Abstract
Sagittal curvatures of the spine can be assessed using the constrained or non-constrained Cobb techniques. However, there is no study that specifically compares these two techniques. The objective of this study is to assess the reproducibility and clinical relevance of the non-constrained Cobb technique (non-constrained limit vertebrae) compared to the constrained Cobb technique (constrained limit vertebrae). Standing sagittal radiographs of the spine of ten adolescents with idiopathic scoliosis, ten adolescents with spondylolisthesis and ten normal adolescents were selected. Thoracic kyphosis (TK) and lumbar lordosis (LL) were measured twice by three observers using both constrained and non-constrained Cobb techniques. Pearson’s correlation coefficients, as well as intra- and inter-observer intra-class correlation coefficients (ICC) were calculated. Inter-observer ICCs were similar for TK and LL with both techniques, ranging from 0.84 to 0.89. Intra-observer ICCs for both techniques were between 0.74 and 0.92 for TK, while they were between 0.87 and 0.97 for LL. The two techniques were highly correlated for the measurement of the TK (r = 0.96) and LL (r = 0.94). Computer-assisted assessment of the sagittal profile using the non-constrained Cobb technique provides excellent reproducibility. As opposed to the constrained Cobb technique, the non-constrained Cobb technique takes into account the variability in the level of transition between the TK and LL. However, adequate use of this technique requires accurate identification of the limit vertebrae in the thoracolumbar spine. Consequently, a computer-assisted technique is recommended when using the non-constrained Cobb technique.
Keywords: Lumbar lordosis, Thoracic kyphosis, Posture, Reproducibility, Radiographic analysis, Sagittal balance, Spine
Introduction
The modified Cobb technique, inspired from the technique originally developed by Cobb [2] to assess the magnitude of scoliosis, is the most widely used technique to evaluate the thoracic kyphosis (TK) and lumbar lordosis (LL) from sagittal radiographs. The use of constrained limit vertebrae (constrained Cobb technique) is most commonly used. However, there is a high variability in the literature concerning the level of the limit vertebrae selected to measure constrained TK and LL. TK values have been reported using various constrained levels such as T1–T12 [6, 7, 10], T2–T12 [12], T3–T12 [1, 20] and T4–T12 [3, 15, 16]. LL has been measured from T12–L5 [13], T12–S1 [8, 11–13, 20], L1–L5 [1, 3, 8, 13], L1–S1 [6, 10, 13] and L2–S1 [5]. Up to now, there is no consensus in the literature on the optimal limit vertebrae to select for the measurement of constrained TK and LL.
Some authors [18, 21] have also used a non-constrained level for the limit vertebra in the thoracolumbar spine (non-constrained Cobb technique), which corresponds to the most tilted vertebra that separates the TK and LL. This vertebra is therefore used as the lower limit vertebra for the measurement of the TK and as the upper limit vertebra for the measurement of the LL, and allows the measurement of the maximal Cobb angle for TK and LL. This concept is in accordance with the original technique developed by Cobb [2], for which the limit vertebrae correspond to the most tilted vertebrae for the measurement of scoliosis on frontal plane radiographs. Also, as opposed to the constrained Cobb technique, the non-constrained Cobb technique allows complete evaluation of the entire kyphotic and lordotic segments of the spine because it takes into account the variability in length of the TK and LL. Accordingly, Vaz et al. [19] have shown that for normal individuals, the number of kyphotic and lordotic vertebral units can vary significantly.
Although there are some theoretical advantages to the use of the non-constrained Cobb technique, recent data have shown a poor inter-observer reproducibility for the manual selection of end vertebrae for scoliosis measurements [14] and suggests that the situation may be the same for sagittal plane measurements. The constrained method remains the most popular and there is no evidence in the literature confirming that measurements obtained with both techniques are comparable. This study introduces a computer-assisted technique for the assessment of TK and LL. It also compares the reproducibility and clinical relevance of the constrained and non-constrained Cobb techniques. These two techniques are evaluated for normal adolescents, as well as for subjects with adolescent idiopathic scoliosis (AIS) and with developmental spondylolisthesis.
Materials and methods
The study design was based on the recommendations of Harrison et al. [8] intended to standardize reliability studies for measurements of radiographic parameters. Accordingly, the current study involves 30 radiographs, three observers and two measuring sessions.
Sample description
Standing lateral radiographs of the spine of ten normal subjects, ten subjects with AIS and ten subjects with L5–S1 developmental spondylolisthesis were randomly selected. None of the patients included in this study had a history or clinical signs of hip, pelvic or lower limb disorder. All radiographs were denominalized and were taken under the same conditions: in an upright position, with the upper limbs in the fists-on-clavicle position, and the hips and knees fully extended [4, 9]. The left lateral radiographs were taken on 30 × 90 cm digital cassettes, ensuring that the two femoral heads and part of the cervical spine were included. All radiographs were stored in digital format for the measurement process.
The mean age for the normal group (6 girls, 4 boys) was 14.6 ± 3.5 years. There were eight girls and two boys with AIS, and the mean age in this group was 15.1 ± 3.6 years. All subjects with AIS presented a double structural thoracic and lumbar curve pattern. The mean Cobb angle for the major scoliotic curve was 56.4 ± 13.1° (range 36.7°– 78.7°). As for subjects with spondylolisthesis, there were six girls and four boys, and the mean age was 14.2 ± 4.0 years. This group was composed of four subjects with Meyerding grade 1 slip, three with grade 2 slip, two with grade 3 slip and one with grade 4 slip.
Measurement technique
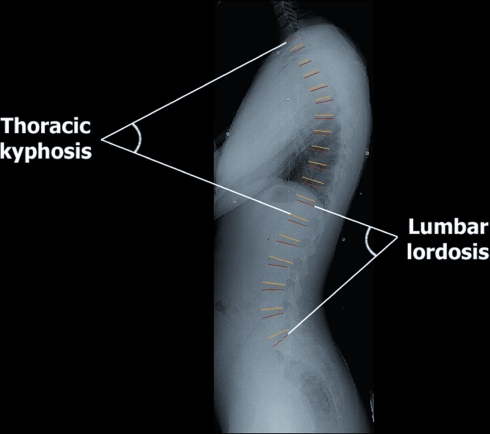
Two techniques of measurement were used to assess the TK and LL: the constrained Cobb technique and the non-constrained Cobb technique. All digital radiographs were assessed using the SpineView software (Surgiview, France) [11, 12]. Although only digital radiographs are used in our institution, images scanned from standard radiographs can also be used with the software. As requested by the software, all observers trace a best-fit line of all vertebral endplates from the superior endplate of T1 to the superior endplate of S1 on each measured radiograph (Fig. 1). Digitization of all vertebral endplates allows subsequent calculation of both the constrained and non-constrained techniques. In the current study, the constrained and non-constrained Cobb values were extracted from the same digitization process (from T1 to S1) on each radiograph. About 3 min is required to identify all vertebral endplates. The software automatically provides the orientation of all identified vertebral endplates with respect to the horizontal (Fig. 1), so that a Cobb angle can be calculated between any two vertebral endplates. For the current study, calculation of constrained and non-constrained Cobb angles based on the orientation of the vertebral endplates was performed by one of the authors using another software (Microsoft Excel, Microsoft Corporation, USA).
Fig. 1.
Measurements using the SpineView software. All vertebral endplates from T1 to S1 are identified by the user. Then, the software automatically provides the orientation of all identified vertebral endplates with respect to the horizontal in a new window. These data can then be copied and processed in any software in order to calculate the constrained and non-constrained Cobb angle between any two vertebral endplates
For each subject, the TK and the LL were measured using both the constrained and the non-constrained Cobb techniques from the orientation of the vertebral endplates automatically provided by the software. For the constrained Cobb technique, the TK was measured between the superior endplate of T1 and the inferior endplate of T12, while the LL was measured between the superior endplate of L1 and the superior endplate of S1.
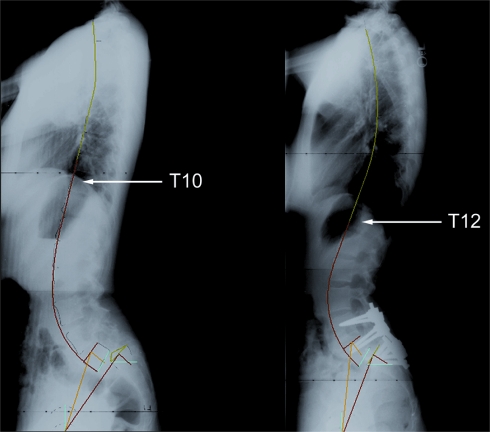
To assess the TK using the non-constrained Cobb technique (Fig. 2), all Cobb angles between the superior endplate of T1 and the inferior endplate of T2 to L5 were calculated, because the level of the most tilted vertebra separating the TK and LL is not known a priori. The maximum Cobb angle value corresponds to the TK value for the non-constrained Cobb technique. Similarly, all Cobb angles between the superior endplate of S1 and the superior endplate of T1 to L5 were calculated. The maximum Cobb angle value corresponds to the LL value for the non-constrained Cobb technique. The lower limit vertebra of the TK was always the same as the upper limit vertebra of the LL in the current study. In cases where the limit vertebrae are different, we recommend that the TK and LL be measured using the same limit vertebra that is associated with the maximal value for the sum of the TK and LL. For example, if the most tilted inferior endplate is T11 and the most tilted superior endplate is T12, then TK and LL are measured sequentially for T11 and T12. First using the T11 limit vertebra, the TK value measured between the superior endplate of T1 and the inferior endplate of T11 is summed with the LL value measured between the superior endplate of T11 and the superior endplate of S1. Then, the same process is done using T12 as the limit vertebra. The proper limit vertebra (with the proper TK and LL values) is that for which the sum of the TK and LL is maximum. The computer-assisted technique is different from the conventional manual technique in which the clinician has to select himself the limit vertebra.
Fig. 2.
In the non-constrained Cobb technique, the lumbar lordosis is assessed from the superior endplate of S1 to the superior endplate of the most tilted vertebra in the thoracolumbar region, while the thoracic kyphosis is assessed from the superior endplate of T1 to the inferior endplate of the most tilted vertebra in the thoracolumbar region
Measurement of the TK and LL using the constrained and non-constrained Cobb techniques was performed by three observers having different levels of experience (an experienced spine surgeon, an orthopedic resident and a medical student). The three observers assessed the TK and LL for all 30 subjects using both techniques in order to evaluate the inter-observer reproducibility of each technique. Assessment of the TK and LL was repeated one week later by each observer, in order to assess the intra-observer reproducibility of the constrained and non-constrained Cobb techniques.
Data analysis
The mean values and standard deviations for TK and LL were calculated for each technique. Pearson’s correlation studies between the two techniques and comparisons using paired Student t tests were also performed. As an error analysis, mean absolute differences of observers’ measurements were also assessed, with the associated 95% confidence interval. All these previous results were determined from the data of the first acquisition session only. Correlation between the two acquisition sessions was assessed using Pearson’s coefficient. Finally, the intra- and inter-observer reproducibility of each technique was calculated using single measure intra-class correlation coefficient (ICC) with a two-way random effects model (absolute agreement definition). The inter-observer ICC was calculated from the data of the first acquisition session only. The intra-observer ICC was calculated for each observer from the data of the two acquisition sessions. The level of significance was set at 0.05.
Results
Mean values and standard deviations for TK and LL, as well as mean absolute differences of observers’ measurements and the associated 95% confidence interval are presented in Tables 1 and 2, respectively. The non-constrained Cobb technique gave significantly higher values of TK (P < 10−22) and LL (P < 10−15), but they were strongly correlated with those obtained with the constrained Cobb technique for TK (r = 0.96) and for LL (0.94). Both techniques provided similar strong correlation coefficients between the two acquisition sessions. The correlation coefficient for LL measurements between the two acquisition sessions was 0.93 and 0.94 for the constrained and non-constrained Cobb techniques, respectively. It was 0.84 and 0.84 for the constrained and non-constrained measurement of the TK, respectively.
Table 1.
Measurement of thoracic kyphosis using the constrained and non-constrained Cobb techniques
| Measuring technique | Thoracic kyphosis (±standard deviation) | Mean absolute difference of three observers | Confidence interval (95%) |
|---|---|---|---|
| Non-constrained Cobb | 39.9 ± 12.0° | 4.5° | 2.6°–6.4° |
| Constrained Cobb | 34.7 ± 12.4° | 5.2° | 3.4°–6.9° |
Table 2.
Measurement of lumbar lordosis using the constrained and non-constrained Cobb techniques
| Measuring technique | Lumbar lordosis (±standard deviation) | Mean absolute difference of three observers | Confidence interval (95%) |
|---|---|---|---|
| Non-constrained Cobb | 68.1 ± 16.7° | 3.4° | 1.8°–5.0° |
| Constrained Cobb | 61.6 ± 13.9° | 3.7° | 2.3°–5.1° |
Table 3 and 4 present the results from the reproducibility study, indicating that both techniques provide similar intra- and inter-observer reproducibility. Concerning the intra-observer reproducibility, there is no obvious relationship with the observer’s clinical experience. Intra-observer ICCs varied between 0.74 and 0.92 for the measurement of TK, while they were between 0.87 and 0.97 for the measurement of LL. Globally, intra-observer ICCs were higher for the measurement of LL. Inter-observer ICCs were similar for TK and LL, ranging from 0.84 to 0.89. For the measurement of LL, inter-observer ICCs were lower than intra-observer ICCs, while there was no particular relationship between intra- and inter-observer ICCs for the measurement of TK.
Table 3.
Intra-observer reproducibility of the constrained and non-constrained Cobb techniques for each observer based on intra-class correlation coefficients (95% confidence interval)
| Measuring technique | Thoracic kyphosis | Lumbar lordosis | ||||
|---|---|---|---|---|---|---|
| Observer 1 | Observer 2 | Observer 3 | Observer 1 | Observer 2 | Observer 3 | |
| Non-constrained Cobb | 0.74 (0.49–0.87) | 0.90 (0.79–0.95) | 0.92 (0.84–0.96) | 0.97 (0.94–0.99) | 0.97 (0.93–0.98) | 0.90 (0.80–0.95) |
| Constrained Cobb | 0.80 (0.60–0.90) | 0.81 (0.65–0.91) | 0.92 (0.83–0.96) | 0.95 (0.90–0.98) | 0.96 (0.91–0.98) | 0.87 (0.72–0.94) |
Table 4.
Inter-observer reproducibility of the constrained and non-constrained Cobb techniques based on intra-class correlation coefficients (95% confidence interval)
| Measuring technique | Thoracic kyphosis | Lumbar lordosis |
|---|---|---|
| Non-constrained Cobb | 0.89 (0.80–0.94) | 0.87 (0.75–0.93) |
| Constrained Cobb | 0.84 (0.74–0.92) | 0.84 (0.70–0.92) |
Discussion
As previously suggested by Vaz et al. [19], the level of transition between the TK and LL can vary widely in the normal young adult population. In their study population, they reported that the length of the spinal kyphotic segment varied between 6 and 13 vertebrae, while the lordotic segment spanned between 1 to 6 vertebrae. Treatment of spinal disorders, such as spondylolisthesis, can also have a significant effect on the length of the TK and LL (Fig. 3). This is the reason why the use of the non-constrained Cobb technique can be appealing. On the opposite side, the constrained Cobb technique does not always allow to assess the entire kyphotic and lordotic segments of the spine, such as for cases where part of the kyphotic segment extends into the lumbar spine or vice versa. This explains why the non-constrained Cobb technique consistently gave higher mean values than the constrained Cobb technique for TK and LL, but there was nevertheless a strong correlation between both techniques, confirming that measurements with the non-constrained Cobb technique vary in the same fashion as with the constrained Cobb technique.
Fig. 3.
Pre- and post-operative lateral radiographs of a patient with developmental spondylolisthesis. Pre-operatively, the patient has a kyphotic segment that spans from T1 to T10 and a lordotic segment from T10 to S1. Post-operatively, the kyphosis is from T1 to T12 and the lordosis is from T12 to S1
The present study specifically evaluated if the reproducibility of the non-constrained Cobb technique was similar to that of the constrained Cobb technique. Based on Shrout and Fleiss criteria for reproducibility testing (poor, ICC < 0.40; fair to good, ICC 0.40 to 0.75; excellent, ICC > 0.75) [17], intra- and inter-observer reproducibility was excellent for both techniques. Harrison et al. [7, 8] obtained even higher ICCs (between 0.94 and 0.99) for the constrained Cobb technique in their reproducibility study on adult subjects. The authors believe that this is related to the fact that the current study included subjects with AIS and spondylolisthesis, in addition to normal adolescents. Identification of vertebral endplates is more difficult in pediatric than in adult subjects. Accurate identification of vertebral endplates is also more difficult in subjects with AIS because vertebrae are superimposed and rotated when viewed on the lateral radiograph. This is particularly true for AIS subjects in this study because they all had a double structural thoracic and lumbar curve pattern. As for subjects with high-grade spondylolisthesis, remodeling and doming of S1 adds to the complexity of accurately identifying the S1 upper endplate.
For both constrained and non-constrained Cobb techniques, intra-observer reproducibility appeared slightly better for the measurement of LL than for the measurement of TK. This may be due to the decreased visibility of the thoracic spine, which can be associated with inadequate identification or digitization of T1.
One main concern related to the use of the non-constrained Cobb technique is the accurate identification of the most inclined vertebra that separates the TK and the LL. As reported by Potter et al. [14] for coronal radiographs of scoliotic spines, manual identification of the end vertebrae can be difficult and highly dependent on observer experience. Accordingly, they have shown that this task can be associated with poor inter-observer reliability (Kappa correlation coefficient of 0.3) despite high intra-observer reliability (Kappa correlation coefficient between 0.69 and 0.88). We believe that this problem could have been even worse in the current study since identification of the most tilted vertebrae is more difficult on lateral radiographs due to poorer visibility of anatomical landmarks. On the contrary, our results demonstrate that observer experience has no obvious influence on the intra-observer reproducibility for the non-constrained Cobb technique. In addition, we found no discrepancy between the intra- and inter-observer reproducibility, which is in sharp contrast with the results of Potter et al. [14]. We believe these findings are mainly explained by the use of a computer-assisted technique in the present study, which ensured more accurate and reproducible identification of the most inclined vertebra for the non-constrained Cobb technique. The conventional manual technique [18, 21] can be associated with significant errors because the clinician calculates the TK and LL based on a limit vertebra that appears to be the most inclined vertebra that separates the TK and LL. As suggested by Potter et al. [14], inter-observer discrepancy with the conventional technique is related to the “level of ambiguity” that occurs when two or more vertebrae have a similar orientation. In this situation, each clinician tends to use his own judgment and experience to select the limit vertebra. Each clinician will tend to reproduce his personal method of selecting the limit vertebra, thereby resulting in good intra-observer reproducibility. However, different clinicians will have different methods of selecting the limit vertebra, so that the inter-observer reproducibility can be worse. The computer-assisted technique eliminates this “level of ambiguity” because the user digitizes all vertebral endplates and the software automatically calculates their orientation with respect to a horizontal line. Since the orientation of all vertebral endplates is provided by the software, it becomes easy to identify the proper limit vertebra.
Therefore, the authors strongly recommend a computer-assisted technique when using the non-constrained Cobb technique. Although this process can be more time-consuming than the manual method, it provides adequate intra- and inter-observer reproducibility for the measurement of TK and LL. While all vertebral endplates from T1 to S1 were digitized in this study, the time required to accurately identify the most tilted vertebra could be minimized if only a limited number of vertebrae in the thoracolumbar segment were digitized. The software could also be easily implemented in order to automatically calculate the maximal Cobb angle after the identification of the vertebral endplates, without the need of post-processing the data as in the current study. Alternatively for those who already use a digital radiograph system allowing on-screen angular measurements, the user could sequentially measure the TK and LL using different limit vertebrae (for example the three most inclined vertebrae selected visually) in order to obtain the maximal TK and LL values.
Conclusion
This study demonstrates that the reproducibility of the non-constrained Cobb technique is similar to that of the more widely used constrained Cobb technique. However, as opposed to the constrained Cobb technique, the non-constrained Cobb technique has the important advantage of taking into account the variability in the level of transition between the TK and LL, thus allowing a better evaluation of the full magnitude of the sagittal curves of the spine. A computer-assisted technique is however recommended when using the non-constrained Cobb technique in order to ensure adequate intra- and inter-observer reproducibility.
Acknowledgments
The authors sincerely thank Surgiview (Paris, France) for providing the Spineview software.
Footnotes
A reviewer’s comment on this paper is available at http://dx.doi.org/10.1007/00586-007-0315-0.
References
- 1.Bernhardt M, Bridwell KH. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989;14:717–721. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Cobb JR. Outline for the study of scoliosis. Instr Course Lect. 1948;5:261–275. [Google Scholar]
- 3.Jonge T, Dubousset J, Illés T. Sagittal plane correction in idiopathic scoliosis. Spine. 2002;27:754–761. doi: 10.1097/00007632-200204010-00013. [DOI] [PubMed] [Google Scholar]
- 4.Faro FD, Marks MC, Pawelek J, et al. Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine. 2004;29:2284–2289. doi: 10.1097/01.brs.0000142224.46796.a7. [DOI] [PubMed] [Google Scholar]
- 5.Fernand R, Fox DE. Evaluation of lumbar lordosis: a prospective and retrospective study. Spine. 1985;10:799–803. doi: 10.1097/00007632-198511000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Hammerberg EM, Wood KB. Sagittal profile of the elderly. J Spinal Disord. 2003;16:44–50. doi: 10.1097/00024720-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Harrison DE, Cailliet R, Harrison DD, et al. Reliability of centroid, Cobb, and posterior tangent methods: which to choose for analysis of thoracic kyphosis. Spine. 2001;26:E227–E234. doi: 10.1097/00007632-200106010-00002. [DOI] [PubMed] [Google Scholar]
- 8.Harrison DE, Harrison DD, Caillet R, et al. Radiographic analysis of lumbar lordosis: centroïd, Cobb, TRALL, and Harrison posterior tangent methods. Spine. 2001;26:E235–E242. doi: 10.1097/00007632-200106010-00003. [DOI] [PubMed] [Google Scholar]
- 9.Horton WC, Brown CW, Bridwell KH, et al. Is there an optimal patient stance for obtaining a lateral 36″ radiograph? Spine. 2005;30:427–433. doi: 10.1097/01.brs.0000153698.94091.f8. [DOI] [PubMed] [Google Scholar]
- 10.Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex and size. A prospective controlled clinical study. Spine. 1994;14:1611–1618. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 11.Korovessis P, Dimas A, Iliopoulos P, et al. Correlative analysis of lateral vertebral radiographic variables and medical outcomes study short-form health survey. J Spinal Disord. 2002;15:384–390. doi: 10.1097/00024720-200210000-00007. [DOI] [PubMed] [Google Scholar]
- 12.O’Brien MF, Kuklo TR, Blanke KM et al (2004) Spinal deformity study group. Radiographic measurement manual. Medtronic Sofamor Danek, USA
- 13.Polly DW, Jr, Kilkelly FX, McHale KA, et al. Measurement of lumbar lordosis: evaluation of intraobserver, interobserver, and technique variability. Spine. 1996;21:1530–1535. doi: 10.1097/00007632-199607010-00008. [DOI] [PubMed] [Google Scholar]
- 14.Potter BK, Rosner MK, Lehman RA, Jr, et al. Reliability of end, neutral and stable vertebrae identification in adolescent idiopathic scoliosis. Spine. 2005;30:1658–1663. doi: 10.1097/01.brs.0000170290.05381.9a. [DOI] [PubMed] [Google Scholar]
- 15.Rajnics P, Pomero V, Templier A, et al. Computer-assisted assessment of spinal sagittal plane radiographs. J Spinal Disord. 2001;14:135–142. doi: 10.1097/00002517-200104000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Rillardon L, Levassor N, Guigui P, et al. Validation of a tool to measure pelvic and spinal parameters of sagittal balance. Rev Chir Orthop Reparatrice Appar Mot. 2003;89:218–227. [PubMed] [Google Scholar]
- 17.Shrout PE, Fleiss JL. Intraclass correlation: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 18.Stagnara P, Mauroy JC, Dran G, et al. Reciprocal angulation of vertebral bodies in the sagittal plane: approach to references for the evolution of kyphosis and lordosis. Spine. 1982;7:335–342. doi: 10.1097/00007632-198207000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Vaz G, Roussouly P, Berthonnaud E, et al. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11:80–87. doi: 10.1007/s005860000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vedantam R, Lenke LG, Keeney JA, et al. Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults. Spine. 1998;23:211–215. doi: 10.1097/00007632-199801150-00012. [DOI] [PubMed] [Google Scholar]
- 21.Voutsinas SA, MacEwen GD. Sagittal profiles of the spine. Clin Orthop. 1986;210:235–242. [PubMed] [Google Scholar]