, 45]. Ultimately, most of these factors influence the anatomical structures on which motion is dependent. These are the intervertebral disk, the endplates, the facet joints, the joint capsules, the ligaments, the muscles and the soft tissue. Naturally, of the factors mentioned above, only those that can be evaluated on MRI were addressed in this study.
The segmental distribution of the degenerative findings as seen on MRI in our study is comparable to what has been published previously [16, 22, 46, 47]. In general, the two lowest discs show the greatest proportion of degenerated changes in the lumbar spine. The highly significant correlation between the grade of DD and disc form has been published previously [8] and is supported by our data. Normal or bulging discs seldom show advanced degenerative changes while pro- and extruding disc forms were seen more commonly in degenerative discs. Mechanical stress over years may alter the synthesis of matrix protein [40]. This leads to structural changes as we see in DD and weakened or torn fibers as in disc pro-/extrusion. The reason why we could not find a correlation between degeneration and age may be explained by the relatively small age span of our cohort of working women aged 45–63. In this age group, the proportion of degenerative changes is relatively steady [8].
Mobility tests
The modified Schober is one of the most widely used and accepted methods to measure lumbar spinal ROM. Several studies report varying reliability from low [4, 21, 32, 41] to high [14, 20, 28, 31, 44]. Within our study, we did not find any statistically significant correlation between the modified Schober test and MRI findings. Clinical studies have found the reliability of the FTFD ranging from low [31] to high [4, 15, 19, 39]. In our study, the relationship between structural changes of the lumbar spine and the FTFD was only weakly correlated to endplate changes on level L4-5. This may be explained by the fact that the FTFD neither differentiates the movement of the hip from that of the lumbar spine nor does it take into consideration different arm or leg lengths, which may compensate for reduced segmental motion in the low back.
Although lateral bending manoeuvre showed occasional correlation to DD and FJO on the lower lumbar level, lateral bending represents a global assessment of motion, too, and the restrictions on the lateral lumbar spine motion by structural alterations may be too small to influence these measurements.
In order to obtain more specific information on local mobility, the ZEBRIS motion system was used. This system uses ultrasound receivers that are taped to the skin over each lumbar spinal process to record the motion of the spine. Previous studies found no correlation [43] in functional radiographs of the lumbar spine and the ZEBRIS motion analysis. Skin elasticity and varying soft tissue thickness may have lead to some errors in the placement of the transmitters. The tapes used to attach the transmitters to the skin sometimes lay so close to each other that the sticking together of the transmitters could not always be prevented. In an effort to reduce measurement errors, only the change in the distance between the reference transmitter nr. 3 (between spinous process of S2 and S3) and transmitter nr. 8 (L1-2) was considered in our study. The analysis of correlation between the mobility measured by the ZEBRIS system and the MRI findings showed only scattered results.
Although occasional statistically significant correlations between MRI findings and the results of the mobility tests could be found in our study, these correlations are limited to the lower lumbar segments and very weak. Therefore, they are considered to be beyond clinical relevance.
In a review of low back measurements, a considerable lack of information about the reproducibility of functional tests was found [12]. The authors recommend the use only on groups, but found it not to be applicable when single measurements are compared. This conclusion is supported by our data. The validity of the mobility tests with respect to segmental spinal degeneration has to be questioned.
Expert observation of posture and ROM
We found several significant relationships between the ROM that was observed by clinical experts and the MRI results. We found observed lateral flexion to the right to be reduced with an abnormal disc form at the level of L2-3. Cadaver [37, 48] and in vivo [38] studies found the greatest motion of lateral bending to occur at the level L2-3. Any observable reduction in lateral flexion should be most obvious at this level. The fact that we had a significant finding only to the right side, however, may be explained by the influence of the dominant right side most people have. FJO at the level of L2-3 showed a significant relationship to observed reduced flexion and to a lesser extent also to observed reduced extension. This relationship was also seen in cadaver studies [17, 45] and functional radiographs [18]. FJO seems to decrease lumbar motion, but this limitation can only be clinically detected by close observation and only in the upper lumbar spine. We found a significant relationship of observed restriction in extension and endplate changes of L2-3. Since the intervertebral disc in the adult is avascular, the cartilaginous endplate supplies the disc with nutrients by diffusion. Increasing calcification of the endplates reduces permeability, which eventually may lead to the dehydration of the disc [13] and could explain restricted motion. Yet it remains unclear why these changes should only affect extension and why this effect is not seen with DD. The observation of a decompensated scoliosis showed some correlation to the finding of highly degenerated intervertebral disks at L5-S1 and FJO at L2-3. Altered weight bearing forces in scoliosis put increased stress on the spinal structures, leading to abnormal calcification of the endplate, reducing its permeability and decreasing nutrient supply to the disc [2].
There is only one previous study comparing MRI findings with the clinical performance [6]. They looked at the sagittal flexibility of 214 men ranging from 35 to 69 years measured with the flexicurve technique. The MRIs were evaluated for the disc height, disc bulging, signal intensity and presence of osteophyte formation. No attention was paid to the facet joints. The authors found age (20%), disc height (7%), weight (3%) and frequency of low back pain (1%) to predict a total of 31% of the variance in flexibility. The differences in age compared to our study may explain why in their study age was more likely to play a substantial role in flexibility compared to our study. The disc height was evaluated by comparing the disc in question with the disc above. The scores for each disc were then averaged over the upper (T12-L4) and lower (L4-S1) lumbar regions. Despite the relatively small difference in analysis, we cannot support this finding.
Methodical considerations
The NEW study was designed as a case–control study including subjects with and without a history of low back pain working as nurses or secretaries [24]. With respect to the relatively small numbers in the single groups, we decided to merge the groups into one cohort and perform a further exploratory analysis. This may lead to methodical concerns. Nevertheless, the initial groups did not differ concerning mobility tests, clinical and MRI findings and a possible interaction between pain and the result of the mobility test could be excluded.
The effect of low back pain causing decreased flexibility was often attributed to two factors, one being a fear of pain, the other being a behavioural response resulting in tissue adaptation. In our cohort, flexibility was neither influenced by actual pain nor by the pain history. With respect to the central research question, elderly working women were selected and we did not include any acute, relief-seeking patient or patients with chronic disabling pain.
Clinical examinations were conducted by one of the two clinical experts. Clinical expert observation is generally considered to have a low inter-examiner reliability. Therefore, the results concerning clinical examinations should always be treated with some caution. The two examiners involved in this study have been working together for several years and had consensus training on their examination criteria at the beginning and once again during the course of the study and they had been blinded with respect to pain reporting, profession and MRI findings. Despite this efforts to optimize the result, we do not consider it as a systematic approach but as a qualitative comparison to the measured tests. However, this limitation did not interfere with the main purpose of the study.
Neither actual pain, pain history nor age did change any association between MRI findings and mobility in our cohort.
Conclusion
Among the several factors influencing ROM, we looked at the effect of common MRI findings on mobility tests of the lumbar spine. Even though MRI reflects the morphologic alteration of structures that are reported to influence motion in cadavers, there is just a weak relationship between structural changes and the applied mobility tests. More sophisticated mobility tests, such as the ZEBRIS system, do not provide more information than commonly used mobility tests. Furthermore, our findings suggest that clinical observation of spinal motion may provide at least equal information about the influence of spinal structures on motion than the commonly used measured mobility tests do. This may be most likely because the trained eye of an experienced examiner is more sensitive to a regionally reduced motion of the lumbar spine than measurements that are dependent on other factors such as skin elasticity and functionality of other body regions.
Acknowledgments
The authors wish to thank Prof. R. Merletti for managing the European cost shared project NEW (Neuromuscular assessment in the Elderly Worker, contract Nr. QLRT-2000-00139) as well as the Swiss State Secretariat for Education and Research for funding. Furthermore, we wish to thank Leanne Pobjoy for her help with the manuscript. The study was approved by the local ethical commission.
References
- 1.Battie MC, Bigos SJ, Sheehy H, Wortley MD. Spinal flexibility and individual factors that influence it. Phys Ther. 1987;67:653–658. doi: 10.1093/ptj/67.5.653. [DOI] [PubMed] [Google Scholar]
- 2.Bibby SR, Jones DA, Lee RB, Yu J, Urban JPG. The pathophysiology of the intervertebral disc. Joint Bone Spine. 2001;68:537–542. doi: 10.1016/S1297-319X(01)00332-3. [DOI] [PubMed] [Google Scholar]
- 3.Biering-Sorensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine. 1984;9:106–119. doi: 10.1097/00007632-198403000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Burdett RG, Brown KE, Fall MP. Reliability and validity of four instruments for measuring lumbar spine and pelvic positions. Phys Ther. 1986;66:677–684. doi: 10.1093/ptj/66.5.677. [DOI] [PubMed] [Google Scholar]
- 5.Burton AK, Tillotson KM. Does leisure sports activity influence lumbar mobility or the risk of low back trouble? J Spinal Disord. 1991;4:329–336. doi: 10.1097/00002517-199109000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Burton AK, Battie MC, Gibbons L, Videman T, Tillotson KM. Lumbar disc degeneration and sagittal flexibility. J Spinal Disord. 1996;9:418–424. doi: 10.1097/00002517-199610000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Cox ME, Asselin S, Gracovetsky SA, Richards MP, Newman NM, Karakusevic V, Zhong L, Fogel JN. Relationship between functional evaluation measures and self-assessment in nonacute low back pain. Spine. 2000;25:1817–1826. doi: 10.1097/00007632-200007150-00013. [DOI] [PubMed] [Google Scholar]
- 8.DeCandido P, Reinig JW, Dwyer AJ, Thompson KJ, Ducker TB. Magnetic resonance assessment of the distribution of lumbar spine disc degenerative changes. J Spinal Disord. 1988;1:9–15. doi: 10.1097/00002517-198801000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Dickey JP, Pierrynowski MR, Bednar DA, Yang SX. Relationship between pain and vertebral motion in chronic low-back pain subjects. Clin Biomech (Bristol, Avon) 2002;17:345–352. doi: 10.1016/S0268-0033(02)00032-3. [DOI] [PubMed] [Google Scholar]
- 10.Dopf CA, Mandel SS, Geiger DF, Mayer PJ. Analysis of spine motion variability using a computerized goniometer compared to physical examination: a prospective clinical study. Spine. 1994;19:586–595. doi: 10.1097/00007632-199403000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Ensink FB, Saur PM, Frese K, Seeger D, Hildebrandt J. Lumbar range of motion: influence of time of day and individual factors on measurements. Spine. 1996;21:1339–1343. doi: 10.1097/00007632-199606010-00012. [DOI] [PubMed] [Google Scholar]
- 12.Essendrop M, Maul I, Laubli T, Riihimaki H, Schibye B. Measures of low back function: a review of reproducibility studies. Clin Biomech (Bristol, Avon) 2002;17:235–249. doi: 10.1016/S0268-0033(02)00022-0. [DOI] [PubMed] [Google Scholar]
- 13.Ferguson SJ, Steffen T. Biomechanics of the aging spine. Eur Spine J. 2003;12(Suppl 2):S97–S103. doi: 10.1007/s00586-003-0621-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fitzgerald GK, Wynveen KJ, Rheault W, Rothschild B. Objective assessment with establishment of normal values for lumbar spinal range of motion. Phys Ther. 1983;63:1776–1781. doi: 10.1093/ptj/63.11.1776. [DOI] [PubMed] [Google Scholar]
- 15.Frost M, Stuckey S, Smalley LA, Dorman G. Reliability of measuring trunk motions in centimeters. Phys Ther. 1982;62:1431–1437. doi: 10.1093/ptj/62.10.1431. [DOI] [PubMed] [Google Scholar]
- 16.Fujiwara A, Tamai K, Yamato M, An HS, Yoshida H, Saotome K, Kurikashi A. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J. 1999;8:396–401. doi: 10.1007/s005860050193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fujiwara A, Lim TH, An HS, Tanaka N, Jeon CH, Andersson GB, Haughton VM. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine. 2000a;25:3036–3044. doi: 10.1097/00007632-200012010-00011. [DOI] [PubMed] [Google Scholar]
- 18.Fujiwara A, Tamai K, An HS, Kurikashi A, Lim TH, Yoshida H, Saotome K. The relationship between disc degeneration, facet joint osteoarthritis, and stability of the degenerative lumbar spine. J Spinal Disord. 2000b;13:444–450. doi: 10.1097/00002517-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Gauvin MG, Riddle DL, Rothstein JM. Reliability of clinical measurements of forward bending using the modified fingertip-to-floor method. Phys Ther. 1990;70:443–447. doi: 10.1093/ptj/70.7.443. [DOI] [PubMed] [Google Scholar]
- 20.Gill K, Krag MH, Johnson GB, Haugh LD, Pope MH. Repeatability of four clinical methods for assessment of lumbar spinal motion. Spine. 1988;13:50–53. doi: 10.1097/00007632-198801000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Hyytiainen K, Salminen JJ, Suvitie T, Wickstrom G, Pentti J. Reproducibility of nine tests to measure spinal mobility and trunk muscle strength. Scand J Rehabil Med. 1991;23:3–10. [PubMed] [Google Scholar]
- 22.Jarvik JJ, Hollingworth W, Heagerty P, Haynor DR, Deyo RA. The longitudinal assessment of imaging and disability of the back (LAIDBack) study: baseline data. Spine. 2001;26:1158–1166. doi: 10.1097/00007632-200105150-00014. [DOI] [PubMed] [Google Scholar]
- 23.Kaigle AM, Wessberg P, Hansson TH. Muscular and kinematic behavior of the lumbar spine during flexion-extension. J Spinal Disord. 1998;11:163–174. [PubMed] [Google Scholar]
- 24.Laubli T, Hermens H, SjØgaard G. Neuromuscular assessment of the elderly worker, NEW: a multidisciplinary European research project. Eur J Appl Physiol. 2006;96(2):107–109. doi: 10.1007/s00421-005-0045-0. [DOI] [PubMed] [Google Scholar]
- 25.Loebl WY. Measurement of spinal posture and range of spinal movement. Ann Phys Med. 1967;9:103–110. doi: 10.1093/rheumatology/9.3.103. [DOI] [PubMed] [Google Scholar]
- 26.Lund T, Nydegger T, Schlenzka D, Oxland TR. Three-dimensional motion patterns during active bending in patients with chronic low back pain. Spine. 2002;27:1865–1874. doi: 10.1097/00007632-200209010-00012. [DOI] [PubMed] [Google Scholar]
- 27.Macrae IF, Wright V. Measurement of back movement. Ann Rheum Dis. 1969;28:584–589. doi: 10.1136/ard.28.6.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCombe PF, Fairbank JC, Cockersole BC, Pynsent PB. 1989 Volvo award in clinical sciences. Reproducibility of physical signs in low-back pain. Spine. 1989;14:908–918. doi: 10.1097/00007632-198909000-00002. [DOI] [PubMed] [Google Scholar]
- 29.McGregor AH, Dore CJ, McCarthy ID, Hughes SP. Are subjective clinical findings and objective clinical tests related to the motion characteristics of low back pain subjects? J Orthop Sports Phys Ther. 1998;28:370–377. doi: 10.2519/jospt.1998.28.6.370. [DOI] [PubMed] [Google Scholar]
- 30.Mellin G. Correlations of spinal mobility with degree of chronic low back pain after correction for age and anthropometric factors. Spine. 1987;12:464–468. doi: 10.1097/00007632-198706000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Merritt JL, McLean TJ, Erickson RP, Offord KP. Measurement of trunk flexibility in normal subjects: reproducibility of three clinical methods. Mayo Clin Proc. 1986;61:192–197. doi: 10.1016/s0025-6196(12)61848-5. [DOI] [PubMed] [Google Scholar]
- 32.Miller SA, Mayer T, Cox R, Gatchel RJ. Reliability problems associated with the modified Schober technique for true lumbar flexion measurement. Spine. 1992;17:345–348. doi: 10.1097/00007632-199203000-00017. [DOI] [PubMed] [Google Scholar]
- 33.Mimura M, Panjabi MM, Oxland TR, Crisco JJ, Yanamoto I, Vasavada A. Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine. 1994;19:1371–1380. doi: 10.1097/00007632-199406000-00011. [DOI] [PubMed] [Google Scholar]
- 34.Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166:193–199. doi: 10.1148/radiology.166.1.3336678. [DOI] [PubMed] [Google Scholar]
- 35.Moll JM, Wright V. Normal range of spinal mobility. An objective clinical study. Ann Rheum Dis. 1971;30:381–386. doi: 10.1136/ard.30.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nachemson AL, Schultz AB, Berkson MH. Mechanical properties of human lumbar spine motion segments. Influence of age, sex, disc level, and degeneration. Spine. 1979;4:1–8. doi: 10.1097/00007632-197901000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Panjabi MM, Oxland TR, Yamamoto I, Crisco JJ. Mechanical behavior of the human lumbar and lumbosacral spine as shown by three-dimensional load–displacement curves. J Bone Joint Surg Am. 1994;76:413–424. doi: 10.2106/00004623-199403000-00012. [DOI] [PubMed] [Google Scholar]
- 38.Pearcy MJ, Tibrewal SB. Axial rotation and lateral bending in the normal lumbar spine measured by three-dimensional radiography. Spine. 1984;9:582–587. doi: 10.1097/00007632-198409000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Perret C, Poiraudeau S, Fermanian J, Colau MM, Benhamou MA, Revel M. Validity, reliability, and responsiveness of the fingertip-to-floor test. Arch Phys Med Rehabil. 2001;82:1566–1570. doi: 10.1053/apmr.2001.26064. [DOI] [PubMed] [Google Scholar]
- 40.Rannou F, Corvol M, Revel M, Poiradeau S. Disk degeneration and disk herniation: the contribution of mechanical stress. Joint Bone Spine. 2001;68:543–546. doi: 10.1016/S1297-319X(01)00325-6. [DOI] [PubMed] [Google Scholar]
- 41.Reynolds PM. Measurement of spinal mobility: a comparison of three methods. Rheumatol Rehabil. 1975;14:180–185. doi: 10.1093/rheumatology/14.3.180. [DOI] [PubMed] [Google Scholar]
- 42.Schenk P, Laeubli T, Hodler J, Klipstein A. MRI of the lumbar spine in nurses and secretaries. Do light static and heavy dynamic work matter? Spine. 2006;31:12701–1706. doi: 10.1097/01.brs.0000244570.36954.17. [DOI] [Google Scholar]
- 43.Schreiber T. Vergleich von 3D-Bewegungsanalysen und Röntgenfunktionsaufnahmen bei Patienten mit Verdacht auf segementale Instabilität der Lendenwirbelsäule. Phys Med Rehab Kurort. 2001;11:113–122. doi: 10.1055/s-2001-16443. [DOI] [Google Scholar]
- 44.Strender LE, Lundin M, Nell K. Interexaminer reliability in physical examination of the neck. J Manipulative Physiol Ther. 1997;20:516–520. [PubMed] [Google Scholar]
- 45.Tanaka N, An HS, LIM TH, Fujiwara A, Jeon CH, Haughton VM. The relationship between disc degeneration and flexibility of the lumbar spine. Spine J. 2001;1:47–56. doi: 10.1016/S1529-9430(01)00006-7. [DOI] [PubMed] [Google Scholar]
- 46.Toyone T, Takahashi K, Kitahara H, Yamagata M, Murakami M, Moriya H. Vertebral bone-marrow changes in degenerative lumbar disc disease. An MRI study of 74 patients with low back pain. J Bone Joint Surg Br. 1994;76:757–764. [PubMed] [Google Scholar]
- 47.Weishaupt D, Zanetti M, Hodler J, Boos N. MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology. 1998;209:661–666. doi: 10.1148/radiology.209.3.9844656. [DOI] [PubMed] [Google Scholar]
- 48.Yamamoto I, Panjabi MM, Crisco JJ, Thibodeau L, Yanamoto I. Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine. 1989;14:1256–1260. doi: 10.1097/00007632-198911000-00020. [DOI] [PubMed] [Google Scholar]